Introduction
Acute generalized pustular psoriasis (AGPP) is a rare but potentially life-threatening variant of psoriasis vulgaris, with many possible triggers, including medications, illness, and pregnancy.1 Here, we describe, to our knowledge, the first reported case of AGPP following the COVID-19 messenger RNA (mRNA) vaccine.
Case report
A man in his 40s with morbid obesity, hypertension, depression/anxiety, and psoriasis presented with an acute, rapidly progressive skin eruption. His preexisting psoriasis had been present for years, with minimally symptomatic transient plaques managed with emollients. His medications included lisinopril and bupropion, which were started 1 month earlier. He received Pfizer vaccine (first dose) 5 days before the development of the rash, with no recent illnesses or new medication exposures. The rash began with tender, erythematous patches and plaques on his abdomen and arms, with progression to his legs and buttocks. Two days after onset, an immediate care clinic diagnosed a yeast infection and prescribed fluconazole 100 mg orally (1 dose taken) and nystatin cream. The following day, he had significantly more surface area involvement of rash with worsening malaise, and upon presentation to the emergency department, he was prescribed prednisone 50 mg/d (0.3 mg/kg/d; patient's weight, 172.36 kg) and doxycycline 100 mg twice a day and given 1 dose of intravenous methylprednisolone 125 mg. The tick-borne illness panel was negative, and he was instructed to discontinue lisinopril and bupropion.
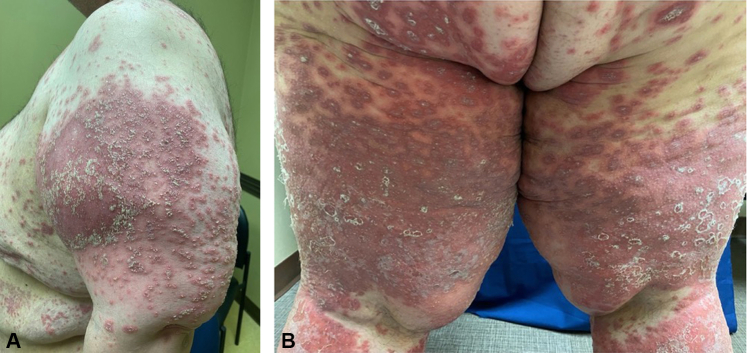
With worsening cutaneous and systemic symptoms, the patient presented to the dermatology department approximately 1 week into his rash. On examination, he was ill-appearing with chills, malaise, decreased oral intake for several days, and diffuse erythematous patches studded with fine pustules involving his trunk, arms, and legs (Fig 1, A and B).
Fig 1.
A, Diffuse erythematous plaques studded with pustules on the proximal aspect of the upper portion of the patient's arm. B, Proximal aspect of the upper portion of the patient's thighs and buttocks showing coalescing erythematous patches.
Two skin biopsies were performed, and the patient was promptly admitted to the hospital. He had leukocytosis and acute kidney injury secondary to dehydration. Blood cultures showed no growth. He was given intravenous fluids and was treated with cyclosporine 4 mg/kg/d and a single dose of infliximab 5 mg/kg. The biopsies showed psoriasiform dermatitis with intraepidermal neutrophilic pustules, supporting the clinical diagnosis of AGPP. He had significant improvement after 3 days of treatment, and cyclosporine was decreased to 2 mg/kg/d for 2 days secondary to the elevated creatinine levels. He was discharged with clearance of his pustular psoriasis and started on secukinumab as an outpatient.
Discussion
The etiology of AGPP is uncertain; however, it has been associated with various medications, viral and bacterial infections, the influenza vaccine, hypocalcemia, and pregnancy, among other triggers. Traditionally, dermatologists have avoided the use of systemic steroids in patients with psoriasis for fear of inducing AGPP upon withdrawal.1 However, a recent study reported conflicting evidence in which <1.5% of patients with psoriasis developed flares after exposure to a systemic glucocorticoid, with no cases of pustular psoriasis.2 It is important to note that our patient presented with AGPP before the addition of a systemic glucocorticoid, and he received low-dose treatment with oral prednisone for only 3 days. Therefore, systemic steroids are not a favored etiology in this case.
