Abstract
Introduction
The COVID‐19 pandemic has presented a major challenge to mental health and emotional wellbeing. The present study examined whether training in emotional intelligence (EI) skills, provided before the pandemic, would serve as a protective factor for sustaining mental health during the COVID‐19 crisis.
Methods
Data came from a longitudinal study (N = 89) that was initially designed to test the effectiveness of an EI training program versus a non‐emotion‐focused placebo program. The design and timing of the study were such that baseline and posttraining assessments of depression and anxiety had been completed before the pandemic, and planned 6‐month follow‐ups were serendipitously scheduled to occur after the onset of the COVID‐19 crisis. This provided us with an unexpected real‐world opportunity to investigate whether EI training would bolster emotional resilience to the challenges posed by the COVID‐19 pandemic.
Results
Although mental health concerns generally increased after the start of the pandemic, individuals who completed the EI training program scored lower on depression, suicidal ideation, and state anxiety relative to individuals who had been assigned to the placebo training program.
Conclusion
Online EI training appears to be effective at sustaining critical aspects of mental health during a subsequent real‐life crisis.
Keywords: anxiety, COVID‐19, depression, emotional intelligence, emotional intelligence training
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) has posed a significant threat to mental health and emotional wellbeing. The contagious and deadly nature of the SARS‐CoV‐2 virus can lead to fears of infection, worries about family members' health, grief over the loss of loved ones, and potential trauma from surviving an active COVID‐19 infection (Bo et al., 2020; Dai et al., 2020; Taylor et al., 2020; Wang et al., 2020). Strategies to contain the spread of the virus have been associated with increased feelings of loneliness and social isolation (Killgore et al., 2020) and have also introduced many personal and economic stressors as people grapple with unemployment, changing work roles, and disruptions to daily routine (Achdut & Refaeli, 2020; Kniffin et al., 2021). In addition, the uncertainty surrounding COVID‐19, the relative lack of control over events, and the long‐term nature of the pandemic may tax people's abilities to effectively cope with such issues and can, in turn, further exacerbate mental health challenges (Bosewell et al., 2013). Taken together, the features of the COVID‐19 pandemic have created a climate in which mental health disorders could emerge and persist. In fact, since the start of the pandemic, studies have documented increasing rates of mental health problems, including stress, depression, and anxiety (Wang et al., 2020), loneliness and suicidal ideation (Killgore et al., 2020), emotional distress (Shanahan et al., 2020), and posttraumatic stress disorder (Johnson et al., 2020).
As an increasing amount of evidence shows a worsening of psychiatric outcomes, there has been an emphasis on identifying potential protective factors that can help reduce the mental health consequences of the pandemic (Holmes et al., 2020; Killgore et al., 2020). Given that the negative emotions elicited by the pandemic are likely to play a central role in the development of mood and anxiety disorders (Watson et al., 1988), one possible protective factor that may confer psychological resilience is a set of skills, abilities, and competencies known as emotional intelligence (Extermera, 2020). Emotional intelligence (EI) can be defined as the ability to perceive, use, understand, and manage emotions in oneself and others (Mayer et al., 2000). Previous research has found relationships between EI and positive mental health outcomes (Schutte et al., 2007) through a number of mechanisms, including abilities to accurately perceive, understand, and regulate negative emotions, use of adaptive coping strategies (Zeidner et al., 2006), and having satisfying social relationships and stronger social support networks (Lopes et al., 2003; Zeidner & Matthews, 2016). Individuals with higher levels of EI may, therefore, have greater abilities and resources to adaptively navigate the emotional challenges posed by this pandemic.
In support of the notion that EI may serve as a protective factor for mental health, several recent studies have examined the benefits of EI during the COVID‐19 pandemic. Higher EI was linked to the lower intensity of negative emotions experienced during a week of lockdown (Moroń & Biolik‐Moroń, 2021), decreased depression, stress, and anxiety in frontline nurses (Sun et al., 2020), the use of effective coping strategies for handling government‐mandated preventative restrictions (Prentice et al., 2020), and higher levels of social support (Zysberg & Zisberg, 2020). However, these studies are limited by cross‐sectional designs, and it is, therefore, difficult to draw any causal conclusions regarding EI and mental health outcomes, and it remains uncertain whether it is possible to equip individuals with these skills in a way that would bolster resilience to a real‐life stressful experience.
