Supplemental Digital Content is available in the text.
Key Words: rural, health care access, disparities, geography
Abstract
Background:
The federal government uses multiple definitions for identifying rural communities based on various geographies and different elements of rurality.
Objectives:
The objectives of this study were to: (1) assess the degree to which rural definitions identify the same areas as rural; and (2) assess rural-urban disparities identified by each definition across socioeconomic, demographic, and health access and outcome measures.
Research Design:
We determined the rural status of each census tract and calculated the rural-urban disparity resulting from each definition, as well as across the number of definitions in which tracts were designated as rural (rurality agreement).
Subjects:
The population in 72,506 census tracts.
Measures:
We used 8 federal rural definitions. Population characteristics included percent with a bachelor’s degree, income below 200% poverty, population density, percent with health insurance and whether various health care services were within 30 minutes driving time of the tract centroid.
Results:
The rural population varied from slightly < 6.9 million people to >75.5 million across definitions. The largest rural-urban disparities were found using Urban Influence Codes. Urbanized Area and Urbanized Cluster tended to generate smaller disparities. Population characteristics such as population density and percent White had notable discontinuities across levels of rurality, while others such as percent with a bachelor’s degree and income below 200% poverty varied continuously.
Conclusions:
Rural-urban populations and disparities were sensitive to the specific definition and the relative strength of definitions varied across population characteristics. Researchers and policymakers should carefully consider the choice of outcome and region when deciding the most appropriate rural definition.
Roughly 20% of Americans live in a rural area according to some estimates.1 On most dimensions, health outcomes for rural populations lag those of Americans living in urban areas.2 For some of these outcomes, for example, mortality, the gap has grown over time, especially in the last 2 decades.3 Recently, a number of policies and initiatives have been developed that aim to address these disparities. While the causes of these disparities are multidimensional, variation in health care provider supply is often identified as paramount.4 Physician supply is lower in rural areas, and previous research has demonstrated the link between primary care supply and mortality.5 Access to most types of health care is lower in rural areas; rural residents live further from their closest hospital, and the increasing rate of rural hospital closures has been shown to affect intermediate outcomes such as travel time to emergency services, as well as key health outcomes.6–8
A fundamental challenge to policymaking and interventions designed to mitigate rural-urban disparities lies in the ambiguity of which areas and populations should be considered as rural. Previous research has documented these types of challenges.9–11 Some innovative approaches have been designed to acknowledge the multidimensional nature of rurality.12,13
The presence of various rural definitions complicates research into rural-urban disparities and subsequent efforts to address underlying factors. For example, poverty rates are higher in urban areas when using the US Census Bureau’s Urbanized Areas and Urbanized Clusters definition, but are lower in urban areas when using most other measures of rurality.14 Meanwhile, eligibility for planning efforts to increase rural residency programs were based on the Health Resources and Services Administration’s (HRSA) definition of rurality, despite evidence that long-term financial sustainability is likely largely determined by the Centers for Medicare and Medicaid Services’ (CMS) definition. Although some issues of these definitions are fundamental—should a provider’s “rurality” be based on its facility location or on the population it serves?—others stem from the multitude of rurality definitions that have propagated throughout the federal government, as well as numerous state-specific and local definitions.
Differences in rural definitions largely stem from different visions of what it means to be “rural,” which include a multitude of conceptualizations including proximity to an urbanized core, “connectedness” to a core (largely measured via commuting patterns), population density, population size, or the sharing of a political border (eg, county) with an “urban area.” In practice, the relationship between these various measures of rurality and key community measures will vary; for example, there may be a steeper gradient in the relative supply of subspecialists and high complexity services across rurality than for primary care supply. Likewise, different notions of rurality may better explain differences in access to high acuity/occasional services (eg, chemotherapy or hip replacement) than for repeated visits (eg, radiation therapy).
