Abstract
The Hospital Incident Command System (HICS) is an incident management system specific to hospitals based on the principles of Incident Command System (ICS), and it includes prevention, protection, mitigation, response, and recovery. It plays a crucial role in effective and timely response during the periods of disasters, mass casualties, and public health emergencies. In recent times, hospitals have used a customized HICS structure to coordinate effective responses to public health problems such as the Ebola outbreak in the US and SARS epidemic in Taiwan.
The current COVID-19 pandemic has placed unprecedented challenges on the healthcare system, necessitating the creation of HICS that can help in the proper allocation of resources and ineffective utilization of healthcare personnel. The key elements in managing a response to this pandemic include screening and early diagnosis, quarantining affected individuals, monitoring disease progression, delivering appropriate treatment, and ensuring an adequate supply of personal protective equipment (PPE) to healthcare staff.
Keywords: COVID, crisis, emergency preparedness, incident command center, emergency management, hospital resiliency
Introduction
Incident command centers originated after complications involving controlling wildfires in California during the 1970s [1]. Multiple organizations are involved and required to orchestrate the mitigation of damages effectively. Several modifications and alterations have led to what we know today as the National Incident Management System (NIMS) led by Federal Emergency Management Act (FEMA). The NIMS takes a comprehensive approach to address the diverse set of threats, hazards, and events. The size, frequency, complexity, and scope of these incidents vary. Still, all involve a range of personnel and organizations to coordinate efforts to save lives, stabilize the incident, and protect property and the environment [2].
Every day, jurisdictions and organizations work together to share resources, integrate tactics, and act collaboratively. Whether these organizations are nearby or support each other from across the country, their success depends on a common, interoperable approach to sharing resources, coordinating and managing incidents, and communicating information [2].
A Hospital Incident Command Center/System (HICS) is the adoption of these tactics, employed during disasters, to organize and coordinate response operations [1]. It is generally a hierarchal structure composed of a prominent figure with several subunits and division leaders. Each subunit is responsible for their respective objectives, goals, and protocols addressing the hospital and coordinating a response if needed [1]. It is the responsibility of each unit to forecast and predict possible damages. It requires a proactive approach before any significant event or disaster for implementation to be made effective immediately. The command center's importance is to accept the disaster's burden and survive it and remain afloat beyond the disaster. Hospital incident command centers are also in effect for the benefit and protection of both the patient and healthcare worker.
Operating room incident command centers function as a limited unit directly involved in deterring further tribulations in the OR. Protocols and checklists have been embraced to limit potential risk and exposure to patients. While an OR incident command center is in effect, it aims for improvisations, not limited to when a pandemic or disaster occurs.
During COVID, the HICS plays an extremely vital role in successfully mitigating the pandemic within the hospital. Judicious record-keeping decreases unforeseen damages and impending repercussions. Effective communication and transparency through local, state, and federal systems provide more stability. As mentioned, it is a multi-organizational prevention-directed approach to combat the pandemic.
This paper will discuss principles of emergency management, planning, and implementation of an incident command center. We will also review the incident management team chain of command, their respective roles, and responsibilities. Next, we will discuss the response and action process, including the importance of proper planning, documentation, and assessment, with indicant action plans. Finally, we will examine how financial and administrative decisions impact the team and this executive branch of the command center's roles. This includes chief command responsibilities, accounting, negotiations, analyzing and forecasting costs, and completing necessary documentation for work-related compensations.
Principles, planning, and implementation
Emergency management team
Operationalizing the incident command center
HICS is also known as the Hospital Incident Command System. This is an emergency and preparedness system for hospitals. It improves a hospital's emergency capabilities in itself or as part of a broader response community. Apart from this, HICS also provides guidance for daily operational performance, pre-planned events, and non-emergencies. In the United States, HICS started in the 1980s. Hospitals adopted an incident management system based on the principles of Incident Command System (ICS). Other countries have implemented similar systems. The United States HICS Guidebook is published by the California Emergency Medical Services Authority (EMSA) [3,4]. This guidebook is a living document updated as additional best practices evolve. This guidebook intends to provide hospitals with the necessary tools to improve their emergency response capabilities and preparedness.
