Abstract
The current COVID-19 pandemic is testing political leaders and healthcare systems worldwide, exposing deficits in crisis communication, leadership, preparedness and flexibility. Extraordinary situations abound, with global supply chains suddenly failing, media communicating contradictory information, and politics playing an increasingly bigger role in shaping each country's response to the crisis. The pandemic threatens not just our health but also our economy, liberty, and privacy. It challenges the speed at which we work, the quality of our research, and the effectiveness of communication within the scientific community. It can impose ethical dilemmas and emotional stress on healthcare workers. Nevertheless, the pandemic also provides an opportunity for healthcare organizations, leaders, and researchers to learn from their mistakes and to place their countries and institutions in a better position to face future challenges.
Keywords: pandemic, crisis, leadership, communications, research, preparedness, ethics, dilemma
Introduction
From its origin in Wuhan, China, the novel Coronavirus Disease (COVID-19) has traveled the world. It was declared a pandemic by the World Health Organization (WHO) on March 3, 2020, and has caused about 50 million infections worldwide so far. By September 2020, the death toll had reached 1 million worldwide, and it continues to rise.
The unprecedented speed at which the virus has traveled and its dramatic consequences have forced leaders worldwide to come up with new game plans. Although they all face the same opponent, they have at times reacted very differently, with results ranging from successful containment of the disease to largely uncontrolled growth.
During acute phases of a pandemic, a nation's fate lies in the hands of the responsible political leader, who needs to act quickly. Most Western European countries battling COVID-19 have bypassed normal legislative channels, calling on laws governing national emergencies in order to avoid delays deemed unacceptable. Therefore, a nation's well-being has largely been dependent on the leadership skills of its executive authority.
The imposed restrictions have greatly changed citizens' lives, as economies were partially or completely shut down in many areas. After the first COVID-19 ‘wave’, leaders were under pressure to reopen economies, as negative consequences of the lockdown began to outweigh potential benefits. In parallel, the public's expectations and corresponding pressure on the scientific community to provide answers and guidelines rose steadily, leading to a surge in scientific publications. While the mass media can contribute to the rapid delivery of important information in real time, some sources have instead played a disruptive role, providing a platform for misleading information.
By analyzing how well leaders have been able to cope with the COVID-19 challenge and how institutions and communities are learning to live with the virus, we can draw conclusions for the future.
Role of media and communication
The COVID-19 pandemic is the first global event that we have been able to observe and react to in real time from everywhere, through global high-speed data networks, television, social media, and interpersonal contact. Anyone with a mobile telephone, a computer, or a tablet has access to the most recent facts and data around the clock.
This is not always a good thing. As growing numbers of infections and deaths are reported without corresponding information about appropriate counter measures, fear has spread, and many people have turned to self-proclaimed ‘specialists’ who claim to have the knowledge necessary to deal with the situation. Some of these ‘gurus’ share their own views with the community via social media [1]. Others are members of the media who judge the ability to generate clicks more important than the ability to provide their customers with concise and reliable information.
Journalists and publishers must be aware of the important role they play in health communications and of the influence they have on public opinion [2]. As seen in the climate change debate, uncertainty can be used to sow doubt and to manipulate public opinion. In addition, the absence of governmental guidance and the existence of conflicting information have fostered the spread of rumors and unsubstantiated news reports. To underline the severity of this development, the situation was even referred to as an ‘infodemic’ by World Health Organization (WHO) Director-General Tedros Adhanom Ghebreyesus [3]. This shows the importance but also the difficulty of providing early, clear, and effective communication, especially in the face of rapidly growing but still incomplete knowledge. Risks inherent in the use of social media have led to the suggestion that guidelines be provided for professional use [4].
In view of the special circumstances of the pandemic, there should be close collaboration between journalists and scientists. Despite intrinsic differences in motivation, providing the public an overview of the current scientific evidence and consensus in understandable words is key.
What are the main aspects of good communication during a crisis? In general, communication should happen frequently – certainly more often than one thinks. It should be empathetic, honest, transparent and understandable, able to build trust, and foster resilience. Communication should focus on the provision of honest information, which clearly distinguishes between facts and assumptions, and labels them.
