Abstract
Background
Falls in later life that require admission to hospital have well-established consequences for future disability and health. The likelihood and severity of a fall will result from the presence of one or more risk factors. The aim of this study is to examine risk factors identified for their ability to prevent falls and to assess whether they are associated with hospital admission after a fall.
Methods
Analyses of data from the English Longitudinal Study of Aging (ELSA), a prospective cohort study. In a sample of 3783 men and women older than 60 years old, a range of potential risk factors measured at Wave 4 (demographic, social environment, physical, and mental functioning) were examined as predictors of fall-related hospitalizations, identified using International Classification of Diseases, 10th Revision (ICD-10) code from linked hospital records in the United Kingdom. Subdistribution hazard models were used to account for competing risk of death.
Results
Several risk factors identified by previous work were confirmed. Suffering from urinary incontinence (subdistribution hazard ratio = 1.49; 95% CI: 1.14, 1.95) and osteoporosis (subdistribution hazard ratio = 1.48; 95% CI: 1.05, 2.07), which are not commonly considered at an early stage of screening, were found to be associated with hospital admission after a fall. Both low and moderate levels of physical activity were also found to somewhat increase the risk of hospital admission after a fall.
Conclusions
Several predictors of having a fall, severe enough to require hospital admission, have been confirmed. In particular, urinary incontinence should be considered at an earlier point in the assessment of risk.
Keywords: Falls, Hospital admission, Risk factors, Urinary incontinence
Falls among older people are common, with around a third of people over age 65 and around half of people aged 80, experiencing at least one fall a year (1). Falls in later life can have serious consequences, as injuries occur in around 20% of these falls (2) and approximately 5% of older people will require hospitalization as a result (3). Therefore, not all falls among older people will be severe enough to cause injury and not all falls that result in injury or harm will require hospital admission. However, those who are hospitalized after an unintentional fall are often more likely to have experienced a serious injury and will have an increased risk of future disability (4) or admission to a nursing home (5). Although not all injurious falls will require admission to hospital, those that do impose a substantial burden on health and social care services (6).
Current guidelines in the United Kingdom and the United States (the National Institute for Health and Care Excellence [NICE], American Geriatrics Society/British Geriatrics Society) for the prevention of falls in older people recommend a 2-stage assessment (7,8). Research has identified that the strongest predictor of falls in later life are muscle weakness, history of falls, gait abnormality, and balance deficit (9–11). They advise that people older than 65 are first screened for history of falls and difficulties with walking or balance (self-reported or evaluated by a health care professional) to identify those at greatest risk. It is then recommended that those identified high risk be offered a further multifactorial assessment which may include a range of other predictors, such as visual impairment, osteoporosis risk, cognitive impairment, urinary incontinence, assessment of home hazards, cardiovascular examination and medication review, perceived functional ability, and fear relating to falling (8,11,12). It is recommended that these assessments be carried out by professionals or organizations, which have health and social care as part of their remit and to refer older people to appropriate interventions, such as strength and balance exercise programs. However, many of these predictors have been identified from studies that use a definition of fall which encompasses a wide range of severity: from falls that do not lead to injury, to injurious falls where medical treatment is sought, and to falls which result in hospitalization (7). Therefore, the impact of these risk factors on falls of higher severity may not be understood. Participants in the English Longitudinal Study of Aging (ELSA), a large population-based study, have been linked to hospital administrative data that offer a unique opportunity to examine hospital admission following a fall. Therefore, this study aims firstly to examine the association between being admitted to hospital after an unintentional fall, with the risk factors currently prioritized as screening tools (history of falls and difficulties with walking or balance). Secondly, we wish to identify additional risk factors (demographic, health behaviour, chronic illness, health-related) which remain predictive, independent of these screening factors. These additional risk factors were selected based on their availability in ELSA and were chosen to reflect established risk factors, according to current guidelines (7,12) and a recent review of the literature (11). In addition, several risk factors which have been studied less frequently (living arrangements, wealth body mass index (BMI), smoking status, physical activity) were explored.
Method
Study Population
English Longitudinal Study of Aging is an ongoing nationally representative sample of individuals aged 50 and older living in England. The study began in 2002–2003 (Wave 1) with 11 391 individuals. Repeat assessments have been conducted every 2 years. The primary form of data collection in ELSA is a face-to-face computer-assisted personal interview which takes place in the participant’s home. However, in 2004–2005, 2008–2009, and 2012–2013, a nurse visit which included various physical performance assessments was also carried out (13). For the purpose of this analysis, the “baseline” was taken as being 2008–2009 (Wave 4) since it included a refreshment sample, thus providing the greatest power for our analysis. English Longitudinal Study of Aging was conducted in accordance with the Declaration of Helsinki and ethical approval and experimental protocols were granted by National Health Service (NHS) Research Ethics Committees under the National Research and Ethics Service. All participants provided informed consent.
Analytical Sample
At Wave 4 (2008–2009), 8643 members had a nurse visit. Of these, 7654 participants consented to have their Hospital Episode Statistic data linked. Of these, 5409 older than 60 years of age were eligible for a walking speed test and responded to questions about fall status. Exclusions were made for participants who had missing data on key variables (n = 1416) and 144 participants who had experienced a fall before their Wave 4 interview, the average length of time that these falls occurred was 5 years before their interview date. A small number of participants resided in a nursing home (n = 68) and this could alter their chance of being admitted to hospital after a fall; however, our sample did not include anyone who was currently living in a nursing home. These exclusions are depicted in Supplementary Figure S1 (Supplementary Tables S1–S8).
Outcome Measure: Hospital Admission After a Fall
Hospital admission after a fall were ascertained using electronic health records and linked to study members. Administrative data collated on a monthly basis and supplied by all English hospitals in the National Health Service (NHS), data are collected by the care provider while the patient receives treatment. For each participant, a record of every episode of admission to hospital is available, with admission date, primary and secondary diagnoses. However, those who received medical treatment in a different setting such as outpatient care or a GP surgery will not be captured by these data. Diagnoses were coded according to the International Classification of Diseases, 10th version (ICD-10). Falls correspond to the ICD-10 codes W00 to W19. These codes are used as secondary diagnoses to provide additional information about a primary cause of admission, especially when the primary diagnosis is due to external causes. These codes have been previously used to assess fall-related admissions in the United Kingdom (14–16). Participants were followed up for hospital in-patient admissions from the year and month immediately after the interview date at Wave 4 (2008 or 2009) up to January 31, 2018, the last date of record linkage. Mortality up to April 2018 was ascertained from linked mortality register data. By the end of follow-up 658 deaths occurred. The majority of fall-related admissions in this sample were due to a primary diagnosis of injury (78%) and of those, the majority of injuries were fractures (43%). Sensitivity analysis was carried out restricting the outcome to those who were admitted due to a fall-related injury: primary diagnosis of injury (ICD-10-AM codes S00 to T75).
