Abstract
The COVID‐19 pandemic rapidly changed genetic counseling services across the United States. At the University of Pennsylvania (UPenn), a large academic hospital in an urban setting, nearly all genetic counseling (GC) visits for adult–onset disorders within the Department of Neurology were conducted via secure videoconferencing (telegenetics) or telephone between March and December 2020. Although telemedicine services have been steadily emerging, many clinical programs, including the neurogenetics program at UPenn, had not built infrastructure or widely utilized these services prior to the pandemic. Thus, little is known about patient attitudes toward receiving clinical GC services remotely. From May 18 to October 18, 2020, all individuals seen remotely for GC in adult neurology via telephone or telegenetics were surveyed about their satisfaction with telehealth GC (N = 142), with a response rate of 42% (N = 60/142). Telephone and telegenetics services were referred to as ‘telehealth’ in the surveys to capture patient perspectives on all remote GC services, though the majority (N = 49/60) of these visits were completed via telegenetics. Surveys included the modified telehealth usability questionnaire (MTUQ), genetic counseling satisfaction scale (GCSS), and novel questions about future telehealth use. Preliminary results suggest that patients were satisfied with receiving remote GC services in adult neurology, with most participants strongly agreeing to all items about satisfaction with telehealth. Just 2% of participants preferred only in‐person visits in the future, but every participant was willing to consider using telehealth for future visits if their genetic counselor felt it was appropriate. Most participants preferred a hybrid model (73%), and some (25%) preferred only telehealth for future visits. Additionally, we found no differences in satisfaction with remote services based on visit type (initial vs. results disclosure) nor age. We conclude that remote GC is an acceptable method for the provision of services in adult neurology that is well‐received by patients.
Keywords: COVID‐19, genetic counseling, neurogenetics, telegenetics, telehealth, telemedicine
What is known about this topic
The COVID‐19 pandemic has resulted in a rapid transition of genetic counseling from traditional in‐person to remote counseling via telephone or videoconferencing (telegenetics). In genetic counseling, telephone and telegenetics use had been reported in the literature with overall positive results but published studies have been generally limited to oncogenetics services and research settings.
What this paper adds to this topic
In response to the COVID‐19 pandemic, telephone and telegenetics were used almost universally for clinical genetics care at the University of Pennsylvania. Our study assessed patient satisfaction with and attitudes toward remote genetic counseling in adult neurogenetics consultations during the pandemic.
1. INTRODUCTION
In March 2020, the United States recognized the outbreak of the SARS‐CoV‐2 virus, known as the coronavirus disease 2019 (COVID‐19) pandemic. Prior to the pandemic, there were reports of remote services being implemented and studied in neurology, neurogenetics, and genetic counseling (Achey et al., 2014; Alcalay et al., 2020; Cohen et al., 2016; Ekeland et al., 2010; Greenberg et al., 2020; Hilgart et al., 2012; Kane & Gillis, 2018; Mitchell & Demiris, 2005). Remote services have been described by the terms teleneurology, telemedicine, and telehealth (Achey et al., 2014; Alani, 2020; Alcalay et al., 2020; Cheney, 2020; Eberly et al., 2020; Ekeland et al., 2010; Kane & Gillis, 2018; Parmanto et al., 2016; Spindler et al., 2020; Wilkinson et al., 2016). In genetic counseling, the remote service delivery models have been defined as either ‘telephone genetic counseling’ for a session about a new indication conducted entirely via telephone, or ‘telegenetics’ for a web‐based videoconferencing or telemedicine genetic counseling visit (Cohen et al., 2012). However, telegenetics services have historically been underutilized in clinical genetic counseling. At least two different surveys from the National Society of Genetic Counselors (NSGC) have noted this, as one study reported that 37% of genetic counselor respondents had never used telegenetics before, and another found that only 7% reported using telegenetics ‘always’ or ‘often’ (Greenberg et al., 2020; Zierhut et al., 2018).
The traditional ‘in‐person’ genetic counseling model typically includes 1–2 in‐person visits with a genetics provider at a healthcare facility or private office (Cohen et al., 2012). Traveling to in‐person visits that may not be located nearby have resulted in reported cost and time burdens, and there is evidence that a decreasing number of patients are traveling far to reach such visits (Bradbury et al., 2016; Cohen et al., 2019; Greenberg et al., 2020; Solomons et al., 2018). However, expanding telegenetics services could alleviate these burdens and may also increase access to genetics services for traditionally underserved populations, including individuals living in rural areas, in communities of diverse socioeconomic status, or in communities without a local genetics provider (Boothe & Kaplan, 2018; Bradbury et al., 2016; Cohen et al., 2019; Greenberg et al., 2020). Still, studies report conflicting results when assessing which indications or situations are best suited for remote genetic counseling. A review of randomized controlled trials found telephone counseling to be non‐inferior to traditional in‐person genetic counseling in prenatal, oncology, and neurologic sub‐specialties, and at least one teleneurology study has noted that telegenetics expands access to genetics services (Athens et al., 2017; Chirra et al., 2019). Patients believe that telehealth and/or telegenetics can offer increased convenience, access to specialized and multidisciplinary care, and cost and time savings, and feel that these remote services result in higher perceived personal control (Abrams & Geier, 2006; Buchanan et al., 2016; Solomons et al., 2018; Wilkinson et al., 2016; Zilliacus et al., 2010, 2011). However, in‐person visits have been preferred by some patients, including those with a new cancer diagnosis, those having had multi‐gene testing, and those with higher reported anxiety, depression, cancer‐specific distress, and remaining uncertainty after their initial visit (Beri et al., 2019; Bradbury et al., 2018, 2011; Patrick‐Miller et al., 2010; Zilliacus et al., 2010). As these studies have shown, there are many factors that can influence a patient's receptiveness to receiving remote genetic counseling.