Before the COVID‐19 outbreak, our lab had been conducting a longitudinal study on the effectiveness of a web‐based EI training program and had found promising results related to the program's ability to increase EI scores (Alkozei et al., 2019; Persich et al., 2021). As initially designed, the study contained three assessment timepoints—a baseline assessment, an assessment immediately following completion of the training program, and a 6‐month follow‐up assessment. These assessments included measures of depression and anxiety at all three timepoints as indicators of emotional functioning. The timing of the study was such that the 6‐month follow‐up assessments were scheduled to begin in April of 2020. However, the United States experienced the initial outbreak of COVID‐19 in February 2020 and a state of emergency was declared in March 2020, resulting in a serendipitous opportunity to evaluate the effectiveness of the prepandemic intervention at sustaining mental health after the outset of the pandemic. Specifically, our data include two prepandemic assessments and one assessment following the start of the pandemic, giving us a real‐world opportunity to investigate whether training EI skills would help people respond more adaptively to the emotional challenges faced during COVID‐19. We expected that depression and anxiety would increase for all participants between the posttreatment assessment and 6‐month follow‐up due to the stress of the pandemic, but also that the EI training would provide protection against the stressful effects of the pandemic, such that rates of depression, suicidal ideation, and anxiety would be lower among individuals who underwent the EI training program 6‐months earlier.
2. METHODS
In September of 2019, our lab began a longitudinal study to assess the effectiveness of an emotional intelligence intervention. This intervention was a web‐based training program that took approximately 9–11 hours to complete over the course of several days (roughly 1–1.5 h/day) and targeted key emotional skills such as perceiving emotions in oneself and others, understanding emotions, using emotions in adaptive ways, and regulating one's own and other's emotions (Mayer et al., 2000; for more details see Persich et al., 2021) Participants were recruited from a large university and surrounding metropolitan area in the Southwestern United States. Participants completed a baseline assessment (T1) and were then randomly assigned to take either the emotional intelligence training (EIT) program or a matched placebo awareness training (PAT) program of similar duration and complexity that trained external (i.e., nonemotional) awareness (e.g., focusing on learning to categorize plants and animals in different environments). Upon completion of their assigned program, participants completed a posttraining assessment (T2). Six months after the T2 assessments, these participants were contacted to complete the long‐term follow‐up assessment (T3). All T1 and T2 assessments were completed before March 17, 2020. The first government‐mandated “stay‐at‐home” orders to control the spread of the virus were initiated on March 19, 2020, between the last T2 session and the first T3 session. All T3 assessments were initiated after April 21, 2020. Due to the pandemic, participants completed the T3 assessments online and were provided some flexibility in their response window for completing the long‐term follow‐up assessment. The majority of participants (87%) did complete their T3 assessment 6 months from their T2 assessment between April and September of 2020, with the remainder of the sample completing in October (11%), November (1%), or December (1%) (Overall M = 202 days from T2 assessment date). The study officially concluded on December 15, 2020.
The study began with a sample of n = 448 participants at T1 and n = 326 at T2. However, a large number of these participants were not eligible to participate in the 6‐month follow‐up due to being debriefed after T2. A total of 89 participants completed assessments at all three timepoints, M age = 23.5, SD age = 5.59, 70.8% female, 7.9% Asian, 3.4% Black or African American, 66.3% Caucasian, 19.1% Latino or Hispanic, 2.2% more than one race, 1.1% preferred not to say. Among the 89 participants, n = 52 had been assigned to the EIT program and n = 37 had been assigned to the PAT program. At each timepoint, the participants completed the Beck Depression Inventory (BDI‐II), a 21‐item scale that measures symptoms of depression (Beck et al., 1996). Each item on the BDI is scored from 0 to 3, with higher scores being consistent with depressive symptomatology. This scale also contains one item assessing suicidal ideation (i.e., item 9). Participants also completed the State–Trait Anxiety Inventory (STAI), which is a 40‐item scale that measures anxiety at the present moment (state anxiety), and in general (trait anxiety) (Spielberger, 1983).
Analyses were conducted using SPSS 26. We first checked whether the reported sample with complete data sets for all three timepoints significantly differed from the larger initial sample that did not complete the long‐term follow‐up. We then examined potential factors that may explain additional variance in the outcomes. In particular, we targeted age, gender, race, and length of time between the start of the pandemic and when the participant completed the T3 assessment. In addition, we conducted independent‐samples t tests to determine whether there were baseline differences between program conditions. We then quantified the BDI and STAI scores in terms of clinical cutoffs (Julian, 2011; Smarr & Keefer, 2011) to test whether clinical rates increased between pre‐ and mid‐pandemic assessments. Finally, to examine our main hypothesis that the EIT program would serve as a protective factor, we conducted a series of two (EIT, PAT) × three (T1, T2, T3) repeated‐measures analyses of variance (ANOVAs).
