Abstract
Background
Transit workers have jobs requiring close public contact for extended periods of time, placing them at increased risk for severe acute respiratory syndrome coronavirus 2 infection and more likely to have risk factors for coronavirus disease 2019 (COVID‐19)‐related complications. Collecting timely occupational data can help inform public health guidance for transit workers; however, it is difficult to collect during a public health emergency. We used nontraditional epidemiological surveillance methods to report demographics and job characteristics of transit workers reported to have died from COVID‐19.
Methods
We abstracted demographic and job characteristics from media scans on COVID‐19 related deaths and reviewed COVID‐19 memorial pages for the Amalgamated Transit Union (ATU) and Transport Workers Union (TWU). ATU and TWU provided a list of union members who died from COVID‐19 between March 1–July 7, 2020 and a total count of NYC metro area union members. Peer‐reviewed publications identified through a scientific literature search were used to compile comparison demographic statistics of NYC metro area transit workers. We analyzed and reported characteristics of ATU and TWU NYC metro area decedents.
Results
We identified 118 ATU and TWU NYC metro area transit worker COVID‐19 decedents with an incidence proportion of 0.3%. Most decedents were male (83%); median age was 58 years (range: 39–71). Median professional tenure was 20 years (range: 2–41 years). Operator (46%) was the most reported job classification. More than half of the decedents (57%) worked in positions associated with close public contact.
Conclusion
Data gathered through nontraditional epidemiological surveillance methods provided insight into risk factors among this workforce, demonstrating the need for mitigation plans for this workforce and informing transit worker COVID‐19 guidance as the pandemic progressed.
Keywords: COVID‐19, essential workers, New York City transit workers, occupational health
1. INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), the virus that causes coronavirus disease 2019 (COVID‐19), was first identified in China in late 2019. Following widespread international transmission, the World Health Organization declared the outbreak a pandemic on March 11, 2020.1 New York City (NYC) was the first major metropolitan area in the United States to be severely impacted by the pandemic. The first case of COVID‐19 in NYC was reported on March 1, 2020.2 Within three weeks the number of cases and hospitalizations rose sharply and by April 15, 2020, NYC had over 117,000 cases.3 On March 22, 2020, stay‐at‐home orders issued by the governors of Connecticut, New Jersey, and New York (NY) went into effect.4, 5 However, healthcare workers and other essential workers were required to continue reporting to work, including staff of the Metropolitan Transit Authority (MTA), which provides mass transportation for the NYC metropolitan area. Approximately 80% of MTA workers were members from either the Amalgamated Transit Union (ATU) or Transport Workers Union (TWU).
Many MTA workers have jobs that require close contact with the public for extended periods, potentially increasing risk of exposure to SARS‐CoV‐2. Until March 8, 2020, transit workers were not permitted to wear face masks or gloves while performing their job.6, 7 On March 27, 2020, MTA announced it would provide MTA workers with face masks; on April 4, 2020, MTA began providing face masks to MTA workers.8 The public was required to wear face masks while riding on public transportation starting April 15, 2020 when the Governor of NY issued a mandate for New Yorkers to wear face masks in public when unable to socially distance.9
Occupational data about persons with COVID‐19 among essential worker populations can help improve local, state, and federal public health guidance for worker safety and health. Collecting occupational data can also help protect spread of infection among the community and improve public health. Collecting timely data on occupation and industry of ill persons may not be feasible during a public health emergency. To overcome the challenge, we used nontraditional public health surveillance methods including monitoring of media reports and review of union records to track COVID‐19‐related deaths among NYC metro area transit workers.
In addition to working in positions with close public contact, transit workers face multiple occupational hazards, which can affect their health and safety and put them at increased risk of infection for SARS‐CoV‐2.10, 11, 12, 13, 14, 15, 16, 17, 18 Previous studies have quantified the burden of a range of injuries and illnesses associated with transit worker jobs, including chemical, safety, ergonomic, emotional, psychological, and biological hazards; these hazards can affect workers' health individually and synergistically.15, 16, 19, 20, 21, 22, 23 Furthermore, transit workers are commonly male, aged >50 years, people of color, and almost one‐fourth have incomes below the poverty level.24, 25 All of these demographic and socioeconomic groups are disproportionately affected by COVID‐19.24, 25, 26, 27, 29, 30
Both the occupational hazards faced by transit workers and their demographic characteristics may increase their risk of exposure to SARS‐CoV‐2 and COVID‐19 complications. Here, we present information collected through nontraditional public health surveillance methods to describe COVID‐19‐related fatalities among transit workers in the NYC metro area early during the pandemic.