On the basis of previous experience from the outbreaks of BSE (bovine spongiform encephalopathy) and Ebola, a five-step checklist for effective health communication practice has been developed [5]:
-
1.
Set shared goals
-
2.
Establish a coordinated response
-
3.
Devise a communications strategy
-
4.
Implement the communications plan
-
5.
Be ready to adapt
To reach the target audience, communication needs to be proactive, as it is competing with many other sources of information. It should aim to establish trust and contradict false information. This can be achieved by focusing on people and their needs and expectations.
Even if core messages – which are usually of unpleasant nature – must be repeated frequently, we can still counter them with bright spots and opportunities. Ideally, leaders should react to the special circumstances of a pandemic, offering safe feedback channels, addressing concerns, providing adequate plans for the future, and supporting remote communications like video calls [6].
Challenges for the scientific community
Research questions are often triggered by unforeseeable events. When a hypothesis is formulated, peer-reviewed publication in a scientific journal is usually years of hard work away. Therefore, scientific work-up inevitably lags behind frontline development. But during times of crisis, and especially during a pandemic, there is enormous interest in information, and people expect to get answers quickly. Some researchers choose to respond to the public directly, often taking advantage of social media. Others reach out to their peers, bypassing the normal scientific process of data generating, discussion, scientific failure and success to publish unverified theories. The result is an increase in public uncertainty and a possible loss of trust in science. This dilemma is a major challenge for the scientific community.
The interest of the scientific community and enormous socio-economic pressure have led to a surge of scientific publications about COVID-19, with mixed consequences [7]. Open access publications and collaboration between researchers were fostered. But pressure, lack of time, inadequate research facilities, and lack of experience may lead to avoidable scientific waste, which has been reported to be as high as 85%, even in the pre-pandemic era [8].
One option for making new research data rapidly accessible to the scientific community are preprints. Their use has massively increased in the current year [9,10]. Initially conceived as a basis for discussion within the scientific community, preprints risk being misinterpreted if they are not scrutinized by experts but are accepted as completely true by laypersons. In addition, inaccurate or questionable results already communicated by the media are difficult to retract or eliminate and may be misleading, undermining the credibility of properly performed scientific work and aggravating the problem of “fake news.” [11].
An additional challenge for the community is to avoid duplicate work, as it is difficult to oversee all research in progress without an internationally centralized infrastructure providing an overview. Therefore, the research community has the responsibility to challenge and test its own results in-depth before making them available to the public or labeling them as “evidence-based.” The scientific community must resist the temptation to ignore scientific rules of good practice in order to fulfill the wishes of leaders, sponsors, and peers. What seems to be a win–win situation in the beginning may endanger trust in science in the future, for example, if severe side effects or lack of efficacy of a vaccination are discovered after a premature launch of the product [12].
To ease the dilemma between speed and quality, centralized infrastructure and pre-established networks have proven useful for the rapid set-up of appropriate studies, as shown by the United Kingdom's multicenter trials infrastructure being used to set up the RECOVERY trial [13]. The peer-review process must be more scalable and adaptable without putting quality at risk [14,15]. Currently, even renowned journals seem to be struggling to maintain the quality of the scientific review process [16]. For example, an article describing a novel COVID-19 vaccination using a vector virus has been heavily criticized by the scientific community since its publication [17,18].
Despite the best intentions and quality assurance, scientific evidence and consensus will shift over time. To maintain public support for science-based policies, careful, effective, and honest science communication is critical [19].
Good leadership in a time of crisis
In response to the rising number of infections and fatalities during the first COVID-19 wave, most Western European countries and the US went into lockdown, just as China had in the previous weeks and months. These lockdowns partially shut down economies and led to increased national debt, unemployment, and exacerbation of existing socioeconomic disparities. However, only a few countries chose a different strategy – for example, Sweden, which did not go into lockdown in Spring but paid a high price for the failure to protect elderly people from the virus [20]. It is too early to determine which model is better or to predict which will be the ‘right’ approach to take, especially given the concurrent annual common cold and flu season and the accompanying rise in the number of respiratory infections.