These issues also have implications for rural-urban equity in the health workforce. Fundamentally, efforts to increase workforce supply in rural areas must start with the baseline question of “how are we defining rural?” For example, current methods of capturing underserved (rural) populations—specifically Health Professional Shortage Areas (HPSAs)—may be insufficient for identifying the most underserved populations. There is interest in how well HPSA designations align with measures of health as well as evidence that regional variations may be strong.15
In this manuscript, we consider 8 of the most common definitions of rurality used by the federal government and evaluate differences in socioeconomic and demographic characteristics, health care access, and health outcome across these various measures of rurality. Specifically, we ask:
To what extent do commonly used federal definitions of rurality agree? How much overlap is there in the population they designate as “rural”?
How do population characteristics vary across the definitions of rurality?
METHODS
Rural Definitions
We considered 8 key federal rural definitions. Four definitions from the US Department of Agriculture’s (USDA) Economic Research Service were used, including Rural-Urban Commuting Areas (RUCAs), Rural Continuum Codes (RCCs), Urban Influence Codes (UICs), and Frontier and Remote (FAR) Access Codes. The 4 others included definitions from the Federal Office of Rural Health Policy at the HRSA, the National Center for Health Statistics at the Centers for Disease Control and Prevention (CDC), Core-Based Statistical Areas (CBSAs) from the Office of Management and Budget and Urban Areas/Urban Clusters (UA/UCs) as defined by the Census Bureau. While many of the definitions are related, they have important variations. For example, UICs can be collapsed into the metropolitan/micropolitan/noncore taxonomy used by CBSA, but further delineates counties by their contiguity to other county types and population size.16 Figure 1 shows several key properties of the 8 definitions and the connections between them, for example, RUCAs, CBSAs, and UA/UCs all derive their definitions directly from decennial census data, while the other 5 definitions use these 3 as the foundation for their own versions. All 4 definitions from the USDA Economic Research Service are “multilevel”—that is, they include between 4 and 12 levels of rurality, spanning between concentrated metro areas and sparsely populated rural areas. The base geographic units also vary among definitions, with some utilizing census-based geographies of tracts or counties, while others are variable or independent of administrative boundaries (ie, ZIP codes). More information about each definition and the agencies that produce them is provided in Supplementary Table (Supplemental Digital Content 1, http://links.lww.com/MLR/C307).
FIGURE 1.
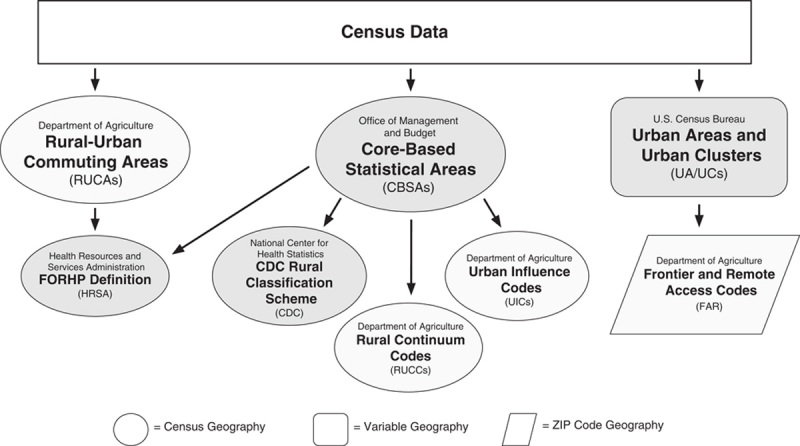
Flow of information for 8 federal rural definitions. CDC indicates Centers for Disease Control and Prevention. Light shading indicates a multilevel definition. Dark shading indicates a dichotomous definition.
Data Sources and Preprocessing
We constructed dichotomous (rural or urban) tract-level spatial data layers for each rural definition. This process was broken into 2 general steps: (1) creating a dichotomous representation of the definitions with a multilevel classification scheme; and (2) using a Geographic Information System (GIS) to assign rural or urban status to census tracts for definitions that were not based on standard census geography.
