Abstract
Background
As the coronavirus disease 2019 (COVID‐19) pandemic continues to spread, it remains unclear how vulnerable populations with preexisting health conditions like cancer have been affected.
Methods
Between July and September of 2020, the authors conducted a cross‐sectional study that surveyed 2661 patients with breast cancer who were registered in the Chicago Multiethnic Epidemiologic Breast Cancer Cohort and received 1300 responses (71.5% White patients and 22.4% Black patients). The survey measured the psychosocial well‐being of participants before and during the COVID‐19 pandemic and examined whether they experienced any type of financial challenges or treatment disruption.
Results
The results indicated that feelings of isolation increased significantly during the pandemic. Meanwhile, the overall median isolation/stress score was 1.2 on a scale from 0 (never) to 4 (always), which was not significantly different between White patients and Black patients. One‐third of patients experienced some type of financial challenge during this time. Medicaid recipients, of whom almost 80% were Black, were more likely to experience financial challenges. In addition, approximately one‐fourth of patients experienced difficulty getting treatment.
Conclusions
This study indicates that the quality of life of patients with breast cancer and their scheduled treatments have been adversely affected during the COVID‐19 pandemic. These findings suggest that more support should be provided by hospital centers and the medical research community to patients with cancer during this challenging pandemic.
Lay Summary
The authors surveyed patients with breast cancer in Chicago using a questionnaire to examine how their lives have been affected during the coronavirus disease 2019 (COVID‐19) pandemic.
The results indicate that the lives of patients with breast cancer and their scheduled treatments have been adversely affected during the pandemic.
In addition, patients who were covered by Medicaid, most of whom were Black, were more likely to experience financial challenges.
The findings suggest that hospital centers and the medical research community should reach out and provide more information to support patients with cancer during this challenging pandemic.
Keywords: breast cancer, coronavirus disease 2019 (COVID‐19), epidemiology, quality of life, racial disparities
Short abstract
The quality of life of patients with breast cancer and their scheduled treatments have been adversely affected during the coronavirus disease 2019 pandemic. The findings also suggest that more support should be provided by hospital centers and the medical research community to patients with cancer during this challenging pandemic.
Introduction
As the coronavirus disease 2019 (COVID‐19) pandemic continues, a growing concern is how the global pandemic has been affecting vulnerable populations with preexisting health conditions such as cancer. In this regard, studies have been conducted to assess the adverse effects of cancer on COVID‐19 incidence rates and survival outcomes. These studies found that patients with cancer overall were more vulnerable to COVID‐19 infection, especially those with hematologic and lung cancers. 1 , 2 The studies also indicated that patients with cancer, including both those undergoing active treatment and survivors, had a higher risk of severe complications once they were infected because of underlying malignancy, treatment‐related immunosuppression, and/or increased comorbidities. 1 , 3 , 4
Although several studies have examined the clinical outcomes of patients who have cancer associated with COVID‐19, few have investigated these patients' psychosocial health and financial burden during the pandemic, factors that also play a crucial role in their quality of life after a cancer diagnosis. 5 , 6 , 7 Particularly for breast cancer, it has also been well established that racial disparities exist in prognosis and survival, with Black women more likely to be diagnosed with breast cancers that have poorer prognostic features and experiencing higher mortality rates. 8 , 9 , 10 Adding to existing racial disparities in cancer mortality rates are new data revealing profound racial differences in COVID‐19 cases and deaths. 11 , 12 According to the Centers for Disease Control and Prevention, African Americans comprised one‐third of the total COVID‐19 hospitalizations while only accounting for 18% of the population in the 14 states studied. 13 Whether patients with cancer in racial and ethnic minority groups have been disproportionately experiencing more negative psychosocial or financial effects during the pandemic remained unanswered. Therefore, the objective of the current study was to examine these and other quality‐of‐life indicators in a breast cancer population.
In addition to studying cancer patients' quality of life during the pandemic, it is important to explore the adverse impact on diagnosis and treatment. During this global crisis, the goal of reducing COVID‐19 infection risk through limiting the provision of medical resources may not be aligned with the evidence that early diagnosis, consistent and uninterrupted treatment, and regular checkups are critically linked with improved cancer prognosis and survival rates. To address this dilemma, treatment recommendations and guidelines have been issued to redefine the priorities in the management of patients with cancer and guide clinical practices. 14 , 15 , 16 In this study, we sought to describe whether and how the treatment of patients with breast cancer in our institution has been disrupted during the pandemic and whether it differs for: 1) different subtypes and stages of breast cancer, 2) different types of treatments, and 3) different racial groups.
Materials and Methods
Study Design
This was a cross‐sectional study that surveyed patients with breast cancer and healthy controls registered in the Chicago Multiethnic Epidemiologic Breast Cancer Cohort (ChiMEC). The ongoing ChiMEC cohort consists of 4372 patients who were diagnosed with breast cancer from 1993 to 2019 and 1841 healthy controls. The ChiMEC cohort has been described in more detail in a previous publication. 17 Between July and September of 2020, we sent out 3898 online questionnaires to both patients with breast cancer (n = 2661) and healthy controls (n = 1237) using research electronic data capture (REDCap) tools hosted at The University of Chicago 18 , 19 to those who consented to complete follow‐up questionnaires. Through the questionnaires, we gathered information on patients' psychosocial well‐being, financial challenges, and treatment difficulties experienced during the pandemic. In August 2020, we reached out by telephone to participants who did not reply to the previously emailed online questionnaire. The response rate in healthy controls (26.6%) was lower than that in the patients with breast cancer (48.9%). Therefore, this report is focused on responses from the patients with breast cancer.