In response to the pandemic, the adult Neurology Department at the University of Pennsylvania (UPenn), a large academic hospital in an urban setting, quickly transitioned to a remote care delivery model for clinical consultations. Prior to March 2020, telemedicine visits in the UPenn Neurology Department accounted for about 0.05%–0.1% of weekly visits; March 13th was the last day of pre‐pandemic in‐person operations, and by April 1, 2020, more than 90% of outpatient visits were conducted via a secure, institutionally approved videoconferencing platform (Spindler et al., 2020). Given the rapid transition to telemedicine during the COVID‐19 pandemic, our team of four neurogenetics counselors sought to assess patient experience and satisfaction with exclusively remote clinical counseling.
2. STUDY AIMS
Our study was exploratory and hypothesis generating due to the preliminary nature and small sample size. We aimed to determine whether participants were satisfied with remote (telephone and telegenetics) genetic counseling in neurology. We evaluated whether visit type (initial vs. results disclosure) and patient age were associated with satisfaction with remote genetic counseling. We also explored participant willingness to use telehealth in the future. Finally, we aimed to assess whether there were differences in survey responders and non‐responders by race, gender, and age that could impact the significance of the results.
3. METHODS
3.1. Participants and procedures
Participants included individuals seen for remote (telegenetics or telephone) services by one of four board‐certified genetic counselors (GCs) in the UPenn Department of Neurology (LD, TB, RP, AB) for an initial or disclosure visit. Initial genetic counseling visits were typically 30–60 min and completed for individuals coming for outpatient neurogenetics with a personal and/or family history of a neurologic condition. Some patients saw a physician on the same day, while others were seen by the GC alone. At the initial genetics visit, patients were offered genetic testing if appropriate, or already had a genetic test result. Disclosure genetic counseling visits included review of diagnostic or predictive results. In addition to education about relevant conditions and genetic testing options, visits included psychosocial counseling to assess patients’ needs and to empower patients. Although the content of the genetic counseling sessions was unchanged by the transition to telephone and telegenetics, there was a major shift in workflow during remote visits, such as at‐home sample collection.
Survey invitations were sent by email to every individual who had a remote visit with a GC in neurology from May 18, 2020, through October 18, 2020; the invitation was sent within 24 hr after the visit. Study data were collected and managed using REDCap (Research Electronic Data Capture) tools hosted at UPenn (Harris et al., 2009, 2019). REDCap is a secure, web‐based software platform designed to support data capture for research studies. If a survey was not completed within two days, a reminder email was sent to potential participants at two and four days following the initial invitation. Surveys were sent to the email address on file for the participant; it was not assessed who was completing the survey, so ‘responders’ could be participants or their care partners. To avoid biased responses, participants were explicitly notified that their individual responses would remain anonymous. The study was classified as a quality improvement (QI) protocol by UPenn's Institutional Review Board (IRB); as such, no informed consent was required but implied informed consent was obtained for individuals who voluntarily completed the survey and submitted their responses.
3.2. Instrumentation
Basic demographic information including age, sex, race, and referral indication was collected from the medical record. The single survey included items from two questionnaires to assess satisfaction with genetic counseling and with telephone and telegenetics (referred to as ‘telehealth’ in the surveys) as outlined below.
3.2.1. Genetic Counseling Satisfaction Scale (GCSS)
Satisfaction with genetic counseling services was assessed via the Genetic Counseling Satisfaction Scale, originally developed and validated with strong internal consistency (Cronbach's alpha 0.8) by Tercyak et al. (2001). The GCSS contains six items, which are presented on a 5‐point Likert scale to assess participants’ perception of the GC’s understanding of and compassion toward their stressors and needs, and the participants’ perceived utility of the appointment content and length (Tercyak et al., 2001). The GCSS was digitized to be administered via REDCap (Table S1).
3.2.2. Modified Telehealth Usability Questionnaire (MTUQ)
Participant attitudes toward and experience with telehealth were evaluated using a modified version of the Telehealth Usability Questionnaire (TUQ), originally developed by Parmanto et al. (2016) as a 21‐item measure scored on a 7‐point Likert scale determined to have strong content validity and reliability (Cronbach's alpha >0.8 for all assessments). The modified version (MTUQ) includes six items from the TUQ that were selected for their focus on the participant's experience of healthcare via telehealth services, rather than on the telehealth service delivery platform itself. Items were revised such that when the original scale inquired about ‘healthcare services’, the modified version inquired about ‘neurogenetics services’. Similarly, the word ‘clinician’ was replaced with ‘genetic counselor’ for clarity. The scale was also modified to be presented on the same 5‐point Likert scale described for the GCSS above. This was done to provide consistent response options for the participants. In addition, two new items were added (MTUQ #7‐8) to assess whether participants would consider utilizing telehealth services for future genetic counseling visits (Table S2).
3.3. Data analysis
We calculated descriptive statistics of participant characteristics and main measures (GCSS and MTUQ). We used the Shapiro–Wilk normality test and determined that the datasets did not follow a normal distribution. Therefore, we used non‐parametric tests. Chi‐square tests were utilized to determine whether there were significant differences in the demographic characteristics (sex, race, and age) of those who responded to the survey versus those who did not respond to the survey. MTUQ responses were converted to numeric values of 1–5 from the Likert scale values of strongly disagree to strongly agree, respectively. A summary MTUQ score was calculated for each participant adding together individual responses to the 6‐item Likert scale (most agreeable score is 30, least is 5). A Mann–Whitney test was performed to assess whether mean satisfaction with telehealth differed by clinic visit type (initial vs. disclosure visit). A Brown–Forsythe one‐way ANOVA was performed to assess whether mean satisfaction with telehealth differed by age‐group.
4. RESULTS
The survey was sent to 142 patients who had a remote genetic counseling visit at the UPenn Neurogenetics clinic between May 18 and October 18, 2020. The overall response rate was 42% (60/142); individuals were considered a ‘responder’ if they answered at least one question. Several (8/60) responders did not answer the MTUQ items. All other responders (n = 52) completed the entire survey.