Principles, planning, and implementation
Principles
The HICS is based on the same principles as the NIMS. However, the HICS has been adapted for the healthcare environment. The principles apply to all mission areas of the HICS and include mitigation, prevention, protection, response, and recovery [3,4].
HICS principles:
-
1.
Management by objectives: this consists of evaluating a problem, developing a plan to solve it, implementing the plan (putting the plan into action), and allocating the necessary resources.
-
2.
The HICS should address any hospital's planning, and response needs irrespective of size; hence, it must be scalable.
-
3.
For optimal outcomes, the HICS should use a modular approach. This provides them the adaptability that is necessary to plan and manage a variety of incidents. 4. Accountability is critical. The accountability of tasks is a crucial function of HICS. This includes prioritization of action checklists.
-
5.
A chain of command with a suggested span of control and effective interagency communication are additional (added) principles of the HICS.
Planning
This is a critical component of the HICS, best viewed as a continuous cycle rather than a definite beginning and end process. Planning is fundamental for emergency preparedness. It is essential for developing strategic, operational, and tactical approaches to meet defined objectives. It is based on threats, hazards, and risks that the hospital has identified while also recognizing current and desired incident management capability levels. The different aspects of planning include assessing risks, evaluating capabilities, and evaluating those capabilities through exercises. This planning phase of HICS should also include stakeholders' engagement to ensure their involvement and representation in the planning process. To develop a realistic HICS, it is necessary to have a diverse planning team. Representatives from different hospital departments, supporting facilities, and community representatives should be part of the team. The basis for planning should cover the effects of emergencies. It should also identify those necessary tasks and the individuals required to accomplish them. The planners for a HICS implementation do not have to anticipate every possible emergency scenario. This is impractical [3,4].
The HICS plan should be flexible: It should address differing scales of incidents, from non-emergent to large-scale disasters. It will be necessary to run exercises to ensure that critical elements can handle these different scenarios. Operational personnel are in a position to understand better and execute a scalable plan [3,4].
Implementation
A designated individual or committee is required to review the HICS Guidebook and associated materials for their applicability to their hospital's mission, risks, and size as described in its annual hazard vulnerability analysis (HVA) for the successful implementation of HICS. Usually, the emergency program manager (EPM) will lead this effort, and the emergency management committee (EMC) will perform oversight.
The integration of HICS into a hospital's current operation involves the following steps:
-
1.
Assigning an individual the task of implementing the HICS according to a plan.
-
2.
The hospital's chief executive officer (CEO) and other senior administrators will need to support the HICS to succeed.
-
3.
It is necessary to allocate adequate financial resources to HICS activities, including emergency staff training.
-
4.
Other requirements of the HICS implementation include its integration into the hospital's existing community-based response.
The emergency management program
A hospital's emergency management program is composed of several critical elements relevant to the four phases of emergency management:
Mitigation, preparedness, response, and recovery
There are several resources a hospital could consult about developing a comprehensive emergency management program. These resources include Emergency Management Principles and Practices for Health Care Systems (2nd Edition), NIMS, National Response Framework (NRF), National Fire Protection Association (NFPA), 1600 Standard on Disaster/Emergency Management, and Business Continuity Programs—2013 Edition, Homeland Security Presidential Directive (HSPD) 5, Presidential Policy Directive (PPD) 8: National Preparedness, and Continuity Guidance Circular 1 (CGC 1): Continuity Guidance for Non-Federal Governments-July 2013. Additionally, one should also consider other appropriate states, local, and non-governmental regulatory and accreditation standards.
The above list provides resources and references that could be useful in developing a comprehensive emergency management program. The US Department of Veterans Affairs created a valuable resource to guide planners called the Emergency Management Program Guidebook [5].
The Veterans Affairs guidance outlines a nine-step process for developing, maintaining, and evaluating a hospital emergency management program. This process includes the following:
-
•
designate an EPM;
-
•
establish the EMC;
-
•
develop the all-hazards emergency operations plan (EOP);
-
•
conduct the HVA;
-
•
develop incident-specific guidance;
-
•
coordinate with external entities;
-
•
train key staff;
-
•
exercise the EOP; and
-
•
conduct program review and evaluation, and plan for and execute improvement processes.
