Abstract
Non-traumatic hepatic hernia is defined as hepatic protrusion through acquired or congenital defects on diaphragm without prior trauma. This event is rare among adults and infrequently reported in literature. 52-year-old Caucasian woman with surgically treated breast cancer with suspected lung metastasis detected during a routine Multidetector Computed Tomography lung exam. Ultrasound and subsequently Magnetic Resonance Imaging (MRI) was performed which revealed an overdiaphragmatic mass in contiguity with liver parenchyma compatible with overdiaphragmatic hepatic hernia. Differential diagnosis should be made with diaphragmatic or pulmonary nodule. Correct diagnosis can avoid further diagnostic investigations or invasive procedures such as biopsy. Magnetic Resonance Imaging is a non-risky method and can clarify interpretative doubts. Currently there are still controversies about traumatic or idiopathic nature of this hernia.
Keywords: Diaphragmatic Hernia, Pulmonary Nodules, Incidentally Found, Liver Herniation, Diaphragmatic Defect
Introduction
Non-traumatic intrathoracic hepatic hernia is rare and can be misdiagnosed as a pulmonary nodule [1]. Less than 35 cases have been described in literature in the last 60 years, all deriving from abdominal trauma [2]. Finding in absence of previous trauma is an occasional event and, as in our case, can occur in patients undergoing Computed Tomography (CT) during oncological follow-up or in patients undergoing chest high-resolution CT. It is important to recognize these hernias in order not to adopt inappropriate diagnostic approaches such as biopsy. Many imaging modalities can be used for diaphragm study: conventional radiographs (CR) usually offer first clue to diagnosis but do not recognize small hernias and do not allow a differential diagnosis with small atelectasis areas or pulmonary nodules. Doppler ultrasound (DU) allows to recognize overdiaphragmatic hepatic nodule and continuity of intranodular vascularization with that of liver allowing differential diagnosis. Magnetic Resonance Imaging (MRI) is a second level exam generally reserved for patients with uncertain CT diagnosis and can be used in patients allergic to CT contrast agent or with renal insufficiency. MRI can provide reconstructions in coronal, axial and sagittal planes for optimal visualization of entire hemidiaphragm when movement is limited by respiratory and cardiac gating [3].
Case presentation
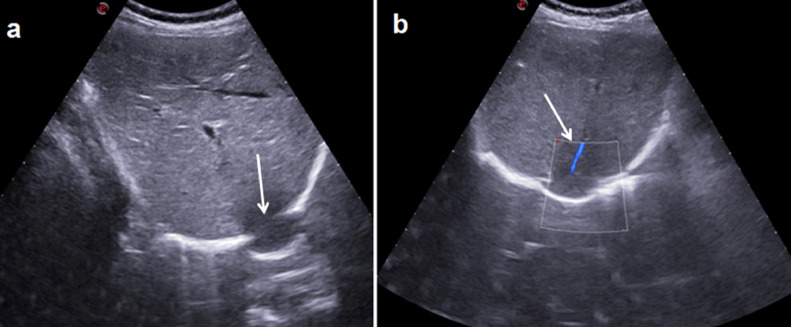
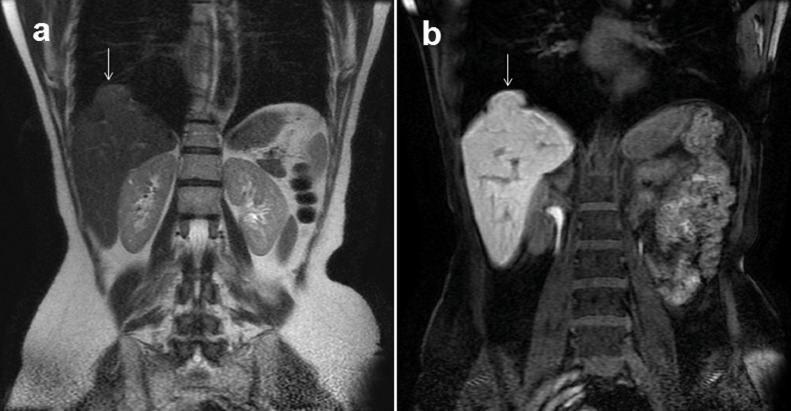
52-year-old Caucasian woman who came to our Radiology Department for appearance of a pulmonary nodule (35 mm in diameter) highlighted in a follow-up CT in right lower lung lobe in contiguity with diaphragm (Figs.1 a and b). Patient had a clinical history of left breast cancer diagnosed and treated with surgery, chemoradiotherapy, hormone therapy and radiotherapy two years previously. We subjected patient to Ultrasound and MRI. Ultrasound examination was performed with a MyLab ™ 9 device (Esaote) with a 3.5 MHz convex probe. B-Mode Ultrasound showed interruption of hyperechoic diaphragmatic line caused by a transdiaphragmatic hepatic hernia that appeared hypoechoic compared to remaining hepatic parenchyma (Fig. 2a). Color Doppler Ultrasound showed contiguity of intranodular vascularization with hepatic vascularization (Fig. 2b). Ultrasound was performed by an operator with 20 years of experience. MRI were performed using a 1.5 Tesla MRI scanner (Signa, GE). MRI confirmed herniation through diaphragm of hepatic parenchyma which appeared hyperintense on T2-weighted images and isointense on T1-weighted images (Fig.3 a); after hepatospecific contrast medium administration, in hepatocellular sequences, overdiaphragmatic nodule appeared isointense to hepatic parenchyma (Fig.3b). Patient was discharged after a few days and managed conservatively with short-term Ultrasound follow-up. Consent was obtained from the patient for publication of this case report and accompanying images.
