Abstract
Background
It remains unclear how transition readiness is associated with various domains of health in children and young adults. Our objective was to describe the transition readiness of children and young adults with inflammatory bowel disease (IBD) and examine its associations with demographic factors, IBD activity, and measures of physical, psychological, and social health.
Methods
We recruited children ages 12 to 17 and young adults ages 18 to 20 from 2 internet-based cohorts sponsored by the Crohn’s & Colitis Foundation. Participants self-reported demographics, IBD activity, transition readiness, health-related quality of life, and Patient-Reported Outcomes Information Systems domains of physical, psychological, and social health.
Results
Among 361 pediatric and 119 adult participants, age and female sex were associated with transition readiness. The association was greater in the pediatric cohort. Having IBD in remission was associated with worse transition readiness in the pediatric cohort only (beta = 0.3; P = 0.003). Health-related quality of life and Patient-Reported Outcomes Information Systems measures of fatigue, pain interference, and sleep disturbance were not associated with transition readiness in either children or adults. We observed few small associations between psychological or social health and transition readiness. Better transition readiness was associated with greater anxiety in adults (beta = –0.02; P = 0.02) and greater peer relationships among children (beta = 0.01; P = 0.009).
Conclusions
In children and young adults with IBD, transition readiness was associated with older age and female sex. Associations between transition readiness and physical, psychological, and social health were either small, inconsistent across age groups, or nonexistent.
Keywords: transition readiness, depression, anxiety, social health, quality of life, inflammatory bowel disease
This study found the direction and strength of associations between transition readiness and physical, psychological, and social health to be less significant and more complex than previously appreciated. This has implications for future research and transition readiness interventions.
BACKGROUND
For the more than 9 million children with chronic health conditions in the United States, the process of transitioning from child- to adult-centered health care is ideally a “purposeful, planned movement.” 1 However, this transition is commonly associated with poor patient and family satisfaction2 and variable access to and quality of posttransfer health care.3–5 The transition process is also associated with poor health outcomes,6–8 including deterioration of baseline health status and the development of new, chronic health conditions or complications of past treatments.9, 10 One-quarter of patients with inflammatory bowel disease (IBD) are diagnosed as children, and the incidence among children is increasing.11, 12 As such, health care transition (the movement from child- to adult-centered health care), transfer to adult care (the handoff from pediatric to adult providers), and transition readiness (the skills and knowledge necessary for a successful transition) are active areas of IBD research, practice innovation, and quality improvement.12 Despite this, only patient age and sex have been consistently associated with transition readiness, and there is still little evidence regarding how to foster transition readiness in children, adolescents, and young adults.
Current expert recommendations and conceptual models hypothesize that patients’ physical, psychological, and social health directly affect transition readiness and therefore transition.13–15 However, the direction and strength of the associations between measures of these domains of health and transition readiness are not well established.16–18 To date, studies of the associations between physical, psychological, or social health have largely focused on how activity-limiting chronic conditions (such a IBD) affect the receipt of transition services in health care settings.19 While prior work has evaluated the relationship of transition readiness with psychological conditions that significantly affect human development or cognition (eg, learning disabilities, behavioral disorders),20 studies of the association between transition readiness and common mental health conditions such as depression, anxiety, or impaired quality of life are lacking. As anxiety and depression are both highly prevalent and treatable in young adults with chronic conditions such as IBD,21 it is important to understand their relationship with transition readiness. Understanding these associations would provide evidence-based targets for interventions aimed at improving transition readiness and support current recommendations to screen patients with chronic conditions for psychological disorders, social dysfunction, and transition readiness.
Expert recommendations include regular assessments of transition readiness, beginning at age 14.22 There are several assessments for use in clinical settings, including the Transition Readiness Assessment Questionnaire, or TRAQ-20.20, 23 This assessment was developed using items gleaned from 9 previously developed expert-recommendation checklists of transition readiness and covers a range of knowledge and skills likely related to a patient’s ability to transition from pediatric- to adult-centered health care.20 To date, transition readiness as measured by the TRAQ-20 has been positively associated with older age and female sex.
Our study objective was to describe the transition readiness of children and young adults with IBD using the TRAQ-20 and examine associations of transition readiness with demographic factors, IBD activity, and measures of physical, psychological, and social health.
MATERIALS AND METHODS
Data for this study were collected from 2 parallel, Web-based cohorts developed and maintained by the Crohn’s & Colitis Foundation. The foundation is a nonprofit volunteer organization that funds, publishes, and advocates for IBD research and provides support for IBD patients. Patients with self-identified IBD are invited to join the foundation’s Web-based cohorts, which serve as a means to access foundation educational resources, receive research updates, and participate in research surveys every 6 months that are focused on the relationships between patient-reported exposures, health behaviors, and outcomes. In 2011, the foundation sponsored the development and maintenance of IBD Partners, a Web-based cohort of more than 15,000 adult patients with self-identified IBD (ie, Crohn disease [CD] and ulcerative or indeterminate colitis [UC/IC]).24, 25 In 2013, the foundation launched a parallel cohort of children with IBD and their parents called IBD Partners Kids & Teens.
