Abstract
Patient: Female, 1-month-old
Final Diagnosis: Intussusception
Symptoms: Rectal bleeding
Medication: —
Clinical Procedure: Ultrasonography
Specialty: Pediatrics and Neonatology
Objective:
Challenging differential diagnosis
Background:
Intussusception is the most common cause of intestinal obstruction in children, with a peak incidence usually before the second year of age, while in neonates it is a rare entity.
We describe a delayed and incidental diagnosis of neonatal intussusception secondary to Meckel’s diverticulum in a neonate with shaken baby syndrome (SBS). This is, to the best of our knowledge, the first reported case of a neonatal intussusception with a Meckel’s diverticulum as a lead point in a neurologically impaired child.
Case Report:
A term baby presented at 22 days of age at our Emergency Department in severe conditions due to a suspected SBS. Eight days following hospitalization in the Intensive Care Unit, an isolated episode of rectal bleeding occurred, without any worsening of general conditions or abdominal distension.
The ultrasonography showed a “doughnut sign” with high suspicion of ileocecal intussusception.
A rectal barium contrast enema was performed but was not resolutive. At exploratory laparotomy an ileocecal intussusception with Meckel’s diverticulum acting as a lead point was identified and an intestinal resection was needed due to the ischemic condition of the ileum.
The post-operative course was uneventful and the baby recovered well; the residual neurological impairment needed long-term follow-up.
Conclusions:
Intussusception is a rare entity in neonates and, when severe neurological impairment is present, the diagnosis can be missed because of the compromised condition of the baby and the paucity of gastrointestinal manifestations. In addition, due to the high incidence of lead point in neonatal cases, we recommend reserving non-operative treatment only for selected cases.
Keywords: Intussusception, Meckel Diverticulum, Shaken Baby Syndrome
Background
Intussusception is the most common cause of intestinal obstruction in children, with a peak incidence usually before the second year of age, while in neonates it is a much rarer entity.
We describe a delayed and incidental diagnosis of neonatal intussusception secondary to Meckel’s diverticulum in shaken baby syndrome (SBS). This is, to the best of our knowledge, the first reported case of a neonatal intussusception with a Meckel’s diverticulum as a lead point in a neurologically impaired child.
Case Report
A term female infant presented at 22 days of age at our Emergency Department in severe condition due to suspected SBS. At admission, the patient was dyspneic and unresponsive; she was immediately intubated and transferred to the Pediatric Intensive Care Unit. A total-body ultrasound survey, mainly focused on the brain, lungs, and abdomen, was performed and excluded injuries to parenchymatous organs, except for the right adrenal gland, which appeared enlarged and inhomogeneous.