Operationalizing the incident command center
Team assembly and use can relate to operationalizing the incident command center. The hospital incident management team (HIMT) assembly depends on a HICS's primary management components. These are the command, finance, logistics, operations, and planning. Assign members of HIMT with appropriate technical skills tasks depending on the nature and scope of a particular emergency. The HICS describes specific positions for the HIMT, but these are only suggestions, as each particular hospital and incident will determine the optimal team [5].
Procedures for the efficient transfer of command between personnel must be included in the HICS. These are especially important during an emergency, where one with more significant experience or seniority can relieve one personnel. Command transfer should generally involve a transition meeting in which the current commander briefs the replacement on the current situation, including response actions, resources, and external agencies [5].
Incident management team structure
The hospital incident management team (HIMT) plays a central role in implementing the principles of ICS in the hospital setting and assigns specific roles to individual team members to ensure a coordinated response during emergencies. COVID-19 pandemic is a significant public health crisis worldwide in recent times, and it is essential to have a strong team to achieve the goals of HICS. A strong team should also be formed with consideration for personality traits. Emotional intelligence is the ability to be aware of and control one's emotions, and to approach peers and relationships with empathy [26]. This is an overall desirable personality trait, which can be of particular importance in a pandemic or disaster situation [6]. Therefore, personality and the individuals' capacity to express emotional intelligence should be considered while forming the HIMT and selecting key section chiefs.
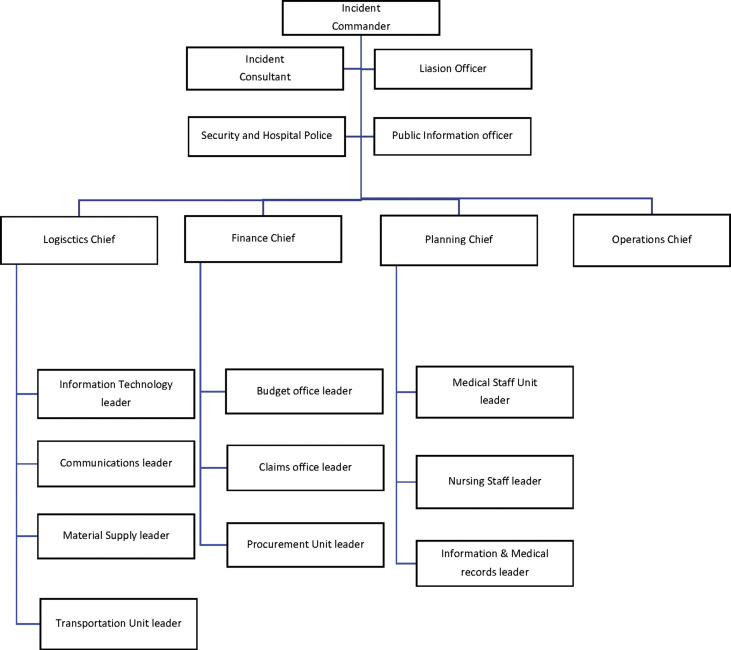
We present a model HIMT structure that can serve as a template, utilizing healthcare staff to effectively address the planning, logistics, clinical operations, and financial needs in hospital settings (Fig. 1 ). Although most of the hospitals might already have some form of ICS [7], COVID-19 crisis is unique in that it is a true pandemic, affecting essentially every single healthcare institution in the world simultaneously, and it certainly requires appropriate modifications to the existing team structure, specifically addressing the overall needs of patients with COVID-19.
Fig. 1.
Subdivisions of hospital incident management team (HIMT).
HIMT consists of command staff and general staff; while the command staff deal with the overall management of the crisis by setting the objectives, strategies, and response priorities, the general staff play an instrumental role in executing the plan.
Command staff
Incident Commander heads the command staff and is usually the most experienced administrator, proficient in tackling healthcare emergencies. During this COVID-19 pandemic era, the hospital administrator is best suited to serve as the Incident Commander.