But why would politicians support such tough measures – putting their political careers at risk – especially if evidence of the real risk (mortality rates) and effectiveness of measures (e.g., social distancing, protective equipment) is scarce?
At the core of good crisis leadership is decision-making. Leaders must make the right decisions at the right time and be able to convince their workforce or constituents that they have done so, even if the decision is unpopular and associated with major restrictions. The goals set must be supported by optimal communication and followed through with progress in the planned direction. Timely decisions made in a state of uncertainty are risky but potentially offer the only chance at a window of opportunity.
For the right decision to be made, a problem must be recognized and correctly assessed. This may involve using risk management tools such as a likelihood/severity of consequences matrix. It is important to incorporate the best available evidence into your decision-making. Humans have a natural tendency to delay decisions and downplay the magnitude of a problem (e.g., cognitive bias). In addition, dysfunctional group dynamics and organizational or economic pressure are often underestimated and threaten the ability of a leader to achieve situational awareness [21].
An example of good leadership and crisis communication comes from New Zealand, where the government gave its population a clear, stepwise escalation and de-escalation plan in the face of the pandemic [21]. In October 2020, New Zealand's Prime Minister Jacinda Ardern won a landslide victory in the country's general election, harvesting the fruits of hard labor [22].
With the situation changing rapidly, every decision must be challenged frequently. Situational awareness is built through an iterative process of continuously analyzing the environment and circumstances. In the words attributed to Helmuth von Moltke (1800–1891), a Prussian General Field Marshall: “No battle plan survives contact with the enemy”; it requires continuous updating and redirecting. In modern terms, this is called ‘adaptive leadership’. It can be remembered through a mnemonic device, the four A's: “Anticipation of likely future needs, trends and options; Articulation of these needs to build collective understanding and support for action; Adaptation so that there is continuous learning and adjustment of responses as necessary, and Accountability, including maximum transparency in decision-making processes and openness to changes and feedback.” [23].
In this process, mistakes are inevitable and must be viewed as an opportunity for productive action. Leaders should avoid blame and stay focused on the superordinate goal [21].
As leaders and their situational analyses differ, so does the timing of measures they support. On the one hand, South Korea's actions were early and effective, with small and controlled numbers of reinfections, building on its experience with the Middle-East Respiratory Syndrome (MERS) epidemic in 2015. In comparison, countries such as the United States and Brazil acted late and less stringently, possibly leading to more infections and deaths [24,25]. Consistency and style of communication chosen by the respective political leaders probably contributed to this, as it did within the US in a comparison of Seattle and New York [26]. Lack of trust in officials and their statements seems to be a common denominator of failure [27].
As the first wave of the pandemic eventually flattened and the economic implications of the lockdown became unbearable, countries had to reopen to an uncertain future based on limited scientific knowledge about the efficacy of protective measures. From a citizen's perspective, civil rights, data protection and individual freedom must be balanced against restrictions due to the need for tracing and containment of outbreaks. Emergency law must be followed by legislative processes. All these measures must be based on an adequate situational analysis taking into account the latest scientific evidence. Balancing these contradictory requirements and choosing the right time to implement them is a major challenge and requires profound leadership skills.
Caring for your employees during a crisis
In the special circumstances of a pandemic, people become more fearful as the future becomes more unclear and the situation appears increasingly unstable. People feel enormous pressure as their daily lives are significantly disrupted. In addition, the pandemic seems to exacerbate inequalities, with wealthy people coping better with the imposed restrictions than the poor [28]. This additional tension can lead to increased racism, discrimination, and aggression [29,2].
In addition to disruption of their private lives, healthcare workers experience a massive increase in pressure at work. As the number of patients spirals upwards and exposure to potential harm increases, holidays are canceled, shifts lengthened, and regulations covering maximum work hours cannot always be followed. If other healthcare professionals or even direct colleagues are affected by the virus and require medical assistance or even die, this intensifies the burden.