3. RESULTS
Participants who took part in the 6‐month follow‐up (n = 89) did not significantly differ from those who did not (n = 359) in terms of their program condition, χ 2 = 1.71, p = .191, age, t(446) = .44, p = .663; race, χ 2(7) = 4.81, p = .683; or gender, χ 2(1) = 0.11, p = .739. Participants who took part in the 6‐month follow‐up had lower depression scores at T1 (M = 5.89, SD = 5.25) relative to those who did not (M = 7.79, SD = 7.21), t(446) = 2.34, p = .020. However, they did not differ on any of the other outcome measures, either at T1, ps = .189 – .499, or T2, ps = .623 – .914. Regarding the key sample that had complete data sets for all three timepoints, there were no significant differences between participants in the EIT and PAT programs in terms of age, gender, length of time between the start of the pandemic and assessment, or baseline depression and anxiety scores, as shown in Table 1. Age, race, sex, and time additionally did not correlate with the study outcomes in this sample, ps = .084– .993. We, therefore, did not include these measures as covariates in the main analyses.
Table 1.
Demographics and baseline differences in age, race, gender, depression, and anxiety, and timing of T3 assessments
| Total | PAT | EIT | Significance test | |
|---|---|---|---|---|
| Age | M = 23.5 (5.59) | M = 22.92 (4.99) | M = 23.92 (5.99) | t(87) = −.79, p = .432 |
| Race | χ 2 (5) = 3.62, p = .604 | |||
| Asian or Pacific Islander | n = 7 (7.9%) | n = 4 (10.8%) | n = 3 (5.8%) | |
| Black or African American | n = 3 (3.4%) | n = 1 (2.7%) | n = 2 (3.4%) | |
| Latino or Hispanic | n = 17 (19.1%) | n = 7 (18.9%) | n = 10 (19.1%) | |
| White or Caucasian | n = 59 (66.3%) | n = 24 (64.9%) | n = 35 (67.3%) | |
| More than one race | n = 2 (2.2%) | n = 0 (0%) | n = 2 (3.8%) | |
| Prefer not to say | n = 1 (1.1%) | n = 1 (2.7%) | n = 0 (0%) | |
| Gender | χ 2 (1) = .01, p = .928 | |||
| Male | n = 26 (29.2%) | n = 11 (29.7%) | n = 15 (28.8%) | |
| Female | n = 63 (70.8%) | n = 26 (70.3%) | n = 37 (71.2%) | |
| BDI | ||||
| Somatic | M = 2.25 (1.86) | M = 2.38 (1.85) | M = 2.15 (1.88) | t(87) = .56, p = .578 |
| Cognitive–affective | M = 3.64 (4.01) | M = 3.37 (3.68) | M = 3.83 (4.43) | t(87) = −.52, p = .606 |
| Total | M = 5.89 (5.25) | M = 5.76 (5.03) | M = 5.98 (5.45) | t(81) = −.20, p = .842a |
| Suicidal Ideation | M = .04 (.21) | M = .03 (.16) | M = .06 (.24) | t(87) = −.68, p = .497 |
| Anxiety | ||||
| State anxiety | M = 29.11 (7.89) | M = 27.97 (5.23) | M = 29.92 (9.30) | t(83) = −1.26, p = .212a |
| Trait anxiety | M = 36.00 (10.18) | M = 35.19 (9.12) | M = 36.58 (10.93) | t(87) = −.63, p = .529 |
| Timing | ||||
| Days from pandemic start | M = 124.18 days (62.21) | M = 119.11 days (61.94) | M = 127.79 days (62.74) | t(78) = −.65, p = .519a |
| Completed in April | n = 10 (11.2%) | n = 5 (13.5%) | n = 5 (9.6%) | |
| May | n = 19 (21.3%) | n = 8 (21.6%) | n = 11 (21.1%) | |
| June | n = 6 (6.7%) | n = 2 (5.4%) | n = 4 (7.6%) | |
| July | n = 9 (10.1%) | n = 4 (10.8%) | n = 5 (9.6%) | |
| August | n = 21 (23.6%) | n = 9 (24.3%) | n = 12 (23.1%) | |
| September | n = 12 (13.5%) | n = 4 (10.8%) | n = 8 (15.4%) | |
| October | n = 10 (11.2%) | n = 5 (13.5%) | n = 5 (9.6%) | |
| November | n = 1 (1.1%) | n = 0 (0%) | n = 1 (1.1%) | |
| December | n = 1 (1.1%) | n = 0 (0%) | n = 1 (1.1%) | |
Abbreviations: BDI, Beck Depression Inventory; EIT, emotional intelligence training; PAT, placebo awareness training.
Adjusted for unequal variances.
Without regard to training conditions, the present descriptive statistics highlight the negative consequences of the COVID‐19 pandemic for mental health and adds to the growing literature on the increasing rates of anxiety and depression. On the basis of the clinical cut‐off scores, only 1.1% of the sample met the criteria for moderate to severe levels of depression based on their BDI score at T1 (BDI > 20; Smarr & Keefer, 2011). By T3, however, this number had grown such that 15.7% of the sample reported moderate to severe depression. Similarly, only 4.4% of participants reported some level of suicidal ideation at T1, but this number increased to 14.4% by T3. Finally, participants meeting the recommended cutoff score for probable clinical anxiety (STAI‐S > 40; Julian, 2011) increased from 11.2% at T1 to 40.0% at T3. This is consistent with evidence that mental health issues increased during the early months of the pandemic (Killgore et al., 2021).