Measures
The survey consisted of a set of questions designed to measure the psychosocial well‐being of participants before and during the pandemic (for the questionnaire, see the Supporting Materials). The questions were adopted from Patient‐Reported Outcomes Measurement Information System items for emotional distress‐anxiety, emotional impact, emotional well‐being, positive affect, and social isolation, 20 as well as a recent survey of COVID‐19–related risk perception and coping in the general population. 21 Thirteen questions about participants' feelings of isolation, stress, and anxiety were presented on 5‐point Likert scales, with scores ranging from 0 (never) to 4 (always). These items were combined into total scores to represent patients' feelings of isolation before COVID‐19 (2 items; Cronbach α = .796), feelings of isolation during COVID‐19 (4 items; Cronbach α = .702), feelings of stress during COVID‐19 (7 items; Cronbach α = .814), and an overall isolation/stress score during COVID‐19 combining all items (11 items; Cronbach α = .848).
The pandemic‐related financial challenges of participants were measured through 7 items that questioned whether the participant had experienced any type of financial challenge during the COVID‐19 pandemic. This section entailed any financial challenges because of loss of employment, loss of health insurance, and/or other financial loss, as well as whether the participant had any difficulties in affording life expenses and/or affording food.
For patients with breast cancer, specific questions were asked about whether any of their scheduled treatments (including surgery, chemotherapy, radiotherapy, and hormonal therapy) were delayed or could not be maintained because of a COVID‐19–related lockdown. They were also asked about whether they had experienced any difficulty in making medical appointments and about their use of telemedicine.
Participants were also asked whether they had undergone COVID‐19 testing and whether they had tested positive. In addition to these queries, participants were given the opportunity to share their experiences and thoughts about their initial perceptions and feelings upon first hearing about the coronavirus in an open‐ended question at the end of the survey.
Demographic and clinical characteristics (ie, race/ethnicity, age at survey, age at diagnosis, time from diagnosis to survey, insurance status, number of family members that lived together, American Joint Committee On Cancer (AJCC) stage, tumor subtype, comorbidities) were collected through the baseline questionnaire during participant recruitment and/or were extracted from electronic medical records.
Statistical Analysis
The demographic, clinical, and socioeconomic characteristics of Black patients and White patients with breast cancer were compared using t tests for continuous variables and χ2 tests for categorical variables.
In terms of psychosocial well‐being, Wilcoxon rank‐sum tests were used to compare patients' responses to individual 5‐point Likert scale questions, and t tests were used to compare the combined scores. Multiple linear regression was used to assess whether racial disparity existed in the combined scores, adjusting for potential confounding demographic and clinical characteristics (ie, age, time from diagnosis to survey, insurance status, number of family members that lived together, pre–COVID‐19 feelings of isolation, AJCC cancer stage, tumor subtype, comorbidities). To compare the feelings of isolation before and during COVID‐19 in particular, Wilcoxon signed‐rank tests were used to compare the 2 corresponding questions, and paired t tests were used to compare the combined isolation scores before and during the COVID‐19 pandemic for Black patients and White patients.
The χ2 test was used to compare the experience of financial challenges and treatment difficulty between Black patients and White patients. Wilcoxon rank‐sum tests were used to compare patients' satisfaction with telemedicine. Multivariable logistic regression was used to explore which clinical and demographic factors contributed to the odds of financial challenges and treatment difficulty (ie, age, time from diagnosis to survey, insurance status, AJCC cancer stage, tumor subtype, comorbidities).
To address the issue of nonresponse, a sensitivity analysis was conducted using inverse probability weighting to examine the robustness of the results. 22 The nonresponse probabilities were estimated using a logistic regression model with race, time from diagnosis to survey, comorbidities, AJCC cancer stage, and insurance status as the predictors. The data were extracted from electronic medical records. All statistical analyses were conducted using the STATA 16 statistical software package (StataCorp).
Results
Among the 2661 surveys sent, 1300 individuals responded (48.9%). Of the responders, 930 (71.7%) were non‐Hispanic White, 291 (22.4%) were non‐Hispanic Black, 28 (2.2%) were Hispanic, 47 (3.6%) were Asian, and 2 (0.2%) were Native American. Limited by sample size, the comparison was conducted between non‐Hispanic Black patients (referred as Black patients) and non‐Hispanic White patients (referred as White patients) to examine whether racial disparities existed. A general description of the cohort stratified by racial group is provided in Table 1.
TABLE 1.
