Abstract
The Healthy People Initiative has served as the leading disease prevention and health promotion roadmap for the nation since its inception in 1979. Healthy People 2020 (HP2020), the initiative’s current iteration, sets a national prevention agenda with health goals and objectives by identifying nationwide health improvement priorities and providing measurable objectives and targets from 2010 to 2020. Central to the overall mission and vision of Healthy People is an emphasis on achieving health equity, eliminating health disparities, and improving health for all population groups. The Heart Disease and Stroke (HDS) Work Group of the HP2020 Initiative aims to leverage advances in biomedical science and prevention research to improve cardiovascular health across the nation. The initiative provides a platform to foster partnerships and empower professional societies and nongovernmental organizations, governments at the local, state, and national levels, and healthcare professionals to strengthen policies and improve practices related to cardiovascular health. Disparities in cardiovascular disease burden are well recognized across, for example, race/ethnicity, sex, age, and geographic region, and improvements in cardiovascular health for the entire population are only possible if such disparities are addressed through efforts that target individuals, communities, and clinical and public health systems. This article summarizes criteria for creating and tracking the 50 HDS HP2020 objectives in 3 areas (prevention, morbidity/mortality, and systems of care), reports on progress toward the 2020 targets for these objectives based on the most recent data available, and showcases examples of relevant programs led by participating agencies. Although most of the measurable objectives have reached the 2020 targets ahead of time (n=14) or are on track to meet the targets (n=7), others may not achieve the decade’s targets if the current trends continue, with 3 objectives moving away from the targets. This summary illustrates the utility of HP2020 in tracking measures of cardiovascular health that are of interest to federal agencies and policymakers, professional societies, and other nongovernmental organizations. With planning for Healthy People 2030 well underway, stakeholders such as healthcare professionals can embrace collaborative opportunities to leverage existing progress and emphasize areas for improvement to maximize the Healthy People initiative’s positive impact on population-level health.
Keywords: heart disease, prevention, public policy, stroke
Age-adjusted death rates from cardiovascular disease (CVD) have declined >70% since the 1960s1 because of advances in prevention and treatment.2,3 However, the most recent data suggest that the declines in mortality have begun to stall.4,5 CVD remains the leading cause of death in the United States, accounting for >800 000 deaths annually6 with coronary heart disease, stroke, high blood pressure, and heart failure comprising nearly 80% of the deaths attributable to CVD.7 The burden of CVD and associated risk factors is not distributed equally across population groups, and there are wide geographic and demographic variations in mortality, particularly for ischemic heart disease and stroke.8-10
The Healthy People Initiative, a large, national health agenda overseen by the US Department of Health and Human Services, establishes nationwide health improvement priorities and targets to be achieved each decade.11 Healthy People 2020 (HP2020) includes 50 Heart Disease and Stroke (HDS) objectives12 that emphasize key cardiovascular health goals. The tracking of these objectives provides information to state and local health departments, tribal organizations, and other health practitioners to help guide priorities and for decision making and planning, which collectively may lead to improvements in CVD-related morbidity and mortality. Progress was evaluated for the measurable heart disease and stroke objectives, and results were detailed in the HP2020 Midcourse Review,13 which was released in January 2017. Data for the objectives have been updated since that time, and the most recent data points are reflected in this paper.
In this paper, we provide a brief background about the Healthy People initiative and an overview of the current HP2020 HDS objectives, summarize progress according to recent data including identified disparities, and highlight examples of relevant federal agency research and programs that facilitate improvement toward the health targets. The objective of this paper is to raise awareness among state and local health departments, tribal organizations, and research and health professional communities of the potential for HP2020 as a tool that can be used for priority setting and planning, research, and other activities that lead to improved population health. With planning for Healthy People 2030 (HP2030) well underway, stakeholders can embrace collaborative opportunities to leverage existing progress and emphasize areas for improvement to maximize the Healthy People initiative’s positive impact on population-level health.
THE HEALTHY PEOPLE INITIATIVE
The Healthy People Initiative sets science-based, national objectives with 10-year targets to improve the health of the nation. Launched in 1979 with a Surgeon General’s Report,14 each subsequent iteration of the Healthy People initiative has identified emerging public health priorities and helped to align disease prevention and health promotion strategies, research, and resources. The Healthy People initiative uses a systematic, evidence-based approach to create benchmarks and monitor progress over time and serves as the disease prevention and health promotion roadmap for the nation (Appendix in the online-only Data Supplement).
The Healthy People initiative encourages collaboration across communities and sectors, and provides a framework and resources to guide research agendas, program planning, and public policy on federal and local levels (Table I in the online-only Data Supplement). States and territories use the Healthy People initiative in a variety of ways that range from priority identification and planning, to conducting community assessments as part of health department accreditation, to developing their own state-specific Healthy People plans.15,16
HP2020 identified 1288 objectives that were organized into 42 topic areas, including HDS, led by subject matter experts from across the US Department of Health and Human Services (Figure I in the online-only Data Supplement). To further focus action and capture public and stakeholder attention, HP2020 recognizes a subset of 26 objectives as Leading Health Indicators (Table II in the online-only Data Supplement). The Leading Health Indicators represent high-priority health issues that, if addressed appropriately, will reduce the leading causes of preventable deaths and illnesses. Acknowledging the importance of hypertension control, the Leading Health Indicators include HDS-12, which seeks to “increase the proportion of adults with hypertension whose blood pressure is under control.”
The Healthy People Initiative has an overarching emphasis on eliminating health disparities and achieving health equity, and data on relevant subgroup populations are presented for all Healthy People initiative objectives when possible. Health disparities refer to health differences that are closely linked with social, economic, or environmental disadvantage, and are observed among groups of people who have systematically experienced greater obstacles to health based on their racial or ethnic background, religion, socioeconomic status, sex, age, mental health, disability status, sexual orientation or gender identity, geographic location, or other characteristics linked to discrimination or exclusion. In this paper, we present and discuss some of the disparities identified for the HDS objectives.
HP2020 HDS OBJECTIVES AND TARGETS
The HP2020 HDS topic area objectives can be grouped into 3 broad categories: (1) prevention (risk factor detection, management, treatment and control), (2) morbidity and mortality, and (3) systems of care (emergency medical response, time to treatment of acute conditions). Of the 50 HDS objectives, 13 remain in developmental status, which means a data source has been identified, but data are not yet available or changes in national guidelines and recommendations have limited their utility in monitoring; these will not be discussed further in this paper (Table).
Table.
Heart Disease and Stroke Objectives
| Number | Title | Data Source | Category |
|---|---|---|---|
| HDS-1 | (Developmental) Increase overall cardiovascular health in the US population | NHANES | Prevention |
| HDS-2 | Reduce coronary heart disease deaths | NVSS–M | Morbidity/Mortality |
| HDS-3 | Reduce stroke deaths | NVSS–M | Morbidity/Mortality |
| HDS-4 | Increase the proportion of adults who have had their blood pressure measured within the preceding 2 years and can state whether their blood pressure was normal or high | NHIS | Prevention |
| HDS-5.1 | Reduce the proportion of adults with hypertension | NHANES | Morbidity/Mortality |
| HDS-5.2 | Reduce the proportion of children and adolescents with hypertension | NHANES | Morbidity/Mortality |