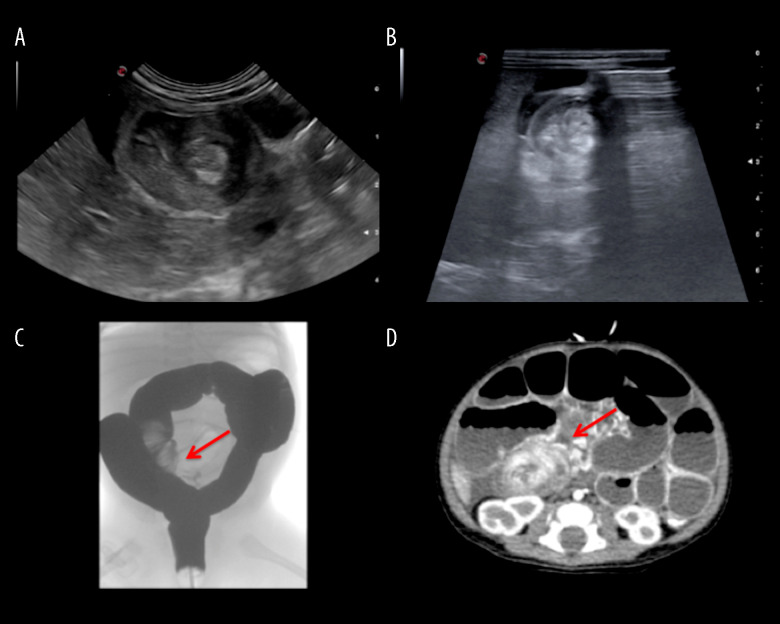
Eight days after hospitalization, a rectal stimulation was performed because of persistent constipation for 4 days, considered secondary to the neurological impairment and to sedation with intravenous benzodiazepine. During the procedure, a sudden and isolated episode of rectal bleeding occurred, without any worsening of general condition or abdominal distension. No signs of pneumoperitoneum or air-fluid levels were shown in the plain abdominal film, while the ultrasonography showed a “doughnut sign” with high suspicion of ileocecal intussusception (Figure 1A, 1B). Immediately, a rectal barium contrast enema was performed: during the exam, the liquid contrast identified a minus image localized in the right inferior abdominal quadrant suggesting an ileocecal intussusception (Figure 1C). Despite the presence of contrast within the appendix, due to uncertainty about the efficacy of non-operative management and to further investigate possible abdominal conditions, we decided to perform an abdominal CT scan, which showed persistent intussusception (Figure 1D).
Figure 1.
(A, B) Abdominal ultrasound showing a “doughnut sign” typical of ileocecal intussusception. (C) Rectal barium contrast enema with the liquid contrast identifying a minus image localized in the right inferior abdominal quadrant, suggesting an ileocecal intussusception. (D) Abdominal CT scan showing persistent intussusception.
Exploratory laparotomy was planned. Intraoperatively, ileocecal intussusception with Meckel’s diverticulum acting as a lead point was identified (Figure 2). The intussusception was manually reduced, a 15-cm segment of ischemic small bowel, including the Meckel diverticulum, was resected with preservation of the ileocecal valve, and an ileo-ileal anastomosis was performed.
Figure 2.
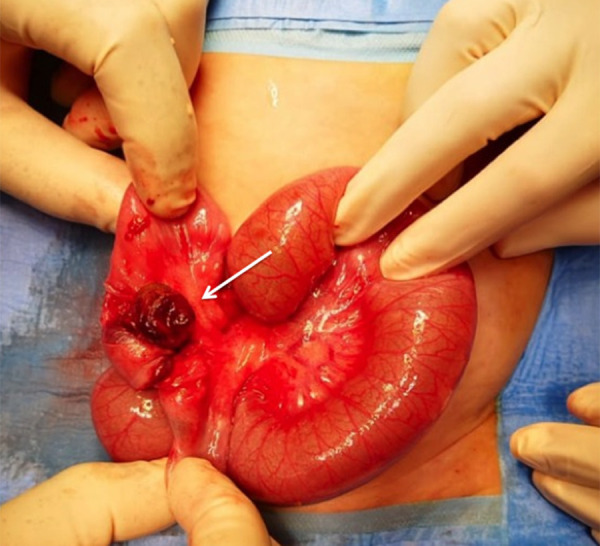
Intra-operative appearance of the ileocecal intussusception with Meckel’s diverticulum acting as a lead point.
Discussion
Intussusception is the most common cause of intestinal obstruction in children, with a peak incidence usually before the second year of age [1]. In neonates it is a much rarer entity, with an incidence of about 1 case per 6000 [2]. During an intussusception, a proximal portion of bowel pushes inside the adjacent distal segment, leading to intestinal obstruction and, eventually, vascular ischemia and necrosis [1]. The etiology is often unknown, but in 10% of cases an anatomic lead point that predispose to the intussusception can be identified [2]. The etiology of neonatal intussusception presents differences between full-term and premature infants: in full-term babies it is often associated with the presence of a lead point [3], the most common being Meckel diverticulum, followed by polyps or duplications [4], a malignancy is rarely detected. However, it has been hypothesized that perinatal risk of intestinal hypoperfusion/hypoxia and dysmotility can act as a lead point for intussusception in premature infants [5].