Liaison Officer serves as a bridge between the internal HIMT and external response partners and is responsible for maintaining updates on the organization's status and bed availability, and also to coordinate with the local or regional Emergency Operations Center as well as other community response partners.
Safety Officer is generally one of the hospital security or police staff who closely works with the local law enforcement agencies to ensure safeguarding the healthcare staff and the facility and to implement safety precautions for everyone.
Public Information Officer plays a vital role in raising the awareness among the public about the COVID-19 disease process and preventive measures.
Incident Consultant provides the expert clinical and technical advice to the Incident Commander, with details specific to the problem such as the current pandemic.
General staff
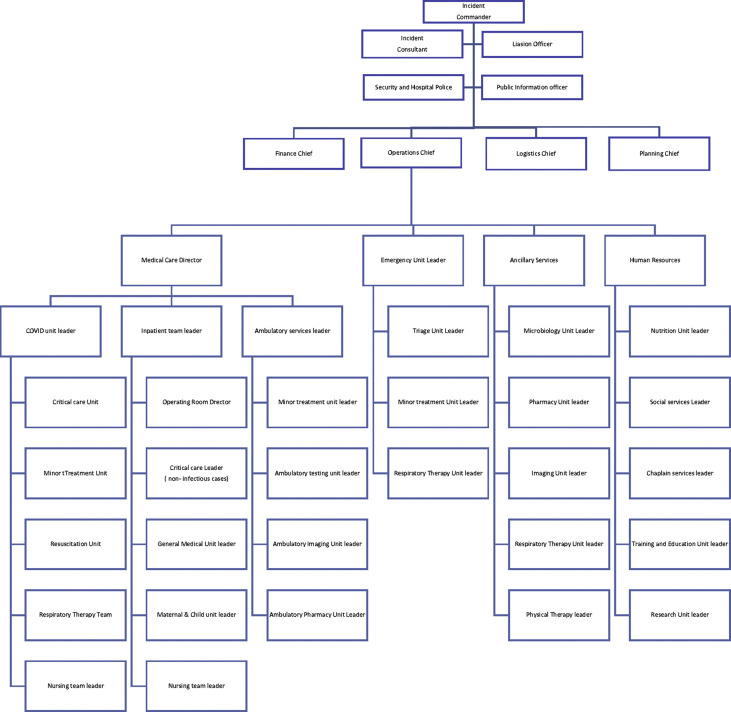
Operations Chief plays a vital role in executing the objectives laid out by the command staff and is capable of handling the increased case load and making sure that all the resources are appropriately allocated. A well-designed multidisciplinary team is essential to effectively treat patients suffering from rapidly spreading infectious disease such as COVID-19 and to ensure that there is no spread among other patients (Fig. 2 ).
Fig. 2.
Structure of hospital incident management team (HIMT) with subdivisions of operations.
Patient care is supervised by a medical staff director and there will be separate leaders for different units such intensive care units (ICUs), general medical floors as well as clinics. A dedicated airway team is usually responsible for emergency airway management, whereas an infectious disease specialist serves as a consultant and subject expert and oversees the microbiology team. Emergency medicine physicians are the first personnel to evaluate patients with COVID-19 coming through ER and will be responsible for stabilizing and assigning the patients to different levels of acuity of care such as medical floors and ICUs. It is a teamwork indeed, and other healthcare staff such as pharmacists, respiratory therapists, physical therapists, social workers, and case managers play a vital role in overall effective management of patients.
Along with the patient care, healthcare facilities should also strive to educate trainees, patients, and general public. Research and development of newer drugs, tests, and vaccines is an important part of effective management of the disease and helps in tackling the disease more efficiently in the future.
The health and well-being of the general and nadir healthcare staff must be preserved for the incident command center to function properly. This is especially important in specific areas of the hospital such as the ICU, where the staff are highly specialized and cannot be immediately replaced. A July 2020 study implemented a pandemic-adjusted staffing model to explore whether staff shortages can be prevented in the event of a pandemic if the shift scheduling is adjusted accordingly [8]. Their suggested model is for each staff member to work 7 days × 12 h/d = 84 h for week one, quarantine week two, and repeat, for a total of 168 h of coverage; 168 h divided by 84 h of coverage per staff member = 2.0 full-time employees per 20 patients during week one; 2.0 × 20 = 40 total staff members for week 1, and a completely separate staff of 40 people for week two, while week one staff is quarantined = 80 staff total. This requires 5% less staffing than the standard work week of 40 h with 2:1 patient-to-staff ratio assumption. This model could be the answer to preserving the vital general and nadir healthcare staff in the event of a pandemic.