Responders and non‐responders did not differ in their sex (X 2 (1, N = 142) = 0.11, p = .74) or age (X 2 (5, N = 142) = 8.73, p = .12). However, the groups differed by race such that non‐White individuals were significantly less likely to respond to the survey than White individuals. The response rate of White individuals was 47% (57/122), while that of non‐White individuals was 15% (3/20) (X 2 (1, N = 142) = 7.09, p = .01) (Figure S1).
4.1. Responder demographics
Most responders (78%, n = 47/60) completed their survey after an initial genetic counseling visit. Initial consultations were more often completed via videoconferencing (93%, n = 44/47) than telephone. The remaining responders (22%, n = 13/60) completed their survey after a results disclosure visit. In contrast, disclosure visits were more often completed by phone (61%, n = 8/13) than video. In summary, 49 individuals were seen via videoconferencing (telegenetics) and 11 via telephone. A slight majority of the responders were female (53%, 32/60), and nearly all were White (95%, 57/60). Most responders (70%, 42/60) were 50–79 years old. See Table 1 for a complete summary of responder characteristics. Most survey responders were undergoing counseling to identify a genetic etiology for their condition (83%, 50/60). The remaining responders (17%, 10/60) were undergoing predictive genetic counseling for family history of a neurologic disease (Figure 1).
TABLE 1.
Demographics of responders
| Characteristic | N | % |
|---|---|---|
| Sex | ||
| Female | 32 | 53 |
| Male | 28 | 47 |
| Race | ||
| White | 57 | 95 |
| Black | 2 | 3 |
| American Indian or Alaska Native | 0 | 0 |
| Asian | 1 | 2 |
| Native Hawaiian or Other Pacific Islander | 0 | 0 |
| Age (years) | ||
| 18–29 | 4 | 7 |
| 30–39 | 8 | 13 |
| 40–49 | 6 | 10 |
| 50–59 | 12 | 20 |
| 60–69 | 16 | 27 |
| 70–79 | 14 | 23 |
| 80–89 | 0 | 0 |
| Visit type | ||
| Initial | 47 | 78 |
| Disclosure | 13 | 22 |
| Indication type | ||
| Diagnostic | 50 | 83 |
| Predictive | 10 | 17 |
Demographic characteristics are presented for survey responders. Also presented are visit type and indication/testing type of each responder.
FIGURE 1.
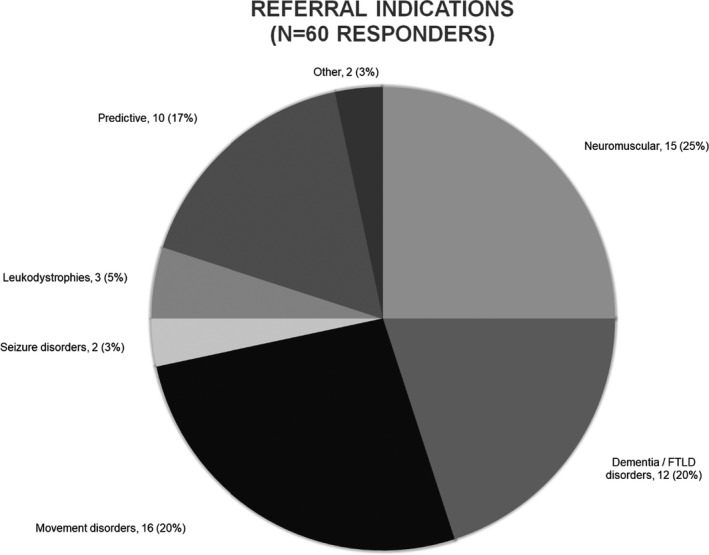
Referral Indications. A visual overview of participant diagnoses/referral indications. Those in the predictive category were referred for family history of various neurologic disorders such as those presented on this chart. Numbers represent N (% of cohort)
4.2. Satisfaction with telegenetics
Of the 60 responders, 52 responded to the MTUQ section of the survey that assessed satisfaction with genetic counseling via telephone or telegenetics (telehealth). A Mann–Whitney test found no significant difference with telehealth satisfaction between those responding to the survey after an initial visit versus after a results disclosure visit (U(N initial = 47, N disclosure = 13) = 290.5, p = .78, see Figure S2).
The youngest (18–29 years old) and oldest (70–79 years old) groups reported the highest satisfaction with telehealth (Figure S3). However, a Brown–Forsythe one‐way ANOVA found no significant difference in telehealth satisfaction between age‐groups (F(5,46) = 1.19, p = .33, Figure S4).
Overall satisfaction with telehealth services as assessed by MTUQ questions 1–6 was high (Figure 2). The majority of respondents strongly agreed that they were satisfied with the telehealth system overall (80%), would use telehealth services again (85%), felt comfortable communicating with the GC via telehealth (85%), and felt that telehealth improved access to neurogenetics services (73%). Most respondents strongly agreed that telehealth is an acceptable way to receive neurogenetics services (75%) and felt that telehealth provided for their neurogenetics needs (62%). One individual responded ‘strongly disagree’ to all items.
FIGURE 2.
