Abstract
What is already known about this topic?
Plague is an acute infectious disease caused by Yersinia pestis (Y. pestis) and is primarily transmitted by rodents. Human can be infected by bites of bacterium-bearing fleas or direct contact with diseased or dead plague-infected animals. In 2004, the last human plague case was reported in Inner Mongolia Autonomous Region due to skinning a dead hare.
What is added by this report?
This is the first case of pneumonic plague imported into a major city since the founding of the People's Republic of China. Two primary pneumonic plague cases (Patients A and B) found in residents of Inner Mongolia were confirmed in Beijing on November 12, 2019. Another case (Patient C) of Y. pestis was identified as bubonic plague on November 14. Patient A most likely became infected from aerosol exposure to infective droplets while digging on his farm, located in an Meriones unguiculatus (M. unguiculatus) natural plague focus. Patient B became infected from contact with Patient A (her husband). Patient C became infected after skinning a dead hare. There was no epidemiological relationship between the Patient A/B and Patient C.
What are the implications for public health practice?
When epizootic plague is detected, local health-care providers and the public should be alerted about any possible risks. Public education efforts should focus on promoting personal protection measures.
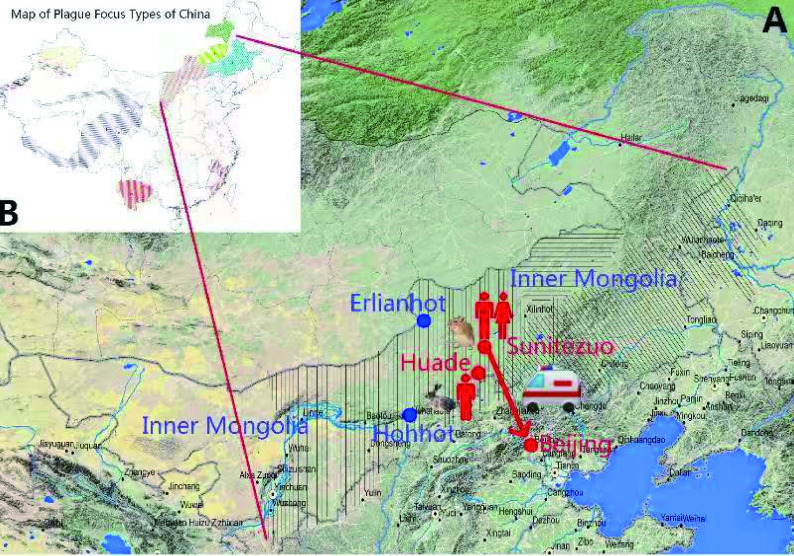
On November 11, 2019, Beijing Center for Disease Control (Beijing CDC) identified two cases of Yersinia pestis (Y. pestis)-induced pneumonic plague in a husband and wife from the Sunitezuo Qi (County) of the Xilinguole League (Prefecture) in Inner Mongolia Autonomous Region. Three days later on November 14, 2019, another case of Y. pestis was identified in a patient from Huade County of Ulanchabu City in Inner Mongolia, 130 kilometers from the first two cases. China CDC established no epidemiological relationship between the two events (Figure 1).
Figure 1.
Geographic distribution and relation of the three human plague cases in Inner Mongolia and Beijing. Part A: vertical line area: Meriones unguiculatus plague focus; horizontal line area: Microtus brandti focus; slant line area: Spermophilus Dauricus focus; cross line area: overlap area between Meriones unguiculatus and Spermophilus Dauricus. Part B: map of plague focus types in China..
A total of 447 persons with direct contact in Beijing and 46 in Inner Mongolia were quarantined for medical observation. As of November 21, 2019, all persons with direct contact were discharged from medical observation.
Investigation and Results
Patient A.The index case (Patient A) was a 43-year-old male herdsman. On October 25, the day after working the soil on his farm, he had sudden onset of fever (40 ºC), with chills, vomiting, chest pain, breathlessness, and cough with blood-tinged sputum. He reported no swollen lymph nodes. He sought treatment in a local county hospital, where he was admitted and stayed for two days. On October 27, his condition deteriorated and he was transferred to League Central Hospital (LCH) by ambulance and was admitted to the intensive care unit (ICU) where he stayed for seven days.
Patient B. On October 31, while Patient A was in the ICU, his wife (Patient B, 46 years old), who had accompanied and cared for him, had onset of cough with a low-grade fever (38 ºC). She was hospitalized in LCH. Over the next 24 hours her condition worsened with increasing cough, blood-tinged sputum production, nausea, vomiting, and diarrhea. Computerized tomography revealed pneumonia. Husband and wife were treated with antibiotics in the local hospital from October 25 to November 2 but did not show significant improvement. They were transferred by ambulance to a general hospital in Beijing on November 3 and were given Moxifloxacin and Cefoperazone sodium along with supportive treatment. There was no clinical improvement.