About 90% of pediatric intussusceptions are located in the ileocolic region [1]. Classic manifestations of intussusception in children include crampy abdominal pain, usually accompanied by rectal bleeding, “red currant jelly” stool, lethargy, and presence of a palpable mass in the right lower abdominal quadrant [5]. Neonates with intussusception often manifest with non-specific symptoms, such as unstable general condition, abdominal distension, and haematochezia, more suggestive of other abdominal conditions such as necrotizing enterocolitis [6]. The atypical presentation may lead to a delay in the diagnosis and treatment, requiring operative management with extended bowel resection during surgery.
In our case, intussusception was diagnosed incidentally in a patient with severe neurological impairment due to SBS brain injury. The abdominal clinical picture was non-specific and shaded by the neurological impairment with no worsening of general conditions, scanty abdominal symptoms, and rectal bleeding only after stimulation. As the initial management consisted of support of vital conditions following SBS, we could not establish the exact timing of the intussusception; we might even suppose that the intussusception presented with classical signs of irritability and abdominal pain and it might have been the trigger for SBS.
Early management, either radiological or surgical, is mandatory to prevent bowel necrosis. A rectal contrast enema is the treatment of choice, but this is usually avoided in neonates because of the high vulnerability of the intestine to perforation and the high incidence of failure of non-operative treatment due to the delay in the diagnosis or the presence of a lead point. As a consequence, in neonates, surgical treatment in often considered the safest option [7]. In our case, despite an initial trial of non-operative management, we ended up performing a laparotomy and bowel resection.
Conclusions
Intussusception is a rare entity in neonates and, when severe neurological impairment is present, the diagnosis can be missed because of the compromised condition of the baby and the paucity of gastrointestinal manifestations. In addition, due to the high incidence of a lead point in neonatal cases, we recommend reserving non-operative treatment for selected cases, while surgery must be considered mandatory to identify the presence of the lead points and to evaluate the involved intestine.
Ethics approval
All procedures performed in this study were in accordance with the ethics standards of the Institutional and National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethics standards.
Abbreviations:
- SBS
shaken baby syndrome
Footnotes
Conflict of Interest
None declared.
Declaration of Figures Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1.Gluckman S, Karpelowsky J, Webster A, McGee RG. Management for intus-susception in children. Cochrane Database Syst Rev. 2017;6(6):CD006476. doi: 10.1002/14651858.CD006476.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Loukas M, Pellerin M, Kimball Z, et al. Intussusception: An anatomical perspective with review of the literature. Clin Anat. 2011;24(5):552–61. doi: 10.1002/ca.21099. [DOI] [PubMed] [Google Scholar]
- 3.Loukas I, Baltogiannis N, Plataras C, et al. Intussusception in a premature neonate: A rare often misdiagnosed cause of intestinal obstruction. Case Rep Med. 2009;2009:607989. doi: 10.1155/2009/607989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Samad L, Marven S, Bashir H, et al. Prospective surveillance study of the management of intussusception in UK and Irish infants. Br J Surg. 2012;99(3):411–15. doi: 10.1002/bjs.7821. [DOI] [PubMed] [Google Scholar]
- 5.Slam K, Teitelbaum D. Multiple sequential intussusceptions causing bowel obstruction in a preterm neonate. J Pediatr Surg. 2007;42(7):1279–81. doi: 10.1016/j.jpedsurg.2007.02.028. [DOI] [PubMed] [Google Scholar]
- 6.Raza HA, Basamad MS, El Komy MS, et al. Diagnosing intussusception in pre-term neonates: Case report and overview. J Clin Neonatol. 2014;3(2):103–5. doi: 10.4103/2249-4847.134696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keese D, Rolle U, Gfroerer S, Fiegel H. Symptomatic Meckel’s diverticulum in pediatric patients – case reports and systematic review of the literature. Front Pediatr. 2019;7:267. doi: 10.3389/fped.2019.00267. [DOI] [PMC free article] [PubMed] [Google Scholar]