To examine whether the EIT program served as a protective factor against the stresses of the pandemic, we conducted a series of two (EIT, PAT) × three (T1, T2, T3) repeated‐measures ANOVAs. For depressive symptoms, there was a significant effect of program × time on BDI Total scores, F(2, 174) = 3.60, p = .029, η p 2 = 0.04. As shown in Figure 1, participants in the EIT condition demonstrated significantly lower BDI scores at T2 relative to those in the PAT condition, suggesting that the program was effective at reducing depressive mood. Moreover, these scores remained lower in the EIT group than the PAT group at T3. A similar effect was found for suicidal thoughts, F(2, 174) = 3.79, p = .024, η p 2 = 0.04, such that participants in the EIT conditions had lower mean suicidal ideation at T3 than the PAT group, as shown in Figure 2. The EIT program also had a protective effect on state anxiety, F(2, 174) = 4.19, p = .017, η p 2 = 0.05, with a less steep slope for those in the EIT group. This interaction is depicted in Figure 3. Finally, there was a marginal program × time effect predicting trait anxiety, F(2, 174) = 3.04, p = .050, η p 2 = 0.03, shown in Figure 4.
Figure 1.
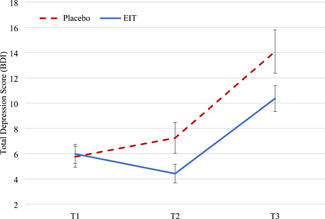
Total depression score as a function of time and program condition (mean ± 1 SE). BDI, Beck Depression Inventory; EIT, emotional intelligence training
Figure 2.
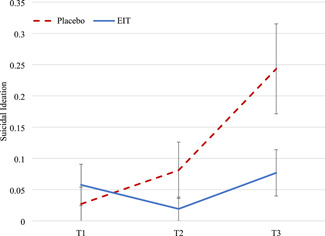
Suicidal ideation as a function of time and program condition. Suicidal ideation is quantified as the mean score (±1 SE) on item 9 of the Beck Depression Inventory. EIT, emotional intelligence training
Figure 3.
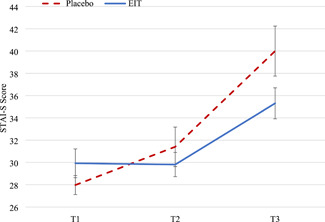
State anxiety as a function of time and program condition (mean ± 1 SE). EIT, emotional intelligence training; STAI‐S, State–Trait Anxiety Inventory (state anxiety)
Figure 4.
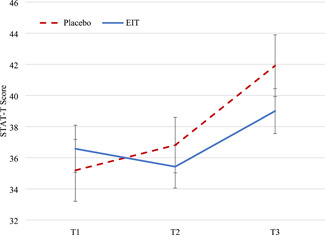
Trait Anxiety as a function of time and program condition (mean ± 1 SE). EIT, emotional intelligence training; STAI‐T, State–Trait Anxiety Inventory (trait anxiety)
Comparisons of the results reveal some differential patterns of the effect of EIT on depression and anxiety symptoms over time. In particular, depression was lower for individuals in the EIT condition at both T2 and T3 but demonstrated a similar increase between timepoints for both conditions. By contrast, individuals in the PAT condition tended to show steeper increases between T2 and T3 for suicidal ideation and anxiety relative to the EIT condition. We hypothesized that this differential pattern may be driven by the somatic component of the BDI (Whisman et al., 2000), as these symptoms (i.e., changes in sleep, fatigue, loss of energy, difficulty concentrating, and changes in appetite) could result from less controllable aspects of the pandemic and processes that may not be as strongly affected by emotional intelligence (e.g., lockdown and social distancing policies affecting circadian rhythms; Murray et al., 2020). Therefore, we would expect that the EIT program would largely help people manage the cognitive–affective symptoms of depression, but would have a lesser effect on somatic symptoms.
Accordingly, we conducted an exploratory follow‐up analysis of depression using the two‐factor structure of the BDI (Whisman et al., 2000). As shown in Figure 5, there was a significant program × time interaction predicting the cognitive–affective component of the BDI, F(2, 174) = 5.36, p = .006, η p 2 = 0.06. Moreover, the pattern of cognitive‐affective symptoms over time was similar to the patterns of suicidal ideation and anxiety. Conversely, there was no significant time × program interaction for the somatic component of the BDI, F(2, 174) = 1.46, p = .235, η p 2 = 0.02, with both groups demonstrating similar levels of somatic symptoms at T3.