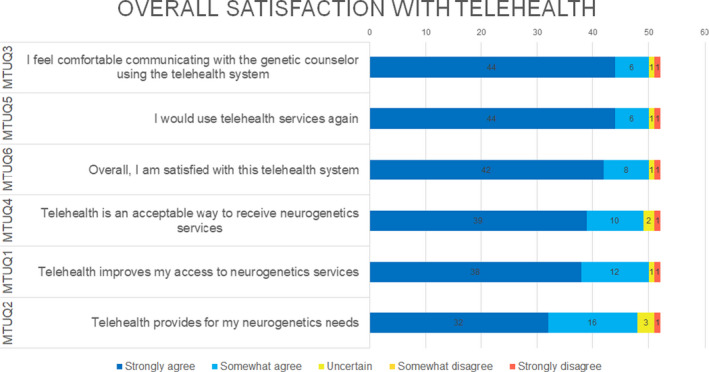
Overall satisfaction with telehealth. Responses to MTUQ questions 1–6 are presented for the N = 52 participants who responded to the MTUQ. Numbers displayed represent the number of responders
4.3. Satisfaction with genetic counseling
All responders completed the six GCSS items that assessed satisfaction with genetic counseling. Overall satisfaction with genetic counseling was high; responses to each item are shown in Figure 3. Survey results showed that most respondents strongly agreed that the GC session was valuable (87%) and about the right length of time (90%). Additionally, the majority of responders strongly agreed that the GC helped them to identify what they needed to know to make decisions (85%) and seemed to understand the stresses they were facing (82%). Similarly, 88% said they strongly agreed that the GC was truly concerned about their well‐being. The item with the most variable response was ‘I felt better about my health after meeting with my genetic counselor’. For this item, 50% of people strongly agreed and 23% somewhat agreed, while 20% of people were uncertain and 7% strongly disagreed.
FIGURE 3.
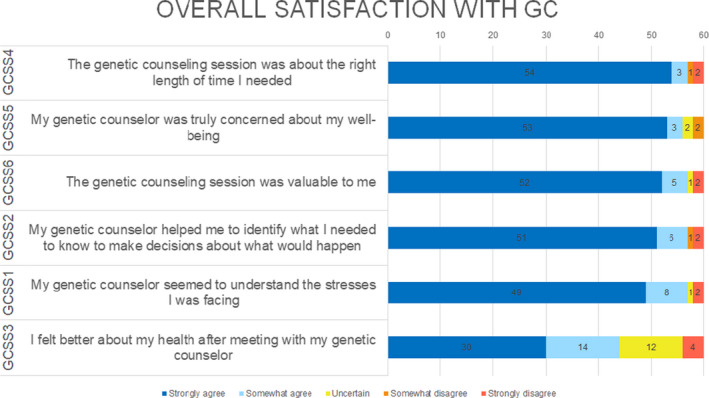
Overall satisfaction with genetic counseling. Responses to GCSS items 1–6 are presented for the N = 60 participants who responded. Numbers displayed represent the number of responders
4.4. Willingness to use telehealth and preferences for future visits
Participants who responded to the MTUQ were also asked about their attitudes toward future telehealth use for GC visits via MTUQ questions #7–8. Most (71%) reported they would use telehealth again. The remaining participants (29%) indicated ‘it depends’, while none said they would not use telehealth again (Figure 4). Similarly, most participants (73%) reported a preference for a combination of telehealth and in‐person visits in the future, while 25% would prefer telehealth only and 2% (1 participant) would prefer in‐person only (Figure 4).
FIGURE 4.
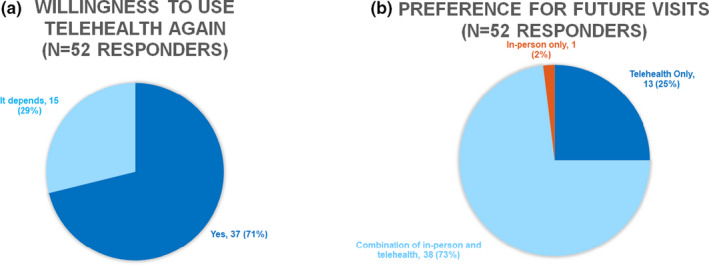
Willingness to use telehealth and preference for future visit types. N = 52 participants responded to MTUQ question 7 shown in panel a and question 8 shown in panel b. Numbers represent N (% of cohort)
5. DISCUSSION
Our study assessed patient experience and satisfaction with remote genetic counseling (GC). This survey was completed in the adult neurogenetics clinic after the rapid implementation of remote clinical care due to the COVID‐19 pandemic. In this hypothesis‐generating, quality improvement study, we demonstrate high patient satisfaction with telephone and telegenetics visits, high patient satisfaction with their GC in neurogenetics, and acceptance of and future interest in combination of in‐person and remote visits for neurogenetics services.
Though we combined telephone and videoconferencing (telegenetics) under the telehealth umbrella, the majority of our data are from individuals who had telegenetics visits. This is unique, considering much of the existing telehealth literature is dominated by studies of telephone counseling, and more work is needed to understand how patient preferences differ among different remote modalities. Our results suggest that remote GC is well‐received by patients and is a suitable method to provide GC. Continued use of remote services may remove known barriers to in‐person care such as time commitment and cost. In this study, satisfaction with remote GC did not differ significantly between age‐groups. Though there are limited data regarding remote services preferences by age‐group, there have been reports related to older individuals’ difficulties with traveling to in‐person visits, and reports of difficulties regarding cost, impact on work and childcare for adults with jobs and children when travel is required (Cheney, 2020; Solomons et al., 2018). We also hypothesize that younger individuals may be most comfortable with the technology used for telegenetics. Comfort with computers has been found to be a significant predictor of willingness to participate in telegenetics visits (Buchanan et al., 2015). Though younger individuals may have more experience with the technology needed for remote visits, descriptive studies have shown that older individuals are able to utilize telemedicine and telegenetics (Cheney, 2020; Solomons et al., 2018). Future studies with larger sample sizes will be useful in determining if there is a relationship between age and satisfaction with remote visits, while considering other confounding factors such as comfort with technology. Patients reported that they were willing to use telehealth for future visits, and some preferred telehealth over in‐person visits. Though more research about patients’ preferences will be needed after the pandemic ends to conclude that preferences were not influenced by the pandemic itself, this overall willingness to engage with remote services in the future may suggests that desire for remote services is not limited to pandemic times.