| HDS-6 | Increase the proportion of adults who have had their blood cholesterol checked within the preceding 5 years | NHIS | Prevention |
| HDS-7 | Reduce the proportion of adults with high total blood cholesterol levels | NHANES | Morbidity/Mortality |
| HDS-8 | Reduce the mean total blood cholesterol levels among adults | NHANES | Prevention |
| HDS-9 | Increase the proportion of adults with prehypertension who meet the recommended guidelines for | ||
| HDS-9.1 | Body mass index | NHANES | Prevention |
| HDS-9.2 | Saturated fat consumption | NHANES | Prevention |
| HDS-9.3 | (Developmental) Sodium intake | NHANES | Prevention |
| HDS-9.4 | Physical activity | NHANES | Prevention |
| HDS-9.5 | (Developmental) Moderate alcohol consumption | NHANES | Prevention |
| HDS-10 | Increase the proportion of adults with hypertension who meet the recommended guidelines for: | ||
| HDS-10.1 | Body mass index | NHANES | Prevention |
| HDS-10.2 | Saturated fat consumption | NHANES | Prevention |
| HDS-10.3 | Sodium intake | NHANES | Prevention |
| HDS-10.4 | Physical activity | NHANES | Prevention |
| HDS-10.5 | (Developmental) Moderate alcohol consumption | NHANES | Prevention |
| HDS-11 | Increase the proportion of adults with hypertension who are taking the prescribed medications to lower their blood pressure | NHANES | Prevention |
| HDS-12 | Increase the proportion of adults with hypertension whose blood pressure is under control | NHANES | Prevention |
| HDS-13 | (Developmental) Increase the proportion of adults with elevated low-density lipoprotein cholesterol who have been advised by a healthcare provider regarding cholesterol-lowering | ||
| HDS-13.1 | (Developmental) Diet | NHANES | Prevention |
| HDS-13.2 | (Developmental) Physical activity | NHANES | Prevention |
| HDS-13.3 | (Developmental) Weight control | NHANES | Prevention |
| HDS-13.4 | (Developmental) Prescribed drug therapy | NHANES | Prevention |
| HDS-14 | (Developmental) Increase the proportion of adults with elevated low-density lipoprotein cholesterol who adhere to prescribed cholesterol-lowering | ||
| HDS-14.1 | (Developmental) Diet | NHANES | Prevention |
| HDS-14.2 | (Developmental) Physical activity | NHANES | Prevention |
| HDS-14.3 | (Developmental) Weight control | NHANES | Prevention |
| HDS-14.4 | (Developmental) Prescribed drug therapy | NHANES | Prevention |
| HDS-15.1 | Increase aspirin use as recommended among women aged 55 to 79 years with no history of cardiovascular disease | NAMCS | Prevention |
| HDS-15.2 | Increase aspirin use as recommended among men aged 45 to 79 years with no history of cardiovascular disease | NAMCS | Prevention |
| HDS-16.1 | Increase the proportion of adults aged 20 years and older who are aware of the early warning symptoms and signs of a heart attack and the importance of accessing rapid emergency care by calling 9–1–1 or another emergency number | NHIS | Systems of Care |
| HDS-16.2 | Increase the proportion of adults aged 20 years and older who are aware of the early warning symptoms and signs of a heart attack | NHIS | Systems of Care |
| HDS-16.3 | Increase the proportion of adults aged 20 years and older who are aware of the importance of accessing rapid emergency care for a heart attack by calling 9–1–1 or another emergency number | NHIS | Systems of Care |
| HDS-17.1 | Increase the proportion of adults aged 20 years and older who are aware of the early warning symptoms and signs of a stroke and the importance of accessing rapid emergency care by calling 9–1–1 or another emergency number | NHIS | Systems of Care |
| HDS-17.2 | Increase the proportion of adults aged 20 years and older who are aware of the early warning symptoms and signs of a stroke | NHIS | Systems of Care |
| HDS-17.3 | Increase the proportion of adults aged 20 years and older who are aware of the importance of accessing rapid emergency care for a stroke by calling 9–1–1 or another emergency number | NHIS | Systems of Care |
| HDS-18 | (Developmental) Increase the proportion of out-of-hospital cardiac arrests in which appropriate bystander and emergency medical services were administered | CARES | Systems of Care |
| HDS-19.1 | Increase the proportion of eligible patients with heart attacks who receive fibrinolytic therapy within 30 min of hospital arrival | ACTION-GWTG | Systems of Care |
| HDS-19.2 | Increase the proportion of eligible patients with heart attacks who receive percutaneous intervention within 90 min of hospital arrival | ACTION-GWTG | Systems of Care |
| HDS-19.3 | Increase the proportion of eligible patients with strokes who receive acute reperfusion therapy within 3 h from symptom onset | GWTG-Stroke | Systems of Care |
| HDS-20.1 | Increase the proportion of adults with coronary heart disease who have their low-density lipoprotein cholesterol at or below recommended levels | NHANES | Prevention |
| HDS-20.2 | Increase the proportion of adults who have had a stroke who have their low-density lipoprotein cholesterol at or below recommended levels | NHANES | Prevention |
| HDS-21 | Increase the proportion of adults with a history of cardiovascular disease who are using aspirin or antiplatelet therapy to prevent recurrent cardiovascular events | NAMCS | Prevention |
| HDS-22 | Increase the proportion of adult heart attack survivors who are referred to a cardiac rehabilitation program at discharge | ACTION-GWTG | Systems of Care |
| HDS-23 | Increase the proportion of adult stroke survivors who are assessed for and/or referred to rehabilitation services. | GWTG-Stroke | Systems of Care |
| HDS-24.1 | Reduce hospitalizations of adults aged 65 to 74 years with heart failure as the principal diagnosis | NHDS | Morbidity/Mortality |
| HDS-24.2 | Reduce hospitalizations of adults aged 75 to 84 years with heart failure as the principal diagnosis | NHDS | Morbidity/Mortality |
| HDS-24.3 | Reduce hospitalizations of adults aged 85 years and older with heart failure as the principal diagnosis | NHDS | Morbidity/Mortality |
| HDS-25 | Increase the proportion of patients with hypertension in clinical health systems whose blood pressure is under control | NAMCS | Prevention |
The table lists each of the Healthy People 2020 Heart Disease and Stroke (HDS) Objectives with the number, title, data source, and category. Data source definitions: ACTION-GWTG indicates Acute Coronary Treatment and Intervention Outcomes Network Registry–Get With the Guidelines, American College of Cardiology; CARES, Cardiac Arrest Registry to Enhance Survival, Emory University; GWTG-Stroke, Get With the Guidelines Stroke Registry, American Heart Association and American Stroke Association; NAMCS, National Ambulatory Medical Care Survey, Centers for Disease Control and Prevention (CDC)/National Center for Health Statistics (NCHS); NHANES, National Health and Nutrition Examination Survey, CDC/NCHS; NHDS, National Hospital Discharge Survey, CDC/NCHS; NHIS, National Health Interview Survey, CDC/NCHS; and NVSS–M, National Vital Statistics System–Mortality, CDC/NCHS.
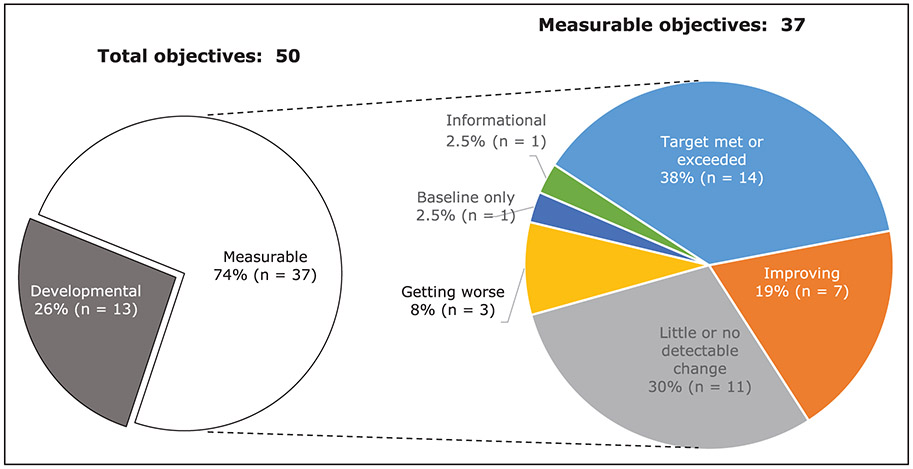
Targets for each objective were developed to be meaningful and attainable, based on modeling, on projected trends, and with consideration of scientific findings and current interventions. When such data or expertise were not available, the targets represent the greater measure of either a 10% improvement from baseline or minimally statistically significant improvement or for objectives with a baseline >90%, targets represented a 2 percentage point increase.17 In 2017, the HP2020 Midcourse Review reported progress from baseline for the 36 measurable HDS objectives13 (one additional objective, HDS-22, was moved to measurable status after the Midcourse Review). Updated results based on the most recent data showed that 14 measurable objectives met or exceeded their 2020 targets, 7 objectives were improving or change from baseline was moving in the direction of the target, 11 objectives had little or no detectable change, 3 objectives were getting worse or change from baseline was away from the target, and progress could not be assessed for 2 objectives (Figure 1).
Figure 1. Status of target attainment for 37 measurable objectives for the Heart Disease and Stroke section of Healthy People 2020, as of January 2019.
Target met or exceeded: The most recent value was equal to or exceeded the target. Improving: Movement was toward the target and statistically significant. Little or no change: Movement toward the target or away from the baseline was not statistically significant. Getting worse: Movement was away from the baseline and target and statistically significant. Measurable: Objective has a national baseline value. Developmental: Objective does not have baseline data. Baseline only: Objective has one data point only so progress cannot be assessed. Informational: Objective does not have a target so progress cannot be assessed. Percent of targeted change achieved = 100 × (most recent value – baseline value) / (HP2020 target – baseline value); percent in deficit = 100 × ∣most recent value – baseline value∣ / (baseline value). This figure was originally published as part of the Healthy People 2020 Midcourse Review (https://www.cdc.gov/nchs/healthy_people/hp2020/hp2020_midcourse_review.htm)13 and has been adapted for this paper.