Risk Factors
Self-reported previous falls (12 months)
It is recommended that older people are regularly asked by health and social care professionals about previous falls and that this acts as a screening tool to identify older people who will require a more comprehensive risk assessment (11,12). We wished to capture this self-reported assessment as a predictor of hospital admission after a fall. We used a self-reported assessment of falls drawn from survey data so that we could capture previous falls that needed medical treatment, but might not have been serious to require admission to hospital. We captured this information using a question that asked participants who were aged 60 or older if they had “fallen down in the last year for any reason.” Those who in a follow-up enquiry confirmed they had “injured themselves seriously enough to need medical treatment” were classified as having reported a “severe previous fall.”
Physical performance assessments
Short Physical Performance Battery (balance tests, chair rises, gait speed) The Short Physical Performance Battery (SPPB) is a group of measures that examine lower limb mobility; it is comprised of walking/gait speed, time to complete 5 chair rises, and balance tests. This battery has been extensively validated and has found to be predictive at the preclinical stage of later disability (17). It has also been found to be predictive of falls in older people living in the community (11). The balance tests evaluate the respondent’s ability to hold for 10 seconds 3 separate stands side by side, semi-tandem, and full tandem. All participants for whom it was judged safe to do and who had successfully held the previous position were asked to complete the test and were timed by the nurse. A walking speed test was performed among participants aged 60 and older (18). The test involved measuring the time taken to walk a distance of 8 feet, and the walking speed of respondents (m/s) was computed. Respondents were asked to stand up from a firm chair without using their arms. If they succeeded in doing a single rise, they were asked to stand up and sit down as quickly as they could for 5 rises and the time taken was noted. A total SPPB score was calculated which combines the results of the gait speed, chair stand, and balance tests (0–12). Poor performance was defined as a score of 8 or lower (17). Grip strength: Grip strength is included in cohort studies as a measure of upper body strength and it was tested using a gripometer in all respondents for whom it was safe, for example, those without swelling, pain, or recent injury. Three values were recorded for each hand, using a Smedley dynamometer in a standing position, starting with the nondominant hand and alternating between hands and the maximum value for the dominant hand was used in the analysis (19,20).
Demographics
Age and sex were taken into account throughout the analyses. Household wealth was assessed via the face-to-face interview, which collected information on the financial circumstances of respondents using 45 questions regarding household income and 31 questions regarding household wealth. An aggregate measure of total nonpension household wealth was derived from these components by economists at the Institute for Fiscal Studies (IFS) including financial assets, physical assets, and housing wealth but not pension wealth (21). Living alone is defined as whether the participant lived in a solo household or resided with other people.
Physical health/functioning
Visual impairment Participants were asked to rate their eyesight (with glasses if used) using 5 categories as excellent, very good, fair, poor, or registered or legally blind. We grouped these responses into 2 categories: excellent/very good versus fair/poor or blind. Urinary incontinence: Participants were asked whether in the last 12 months they had lost any amount of urine beyond their control. Activities of daily living and instrumental activities of daily living: Respondents were asked to report whether they had any difficulty with the following activities of daily living (ADLs): dressing, walking across a room, bathing or showering, eating, getting out of bed, using the toilet. Similarly, they reported difficulties with instrumental ADLs (IADLs): using a map, preparing a hot meal, shopping for groceries, making phone calls, taking medications, doing work around the house, managing money. The number of difficulties with ADLs and IADLs were used as binary predictors (one or more or no difficulties). Body mass index was derived from weight and height measured during a home visit by a nurse (kg/m2) and 3 categories created: underweight/normal (<18–24.9), overweight (25.0–29.9), and obese (30+). It was not possible to explore separately the underweight category of BMI due to the small sample size (n = 28, 0.7% of the full sample).
Mental health/functioning
Depressive symptoms Depressive symptoms were assessed using the 8-item version of the Center for Epidemiological Studies-Depression scale (CESD-8) administered in the face-to-face interview (22). Enquiries were made about the degree to which the respondent had experienced depressive symptoms such as restless sleep and being unhappy over the prior month. We used a binary variable to define a high level of depressive symptoms as those reporting 4 or more (23). Cognitive impairment: This was measured using an index that combined the scores on the 2 memory tests (immediate and delayed memory), ranging from 0 to 20. Higher scores indicate better memory (24).
Chronic health conditions
Respondents were asked whether a physician had ever told them that they suffered from any of the following conditions: coronary heart disease, diabetes, stroke, arthritis, and osteoporosis or Parkinson’s disease.
Health behaviors
Physical activity Participants were asked how often (more than once a week, once a week, 1–3 times a month, and hardly ever/never) they took part in vigorous-, moderate-, and low-intensity physical activity. This questionnaire has been described in further detail elsewhere (25). We computed a 5-level score from inactive to active: (1) hardly ever/never does vigorous or moderate activity, (2) no vigorous & once a week/1–3 times a month (moderate), (3) no vigorous, but high moderate, (4) medium amount of moderate/vigorous, (5) regular vigorous. Frequency of alcohol intake in the last 12 months was ascertained in the self-completion questionnaire; responses were recoded into a binary variable defined as having an alcoholic drink daily (5/7 days a week) or less than daily (<5 days a week). Smoking status was recorded as current smoker, ex-smoker, or nonsmoker.
Statistical Method
Subdistribution hazard ratios (SHRs) with accompanying 95% confidence intervals (CIs) were by competing risk regression models; using a version of the subdistribution hazard model. This subdistribution hazard model allows the effect of covariates on the primary event (hospital admission after a fall) to be modeled after accounting for competing events that might occur during the follow-up instead of the event of interest, in this case, mortality (26). In additional sensitivity analysis, hazard ratios with accompanying 95% CIs were estimated using Cox proportional hazards regression models. All effect estimates were adjusted for a series of covariates. Interactions terms between each risk factor and sex were also examined. Survival time was measured from the date of the Wave 4 interview to first recorded hospital admission with secondary diagnoses of a fall, date of death, or end of follow-up (March 31, 2018).
To examine the association between quantitative covariates and the outcome we used restricted cubic spline regressions with Harrell knots (27). Restricted cubic splines offer a mechanism to model nonlinear relationships in regression models, by transformation of a continuous predictor.