Recruitment and Eligibility
Children with IBD and their parents and young adults with IBD were recruited by the foundation through their Website, e-mail rosters, social media outlets, word-of-mouth at foundation educational and fundraising events, and other promotional efforts. Enrollment for both cohorts remains ongoing. To date, the Kids & Teens cohort includes participants from 49 states. The adult cohort includes participants from all 50 states. For the present analyses, we analyzed data collected through March 2017.
IBD Partners Kids & Teens (pediatric) cohort
Children ages 12 to 17 completed transition readiness and disease-related survey questions themselves, including the TRAQ-20 and Patient-Reported Outcomes Measurement Information Systems (PROMIS) instruments specifically designed for child respondents. Parents completed survey questions regarding their participating child’s diagnosis of IBD, demographic information, and family history.
IBD Partners (young adult) cohort
Young adults ages 18 to 20 completed all survey questions themselves, including the TRAQ-20 and adult PROMIS instruments to assess the same or similar health domains as those assessed in the pediatric cohort.
Analyses
We performed cross-sectional analyses of baseline data reported by both cohorts. We chose to maintain separate analyses for the pediatric and adult cohorts because of differences in outcome measures available and possible differences in the relationships of the measures in the different cohorts. Our analysis aimed to assess the association between health care transition readiness, as measured by the TRAQ-20, and (1) age, sex, IBD activity, and health-related quality of life (HRQoL); and (2) measures of physical (fatigue, pain interference, and sleep disturbance), psychological (anxiety, depression), and social health (peer relationships or social satisfaction).
MEASURES
Patient Demographics, IBD Characteristics, and IBD Activity
In both cohorts, we collected information regarding patient demographics, age at IBD diagnosis, years since diagnosis, and past and current IBD medication use—oral 5-aminosalicylates, oral corticosteroids, immunomodulators (methotrexate, azathioprine, and 6-mercaptopurine), and biologic therapies (infliximab, adalimumab, certolizumab pegol, and natalizumab). In an effort to minimize survey length and respondent burden, we did not survey patients about site of IBD care or details of past mental health diagnoses, conditions, or treatments other than IBD.
Pediatric cohort
We measured patient-reported disease activity using the Short Crohn’s Disease Activity Index (SCDAI) and the Pediatric Ulcerative Colitis Activity Index (PUCAI).26, 27 Remission of IBD was defined as an SCDAI score of less than 150 or a PUCAI score of less than 10. These indices have all been validated and are in routine use in IBD research and clinical care. We did not utilize the Pediatric Crohn’s Disease Activity Index because this index requires physical examination and laboratory assessments and is therefore not feasible for survey research.27 To assess HRQoL, we administered the IMPACT-35, a valid measure for use in children and adolescents with IBD in which higher scores indicate greater HRQoL.28
Young adult cohort
As in the pediatric cohort, we administered the SCDAI to assess CD activity. To assess UC activity, we administered the Simple Clinical Colitis Activity Index (SCCAI).27, 29, 30 Remission of IBD was defined as an SCDAI score of less than 150 or an SCCAI score of less than 4.
To assess HRQoL, we administered the Short Inflammatory Bowel Disease Questionnaire (SIBDQ), with higher scores indicating greater HRQoL.31 All of these scales are validated for use in adults with IBD and are in wide use in clinical practice and/or research.24
Patient-Reported Physical, Psychological, and Social Health
Participating children and young adults completed 4-item short forms of PROMIS instruments to assess physical, psychological, and social health. We selected these PROMIS instruments in collaboration with IBD clinical specialists and experts in PROMIS methodology because they measure domains of health affected by IBD in children and young adults.25, 30 We chose 4-item short forms to minimize respondent burden and enhance long-term cohort retention.30 The PROMIS instruments are calibrated using a T-score metric with the mean of the original calibration population equal to 50 and the SD in the calibration population equal to 10. Higher scores in any PROMIS domain indicate more of the domain being measured—therefore, higher scores for anxiety, depression, fatigue, and pain interference indicated poorer well-being whereas higher scores for peer relationships indicated better relationships with peers and thus better well-being.
Pediatric cohort
Participating children completed the following PROMIS pediatric instruments for child respondents: (1) fatigue, (2) pain interference (a measure of the consequences of pain on various aspects of life, including social, cognitive, emotional, physical, recreational activities, sleep, and enjoyment of life), (3) anxiety, (4) depression, and (5) peer relationships (a measure of the quality of relationships with friends and other acquaintances).
Young adult cohort
Participating young adults completed the following PROMIS instruments for adult respondents: (1) fatigue, (2) pain interference, (3) sleep disturbance, (4) anxiety, (5) depression, and (6) social satisfaction (a measure of satisfaction with social roles and activities).