Planning Chief is responsible for developing action plans for handling the crisis in general and also for preparing various teams and units of the hospital to tackle the healthcare emergency. The planning team also tracks important briefings, statistics, and future plans related to the pandemic.
Logistics Chief is responsible for procuring the resources for various sections of the hospital, to ensure adequate supply of personal protective equipment (PPE) and surgical supplies to all the healthcare staff and to communicate with external agencies in order to replenish these resources.
Finance Chief is accountable for monitoring the cost related to the given incident while handling accounting, procurement, and cost analyses [9].
Incident response and action planning
Planning an incident response is more of a circular process than linear [3]. There are four fundamental pillars of a pandemic response: surveillance, vaccine, and antiviral drug delivery, emergency response, and communication [10]. Surveillance is the rapid detection of an infection in humans, and it is the cornerstone of the response. This has been recognized since the early stages of state and local planning [11]. Antiviral medications are critical to the pandemic response, especially when there is no vaccine available or a vaccine is in low supply. The next pillar exhibits the need for the emergency response staff and public health authorities' interconnectedness to develop and put into action the response plan. The last pillar is communication, highlighting the need for timely, transparent, and proactive communication in an outbreak's early stage. This is especially important when the demand for information for general guidance is high.
Incident planning and documentation
Incident planning primarily consists of identifying a method of prevention to stop the incident from occurring on a large scale in the first place. Concerning the Avian flu of 2009, the world was ill-prepared to face an influenza pandemic [12]. Afterward, several essential practices were identified and included stockpiling vaccines and antivirals and taking effective control measures to stop spreading the virus at its source [12]. There are key objectives in the response planning process which are: 1) to identify, triage, isolate, and treat infectious individuals, 2) protect patients and staff from exposure, 3) assure both safety of patients and staff, and 4) admit a large number of contagious patients while protecting the patients who are not infected [13].
Documentation of the process seemingly relies on a series of checklists to ensure that no steps or essential personnel are missed to implement the incident planning or action process. In a process detailed by the EMSA, the incident planning process should also address mitigation, preparedness, immediate and intermediate responses, and extended response and system recovery. Mitigation covers if the hospital uses expert information sources, provides that information to the staff, and participates in pre-incident local response planning with public safety officials. Preparedness details things such as if the hospital has an infectious disease plan, whether this plan is exercised yearly and revised as needed, and whether the hospital has a plan to obtain and dispense vaccines and medicines to the public.
Immediate and intermediate responses cover if the hospital has a policy to monitor the health status and absenteeism of the staff during the incident, if there is a plan to track emergency department, inpatient, and clinic census and symptoms, and if there is a trigger to implement the infectious disease plan. It also covers plans to keep the hospital safe, deciding on triage locations and the ingress and egress routes for emergency medical services providers and procedures to receive information about area hospitals' status. Extended response and system recovery cover what criteria would be needed to restore the hospital operations to normal, criteria to prioritize business continuity and recovery activities, including repair and disinfection of the hospital. Does the hospital have a continuous process to capture all costs and expenditures related to the incident?
Assessment
Assessment of the incident response plan is critical to ensure success in the future. Plans should be assessed and implemented yearly with revisions when necessary [13]. This process looks at the weakness, and the missed opportunities or near misses during the response process. An example in literature is seen when researchers were assessing a cholera outbreak in Africa. Looking back at the response process, they found the areas that needed improvement included The authors found that there was inadequate community-based surveillance data available, resulting in late reporting of deaths, and there was inadequate community knowledge about prevention measures [15]. Assessment can also take part while the plan is being developed. A study looking at pandemic flu prevention in Southeast Asia assessed the effectiveness of specific interventions. They looked at antiviral prophylaxis, which should be able to eliminate a pandemic virus. Still, they found that this policy would require enough drugs to give to everyone for up to three weeks and found it unfeasible [16]. Assessment of these incident response plans will provide the implementer an idea of if it would be possible for future use.