The HRSA, CDC, UA/UC, and CBSA all use a dichotomous rural and urban classification, thus no reclassification was necessary. For the FAR definition, any region in 1 of the 4 FAR categories was considered rural. The 3 remaining definitions (RUCAs, RCCs, and UICs) contained between 9 and 12 levels of rurality. We identified any regions with a RUCA code ≥4 as rural, a commonly used cutoff point in rural health literature.11 The rural-urban cutoff points for RCCs (≥7) and UICs (≥9) were based on recent research considering the alignment of HPSAs with other indicators of social determinants and rurality.15 As such, we are not, strictly speaking, assessing each definition as it exists but of elements of it. That is, many of the schemes use metropolitan status as one aspect of the definition. We are examining finer elements of the definitions (eg, UIC). For more information for each definition and the preprocessing performed, see Supplementary Table (Supplemental Digital Content 1, http://links.lww.com/MLR/C307).
The RUCA and HRSA definitions use census tracts as the underlying geographic unit, so no processing was necessary. Since the CDC, RCC, and UICs definitions use counties as the underlying unit, tracts were assigned a rural status based on the county they are located within (tracts nest perfectly inside counties). For the CBSA, UA/UC, and FAR definitions, tracts were assigned a rural status by evaluating whether its population-weighted centroid was located inside a rural region using a GIS overlay operation. Because CBSAs are counties or collections of counties, tracts nest perfectly inside them. For the UA/UC and FAR definitions, some tracts were split between urban and rural regions. Assigning an entire tract’s urban or rural status based on whether its population-weighted centroid fell inside of the rural area surely resulted in some misclassification; however, there was no reason to suspect this would lead to any bias in the estimates for these 2 definitions, as the misclassifications could only occur near the urban/rural boundary and would include both errors of omission and commission.
We gathered tract-level population characteristics from 2010 decennial census data from the Census Bureau, 2014–2018 5-year American Community Survey (ACS) population estimates from the IPUMS NHGIS and Social Explorer, the Provider of Services file (hospitals), and the National Plan and Provider Enumeration System (physicians and dentists) files from CMS. Tract-level health outcomes data were gathered from PolicyMap, which uses data from numerous sources to estimate the prevalence of chronic disease in the adult (18+ y) population.17 We evaluated asthma, diabetes, heart disease, and depression prevalence to capture the most prevalent chronic diseases that may drive people to seek care.18 While these data on health outcomes are only estimates, we sought to utilize publicly available datasets at the most granular level possible that would be commonly used by public health officials in local, rural contexts.
Analysis
First, we calculated the number of people identified as rural in each definition. We evaluated agreement among definitions by calculating the percent of each definition’s rural population identified as rural in the other definitions. We examined differences between the rural and urban populations of each definition by comparing population totals, density, and change (from 2010 to 2018); demographic characteristics including percent of the population that are (non-Hispanic) White, Black, American Indian and Alaska Native, Asian, and Hispanic, as well as age 65 years and older; socioeconomic characteristics including percent of the population with a bachelor’s degree and living in a household making < 200% of the federal poverty level; health care access variables including percent of the age 0–64 population with health insurance and percent of the population with 30-minute travel time access to a primary care provider, dentist, acute care hospital, hospital with at least 100 beds, and hospital with an operating room; and health outcome measures including the percent of the adult population (age 18+) with asthma, diabetes, heart disease, and depression. For the health access measures, we identified whether each tract has access within a 30-minute drive time from the population-weighted centroid of the tract using ESRI’s online network analysis API; tract population-weighted centroids were located using the 2010 census block populations.19 For each characteristic, we calculated the difference between the urban and rural populations.
To further evaluate the agreement among rural definitions, we summed the 8 tract-level dichotomous rural layers. As such, each tract could have a value ranging from 0 (not identified as rural in any of the definitions) to 8 (identified as rural in every definition), which we refer to as the “rurality agreement.” This measure does not represent a truly continuous scale but the number of rural definitions applying to a specific tract, thus can be conceptualized as agreement among definitions, not intensity of rurality. We aggregated each of the population characteristics across levels of rurality agreement.