Health Care Transition Readiness
All participating patients in both cohorts completed the TRAQ-20, a patient-reported, validated scale of 5 knowledge and skills domains related to a patient’s ability to transition from pediatric- to adult-centered health care: managing medications, appointment-keeping, tracking health issues, talking with providers, and managing daily activities.20 The TRAQ-20 uses a 5-point ordinal response scale with options based on the transtheoretical-model stages of change. Scores are calculated for each domain and overall as means ranging from 1 to 5, with higher scores indicating a higher level of transition readiness. In previous validation work, participants younger than 18 had an overall TRAQ-20 mean score of 3.23, while those older than 18 had an overall TRAQ-20 mean score of 3.99.23 Factor scores for those younger than 18 ranged from 2.70 for appointment-keeping up to 4.43 for talking with providers. Factor scores for those older than 18 ranged from 3.77 for appointment-keeping to 4.57 for talking with providers.
Statistical Analysis
We performed cross-sectional analyses of baseline data from both cohorts. We used bivariate comparisons to assess the relationships between TRAQ-20 scores and patient age, years since diagnosis, sex, IBD activity and remission status (measured by SCDAI for those with CD and measured by PUCAI or SCCAI for those with UC/IC), HRQoL, and PROMIS measures of physical, psychological, and social health. We also assessed the associations between TRAQ-20 scores and disease activity as categorical (remission, mild, moderate, and severe) and continuous SCDAI, PUCAI, or SCCAI scores.
Bivariate analyses identified several factors that could confound the relationship between TRAQ-20 scores and measures of psychological and social health (age, sex, and remission status). We used multiple linear regression to assess the magnitude and direction of the associations between potential confounders and TRAQ-20 scores. We then used multivariate linear regression to evaluate associations between TRAQ-20 scores and PROMIS measures of psychological and social health. Using a likelihood-ratio method, we investigated possible interactions between potential confounders. After fitting models that included all potential confounders, we used a change-in-effect method to remove any variable that did not confound the relationship between the TRAQ-20 scores and psychological or social health (see footnotes for Tables 2-4).
TABLE 2.
Associations Between Transition Readiness, Patient Characteristics, and Disease Activity
| Pediatric Cohort | Young Adult Cohort | |||
|---|---|---|---|---|
| n = 348 | n = 102 | |||
| Patient characteristics | Beta (95% CI) | P | Beta (95% CI) | P |
| Age* | 0.1 (0.08 to 0.2) | <0.001 | 0.3 (0.1 to 0.5) | 0.001 |
| Sex† | 0.2 (0.7 to 0.4) | 0.006 | 0.5 (0.2 to 0.8) | 0.002 |
| Remission status‡ | –0.3 (–0.5 to –0.1) | 0.003 | 0.3 (–0.03 to 0.6) | 0.08 |
| HRQoL‡, § | –0.001 (–0.005 to 0.003) | 0.6 | 0.1 (–0.03 to 0.2) | 0.1 |
*Adjusted for sex, remission status, and years since diagnosis.
†adjusted for age, remission status, and years since diagnosis.
‡adjusted for age, sex, and years since diagnosis.
§HRQoL measured by IMPACT-35 in pediatric cohort, SIBDQ in young adult cohort.
TABLE 4.
Associations Between Transition Readiness and Psychological and Social Health
| Pediatric Cohort | Young Adult Cohort | |||
|---|---|---|---|---|
| n = 348 | n = 102 | |||
| PROMIS measure* | Beta (95% CI) | P | Beta (95% CI) | P |
| Anxiety | –0.005 (–0.01 to 0.004) | 0.3 | –0.02 (–0.04 to –0.003) | 0.02 |
| Depression | –0.009 (–0.02 to 0.002) | 0.1 | –0.02 (–0.03 to 0.001) | 0.07 |
| Peer relationships | 0.01 (0.003 to 0.02) | 0.009 | - | - |
| Social satisfaction | - | - | 0.02 (–0.0004 to 0.03) | 0.06 |
*Adjusted for age, sex, remission status, and years since diagnosis.
Ethical Considerations
All data were prepared using SAS version 9.3 and analyzed using Stata version 13.1. The study protocol was approved by the University of North Carolina at Chapel Hill institutional review board.
RESULTS
Baseline Characteristics
Age
Three hundred-sixty one children ages 12 to 17 with parent-reported IBD enrolled in the pediatric cohort during the study period (Table 1). The mean age of this cohort was 14.5 (range 12-17 years), and the mean of the years since IBD diagnosis was 4.6 (range 0-16 years).
TABLE 1.