Much like the high levels of satisfaction seen with telehealth (telephone and telegenetics) in this study, patient satisfaction with GC overall was high. Outside of neurogenetics, patients have been found to have high satisfaction with GC (Pitini et al., 2019). Yet, there are considerable differences between neurology and other clinical settings, such as oncology and prenatal genetic counseling, that have more management options available for consideration. Still, most participants in our present study strongly agreed to items in the GCSS that assessed whether they found value in the visit and whether the counselor helped them to identify what they needed to know to make decisions for the future. In neurology, patients often receive genetic results that do not have an associated cure currently available. Our results from the present study and experience in the clinic suggest that patients are finding personal value in genetic counseling for neurologic diseases, such as empowerment and gaining information needed for life decision‐making. Additionally, the importance of a therapeutic relationship in healthcare has been well established and championed as integral to GC (Austin et al., 2014; McCarthy Veach et al., 2007). Nearly all the participants felt that their GC was truly concerned about their well‐being and understood the stress that they were facing, suggesting that patients in neurogenetics feel their psychosocial concerns are being met. Even when discussing the inherently challenging topic of neurologic disease, just under three quarters of participants felt better about their health after meeting with a GC.
5.1. Study limitations
The primary limitation is the small sample size, which constrained our ability to perform statistical analyses; therefore, these are preliminary data. Survey distribution is ongoing. However, given the limited available research on telegenetics and telemedicine satisfaction in the setting of the ongoing COVID‐19 pandemic, we feel these data may impact ongoing neurogenetics care outside of UPenn (see future directions).
As is true in any study, our data reflect the opinions of those who chose to respond to our survey; it is possible that non‐responders had different levels of satisfaction with remote genetic counseling and genetic counseling overall. Additionally, despite our explicit statement that participant responses would remain anonymous to their clinicians, it is possible that respondents engaged in socially desirable responding or those who did not have favorable opinions did not respond (Steenkamp et al., 2010). Satisfaction with remote services may have also been influenced by factors related to COVID‐19, and further research will be needed in the post‐pandemic era. Generalizability may also be limited given that non‐White patients were significantly less likely to respond to the survey.
An analysis limitation is that we were not able to evaluate satisfaction with telephone and telegenetics services separately. During the quick transition to remote GC, telephone counseling was utilized while awaiting institutional approval for novel videoconferencing platforms. Due to the relatively small sample of telephone genetic counseling cases, we consolidated all remote visits (telegenetics and telephone) whereas it would have been preferable to compare video to phone appointments as these are subjectively different experiences.
Three survey design limitations will be modified for ongoing data collection. First, there was not a mechanism for participants to indicate who was filling out the survey. This is relevant because care partners may have different opinions on telegenetics than the patients themselves. Second, respondents had to click forward to a second page to access the MTUQ questionnaire; this may explain why eight respondents did not answer those questions. A third limitation is that we did not collect qualitative data to better understand the context for participant responses There are additional limitations inherent to the surveys that were adapted for this study (Parmanto et al., 2016; Tercyak et al., 2001). The GCSS was originally assessed in a high‐risk prenatal setting with all female responders, a different population than our participants. The MTUQ is a validated scale, but only a select few items were used in this study and they were presented on a 5‐point rather than 7‐point Likert scale.
5.2. Future directions and research recommendations
Although the COVID‐19 pandemic will end, it is likely that there will be lasting changes to the provision of genetic counseling services (Bergstrom et al., 2020). Thus, it is imperative that GCs continue to explore patient experiences with alternative service delivery models to inform best practices. The data collected thus far have generated hypotheses to be tested in the future. We will explore other factors that may influence satisfaction such as diagnosis, result type, and timing of results. Additionally, we plan to collect GC outcome measures and data regarding the ease and comfort of collecting and returning genetic testing samples from home given this is a major shift in workflow and at least one center reported that patient compliance with sample return was an obstacle to remote care (Shannon et al., 2020). Qualitative designs such as free text responses or semi‐structured interviews may help us to better understand the nuances of individual preferences. It will be interesting to discern whether there are differences in visit type preferences during an era of pandemic precautions versus in a future era without pandemic precautions. We will also further characterize the non‐responders to determine whether there are key differences that may need to be addressed.
Furthermore, research is needed to better understand the influence of telemedicine on mitigating or exacerbating healthcare disparities among traditionally underserved populations. At least one study has found inequities in accessing telemedicine care during the COVID‐19 pandemic such that older patients, Asian patients, and non‐English‐speaking patients had lower rates of telemedicine use (Eberly et al., 2020). This, coupled with pre‐pandemic findings of racial disparity in access to genetic counseling and testing (Armstrong et al., 2015; Carroll et al., 2020), suggests GC and testing are not occurring at an acceptable rate for ethnic minority patients and telegenetics alone may not be enough to narrow the gap. Expanding genetic services to these groups is of great importance and may be realized through increasing targeted outreach and establishing relationships with community clinics and providers (Zhou et al., 2017).
5.3. Practice implications
Although it remains unclear whether nation‐wide neurogenetics services will have to return to an in‐person model after the pandemic accommodations expire, the present study supports incorporating a hybrid model of telehealth (telephone and telegenetics) and in‐person options based on patient‐reported preference and satisfaction. Further, the present study suggests that patients of all ages are able and willing use telehealth services; however, we may need to do more to adequately expand neurogenetics services to underserved populations. It remains unclear whether remote genetic counseling benefits underserved groups or exacerbates inequities; there have been conflicting data about access and preference from studies of community or rural populations (Boothe & Kaplan, 2018; Bradbury et al., 2016; Eberly et al., 2020; McDonald et al., 2014; Solomons et al., 2018). Throughout the United States, challenges for implementing telemedicine in neurology during the COVID‐19 pandemic have included patients’ access to internet or device use, as well as training both patients and clinicians on the telemedicine platform (Alani, 2020). Therefore, when planning for future telemedicine and telegenetics implementation, centers may need to consider a multitude of factors, such as available clinic resources for setup, management, training, and assistance/troubleshooting; patients’ overall comfort with computer use; ease of use of the platform chosen; patient preference; and/or patients' available internet access or devices for the consultation. As most participants preferred a combination of future telehealth and in‐person visits, a hybrid model may be best to implement moving forward. It is important to acknowledge that in‐person visits are still desired by some and may prove to be more valuable for certain indications or situations.