Results
Our analytical sample comprised 3783 individuals (1992 women) of whom 315 had experienced admission to hospital after a fall (8%) during a median of 9 years of follow-up. Of these 315 events, 236 (75%) had sustained an injury as their principal diagnosis. Participants’ baseline characteristics (Table 1) show some differences between participants who were admitted to hospital for a fall-related injury and those who were not. Those participants, who had a hospital admission after a fall, were more likely to be older, female, living alone, and to be in the lowest wealth quintile than those who did not fall. Moreover, around 50% of those who fell scored lower than 8 on the SPPB test (0–12) compared to 20% of those who did not experience a fall. They were also more likely to report having had a severe fall that required medical attention in the past year, to report a chronic disease (coronary heart disease, diabetes, stroke, arthritis, osteoporosis, Parkinson’s disease), vision impairment, urinary incontinence, and difficulty with both ADLs and IADLs. There were no substantial differences in mean BMI, alcohol use, or smoking status, although participants who had a hospital admission after a fall were more likely to report low levels of physical activity.
Table 1.
Baseline Characteristics of Sample According to Fall Status
| Total (N = 3783) | No Fall (3468) | Hospital Admission After a Fall (N = 315) | p Value (test for trend) | |
|---|---|---|---|---|
| Age (y): mean (SD) | 69.6 (7.6) | 69.1 (7.2) | 74.4 (9.2) | <.0001 |
| Women | 1992 (52.7) | 1793 (51.7) | 199 (63.2) | <.0001 |
| Living alone | 948 (25.1) | 825 (23.8) | 123 (39.1) | <.0001 |
| Wealth (lowest quintile) | 511 (13.5) | 440 (12.7) | 71 (22.5) | <.0001 |
| Balance (side-by-side stand) | 88 (2.3) | 68 (2.0) | 20 (6.4) | <.0001 |
| Balance (tandem) | 715 (18.9) | 584 (16.8) | 131 (41.6) | <.0001 |
| Chair rises (single) | 307 (8.1) | 244 (7.0) | 63 (20.0) | <.0001 |
| Gait (m/s): mean (SD) | 0.86 (0.33) | 0.87 (0.33) | 0.67 (0.32) | <.0001 |
| Short Physical Performance Battery (≤8) | 1244 (32.9) | 1057 (30.5) | 187 (59.4) | <.0001 |
| Handgrip (kg): mean (SD) | 30.1 (11.0) | 30.6 (11.0) | 25.2 (10.0) | <.0001 |
| Self-reported previous fall (12 mo) | 929 (24.6) | 822 (23.7) | 107 (34.0) | <.0001 |
| Self-reported severe fall (12 mo) | 213 (5.6) | 171 (4.9) | 42 (13.3) | <.0001 |
| Vision impairment (fair/poor/blind) | 417 (11.0) | 359 (10.4) | 58 (18.4) | <.0001 |
| Urinary incontinence | 574 (15.2) | 489 (14.1) | 85 (27.0) | <.0001 |
| Difficulty with ADLs (1+) | 598 (15.8) | 501 (14.5) | 97 (30.8) | <.0001 |
| Difficulty with IADLs (1+) | 697 (18.4) | 572 (16.5) | 125 (39.7) | <.0001 |
| Depression (caseness) | 439 (11.6) | 377 (10.9) | 62 (19.7) | <.0001 |
| Cognition (verbal fluency): mean (SD) | 20.7 (6.5) | 20.9 (6.4) | 18.6 (6.7) | <.0001 |
| Coronary heart disease (CHD) | 458 (12.1) | 394 (11.4) | 64 (20.3) | <.0001 |
| Diabetes | 406 (10.8) | 362 (10.4) | 47 (14.9) | .014 |
| Stroke | 163 (4.3) | 139 (4.00) | 24 (7.6) | .003 |
| Arthritis | 1489 (39.4) | 1323 (38.2) | 166 (52.7) | <.0001 |
| Osteoporosis | 274 (7.2) | 231 (6.7) | 43 (13.7) | <.0001 |
| Parkinson’s disease | 23 (0.6) | 14 (0.4) | 9 (2.9) | <.0001 |
| BMI (kg/m2): mean (SD) | 28.2 (5.1) | 28.3 (5.0) | 27.8 (5.3) | .15 |
| Alcohol use (daily (5/7 days a week) | 925 (24.5) | 859 (24.8) | 66 (21.0) | .32 |
| Smoking (current smoker) | 386 (10.2) | 353 (10.2) | 33 (10.5) | .79 |
| Physical activity (sedentary) | 168 (4.4) | 141 (4.1) | 27 (8.6) | <.0001 |
Notes: ADLs = activities of daily living; BMI = body mass index; IADLs = instrumental activities of daily living. Values are numbers (percentages) unless stated otherwise.
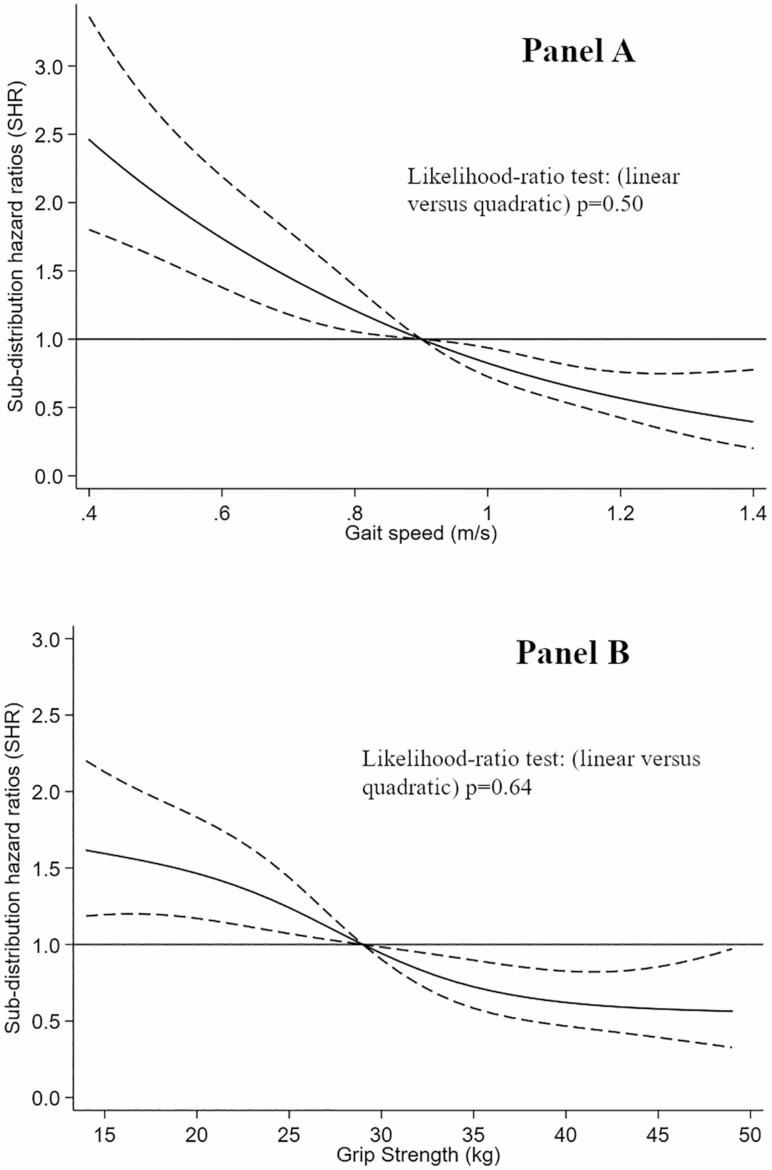
Age was a consistent independent predictor of admission to hospital after a fall in all models, and this association was found to be linear (likelihood-ratio test: linear vs quadratic; this linear association is depicted in Supplementary Figure S2; p = .63); therefore, age was included as a linear term in further models. After adjustment for age and sex, all objective assessments of mobility examined (balance tests, gait speed, chair rises, handgrip) were significantly associated with hospital admission after a fall (Table 2). However, after adjustment for other physical performance assessments (Model 2) only the 2 most difficult balance tests (semi-tandem, tandem) remained associated, with the tandem balance test showing the strongest association (SHRs = 1.57; 95% CI: 1.18, 2.09). Completing a single chair rise was associated with a higher risk of hospital admission after a fall, although after