2. MATERIALS AND METHODS
From March 30–July 7, 2020, we monitored a continuous Google® alert (referred to as media scanning hereafter) for one or more of the following terms: transportation workers and confirmed cases of COVID‐19, to identify online reports of COVID‐19‐related deaths among transit workers in the NYC metro area that occurred between March 1 and July 7, 2020. We defined a transit worker as a worker of public ground transportation including bus, subway, and train systems. Based on the NYC Planning Metro Region Explorer,31 we defined the NYC metro area as NYC's five boroughs and 26 surrounding counties in New York, North New Jersey, and southwest Connecticut, an area that roughly represents the NYC commuter shed. Through media scanning, we identified memorial website pages from ATU and TWU. We contacted ATU and TWU national leadership to confirm that according to union records the transit worker decedents identified during the media scanning process reportedly died from COVID‐19 and to request total ATU and TWU transit worker population data for the NYC metro area for comparison with media scanning data. Because ATU and TWU were able to provide denominator data for union members who work in the NYC metro area and at least 80% of MTA transit workers are members of ATU and TWU, we limited our analysis to transit worker decedents who were known members of a local union section of ATU or TWU in the NYC metro area. For the local union sections in the defined area, ATU and TWU provided membership lists and information about members who worked in the NYC metro area and reportedly died from COVID‐19. We reviewed media reports and information from ATU and TWU to determine demographic and occupational data (including work location) of the deceased workers. Using the internet and each decedent's name and work location as search terms, we found additional information through obituaries and local news reports.
With guidance from ATU and TWU leadership, we grouped transit worker decedent job titles into three worker classifications based on job function: operator (e.g., bus driver, train operator, train conductor); maintenance worker (e.g., bus mechanic, heating and air conditioning maintainer, trackworker); and support staff (e.g., supervisor, station agent, coach cleaner, call center operator). We categorized job titles as either public contact positions or nonpublic contact positions based on the job function and guidance from the Union leadership. We defined public contact as close contact with the public while preforming their job duties.
Although we were able to obtain demographic data for NYC metro area transit workers who died from COVID‐19, we were unable to obtain such data for workers who did not die from COVID‐19. Therefore, for comparison, we used published demographic data for all NYC metro area workers.20, 30, 32, 33 To find such published data, we performed a comprehensive search of the scientific literature to identify peer‐reviewed publications describing demographic statistics of NYC metro area transit workers. We searched PubMed, Scopus, CINHAL, Cochrane Reviews, and Google® Scholar using one or more of the search terms from the following list: transit worker, transit employee, transit operator, transportation worker, transportation employee, and transport worker with no date limits in the databases. We reviewed up to 500 abstracts from each search engine, up to 2500 total, and identified potentially relevant articles. We reviewed full articles and included those with demographic statistics of NYC metro area transit workers. Through this process we identified demographic data collected in 2002, 2009, and 2020.
We calculated descriptive statistics for COVID‐19 deaths among NYC metro area transit workers using mean (standard deviation) for continuous variables and n (%) for categorical variables. We calculated the incidence proportion for COVID‐19 deaths among NYC metro area ATU and TWU transit workers over the 129‐day period from March 1 to July 7, 2020. We established our denominator for the incidence proportion calculation using the lists provided by the unions of all ATU and TWU transit members as of July 9, 2020 in the NYC metro area. We compared sex and age distributions among decedents and published demographic data for NYC metro area transit workers using chi‐squared tests. All analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA). This activity was reviewed by the Centers for Disease Control and Prevention (CDC) and was conducted consistent with applicable federal law and CDC policy.a
3. RESULTS
Through media scanning, we identified 128 transit workers who reportedly died from COVID‐19 during March 1–July 7, 2020. We excluded 40 decedents who did not work in the NYC metro area and 20 who were not members of ATU or TWU. Information from ATU and TWU confirmed the transit decedents identified through media scanning and added 50 additional transit worker decedents, bringing the total to 118 decedents (Figure 1). Twenty‐two decedents were ATU members, and 96 were TWU members. ATU reported having 9374 members in the NYC metro area, and TWU reported having 37,700. The incidence proportion for death from COVID‐19 among ATU and TWU transit workers in the NYC metro area during March 1–July 7, 2020 was 0.3%. The incidence proportion among ATU members was 0.2% and among TWU members was 0.3%. The majority (83%) of transit worker decedents were male, and the median age was 58 years (range: 39–71 years) (Table 1). The median tenure among transit worker decedents was 20 years (range: 2–41 years). Place of birth was available for 30 (25%) decedents; 23 (77%) were not born in the United States.