Figure 5.
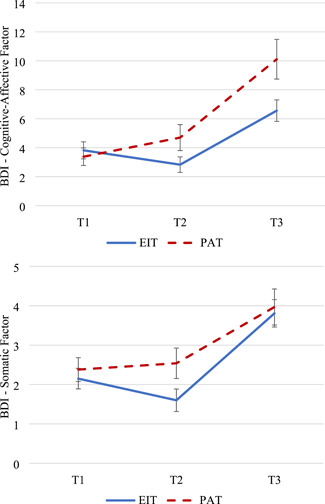
Follow‐up analyses of the BDI demonstrating the cognitive‐affective factor (top) and the somatic factor (bottom) of the BDI as a function of time and program condition (mean ± 1 SE). BDI, Beck Depression Inventory; EIT, emotional intelligence training; PAT, placebo awareness training
4. DISCUSSION
Consistent with prior studies, we found that the COVID‐19 pandemic had an adverse effect on mental health. This longitudinal study showed that clinical levels of depression and anxiety increased significantly among a sample of individuals who were relatively healthy before the pandemic. Moreover, we found that individuals who completed an EI training program had notably lower levels of depression, suicidal ideation, and state anxiety relative to individuals who had been assigned to a matched nonemotional placebo awareness program. These findings suggest that the online EI training program was effective at protecting individuals against the adverse mental health effects of the pandemic relative to a placebo program without emotion‐focused content.
These findings are consistent with previous research linking EI to positive mental health outcomes (Schutte et al., 2007; Zeidner et al., 2006) and are in line with other pandemic‐specific cross‐sectional studies that find EI to be beneficial (Moroń & Biolik‐Moroń, 2021; Prentice et al., 2020; Sun et al., 2020; Zysberg & Zisberg, 2020). The experimental nature of the study extends this previous work by allowing us to make causal inferences about the role of EI and to rule out possible bidirectional effects (e.g., increased stress and attentional demands harming emotional processing abilities; Matthews et al., 2015). Further, the unfortunate but serendipitous timing of the pandemic in the course of the study provided a serious and consequential real‐life stressor that allowed an authentic testing of the effectiveness of the EIT program at sustaining mental health and resilience. Thus, the current study provides support for the clinical implications of EI and EI training and suggests that helping people develop the emotional skills needed to accurately perceive, understand, and regulate their negative emotions may be important for mitigating the mental health problems associated with the pandemic.
The present study also provides support for the effectiveness and external validity of our EIT program. The program we created, and previously validated (Persich et al., 2021), was specifically designed to build critical emotional skills, with the ultimate goal of enhancing resilience in the face of major stressors and emotion‐eliciting events, such as military combat or disasters. Previous validation efforts on earlier versions of this training had established the ability of the EIT program to increase EI scores (Alkozei et al., 2019; Persich et al., 2021). However, the COVID‐19 pandemic provided a unique opportunity to test whether the program could be helpful during a worldwide crisis characterized by high levels of stress and negative emotions. The findings that individuals in the EIT program demonstrated significantly lower levels of depression and anxiety at follow‐up than their counterparts in the placebo group are encouraging for the practical usefulness of the program. The web‐based nature of the EIT program also makes it possible to safely administer the program to a wide population without the need for in‐person coaching or training sessions. In addition, these findings may promote further applications of the program in other emotionally challenging contexts, such as stressful and hazardous occupations (e.g., military and first responders) and jobs characterized by high levels of emotional labor (Joseph & Newman, 2010).
It should be noted that this study was not initially designed to be a study of COVID‐19‐related mental health. Rather, it was originally conceived as a basic validation study of the EIT program, and just so happened to intersect with the start of the pandemic. As a result, there remain several limitations and questions for future research to address. Most importantly, although we found that the EIT program was protective for mental health during the pandemic, we do not have in‐depth data to uncover the precise mechanism by which it did so. However, the differential patterns for symptoms across time, and our exploratory follow‐up analysis of the BDI suggests one possible mechanism, namely that the training may have helped people more adaptively manage their cognitive and affective responses to the pandemic (relative to somatic responses). The COVID‐19 pandemic has been highly disruptive, sometimes in ways that are insensitive to personal characteristics and operate outside of one's personal control. EI training is not expected to be a panacea that makes people immune from all disruptions and challenges related to the COVID‐19 pandemic, and, in fact, individuals in the EIT condition reported similar levels of somatic symptoms as those in the placebo program. However, the training may have helped individuals respond to negative and disruptive experiences without the cognitive distortions, sense of hopelessness, personal distress, and dysregulated affect that contributes to depression, suicidal ideation, and anxiety (Klonsky & May, 2015; Raj et al., 2020). Future research may benefit by further investigating the particular mechanisms through which EI helps individuals adaptively manage the emotional challenges of COVID‐19, and by exploring whether there are particular components of EI training that are especially beneficial (Extermera, 2020).