Incident action plan
According to the US Department of Health and Human Services, an incident action plan is one that designed “to protect the facility, personnel, and non-incident patients from the effects of the hazard (i.e., infectious disease) while providing optimal care to incident victims and maintaining normal medical operations” [17]. The ultimate goal is to ensure the staff's safety, non-infected public, and treatment of those infected. This type of planning is essential for a successful recovery from an incident [3]. It should consider where the response system wants to be at the end of the response [17]. The incident action plan is usually the planning section chief's responsibility, part of the incident command system [18]. The planning section chief develops the incident action plan at a planning meeting, where the purpose is to gain concurrence of all participating parties for the next stage of the response process.
Finance/administration
The backbone of a properly functioning ICS is an incident commander. The incident commander should be the staff member with the most experience, a wide range of knowledge, and many connections within their given community [20]. Unfortunately, COVID-19 has caused significant emotional and economic damage to millions of people worldwide and is a strong reason for the need for implementation of a well-designed ICS. During the coronavirus pandemic, many issues centered around the lack of and procurement of PPE for front-line healthcare workers. Hospitals were faced with having to deal with furloughed workers while others were working around the clock, almost non-stop. The finance and administration section chief is a highly trained individual poised to handle all things related to dealing with costs in emergencies such as the global pandemic caused by coronavirus. The financial and administration section chief (FASC) is prepared for a wide variety of needs and situations, such as the need for more operating rooms and staff or the need for more critical care and medical floor staff or both. The FASC must quickly analyze the situation so they can develop a strategy for their team as to how to proceed [21].
Hospital incident command systems (HICS) have multiple section chiefs, each with separate duties and responsibilities, all reporting back to the incident commander. The FASC is responsible for all financial, administrative, and cost analysis regarding the incident according to the FEMA definition in National Qualification System Emergency Management [21]. The FASC is responsible for monitoring personnel time, negotiating and monitoring of contracts, cost analysis, and completing necessary reimbursement documentation related to injury and damage to property/fatalities. The Robert T. Stafford Disaster Relief and Emergency Assistance Act, known as the “Stafford Act,” for reimbursement of eligible emergency protective measures to be taken during an emergency under Category B of FEMA's Public Assistance Program [22]. All costs associated with the response to the incident must be recorded from the beginning of the incident to be eligible. The FASC must be aware of state and federal reporting requirements for emergencies. State requirements may suffice as they take responsibility for reporting to the federal government [23,24].
The FASC must have four competent and experienced staff members to work for them as their unit leaders. Each unit leader oversees one of the four core tasks the FASC must accomplish and reports back to them. The time unit leader is responsible for coordinating and recording personnel time. This could prove challenging in scenarios such as the shootings in Orlando and Las Vegas where “all hands-on deck” were needed or if outside staff are brought in to respond to a large incident, everyone's times must be recorded in order for proper reimbursement. The procurement unit leader initiates contracts and orders items through existing contracts and connections. In events such as coronavirus, the procurement leader must have good connections to be able to move swiftly and quickly to procure PPE for staff and ventilators for patients. The compensation/claims unit leader arranges for personnel-related payments and worker's compensation. They depend upon the time unit leader for accurate time reporting, so personnel can get adequately paid for their workload during a response. Lastly, the cost unit leader tracks all costs from the response and recovery and completes payment of invoices. FASCs should also consider resource allocation and adapt an ICS for active shooters within the hospital such that the delivery of proper anesthesia and surgical care can continue [25].