Figure 1.
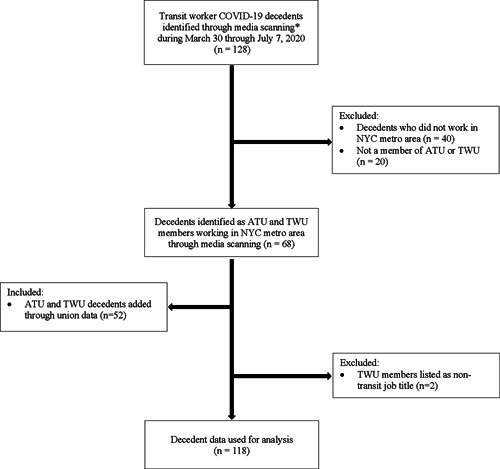
Population included in the current investigation of coronavirus disease 2019 (COVID‐19)‐related deaths among Amalgamated Transit Union (ATU) and Transport Workers Union (TWU) members in the NYC metro area, March 1–July 7, 2020. *Media scanning is defined as monitoring a continuous Google® alert for one or more of the following terms: transportation workers and confirmed cases for COVID‐19
Table 1.
Distribution of 118 Amalgamated Transit Union (ATU) and Transport Workers Union (TWU) New York City (NYC) metro area transit workers who died from COVID‐19 by demographic, work‐related, and clinical characteristics—March 30, 2020–July 7, 2020
| ATU and TWU NYC metro area transit worker decedents | ATU and TWU NYC metro area transit worker decedents | |
|---|---|---|
| Demographics | N = 118 | % |
| Sex | ||
| Female | 12 | 10 |
| Male | 98 | 83 |
| Unknown | 8 | 7 |
| Age | ||
| Median age (range) | 58 (39–71) | |
| Age category (years) | ||
| 30–39 | 1 | 1 |
| 40–49 | 10 | 8 |
| 50–59 | 34 | 29 |
| 60+ | 28 | 24 |
| Missing/not reported | 45 | 38 |
| Place of birth | ||
| United States | 7 | 6 |
| Not in the United States | 23 | 19 |
| Unknown | 88 | 75 |
| Work‐related characteristics | ||
| Worker classification | ||
| Operator | 54 | 46 |
| Support staff | 35 | 30 |
| Maintenance | 26 | 22 |
| Unknown | 3 | 2 |
| Contact with the public | ||
| Public contact positions | 67 | 57 |
| Nonpublic contact positions | 48 | 41 |
| Unknown | 3 | 2 |
| Tenure in profession | ||
| Median tenure in years (range) | 20 (2–41) | |
| Clinical characteristics | ||
| Hospitalized | ||
| Yes | 17 | 14 |
| No | 1 | 1 |
| Unknown | 100 | 85 |
| Placed on a ventilator | ||
| Yes | 8 | 7 |
| No | 1 | 1 |
| Unknown | 109 | 92 |
| Symptoms reported (n = 10) | ||
| Fever | 6 | — |
| Shortness of breath | 5 | — |
| Cough | 4 | — |
| Fatigue | 2 | — |
| Gastrointestinal symptoms | — | |
| Loss of taste | 1 | — |
| Chest pain | 1 | — |
| Co‐morbidities | ||
| Known | 4 | 3 |
| Unknown | 114 | 97 |
Of the 115 transit worker decedents for whom worker classification was available, 54 (46%) worked in a position classified as an operator. Sixty‐seven decedents (57%) worked in a job that involved public contact. Decedent data collected through media scanning compared with decedent data provided by the unions reported similar worker classification and public contact information. When comparing worker classification and public contact information among ATU and TWU decedents, the majority (73%) of ATU decedents worked in a position classified as an operator or a position that involved public contact. ATU and TWU unions represent bus, subway, and train system workers in the NYC metro area but, the majority of decedent data were missing work system information and was not analyzed. Hospitalization, symptom, and co‐morbidity information was collected, but was missing in the majority of media reports and was not analyzed.