The present study did not find significant relationships between demographic characteristics of the sample and psychopathologic outcomes. However, the interpretation of these results should be qualified by the size, composition, and timing of the present sample. Previous research has identified disparities related to age, gender, and race/ethnicity for both illness and mortality (Carethers, 2021), and for the social, psychological, and economic impacts of the COVID‐19 pandemic (Kantamneni, 2020; Ruprecht et al., 2021). The present sample was primarily composed of young adults (M age = 23.5) residing in the United States and was 66.3% Caucasian. Moreover, the study's small sample size meant that many racial/ethnic minority subgroups were underrepresented (see Table 1) and limited our ability to conduct meaningful between‐group comparisons. Although it will be difficult to replicate the precise situational context in which the present data were collected, it will be important to investigate the effects of EIT on mental health in larger samples, including in‐depth examinations of whether gender, age, or race/ethnicity moderate the effects. Finally, it should be noted that the majority of the data were collected between April and September of 2020, and the study largely concluded before the surge of COVID‐19 cases in the United States during the winter of 2020. Again, the sample size was not sufficiently large enough to examine the systematic effects of timing, which is an important limitation as COVID‐19 rates and associated stressors have fluctuated throughout the course of the pandemic. Future research would benefit by investigating whether the benefits of EIT vary as a function of the severity and the nature of experienced stressors.
In conclusion, we find evidence suggesting that training in EI skills before the onset of the COVID‐19 pandemic provided protection against adverse mental health outcomes once the pandemic was underway. The pandemic had a profound effect on mental health outcomes and will likely continue to have an effect as the world struggles to understand, control, and cure the virus. Even as vaccines provide a possible pathway back to “normal,” it will likely be a long road to full recovery from the physical, mental, social, and economic consequences of the pandemic (Taylor & Asmundson, 2020). A key objective for mental health and public health experts will be to find ways to lessen the long‐term mental health impact of these adverse circumstances. The present research suggests that building emotional intelligence skills may be a critical component of such efforts.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
ACKNOWLEDGMENT
This project was supported by a grant from the U.S. Army Medical Research and Development Command (USAMRDC) to William D. S. Killgore (W81XWH‐16‐1‐0062).
Persich, M. R. , Smith, R. , Cloonan, S. A. , Woods‐Lubbert, R. , Strong, M. , & Killgore, W. D. S. (2021). Emotional intelligence training as a protective factor for mental health during the COVID‐19 pandemic. Depression Anxiety, 38, 1018–1025. 10.1002/da.23202
DATA AVAILABILITY STATEMENT
The data and materials that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Achdut, N. , & Refaeli, T. (2020). Unemployment and psychological distress among young people during the COVID‐19 pandemic. Psychological resources and risk factors. International Journal of Environmental Research and Public Health, 17, 7163. 10.3390/ijerph17197163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkozei, A. , Smith, R. , Demers, L. A. , Weber, M. , Berryhill, S. M. , & Killgore, W. D. S. (2019). Increases in emotional intelligence after an online training program are associated with better decision‐making on the Iowa Gambling Task. Psychological Reports, 122, 853–879. 10.1177/0033294118771705 [DOI] [PubMed] [Google Scholar]
- Beck, A. T. , Steer, R. A. , & Brown, G. (1996). Beck Depression Inventory‐II (BDI‐II). Psychological Corporation. [Google Scholar]
- Bo, H. X. , Li, W. , Yang, Y. , Wang, Y. , Zhang, Q. , Cheung, T. , Wu, X. , & Xiang, Y. (2020). Posttraumatic stress syndrome and attitude toward crisis mental health services among clinically stable patients with COVID‐19 in China. Psychological Medicine, 51, 1–2. 10.1017/S0033291720000999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosewell, J. F. , Thompson‐Holland, J. , Farchione, T. J. , & Barlow, D. H. (2013). Intolerance of uncertainty: A common factor in the treatment of emotional disorders. Journal of Clinical Psychology, 69, 630–645. 10.1002/jclp.21965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carethers, J. M. (2021). Insights into disparities observed with COVID‐19. Journal of Internal Medicine, 289, 463–473. 10.1111/joim.13199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai, Y. , Hu, G. , Xiong, H. , Qiu, H. , & Yuan, X. (2020). Psychological impact of the coronavirus disease 2019 (COVID‐19) outbreak on healthcare workers in China. MedRxiv, 1–22. 10.1101/2020.03.03.20030874 [DOI] [Google Scholar]