RESULTS
The number of people identified as rural varied from slightly < 6.9 million in the UIC definition to slightly >75.5 million in the CDC definition (Table 1). Table 1 also contains the amount of agreement among the definitions such that each row contains the percent of agreement based on the row’s definition. For example, if considering the rural population identified by HRSA as the base, the CDC definition identified 86.6% of the same people as rural, while the RCC definition only identified 22.6%. The table is not symmetric, as definitions with smaller rural populations generally identified a much lower percent of definitions with larger rural populations; for example, HRSA has 100% overlap with UIC (ie, every tract designated as rural under UIC is also designated as rural under HRSA), but UIC only captures 12.1% of HRSA’s rural population). Notable results include the relatively low agreement (<60%) between the 2 definitions identifying the largest rural populations (CDC and UA/UC) and the high agreement (>80%) between some of the broader definitions (eg, HRSA, CDC, and RUCA).
TABLE 1.
Rural Population Totals and Agreement (%) Among Definitions
| Definition | Population | HRSA | CDC | RUCA | RCC | UIC | UA/UC | CBSA | FAR |
|---|---|---|---|---|---|---|---|---|---|
| HRSA | 56,860,884 | 100 | 86.6 | 89.4 | 22.6 | 12.1 | 63.5 | 31.5 | 21.1 |
| CDC | 75,517,281 | 65.2 | 100 | 57.5 | 17.0 | 9.1 | 54.1 | 23.6 | 15.6 |
| RUCA | 50,827,445 | 100 | 85.5 | 100 | 23.8 | 13.3 | 60.6 | 30.1 | 23.4 |
| RCC | 12,839,851 | 100 | 100 | 94.2 | 100 | 53.7 | 78.2 | 66.6 | 55.7 |
| UIC | 6,897,898 | 100 | 100 | 98.3 | 100 | 100 | 79.2 | 95.9 | 66.2 |
| UA/UC | 73,256,242 | 49.3 | 55.8 | 42.0 | 13.7 | 7.5 | 100 | 20.0 | 10.8 |
| CBSA | 18,209,930 | 98.4 | 97.9 | 83.9 | 47.0 | 36.3 | 80.4 | 100 | 28.2 |
| FAR | 11,977,592 | 100 | 98.4 | 99.1 | 59.7 | 38.1 | 65.8 | 42.8 | 100 |
The rows are used as the “base” population for calculating agreement, for example, 86.6% of the rural population identified by the HRSA definition was also identified in the CDC definition, while 65.2% of the rural population identified by the CDC definition was also identified in the HRSA definition.
CBSA indicates Core-Based Statistical Area; CDC, Centers for Disease Control and Prevention; FAR, Frontier and Remote; HRSA, Health Resources and Services Administration; RCC, Rural Continuum Code; RUCA, Rural-Urban Commuting Area; UA/UC, Urban Area/Urban Cluster; UIC, Urban Influence Code.
Differences across population characteristics and definitions are presented in Table 2. The definition generating the largest (absolute) difference between urban and rural populations is highlighted in dark gray, and the second-largest difference is in light gray. For example, the largest difference between rural and urban areas for percent of the population with a bachelor’s degree was identified by the CBSA definition (14.18 percentage points) and the second-largest difference by the HRSA definition (13.51 percentage points). The UIC definition generated the largest difference for 7 measures: poverty, population growth, percent of nonelderly uninsured, and each health care access measure. The UA/UC definition generated the largest difference in population density, and the CBSA definition generated the largest difference in the percent with some college. The CBSA and FAR generated the most “second-largest difference” measures, while the HRSA measures were the second-largest difference for 2 measures each. In only one comparison (poverty for UA/UCs), does the urban area have the less healthy value.
TABLE 2.