AUTHOR CONTRIBUTIONS
All authors were involved in manuscript revision, and all gave final approval of this version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Author TB confirms that she had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. TB was involved in conception, design, and data interpretation. LD was involved in conception, design, data acquisition and interpretation, and drafting. RP and AB were involved with interpretation of data and drafting. MB was involved in data acquisition and interpretation. PGA was involved in data analysis and interpretation. TT and AR were involved in conception and design.
COMPLIANCE WITH ETHICAL STANDARDS
CONFLICT OF INTEREST
TB receives consulting fees from Genome Medical, Inc., a telehealth company. PGA has received consulting fees unrelated to this work from Spark Therapeutics, Eisai Therapeutics and NeuExcell, research funding from the NIH and funds from clinical trial execution from BioHaven. TT reports no disclosures specific to this study. He has received grants from the NIH/NINDS (K23‐NS11416‐01A1), and research support from the Parkinson Foundation (PDGENEration Site Investigator) and The Michael J Fox Foundation. He has received consulting fees and honoraria from the Parkinson Foundation and Sanofi Genzyme. RP reports no financial disclosures for this study; she provides telegenetics counseling for the Parkinson Foundation's PDGENEration study. AR, LD, AB, and MB declare no conflicts of interest.
HUMAN STUDIES AND INFORMED CONSENT
This study was determined to be QI data collection per the UPenn IRB; no formal consent process was needed but individuals who voluntarily submitted responses implied their consent.
ANIMAL STUDIES
No non‐human animal studies were carried out by the authors for this article.
DATA SHARING AND DATA ACCESSIBILITY
The data that support the findings of this study are available within the article and from the corresponding author upon reasonable request.
Supporting information
Supplementary Material
Dratch, L., Paul, R. A., Baldwin, A., Brzozowski, M., Gonzalez‐Alegre, P., Tropea, T. F., Raper, A., & Bardakjian, T. (2021). Transitioning to telegenetics in the COVID‐19 era: Patient satisfaction with remote genetic counseling in adult neurology. Journal of Genetic Counseling, 30, 974–983. 10.1002/jgc4.1470
REFERENCES
- Abrams, D. J., & Geier, M. R. (2006). A comparison of patient satisfaction with telehealth and on‐site consultations: A pilot study for prenatal genetic counseling. Journal of Genetic Counseling, 15(3), 199–205. 10.1007/s10897-006-9020-0 [DOI] [PubMed] [Google Scholar]
- Achey, M., Aldred, J. L., Aljehani, N., Bloem, B. R., Biglan, K. M., Chan, P., Cubo, E., Ray Dorsey, E., Goetz, C. G., Guttman, M., Hassan, A., Khandhar, S. M., Mari, Z., Spindler, M., Tanner, C. M., van den Haak, P., Walker, R., Wilkinson, J. R., & International Parkinson and Movement Disorder Society Telemedicine Task Force (2014). The past, present, and future of telemedicine for Parkinson's disease. Movement Disorders, 29(7), 871–883. 10.1002/mds.25903 [DOI] [PubMed] [Google Scholar]
- Alani, J. (2020). Telemedicine: An opportunity to bring better care to all. https://www.neurologylive.com/view/telemedicine‐an‐opportunity‐to‐bring‐better‐care‐to‐all [Google Scholar]
- Alcalay, R. N., Kehoe, C., Shorr, E., Battista, R., Hall, A., Simuni, T., Marder, K., Wills, A.‐M., Naito, A., Beck, J. C., Schwarzschild, M. A., & Nance, M. (2020). Genetic testing for Parkinson disease: Current practice, knowledge, and attitudes among US and Canadian movement disorders specialists. Genetics in Medicine, 22(3), 574–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong, J., Toscano, M., Kotchko, N., Friedman, S., Schwartz, M. D., Virgo, K. S., & Sutphen, R. (2015). Utilization and outcomes of BRCA genetic testing and counseling in a national commercially insured population: The ABOUT study. JAMA Oncology, 1(9), 1251–1260. [DOI] [PubMed] [Google Scholar]
- Athens, B. A., Caldwell, S. L., Umstead, K. L., Connors, P. D., Brenna, E., & Biesecker, B. B. (2017). A systematic review of randomized controlled trials to assess outcomes of genetic counseling. Journal of Genetic Counseling, 26(5), 902–933. 10.1007/s10897-017-0082-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin, J., Semaka, A., & Hadjipavlou, G. (2014). Conceptualizing genetic counseling as psychotherapy in the era of genomic medicine. Journal of Genetic Counseling, 23(6), 903–909. 10.1007/s10897-014-9728-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergstrom, K. L., Brander, T. E., Breen, K. E., & Naik, H. (2020). Experiences from the epicenter: Professional impact of the COVID ‐19 pandemic on genetic counselors in New York. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 187(1), 28–36. 10.1002/ajmg.c.31855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beri, N., Patrick‐Miller, L. J., Egleston, B. L., Hall, M. J., Domchek, S. M., Daly, M. B., Ganschow, P., Grana, G., Olopade, O. I., Fetzer, D., Brandt, A., Chambers, R., Clark, D. F., Forman, A., Gaber, R., Gulden, C., Horte, J., Long, J., Lucas, T., … Bradbury, A. R. (2019). Preferences for in‐person disclosure: Patients declining telephone disclosure characteristics and outcomes in the multicenter Communication Of GENetic Test Results by Telephone study. Clinical Genetics, 95(2), 293–301. 10.1111/cge.13474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boothe, E., & Kaplan, J. (2018). Using telemedicine in Mississippi to improve patient access to genetic services. Journal of Genetic Counseling, 27(2), 320–322. 10.1007/s10897-017-0192-6 [DOI] [PubMed] [Google Scholar]