Prevention
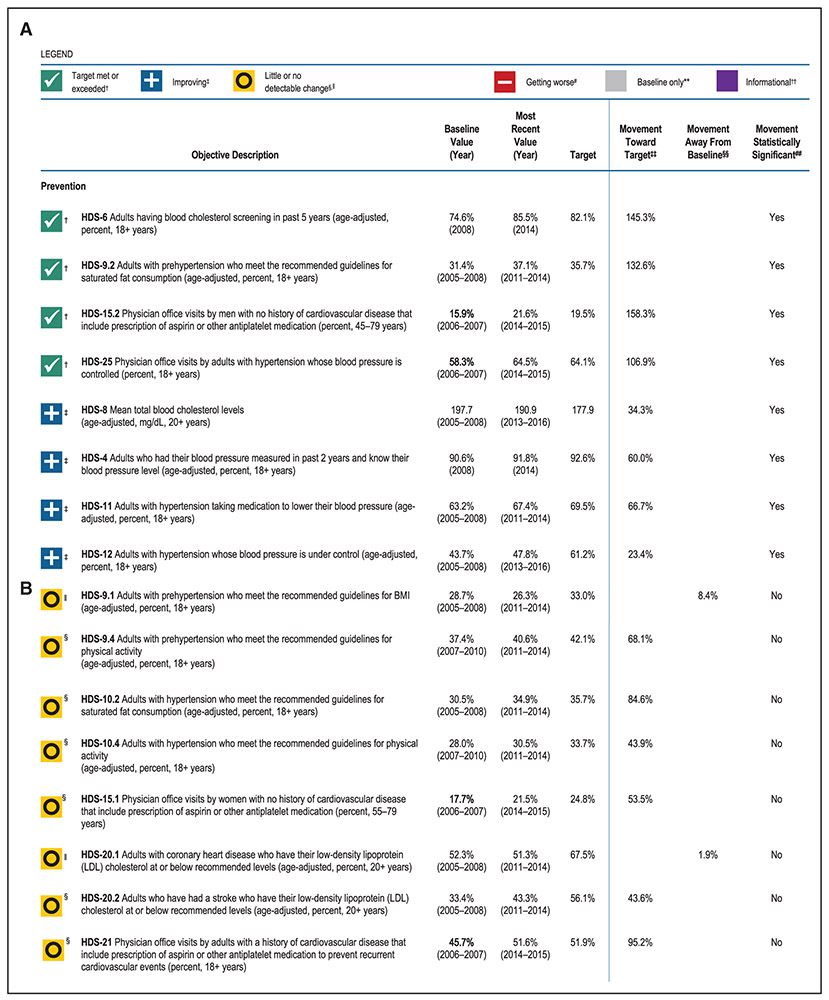
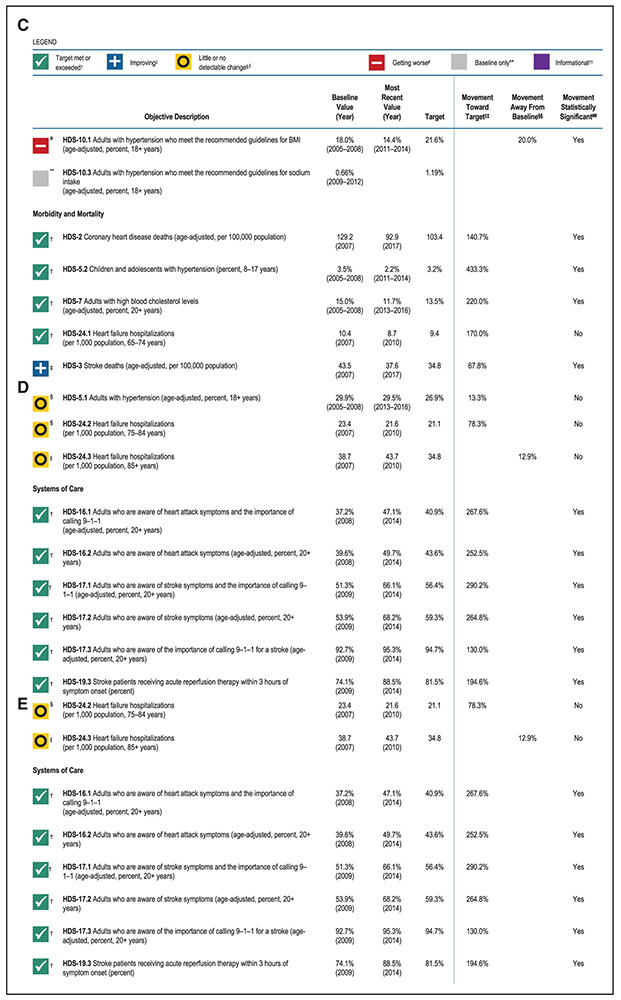
In the area of prevention, the objectives that met their targets were the proportion of adults who had their blood cholesterol screened in the past 5 years (HDS-6), proportion of adults with prehypertension who met guidelines for saturated fat consumption (HDS-9.2), and physician office visits by adults with hypertension whose blood pressure is controlled (HDS-25) or that include prescription of aspirin or other antiplatelet medication among men aged 45-79 years with no history of CVD for primary prevention (HDS-15.2; Figure 2). Improvements toward the target were observed for mean total blood cholesterol (HDS-8), and hypertension awareness (HDS-4), treatment (HDS-11), and control (HDS-12). The proportion of adults aged 18 years and over with hypertension who met the recommended guidelines for body mass index (HDS-10.1) was getting worse. There was little or no detectable change in the proportion of adults with prehypertension who met the recommended guidelines for body mass index (HDS-9.1) or physical activity (HDS-9.4), adults with hypertension who met the recommended guidelines for saturated fat consumption (HDS-10.2) or physical activity (HDS-10.4), and adults with coronary heart disease (HDS-20.1) or who had a stroke (HDS-20.2) who had their low-density lipoprotein cholesterol at or below recommended levels. There was also little or no detectable change in the proportion of physician office visits that included prescription of aspirin or other antiplatelet medication among women aged 55 to 79 years with no history of CVD for primary prevention (HDS-15.1) or among adults with a history of CVD for secondary prevention of recurrent events (HDS-21).
Figure 2. Most recent progress for Healthy People 2020 measurable* Heart Disease and Stroke Objectives, January 2019.
The figure shows progress based on most recent available data for measurable Healthy People 2020 Heart Disease and Stroke Objectives. See HealthyPeople.gov11 for all Healthy People 2020 data, and the Healthy People Statistical Note17 provides more information on the measures of progress. Objectives categorized as Prevention are shown in panels A–C, Morbidity and Mortality in panels C and D, and Systems of Care in panels D and E. This figure was originally published as part of the Healthy People 2020 Midcourse Review (https://www.cdc.gov/nchs/healthy_people/hp2020/hp2020_midcourse_review.htm)13 and has been adapted for this paper. The objectives have been reorganized and updated with the most recently available data and thus will be different from the data presented in the Midcourse Review. Baseline values have been updated for 4 objectives (HDS-15.2, HDS-25, HDS-15.1, and HDS-21), and 1 baseline value is new (HDS-22) since the Midcourse Review publication; these revised baseline values are depicted in bold. *Measurable objectives had a national baseline value. †Target met or exceeded: The most recent value was equal to or exceeded the target. (The percentage of targeted change achieved was equal to or greater than 100%.) ‡Improving: Movement was toward the target, and the percentage of targeted change achieved was statistically significant. Little or no detectable change: §Movement was toward the target, but the percentage of targeted change achieved was not statistically significant. ∥Movement was away from the baseline and target, but the percentage change relative to the baseline was not statistically significant. #Getting worse: Movement was away from the baseline and target, and the percentage change relative to the baseline was statistically significant. **Baseline only: The objective only had 1 data point, so progress toward target attainment could not be assessed. ††Informational: A target was not set for this objective, so progress toward target attainment could not be assessed. ‡‡For objectives that moved toward their targets, movement toward the target was measured as the percentage of targeted change achieved: §§For objectives that moved away from their baselines and targets, movement away from the baseline was measured as the magnitude of the percentage change from baseline: ##Statistical significance was tested when the objective had a target and at least 2 data points, and a normal distribution could be assumed. Statistical significance of the percentage of targeted change achieved or the magnitude of the percentage change from baseline was assessed at the 0.05 level using a normal 1-sided test. BMI indicates body mass index; and HDS, Heart Disease and Stroke.
Morbidity and Mortality
Over the HP2020 tracking period, targets were met for coronary heart disease deaths (HDS-2), the proportion of children and adolescents with hypertension (HDS-5.2), the proportion of adults with high blood cholesterol levels (HDS-7), and the rate of heart failure hospitalizations among persons aged 65 to 74 years (HDS-24.1). Improvement toward the target has been made for stroke deaths (HDS-3). Little or no detectable change was observed in adult hypertension prevalence (HDS-5.1) and heart failure hospitalizations among persons aged 75 to 84 years (HDS-24.2) and 85 years and over (HDS-24.3; Figure 2).
Systems of Care
In the area of systems of care, the objectives that met their targets were the composite and individual objectives related to awareness and emergency response for a heart attack (HDS-16.1, HDS-16.2) and stroke (HDS-17.1, HDS-17.2, HDS-17.3). Improvements toward the target were observed for emergency response for a heart attack (HDS-16.3). There was improvement toward the target in the proportion of stroke patients receiving acute reperfusion therapy within 3 hours of symptom onset (HDS-19.3) and in the proportion of heart attack patients receiving percutaneous intervention within 90 minutes of hospital arrival (HDS-19.2). Measures that have gotten worse since baseline include the proportion of heart attack patients receiving fibrinolytic therapy within 30 minutes of hospital arrival (HDS-19.1) and the proportion of heart attack survivors referred to a cardiac rehabilitation program (HDS-22). The proportion of adult stroke survivors who are referred for rehabilitation services (HDS-23) exceeded 95% at baseline, making it difficult to measure progress, but the workgroup continued to track it during HP2020 solely for informational purposes.