Employers in the healthcare sector have to take into account the fact that their workforce is especially at risk of disease transmission. While providing advice, training, and equipment for personal protection is key to maintain confidence and avoiding cross-contamination, staffing and roster models should be revised in light of the threat. As it is unclear how long the pandemic will last and how many employees will be affected, sufficient reserves should be planned in advance in order to be able to maintain service even if the situation becomes worse than expected. For example, adapting the staff roster to meet the epidemiological characteristics of the pandemic might significantly reduce intensive care staffing shortages [30].
Steps necessary to keep hospital services running must be carefully chosen and extensively communicated, as informed personnel tend to work better and show more understanding. This should be done in close collaboration with labor unions to prevent unnecessary – and in such a situation dangerous – opposition. It is of utmost importance to emphasize that abolition of an employee's rights must be a temporary measure, and that the employer can be held responsible in the aftermath of a pandemic.
Whereas working remotely has proven to be an option for many members of the workforce, it is less feasible on the healthcare frontline, where having enough workers available on the spot is key to keep services up and running. Employees at risk should be allowed to work from home or in other roles that minimize their exposure, but employers must be cognizant of the fact that this requires different management skills. It can be more difficult to maintain efficiency and productivity in a remote setting, which requires more trust and potentially more technical resources, and imposes a different kind of stress on the home-based worker [31]. In addition, who will handle the costs of the technology needs must be clarified. In Switzerland, for example, a court ruled that employees have to be compensated for the use of their infrastructure [32].
Workers in the acute care setting during a pandemic – especially in emergency departments and intensive care units – may face ethical dilemmas when balancing therapy options. In the case of rapidly increasing numbers of sick patients and scarce resources (hospital/intensive care beds, respirators, etc.), doctors and nurses may find themselves in a situation for which they have not been adequately trained. Under normal circumstances, the aim is to provide the best possible care to every patient treated. In a pandemic, it may be necessary to decide which patient receives treatment and which has to be denied [33,34].
Trying to respect all four principles of medical ethics – autonomy, non-maleficence, beneficence and especially justice – can place huge emotional pressure on healthcare workers [35]. To ease this pressure and to help maintain the public's confidence in medical institutions, in March 2020 [36], the Swiss Academy of Medical Sciences published national guidelines in collaboration with the Swiss Society of Intensive Care Medicine (updated in November 2020) [37]. The Swiss guidelines focus on the potential benefit of intensive care therapy, irrespective of age (although age of course influences the potential benefit as physiological reserves diminish). The guidelines have been criticized for not adequately respecting patients' wishes, but have been widely accepted in practice [38]. In contrast to the Swiss guidelines, their Italian counterpart focuses more on years of life expectancy saved [39]. Whichever strategy is preferred, clear and accepted guidelines are of utmost importance for employees on the frontlines. Having medical and scientific societies communicate sound guidelines in a timely fashion can help overcome the many single voices of scientists communicating their own agendas to the public.
From a leadership perspective, employers must offer as many resources and strategies as possible to help employees build up their resilience and coping strategies. This starts with the good communication described earlier and includes rapid development of clinical and institutional guidelines and a commitment to offer safe and open feedback channels and a positive learning culture throughout the institution.
Preparing for the ‘unthinkable’
During the first wave of a pandemic, hospitals have to cope with high, exponentially growing, unforeseen workload. They have to be able to recruit resources in a short period of time (e.g., retired workers, students, personal protective equipment) and to follow a steep learning curve in adaptation (and if possible simplification) of treatment processes in order to meet increasing demand. In this situation, an organization should aim for an imperfect but practicable solution, rather than aiming for a perfect solution which comes too late.
As we learned from the initial stages of the pandemic, personal protective equipment (such as face masks) is rapidly out of stock if the spread of the virus is global and production facilities are concentrated in one region or country. Previously well-functioning supply chains are suddenly disrupted, and the very efficient just-in-time approach to production stagnates, as production ceases and transportation facilities are lacking.