On November 12, blood and sputum specimens were tested by Beijing CDC and were found to be positive by RT-PCR and colloidal gold-immunochromatography assay targeting the F1 antigen and by reverse indirect hemagglutination assay (RIHA). Although Y. pestis was not able to be isolated by culture, NGS sequencing was weakly positive for Y. pestis genetic material. Beijing CDC and Inner Mongolia CDC immediately initiated a coordinated investigation, including evaluation of potential exposures to the patient and an environmental assessment to determine risk of further transmission. The Inner Mongolia Plateau is home to Meriones unguiculatus (M. unguiculatus), a primary mammalian host of Y. pestis, with cases of intense wild rodent epizootic disease in 2019.
Patient C. On November 11, 2019, Patient C (55-year-old male) sought treatment in a local hospital in Huade County for swollen lymph nodes and fever. Patient C had eaten a dead hare he found in the field. A clinician noted this exposure and suspected Y. pestis infection. The Inner Mongolia CDC laboratory identified Y. pestis by culture with the phage lysis test and with RT-PCR from lymph nodes aspirates. Blood cultures were negative for Y. pestis. On November 13, the patient was reported to Huade County CDC as having bubonic plague. An epidemiological investigation indicated no relation between Patients A/B and Patient C. However, Patient C lives in a county that is known to be a natural focus of Y. pestis.
Public Health Response
When epizootic plague is detected, local health-care providers and the public should be alerted to potential risks of plague. Educational efforts should promote personal protection measures, including: 1) educating the public to avoid direct contact with sick or dead animals (e.g., rodents and rabbits in Inner Mongolia); 2) wearing long pants and applying insect repellent on the skin, to clothing, and to outer bedding of anyone who engages in outdoor activities in an area that is an endemic focus for plague; 3) abstaining from handling or skinning wild or domestic animals that died of unknown reasons and using gloves when handling animals killed by trapping or hunting; 4) taking prophylactic antibiotics if risk of exposure is high; and 5) keeping pet dogs and cats in natural plague foci free from fleas and not allowing them to wander freely (1).
In response to the events reported above, key preventive measures have been implemented in Inner Mongolia. These include: 1) enhanced surveillance for plague in rodents and rodent predators in enzootic areas; 2) use of insecticides and rodenticides to eliminate wild rodent fleas and reservoirs; 3) strengthening of professional training and alerting doctors to the forms of plague; 4) strengthening of professional training for local CDC and clinical laboratory staff; 5) monitoring rodent die-offs and educating the public to report sightings of dead animals and reductions in animal colony size; and 6) considering plague in the differential diagnosis of ill domestic animals, including dogs and cats, in the natural plague foci areas.
Discussion
Plague is an acute, often fulminating, infectious disease caused by Y. pestis. There are three main forms of plague, with the specific form depending upon route of infection: bubonic plague, septicemic plague, and pneumonic plague (1). Most human plague cases are of the bubonic form, which results from bites by infected fleas. However, plague can also be transmitted to humans by handling infected animals or by inhaling infectious aerosols from persons with pneumonic plague and from diseased or dead animals. The family of patients A and B lived in an independent house in a grassland, and investigators determined that the index patient most likely became infected while working the soil on his farm, an area where M. unguiculatus serves as a primary plague host. Five hundred meters from the house of Patients A and B, a live M. unguiculatus was trapped and found to be culture-positive for Y. pestis. A large rodent die-off was also observed in the area, raising the possibility that the decayed bodies in the dirt or in rat holes could have produced infectious aerosols. The wife (Patient B) most likely was infected from contact with her husband.
Plague is primarily a rodent-hosted, transmitting disease. Animal to animal transmission is mediated by the bites of fleas that were became infected by biting infected animals. Humans can be infected by the bites of bacterium-bearing fleas or by direct contact with wild or domestic animals that died from plague or are diseased with plague (marmots, foxes, lynxes and badgers, dogs (2), Tibetan sheep (3), and cats). Person-to-person transmission occurs only with pneumonic plague. Plague is categorized as a Class A infectious disease, the most serious category under China’s Law on the Prevention and Treatment of Infectious Diseases (4).
Plague in Inner Mongolia
Human plague has been well controlled since 1959 in Inner Mongolia. During 1960-2018, only nine human plague cases with two deaths occurred in Inner Mongolia (5). The most recent human plague cases were reported from this focus in 2004, and as with Patient C, were due to skinning a dead hare (6).