Acute generalized exanthematous pustulosis from bupropion must also be considered in the differential diagnosis.3 Acute generalized exanthematous pustulosis, however, develops within 1 to 2 days following exposure to the causative drug and quickly resolves with the withdrawal of the medication, in contrast to AGPP, which typically develops within 2 to 7 weeks following consumption of the responsible drug.4,5 Our patient had been on bupropion for 1 month before the development of the rash and experienced progression for up to a week, despite discontinuation of the medication.
To date, McMahon et al6 have documented 2 exacerbations of existing psoriasis (unknown type) among 414 patients after receiving the COVID-19 vaccine. The mechanisms responsible for the exacerbation of AGPP after COVID-19 mRNA vaccination are not yet understood. Rare cases of psoriasis have been reported following the administration of tetanus-diphtheria and bacillus Calmette–Guérin vaccines, which are both mRNA vaccines.7,8 Researchers have shown that proteins generated in response to the vaccine induce interleukin 6 production, which, in turn, promotes the development of Th1 and Th17 cells, which trigger the release of downstream cytokines that play a key role in the development of the epidermal changes seen in AGPP.7,8 Viswanathan et al9 described how stress-induced (by vaccination) increase in leukocyte trafficking to the sites of immune activation may be beneficial for promoting immunoprotection during vaccination but may also mediate the exacerbation of autoimmune diseases. The close temporal relationship between vaccination and the onset of AGPP in our patient suggests a causal role. Although a case of AGPP has been reported in Turkey following the administration of the Sinovac BioTech inactivated virus vaccine (CoronoVac), this case is, to our knowledge, the first documented instance of AGPP related to an mRNA COVID-19 vaccination.10
Conflicts of interest
None disclosed.
Acknowledgments
The authors acknowledge Katie Cregor, APRN, for providing one of the clinical images in this case.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Hoegler K.M., John A.M., Handler M.Z., Schwartz R.A. Generalized pustular psoriasis: a review and update on treatment. J Eur Acad Dermatol Venereol. 2018;32(10):1645–1651. doi: 10.1111/jdv.14949. [DOI] [PubMed] [Google Scholar]
- 2.Gregoire A.R.F., DeRuyter B.K., Stratman E.J. Psoriasis flares following systemic glucocorticoid exposure in patients with a history of psoriasis. JAMA Dermatol. 2021;157(2):198–201. doi: 10.1001/jamadermatol.2020.4219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ray A.K., Wall G.C. Bupropion-induced acute generalized exanthematous pustulosis. Pharmacotherapy. 2011;31(6):621. [Google Scholar]
- 4.Feldmeyer L., Heidemeyer K., Yawalkar N. Acute generalized exanthematous pustulosis: pathogenesis, genetic background, clinical variants and therapy. Int J Mol Sci. 2016;17(8):1214. doi: 10.3390/ijms17081214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Behrang E., Hallaji Z., Ghiasi M. Hydroxychloroquine-induced unusual generalized pustular cutaneous reaction as a new clinical entity: a case series. Immunoregulation. 2020;3(1):67–72. [Google Scholar]
- 6.McMahon D.E., Amerson E., Rosenbach M. Cutaneous reactions reported after Moderna and Pfizer COVID-19 vaccination: a registry-based study of 414 cases. J Am Acad Dermatol. 2021;85(1):46–55. doi: 10.1016/j.jaad.2021.03.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Takayama K., Satoh T., Hayashi M., Yokozeki H. Psoriatic skin lesions induced by BCG vaccination. Acta Derm Venereol. 2008;88(6):621–622. doi: 10.2340/00015555-0496. [DOI] [PubMed] [Google Scholar]
- 8.Macias V.C., Cunha D. Psoriasis triggered by tetanus-diphtheria vaccination. Cutan Ocul Toxicol. 2013;32(2):164–165. doi: 10.3109/15569527.2012.727936. [DOI] [PubMed] [Google Scholar]
- 9.Viswanathan K., Dhabhar F.S. Stress-induced enhancement of leukocyte trafficking into sites of surgery or immune activation. Proc Natl Acad Sci U S A. 2005;102(16):5808–5813. doi: 10.1073/pnas.0501650102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Onsun N., Kaya G., Işık B.G., Güneş B. A generalized pustular psoriasis flare after CoronaVac COVID-19 vaccination: case report. Health Promot Perspect. 2021;11(2):261–262. doi: 10.34172/hpp.2021.32. [DOI] [PMC free article] [PubMed] [Google Scholar]