Geographic and Racial/Ethnic Disparities
In the US, there are well-established differences in CVD outcomes between communities of color and whites, and the US Department of Health and Human Services places high priority on improving cardiovascular health for diverse populations. In HP2020, health disparities data are available for 37 population-based measurable HDS objectives, and although there has been notable progress in recent years, persistent CVD disparities by sex, race and ethnicity, educational attainment, family income, disability status, and geographic location are evident in the data discussed in this paper. Hispanics or Latinos have the least favorable rate for 13 of the 32 HDS objectives with data for this group (HDS-5.2, HDS-8, HDS-9.1, HDS-9.4, HDS-10.1, HDS-10.4, HDS-15.2, HDS-16.1, HDS-16.2, HDS-17.1, HDS-17.2, HDS-17.2, HDS-22), and non-Hispanic blacks have the least favorable rate for 11 of the 35 objectives with data for this group (HDS-2, HDS-3, HDS-5.1, HDS-15.1, HDS-19.1, HDS-19.2, HDS-21, HDS-24.1, HDS-24.2, HDS-24.3, HDS-25), compared with non-Hispanic whites, who have the least favorable rate for 5 of the 37 objectives with data for this group (HDS-7, HDS-9.2, HDS-10.2, HDS-10.3, HDS-20.2). Some of these data are discussed further below, and a web-based Health Disparities Data Tool (https://www.healthypeople.gov/2020/data-search/health-disparities-data)18 is available for further exploration of health disparities within HP2020 objectives.
Health Data Collection Systems Used for HP2020 HDS Objectives
HP2020 HDS Objectives rely on established surveillance systems including the National Vital Statistics System–Mortality (NVSS–M), National Health and Nutrition Examination Survey (NHANES), National Health Interview Survey (NHIS), National Hospital Discharge Survey (NHDS), and National Ambulatory Medical Care Survey (NAMCS). These data sources are nationally representative, use standardized questionnaires and methods, and are collected on a routine basis, allowing for continuity of measures. NHANES uses laboratory data to confirm or evaluate many common conditions, including those reported here such as hypertension and blood cholesterol levels. Some of the limitations include lack of accuracy in race/ethnicity identification and exact primary cause of death (NVSS–M), self-reported history of disease diagnosis (NHANES, NHIS), and occurrences or episodes (rather than persons) counted (NHDS, NAMCS). Five objectives are tracked with data from national registries such as the American Heart Association (AHA)’s Get With The Guidelines (GWTG) stroke module (GWTG-Stroke) and AHA and American College of Cardiology’s Action-GWTG registry of coronary artery disease. Although these registries collect data nationwide, the data are not nationally representative by design.
DISCUSSION
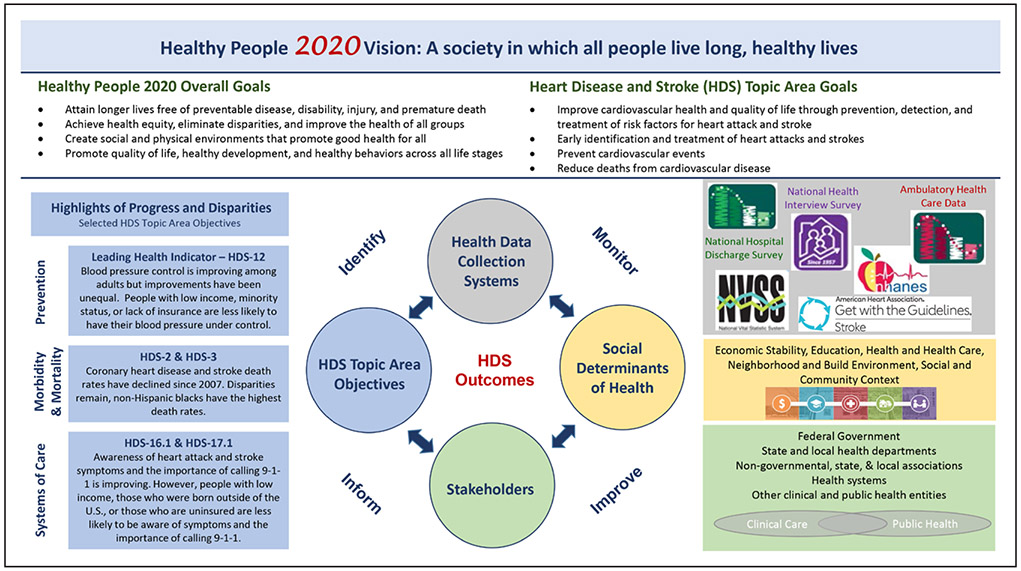
The vision of HP 2020 is of a society in which all people live long, healthy lives. The overall goal and HDS Topic Area goals support this vision through identification of priority areas and specific objectives. The objectives described above illustrate several areas of progress and also highlight room for improvement in improving HDS outcomes and the cardiovascular health of the nation. Progress toward or movement away from each objective target is monitored throughout the decade using various health data collection systems described above. Stakeholders can use the regular updates provided through this national platform to implement changes and influence improvement. In addition, understanding where the disparities are occurring allows stakeholders to consider social determinants of health that may be slowing or blocking progress for specific subpopulations. By identifying, monitoring, and informing clinical and public health practice, we can continue to work toward achieving cardiovascular health for the nation (Figure 3). The progress, challenges, and key themes of these results as well as implications for clinical and public health practice of key stakeholders and social determinants of health are discussed further here.
Figure 3. Model depicting the interconnection of the Healthy People 2020 Vision and Goals and improvement in Heart Disease and Stroke (HDS) outcomes through key components which identify, monitor, and inform Heart Disease and Stroke topic area objectives.
The figure depicts the interconnection of the Healthy People 2020 vision and goals, the HDS topic area goals, and changes in HDS outcomes through key components that identify, monitor, and inform HDS topic area objectives. The HDS topic area objectives were categorized into 3 areas: prevention, morbidity and mortality, and systems of care. Highlights of progress and disparities in each of these areas are described in the blue boxes with the objective number indicated. Objective HDS-12 proposed to increase the proportion of adults with hypertension whose blood pressure is under control. HDS-2 and HDS-3 proposed to reduce coronary heart disease deaths and stroke deaths. HDS-16.1 and 17.1 proposed to increase the proportion of adults aged ≥20 years who are aware of the early warning symptoms and signs of a heart attack and the importance of accessing rapid emergency care by calling 9–1–1 or another emergency number. Examples of Health Data Collection Systems used by the HDS topic are shown in the gray box, 5 social determinants of health recognized by the Healthy People initiative are shown in the yellow box, and stakeholders which work independently and collaboratively, and who span the clinical care and public health arenas, are listed in the green box. For more information, please visit: https://www.healthypeople.gov/ and https://www.cdc.gov/nchs/healthy_people/hp2020/hp2020_midcourse_review.htm. NHANES indicates National Health and Nutrition Examination Survey; and NVSS, National Vital Statistics System.
Progress and Challenges for Risk Factor Prevention and Management
Factors such as poor diet,19 physical inactivity,20 high blood pressure,21 high cholesterol,22 and the presence of overweight and obesity23 are all independently associated with greater risk for developing CVD. In HP2020, positive gains have been seen in screening, prevalence, and management for some of these risk factors as described in the preceding section (eg, cholesterol screening and management: HDS-6, HDS-8; risk factor management and awareness in adults with hypertension: HDS-4, HDS-11, HDS-25, HDS-12). Room for improvement remains, however, particularly with regard to meeting recommended guidelines for lifestyle factors, preventive medications (eg, aspirin for primary prevention in women, HDS-15.1, and for secondary prevention, HDS-21), and cholesterol control in the context of secondary prevention (HDS-20.2, HDS-20.2).
One challenge faced in the Healthy People initiative is ensuring the objectives and targets keep up with changing clinical guidelines. The aspirin objectives tracked during this decade are based on the US Preventive Services Task Force recommendations in place at that time, which gave Grade A recommendations for aspirin use for primary prevention in men aged 45 to 79 years and women aged 55 to 79 years.24 The recommendations acknowledged the need to consider both age and 10-year CVD risk when weighing benefits of CVD event prevention and increased risk of bleeding. The HDS workgroup is aware that the US Preventive Services Task Force updated these recommendations in 201625 and will take those into account when planning for HP2030.
The HP2020 HDS topic area also includes an objective (HDS-1) to track overall cardiovascular health among US adults. This objective remains developmental because of challenges synthesizing data metrics on separate behaviors and outcomes into a single summary measure, but its inclusion reflects support for the concept of overall cardiovascular health, which is not only absence of CVD risk factors but attainment of optimal levels for the major cardiovascular health indicators.26 This objective is aligned with the AHA’s Life’s Simple 7 program that identifies 7 cardiovascular health metrics that can lead to overall improved health.27-29 Despite differing measurement definitions of cardiovascular health, available data have demonstrated that few children and adolescents and even fewer adults meet current recommendations for individual cardiovascular health metrics.7
CVD risk factors are influenced by determinants of health such as individual behaviors, neighborhood availability of healthy foods and safe opportunities for physical activity, and access to high-quality health care, and are often more prevalent in racial/ethnic minority groups who experience greater social and economic barriers to healthy environments and receiving the best overall care. Effective prevention is complex and requires engagement across myriad sectors to impact both the health determinants and outcomes. Preserving a population that ages free from significant risk factors for CVD can significantly reduce risk of developing CVD in later life.30 However, maintaining an ideal state of cardiovascular health remains aspirational for most,7 and appropriate management of existing disease becomes the focal point.