Description of the Study Cohort by Race/Ethnicity in 1300 Patients With Breast Cancer
| Variable | No. of Patients (%) | P b | ||
|---|---|---|---|---|
| White Patients, n = 930 | Black Patients, n = 291 | Other Patients, n = 79 a | ||
| Age at survey: Mean ± SD, y | 61.6 ± 11.6 | 63.6 ± 11.9 | 54.9 ± 12.5 | .011 |
| Age at diagnosis: Mean ± SD, y | 54.3 ± 11.5 | 56.2 ± 12.1 | 49.0 ± 12.5 | .017 |
| Time from diagnosis to survey: Mean ± SD, y | 6.8 ± 5.5 | 7.0 ± 5.9 | 5.6 ± 4.3 | .78 |
| Breast cancer subtype c | ||||
| HR+/Her2− | 468 (50.3) | 121 (41.6) | 32 (40.5) | .001 |
| HR+/Her2+ | 59 (6.3) | 24 (8.2) | 13 (16.5) | |
| HR−/Her2+ | 31 (3.3) | 18 (6.2) | 1 (1.3) | |
| TNBC | 98 (10.5) | 48 (16.5) | 10 (12.7) | |
| Unknown/not applicable | 274 (29.5) | 80 (27.5) | 23 (29.1) | |
| AJCC stage group | ||||
| 0 | 142 (15.3) | 54 (18.6) | 13 (16.5) | .12 |
| I | 388 (41.7) | 102 (35.1) | 29 (36.7) | |
| II | 220 (23.7) | 85 (29.2) | 21 (26.6) | |
| III | 84 (9.0) | 24 (8.2) | 8 (10.1) | |
| IV | 7 (0.8) | 4 (1.4) | 0 (0.0) | |
| Unknown | 89 (9.6) | 22 (7.6) | 8 (10.1) | |
| Charlson comorbidity index | ||||
| 0 | 759 (81.6) | 221 (75.9) | 64 (81.0) | .007 |
| 1 | 44 (4.7) | 19 (6.5) | 3 (3.8) | |
| ≥2 | 50 (5.4) | 31 (10.7) | 6 (7.6) | |
| Unknown | 77 (8.3) | 20 (6.9) | 6 (7.6) | |
| Insurance type | ||||
| Uninsured | 1 (0.1) | 1 (0.3) | 0 (0.0) | <.001 |
| Any Medicaid | 13 (1.4) | 50 (17.2) | 0 (0.0) | |
| Medicare | 169 (18.2) | 75 (25.8) | 11 (13.9) | |
| Private insurance | 642 (69.0) | 138 (47.4) | 59 (74.7) | |
| Other/unknown | 105 (11.3) | 27 (9.3) | 9 (11.4) | |
| COVID‐19 testing | ||||
| No | 729 (78.4) | 176 (60.5) | 61 (77.2) | <.001 |
| Yes | 193 (20.8) | 104 (35.7) | 17 (21.5) | |
| Missing | 8 (0.9) | 11 (3.8) | 1 (1.3) | |
| COVID‐19 test positive | ||||
| No | 914 (98.3) | 272 (93.5) | 77 (97.5) | .048 |
| Yes | 7 (0.8) | 6 (2.1) | 2 (2.5) | |
| Missing | 9 (1.0) | 13 (4.5) | 0 (0.0) | |
Abbreviations: −, negative; +, positive; AJCC, American Joint Commettee on Cancer; COVID‐19, coronavirus disease 2019; HER2, human epidermal growth factor receptor 2; HR, hormone receptor; TNBC, triple‐negative breast cancer.
There were 47 Asian patients, 28 Hispanic patients, 2 Native American patients, and 2 patients with their race/ethnicity identified as multiethnicity.
P values for the comparison between White patients and Black patients were estimated using t tests for continuous variables and χ2 tests for categorical variables (including missing categories).
The 4 breast cancer subtypes are: HR+/HER2− (estrogen receptor [ER]‐positive or progesterone receptor [PR]‐positive [together referred as HR+] and HER2‐negative [HER2−]); HR+/HER2+ (ER‐positive or PR‐positive and HER2‐positive); HR−/HER2+ (ER‐negative, PR‐negative, and HER2‐positive); and TNBC (ER‐negative, PR‐negative, and HER2‐negative).
COVID‐19 Testing and Prevalence of Positive Results
In the study, 314 patients (24.5%) reported having been tested for COVID‐19. Of these, 15 patients (4.8%) tested positive, and 2 (13.3%) of those who tested positive were consequently hospitalized (Table 1). Therefore, the prevalence of having a positive testing result for COVID‐19 was 1.2% among patients with breast cancer in the study sample. These findings seem to be roughly consistent with the statistics released by the Chicago Department of Public Health in September 2020, with a 4.5% positivity rate among those tested and a prevalence rate of 2.8%. 23
Psychosocial Well‐Being
The median overall isolation/stress score was 1.2 on a scale from 0 (never) to 4 (always), which was not significantly different between White patients and Black patients (Table 2). White patients reported feeling left out and isolated more often than Black patients before the pandemic (P < .001). However, the study found no significant racial difference for feelings of isolation scores during COVID‐19. In both Black patients and White patients (P < .001 for both; paired t test), the feelings of isolation scores were significantly higher during COVID‐19 than before the pandemic (Fig. 1). There was also no significant racial difference in the feelings of stress score during the pandemic (Table 2). In terms of the overall isolation/stress score, it was significantly associated with the previous feelings of isolation score and insurance status in multiple linear regression but had no significant association with race/ethnicity of the patient or other clinical characteristics. Regarding individual questions (Fig. 2), it is noteworthy to point out that White patients felt significantly more confident in getting medical help and better in keeping up with work and home responsibilities compared with Black patients. Conversely, Black patients felt significantly more often hopeful, less often fearful, and less often nervous/stressed than White patients.