COVID‐19 deaths among NYC metro area transit workers followed a similar trend to those among the general NYC population, with a peak in deaths during the week of April 5th followed by a drop in the number of deaths (Figure 2).34 The decrease in deaths occurred approximately three weeks after the NYC metro area's stay‐at‐home orders were issued and MTA started issuing face masks to transit workers.5, 8 Furthermore, there was a concurrent steady decline in identified NYC metro area transit worker deaths and public deaths after the public was required to wear face masks on public transportation.9
Figure 2.
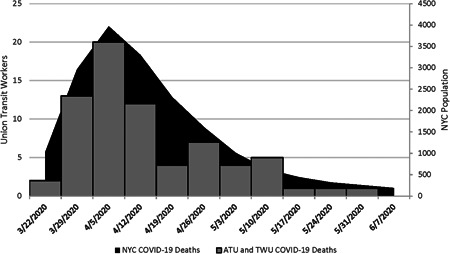
Deaths from coronavirus disease 2019 (COVID‐19) among Amalgamated Transit Union (ATU) and Transport Workers Union (TWU) New York City (NYC) Metro Area Transit Workers and all NYC Residents during March 1, 2020 through June 7, 2020*, by Week of Death. *Represents NYC Metro Area Transit Worker's week of death
Our literature search identified six publications providing limited information on demographics for NYC metro area transit workers, four of which were published within the last 20 years. By combining demographic data obtained from the four articles published in the past 20 years, we were able to make comparisons with the NYC metro area transit worker decedent data. The four most recent studies described the mean age of transit workers between 43 and 45 years old, with a large proportion (43%–47%) having been over 50 years old.20, 24, 32, 33 Two transit worker studies reported their study population comprising mostly male (range 71%–85%).20, 32 The two studies describing tenure reported most transit workers were full‐time workers (81%) who had worked for an average of 12 years as a union member in a transit position.20, 24 Self‐identified racial categories were more varied between the two studies reporting race: White (range 41%–55%), Black (range 26%–42%), and Asian/Pacific Islander (3%–4%). The variation in estimates of the racial/ethnic distributions of transit workers could be explained because one study reported racial categories for all US public transit workers and the other study focused on NYC transit workers. Approximately 40% had some college education and between 11% and 13% had a college degree. By combining demographic data obtained from these articles, we were able to determine a larger proportion of decedents in this study were 50 years old or older than the general NYC transit worker population (p < .0001) (Table 2).
Table 2.
Comparison of age category between Amalgamated Transit Union and Transport Workers Union New York City metro area transit worker COVID‐19 deaths and transit worker population identified during literature search
| Age category | |||
|---|---|---|---|
| COVID‐19 deaths N = 73 | Leffler et al.32, a N = 50,230 | ||
| 30–39 years | 1 (1%) | 11,425 (23%) | |
| 40–49 years | 10 (14%) | 15,080 (30%) | |
| 50–59 years | 34 (47%) | 15,520 (31%) | |
| 60+ years | 28 (38%) | 8205 (16%) | |
| p value | <.00001 | ||
Leffler et al. uses data related to COVID‐19 deaths among NYC MTA Transit Workers through May 6, 2020.
4. DISCUSSION
Our study described the mortality burden from COVID‐19 between March 1 and July 7, 2020 among ATU and TWU NYC metro area transit workers, an essential worker group. Currently, there is no active national surveillance program for COVID‐19 deaths among non‐healthcare essential workers. Systematically collecting timely occupational data on ill persons during a pandemic can provide information about disproportionately affected occupational groups and improve recommendations to protect workers, the community, and public health.35, 36, 37 In the absence of occupational data collected systematically through case report forms, we have demonstrated that the identification of COVID‐19 related deaths among a specific group of workers using media reports and union records can yield useful information about these decedents.