A Focus on Hypertension
In recognition of the significant burden of hypertension and its causal role in both heart disease and stroke, 16 of the HP2020 HDS objectives focus on persons with prehypertension or hypertension, addressing factors such blood pressure screening and awareness, treatment and control, or related risk factors. Improving hypertension control was included as an Leading Health Indicator because of its importance in reducing CVD events and the significant opportunities for improvement. According to the standards currently used in HP2020, about 1 in 3 adults has hypertension, and among these 67.4% were taking medication to lower their blood pressure, and only 47.8% have their blood pressure under control (Figure 2).11
Tracking HDS objectives demonstrated that progress has been made over the last decade31; for example, we have seen improvement in hypertension control (HDS-12, 2006–2007: 58.3%; 2014–2015: 64.5%) but little change in the burden of hypertension has been realized among adults (HDS-5.1, 2005–2008: 29.9%; 2013–2016: 29.5%). Disparities in hypertension prevalence and control were evidenced by population groups that had the highest prevalence of hypertension (HDS-5.1) in 2013 to 2016, including non-Hispanic black adults, adults aged ≥25 years with a high school education, adults with family incomes below the poverty threshold, adults aged ≥20 years with activity limitations, and adults with public health insurance aged <65 years. During this period, population groups with the lowest rates of hypertension control among adults with hypertension (HDS-12) included men, Asian non-Hispanic adults, adults with family incomes <200% of the poverty threshold, adults aged ≥20 years without activity limitations, and uninsured adults aged <65 years.
Because definitions for these objectives were established in 2010, hypertension was defined as blood pressure <140/90 mm Hg following the national guideline recommendations in use at that time.32 However, new guidelines that address the prevention, detection, evaluation, and management of high blood pressure were released by the American College of Cardiology, AHA, and other organizations in 2017.33 The new guideline updated blood pressure classifications and lowered the threshold for hypertension (defining stage 1 as 130-139 mm Hg systolic/80-89 mm Hg diastolic and stage 2 as ≥140/90 mm Hg), resulting in an increase in the prevalence of hypertension to nearly 1 in 2 adults, with only a quarter of adults having controlled hypertension.33,34 To achieve greater improvements, growing evidence supports a multilevel approach to blood pressure control that involves patients and families, community organizations, and healthcare professionals and delivery systems.23 Additional pharmacological treatment and services will be needed to address the lifestyle modification recommendations in the 2017 guidelines.34
Federal Agency Programs Addressing Risk Factor Management
Numerous federally funded programs and research initiatives are being implemented that address CVD risk factors and outcomes that may facilitate progress toward meeting these HDS targets. The Million Hearts initiative aims to prevent a million heart attacks and strokes over a 5-year period,35 by improving awareness, treatment, and control of blood pressure and cholesterol, and by reducing sodium intake. The initiative promotes the alignment and coordination of activities in public health and healthcare systems to emphasize high-burden population-level risk factors, through optimized care, preservation of health through population-level interventions (eg, sodium reduction), and focusing on high-risk populations. Resources are available to diverse stakeholders interested in improving hypertension control within their settings, and high-functioning health systems with exceptional gains in hypertension control have been recognized as Million Hearts Hypertension Control Champions. Many of the activities promoted through the Million Hearts initiative are realized through programmatic funding of the Centers for Disease Control and Prevention (CDC) to all 50 states and numerous communities. These programs aim to promote the implementation of evidenced-based interventions and activities in communities and health systems—with the improvement of hypertension control retaining a prominent position.
Federally-funded, community-based programs are also developing, testing, and delivering proven risk factor control strategies within different clinical and community settings and diverse populations. CDC’s Sodium Reduction in Communities Program currently funds 8 communities across the country to implement strategies to reduce sodium intake to no more than the recommended maximum amount as defined in the Dietary Guidelines for Americans. Strategies targeted at specific subpopulations are also important because our results show that improvements in HDS objectives have not been equally realized among all people. For example, blood pressure control (HDS-12) has improved for the population as a whole, but improvement was not seen equally among all subpopulations; individuals with low income, minority status, or a lack of insurance were less likely to have their blood pressure under control. One example of a successful community-based approach to blood pressure control supported by the National Institutes of Health (NIH) is a randomized clinical trial that showed a 21.6–mm Hg greater reduction in blood pressure among black male patrons of barbershops where patrons met with pharmacists to receive prescription drug therapy compared to the control group (P<0.001).36 The National Institute of Neurological Disorders and Stroke (NINDS)–sponsored Stroke Prevention/Intervention Research Program, funded from 2012 to 2017, formed partnerships with community organizations, local health departments, and healthcare providers to target multiple points of intervention for blood pressure control, including primary care settings, lifestyle and behavior factors, home health care, community health workers, and mobile health technology, with a specific emphasis on addressing health disparities among racial/ethnic minority populations. The CDC’s WISEWOMAN program (Well-Integrated Screening and Evaluation for Women Across the Nation) provides low-income, uninsured, and underinsured women aged 40 to 64 years services to promote lasting heart-healthy lifestyles, such as heart disease and stroke risk factor screenings and support for healthy behaviors. Twenty-one WISEWOMAN programs are currently in 19 states and 2 tribal organizations. NINDS and the National Heart Lung and Blood Institute are also partnering with the Patient-Centered Outcomes Research Institute to test hypertension control strategies at the community and health system levels within racial and ethnic minority communities.
Stakeholders work to inform and improve cardiovascular health through research as well. NIH-supported clinical trials such as the SPRINT trial (Systolic Blood Pressure Intervention Trial) have demonstrated that lower blood pressure treatment targets could more effectively prevent cardiovascular events when compared to standard treatment targets,37 providing evidence to support positive benefits of clinical hypertension control practices that target lower thresholds. NIH also provides grant funding for numerous large-scale studies and targeted programs to understand and address CVD, stroke, and associated risk factors in diverse settings and population groups. For example, the Framingham Heart Study (FHS) cohorts, the Reasons for Geographic and Racial Differences in Stroke study (REGARDS), the Multi-Ethnic Study of Atherosclerosis (MESA), the Jackson Heart Study, the Strong Heart Study (SHS), the Northern Manhattan Stroke Study (NOMAS), and the Hispanic Community Health Study/Study of Latinos program (HCHS/SOL) are all large epidemiological cohort studies that have actively recruited racial and/or ethnic minority populations in various locations in order to study risk, burden, and CVD-related outcomes and differences in these by race/ethnicity and geographic region. Recently, the NIH established the Centers for Population Health and Health Disparities, which is cosponsored by the Office of Behavioral and Social Science Research, the National Cancer Institute, and the National Heart Lung and Blood Institute to gain a deeper understanding of the effects of community and societal influences on overall health and well-being in diverse and underserved populations. These centers are taking multifaceted approaches to understand various health disparities, including CVD and associated risk factors.38
Educational and media campaigns are another method by which federal agencies work to improve HDS outcomes through efforts to raise awareness about heart disease and encourage people to live active lifestyles. For example, The Heart Truth program, funded by National Heart Lung and Blood Institute, educates women about heart disease and the leading risk factors. The Heart Truth Champions Program trains community health workers on messaging, tools, and strategies to educate others about heart-healthy living with an emphasis on vulnerable populations. From 2007 to 2015, the Champions Program trained 678 Heart Truth Champions, and conducted >790 community events, reaching >633 000 people. Each year The Heart Truth partners with the AHA to sponsor and provide scientific oversight for the Red Dress Collection Fashion Show in New York City. Finally, the Mind Your Risks campaign sponsored by NINDS aims to raise awareness of the importance of preventing or controlling hypertension to promote brain health later in life. These campaigns among others produce materials and tools that promote health behavior change and improve health literacy.