TABLE 2.
Psychosocial Well‐Being Combined Scores by Race/Ethnicity in Patients With Breast Cancer
| Variable | Total Cohort, n = 1300 a | White Patients, n = 930 | Black Patients, n = 291 | P b |
|---|---|---|---|---|
| Feeling of isolation pre–COVID‐19: Median (IQR) | 0.5 (0.0‐1.0) | 0.5 (0.0‐1.0) | 0.0 (0.0‐1.0) | <.001 |
| Feeling of isolation: Median (IQR) | 0.8 (0.5‐1.3) | 0.8 (0.5‐1.2) | 0.8 (0.5‐1.2) | .35 |
| Feeling of stress: Median (IQR) | 1.3 (0.9‐1.7) | 1.3 (0.9‐1.7) | 1.3 (0.7‐1.9) | .33 |
| Overall isolation/stress score: Median (IQR) | 1.2 (0.7‐1.5) | 1.2 (0.7‐1.5) | 1.1 (0.7‐1.5) | .28 |
| Number of people currently living together: Mean ± SD | 1.6 ± 1.4 | 1.6 ± 1.4 | 1.6 ± 1.5 | .54 |
Abbreviations: COVID‐19, coronavirus disease 2019; IQR, interquartile range.
In addition to 930 White patients and 291 Black patients, the cohort also included 47 Asian patients, 28 Hispanic patients, 2 Native American patients, and 2 patients with their race/ethnicity identified as multiethnicity.
P values for the comparison between White patients and Black patients were estimated using t tests for the number of people currently living with COVID‐19 and Wilcoxon rank‐sum tests for the combined Likert scales.
Figure 1.
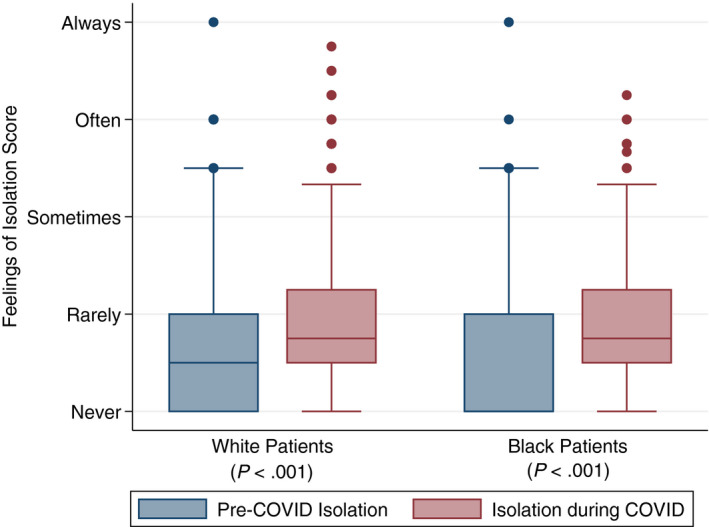
Box plots illustrate isolation scores before and during the coronavirus disease 2019 (COVID‐19) pandemic among Black patients and White patients. P values were estimated using paired t tests for the comparison of isolation scores before and during the COVID‐19 pandemic.
Figure 2.
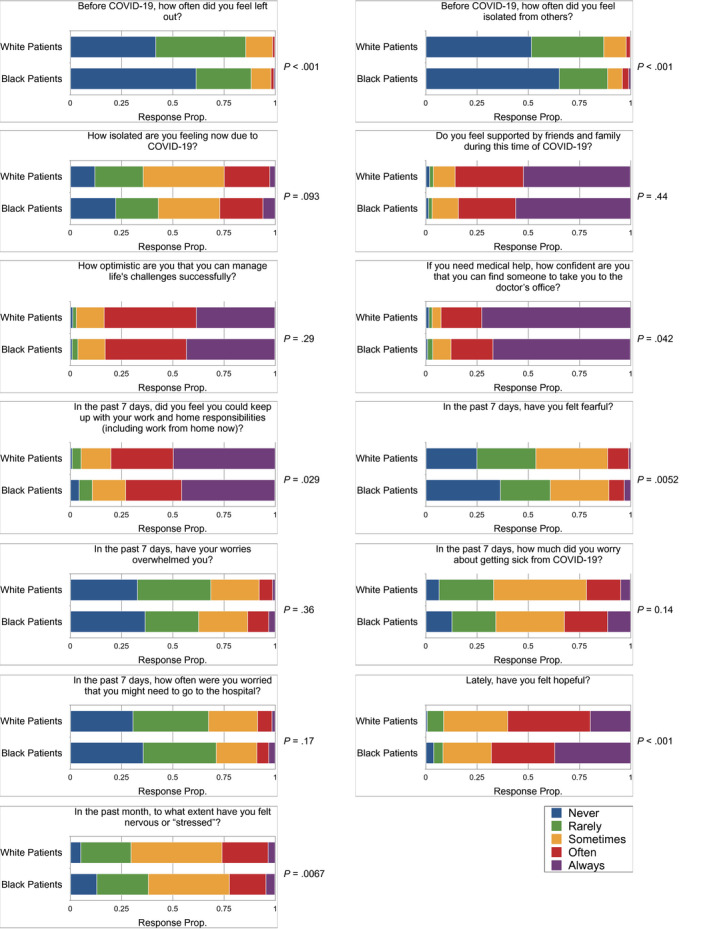
Stacked bar charts illustrate the responses to 13 individual questions on feelings of isolation and stress for Black patients and White patients. P values shown in the figure were estimated using Wilcoxon rank‐sum tests for the comparison between Black patients and White patients. COVID‐19 indicates coronavirus disease 2019; Prop, proportion.