Fig.1 – MDCT.
a: Coronal plane reconstruction shows an overdiaphragmatic nodular mass (arrow) in contact with hepatic surface best evident in 3D reconstruction -b (arrow) showing "hump sign".
Fig.2 – US.
a: B-Mode US scans show hepatic parenchyma herniation (long arrow) across a continuum of diaphragm (arrow). b: Color Doppler US shows a hepatic vessel (arrow) in continuity with herniated parenchyma.
Fig.3 – MR.
Coronal T2-weighted acquisition and spoiled GRE 3D-T1 weighted after intravenous administration of hepatospecific contrast agent-MR (Gd-EOB-DTPA, Primovist) (b) show herniation of hepatic tissue into thoracic cavity through a diaphragm defect. In T2-weighted acquisition (a) herniated tissue shows isointense signal with some weakly hyperintense areas referable to compressed liver parenchyma; in images after contrast agent-MR (b) it is possible to appreciate regular uptake of contrast agent and homogeneous signal with respect to underlying liver parenchyma which confirms hepatic origin of herniated tissue.
Discussion
Diagnosis of non-traumatic diaphragmatic hepatic hernia is difficult because it can be mistakenly confused with other pathologies such as lung neoplasms or diaphragmatic tumor implants as reported in literature [4,5,6]. Right diaphragmatic defect found incidentally may be due to several causes such as Bochdalek's hernia, which can be asymptomatic and undiagnosed until adulthood (0.17% incidence of congenital hernia diagnosed in adulthood) [7, 8] or it can arise as a consequence of abdominal trauma with incidence from 5% to 7% in diaphragmatic lesions and from 3% to 15% in penetrating lesions [9], with presentation that can be acute and symptomatic or asymptomatic and late. Other predisposing causes or factors described in literature are iatrogenic lesions from abdominal or thoracic surgery. Sanna S et al. [10,11] report spontaneous diaphragmatic abduction and hepatic hernia in patients with endometriosis (endometrial cells are aggressive and can invade diaphragm) [12]. Diaphragmatic hepatic hernia we described is of unknown type; patient was unaware of it and had no clinical history of trauma or surgery. In these cases, imaging is essential and allows us to locate lesion and make differential diagnosis. Desir and Ghaye [13] describe various CT signs that indicate diaphragmatic rupture: direct or indirect signs of rupture and signs of uncertain origin. Direct signs include a segmental diaphragmatic defect representing a sudden and focal loss of continuity in diaphragm. Dangling diaphragm is produced by free edge of torn diaphragm curling inward from its normal course. The sign of absent diaphragm is represented by absence of part or all of hemidiaphragm, usually associated with a large hernia. Indirect signs are represented by "collar sign" which corresponds to a constriction in diaphragmatic rupture site of herniated structure and can also be observed in congenital and acquired non-traumatic diaphragmatic hernias. The "hump" signs and "fascia" are both expressions of hepatic hernia through a rupture of right diaphragm: hump sign refers to shape of hepatic hernia placed over diaphragm that mimics a hump. The fascia sign corresponds to a linear area of hypoattenuation that dissects hepatic hernia between torn diaphragm flaps; it is hypothesized that it derives from compression, which causes hepatic hypoperfusion. Most CT signs of diaphragmatic lesions are also applicable to MRI and Ultrasound. Axial, coronal, and sagittal T2-weighted MRI images are useful for identifying diaphragm defects. Images obtained after gadolinium intravenous injection can characterize contents of hernial sac and evaluate complications of herniated organs. Dynamic imaging during inhalation, exhalation, and Valsalva maneuvers can be helpful in showing hernia changes with different abdominal or intrathoracic pressures. In our case some of these signs (collar sign, hump sign, fascia sign and segmental diaphragmatic defect) were highlighted on CT examination, but only with MRI it was possible to better identify rupture point of diaphragm and hepatic parenchyma involvement thanks to the greater sensitivity of MRI for soft tissues, while Doppler Ultrasound allowed us to highlight continuity between hepatic vascularization and overdiaphragmatic nodule. Positron Emission (PET) / Computed Tomography (CT) and Scintigraphy could potentially be very sensitive for recognition of overdiaphragmatic liver parenchyma, but due to higher risks they should only be used in our judgment when Ultrasonography and MRIs present interpretative doubts.