adjustment for the other physical performance assessments (Model 2), significance at conventional levels was not apparent. Nevertheless, a significant interaction with sex (p = .040) suggested that not being able to complete a single chair raise remained a consistent predictor for men (SHR = 2.46; 95% CI: 1.47, 4.13) but less so for women (SHR = 1.48; 95% CI: 0.98, 2.22). However, in sensitivity analysis where we examined only those who were admitted after an injury, this association attenuated. Slower gait speed was found to be a significant linear predictor (Table 2; Figure 1). Poor overall performance on the SPPB test (cut point ≤ 8) was consistently associated across all 3 models with increased risk of a hospital admission after a fall (Model 2: SHR = 1.57; 95% CI: 1.19, 2.08). This measure was also found to be associated with hospital admission for a fall-related injury (Model 2: SHR = 1.49; 95% CI: 1.09, 2.05). A significant interaction with sex (p = .038), suggested that this binary measure of SPPB performance was a stronger predictor of the outcome for men (SHR = 2.34; 95% CI: 1.53, 3.59) than women (SHR = 1.51; 95% CI: 1.08, 2.11). The association between handgrip strength and the outcome was initially found to be linear (Figure 1); however, after adjustment for chronic health conditions, BMI, and health behaviors, significance at conventional levels was not apparent. In Table 2, we show an association between reporting any previous fall in the last 12 months and admission to hospital for a fall-related injury (Model 1), although adjustment for covariates had an attenuating effect (Model 2 and Model 3). However, when the effect for the self-reported history of severe falls was examined, that remained consistent upon adjustment for a range of covariates (Model 2: SHR = 1.88; 95% CI: 1.34, 2.64). Self-reported history of severe falls was also found to be associated with hospital admission for a fall-related injury (Model 2: SHR = 1.66; 95% CI: 1.10, 2.51).
Table 2.
Association Between Objective Mobility Assessments, Self-Reported Previous Falls, and Hospital Admission for a Fall-Related Injury
| Competing Risk | ||||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||
| 315/3783 | SHR (95% CI) | p Value (test for trend) | SHR (95% CI) | p Value (test for trend) | SHR (95% CI) | p Value (test for trend) |
| Balance (side by side) | ||||||
| Completed (10 s) | 1.00 (Ref) | .013 | 1.00 | .18 | 1.00 | .05 |
| Not completed | 1.93 (1.15, 3.24) | 1.44 (0.85, 2.42) | 1.67 (1.02, 2.79) | |||
| Balance (semi-tandem) | ||||||
| Completed (10 s) | 1.00 (Ref) | <.001 | 1.00 | .028 | 1.00 | .004 |
| Not completed | 2.03 (1.45, 2.84) | 1.49 (1.04, 2.13) | 1.71 (1.19, 2.45) | |||
| Balance (tandem) | ||||||
| Completed (10 s) | 1.00 (Ref) | <.001 | 1.00 | .002 | 1.00 | <.001 |
| Not completed | 2.05 (1.55, 2.60) | 1.57 (1.18, 2.09) | 1.77 (1.35, 2.33) | |||
| Chair rises (single) | ||||||
| Completed | 1.00 (Ref) | <.001 | 1.00 | .065 | 1.00 | .002 |
| Not completed | 1.99 (1.46, 2.71) | 1.37 (0.98, 1.93) | 1.70 (1.22, 2.35) | |||
| Gait speed: (tertiles) | ||||||
| 1 (High) | 1.00 (Ref) | (<.001) | 1.00 | (<.001) | 1.00 | (<.001) |
| 2 | 1.83 (1.32, 2.53) | <.001 | 1.71 (1.23, 2.38) | .001 | 1.68 (1.20, 2.34) | .002 |
| 3 (Low) | 2.94 (2.09, 4.13) | <.001 | 2.12 (1.46, 3.10) | <.001 | 2.36 (1.62, 3.43) | <.001 |
| Short Physical Performance Battery | ||||||
| >8 | 1.00 (Ref) | <.0001 | 1.00 | .001 | 1.00 | <.001 |
| ≤8 | 2.12 (1.64, 2.74) | 1.57 (1.19, 2.08) | 1.75 (1.34, 2.29) | |||
| Handgrip tertiles | ||||||
| 1 (High) | 1.00 (Ref) | (.017) | 1.00 | (.12) | 1.00 | (.10) |
| 2 | 1.40 (0.95, 2.07) | .086 | 1.36 (0.92, 2.00) | .124 | 1.28 (0.87, 1.89) | .21 |
| 3 (Low) | 1.87 (1.20, 2.90) | .005 | 1.61 (1.02, 2.53) | .039 | 1.47 (0.93, 2.32) | .10 |
| Previous fall (12 mo) | ||||||
| No | 1.0 (Ref) | <.001 | 1.0 | .22 | 1.0 | .05 |
| Yes | 1.42 (1.12, 1.80) | 1.16 (0.91, 1.48) | 1.27 (1.00, 1.62) | |||
| Previous severe fall (12 mo) | ||||||
| No | 1.00 (Ref) | <.001 | 1.0 | <.001 | 1.0 | <.001 |
| Yes | 2.35 (1.70, 3.26) | 1.88 (1.34, 2.64) | 2.21 (1.59, 3.09) | |||
Notes: Model 1: age, sex; Model 2: Model 1 + living alone, wealth, fair/poor eyesight, urinary incontinence, ADLs, IADLs, and CESD-8; Model 3: Model 1 + chronic conditions (CHD, diabetes, stroke, arthritis, osteoporosis, Parkinson’s disease), BMI (normal, overweight, obese), smoking status (never, previous, current), alcohol drinking risk (5/7 days a week vs less). ADLs = activities of daily living; BMI = body mass index; CHD = coronary heart disease; IADLs = instrumental activities of daily living; SHR = subdistribution hazard ratio.