Characteristics of the Study Population
| Pediatric Cohort | Young Adult Cohort | ||
|---|---|---|---|
| n = 361 | n = 119 | ||
| Demographics | Age, y, mean (range) | 14.5 (12-17) | 18.8 (18-20) |
| Female, % | 47.4 | 63.9 | |
| Race, % | |||
| White | 89.4 | 90.7 | |
| African American | 3.6 | 1.7 | |
| Hispanic | 5.9 | 3.3 | |
| Asian | 4.5 | 0.8 | |
| Multiracial | 0.6 | 5.9 | |
| IBD characteristics and activity | IBD type, % | ||
| CD | 79.8 | 73.1 | |
| UC/IC | 20.2 | 26.9 | |
| Age at diagnosis, y, mean (range) | 10.3 (1-17) | 12.8 (2-17) | |
| Y since diagnosis, mean (range) | 4.6 (0-16) | 6.1 (1-16) | |
| Current therapy, % | |||
| 5-aminosalicylates* | 24.1 | 19.5 | |
| Immunomodulators† | 35.7 | 36.8 | |
| Biologics‡ | 59.0 | 58.1 | |
| Corticosteroids§ | 10.8 | 15.3 | |
| Disease-specific activity scores, mean (SD) | |||
| CD¶ | 97.0 (71.8) | 118.8 (86.3) | |
| UC/IC‖ | 13.2 (15.7) | -- | |
| UC/IC** | -- | 3.25 (1.6) | |
| CD activity categories, n (%)¶ | |||
| Remission | 228 (82.6) | 55 (70.5) | |
| Mild | 29 (10.5) | 14 (18.0) | |
| Moderate to severe | 19 (6.9) | 9 (11.5) | |
| UC/IC activity categories, n (%)‖ , ** | |||
| Remission | 31 (52.5) | 8 (33.3) | |
| Mild | 18 (30.5) | 14 (58.3) | |
| Moderate to severe | 10 (17.0) | 2 (8.3) | |
| In remission, % | |||
| CD | 82.6† | 70.5† | |
| UC/IC | 52.5‡ | 33.3§ | |
| HRQoL scores, mean (SD) | |||
| IMPACT-35†† | 135.9 (22.8) | -- | |
| SIBDQ‡‡ | -- | 4.9 (1.2) | |
| Patient-reported measures of physical, psychological, and social health | PROMIS T-scores, mean (SD)§§ | ||
| Fatigue | 47.7 (12.2) | 54.1 (11.6) | |
| Pain interference | 45.2 (10.7) | 50.4 (9.9) | |
| Sleep disturbance | -- | 52.3 (3.6) | |
| Anxiety | 46.6 (10.3) | 54.0 (10.5) | |
| Depression | 43.3 (8.3) | 51.0 (10.2) | |
| Peer relationships | 49.2 (9.3) | -- | |
| Social satisfaction | -- | 51.9 (10.1) | |
| Transition readiness | TRAQ-20 scores, mean (SD)¶¶ | 2.6 (0.8) | 3.9 (0.8) |
| Subscale scores, mean (SD) | |||
| Managing medications | 2.8 (1.1) | 4.0 (0.9) | |
| Appointment-keeping | 1.8 (1.1) | 3.4 (1.1) | |
| Tracking health issues | 2.1 (1.1) | 3.9 (1.0) | |
| Talking with providers | 4.6 (0.8) | 4.8 (0.6) | |
| Managing daily activities | 3.6 (1.1) | 4.3 (0.8) |
*5-aminosalicylates: azulfidine, mesalamine, balsalazide, and olsalazine sodium.
†Immunomodulators: methotrexate, azathioprine, and 6-mercaptopurine.
‡Biologics: infliximab, adalimumab, certolizumab pegol, natalizumab, andvedolizumab.
§Systemic steroids: budesonide, dexamethasone, methylprednisolone, prednisone, and prednisolone.
¶SCDAI: 3-item questionnaire of CD activity. Score <150 indicates remission, 150-220 mild, 221-450 moderate, and >450 severe CD.
‖PUCAI: 6-item questionnaire of UC/IC activity in childrenS score <10 indicates remission, 10-29 mild, and ≥30 moderate to severe UC/IC.
**SCCAI: 12-item questionnaire of UC/IC activity in adults. Score ≤2 indicates remission, 3-5 mild, 6-11 moderate, and ≥12 severe UC/IC.
††IMPACT-35: 35-item questionnaire of HRQoL in pediatric IBD patients. Scores range from 35 (worst) to 175 (best).
‡‡SIBDQ: 10-item questionnaire of HRQoL in adult IBD patients. Scores range from 1 (worst) to 7 (best).
§§PROMIS: 4-item short forms. Standard population T-score mean = 50 and SD = 10.
¶¶TRAQ-20: 20-item questionnaire assessing 5 domains of transition readiness. Total and subscores range from 0 (worst) to 5 (best).
One-hundred-nineteen young adults ages 18 to 20 with self-reported IBD enrolled in the young adult cohort during the study period (Table 1). The mean age of this cohort was 18.8 (range 18-20 years), and the mean age since diagnosis was 6.1 years (range 2-17 years).
Sex
Approximately half (47%) of the pediatric cohort and more than half (64%) of the young adult cohort were female (Table 1).
IBD characteristics and activity
The majority (80% of children and 73% young adults) reported a diagnosis of CD and the remainder reported a diagnosis of UC/IC. More than half (59% of children and 58% of young adults) were treated with biologics. Per patient-reported IBD activity scores, the majority of those with CD (83% of children and 71% of young adults) were in remission, and 53% of children and 33% of young adults with UC/IC were in remission (Table 1).