Summary
Incident command centers are a culmination of people tasked with managing and averting crises during emergency and non-emergency situations. Their responsibility involves handling various sources of danger or threats and preventing further damages from occurring. The HICS guidebook is embraced by the FEMA and hospital systems throughout the country and involves instructions for how to reduce damage, planning, and responses, and how to recover from a disaster. Within an incident management team at a hospital, there are multiple section chiefs. Each section chief has separate duties and responsibilities, all reporting back to the incident commander. The incident commander acts as a chief and backbone to the organizational process across all subunits. An incident response is not an individual or direct act, but involves closed-loop feedback, which allows for evaluating the effectiveness of that response. Proper documentation is an important means of effective communication during an incident as it logs the process in trial. Further assessment of the situation and response is necessary to ensure it is avoided and prevented in the future. As some disasters are unavoidable, a strong plan is essential for ultimate alleviation of the emergency or non-emergency with simultaneous successful recovery. These concepts are the framework for creating an incident command center.
Conclusion
Planning for an incident command center is a necessary process that can prevent chaos in the event of a disaster or pandemic. Overall, the selection of key leaders to be section chiefs is of critical importance to the success of the incident command center. Each section chief must accept their authority, responsibility, and the demands that will be called upon them as they will guide and motivate the people within their sections. Lastly, proper documentation, paperwork, and record keeping are also necessary for the success of the command center. These two key components are the pillars of a successful incident command center.
Practice points.
-
•
The Hospital Incident Command System (HICS) is an incident management system specific to hospitals based on the principles of Incident Command System (ICS) and includes prevention, protection, mitigation, response, and recovery.
-
•
HICS plays a crucial role in effective and timely response during the periods of disasters, mass casualties, and public health emergencies.
-
•
The current COVID-19 pandemic has placed unprecedented challenges on the healthcare system, necessitating the creation of HICS that can help in the proper allocation of resources and ineffective utilization of healthcare personnel.
-
•
The key elements in managing a response to this pandemic include screening and early diagnosis, quarantining affected individuals, monitoring disease progression, delivering appropriate treatment, and ensuring an adequate supply of personal protective equipment (PPE) to healthcare staff.
Research agenda.
-
•
Understand the ideal makeup of the incident management team at a hospital.
-
•
The importance of the incident response as a closed-loop feedback, which allows for evaluating the effectiveness of that response.
-
•
Better ways to perform assessment of the situation and response to ensure it is avoided and prevented in the future.
-
•
As some disasters are unavoidable, a strong plan is essential for ultimate alleviation of the emergency or non-emergency with simultaneous successful recovery.
-
•
Components of an ideal framework for creating an incident command center.
Conflict of interest
Richard D. Urman reports research or fees from Merck, Medtronic/Coviden, AcelRx, Pfizer, Heron and Takeda. Alan D. Kaye reports fees from Merck. Other authors report no conflicts of interest.
Acknowledgements
None.
References
- 1.Gossman W., Khetarpal S., Furin M., et al. StatPearls Publishing; 2020. EMS, Incident Command System (ICS). StatPearls. [PubMed] [Google Scholar]
- 2.FEMA. NIMS components - guidance and tools. Last updated July 20, 2020. Available at: https://www.fema.gov/emergency-managers/nims/components. Accessed November 25, 2020.
- 3.Strawser B. An overview of the Hospital Incident Command System (HICS). Bryghtpath. https://bryghtpath.com/an-overview-of-the-hospital-incident-command-system-hics/ Available at.