It therefore seems prudent to have a stockpile of critical goods and to strive for diversification of your supply chains, as these seem to be more vulnerable than we previously thought [40]. These stockpiles must be correctly sized and actively managed, as Taiwan has demonstrated in exemplary fashion, based on the experience gained from the outbreak of the Severe Acute Respiratory Syndrome (SARS) in 2003 [41]. The costs of critical goods have risen, and production machinery and know-how had to be reimported into many western countries. If disaster strikes, every country will be looking out for itself. This was seen in the current pandemic, with countries confiscating protective equipment being transported on the ground through their territories, even when bought by friendly, neighboring countries [42].
With the flattening of the first wave, recommencement of elective surgeries has to be planned, all the while keeping in mind the likelihood of a second wave and the possibility of further waves. During this planning process, every step that helped us cope with the first wave of the COVID-19 virus (e.g., newly installed piping for critical care facilities, conversion of non-clinical into clinical areas, staff pools) should be documented and condensed into a plan of action for the next wave.
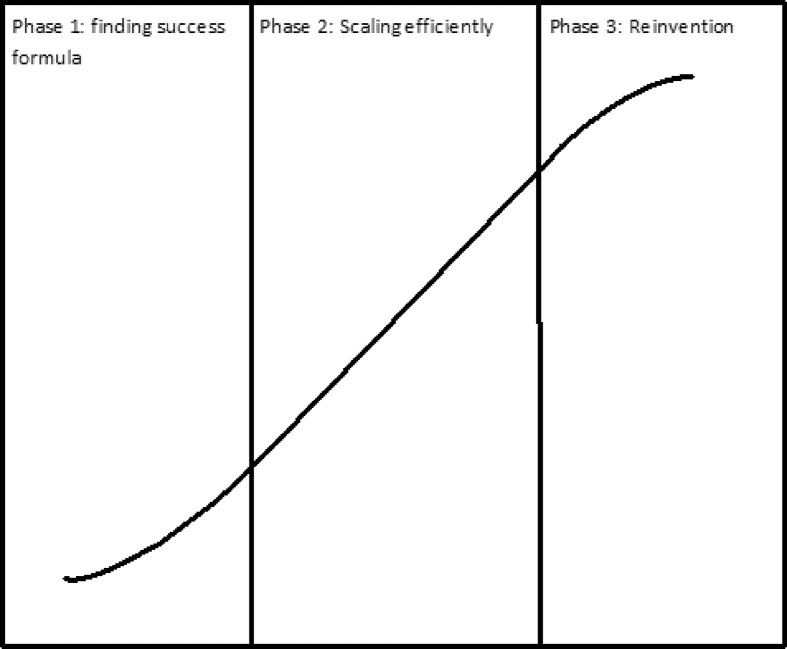
The leadership needed during these different phases might be compared to the leadership needed in start-ups, which follow the so-called S-curve model [43]. During the initial phase, start-ups struggle immensely and experiment vigorously to determine what works and how to streamline processes. It takes them a while to find the formula for success. Approaching their work systematically by documenting the processes they use helps in reaching phase two, in which an institution can cope with rising demand due to optimized efficiency. After a while, the situation will change again (e.g., recommencement of elective surgical service, onset of the second pandemic wave) and your initial formula for success will become obsolete, as it does not meet the new needs. To master the transition to this third phase successfully, you will need to constantly reassess and analyze the situation.
By combining communication, leadership, management and science, leaders can play an important role in the way their citizens and workforces experience and overcome a crisis. To succeed, leaders must make the right decisions at the right time; communicate their decisions in an understandable, honest and transparent way; and be ready to adapt – the situation will change repeatedly (see Fig. 1 ).
Practice points.
Communication
-
•
Communicate more often than you think is necessary;
-
•
Be honest, transparent, understandable, and empathetic;
-
•
Repeat core messages, but also highlight bright spots and opportunities;
-
•
Offer safe feedback channels.