HRQoL
In both cohorts, the mean HRQoL scores—IMPACT-35 for the pediatric cohort and SIBDQ for the young adult cohort—were consistent with scores reported by patients with active CD or UC/IC (Table 1).28, 31
Patient-reported physical, psychological, and social health
Mean T-scores of PROMIS physical (fatigue, pain interference, sleep disturbance), psychological (anxiety, depression), and social (peer relationships or social satisfaction) health in the pediatric cohort were similar to or slightly better than for the pediatric reference population (Table 1). Mean T-scores for similar measures in the young adult cohort were generally similar to those for the adult reference population though slightly worse for the domains of fatigue and anxiety (Table 1).
Transition readiness
The mean TRAQ-20 score in the pediatric cohort was 2.6, and in the young adult cohort it was 3.9. In both cohorts, the highest subscore was for talking with providers, and the lowest was for appointment-keeping (Table 1).
Associations Between Demographic Factors and IBD Activity, HRQoL, and Transition Readiness
Age
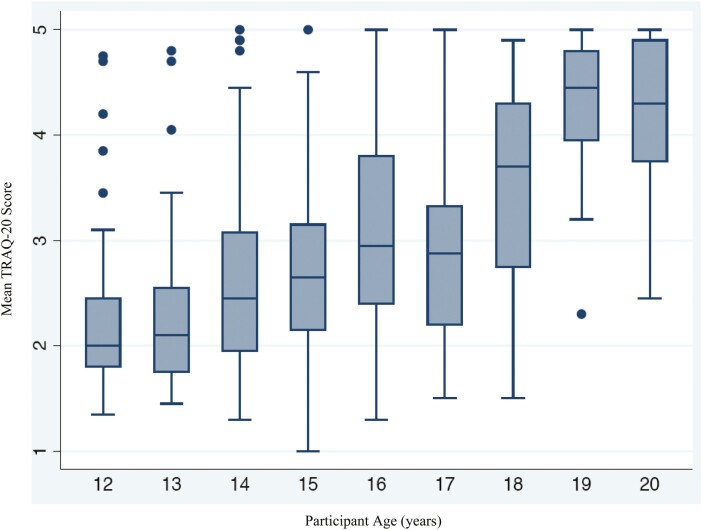
In both bivariate and linear regression analyses, age was significantly associated with transition readiness (Fig. 1). Within the pediatric cohort, a 1-year increment in age was associated with a 0.1-point-higher TRAQ-20 total score, indicating greater transition readiness (P < 0.001; Table 2). This association was greater in the young adult cohort, in which each 1-year increment in age was associated with a 0.3-point-higher TRAQ-20 score (P = 0.001; Table 2).
FIGURE 1.
Associations between transition readiness and age.
Sex
Compared to males, females had a 0.2-point-higher TRAQ-20 score within the pediatric cohort (P = 0.006) and a 0.5-point-higher TRAQ-20 score in the young adult cohort (P = 0.002).
IBD activity
IBD remission status as measured by patient-reported activity scores (SCDAI, PUCAI, or SCCAI) was not consistently associated with transition readiness among all participants, even when controlling for age and time since diagnosis. In the pediatric cohort, remission status was associated with a 0.3-point-lower TRAQ-20 score, indicating that those in remission had less transition readiness (P = 0.003; Table 2). Among the young adult cohort, the relationship between remission status and IBD activity was not significant (Table 2). When we assessed the associations between TRAQ-20 scores and disease activity as categorical (remission, mild, moderate, or severe, rather than remission vs active) and continuous scores, we found the same pattern and lack of consistent associations (data not shown). Years since diagnosis were not associated with disease activity or transition readiness in either cohort and did not confound the relationship between disease activity and transition readiness (data not shown). However, we chose to control for years since diagnosis in our regression analyses because there is concern among clinicians and researchers that patients’ familiarity with their diagnosis strongly affects their disease control and could potentially affect transition readiness (Tables 2-4).
HRQoL
In both cohorts, HRQoL scores as measured by IMPACT-35 in the pediatric cohort and SIBDQ in the young adult cohort were not associated with transition readiness (Table 2).
Associations Between Physical, Psychological, and Social Health and Transition Readiness
After controlling for potential confounders, patient-reported measures of fatigue, pain interference, and sleep disturbance were not associated with transition readiness (Table 3).
TABLE 3.
Associations Between Transition Readiness and Physical Health
| Pediatric Cohort | Young Adult Cohort | |||
|---|---|---|---|---|
| n = 348 | n = 102 | |||
| Patient characteristics | Beta (95% CI) | P | Beta (95% CI) | P |
| Fatigue* | –0.0007 (–0.009 to 0.008) | 0.9 | –0.008 (–0.02 to 0.007) | 0.3 |
| Pain interference* | –0.0012 (–0.01 to 0.008) | 0.8 | –0.001 (–0.02 to 0.02) | 0.9 |
| Sleep disturbance* | –0.0094 (–0.02 to 0.0018) | 0.1 | –0.015 (–0.03 to 0.001) | 0.1 |
*Adjusted for age, sex, and years since diagnosis.
There was no association between transition readiness and anxiety among the pediatric cohort, but there was a small but statistically significant association in the young adult cohort (Table 4). Among the young adult cohort, each 1 point in PROMIS anxiety score, indicating worse anxiety, was associated with a 0.02-point-lower TRAQ-20 score. Depression was not associated with transition readiness in either cohort.