- 4.California Emergency Medical Services Authority. Hospital Incident Command System – current guidebook and appendices EMSA. [Internet] https://emsa.ca.gov/disaster-medical-services-division-hospital-incident-command-system/ Updated May 2016. Available from:
- 5.California emergency medical services authority guidebook. 2014. [Google Scholar]
- 6.Luedi M.M., Doll D., Boggs S.D., et al. Successful personalities in anesthesiology and acute care medicine: are we selecting, training, and supporting the best? Anesth Analg. 2017 Jan 1;124(1):359–361. doi: 10.1213/ANE.0000000000001714. https://pubmed.ncbi.nlm.nih.gov/27861434/ [Internet] [cited 2020 Nov 7]. Available from: [DOI] [PubMed] [Google Scholar]
- 7.Arnold J.L., Dembry L.M., Tsai M.C., et al. Recommended modifications and applications of the hospital emergency incident command system for hospital emergency management. Prehospital Disaster Med. 2005;20(5):290–300. doi: 10.1017/s1049023x00002740. [DOI] [PubMed] [Google Scholar]
- 8.Mascha E.J., Schober P., Schefold J.C., et al. Staffing with disease-based epidemiologic indices may reduce shortage of intensive care unit staff during the COVID-19 pandemic. Anesth Analg. 2020 Jul 7;131(1):24–30. doi: 10.1213/ANE.0000000000004849. https://journals.lww.com/10.1213/ANE.0000000000004849 [Internet] [cited 2020 Nov 6]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Louisiana State University Health Sciences Center-Shreveport. Emergency operations plan, LSUHSC-Shreveport. https://www.yumpu.com/en/document/view/37388046/emergency-operations-plan-inside-myhsc Revised March 2011. Available from:
- 10.Iskander J., Strikas R.A., Gensheimer K.F., et al. Pandemic influenza planning, United States, 1978-2008. Emerg Infect Dis. 2013 Jun;19(6):879–885. doi: 10.3201/eid1906.121478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gensheimer K.F., Fukuda K., Brammer L., et al. Emerging infectious diseases. vol. 5. Centers for Disease Control and Prevention (CDC); 1999. Preparing for pandemic influenza: the need for enhanced surveillance; pp. 297–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perez D.R., Sorrell E.M., Donis R.O. Avian influenza. Pediatr Infect Dis J. 2005 Nov;24(Supplement):S208–S216. doi: 10.1097/01.inf.0000188160.83709.b7. [DOI] [PubMed] [Google Scholar]
- 13.California Emergency Medical Services Authority Incident response guide-infectious disease incident response guide: infectious disease. https://emsa.ca.gov/wp-content/uploads/sites/71/2017/07/Infectious-Disease-IRG.pdf Available from. Published July 2017.
- 15.Ohene S.A., Klenyuie W., Sarpeh M. Assessment of the response to cholera outbreaks in two districts in Ghana. Infect Dis Poverty. 2016 Nov;5(1) doi: 10.1186/s40249-016-0192-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferguson N.M., Cummings D.A.T., Cauchemez S., et al. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature. 2005 Sep;437(7056):209–214. doi: 10.1038/nature04017. [DOI] [PubMed] [Google Scholar]
- 17.Public Health Emergency (PHE) What is an incident action plan? https://www.phe.gov/Preparedness/planning/mscc/handbook/Pages/appendixc.aspx Last updated February 14, 2012. Available at:
- 18.Health and Human Services Understanding the hospital incident command system (ICS) module 2. https://files.asprtracie.hhs.gov/documents/epimn-module-2-understanding-hospital-ics.pdf Available from:
- 20.Jensen J., Thompson S. The incident command system: a literature review. Disasters. 2016 Jan 1;40(1):158–182. doi: 10.1111/disa.12135. https://pubmed.ncbi.nlm.nih.gov/26271932/ [Internet] [cited 2020 Oct 9]. Available from: [DOI] [PubMed] [Google Scholar]
- 21.FEMA. Federal Emergency Management Agency . National incident management system. 3rd ed. 2017. [Google Scholar]
- 22.FEMA . 2020. Eligible emergency protective measures; p. 1.https://www.fema.gov/fact-sheet/eligible-emergency-protective-measures [Internet] Available from: [Google Scholar]
- 23.EMSA . 2014. California emergency medical services authority guidebook. [Google Scholar]
- 24.NABH . 2020. COVID-19 guidance for hospital reporting and FAQs for hospitals, hospital laboratory, and acute care facility data reporting. [Google Scholar]
- 25.Leppert J.T., Wren S.M., Bergman J. Operating room preparedness for active shooter events. Surg (United States). 2020 Feb 1;167(2):510–511. doi: 10.1016/j.surg.2019.08.009. [DOI] [PubMed] [Google Scholar]
- 26.Chang B.P., Vacanti J.C., Michaud Y., Flanagan H., Urman R.D. Emotional intelligence in the operating room: analysis from the Boston Marathon bombing. Am J Disaster Med. 2014;9(2):77–85. doi: 10.5055/ajdm.2014.0144. [DOI] [PubMed] [Google Scholar]