- Bradbury, A. R., Patrick‐Miller, L. J., Egleston, B. L., Hall, M. J., Domchek, S. M., Daly, M. B., Ganschow, P., Grana, G., Olopade, O. I., Fetzer, D., Brandt, A., Chambers, R., Clark, D. F., Forman, A., Gaber, R., Gulden, C., Horte, J., Long, J. M., Lucas, T., … Yao, X. (2018). Randomized noninferiority trial of telephone vs in‐person disclosure of germline cancer genetic test results. Journal of the National Cancer Institute, 110(9), 985–993. 10.1093/jnci/djy015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradbury, A. R., Patrick‐Miller, L., Fetzer, D., Egleston, B., Cummings, S. A., Forman, A., Bealin, L., Peterson, C., Corbman, M., O'Connell, J., & Daly, M. B. (2011). Genetic counselor opinions of, and experiences with telephone communication of BRCA1/2 test results. Clinical Genetics, 79(2), 125–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradbury, A., Patrick‐Miller, L., Harris, D., Stevens, E., Egleston, B., Smith, K., Mueller, R., Brandt, A., Stopfer, J., Rauch, S., Forman, A., Kim, R., Fetzer, D., Fleisher, L., Daly, M., & Domchek, S. (2016). Utilizing remote real‐time videoconferencing to expand access to cancer genetic services in community practices: A multicenter feasibility study. Journal of Medical Internet Research, 18(2), e23. 10.2196/jmir.4564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchanan, A. H., Datta, S. K., Skinner, C. S., Hollowell, G. P., Beresford, H. F., Freeland, T., Rogers, B., Boling, J., Marcom, P. K., & Adams, M. B. (2015). Randomized trial of telegenetics vs. in‐person cancer genetic counseling: Cost, patient satisfaction and attendance. Journal of Genetic Counseling, 24(6), 961–970. 10.1007/s10897-015-9836-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchanan, A. H., Rahm, A. K., & Williams, J. L. (2016). Alternative service delivery models in cancer genetic counseling: A mini‐review. Frontiers in Oncology, 6, 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll, N. M., Blum‐Barnett, E., Madrid, S. D., Jonas, C., Janes, K., Alvarado, M., Bedoy, R., Paolino, V., Aziz, N., McGlynn, E. A., & Burnett‐Hartman, A. N. (2020). Demographic differences in the utilization of clinical and direct‐to‐consumer genetic testing. Journal of Genetic Counseling, 29(4), 634–643. 10.1002/jgc4.1193 [DOI] [PubMed] [Google Scholar]
- Cheney, C. (2020). How to use telemedicine with your older patients. https://www.healthleadersmedia.com/clinical‐care/how‐use‐telemedicine‐your‐older‐patients [Google Scholar]
- Chirra, M., Marsili, L., Wattley, L., Sokol, L. L., Keeling, E., Maule, S., Sobrero, G., Artusi, C. A., Romagnolo, A., Zibetti, M., Lopiano, L., Espay, A. J., Obeidat, A. Z., & Merola, A. (2019). Telemedicine in neurological disorders: Opportunities and challenges. Telemedicine Journal and e‐Health, 25(7), 541–550. 10.1089/tmj.2018.0101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, S. A., Bradbury, A., Henderson, V., Hoskins, K., Bednar, E., & Arun, B. K. (2019). Genetic counseling and testing in a community setting: Quality, access, and efficiency. American Society of Clinical Oncology Educational Book, 39, e34–e44. 10.1200/EDBK_238937 [DOI] [PubMed] [Google Scholar]
- Cohen, S. A., Gustafon, S. L., Marvin, M. L., Riley, B. D., Uhlmann, W. R., Liebers, S. B., & Rousseau, J. A. (2012). Report from the National Society of Genetic Counselors Service Delivery Model Task Force: A proposal to define models, components, and modes of referral. Journal of Genetic Counseling, 21(5), 645–651. 10.1007/s10897-012-9505-y [DOI] [PubMed] [Google Scholar]
- Cohen, S. A., Huziak, R. C., Gustafson, S., & Grubs, R. E. (2016). Analysis of advantages, limitations, and barriers of genetic counseling service delivery models. Journal of Genetic Counseling, 25(5), 1010–1018. 10.1007/s10897-016-9932-2 [DOI] [PubMed] [Google Scholar]
- Eberly, L. A., Kallan, M. J., Julien, H. M., Haynes, N., Khatana, S. A. M., Nathan, A. S., Snider, C., Chokshi, N. P., Eneanya, N. D., Takvorian, S. U., Anastos‐Wallen, R., Chaiyachati, K., Ambrose, M., O’Quinn, R., Seigerman, M., Goldberg, L. R., Leri, D., Choi, K., Gitelman, Y., … Adusumalli, S. (2020). Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID‐19 pandemic. JAMA Network Open, 3(12), e2031640. 10.1001/jamanetworkopen.2020.31640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekeland, A. G., Bowes, A., & Flottorp, S. (2010). Effectiveness of telemedicine: A systematic review of reviews. International Journal of Medical Informatics, 79(11), 736–771. 10.1016/j.ijmedinf.2010.08.006 [DOI] [PubMed] [Google Scholar]
- Greenberg, S. E., Boothe, E., Delaney, C. L., Noss, R., & Cohen, S. A. (2020). Genetic counseling service delivery models in the United States: Assessment of changes in use from 2010 to 2017. Journal of Genetic Counseling, 29(6), 1126–1141. 10.1002/jgc4.1265 [DOI] [PubMed] [Google Scholar]