Patient-reported social health (peer relationships or social satisfaction) was statistically significantly associated with transition readiness in the pediatric cohort (beta = 0.01; P = 0.009) but not in the young adult cohort (Table 4).
DISCUSSION
In these analyses, we found that TRAQ-20 transition readiness scores were consistently associated with age and sex, reinforcing prior literature in IBD and other chronic conditions.16, 20, 23, 32–34 However, associations between transition readiness and other measures of physical, psychological, and social health were either small, inconsistent, or nonexistent. Although age was associated with better transition readiness in both study cohorts, the effect was 3 times greater in the young adult cohort than in the pediatric cohort. This raises the possibilities that the relationship between age and transition readiness is not linear and that transition readiness increases faster in young adulthood than in childhood (although this study was not designed to assess this possibility) or that differences in age are actually attributable to other factors we did not assess, such as self-efficacy or resilience, which has been shown in a recent study among adolescents with IBD.35 Similarly, female sex was associated with better transition readiness in both cohorts, but the effect in the young adult cohort was twice that of the pediatric cohort, also suggesting a more complex, cohort-dependent association that could also result from other unmeasured factors.
The direction and significance of the association between IBD activity/remission status and transition readiness varied by cohort and disease activity index, consistent with other literature, which has not found clear associations with transition readiness and disease severity.16, 34, 36 In our primary analyses, remission status was associated with lower transition readiness scores in the pediatric cohort and higher scores in the young adult cohort (Table 2). One possible cause could be the differences in how children and young adults are expected to take responsibility for their own health and health care. For a child’s IBD to be in remission, an adult parent must typically be managing the child’s health and health care, which carries the potential of sheltering the child from developing transition readiness skills. However, young adults may be more likely to be in remission if they are themselves capable of managing their own health and health care because they are living independently from parents. Interestingly, the rates of remission were higher for the pediatric cohort than for the young adult cohort, a finding that will require further study because it suggests that young adults lack important knowledge and skills for managing their illness even as they report higher levels of transition readiness. Given the many developmental tasks of adolescence and young adulthood, it is not surprising that there would be variability in transition readiness by age. However, it is not possible to understand the direction of the associations between age, disease management, and IBD activity without further, longitudinal studies. The findings of such studies will be critical for refining transition readiness models and designing interventions and recommendations.
Overall, we found few associations between patient-reported measures of physical, psychological, and social health and transition readiness. We did find 2 small but statistically significant associations between transition readiness and peer relationships in the pediatric cohort alone and between transition readiness and anxiety in the young adult cohort alone, but these are unlikely to be clinically meaningful. Based on our analyses, a young adult’s PROMIS anxiety score would have to differ by 10 points (SD is equal to 10 points, and minimally important difference is 2.3–4.5 points) to be associated with a 0.2-point difference in the TRAQ-20 score. Therefore, a full SD difference in a young adult’s PROMIS anxiety score would result in a smaller change in the TRAQ-20 score than a 1-year change in age and would have about half the impact of the young adult’s sex. Therefore, our results do not support the current conceptual models that propose a causal relationship between psychological and social factors and transition readiness.13, 14 Our results instead suggest that although impairments in psychological and social health are common for children and young adults with chronic disease, they do not adversely affect transition readiness. Therefore, efforts to improve the psychological or social health of children and young adults, while important, may not affect transition readiness. Rather, interventions aimed at improving transition readiness could focus on promoting specific health literacy and disease self-management skills.
This study in the IBD Partners cohorts—2 national, geographically diverse study populations—is one of the first large-scale assessments of the TRAQ-20’s performance that was not completed in one of a few select tertiary care centers, among patients who were receiving health care transition support. Yet our study reinforces many of the associations between age, sex, and transition readiness that were observed in specialized care settings, supporting its use more broadly to assess transition readiness.
Our study has several limitations affecting the generalizability of our results. First, because our study population was predominantly white and consisted of volunteers, our results may not be generalizable to the overall IBD population in the United States. Second, to minimize respondent burden and improve retention, we did not query patients regarding whether (1) they had received any transition readiness preparation as part of their care, (2) they had transitioned to adult providers at the time they completed the baseline or follow-up assessments, or (3) they had been diagnosed with other behavioral or physical health diagnoses or comorbidities that could also affect their transition readiness. Therefore, we cannot assess associations between these factors and patient-reported transition readiness. Another potential limitation is the relatively small proportion of patients with moderate to severe disease activity and with poor scores on the PROMIS measures, which introduces the possibility of a type II error. However, the proportion of patients in remission was consistent with national data, so this cohort is fairly representative of children with IBD.37
In addition, because of the Web-based nature of the study, we relied on self-report of IBD diagnosis and assessments of disease activity, without input from physicians or the medical record. However, in our validation study of the larger Partners cohort, self-reported IBD status was confirmed by medical records in 96% of participants, suggesting that patients who are involved with the Crohn’s & Colitis Foundation are reliable reporters of their diagnoses.24 Finally, our analysis utilized symptom-based indices to assess disease activity rather than endoscopic assessment. Although endoscopic healing is increasingly recognized as an important clinical target, contemporaneous assessment of transition readiness and mucosal healing would not be practical in a large, multistate internet cohort.