Through media scanning and ATU and TWU data, we found most transit worker COVID‐19 decedents were male, over the age of 50 years, and some had known co‐morbidities. According to an MTA Diversity Report, as of December 31, 2019, 18% of MTA employees were female.30 The lower percentage of female transit worker deaths is consistent with other COVID‐19 studies indicating a sex‐related difference in case fatalities and might support the finding that males are at a higher risk for COVID‐19 complications.26, 27, 38, 39 However, the MTA Diversity Report did not provide a breakdown of sex by age; therefore, we do not know the percentage of male MTA employees over the age of 50 years. Furthermore, we did not have information about union membership by sex and age, so we were unable to estimate mortality rates within these demographic groups. Another study that identified COVID‐19 deaths among MTA transit workers through May 6, 2020, reported a similar relationship of an increasing mortality with increasing age.33 The distribution of ages among NYC metro area transit worker decedents was skewed towards older age categories compared with the published age distribution of all transit workers.33 Tenure among NYC metro area transit worker decedents was higher than tenure identified in the literature search. Our study did not find any information on the decedents race or level of education.
Some underlying conditions are linked to a higher risk of COVID‐19 complications or death.38 Only four transit worker decedent media reports that we reviewed described an underlying condition, and the unions did not have co‐morbidity data for union members. This is likely an underestimation of the decedents in this study who had an underlying condition. A previous investigation reported approximately 40% of MTA transit workers had one or more underlying health problems.40 Previous studies have also indicated bus and subway operators are at higher risk for cardiovascular diseases and abdominal obesity compared with the general population.11, 16, 23, 41
At a national level, people of color, non‐U.S. born persons, and people with household incomes below the federal poverty level are overrepresented among transit workers.24 Persons in these demographic groups might have higher risk of occupational exposure to SARS‐CoV‐2, and in combination with other challenges (e.g., health and social inequities), an elevated risk for COVID‐19 complications. We found among the 30 ATU and TWU transit worker decedents with a known place of birth, nearly 77% were born outside the United States. In this study, country of birth is unknown for 75% of our ATU and TWU transit worker decedents; however, an article by the American Public Health Association reported approximately 33% of COVID‐19 deaths occurred among foreign‐born workers in the United States.42 Therefore, to effectively design worker safety and health protocols, public health professionals and employers should be aware of these important disparities that result in disproportionate exposure to SARS‐CoV‐2. The demographics of workers should be considered to ensure protocols are inclusive and information is communicated in a culturally appropriate way.
When looking at job classifications and public contact, we found more than half of the decedents were categorized as an operator job classification or had a position defined as having public contact. NYC metro area transit workers in operator job categories spend a large portion of their work shift in close contact with the public. Epidemiologic studies have indicated workers who have contact with a large number of people, especially in a congregate setting, have a higher exposure risk.43, 44 Therefore, management should provide control measures and training to transit workers who work in positions with public contact to reduce their potential for exposure to SARS‐CoV‐2 while on the job; control measures may include physical changes to their work space, changes to policies and procedures, and equipment to protect themselves while performing their job duties.45
This study has some limitations. First, media scanning likely missed COVID‐19 deaths among ATU and TWU workers. Decedents whose cause of death was not disclosed or did not have a publicly accessible notice that would have been captured by media scanning would not be included. This was partially addressed by the assistance provided by the ATU and TWU, but still relied on family members agreeing to releasing the decedents information. Therefore, these data are probably an underrepresentation of the actual COVID‐19 deaths among this population. In addition, information about decedents obtained through media reports and union records were often incomplete and lacked information about occupational characteristics (e.g., job title, tenure, location), demographics and anthropometrics (e.g., age, gender, body mass index, smoking status), underlying conditions (e.g., diabetes mellitus, hypertension, chronic respiratory diseases), and COVID‐19 symptoms. Information on whether decedents became infected with SARS‐CoV‐2 through work or community transmission was not available. Finally, because of a delay in reporting COVID‐19 deaths to union leadership, the last recorded fatality in this analysis occurred on June 6, 2020. More fatalities are likely to have occurred during June 6–July 7, 2020 that were not captured during our data collection process, thus underestimating the actual number of deaths in this population.