Progress, Programs, and Opportunities to Improve Clinical Outcomes
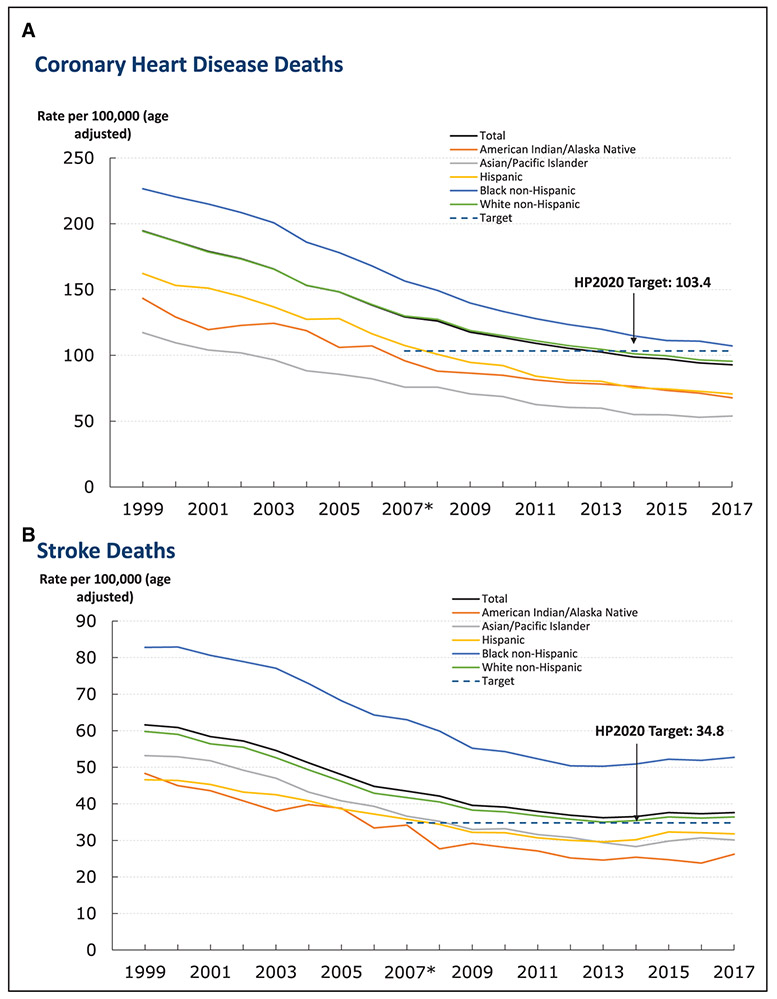
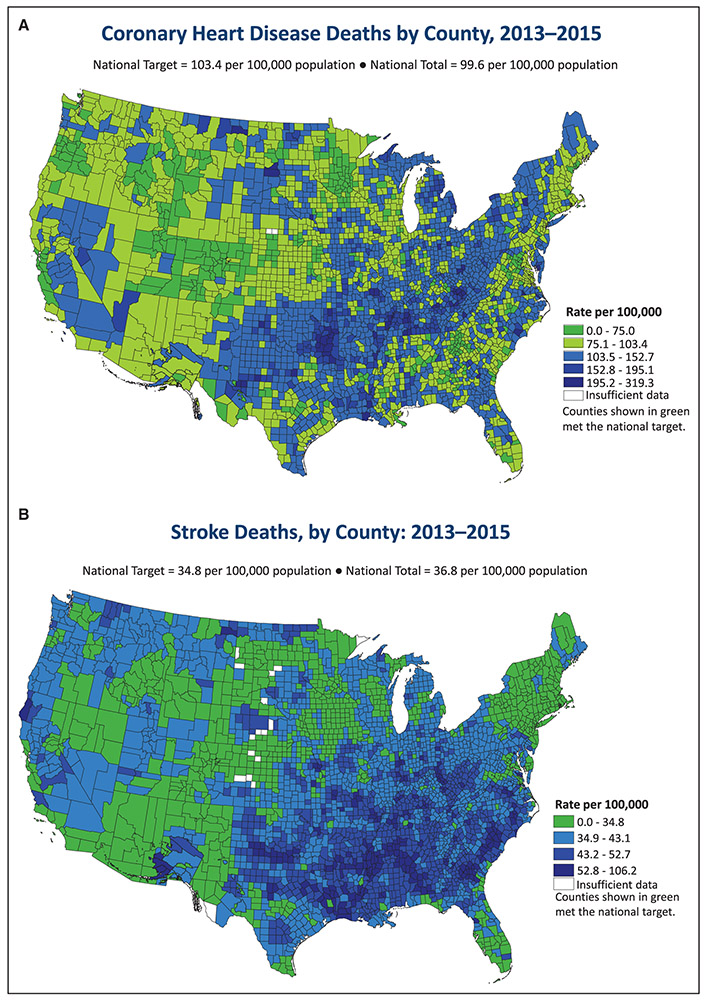
Important among HDS outcomes, the significant decline in CVD mortality has been identified as one of the great public health achievements of the past century.39,40 These gains have been attributed to significant improvements in prevention and treatment of CVD and related risk factors.3,41 In HP2020, mortality declines were observed between 2007 and 2017, but the burden remains disproportionate (Figure 4). Population groups in selected demographic categories with the highest age-adjusted coronary heart disease (HDS-2) and stroke (HDS-3) death rates include men, the non-Hispanic black population, and those living in nonmetropolitan areas. Rates of CHD and stroke deaths were highest among non-Hispanic Black adults. CHD deaths were lowest among Asian/Pacific Islanders, and stroke deaths were lowest among American Indian/Alaska Native adults. County level maps42 also illustrate the higher mortality burden from CHD (Figure 5A) and stroke (Figure 5B) concentrated in the Appalachian and southeastern regions of the US. As reported here and in other recent reports using national data, progress has stalled for certain CVD outcomes.4,5 To continue previous gains in CVD mortality, advances across the risk factor prevention continuum are needed along with appropriate management of disease burden. For example, among those with heart failure, hospitalizations are an indicator of control and system performance, and lowering heart failure hospitalizations is a priority (HDS-24).7 Improvements in these areas may reflect improved individual care, broad prevention efforts, or system improvements resulting in appropriate and timely care.43 Early intervention to preserve cardiovascular health is needed to continue the great progress of lower CVD mortality realized in the past decades.
Figure 4. Mortality trends for coronary heart disease and stroke.
The figure shows trends for deaths from coronary heart disease (A) and stroke (B) by race / ethnicity. *Healthy People 2020 (HP2020) baseline (2007). Data are for the International Classification of Diseases, Tenth Revision, codes I20–I25 (A) or I60–I69 (B) reported as the underlying cause of death (Healthy People objectives HDS-2 and HDS-3, respectively). Rates are age-adjusted to the 2000 standard population. Before 2003, only 1 race category could be recorded; recording ≥1 race was not an option. Beginning in 2003, multiple-race data were reported by some states; multiple-race data were bridged to the single-race categories for comparability. Source: National Vital Statistics System–Mortality, Centers for Disease Control and Prevention (CDC)/National Center for Health Statistics (NCHS); Bridged-Race Population Estimates, CDC/NCHS and Census. This figure has been adapted from documents prepared for the Healthy People 2020 Progress Review and updated with the most recently available data. The original figures can be found on slides 27 and 28 in the presentation at this link: https://www.cdc.gov/nchs/healthy_people/hp2020/hp2020_aocbc_and_hds_progress_review.htm. HDS, Heart Disease and Stroke.
Figure 5. County-level mortality maps of coronary Heart Disease and Stroke (HDS)The figure shows deaths from coronary heart disease (A) and stroke (B) by county.
Data are for International Classification of Diseases, Tenth Revision, codes I20–I25 (A) or I60–I69 (B) reported as the underlying cause of death Healthy People 2020 [HP2020] objectives HDS-2 and HDS-3, respectively). Rates are age-adjusted to the 2000 standard population. Rates are spatially smoothed to enhance the stability of rates in counties with small populations. Data are displayed by a modified Jenks classification for US counties, which creates categories that minimize within-group variation and maximize between-group variation. Sources: National Vital Statistics System–Mortality, Centers for Disease Control and Prevention (CDC)/National Center for Health Statistics (NCHS); Bridged-Race Population Estimates, CDC/NCHS and Census. Interactive Atlas of Heart Disease and Stroke, CDC/National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP) https://nccd.cdc.gov/DHDSPAtlas/.
Use of emergency medical services to get to a hospital as quickly as possible to receive treatment is an important goal to improve outcomes following a CVD event. Substantial progress was observed among HDS objectives measuring symptom awareness and the need to call emergency services for stroke and heart attack (HDS-16.1–HDS 17.3). Attention to disparities will also be important for continued progress in this area because our data demonstrated that persons with low income, those who were born outside of the United States, and those who are uninsured are less likely to be aware of symptoms and the importance of calling 9-1-1. HDS objectives also measure time from symptom onset to reperfusion therapy for strokes and heart attacks. Timely treatment of eligible patients with percutaneous intervention (PCI) for heart attack (HDS 19.2) and tissue plasminogen activator for stroke (HDS-19.3) both showed improvement over the decade, with reductions in the use of fibrinolytic therapy for heart attack (HDS-19.1). PCI is preferred to fibrinolytic therapy when time-to-treatment delays are short and the patient presents to a PCI-capable hospital. The drop in use of fibrinolytic therapy may reflect improved coordination between EMS and hospitals, increasing the number of patients transported to primary PCI-capable hospitals, as well as increasing hospital capacity to deliver PCI.44,45 Initial fibrinolytic therapy is suited for patients with low bleeding risk, who present to a non-PCI capable hospital and who will have a longer delay to PCI, such as in a rural setting. Prehospital administration of fibrinolytic therapy in settings where there may be a delay to care, such as in rural areas, may be beneficial but is not used currently because of a lack of necessary resources or training.44
Federal agencies have supported programs to improve best practices and delivery of timely, evidence-based care. When tissue plasminogen activator was approved for acute ischemic stroke treatment within 3 hours of symptom onset, NINDS launched an extensive public messaging campaign called Know Stroke to increase knowledge of the signs and symptoms of stroke and the importance of dialing 9-1-1. NINDS-funded research has also studied behavioral and system barriers that contribute to underutilization of tissue plasminogen activator in black communities, to facilitate targeted solutions to ensure equity in access to effective stroke treatment.46,47 In addition, NINDS established the Brain Attack Coalition to bring together professionals from the medical, advocacy, government, and scientific communities to discuss best practices and facilitate adoption of evidence-based stroke prevention and treatment strategies. Early accomplishments of this group include advancing stroke systems of care that minimize a stroke patient’s time to treatment with tissue plasminogen activator.48 Recent scientific advances proving benefit of endovascular therapy for acute ischemic stroke, and the ability treat patients in an extended time window based on neuroimaging selection,49,50 bring new opportunities for optimizing systems of care to ensure appropriate, timely, and high-quality delivery of evidence-based care for stroke patients.51
Other federally funded programs that contribute to improvement of care systems include the NIH StrokeNet, which serves as a national clinical trials infrastructure dedicated to stroke clinical research across prevention, treatment, and recovery domains. The network supports efficient and high-quality stroke trials to facilitate translation of the most promising scientific advances into patient benefit.52 In addition, improvement in the quality of stroke care provided is a central component of the CDC-supported Paul Coverdell National Acute Stroke Program. The program aims to improve the quality of stroke care across the continuum of care—from prehospitalization to hospitalization to posthospitalization. Interventions to improve stroke care across the continuum have been informed by this program and are available for review and replication.5
The research and programs mentioned above are not a comprehensive list of all current or past federally funded work that contributes to the improvement of CVD morbidity and mortality across the United States. Key to each program are the efforts of state and local, tribal, and nongovernmental partners who use the funding and the frameworks to develop and tailor programs to populations within their specific health catchment areas. These partners and their efforts are laudable and have positively impacted the communities in which they work. Continued collaboration across sectors and with a wide variety of partners is vital to the realization of improved cardiovascular health for the nation. Although important research and programs from federal agencies such as the Health Resources and Services Administration, Centers for Medicare and Medicaid Services, or Agency for Healthcare Research and Quality contribute to the cardiovascular health of the nation, we have only highlighted those supported by the HP2020 HDS Federal Agency Co-Leads, the CDC and the NIH.