CONCLUSIONS
In our cohort of children and young adults with IBD, patient-reported transition readiness as measured by the TRAQ-20 was associated with older age and female sex, which was consistent with prior studies of this instrument. Interestingly, transition readiness was inversely related to IBD remission in children, suggesting that transition skills do not immediately translate to better health. And finally, transition readiness was not consistently or meaningfully associated with patient-reported HRQoL or psychological and social health, suggesting that transition skills can be acquired or fostered in all patients, regardless of these factors.
Glossary
Abbreviations
- CD
Crohn disease
- HRQoL
health-related quality of life
- IC
indeterminate colitis
- PROs
patient-reported outcomes
- PROMIS
Patient-Reported Outcomes Measurement Information System
- PUCAI
Pediatric Ulcerative Colitis Activity Index
- SCCAI
Simple Clinical Colitis Activity Index
- SCDAI
Short Crohn’s Disease Activity Index
- SIBDQ
Short Inflammatory Bowel Disease Questionnaire
- TRAQ-20
Transition Readiness Assessment Questionnaire
- UC
ulcerative colitis.
Supported by: This research was supported by a grant from the Crohn’s & Colitis Foundation (Kappelman) and the Health Resources and Service Administration National Research Service Award Grant T32 HP14001 (Arvanitis and Hart).
REFERENCES
- 1.Kaufman M, Pinzon J; Canadian Paediatric Society, Adolescent Health Committee. Transition to adult care for youth with special health care needs. Paediatr. Child Health. 2007;12:785–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cheak-Zamora NC, Teti M. “You think it’s hard now … It gets much harder for our children”: youth with autism and their caregiver’s perspectives of health care transition services. Autism. 2015;19:992–1001. [DOI] [PubMed] [Google Scholar]
- 3.Sebastian S, Jenkins H, McCartney S, et al. The requirements and barriers to successful transition of adolescents with inflammatory bowel disease: differing perceptions from a survey of adult and paediatric gastroenterologists. J Crohns Colitis. 2012;6:830–844. [DOI] [PubMed] [Google Scholar]
- 4.Gray WN, Resmini AR, Baker KD, et al. Concerns, barriers, and recommendations to improve transition from pediatric to adult IBD care: perspectives of patients, parents, and health professionals. Inflamm Bowel Dis. 2015;21:1641–1651. [DOI] [PubMed] [Google Scholar]
- 5.Okumura MJ, Kerr EA, Cabana MD, et al. Physician views on barriers to primary care for young adults with childhood-onset chronic disease. Pediatrics. 2010;125:e748–e754. [DOI] [PubMed] [Google Scholar]
- 6.Watson AR. Non-compliance and transfer from paediatric to adult transplant unit. Pediatr Nephrol. 2000;14:469–472. [DOI] [PubMed] [Google Scholar]
- 7.Cole R, Ashok D, Razack A, et al. Evaluation of outcomes in adolescent inflammatory bowel disease patients following transfer from pediatric to adult health care services: case for transition. J Adolesc Health. 2015;57:212–217. [DOI] [PubMed] [Google Scholar]
- 8.Lotstein DS, Seid M, Klingensmith G, et al. ; SEARCH for Diabetes in Youth Study Group . Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics. 2013;131:e1062–e1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wysocki T, Hough BS, Ward KM, et al. Diabetes-mellitus in the transition to adulthood - adjustment, self-care, and health-status. J Dev Behav Pediatr. 1992;13:194–201. [PubMed] [Google Scholar]
- 10.Bell LE, Bartosh SM, Davis CL, et al. Adolescent transition to adult care in solid organ transplantation: a consensus conference report. Am J Transplant. 2008;8:2230–2242. [DOI] [PubMed] [Google Scholar]
- 11.Rocchi A, Benchimol EI, Bernstein CN, et al. Inflammatory bowel disease: a Canadian burden of illness review. Can J Gastroenterol. 2012;26:811–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Philpott JR, Kurowski JA. Challenges in transitional care in inflammatory bowel disease: a review of the current literature in transition readiness and outcomes. Inflamm Bowel Dis. 2019;25:45–55. [DOI] [PubMed] [Google Scholar]
- 13.Betz CL, Ferris ME, Woodward JF, et al. The health care transition research consortium health care transition model: a framework for research and practice. J Pediatr Rehabil Med. 2014;7:3–15. [DOI] [PubMed] [Google Scholar]
- 14.Schwartz LA, Tuchman LK, Hobbie WL, et al. A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child Care Health Dev. 2011;37:883–895. [DOI] [PubMed] [Google Scholar]
- 15.American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians-American Society of Internal Medicine. A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110:1304–1306. [PubMed] [Google Scholar]
- 16.Gray WN, Holbrook E, Morgan PJ, et al. Transition readiness skills acquisition in adolescents and young adults with inflammatory bowel disease: findings from integrating assessment into clinical practice. Inflamm Bowel Dis. 2015;21:1125–1131. [DOI] [PubMed] [Google Scholar]