Despite these limitations, this study used a timely data collection approach, captured information on a relatively large number of deaths drawn from a defined worker population, captured a longer reporting period, and was able to examine the occurrence of those deaths with respect to COVID‐19 deaths in the community. We found that, in the absence of an active surveillance program, this method—using media scanning through Google alerts to comb publicly available data on the internet for key terms—was an efficient and unintrusive method to identify cases in an essential worker population. Lastly, by recording the specific dates of deaths, we were able to demonstrate that the trend in deaths among this essential worker population mirrored the temporal relationship of COVID‐19 deaths in NYC as a whole.
Because of the nature of their work, transit workers in public facing positions are unable to perform their job duties at home and are an essential workforce for local economies, including providing transportation to work for other essential workers such as healthcare professionals, law enforcement, and grocers. Although COVID‐19 deaths over time were similar for NYC transit workers compared with overall NYC residents (Figure 2), our findings highlight important demographic differences among transit worker populations compared with the general population. Transit workers occupational exposures may put them at higher risk for SARS‐COV‐2 infection, but their demographic characteristics may put transit workers at higher risk for COVID‐19 complications. This study highlights the importance for public health professionals to consider the occupational and demographic characteristics of a specific population, such as transit workers, when developing effective public health guidance.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
DISCLOSURE BY AJIM EDITOR OF RECORD
John Meyer declares that he has no conflict of interest in the review and publication decision regarding this article.
AUTHOR CONTRIBUTIONS
Suzanne Tomasi: data acquisition, data analysis, manuscript preparation, and manuscript review. Alejandra Ramirez‐Cardenas: data acquisition, data analysis, manuscript preparation, and manuscript review. Matthew S. Thiese: literature review, data analysis, manuscript preparation, and manuscript review. Jessica L. Rinsky: study design, data analysis, manuscript preparations, and manuscript review. Sophia K. Chiu: study design, data analysis, manuscript preparations, and manuscript review. Sara Luckhaupt: study design, data analysis, manuscript preparations, and manuscript review. Russell Bateman: data acquisition and manuscript review. Sherry L. Burrer: study design, data analysis, manuscript preparations, and manuscript review.
DISCLAIMER
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
ACKNOWLEDGMENTS
The authors thank Brendan Danaher, TWU representative who assisted confirming and collecting data, Alexis Grimes Trotter, NIOSH and Sarah Selica Miura, NIOSH for their assistance with data abstraction and SAS coding.
Tomasi SE, Ramirez‐Cardenas A, Thiese MS, et al. COVID‐19 mortality among Amalgamated Transit Union (ATU) and Transport Workers Union (TWU) workers—March–July 2020, New York City metro area. Am J Ind Med. 2021;64:723‐730. 10.1002/ajim.23281
ENDNOTE
See for example, 45 C.F.R. part 46; 21 C.F.R. part 56; 42 U.S.C. §241(d), 5 U.S.C. §552a, 44 U.S.C. §3501 et seq.
REFERENCES
- 1.WHO Director‐General's opening remarks at the media briefing on COVID‐19, 11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed February 17, 2021.
- 2.West MG. First case of coronavirus confirmed in New York State. Wall Street Journal 2020. https://www.wsj.com/articles/first-case-of-coronavirus-confirmed-in-new-york-state-11583111692. Accessed February 17, 2021.
- 3.NYC Health . NYC Health Coronavirus Disease 2019 (COVID‐19) Daily Data Summary. covid‐19‐daily‐data‐summary‐04162020‐1.pdf (nyc.gov). Accessed June 15, 2021.
- 4.Vazquez J, Shea T, Rajamani M, Price B, Intarasuwan K. Timeline: Tracking the Spread of COVID‐19 in Tri‐State. 2020. https://www.nbcnewyork.com/news/local/timeline-tracking-the-spread-of-covid-19-in-tri-state/2313123/. Accessed December 2020.
- 5.Greve JE2020. US state governors impose tighter restrictions to slow coronavirus spread. https://www.theguardian.com/us-news/2020/mar/20/new-york-coronavirus-andrew-cuomo-non-essential-workers-businesses. Accessed February 17, 2021.