Figure 1.
Association of gait speed (Panel A) and grip strength (Panel B) with hospital admission after a fall. (Panel A) Graph shows age, sex, and body mass index (BMI)-adjusted subdistribution hazard ratios (SHRs) with 95% CI for the relation of gait speed, to the occurrence of admission to hospital after a fall. Gait speed was modeled by right-restricted cubic splines with 4 knots (0.45, 0.80, 1, and 1.35) in a Cox regression model. Reference value is 0.9 (m/s). (Panel B) Graph shows age, sex, and BMI-adjusted SHRs with 95% CI for the relation of grip strength (kg), to the occurrence of admission to hospital after a fall. Grip strength was modeled by right-restricted cubic splines with 4 knots (14, 25, 34, and 49) in a competing risk regression model. The reference value is 29 kg.
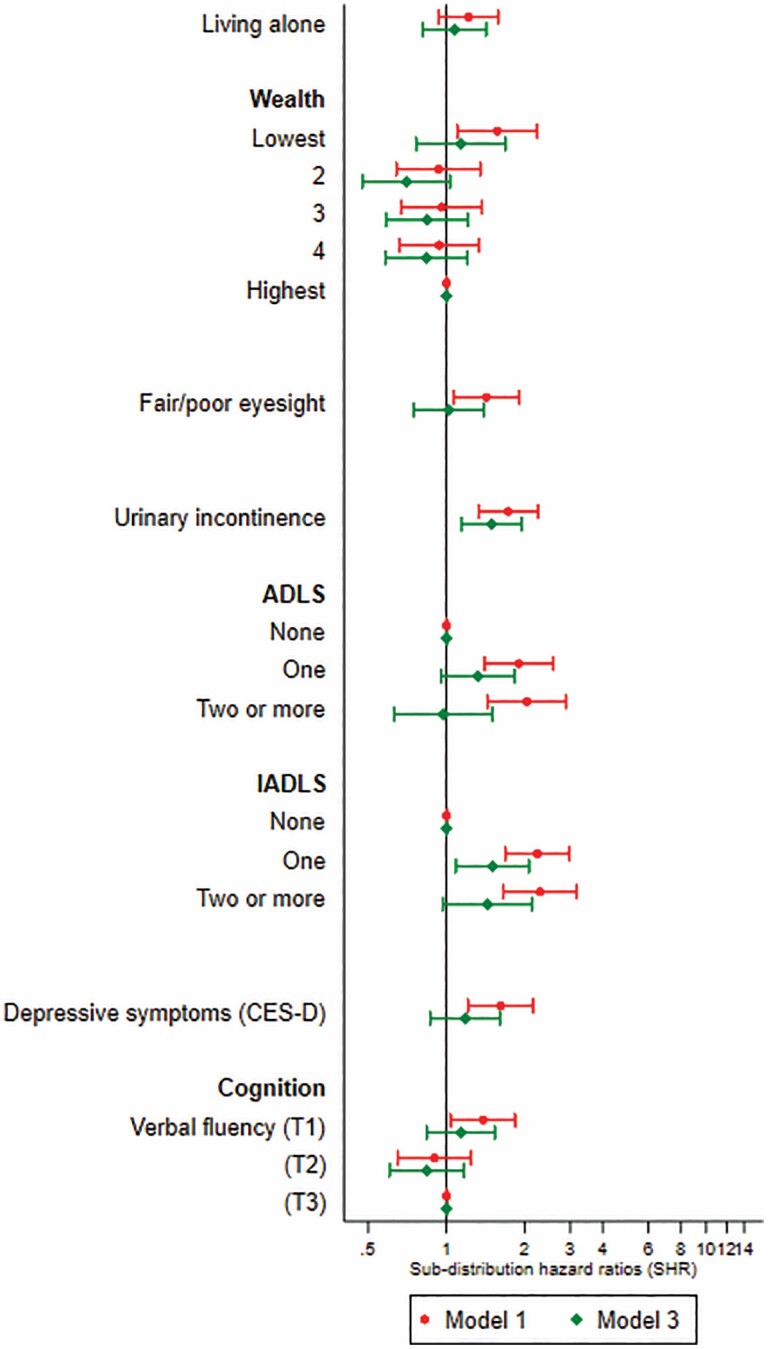
Figure 2 shows the association between demographic, physical, and mental functioning factors with a hospital admission after a fall. In a model including age and sex, those in the lowest quintile of wealth have an increased risk of a hospital admission after a fall (SHR = 1.59; 95% CI: 1.10, 2.23) (Supplementary Table S1). Several risk factors remained independent predictors of admission to hospital after a fall, when physical performance assessments and reporting a severe fall were taken into account. These are (Supplementary Table S1: Model 3) urinary incontinence (SHR = 1.49; 95% CI: 1.14, 1.95), reporting one impaired ADL (SHR = 1.32; 95% CI: 0.95, 1.83) and one impaired IADL (SHR = 1.51; 95% CI: 1.09, 2.08). Urinary incontinence and reporting one impaired IADL were also found to be associated with hospital admission for a fall-related injury, although the association was attenuated for those reporting one impaired ADL. No significant differences in the association between these predictors and the outcome by sex were observed.
Figure 2.
Association between demographic, physical, and mental functioning with hospital admission after a fall. Subdistribution hazard ratios (SHRs) with 95% CIs shown for Model 1 (age- and sex-adjusted), Model 3 mutually adjusted for all other risk factors, + Short Physical Performance Battery (SPPB) (binary), reporting a previous severe fall. *T1 = Tertile 1/T2 = Tertile 2/T3 = Tertile 3.