Leadership
-
•
Be predictable, as this builds trust;
-
•
Strive for situational awareness by assessing likelihood and potential consequences of a threat;
-
•
Use risk management tools and call on expertise as needed;
-
•
Make timely decisions;
-
•
Consider options that are risky but appear in a brief window of opportunity;
-
•
Realize that errors are inevitable and approach them as opportunities rather than a reason to blame;
-
•
Communicate decisions transparently and constantly reassess them thereafter;
-
•
Support your employees by providing open and respectful feedback and a positive learning culture.
Management
-
•
Start preparing before the crisis;
-
•
Have measures ready to minimize a potential loss in workforce by adapting the staff rosters;
-
•
Be aware that supply chains are vulnerable and critical goods might be out of stock quickly;
Science
-
•
Resist the temptation to bend or ignore scientific rules in order to achieve results more quickly.
Research agenda.
The chief research priorities necessary to advance current understanding and practice include:
-
•
An understanding of the need to work with the media in communicating facts about the pandemic;
-
•
Recognition and development of leadership qualities needed to manage large healthcare organizations;
-
•
Provision of resources needed for employees to build up their resilience and coping strategies;
-
•
Creation of guidelines for managing ethical dilemmas, such as triage.
Fig. 1.
Adapted from harvard business review 2020, what hospitals overwhelmed by COVID-19 can learn from startups [43].
Summary
The current COVID-19 pandemic threatens our health, economy, liberty, and privacy. It challenges the speed and quality of research. It exposes deficits in communication, leadership, preparedness and flexibility, but also provides an opportunity for healthcare organizations, leaders, and researchers to learn from their mistakes.
Modern mass media and communication channels offer an opportunity to rapidly distribute important news and guidelines, but come with an inherent risk of being equally efficient at spreading misleading or dangerous information. Journalists and their publishers must be aware of their important role in building public opinion.
Close collaboration between journalists and scientists is necessary to maintain trust in science. Researchers must resist the temptation to ignore the rules of good clinical practice and to publish preliminary data without adequate peer review.
Good communication must be honest, transparent (“What do we know? What do we assume because we don't know?”), understandable, and empathetic. During a crisis, responsible leaders can never communicate too often.
Employees need support during a pandemic. In the case of healthcare workers facing high workload, high emotional pressure, and, at worst, ethical dilemmas, employers should not only provide supplies and training but also psychological and emotional support and robust clinical guidelines. Adapting staff rosters can help minimize staff shortages and work overload and maintain a minimal work-life balance.
The hallmark of good leadership is to make the right decision at the right time even if consequences are unpleasant. Every decision has to be adapted in a timely manner as circumstances change.
Funding
This research did not receive specific support from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
Christian M. Beilstein helped to write the article.
Lutz E. Lehmann helped to write the article.
Matthias Braun helped to write the article.
Richard D. Urman helped to write the article.
Markus M. Luedi helped to write the article.
Frank Stüber helped to write the article.
All authors have seen, reviewed and approved the final manuscript.
Declaration of competing interest
Richard D. Urman reports research funding/fees from Merck, Medtronic/Covidien, AcelRx, Takeda. All other authors declare no conflicts of interest.