- 17.Whitfield EP, Fredericks EM, Eder SJ, et al. Transition readiness in pediatric patients with inflammatory bowel disease: patient survey of self-management skills. J Pediatr Gastroenterol Nutr. 2015;60:36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hart LC, Pollock M, Hill S, Maslow G. Association of transition readiness to intentional self-regulation and hopeful future expectations in youth with illness. Acad Pediatr. 2017;17:450–455. [DOI] [PubMed] [Google Scholar]
- 19.McManus MA, Pollack LR, Cooley WC, et al. Current status of transition preparation among youth with special needs in the United States. Pediatrics. 2013;131:1090–1097. [DOI] [PubMed] [Google Scholar]
- 20.Sawicki GS, Lukens-Bull K, Yin X, et al. Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ–Transition Readiness Assessment Questionnaire. J Pediatr Psychol. 2011;36:160–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mackner LM, Greenley RN, Szigethy E, et al. Psychosocial issues in pediatric inflammatory bowel disease: report of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2013;56:449–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White PH, Cooley WC; Transitions Clinical Report Authoring Group, American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians. . Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2018;142:e20183610. [DOI] [PubMed] [Google Scholar]
- 23.Wood DL, Sawicki GS, Miller MD, et al. The Transition Readiness Assessment Questionnaire (TRAQ): its factor structure, reliability, and validity. Acad Pediatr. 2014;14:415–422. [DOI] [PubMed] [Google Scholar]
- 24.Long MD, Kappelman MD, Martin CF, et al. Development of an internet-based cohort of patients with inflammatory bowel diseases (CCFA Partners): methodology and initial results. Inflamm Bowel Dis. 2012;18:2099–2106. [DOI] [PubMed] [Google Scholar]
- 25.Kappelman MD, Long MD, Martin C, et al. Evaluation of the Patient-Reported Outcomes Measurement Information System in a large cohort of patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2014;12:1315–13 23.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dotson JL, Crandall WV, Zhang P, et al. Feasibility and validity of the Pediatric Ulcerative Colitis Activity Index in routine clinical practice. J Pediatr Gastroenterol Nutr. 2015;60:200–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thia K, Faubion WA Jr, Loftus EV Jr, et al. Short CDAI: development and validation of a shortened and simplified Crohn’s disease activity index. Inflamm Bowel Dis. 2011;17:105–111. [DOI] [PubMed] [Google Scholar]
- 28.Otley A, Smith C, Nicholas D, et al. The IMPACT questionnaire: a valid measure of health-related quality of life in pediatric inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2002;35:557–563. [DOI] [PubMed] [Google Scholar]
- 29.Jowett SL, Seal CJ, Phillips E, et al. Defining relapse of ulcerative colitis using a symptom-based activity index. Scand J Gastroenterol. 2003;38:164–171. [DOI] [PubMed] [Google Scholar]
- 30.Arvanitis M, DeWalt DA, Martin CF, et al. Patient-Reported Outcomes Measurement Information System in children with Crohn’s disease. J Pediatr. 2016;174:153–159.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Irvine EJ, Zhou Q, Thompson AK. The Short Inflammatory Bowel Disease Questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT Investigators. Canadian Crohn’s Relapse Prevention Trial. Am J Gastroenterol. 1996;91:1571–1578. [PubMed] [Google Scholar]
- 32.Zhong Y, Gilleskie DB, van Tilburg MAL, et al. Longitudinal self-management and/or transition readiness per the TRxANSITION index among patients with chronic conditions in pediatric or adult care settings. J Pediatr. 2018;203:361–370.e1. [DOI] [PubMed] [Google Scholar]
- 33.Moynihan M, Saewyc E, Whitehouse S, et al. Assessing readiness for transition from paediatric to adult health care: revision and psychometric evaluation of the Am I ON TRAC for Adult Care questionnaire. J Adv Nurs. 2015;71:1324–1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mackie AS, Rempel GR, Islam S, et al. Psychosocial maturity, autonomy, and transition readiness among young adults with congenital heart disease or a heart transplant. Congenit Heart Dis. 2016;11:136–143. [DOI] [PubMed] [Google Scholar]
- 35.Carlsen K, Haddad N, Gordon J, et al. Self-efficacy and resilience are useful predictors of transition readiness scores in adolescents with inflammatory bowel diseases. Inflamm Bowel Dis. 2017;23:341–346. [DOI] [PubMed] [Google Scholar]
- 36.Fenton N, Ferris M, Ko Z, et al. The relationship of health care transition readiness to disease-related characteristics, psychosocial factors, and health care outcomes: preliminary findings in adolescents with chronic kidney disease. J Pediatr Rehabil Med. 2015;8:13–22. [DOI] [PubMed] [Google Scholar]
- 37.Colletti R. Improve Care Now annual update. 2018. https://www.improvecarenow.org/2018_annual_updateImproveCareNow (1 November 2019, date last accessed).