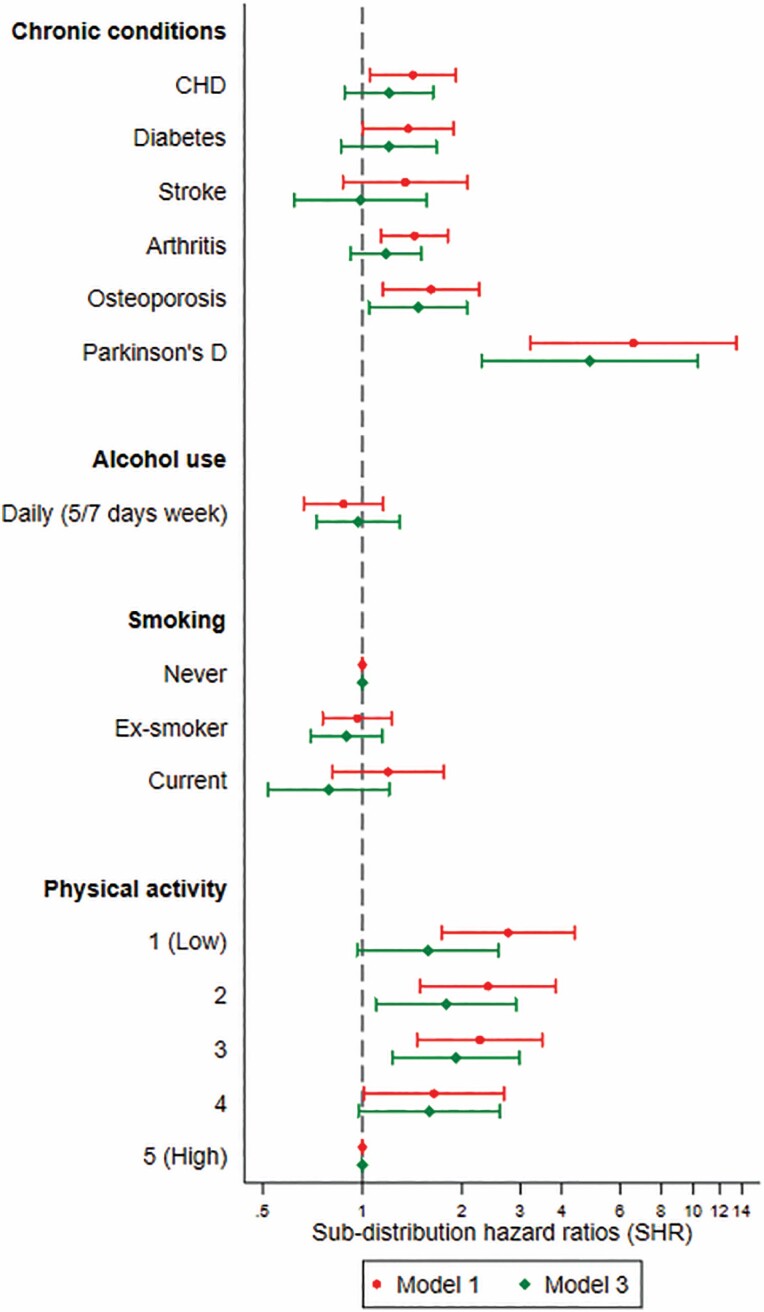
In Figure 3 associations with chronic conditions, BMI and health behaviors are shown. Most of the chronic conditions examined (coronary heart disease, diabetes, arthritis, and osteoporosis) were found to be significant predictors in a model adjusted for age and sex, although losing statistical significance after adjustment for physical performance assessments and fall history except for osteoporosis (SHR = 1.48; 95% CI: 1.05, 2.07) and Parkinson’s disease (SHR = 4.86; 95% CI: 2.29, 2.07). However, the small number of cases of Parkinson’s disease resulted in very wide CIs for these estimates. These predictors also appeared to be associated with hospital admission for a fall-related injury, although again the effect attenuates in these results. There were a significant association with physical activity (Supplementary Table S2: Model 1) so that lower levels of physical activity were associated with higher risks of hospitalization, but BMI, smoking, and alcohol use did not display any clear association. This pattern was confirmed by sensitivity analysis examining hospital admission for a fall-related injury. No significant differences in the association between these predictors and the outcome by sex were observed.
Figure 3.
Association between chronic health conditions, body mass index (BMI), and health behaviors with hospital admission after a fall. Subdistribution hazard ratios (SHRs) with 95% CIs shown for Model 1 (age- and sex-adjusted), Model 3 mutually adjusted for all other risk factors + Short Physical Performance Battery (SPPB) (<8/8+) and having had a previous severe fall.
Discussion
Main Results
In this prospective cohort study, we examined a range of risk factors to identify those that could be used to screen older people at risk of admission to hospital after a fall. We found that being unable to complete the most difficult balance test (tandem), having a slow walking speed and reporting a severe fall in the previous 12 months were the strongest predictors, once potential confounders had been taken into account in the model. We also found that gait speed and grip strength (a measure of upper body strength) exhibited a linear association with risk of a hospital admission after a fall.
Several other predictors—urinary incontinence, reporting a problem with an IADL, reporting a diagnosis of osteoporosis, or undertaking lower levels of physical activity—were predictive of an admission to hospital after a fall.
Strengths and Limitations of the Study
Our study has several methodological strengths. Firstly, we used a large nationally representative prospective cohort study, collecting a wide range of potential predictors, including objective measures of mobility, assessed by trained nurses. It was also possible to use a longitudinal research design to examine our research questions. We used an objective outcome, drawn from administrative health records, which allowed us to examine those who had been admitted to a hospital in the United Kingdom with an injury that was related to having experienced a fall. This minimized any potential recall bias associated with self-reported fall data and allowed us to examine only falls that had been severe enough to warrant hospital admission (7). However, this approach is not without limitations, firstly as this outcome might also be measuring the different potential care pathways to hospital admission that exist when an older person experiences a fall in the United Kingdom, for example, older people living in nursing homes might be less likely to be admitted to hospital after a fall. Furthermore, those who received medical treatment in a different setting were not captured. Secondly, there are limitations to using ICD-10 codes to assess a hospital admission after a fall, especially those that identify external causes and are used to report a secondary diagnosis related to hospital admission. Although these codes have previously been used in the United Kingdom to identify hospital admissions related to falls, we cannot rule out that there might be regional variation in the documentation or clinician variation in the coding of diagnoses which could lead to measurement error and underreporting. Furthermore, a number of participants did not authorize the use of linkage to hospital records and so these missing cases might contribute to underreporting. Finally, although we were able to cover a wide range of risk factors, several potentially important risk factors such as polypharmacy, environmental hazards, and syncope were not available at baseline.
Comparison With Other Studies
Research in this area has emphasized how falls among older people in the community are associated with a wide range of risk factors (3,7,11,28–30) with those most predictive of falling being gait and balance problems and a history of falls. Our present findings confirm the importance of these risk factors for admission to hospital after a fall. However, not all studies differentiate between falls events according to their severity (11) or document differences in how risk factors are associated with falls or their subcategories, for example, such as injurious falls or admission to hospital after a fall (10,11). We find that self-report of a severe fall, which required medical treatment, was the clearest predictor of admission to hospital. Additionally, we show that there is a linear association between slower walking speed and risk of admission to hospital after a fall, suggesting no adaptive mechanism to reduce fall risk (31). We find that the SPPB score was a strong predictor of the risk of hospital admission following a fall; this measure has also been found to be associated with falls occurring after discharge from hospital (32). The SPPB measure was found not to be associated with injurious falls (ascertained through interviews); however, the chair stand component was found to be an independent predictor of injurious falls (33). The chair stand component alone has also been found by previous studies to be associated with subsequent falls (34). We also find that this component was associated with hospital admission after a fall, although we find that the full battery of tests is more consistent as a predictor. The full battery of tests could be used to identify older people at risk of hospital admission after a fall (11). However, further research would be needed to confirm this in different settings and to explore the sensitivity of different cutoff scores.