There are four plague foci in Inner Mongolia (7). These are an M. unguiculatus plague focus in the Inner Mongolian Plateau, a Microtus brandti plague focus in the Xilin Gol Grassland, a Spermophilus Dauricus plague focus in the Song-Liao Plain and a Marmota sibirica plague focus in the Hulun Buir Plateau (a silent plague focus). The M. unguiculatus plague focus in Inner Mongolia can be divided into two parts - the Ordos plateaus and the desert steppe of the Ulanqab plateaus. The S. dauricus focus includes the Song-Liao plain hills and the dry steppe of Qahar area (5).
Combining previous plague epizootic data (5) and recent surveillance data, the Inner Mongolia animal plague epidemic can be divided into four phases, as illustrated in Table 1. The Inner Mongolia plateau focus of M. unguiculatus was first identified in 1954. The total area of this focus is 134,803 km2 and encompasses 22 counties (Qi) in the middle and western parts of Inner Mongolia (5). In the last 5 years, the Inner Mongolia natural foci of animal plague has been active. In 2019, virulent animal plague epidemics occurred in this focus, which has a high density of rats.
Table 1. Animal plague epidemics in Inner Mongolia in the last 70 years.
| Phase | Years | Main host in epizootic | Plague sub-focus † |
| *Virulent animal plague epidemics occurred in the second phase. The epidemics swept all three foci of Inner Mongolia.
†Microtus brandti plague focus of the Xilin Gol Grassland was not included because the Y. pestis isolated in this focus was considered to have low pathogenicity to humans. | |||
| First epizootic | 1954-1955 | S. dauricus | Qahar area (1985-1989) |
| Second epizootic * | 1969-1972 | M. unguiculatus | Ordos plateau, Ulanqab plateaus (1968-1969) |
| S. dauricus | Qahar area (1970) | ||
| Third epizootic | 1973-1998 | M. unguiculatus | Ordos plateau (1973-1976,1987-1990,1996) |
| Ulanqab plateaus (1974,1979,1991)Baoto City (1982,1985) | |||
| S. dauricus | Song-Liao Plain (1985-1989) | ||
| Qahar area (1973-1974, 1988-1994) | |||
| Fourth epizootic | 2001-2019 | M. unguiculatus | Ordos plateau (2015, 2016) |
| Spread throughout all M. unguiculatus plague focus (2019) | |||
Since the founding of the People’s Republic of China, this is the first instance in which pneumonic plague was imported into a major city in China. Although clearly a transported case, awareness and appropriate measures should always be implemented. These three cases can provide important lessons for public health practitioners.
Acknowledgments
We thank China CDC colleagues participating in the outbreak investigation; we are grateful to Beijing CDC colleagues participating in the investigation and response; and we thank those who collected surveillance data from the Inner Mongolia Autonomous Region.
This work was supported by National Key Scientific and Technology Project (2018ZX10101002-002), National Mega-Projects for Infectious Disease (2018ZX10201002-008-002), and the National Natural Science Foundation (NSFC, 71934002)
Contributor Information
Wei Li, Email: liwei@icdc.cn.
Yanping Zhang, Email: zhangyp@chinacdc.cn.
References
- 1.CDC. Plague. Atlanta, GA: US Department of Health and Human Services, CDC; 2019. Available at http://www.cdc.gov/plague/.
- 2.Wang H, Cui Y, Wang Z, Wang X, Guo Z, Yan Y, et al. A dog-associated primary pneumonic plague in Qinghai Province, China. Clin Infect Dis. 2011 Jan 15;52(2):185 − 90. https://doi.org/10.1093/cid/ciq107.
- 3.Dai R, Wei B, Xiong H, Yang X, Peng Y, He J, et al. Human plague associated with Tibetan sheep originates in marmots. PLoS Negl Trop Dis. 2018;12(8):e0006635. https://doi.org/10.1371/journal.pntd.0006635.
- 4.Cong X, Yin W. Chinese Plague Manual: Prevention, Control and Emergency Response. Beijing Univ Med Press. 2009;1 − 49. (In Chinese).
- 5.Liu J, Zhang W. Inner Mongolia Plague. Huhhot: Inner-Mongol People Publishing House. (In Chinese).
- 6.Han X, Liu G, Yue M. A clinical diagnosis of plague in Inner Mongolia in 2004. Med Ani Prev. 2007;23(12): 918 − 9. (In Chinese).
- 7.The Atlas of Plague and Its Environment in the People’s Republic of China. Science Press; 2000. (ISBN7-03-008197-8/P·1186). (In Chinese).