Conclusion
To avoid unnecessary examinations or surgical procedures, liver tissue herniation should be included in differential diagnosis of intrathoracic nodular opacities in contact with right diaphragm. This pathology is very rare and although similar cases have been reported in literature, there is still a lot of controversy about traumatic or idiopathic origin. Clinical history of our patient does not allow us to associate pathology with traumatic causes or comorbidities, therefore congenital nature cannot be excluded, and if this were true we could be faced with a hernia of an unknown type; obviously this must be supported by larger case histories.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its additional files.
Author contribution
Study design/planning collected data, preparation of manuscript, data analysis/statistics, data interpretation and involved in project development, literature analysis/search AD and GF; collected data, wrote the manuscript, literature analysis/search AC, PVF, IP, ET, CI, GT, TV: wrote the manuscript: AB.
Patient consent
"Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal."
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Funding: There are no sources of funding for the research.
References
- 1.Pataka A, Paspala A, Sourla E. Non traumatic liver herniation due to persistent cough mimicking a pulmonary mass. Hippokratia. 2013;17(4):376–377. [PMC free article] [PubMed] [Google Scholar]
- 2.Harne PS, Mukherjee S, Shepherd Z. Atraumatic Intercostal and Intrathoracic Liver Herniation Related to Influenza A. ACG case reports journal. 2020;7(7):e00427. doi: 10.14309/crj.0000000000000427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iochum S, Ludig T, Walter F. Inc, 22 Spec No; 2002. Imaging of diaphragmatic injury: a diagnostic challenge?. Radiographics: a review publication of the Radiological Society of North America; pp. S103–S118. [DOI] [PubMed] [Google Scholar]
- 4.Luo HF, Lei T, Wang HJ. Non-traumatic diaphragmatic hernia of the liver in an adult: a case report. Hepatobiliary & pancreatic diseases international HBPD INT. 2007;6(2):219–221. [PubMed] [Google Scholar]
- 5.Gupta S, Bali RK, Das K. Rare presentation of spontaneous acquired diaphragmatic hernia. The Indian journal of chest diseases & allied sciences. 2011;53(2):117–119. [PubMed] [Google Scholar]
- 6.Davies SF, Northrup WF, Sarosi GA. Right-sided posttraumatic diaphragmatic hernia presenting as a coin lesion. Southern medical journal. 1979;72(9):1211–1212. doi: 10.1097/00007611-197909000-00039. [DOI] [PubMed] [Google Scholar]
- 7.Schumacher L, Gilbert S. Congenital diaphragmatic hernia in the adult. Thoracic surgery clinics. 2009;19(4):469–472. doi: 10.1016/j.thorsurg.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 8.Kurt A, Yazıcıoğlu KR, İpek A. Right sided diaphragmatic hernia in an adult with no history of trauma: unusual ct findings. European Journal of General Medicine. 2004;1(3):55–57. [Google Scholar]
- 9.Yang GP, Tang CN, Siu WT. Diaphragmatic hernia: an uncommon cause of dyspepsia. JSLS. 2005;9(3):352–355. [PMC free article] [PubMed] [Google Scholar]
- 10.Sanna S, Taurchini M, Monteverde M. Catamenially recurring pneumothorax with partial liver herniation: a particular view. Respiration; international review of thoracic diseases. 2015;82(5):476–477. doi: 10.1159/000328724. [DOI] [PubMed] [Google Scholar]
- 11.Rees O, Mirvis SE. Shanmuganathan K Multidetector-row CT of right hemidiaphragmatic rupture caused by blunt trauma: a review of 12 cases. Clinical radiology. 2005;60(12):1280–1289. doi: 10.1016/j.crad.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 12.Shanmuganathan K, Mirvis SE, White CS. MR imaging evaluation of hemidiaphragms in acute blunt trauma: experience with 16 patients. AJR Am J Roentgenol. 1996;167(2):397–402. doi: 10.2214/ajr.167.2.8686615. Aug. [DOI] [PubMed] [Google Scholar]
- 13.Desir A, Ghaye B. Vol. 32. 2012. pp. 477–498. (CT of blunt diaphragmatic rupture. Radiographics: a review publication of the Radiological Society of North America, Inc). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its additional files.