We also find that reporting one or more ADLs and IADLs were associated with a risk of a hospital admission after a fall and in sensitivity analysis, were found to be associated with hospital admission for a fall-related injury. Reporting one or more impaired IADLs have been previously found to be an important predictor of injurious falls and this is confirmed here (35). Assessment of ADLs and IADLs could compliment objective assessments of physical impairment and also be offered in local community settings; these scores have also been found to be strongly associated with a fear of falling (36).
We also find that low levels of physical activity are a risk factor for serious falls requiring admission to hospital. This confirms previous work that suggests low levels of physical activity are associated with a risk of falls (37,38). Previous work in ELSA using retrospective recall of falls showed that low levels of activity were related a greater risk of reporting both injurious and noninjurious falls (39). However, increasing physical activity may not reduce fall risk, since a decline in physical activity may result from reduced balance, gait problems, and a fear of falling. Additionally, we find that groups who engaged in moderate levels of physical activity were more likely to be at risk of hospital admission following a fall. This might suggest the association between physical activity and risk of a severe fall is nonlinear and moderate levels of physical activity although beneficial for mobility might also increase exposure for falls. Several chronic conditions were consistent risk factors for falls, with the strongest association found for those older people reporting osteoporosis. Osteoporosis is often underdiagnosed among older people and so diagnosis is likely to be the result of having previously sustained a fall-related fracture. Admission to hospital following a fall could be related to the severity of the associated injury. Osteoporosis is related to bone health and combined with a fall is more likely to result in a fracture among older people (40). In addition, we find Parkinson’s disease to be a strong predictor of admission to hospital following a fall, which confirms previous evidence in this area that older adults with Parkinson’s disease are more likely to experience a fall and have higher rates of hospital admission following a fall than those without Parkinson’s disease (41). We also find that urinary incontinence remained a strong predictor of hospital admission after a fall, when comorbidities, physical performance assessments, and reporting a severe fall in the previous year were taken into account. A potential mechanism is that those with urinary incontinence may rush to get to the toilet, increasing their chance of falling, even if their balance and gait are steady under normal circumstances (42). Moreover, if urinary incontinence is being treated with medication it is also possible that this plays a role here, although we were not able to examine this in detail. However, it is important to note the findings of a recent study, which emphasized how risk factors for falls might be clustered together and so combining different risk factors, especially those that suggest physical and cognitive impairment might allow for improved prevention of falls in the community. Although identifying these clusters will require further examination of falls of all severity (38).
In conclusion, we examined a range of risk factors associated with a hospital admission after a fall. We corroborate evidence that the factors used to screen older people as being at high risk of experiencing a fall in the community (history of falls, gait, and balance) are significant predictors. However, we also find that struggling with self-care or urinary incontinence should be considered at an earlier point in the assessment of risk.
Supplementary Material
Acknowledgments
We would like to thank all ELSA participants for their valuable contribution to this study.
Funding
The English Longitudinal Study of Aging was developed by a team of researchers based at the University College London, NatCen Social Research, and the Institute for Fiscal Studies. The data were collected by NatCen Social Research. The funding is currently provided by the US National Institute on Aging (R01AG017644), and a consortium of UK government departments coordinated by the National Institute for Health Research. G.D.B. is partially supported by the UK Medical Research Council (MR/P023444/1) and the US National Institute on Aging (1R56AG052519-01; 1R01AG052519-01A1). The data were made available through the UK Data Service. The data are linked to the UK Data Archive and freely available through the UK data services and can be accessed here: discover.ukdataservice.ac.uk.
Conflict of Interest
None declared.
Author Contributions
J.G.A., P.Z., and G.D.B. contributed to study concept and design. J.G.A. and C.L. contributed to data acquisition and analysis. J.G.A. drafted the manuscript and figures. J.G.A., P.Z., C.L., and G.D.B. contributed to the interpretation of data and critical revision of the manuscript.
References
- 1.Public Health England Falls: Applying All Our Health. Public Health England; 2019. https://www.gov.uk/government/publications/falls-applying-all-our-health/falls-applying-all-our-health. Accessed January 22, 2020. [Google Scholar]
- 2.Lord SR, Sherrington C, Menz H. Falls in Older People. Risk Factors and Strategies for Prevention. Cambridge: Cambridge University Press; 2001. [Google Scholar]
- 3.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(suppl 2):ii37–ii41. doi: 10.1093/ageing/afl084 [DOI] [PubMed] [Google Scholar]
- 4.Gill TM, Murphy TE, Gahbauer EA, Allore HG. Association of injurious falls with disability outcomes and nursing home admissions in community-living older persons. Am J Epidemiol. 2013;178(3):418–425. doi: 10.1093/aje/kws554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337(18):1279–1284. doi: 10.1056/NEJM199710303371806 [DOI] [PubMed] [Google Scholar]
- 6.Scuffham P, Chaplin S, Legood R. Incidence and costs of unintentional falls in older people in the United Kingdom. J Epidemiol Community Health. 2003;57(9):740–744. doi: 10.1136/jech.57.9.740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.NICE. Clinical Guideline: Assessment and Prevention of Falls in Older People. National Institute of Clinical Excellence (NICE); 2013. [PubMed] [Google Scholar]
- 8.AGS/BGS. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–157. doi: 10.1111/j.1532-5415.2010.03234.x [DOI] [PubMed] [Google Scholar]
- 9.Perell KL, Nelson A, Goldman RL, Luther SL, Prieto-Lewis N, Rubenstein LZ. Fall risk assessment measures: an analytic review. J Gerontol A Biol Sci Med Sci. 2001;56(12):M761–M766. doi: 10.1093/gerona/56.12.m761 [DOI] [PubMed] [Google Scholar]
- 10.Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21(5):658–668. doi: 10.1097/EDE.0b013e3181e89905 [DOI] [PubMed] [Google Scholar]
- 11.Vieira ER, Palmer RC, Chaves PH. Prevention of falls in older people living in the community. BMJ. 2016;353:i1419. doi: 10.1136/bmj.i1419 [DOI] [PubMed] [Google Scholar]