CONCLUDING REMARKS AND FUTURE PERSPECTIVES
In this paper, we provide background about the Healthy People initiative and an overview of the current HP2020 HDS objectives, summarize progress according to recent data, and highlight examples of relevant federal agency research and programs that facilitate improvement toward the health targets. The objective of this paper is to raise awareness among the research and professional communities of the potential for HP2020 as a tool to galvanize local efforts toward improved population health, and the commitment of federal partners in facilitating this work. With planning for Healthy People 2030 well underway, stakeholders can embrace collaborative opportunities to leverage existing progress and emphasize areas for improvement to maximize the positive impact of the Healthy People initiative on population-level health.
HP2020 HDS data illustrate the substantial progress made in many of the measured objectives for CVD in the US, while also pointing to remaining challenges for some objectives with less notable progress and identifying disparities that exist even among the objectives where progress has been noted. In the future, innovative data collection approaches (eg, electronic health record or social media data) may enable tracking of progress for additional objectives at national and subnational levels (state, county, metropolitan area and city). Continuing to leverage the collaborative structure of the Healthy People initiative will help maximize the ability of stakeholders to serve the needs of local communities and catalyze cardiovascular health improvements across the nation. Working from a shared health roadmap enables federal, state, local, tribal, and nongovernmental partners to effectively collaborate and achieve common goals. As the initiative transitions to HP2030, further alignment of HDS objectives with strategic goals for cardiovascular diseases put forward by professional societies such as the AHA will help synchronize messages to the public and local organizations regarding priorities and best practices, and will serve to unite public health stakeholders in their work to improve cardiovascular health for all Americans.
Supplementary Material
Acknowledgments
We are grateful for input from subject matter experts from each of the agencies, both on this paper as well as contributions to the work related to the Heart Disease and Topic Area during HP2020. In particular, we acknowledge the work of Kimberly Hurvitz, National Center for Health Statistics, Centers for Disease Control and Prevention, Hyattsville, MD, for her contribution to the workgroup, the data integrity, and tracking progress of the objectives. We also extend special thanks to Joylene John-Sowah and recognize her contributions as a co-lead on the workgroup during her former tenure at the National Heart Lung and Blood Institute, including her involvement in developing the concept for this manuscript. The views expressed in this article are those of the authors and do not necessarily represent the official position of the NIH, the CDC, the US Department of Health and Human Services, or the United States Government.
Footnotes
The online-only Data Supplement is available with this article at https://www.ahajournals.org/doi/suppl/10.1161/circulationaha.118.035408.
Disclosures
None.
Contributor Information
Katherine Pahigiannis, National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda, MD.
Angela M. Thompson-Paul, Division for Heart Disease and Stroke Prevention, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, GA.
Whitney Barfield, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD.
Emmeline Ochiai, Office of Disease Prevention and Health Promotion, Office of the Assistant Secretary for Health, US Department of Health and Human Services, Rockville, MD.
Fleetwood Loustalot, Division for Heart Disease and Stroke Prevention, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, GA.
Susan Shero, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD.
Yuling Hong, Division for Heart Disease and Stroke Prevention, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, GA.
REFERENCES
- 1.U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Health, United States, 2017: With special feature on mortality. 2018. https://www.cdc.gov/nchs/data/hus/hus17.pdf.Accessed March 28, 2019.
- 2.Lackland DT, Roccella EJ, Deutsch AF, Fornage M, George MG, Howard G, Kissela BM, Kittner SJ, Lichtman JH, Lisabeth LD, Schwamm LH, Smith EE, Towfighi A; American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Quality of Care and Outcomes Research; Council on Functional Genomics and Translational Biology. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke. 2014;45:315–353. doi: 10.1161/01.str.0000437068.30550.cf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ford ES, Capewell S. Proportion of the decline in cardiovascular mortality disease due to prevention versus treatment: public health versus clinical care. Annu Rev Public Health. 2011;32:5–22. doi: 10.1146/annurev-publhealth-031210-101211 [DOI] [PubMed] [Google Scholar]
- 4.Sidney S, Quesenberry CP Jr, Jaffe MG, Sorel M, Nguyen-Huynh MN, Kushi LH, Go AS, Rana JS. Recent trends in cardiovascular mortality in the United States and public health goals. JAMA Cardiol. 2016;1:594–599. doi: 10.1001/jamacardio.2016.1326 [DOI] [PubMed] [Google Scholar]
- 5.Yang Q, Tong X, Schieb L, Vaughan A, Gillespie C, Wiltz JL, King SC, Odom E, Merritt R, Hong Y, George MG. Vital signs: recent trends in stroke death rates - United States, 2000-2015. MMWR Morb Mortal Wkly Rep. 2017;66:933–939. doi: 10.15585/mmwr.mm6635e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kochanek KD, Murphy SL, Zu JQ, Arias E. Mortality in the United States, 2013. NCHS Data Brief. 2015;229:1–8. https://www.cdc.gov/nchs/data/databriefs/db178.htm.Accessed March 28, 2019. [PubMed] [Google Scholar]
- 7.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O’Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–e492. doi: 10.1161/CIR.0000000000000558 [DOI] [PubMed] [Google Scholar]
- 8.Casper M, Kramer MR, Quick H, Schieb LJ, Vaughan AS, Greer S. Changes in the geographic patterns of heart disease mortality in the United States: 1973 to 2010. Circulation. 2016;133:1171–1180. doi: 10.1161/CIRCULATIONAHA.115.018663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roth GA, Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, Morozoff C, Naghavi M, Mokdad AH, Murray CJL. Trends and patterns of geographic variation in cardiovascular mortality among US counties, 1980-2014. JAMA. 2017;317:1976–1992. doi: 10.1001/jama.2017.4150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vaughan AS, Quick H, Pathak EB, Kramer MR, Casper M. Disparities in temporal and geographic patterns of declining heart disease mortality by race and sex in the United States, 1973–2010. J Am Heart Assoc. 2015; 4:e002567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion, Washington, D.C. HealthyPeople.gov. About Healthy People. https://www.healthypeople.gov/2020/About-Healthy-People.Accessed August 15, 2018.
- 12.U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion, Washington, D.C. HealthyPeople.gov. Healthy People 2020 Heart Disease and Stroke Topic Area. https://www.healthypeople.gov/2020/topics-objectives/topic/heart-disease-and-stroke.Accessed August 15, 2018.
- 13.National Center for Health Statistics. Chapter 21: Heart disease and stroke. Healthy People 2020 Midcourse Review. Hyattsville, MD: U.S. Department of Health and Human Services. 2016:21-1–21-26. https://www.cdc.gov/nchs/data/hpdata2020/HP2020MCR-C21-HDS.pdf.Accessed March 28, 2019. [Google Scholar]
- 14.U.S Department of Health, Education, and Welfare Public Health Service. Office of the Assistant Secretary for Health and Surgeon General. Healthy People: The Surgeon General’s Report on Health Promotion and Disease Prevention. Washington, DC: U.S. Department of Health, Education, and Welfare. 1979; Publication No. 79-55071:1–262. [Google Scholar]
- 15.Benz J, Blakey C, Oppenheimer CC, Scherer H, Robinson WT. The healthy people initiative: understanding the user’s perspective. J Public Health Manag Pract. 2013;19:103–109. doi: 10.1097/PHH.0b013e318254cc31 [DOI] [PubMed] [Google Scholar]
- 16.Heffernan M, Fromknecht CQ, McGowan AK, Blakey C, Oppenheimer CC. Healthy People for the 21st century: understanding use of Healthy People 2020 as a web-based initiative. J Public Health Manag Pract. 2018;25:1–7. [DOI] [PubMed] [Google Scholar]
- 17.Talih M, Huang DT. Measuring progress toward attainment and the elimination of health disparities in Healthy People 2020. Healthy People Stat Notes. 2016;27:1–19. [Google Scholar]
- 18.U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion, Washington, D.C. HealthyPeople.gov. Health Disparities Data. https://www.healthypeople.gov/2020/data-search/health-disparities-data.Accessed September 28, 2018.