References
- 1.González-Padilla D.A., Tortolero-Blanco L. Social media influence in the COVID-19 Pandemic. Int Braz J Urol. 2020;46(suppl.1):120–124. doi: 10.1590/s1677-5538.ibju.2020.s121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shimizu K. 2019-nCoV, fake news, and racism. Lancet. 2020;395(10225):685–686. doi: 10.1016/s0140-6736(20)30357-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zarocostas J. How to fight an infodemic. Lancet. 2020;395(10225):676. doi: 10.1016/s0140-6736(20)30461-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chan A.K.M., Nickson C.P., Rudolph J.W., et al. Social media for rapid knowledge dissemination: early experience from the COVID-19 pandemic. Anaesthesia. 2020 doi: 10.1111/anae.15057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratzan S.C., Sommariva S., Rauh L. Enhancing global health communication during a crisis: lessons from the COVID-19 pandemic. Public Health Res Pract. 2020;30(2) doi: 10.17061/phrp3022010. [DOI] [PubMed] [Google Scholar]
- 6.Holtom B., Edmondson A.C., Niu D. 5 tips for communicating with employees during a crisis. Harv Business Rev. 2020 [EPub] [Google Scholar]
- 7.Glasziou P.P., Sanders S., Hoffmann T. Waste in covid-19 research. Br Med J. 2020;369:m1847. doi: 10.1136/bmj.m1847. [DOI] [PubMed] [Google Scholar]
- 8.Chalmers I., Glasziou P. Avoidable waste in the production and reporting of research evidence. Lancet. 2009;374(9683):86–89. doi: 10.1016/s0140-6736(09)60329-9. [DOI] [PubMed] [Google Scholar]
- 9.Yan W. New York Times; 2020. Coronavirus tests science's need for speed limits. 14.04.2020. [Google Scholar]
- Kwon D. How swamped preprint servers are blocking bad coronavirus research. Nature. 2020;581(7807):130–131. doi: 10.1038/d41586-020-01394-6. [DOI] [PubMed] [Google Scholar]
- 11.Ioannidis J.P.A. Coronavirus disease 2019: the harms of exaggerated information and non-evidence-based measures. Eur J Clin Invest. 2020;50(4) doi: 10.1111/eci.13222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Torreele E. The rush to create a covid-19 vaccine may do more harm than good. Br Med J. 2020;370:m3209. doi: 10.1136/bmj.m3209. [DOI] [PubMed] [Google Scholar]
- 13.Horby P.P. 2020. A randomised trial of treatments to prevent death in patients hospitalised with COVID-19 (coronavirus). ISRCTN Registry. 02.10.2020. [DOI] [Google Scholar]
- 14.Vabret N., Samstein R., Fernandez N., et al. Advancing scientific knowledge in times of pandemics. Nat Rev Immunol. 2020;20(6):338. doi: 10.1038/s41577-020-0319-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaway E. Will the pandemic permanently alter scientific publishing? Nature. 2020;582(7811):167–168. doi: 10.1038/d41586-020-01520-4. [DOI] [PubMed] [Google Scholar]
- 16.Zdravkovic M., Berger-Estilita J., Zdravkovic B., et al. Scientific quality of COVID-19 and SARS CoV-2 publications in the highest impact medical journals during the early phase of the pandemic: a case control study. PloS One. 2020;15(11) doi: 10.1371/journal.pone.0241826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Logunov D.Y., Dolzhikova I.V., Zubkova O.V., et al. Safety and immunogenicity of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine in two formulations: two open, non-randomised phase 1/2 studies from Russia. Lancet. 2020;396(10255):887–897. doi: 10.1016/s0140-6736(20)31866-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andreev K. Note of concern: open letter to DY Logunov et al., authors of: “Safety and immunogenicity of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine in two formulations: two open, non-randomised phase 1/2 studies from Russia. Lancet. 2020 doi: 10.1016/S0140-6736(20)31866-3. https://cattiviscienziati.com/2020/09/07/note-of-concern/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kreps S.E., Kriner D.L. Model uncertainty, political contestation, and public trust in science: evidence from the COVID-19 pandemic. Sci Adv. 2020 doi: 10.1126/sciadv.abd4563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Habib H. Has Sweden's controversial covid-19 strategy been successful? Br Med J. 2020;369:m2376. doi: 10.1136/bmj.m2376. [DOI] [PubMed] [Google Scholar]