On the basis of responses collected through the open‐ended question, many patients with breast cancer expressed their fear of being more vulnerable to COVID‐19 infection because of their diagnosis and treatment (eg, comorbidities, immunodeficiency). Some patients also expressed concerns about treatment disruption and cancer recurrence, whereas some, conversely, expressed their fears of coming into the hospital for treatments and checkups, all the while lacking information and instructions on these issues.
Financial Challenges
Overall, 33.2% of all patients experienced some sort of financial challenge, and 20.1% of all participants reported experiencing a major financial loss (either savings, investment, and/or retirement plan loss). Compared with White patients with breast cancer, Black patients were significantly more likely to experience unemployment/wage reduction, loss of health insurance, and difficulty in meeting expenses and affording food (Table 3). Nevertheless, after adjusting for age at survey and insurance type through multivariable logistic regression, no significant racial difference was found in terms of experiencing financial challenges of any kind. This suggested that the racial disparity in experiencing financial challenges can be mostly explained by the difference in insurance type. The model also showed that patients who were Medicaid recipients, almost 80% of whom were Black, had a significantly higher odds of experiencing financial challenges compared with patients who had private insurance (see Supporting Table 1). In addition, the odds of experiencing financial challenges of any kind were not significantly associated with any clinical characteristics.
TABLE 3.
Experience of Financial Challenges by Black Patients and White Patients
| Variable | No. of Patients (%) | P a | ||
|---|---|---|---|---|
| Total Cohort, n = 1300 | White Patients, n = 930 | Black Patients, n = 291 | ||
| Any financial challenge | ||||
| No | 869 (66.8) | 637 (68.5) | 182 (62.5) | .059 |
| Yes | 431 (33.2) | 293 (31.5) | 109 (37.5) | |
| Lost job or had reduced wage | ||||
| No | 653 (50.8) | 492 (53.3) | 116 (40.8) | <.001 |
| Yes | 173 (13.5) | 110 (11.9) | 47 (16.5) | |
| Unemployed | 460 (35.8) | 321 (34.8) | 121 (42.6) | |
| Lost health insurance | ||||
| No | 1254 (97.7) | 906 (98.3) | 269 (95.4) | .005 |
| Yes | 18 (1.4) | 8 (0.9) | 10 (3.5) | |
| Uninsured | 11 (0.9) | 8 (0.9) | 3 (1.1) | |
| Concerned about losing insurance | ||||
| No | 1160 (90.9) | 840 (91.3) | 253 (91.0) | .92 |
| Yes | 101 (7.9) | 68 (7.4) | 22 (7.9) | |
| Uninsured | 15 (1.2) | 12 (1.3) | 3 (1.1) | |
| Experienced major financial loss | ||||
| No | 1024 (79.9) | 737 (80.1) | 221 (78.4) | .53 |
| Yes | 257 (20.1) | 183 (19.9) | 61 (21.6) | |
| Difficulty paying life expenses | ||||
| No | 1139 (89.1) | 861 (93.5) | 209 (74.9) | <.001 |
| Yes | 139 (10.9) | 60 (6.5) | 70 (25.1) | |
| Difficulty getting food | ||||
| No | 1225 (95.7) | 894 (97.3) | 254 (90.1) | <.001 |
| Yes | 55 (4.3) | 25 (2.7) | 28 (9.9) | |
P values for the comparison between White patients and Black patients were estimated using χ2 tests for the experience of financial challenges. Missing responses are not listed in the table.
Treatment Difficulty
In terms of receiving treatment, 23% of all patients reported having experienced some sort of treatment disruption or having difficulty scheduling an appointment. The most affected types of treatment were radiotherapy and breast surgery, with 6.5% of patients having their scheduled radiotherapies delayed and 6.1% having their scheduled breast surgeries canceled in total (Table 4). There were no significant differences between Black patients and White patients in treatment difficulty in the multivariable logistic regression, adjusting for age, time since diagnosis, and clinical characteristics. Regarding the use of telemedicine, significantly more Black patients (71%) than White patients (55%) reported using telemedicine. No significant difference was found between Black patients and White patients in terms of the level of satisfaction with the telemedicine experience, with the vast majority of participants (>90%) reporting feeling at least somewhat satisfied (Table 4).
TABLE 4.