- Extermera, N. (2020). Coping with the stress caused by the COVID‐19 pandemic: Future research agenda based on emotional intelligence. International Journal of Social Psychology, 35, 631–638. 10.1080/02134748.2020.1783857 [DOI] [Google Scholar]
- Holmes, E. A. , O'Connor, R. C. , Perry, V. H. , Tracey, I. , Wessely, S. , Arseneault, L. , Ballard, C. , Christensen, H. , Cohen Silver, R. , Everall, I. , Ford, T. , John, A. , Kabir, T. , King, K. , Madan, I. , Michie, S. , Przybylski, A. K. , Shafran, R. , Sweeney, A. , … Bullmore, E. (2020). Multidisciplinary research priorities for the COVID‐19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7, 547–560. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, S. U. , Ebrahimi, O. V. , & Hoffart, A. (2020). PTSD Symptoms among health care workers and public service providers during the COVID‐19 outbreak. PLOS One, 15, e0241032. 10.1371/journal.pone.0241032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph, D. L. , & Newman, D. A. (2010). Emotional intelligence: An integrative meta‐analysis and cascading model. Journal of Applied Psychology, 95, 54–78. [DOI] [PubMed] [Google Scholar]
- Julian, L. J. (2011). Measures of anxiety. Arthritis Care & Research, 63, 1–11. 10.1002/acr.20561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kantamneni, N. (2020). The impact of the COVID‐19 pandemic on marginalized populations in the United States: A research agenda. Journal of Vocational Behavior, 119, e103439. 10.1016/j.jvb.2020.103439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore, W. D. S. , Cloonan, S. A. , Taylor, E. C. , & Dailey, N. S. (2020). Loneliness: A signature mental health concern in the era of COVID‐19. Psychiatry Research, 290, 113117. 10.1016/j.psychres.2020.113117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore, W. D. S. , Cloonan, S. A. , Taylor, E. C. , & Dailey, N. S. (2021). Mental health during the first weeks of the COVID‐19 pandemic in the United States. Frontiers in Psychiatry, 12, 561898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore, W. D. S. , Taylor, E. C. , Cloonan, S. A. , & Dailey, N. S. (2020). Psychological resilience during the COVID‐19 lockdown. Psychiatry Research, 291, 113216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky, E. D. , & May, A. M. (2015). The three‐step theory (3ST): A new theory of suicide rooted in the “ideation‐to‐action” framework. International Journal of Cognitive Therapy, 8, 114–129. 10.1521/ijct.2015.8.2.114 [DOI] [Google Scholar]
- Kniffin, K. M. , Narayanan, J. , Anseel, F. , Antonakis, J. , Ashford, S. P. , Bakker, A. B. , Bamberger, P. , Bapuji, H. , Bhave, D. P. , Choi, V. K. , Creary, S. J. , Demerouti, E. , Flynn, F. J. , Gelfand, M. J. , Greer, L. L. , Johns, G. , Kesebir, S. , Klein, P. G. , Lee, S. Y. , … Vugt, M. V. (2021). COVID‐19 and the workplace: Implications, issues, and insights for future research and action. American Psychologist, 76(1), 63–77. 10.1037/amp0000716 [DOI] [PubMed] [Google Scholar]
- Lopes, P. N. , Salovey, P. , & Straus, R. (2003). Emotional intelligence, personality, and the perceived quality of social relationships. Personality and Individual Differences, 35, 641–658. 10.1016/S0191-8869(02)00242-8 [DOI] [Google Scholar]
- Matthews, G. , Pérez‐González, J. , Fellner, A. N. , Funke, G. J. , Emo, A. K. , Zeidner, M. , & Roberts, R. D. (2015). Individual differences in facial emotion processing: Trait emotional intelligence, cognitive ability, or transient stress? Journal of Psychoeducational Assessment, 33, 68–82. 10.1177/0734282914550386 [DOI] [Google Scholar]
- Mayer, J. D. , Salovey, P. , & Caruso, D. R. (2000). Models of emotional intelligence. In (Ed.) Sternberg, R. J. , Handbook of Intelligence (pp. 396–420). Cambridge University Press. [Google Scholar]