- 19.Micha R, Shulkin ML, Peñalvo JL, Khatibzadeh S, Singh GM, Rao M, Fahimi S, Powles J, Mozaffarian D. Etiologic effects and optimal intakes of foods and nutrients for risk of cardiovascular diseases and diabetes: systematic reviews and meta-analyses from the Nutrition and Chronic Diseases Expert Group (NutriCoDE). PLoS One. 2017;12:e0175149. doi: 10.1371/journal.pone.0175149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shiroma EJ, Lee IM. Physical activity and cardiovascular health: lessons learned from epidemiological studies across age, gender, and race/ethnicity. Circulation. 2010;122:743–752. doi: 10.1161/CIRCULATIONAHA.109.914721 [DOI] [PubMed] [Google Scholar]
- 21.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002; 360:1903–13. [DOI] [PubMed] [Google Scholar]; Erratum in: Lancet. 2003; 361:1060. [Google Scholar]
- 22.Prospective Studies Collaboration, Lewington S, Whitlock G, Clarke R, Sherliker P, Emberson J, Halsey J, Qizilbash N, Peto R, Collins R. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet. 2007; 370:1829–39. [DOI] [PubMed] [Google Scholar]; Erratum in: Lancet. 2008; 372:292.18657707 [Google Scholar]
- 23.Prospective Studies Collaboration, Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009; 373:1083–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.U.S. Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: U.S. preventive services task force recommendation statement. Ann Intern Med. 2009;150:396–404. doi: 10.7326/0003-4819-150-6-200903170-00008 [DOI] [PubMed] [Google Scholar]
- 25.Bibbins-Domingo K; U.S. Preventive Services Task Force. Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2016;164:836–845. doi: 10.7326/M16-0577 [DOI] [PubMed] [Google Scholar]
- 26.Al Rifai M, Greenland P, Blaha MJ, Michos ED, Nasir K, Miedema MD, Yeboah J, Sandfort V, Frazier-Wood AC, Shea S, Lima JA, Szklo M, Post WS, Blumenthal RS, McEvoy JW. Factors of health in the protection against death and cardiovascular disease among adults with subclinical atherosclerosis. Am Heart J. 2018; 198:180–188. doi: 10.1016/j.ahj.2017.10.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guo L, Zhang S. Association between ideal cardiovascular health metrics and risk of cardiovascular events or mortality: a meta-analysis of prospective studies. Clin Cardiol. 2017;40:1339–1346. doi: 10.1002/clc.22836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD; American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- 29.Aneni EC, Crippa A, Osondu CU, Valero-Elizondo J, Younus A, Nasir K, Veledar E. Estimates of mortality benefit from ideal cardiovascular health metrics: a dose response meta-analysis. J Am Heart Assoc. 2017; 6:e006904. doi: 10.1161/JAHA.117.006904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, Greenland P, Van Horn L, Tracy RP, Lloyd-Jones DM. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366:321–329. doi: 10.1056/NEJMoa1012848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D. Hypertension prevalence and control among adults: United states, 2015–2016. NCHS Data Brief. 2017;289:1–8. [PubMed] [Google Scholar]
- 32.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560 [DOI] [PubMed] [Google Scholar]
- 33.Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115. doi: 10.1161/HYP.0000000000000065 [DOI] [PubMed] [Google Scholar]
- 34.Ritchey MD, Gillespie C, Wozniak G, Shay CM, Thompson-Paul AM, Loustalot F, Hong Y. Potential need for expanded pharmacologic treatment and lifestyle modification services under the 2017 ACC/AHA Hypertension Guideline. J Clin Hypertens (Greenwich). 2018;20:1377–1391. doi: 10.1111/jch.13364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Frieden TR, Berwick DM. The “Million Hearts” initiative–preventing heart attacks and strokes. N Engl J Med. 2011;365:e27. doi: 10.1056/NEJMp1110421 [DOI] [PubMed] [Google Scholar]
- 36.Victor RG, Lynch K, Li N, Blyler C, Muhammad E, Handler J, Brettler J, Rashid M, Hsu B, Foxx-Drew D, Moy N, Reid AE, Elashoff RM. A cluster-randomized trial of blood-pressure reduction in black barbershops. N Engl J Med. 2018;378:1291–1301. doi: 10.1056/NEJMoa1717250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, Lewis CE, Kimmel PL, Johnson KC, Goff DC Jr, Fine LJ, Cutler JA, Cushman WC, Cheung AK, Ambrosius WT; SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Krok-Schoen JL, Weier RC, Hohl SD, Thompson B, Paskett ED. Involving community health workers in the centers for population health and health disparities research projects: benefits and challenges. J Health Care Poor Underserved. 2016;27:1252–1266. doi: 10.2105/AJPH.2015.302980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention (CDC). Ten great public health achievements–United States, 1900–1999. MMWR Morb Mortal Wkly Rep. 1999; 48:241–243. [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention (CDC). Ten great public health achievements–United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011; 60:619–623. [PubMed] [Google Scholar]
- 41.Mensah GA, Wei GS, Sorlie PD, Fine LJ, Rosenberg Y, Kaufmann PG, Mussolino ME, Hsu LL, Addou E, Engelgau MM, Gordon D. Decline in cardiovascular mortality: possible causes and implications. Circ Res. 2017;120:366–380. doi: 10.1161/CIRCRESAHA.116.309115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention (CDC). Interactive atlas of heart disease and stroke. https://nccd.cdc.gov/DHDSPAtlas/.Accessed August 15, 2018.
- 43.Ziaeian B, Kominski GF, Ong MK, Mays VM, Brook RH, Fonarow GC. National differences in trends for heart failure hospitalizations by sex and race/ethnicity. Circ Cardiovasc Qual Outcomes. 2017; 10: e003552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.American College of Emergency Physicians, Society for Cardiovascular Angiography and Interventions, O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013; 61:e78–140. [DOI] [PubMed] [Google Scholar]
- 45.Jollis JG, Al-Khalidi HR, Roettig ML, Berger PB, Corbett CC, Doerfler SM, Fordyce CB, Henry TD, Hollowell L, Magdon-Ismail Z, Kochar A, McCarthy JJ, Monk L, O’Brien P, Rea TD, Shavadia J, Tamis-Holland J, Wilson BH, Ziada KM, Granger CB. Impact of regionalization of ST-segment-elevation myocardial infarction care on treatment times and outcomes for emergency medical services-transported patients presenting to hospitals with percutaneous coronary intervention: Mission: Lifeline Accelerator-2. Circulation. 2018;137:376–387. doi: 10.1161/CIRCULATIONAHA.117.032446 [DOI] [PubMed] [Google Scholar]
- 46.Boden-Albala B, Edwards DF, St Clair S, Wing JJ, Fernandez S, Gibbons MC, Hsia AW, Morgenstern LB, Kidwell CS. Methodology for a community-based stroke preparedness intervention: the Acute Stroke Program of Interventions Addressing Racial and Ethnic Disparities Study. Stroke. 2014;45:2047–2052. doi: 10.1161/STROKEAHA.113.003502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hsia AW, Castle A, Wing JJ, Edwards DF, Brown NC, Higgins TM, Wallace JL, Koslosky SS, Gibbons MC, Sánchez BN, Fokar A, Shara N, Morgenstern LB, Kidwell CS. Understanding reasons for delay in seeking acute stroke care in an underserved urban population. Stroke. 2011;42:1697–1701. doi: 10.1161/STROKEAHA.110.604736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Alberts MJ, Latchaw RE, Jagoda A, Wechsler LR, Crocco T, George MG, Connolly ES, Mancini B, Prudhomme S, Gress D, Jensen ME, Bass R, Ruff R, Foell K, Armonda RA, Emr M, Warren M, Baranski J, Walker MD; Brain Attack Coalition. Revised and updated recommendations for the establishment of primary stroke centers: a summary statement from the brain attack coalition. Stroke. 2011;42:2651–2665. doi: 10.1161/STROKEAHA.111.615336 [DOI] [PubMed] [Google Scholar]
- 49.Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, Yavagal DR, Ribo M, Cognard C, Hanel RA, Sila CA, Hassan AE, Millan M, Levy EI, Mitchell P, Chen M, English JD, Shah QA, Silver FL, Pereira VM, Mehta BP, Baxter BW, Abraham MG, Cardona P, Veznedaroglu E, Hellinger FR, Feng L, Kirmani JF, Lopes DK, Jankowitz BT, Frankel MR, Costalat V, Vora NA, Yoo AJ, Malik AM, Furlan AJ, Rubiera M, Aghaebrahim A, Olivot JM, Tekle WG, Shields R, Graves T, Lewis RJ, Smith WS, Liebeskind DS, Saver JL, Jovin TG; DAWN Trial Investigators. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378:11–21. doi: 10.1056/NEJMoa1706442 [DOI] [PubMed] [Google Scholar]
- 50.Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, McTaggart RA, Torbey MT, Kim-Tenser M, Leslie-Mazwi T, Sarraj A, Kasner SE, Ansari SA, Yeatts SD, Hamilton S, Mlynash M, Heit JJ, Zaharchuk G, Kim S, Carrozzella J, Palesch YY, Demchuk AM, Bammer R, Lavori PW, Broderick JP, Lansberg MG; DEFUSE 3 Investigators. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378:708–718. doi: 10.1056/NEJMoa1713973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Warach S, Johnston SC. Endovascular thrombectomy for ischemic stroke: the second quantum leap in stroke systems of care? JAMA. 2016;316:1265–1266. doi: 10.1001/jama.2016.12266 [DOI] [PubMed] [Google Scholar]
- 52.Landis S, Fisher M. Why the United States needs a network for stroke clinical trials. Stroke. 2013;44:1217–1218. doi: 10.1161/STROKEAHA.113.001534 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.