- Kerrissey M., Edmondson A. Vol. 13. HBR; 2020. What good leadership looks like during this pandemic. April. [Google Scholar]
- 22.Roy E.A., Graham-McLay C. The Guardian; 2020. Jacinda Ardern to govern New Zealand for second term after historic victory. 17.10.2020. [Google Scholar]
- 23.Ramalingam B., Nabarro D., Oqubuy A., et al. HBR; 2020. 5 principles to guide adaptive leadership. [Google Scholar]
- 24.Organsiation WH . 2020. WHO Coronavirus disease (COVID-19) dashboard.https://covid19.who.int/ [Google Scholar]
- Editors T Dying in a leadership vacuum. N Engl J Med. 2020;383(15):1479–1480. doi: 10.1056/NEJMe2029812. [DOI] [PubMed] [Google Scholar]
- 26.Duhigg C. 2020. Seattle's leaders let scientists take the lead. New York's did not. The New Yorker; p. 2020. 04.vol. 5. [Google Scholar]
- 27.Fabian Urech A.E. 2020. Vertrauen in die Regierung erleichtert die Bekämpfung der Pandemie. NZZ; p. 2020. 14.10. [Google Scholar]
- 28.Dorn A.V., Cooney R.E., Sabin M.L. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395(10232):1243–1244. doi: 10.1016/s0140-6736(20)30893-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Devakumar D., Shannon G., Bhopal S.S., et al. Racism and discrimination in COVID-19 responses. Lancet. 2020;395(10231):1194. doi: 10.1016/s0140-6736(20)30792-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mascha E.J., Schober P., Schefold J.C., et al. Staffing with disease-based epidemiologic indices may reduce shortage of intensive care unit staff during the COVID-19 pandemic. Anesth Analg. 2020;131(1):24–30. doi: 10.1213/ane.0000000000004849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parker S.K., Knight C., Keller A. HBR; 2020. Remote managers are having trust issues. July 30. [Google Scholar]
- 32.Surber M. NZZ; 2020. Arbeitgeber müssen einen Teil der Wohnungsmiete übernehmen, wenn sie ihre Mitarbeiter ins Home-Office schicken. 25.05.2020. [Google Scholar]
- 33.Jaziri R., Alnahdi S. Choosing which COVID-19 patient to save? The ethical triage and rationing dilemma. Ethics, medicine, and public health. 2020;15:100570. doi: 10.1016/j.jemep.2020.100570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robert R., Kentish-Barnes N., Boyer A., et al. Ethical dilemmas due to the Covid-19 pandemic. Ann Intensive Care. 2020;10(1):84. doi: 10.1186/s13613-020-00702-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sperling D. Ethical dilemmas, perceived risk, and motivation among nurses during the COVID-19 pandemic. Nurs Ethics. 2020 doi: 10.1177/0969733020956376. 969733020956376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scheidegger D., Fumeaux T., Hurst S. 2020. Covid-19-Pandemie: triage von intensivmedizinischen Behandlungen bei Ressourcenknappheit. [Google Scholar]
- 37.Scheidegger D., Fumeaux T., Schaffert B. Sciences SAoM. 2020. COVID-19 pandemic: triage for intensive-care treatment under resource scarcity, 3d updated version. [Google Scholar]
- 38.Peter C. Jusletter; 2020. Wie begrenzte Ressourcen zugeteilt werden sollen. [Google Scholar]
- 39.Vergano M., Bertolinie B., Gannini A., et al. SIAARTI; 2020. Raccomandazioni di etica clinica per l’ammissione a trattamenti intensivi e per la loro sospensione, in Condizioni eccezionali di squilibrio tra necessità e risorse disponibili. [EPub] [DOI] [PubMed] [Google Scholar]
- 40.Rowan N.J., Laffey J.G. Challenges and solutions for addressing critical shortage of supply chain for personal and protective equipment (PPE) arising from Coronavirus disease (COVID19) pandemic - case study from the Republic of Ireland. Sci total Environ. 2020;725:138532. doi: 10.1016/j.scitotenv.2020.138532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen Y.J., Chiang P.J., Cheng Y.H., et al. Stockpile model of personal protective equipment in taiwan. Health Security. 2017;15(2):170–174. doi: 10.1089/hs.2016.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vonplon D. NZZ; 2020. Deutschland lenkt im Exportstreit um die Schutzmasken ein; p. 4. 14.3.2020. [Google Scholar]
- 43.Edmondson A.C. HBR; 2020. What hospitals overwhelmed by covid-19 can learn from Startups. 22.05. [Google Scholar]