- 6.Transit Workers Union Local 100 . 2020. MTA About‐Face on Wearing Masks. http://www.twulocal100.org/story/mta-about-face-wearing-masks. Accessed April 12, 2021.
- 7.Guse C. MTA allows all transit workers to wear face masks amid coronavirus mania. 2020. NYC transit workers can wear masks amid coronavirus fears—New York Daily News (nydailynews.com). Accessed April 12, 2021.
- 8.Tracy T, Mcshane L. A tale of two agencies: NYC transit workers to receive nearly 250,000 N95 masks to protect against coronavirus; correction officers still fighting for PPE. New York Daily News. 2020. NYC transit workers get 250,000 N95 masks for coronavirus—New York Daily News (nydailynews.com). Accessed February 17, 2021.
- 9.Joseph E, Levenson E. New Yorkers must wear masks when unable to socially distance, Gov. Guomo says. CNN. 2020. https://www.cnn.com/2020/04/15/us/new-york-facemasks/index.html. Accessed February 17, 2021.
- 10.French SA, Harnack LJ, Toomey TL, Hannan PJ. Association between body weight, physical activity and food choices among metropolitan transit workers. Int J Behav Nutr Phys Act. 2007;4:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Winkleby MA, Ragland DR, Fisher JM, Syme SL. Excess risk of sickness and disease in bus drivers: a review and synthesis of epidemiological studies. Int J Epidemiol. 1988;17(2):255‐262. [DOI] [PubMed] [Google Scholar]
- 12.Anderson R. The back pain of bus drivers. Prevalence in an urban area of California. Spine. 1992;17(12):1481‐1488. [DOI] [PubMed] [Google Scholar]
- 13.Aronsson G, Rissler A. Psychophysiological stress reactions in female and male urban bus drivers. J Occup Health Psychol. 1998;3(2):122‐129. [DOI] [PubMed] [Google Scholar]
- 14.Barak D, Djerassi L. Musculoskeletal injuries among bus drivers due to motor vehicle accidents and hazardous environmental conditions. Ergonomics. 1987;30(2):335‐342. [DOI] [PubMed] [Google Scholar]
- 15.Evans GW. Working on the hot seat: urban bus operators. Accid Anal Prev. 1994;26(2):181‐193. [DOI] [PubMed] [Google Scholar]
- 16.Ragland DR, Krause N, Greiner BA, Fisher JM. Studies of health outcomes in transit operators: policy implications of the current scientific database. J Occup Health Psychology. 1998;3(2):172‐187. [DOI] [PubMed] [Google Scholar]
- 17.Leigh P, Markowitz S, Fahs M, Landrigan PJ. Burden and Costs of Occupational Injuries and Diseases in the United States. Ann Arbor, Michigan: U of Michigan Press; 2000. [Google Scholar]
- 18.Leigh JP, Robbins JA. Occupational disease and workers' compensation: coverage, costs, and consequences. Milbank Q. 2004;82(4):689‐721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greiner BA, Ragland DR, Krause N, Syme SL, Fisher JM. Objective measurement of occupational stress factors—an example with San Francisco urban transit operators. J Occup Health Psychol. 1997;2(4):325‐342. [DOI] [PubMed] [Google Scholar]
- 20.Tapp LC, Baron S, Bernard B, Driscoll R, Mueller C, Wallingford K. Physical and mental health symptoms among NYC transit workers seven and one‐half months after the WTC attacks. Am J Ind Med. 2005;47(6):475‐483. [DOI] [PubMed] [Google Scholar]
- 21.Chillrud SN, Grass D, Ross JM, et al. Steel dust in the New York City subway system as a source of manganese, chromium, and iron exposures for transit workers. J Urban Health. 2005;82(1):33‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cunradi CB, Chen MJ, Lipton R. Association of occupational and substance use factors with burnout among urban transit operators. J Urban Health. 2009;86(4):562‐570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krause N, Ragland DR, Fisher JM, Syme SL. Psychosocial job factors, physical workload, and incidence of work‐related spinal injury: a 5‐year prospective study of urban transit operators. Spine. 1998;23(23):2507‐2516. [DOI] [PubMed] [Google Scholar]
- 24.Rho HJ, Brown H, Fremstad S. A basic demographic profile of workers in frontline industries. Center for Economic and Policy Research. 2020:7. [Google Scholar]
- 25.Maroko AR, Nash D, Pavilonis BT. COVID‐19 and inequity: a comparative spatial analysis of New York City and Chicago hot spots. J Urban Health. 2020;97(4):461‐470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Penna C, Mercurio V, Tocchetti CG, Pagliaro P. Sex‐related differences in COVID‐19 lethality. Br J Pharmacol. 2020;177(19):4375‐4385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li X, Xu S, Yu M, et al. Risk factors for severity and mortality in adult COVID‐19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146(1):110‐118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ramírez IJ, Lee J. COVID‐19 emergence and social and health determinants in Colorado: a rapid spatial analysis. Int J Environ Res Public Health. 2020;17(11):3856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.The Lancet . The plight of essential workers during the COVID‐19 pandemic. Lancet. 2020;395(10237):1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Metropolitan Transportation Authority . Diversity Committee Meeting Report. February 26, 2020. https://new.mta.info/document/14686. Accessed February 17, 2021.