- Moroń, M. , & Biolik‐ Moroń, M. (2021). Trait emotional intelligence and emotional experiences during the COVID‐19 pandemic outbreak in Poland: A daily diary study. Personality and Individual Differences, 168, 110348. 10.1016/j.paid.2020.110348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray, G. , Gottlieb, J. , & Swartz, H. A. (2020). Maintaining daily routines to stabilize mood: Theory, data, and potential intervention for circadian consequences of COVID‐19. The Canadian Journal of Psychiatry, 66, 9–13. 10.1177/0706743720957825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persich, M. , Smith, R. , Cloonan, S. , Woods‐Lubbert, R. , Skalamera, J. , Berryhill, S. , Weihs, K. , Lane, R. D. , Allen, J. J. B. , Dailey, N. , Alkozei, A. , Vanuk, J. , & Killgore, W. (2021). Development and validation of an online emotional intelligence training program. Psyarxiv. 1–44. 10.31234/osf.io/u945j [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prentice, C. , Zeidan, S. , & Wang, X. (2020). Personality, trait EI, and coping with COVID‐19 measures. International Journal of Disaster Risk Reduction, 51, 101789. 10.1016/j.ijdrr.2020.101789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raj, S. , Ghosh, D. , Singh, T. , Verma, S. K. , & Arya, Y. K. (2020). Theoretical mapping of suicidal risk factors during the COVID‐19 pandemic: A mini‐review. Frontiers in Psychiatry, 11, 589614. 10.3389/fpsyt.2020.589614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruprecht, M. M. , Wang, X. , Johnson, A. K. , Xu, J. , Felt, D. , Ihenacho, S. , Stonehouse, P. , Curry, C. W. , DeBroux, C. , Costa, D. , & Phillips, G. (2021). Evidence of social and structural COVID‐19 disparities by sexual orientation, gender identity, and race/ethnicity in an urban environment. Journal of Urban Health, 98, 27–40. 10.1007/s11524-020-00497-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schutte, N. S. , Malouff, J. M. , Thorsteinsson, E. B. , Bhullar, N. , & Rooke, S. E. (2007). A meta‐analytic investigation of the relationship between emotional intelligence and health. Personality and Individual Differences, 42, 921–933. 10.1016/j.paid.2006.09.003 [DOI] [Google Scholar]
- Shanahan, L. , Steinhoff, A. , Bechtiger, L. , Muarry, A. L. , Nivette, A. , Hepp, U. , Ribeaud, D. , & Eisner, M. (2020). Emotional distress in young adults during the COVID‐19 pandemic: Evidence of risk and resilience from a longitudinal cohort study. Psychological Medicine. Advance online publication. 1–10. 10.1017/S003329172000241X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smarr, K. L. , & Keefer, A. L. (2011). Measures of depression and depressive symptoms. Arthritis Care & Research, 63, 454–466. 10.1002/acr.20556 [DOI] [PubMed] [Google Scholar]
- Spielberger, C. D. (1983). State‐Trait Anxiety Inventory for adults. Mind Garden. [Google Scholar]
- Sun, H. , Wang, S. , Wang, W. , Han, G. , Liu, Z. , Wu, Q. , & Pang, X. (2020). Correlation between emotional intelligence and negative emotions of front‐line nurses during the COVID‐19 epidemic: A cross sectional study. Journal of Clinical Nursing, 30, 385–396. 10.1111/jocn.15548 [DOI] [PubMed] [Google Scholar]
- Taylor, S. , & Asmundson, G. J. G. (2020). Life in a post‐pandemic world: What to expect of anxiety‐related conditions and their treatment. Journal of Anxiety Disorders, 72, 102231. 10.1016/j.janxdis.2020.102231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, S. , Landry, C. A. , Paluszek, M. M. , Fergus, T. A. , McKay, D. , & Asmundson, G. J. G. (2020). Development and initial validation of the COVID stress scales. Journal of Anxiety Disorders, 72, 102232. 10.1016/j.janxdis.2020.102232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , Ho, C. , & Ho, R. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID‐19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17, 1–25. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson, D. , Clark, L. A. , & Carey, G. (1988). Positive and negative affectivity and their relation to anxiety and depression. Journal of Abnormal Psychology, 97, 346–353. [DOI] [PubMed] [Google Scholar]
- Whisman, M. A. , Perez, J. E. , & Ramel, W. (2000). Factor structure of the Beck Depression Inventory—Second Edition (BDI‐II) in a student sample. Journal of Clinical Psychology, 56, 545–551. [DOI] [PubMed] [Google Scholar]
- Zeidner, M. , & Matthews, G. (2016). Ability emotional intelligence and mental health: Social support as a mediator. Personality and Individual Differences, 99, 196–199. 10.1016/j.paid.2016.05.008 [DOI] [Google Scholar]
- Zeidner, M. , Matthews, G. , & Roberts, R. D. (2006). Emotional intelligence, adaptation, and coping. In Ciarrochi J., Forgas J., & Mayer J. D. (Eds.), Emotional intelligence in everyday life: A scientific inquiry (2nd ed., pp. 82–97). Psychology Press. [Google Scholar]
- Zysberg, L. , & Zisberg, A. (2020). Days of worry: Emotional intelligence and social support mediate worry in the COVID‐19 pandemic Advance online publication. Journal of Health Psychology, 1–10. 10.1177/1359105320949935 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data and materials that support the findings of this study are available from the corresponding author upon reasonable request.