- Harris, P. A., Taylor, R., Minor, B. L., Elliott, V., Fernandez, M., O'Neal, L., McLeod, L., Delacqua, G., Delacqua, F., Kirby, J., & Duda, S. N. (2019). The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics, 95, 103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). A metadata‐driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilgart, J. S., Hayward, J. A., Coles, B., & Iredale, R. (2012). Telegenetics: A systematic review of telemedicine in genetics services. Genetics in Medicine, 14(9), 765–776. 10.1038/gim.2012.40 [DOI] [PubMed] [Google Scholar]
- Kane, C. K., & Gillis, K. (2018). The use of telemedicine by physicians: Still the exception rather than the rule. Health Affairs, 37(12), 1923–1930. 10.1377/hlthaff.2018.05077 [DOI] [PubMed] [Google Scholar]
- McCarthy Veach, P., Bartels, D. M., & LeRoy, B. S. (2007). Coming full circle: A reciprocal‐engagement model of genetic counseling practice. Journal of Genetic Counseling, 16(6), 713–728. 10.1007/s10897-007-9113-4 [DOI] [PubMed] [Google Scholar]
- McDonald, E., Lamb, A., Grillo, B., Lucas, L., & Miesfeldt, S. (2014). Acceptability of telemedicine and other cancer genetic counseling models of service delivery in geographically remote settings. Journal of Genetic Counseling, 23(2), 221–228. 10.1007/s10897-013-9652-9 [DOI] [PubMed] [Google Scholar]
- Mitchell, J. A., & Demiris, G. (2005). Telegenetics: The next phase in the provision of genetic services? Genetics in Medicine, 7(1), 1–2. [DOI] [PubMed] [Google Scholar]
- Parmanto, B., Lewis, A. N., Jr., Graham, K. M., & Bertolet, M. H. (2016). Development of the telehealth usability questionnaire (TUQ). International Journal of Telerehabilitation, 8(1), 3. 10.5195/ijt.2016.6196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick‐Miller, L., Bradbury, A. R., & Terry, M. B. (2010). Controversies in communication of genetic screening results for cancer: A report from the American Society of Preventive Oncology’s Screening Special Interest Group (ASPO’s 33rd Annual Meeting, March 8 to 10, 2009, Tampa, Florida). Cancer Epidemiology, Biomarkers & Prevention, 19(2), 624–627. 10.1158/1055-9965.EPI-19-2-ASPO01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitini, E., D’Andrea, E., Rosso, A., Massimi, A., Unim, B., De Vito, C., Marzuillo, C., & Villari, P. (2019). Genetic services for hereditary cancer: A systematic review of patient reported outcomes studies. European Journal of Public Health, 29(Suppl. 4), ckz186‐380. 10.1093/eurpub/ckz186.380 [DOI] [Google Scholar]
- Shannon, K. M., Emmet, M. M., Rodgers, L. H., Wooters, M., & Seidel, M. L. (2020). Transition to telephone genetic counseling services during the COVID‐19 pandemic. Journal of Genetic Counseling, 1–5. 10.1002/jgc4.1365 [DOI] [PubMed] [Google Scholar]
- Solomons, N. M., Lamb, A. E., Lucas, F. L., McDonald, E. F., & Miesfeldt, S. (2018). Examination of the patient‐focused impact of cancer telegenetics among a rural population: Comparison with traditional in‐person services. Telemedicine Journal and e‐Health, 24(2), 130–138. 10.1089/tmj.2017.0073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spindler, M., Jacobs, D., Yuan, K., Tropea, T., Teng, C. W., Perrone, C., Do, D., & Wechsler, L. (2020). A department approach to teleneurology. Telemedicine Journal and e‐Health. [Epub ahead of print]. 10.1089/tmj.2020.0323 [DOI] [PubMed] [Google Scholar]
- Steenkamp, J. B. E., De Jong, M. G., & Baumgartner, H. (2010). Socially desirable response tendencies in survey research. Journal of Marketing Research, 47(2), 199–214. 10.1509/jmkr.47.2.199 [DOI] [Google Scholar]
- Tercyak, K. P., Johnson, S. B., Roberts, S. F., & Cruz, A. C. (2001). Psychological response to prenatal genetic counseling and amniocentesis. Patient Education and Counseling, 43(1), 73–84. 10.1016/S0738-3991(00)00146-4 [DOI] [PubMed] [Google Scholar]
- Wilkinson, J. R., Spindler, M., Wood, S. M., Marcus, S. C., Weintraub, D., Morley, J. F., & Duda, J. E. (2016). High patient satisfaction with telehealth in Parkinson disease: A randomized controlled study. Neurology: Clinical Practice, 6(3), 241–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, Y., Elashoff, D., Kremen, S., Teng, E., Karlawish, J., & Grill, J. D. (2017). African Americans are less likely to enroll in preclinical Alzheimer's disease clinical trials. Alzheimer's & Dementia: Translational Research & Clinical Interventions, 3(1), 57–64. 10.1016/j.trci.2016.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zierhut, H. A., MacFarlane, I. M., Ahmed, Z., & Davies, J. (2018). Genetic counselors’ experiences and interest in telegenetics and remote counseling. Journal of Genetic Counseling, 27(2), 329–338. 10.1007/s10897-017-0200-x [DOI] [PubMed] [Google Scholar]
- Zilliacus, E. M., Meiser, B., Lobb, E. A., Kelly, P. J., Barlow‐Stewart, K., Kirk, J. A., Spigelman, A. D., Warwick, L. J., & Tucker, K. M. (2011). Are videoconferenced consultations as effective as face‐to‐face consultations for hereditary breast and ovarian cancer genetic counseling? Genetics in Medicine, 13(11), 933–941. 10.1097/GIM.0b013e3182217a19 [DOI] [PubMed] [Google Scholar]
- Zilliacus, E. M., Meiser, B., Lobb, E. A., Kirk, J., Warwick, L., & Tucker, K. (2010). Women’s experience of telehealth cancer genetic counseling. Journal of Genetic Counseling, 19(5), 463–472. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
The data that support the findings of this study are available within the article and from the corresponding author upon reasonable request.