Experience of Treatment Difficulties by Black Patients and White Patients
| Variable | No. of Patients (%) | P a | ||
|---|---|---|---|---|
| Total Cohort, n = 1300 | White Patients, n = 930 | Black Patients, n = 291 | ||
| Any treatment difficulty b | ||||
| No | 846 (77.0) | 599 (77.1) | 189 (75.9) | .70 |
| Yes | 252 (23.0) | 178 (22.9) | 60 (24.1) | |
| Breast surgery canceled | ||||
| No | 184 (93.9) | 113 (93.4) | 56 (96.6) | .39 |
| Yes | 12 (6.1) | 8 (6.6) | 2 (3.4) | |
| Chemotherapy delayed | ||||
| No | 166 (97.1) | 109 (97.3) | 47 (95.9) | .64 |
| Yes | 5 (2.9) | 3 (2.7) | 2 (4.1) | |
| Radiotherapy delayed | ||||
| No | 144 (93.5) | 96 (93.2) | 41 (95.3) | .62 |
| Yes | 10 (6.5) | 7 (6.8) | 2 (4.7) | |
| Hormonal therapy disrupted | ||||
| No | 597 (97.1) | 438 (97.6) | 116 (95.1) | .15 |
| Yes | 18 (2.9) | 11 (2.4) | 6 (4.9) | |
| Difficulty of appointment | ||||
| No | 812 (78.2) | 567 (77.6) | 188 (78.7) | .72 |
| Yes | 226 (21.8) | 164 (22.4) | 51 (21.3) | |
| Use of telemedicine | ||||
| No | 467 (41.1) | 364 (45.0) | 73 (29.0) | <.001 |
| Yes | 668 (58.9) | 445 (55.0) | 179 (71.0) | |
| Satisfied with telemedicine | ||||
| Not at all satisfied | 18 (2.7) | 11 (2.5) | 7 (3.9) | .17 |
| A little satisfied | 44 (6.6) | 33 (7.4) | 6 (3.4) | |
| Somewhat satisfied | 191 (28.7) | 122 (27.5) | 56 (31.3) | |
| Very satisfied | 290 (43.5) | 196 (44.2) | 71 (39.7) | |
| Extremely satisfied | 123 (18.5) | 81 (18.3) | 39 (21.8) | |
P values for the comparison between White patients and Black patients were estimated using χ2 tests for the experience of treatment difficulty and Wilcoxon rank‐sum tests for satisfaction with telemedicine.
Treatment difficulty refers to experiencing any kind of treatment disruption (surgery canceled, chemotherapy delayed, radiotherapy delayed, hormonal therapy disrupted) or reporting having difficulty making an appointment to see the physician. Patients who reported that they did not need treatment (not applicable) were not listed.
Sensitivity Analysis
The distribution of selected demographic and clinical characteristics between respondents and nonrespondents are shown in Supporting Table 2. Overall, patients between ages 60 and 70 years, White patients, those diagnosed recently, patients who had less comorbidities, and patients who did not have stage IV diseases were more likely to respond. The major results after weighting for nonresponse are listed in Supporting Table 3. Overall, findings from the inverse probability weighting analysis were similar to those reported above.
Discussion
In this study, we examined self‐reports of psychosocial and financial well‐being during the COVID‐19 pandemic for patients with breast cancer in a racially diverse cohort and also assessed whether and how patients' scheduled medical services were disrupted. We found that feelings of isolation had intensified for both Black patients and White patients since the pandemic. The overall isolation/stress score was moderate, with a median of 1.2 (on a scale ranging from 0 to 4). The median score did not change after weighting for nonresponse. This could be explained by looking at the individual questions. Although many patients worried about getting sick from COVID‐19 and often felt nervous, most felt hopeful and confident about their ability to manage life challenges, suggesting that American patients with breast cancer are optimistic and resilient to the pandemic. These findings are similar to those from several other observational studies conducted among Chinese and European populations, in which it was reported that the prevalence of depression, anxiety, and stress symptoms among patients with cancer significantly increased during the COVID‐19 pandemic. 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 Although these results indicate a similar trend, because different assessment tools were used, it limits direct comparison of the findings across different studies.
In terms of whether racial disparities existed, our findings indicate that the overall psychosocial well‐being of Black patients was similar to that of White patients. However, Black patients experienced more financial challenges in different aspects and had more difficulty in keeping up with work and home responsibilities than White patients. Similar racial disparity was also found in studies before the pandemic, in which racial and ethnic minority cancer survivors were more likely to suffer financial hardship. 6 , 32 In addition, Black patients reported making use of telemedicine more often compared with White patients. Meanwhile, our findings showed that Black patients were subjectively more hopeful and resilient.
From the survey's qualitative items, many patients expressed concerns about whether treatment disruption would do more harm than good. This is in line with findings from other studies, which suggested that the sense of uncertainty because of treatment interruption was causing stress and anxiety among patients with cancer. 27 , 28 Although guidelines on the management of patients with cancer have been issued, as the pandemic continues, the long‐term risks and benefits of balancing protocols designed to mitigate the spread of COVID‐19 and maintaining consistent care for patients might need to be re‐evaluated. More importantly, patients with cancer were disappointed by the lack of available information and instructions targeted to provide them with specific, cancer treatment‐related support. Therefore, health care providers should actively look for ways to provide more information through specialized support, targeted resources, and ongoing communication with patients.