- 31.NYC Department of City Planning . NYC Department of City Planning Metro Region Explorer. https://metroexplorer.planning.nyc.gov. Accessed December 15, 2020.
- 32.Lowinger R, Rombom H. The effectiveness of cognitive behavioral therapy for PTSD in New York City transit workers: a preliminary evaluation. North Am J Psychol. 2012;14:471‐484. [Google Scholar]
- 33.Leffler CT, Hogan MC. Age‐dependence of Mortality from Novel Coronavirus Disease (COVID‐19) in Highly Exposed Populations: New York Transit Workers and Residents and Diamond Princess Passengers. 2020. https://www.medrxiv.org/content/medrxiv/early/2020/05/18/2020.05.14.20094847.full.pdf. Accessed February 17, 2021.
- 34.NYC OpenData . COVID‐19 Daily Counts of Cases, Hospitalizations, and Deaths. 2020. https://data.cityofnewyork.us/Health/COVID-19-Daily-Counts-of-Cases-Hospitalizations-an/rc75-m7u3. Accessed April 22, 2021.
- 35.Olayinka OO, Bayleyegn TM, Noe RS, Lewis LS, Arrisi V, Wolkin AF. Evaluation of Real‐Time Mortality Surveillance Based on Media Reports. Disaster Med Public Health Prep. 2017;11(4):460‐466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Morton M, Levy JL. Challenges in disaster data collection during recent disasters. Prehosp Disaster Med. 2011;26(3):196‐201. [DOI] [PubMed] [Google Scholar]
- 37.Waeckerle JF. Disaster planning and response. N Engl J Med. 1991;324(12):815‐821. [DOI] [PubMed] [Google Scholar]
- 38.Palaiodimos L, Kokkinidis DG, Li W, et al. Severe obesity, increasing age and male sex are independently associated with worse in‐hospital outcomes, and higher in‐hospital mortality, in a cohort of patients with COVID‐19 in the Bronx, New York. Metabolism. 2020;108:154262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus‐infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061‐1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gershon R. Impact of COVID‐19 Pandemic on NYC Transit Workers: Pilot Study Findings. NYU School of Global Public Health. October 2020. https://www.nyu.edu/content/dam/nyu/publicAffairs/documents/PDF/GershonTransitWorkerPilotStudy. Accessed February 17, 2021.
- 41.Pyo J, Lee M, Ock M, et al. Bus workers' experiences with and perceptions of a health promotion program: a qualitative study using a focus group discussion. Int J Environ Res Public Health. 2020;17(6):1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Krisberg K. COVID‐19 killing front‐line health workers, especially people of color. The Nation's Health: APHA. 50(8), 2020:14. [Google Scholar]
- 43.Anderson EL, Turnham P, Griffin JR, Clarke CC. Consideration of the Aerosol Transmission for COVID‐19 and Public Health. Risk Anal. 2020;40(5):902‐907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID‐19): a review. JAMA. 2020;324(8):782‐793. [DOI] [PubMed] [Google Scholar]
- 45.CDC . COVID‐19 Employer Information for Bus Transit Operators. 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/organizations/bus-transit-operator.html. Accessed April 15, 2021.