- 12.Public Health England. Falls and Fracture Consensus Statement: Supporting Commissioning for Prevention. London: Public Health England; 2017. [Google Scholar]
- 13.Steptoe A, Breeze E, Banks J, Nazroo J. Cohort profile: the English Longitudinal Study of Ageing. Int J Epidemiol. 2013;42(6):1640–1648. doi: 10.1093/ije/dys168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gilbert R, Todd C, May M, Yardley L, Ben-Shlomo Y. Socio-demographic factors predict the likelihood of not returning home after hospital admission following a fall. J Public Health (Oxf). 2010;32(1):117–124. doi: 10.1093/pubmed/fdp077 [DOI] [PubMed] [Google Scholar]
- 15.Gilbert T, Neuburger J, Kraindler J, et al. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet. 2018;391(10132):1775–1782. doi: 10.1016/S0140-6736(18)30668-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Welsh C, Celis-Morales CA, Ho F, et al. Association of injury related hospital admissions with commuting by bicycle in the UK: prospective population based study. BMJ. 2020;368:m336. doi: 10.1136/bmj.m336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–M94. doi: 10.1093/geronj/49.2.m85 [DOI] [PubMed] [Google Scholar]
- 18.Zaninotto P, Sacker A, Head J. Relationship between wealth and age trajectories of walking speed among older adults: evidence from the English Longitudinal Study of Ageing. J Gerontol A Biol Sci Med Sci. 2013;68(12):1525–1531. doi: 10.1093/gerona/glt058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dodds RM, Pakpahan E, Granic A, Davies K, Sayer AA. The recent secular trend in grip strength among older adults: findings from the English Longitudinal Study of Ageing. Eur Geriatr Med. 2019;10(3):395–401. doi: 10.1007/s41999-019-00174-4 [DOI] [PubMed] [Google Scholar]
- 20.Dodds RM, Syddall HE, Cooper R, et al. Grip strength across the life course: normative data from twelve British studies. PLoS One. 2014;9(12):e113637. doi: 10.1371/journal.pone.0113637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zaninotto P, Lassale C. Socioeconomic trajectories of body mass index and waist circumference: results from the English Longitudinal Study of Ageing. BMJ Open. 2019;9(4):e025309. doi: 10.1136/bmjopen-2018-025309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Radloff L. The CES-D scale. A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- 23.White J, Zaninotto P, Walters K, et al. Duration of depressive symptoms and mortality risk: the English Longitudinal Study of Ageing (ELSA). Br J Psychiatry. 2016;208(4):337–342. doi: 10.1192/bjp.bp.114.155333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Batty GD, Deary IJ, Zaninotto P. Association of cognitive function with cause-specific mortality in middle and older age: follow-up of participants in the English Longitudinal Study of Ageing. Am J Epidemiol. 2016;183(3):183–190. doi: 10.1093/aje/kwv139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Demakakos P, Hamer M, Stamatakis E, Steptoe A. Low-intensity physical activity is associated with reduced risk of incident type 2 diabetes in older adults: evidence from the English Longitudinal Study of Ageing. Diabetologia. 2010;53(9):1877–1885. doi: 10.1007/s00125-010-1785-x [DOI] [PubMed] [Google Scholar]
- 26.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509. doi: 10.1080/01621459.1999.10474144 [DOI] [Google Scholar]
- 27.Harrell FE Jr. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis. New York: Springer; 2001. [Google Scholar]
- 28.Lusardi MM, Fritz S, Middleton A, et al. Determining risk of falls in community dwelling older adults: a systematic review and meta-analysis using posttest probability. J Geriatr Phys Ther. 2017;40(1):1–36. doi: 10.1519/JPT.0000000000000099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61. doi: 10.1016/j.maturitas.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 30.Tinetti ME, Kumar C. The patient who falls: “It’s always a trade-off”. JAMA. 2010;303(3):258–266. doi: 10.1001/jama.2009.2024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Quach L, Galica AM, Jones RN, et al. The nonlinear relationship between gait speed and falls: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study. J Am Geriatr Soc. 2011;59(6):1069–1073. doi: 10.1111/j.1532-5415.2011.03408.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Quadri P, Tettamanti M, Bernasconi S, Trento F, Loew F. Lower limb function as predictor of falls and loss of mobility with social repercussions one year after discharge among elderly inpatients. Aging Clin Exp Res. 2005;17(2):82–89. doi: 10.1007/BF03324578 [DOI] [PubMed] [Google Scholar]
- 33.Ward RE, Leveille SG, Beauchamp MK, et al. Functional performance as a predictor of injurious falls in older adults. J Am Geriatr Soc. 2015;63(2):315–320. doi: 10.1111/jgs.13203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang F, Ferrucci L, Culham E, Metter EJ, Guralnik J, Deshpande N. Performance on five times sit-to-stand task as a predictor of subsequent falls and disability in older persons. J Aging Health. 2013;25(3):478–492. doi: 10.1177/0898264313475813 [DOI] [PubMed] [Google Scholar]
- 35.Ek S, Rizzuto D, Calderón-Larrañaga A, Franzén E, Xu W, Welmer AK. Predicting first-time injurious falls in older men and women living in the community: development of the first injurious fall screening tool. J Am Med Dir Assoc. 2019;20(9):1163–1168.e3. doi: 10.1016/j.jamda.2019.02.023 [DOI] [PubMed] [Google Scholar]
- 36.Cumming RG, Salkeld G, Thomas M, Szonyi G. Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol A Biol Sci Med Sci. 2000;55(5):M299–M305. doi: 10.1093/gerona/55.5.m299 [DOI] [PubMed] [Google Scholar]
- 37.Pereira CLN, Vogelaere P, Baptista F. Role of physical activity in the prevention of falls and their consequences in the elderly. Eur Rev Aging Phys Act. 2008;5(1):51–58. doi: 10.1007/s11556-008-0031-8 [DOI] [Google Scholar]
- 38.Ek S, Rizzuto D, Fratiglioni L, Johnell K, Xu W, Welmer AK. Risk profiles for injurious falls in people over 60: a population-based cohort study. J Gerontol A Biol Sci Med Sci. 2018;73(2):233–239. doi: 10.1093/gerona/glx115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smith L, Stubbs B, Hamer M. Changes in physical activity behavior and risk of falls over 8 years’ follow-up: English Longitudinal Study of Aging. Mayo Clin Proc. 2019;94(2):365–367. doi: 10.1016/j.mayocp.2018.11.014 [DOI] [PubMed] [Google Scholar]
- 40.Morrison A, Fan T, Sen SS, Weisenfluh L. Epidemiology of falls and osteoporotic fractures: a systematic review. Clinicoecon Outcomes Res. 2013;5:9–18. doi: 10.2147/CEOR.S38721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Paul SS, Harvey L, Canning CG, et al. Fall-related hospitalization in people with Parkinson’s disease. Eur J Neurol. 2017;24(3):523–529. doi: 10.1111/ene.13238 [DOI] [PubMed] [Google Scholar]
- 42.Bresee C, Dubina ED, Khan AA, et al. Prevalence and correlates of urinary incontinence among older community-dwelling women. Female Pelvic Med Reconstr Surg. 2014;20(6):328–333. doi: 10.1097/SPV.0000000000000093 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.