The major strength of the study is that it is a multiethnic cohort, which enabled investigation of quality‐of‐life perceptions during the COVID‐19 pandemic among patients with breast cancer from different racial and ethnic groups. One limitation of the study is that the majority of the patient population had already completed cancer treatment, making it hard to further investigate the factors affecting treatment disruption because of the limited sample size of patients with breast cancer undergoing active treatment. Another limitation is that those who participated in the study may not be fully representative of the study population. Because data were collected through emailed online surveys and telephone calls, those who responded may well be healthier or may have had more spare time. However, the major findings still held after weighting for nonresponse in the sensitivity analysis. The third limitation is that the study only included patients with breast cancer from Chicago, so the study findings might not be generalizable to populations in other locations.
In the current study, surveys were conducted approximately 5 months after the COVID‐19 outbreak in the United States. An additional follow‐up survey is needed in the future to examine longer term perceptions of psychosocial and financial well‐being during the pandemic. With the increasing availability of COVID‐19 vaccines, participants' attitudes and behaviors toward getting vaccinated are also of interest for future exploration. Finally, because we expect to see more COVID‐19–positive patients, further longitudinal research can be conducted to examine how the pandemic is associated with the experience of severe complications and overall survival in patients with cancer.
Conclusions
By surveying a multiethnic cohort of patients with breast cancer, we found that the COVID‐19 pandemic was significantly associated with increased feelings of isolation for all participants and imposed financial challenges to many patients, especially Medicaid recipients. Approximately one‐fourth of patients under active treatment experienced and expressed concerns about some type of treatment difficulty. The findings also suggest that patients with cancer desire more detailed information to support them through this pandemic.
Funding Support
This project was supported by the National Cancer Institute (P20CA233307, P20CA233307‐02W1) and the Breast Cancer Research Foundation (BCRF‐20‐071).
Conflict of Interest Disclosures
Olufunmilayo I. Olopade is supported by Susan G. Komen as a Komen Scholar. The remaining authors made no disclosures.
Author Contributions
Fangyuan Zhao: Contributed to the conceptualization, design, and implementation of the research, conducted the analysis and interpretation of the data, took the lead in drafting the article, provided critical feedback, and contributed to the writing of the article. Tara O. Henderson: Contributed to the conceptualization, design, and implementation of the research, provided critical feedback, and contributed to the writing of the article. Toni M. Cipriano: Contributed to the design and implementation of the research, conducted the analysis and interpretation of the data, provided critical feedback, and contributed to the writing of the article. Brenda L. Copley: Contributed to the design and implementation of the research. Michelle Liu: Contributed to the implementation of the research, provided critical feedback, and contributed to the writing of the article. Rahul Burra: Contributed to the and implementation of the research, provided critical feedback, and contributed to the writing of the article. Sondra H. Birch: Contributed to the implementation of the research, provided critical feedback, and contributed to the writing of the article. Olufunmilayo I. Olopade: Contributed to the conceptualization, design, and implementation of the research. Dezheng Huo: Contributed to the conceptualization, design, and implementation of the research, conducted the analysis and interpretation of the data, provided critical feedback, and contributed to the writing of the article. The article has been read and approved by all named authors.
Supporting information
Supplementary Material
Zhao F, Henderson TO, Cipriano TM, Copley BL, Liu M, Burra R, Birch SH, Olopade OI, Huo D. The impact of coronavirus disease 2019 on the quality of life and treatment disruption of patients with breast cancer in a multiethnic cohort. Cancer. 2021. 10.1002/cncr.33798
We are grateful to the study participants for their time and effort. We also thank Drs. Kevin Krull, Diane Lauderdale, and Patricia Boyle for their advice on questionnaire development.
References
- 1. Al‐Quteimat OM, Amer AM. The impact of the COVID‐19 pandemic on cancer patients. Am J Clin Oncol. 2020;43:452‐455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dai M, Liu D, Liu M, et al. Patients with cancer appear more vulnerable to SARS‐CoV‐2: a multicenter study during the COVID‐19 outbreak. Cancer Discov. 2020;10:783‐791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mehta V, Goel S, Kabarriti R, et al. Case fatality rate of cancer patients with COVID‐19 in a New York hospital system. Cancer Discov. 2020;10:935‐941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yang F, Shi S, Zhu J, Shi J, Dai K, Chen X. Clinical characteristics and outcomes of cancer patients with COVID‐19. J Med Virol. 2020;92:2067‐2073. [DOI] [PubMed] [Google Scholar]
- 5. Shapiro SL, Lopez AM, Schwartz GE, et al. Quality of life and breast cancer: relationship to psychosocial variables. J Clin Psychol. 2001;57:501‐519. [DOI] [PubMed] [Google Scholar]
- 6. Jagsi R, Pottow JA, Griffith KA, et al. Long‐term financial burden of breast cancer: experiences of a diverse cohort of survivors identified through population‐based registries. J Clin Oncol. 2014;32:1269‐1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fallowfield L, Jenkins V. Psychosocial/survivorship issues in breast cancer: are we doing better? J Natl Cancer Inst. 2015;107:335. [DOI] [PubMed] [Google Scholar]
- 8. Silber JH, Rosenbaum PR, Clark AS, et al. Characteristics associated with differences in survival among black and white women with breast cancer. JAMA. 2013;310:389‐397. [DOI] [PubMed] [Google Scholar]
- 9. Daly B, Olopade OI. A perfect storm: how tumor biology, genomics, and health care delivery patterns collide to create a racial survival disparity in breast cancer and proposed interventions for change. CA Cancer J Clin. 2015;65:221‐238. [DOI] [PubMed] [Google Scholar]
- 10. Richardson LC, Henley SJ, Miller JW, Massetti G, Thomas CC. Patterns and trends in age‐specific Black‐White differences in breast cancer incidence and mortality—United States, 1999‐2014. MMWR Morb Mortal Wkly Rep. 2016;65:1093‐1098. [DOI] [PubMed] [Google Scholar]
- 11. Chowkwanyun M, Reed AL Jr. Racial health disparities and Covid‐19—caution and context. N Engl J Med. 2020;383:201‐203. [DOI] [PubMed] [Google Scholar]
- 12. Kullar R, Marcelin JR, Swartz TH, et al. Racial disparity of coronavirus disease 2019 in African American communities. J Infect Dis. 2020;222:890‐893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Garg S, Kim L, Whitaker M, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory‐confirmed coronavirus disease 2019—COVID‐NET, 14 states, March 1‐30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:458‐464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. van de Haar J, Hoes LR, Coles CE, et al. Caring for patients with cancer in the COVID‐19 era. Nat Med. 2020;26:665‐671. [DOI] [PubMed] [Google Scholar]
- 15. Dietz JR, Moran MS, Isakoff SJ, et al. Recommendations for prioritization, treatment, and triage of breast cancer patients during the COVID‐19 pandemic. The COVID‐19 Pandemic Breast Cancer Consortium. Breast Cancer Res Treat. 2020;181:487‐497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Turaga KK, Girotra S. Are we harming cancer patients by delaying their cancer surgery during the COVID‐19 pandemic? Ann Surg. Published online June 2, 2020. doi: 10.1097/SLA.0000000000003967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zhao F, Copley B, Niu Q, et al. Racial disparities in survival outcomes among breast cancer patients by molecular subtypes. Breast Cancer Res Treat. 2020;185, 841‐849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Harris PA, Taylor R, Minor BL, et al. The REDCap Consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cella D, Riley W, Stone A, et al. The Patient‐Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self‐reported health outcome item banks: 2005‐2008. J Clin Epidemiol. 2010;63:1179‐1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gerhold L. Risk perception and coping strategies. PsyArXiv. Published online March 25, 2020. Preprint. Accessed June 10, 2020. doi: 10.31234/osf.io/xmpk4. https://psyarxiv.com/xmpk4/ [DOI] [Google Scholar]
- 22. Harkanen T, Kaikkonen R, Virtala E, Koskinen S. Inverse probability weighting and doubly robust methods in correcting the effects of non‐response in the reimbursed medication and self‐reported turnout estimates in the ATH survey. BMC Public Health. 2014;14:1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chicago Department of Public Health (CDPH) . Chicago COVID‐19 Update. CDPH; 2020. Accessed January 29, 2021. https://www.chicago.gov/content/dam/city/sites/covid/reports/2020‐09‐23/Chicago_COVID‐19_Update_V9_9_23_2020.pdf [Google Scholar]
- 24. Ng DWL, Chan FHF, Barry TJ, et al. Psychological distress during the 2019 coronavirus disease (COVID‐19) pandemic among cancer survivors and healthy controls. Psychooncology. 2020;29:1380‐1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Swainston J, Chapman B, Grunfeld EA, Derakshan N. COVID‐19 lockdown and its adverse impact on psychological health in breast cancer. Front Psychol. 2020;11:2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Magno S, Linardos M, Carnevale S, et al. The impact of the COVID‐19 pandemic on breast cancer patients awaiting surgery: observational survey in an Italian university hospital. Breast J. 2020;26:1597‐1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wang Y, Duan Z, Ma Z, et al. Epidemiology of mental health problems among patients with cancer during COVID‐19 pandemic. Transl Psychiatry. 2020;10:263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chen G, Wu Q, Jiang H, et al. Fear of disease progression and psychological stress in cancer patients under the outbreak of COVID‐19. Psychooncology. 2020;29:1395‐1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Han J, Zhou F, Zhang L, Su Y, Mao L. Psychological symptoms of cancer survivors during the COVID‐19 outbreak: a longitudinal study. Psychooncology. 2021;30:378‐384. [DOI] [PubMed] [Google Scholar]
- 30. Ciazynska M, Pabianek M, Szczepaniak K, et al. Quality of life of cancer patients during coronavirus disease (COVID‐19) pandemic. Psychooncology. 2020;29:1377‐1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Schellekens MPJ, van der Lee ML. Loneliness and belonging: exploring experiences with the COVID‐19 pandemic in psycho‐oncology. Psychooncology. 2020;29:1399‐1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hastert TA, Banegas MP, Hamel LM, et al. Race, financial hardship, and limiting care due to cost in a diverse cohort of cancer survivors. J Cancer Surviv. 2019;13:429‐437. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