Differences in Weighted Averages of Measures by Various Definitions of Rurality
| Definition | Population Characteristics | Percent Within 30 min of | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Rural Definition | BA Degree | <200% Poverty | Pop Change | Pop Density | Health Ins | Hospital | Hosp, 100 Beds | Dentist | Primary Care |
| CDC | −11.43 | 7.01 | −4.85 | −5.93 | 1.16 | −5.25 | −28.99 | −32.845 | −2.81 |
| UA/UC | −10.30 | −1.07 | −2.28 | −6.78 | 0.27 | −8.71 | −29.76 | −31.55 | −3.18 |
| HRSA | −13.51 | 7.48 | −5.69 | −5.95 | 1.65 | −7.71 | −40.50 | −48.15 | −4.04 |
| RUCA (≥4) | −12.95 | 7.73 | −5.57 | −5.76 | 1.60 | −6.45 | −39.07 | −47.08 | −3.86 |
| CBSA | −14.18 | 7.91 | −6.48 | −5.55 | 2.56 | −10.77 | −52.91 | −69.21 | −7.38 |
| RCC (≥7) | −12.55 | 7.72 | −6.14 | −5.39 | 2.20 | −11.71 | −49.52 | −64.60 | −9.23 |
| FAR | −10.02 | 7.04 | −4.84 | −5.12 | 1.89 | −12.36 | −42.59 | −57.56 | −10.43 |
| UIC (≥9) | −12.68 | 7.91 | −6.49 | −5.35 | 2.59 | −13.40 | −55.42 | −71.03 | −12.38 |
The rows are given in decreasing number of the rural population.
Rural-urban differences in population characteristics by rural definition. All data represent differences in weighted averages of measures by various definitions of rurality. Measures include: “BA Degree” is the age +25 population with a bachelor’s degree (%); “<200% poverty” is the population living in households with incomes < 200% of the federal poverty level; “Pop Change” is change in total population from 2010 to 2018 (%); “Pop Density” is population density (people/km2); “Health Ins” is the percentage of population age below 65 with health insurance; “Hospital” is people with 30-minute travel time access to an acute care hospital (%); “Hosp, 100 Beds” is 30-minute access to a hospital with at least 100 beds (%); “Primary Care” and “Dentists” are 30-minute access to a primary care physician and dentist respectively (%).
The largest absolute difference are highlighted in dark gray.
The second-largest absolute difference are highlighted in light gray.
CBSA indicates Core-Based Statistical Area; CDC, Centers for Disease Control and Prevention; FAR, Frontier and Remote; HRSA, Health Resources and Services Administration; RCC, Rural Continuum Code; RUCA, Rural-Urban Commuting Area; UA/UC, Urban Area/Urban Cluster; UIC, Urban Influence Code.
Figure 2 displays the rurality agreement for each census tract. The lightest and darkest areas show tracts with better agreement among the rural definitions, which generally appear to be found in urban centers and the most remote regions. Dissonance among definitions is captured in the gray areas of the map, many of which appear in rings around urban regions (eg, a score of 4 means 4 definitions considered the tract rural and 4 considered it urban). This is particularly noticeable for many tracts in the Southeast, Midwest, and West Coast.
FIGURE 2.
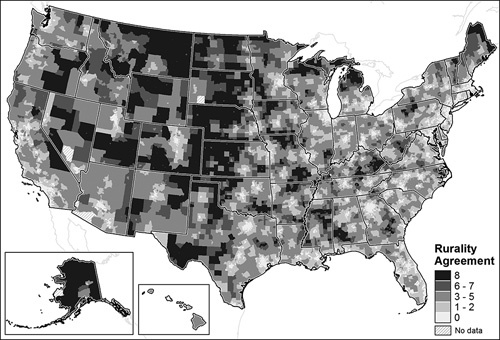
Rurality agreement using federal rural definitions by census tract.
The vast majority of the US population (65.44%) lives in regions not identified as rural in any of the 8 definitions. Another 14.17% of the population are identified as being rural in only a single definition, leaving 20.39% of the population living in regions with a rurality agreement value between 2 and 8. Only 3.16% of all US residents were living in regions identified as rural in 6 or more of the definitions.
Variation in selected population characteristics by rurality agreement can be found in Figure 3 and Supplementary Figure for all characteristics (Supplemental Digital Content 2, http://links.lww.com/MLR/C308). Some characteristics vary smoothly over the levels, while others have notable drops or increases (discontinuities) at a specific level. Notable results include characteristics with large discontinuities at a single rurality agreement (between 0 and 1) such as total population, population density, White, Black, Asian, and Hispanic population percent, and depression prevalence, as well as those with discontinuities when all definitions agree (between 7 and 8), including 30-minute travel time access to a hospital and primary care provider. Other characteristics have large or secondary discontinuities at levels of rurality in between 0 and 8, while others gradually change across the levels of rurality (eg, American Indian and Alaska Native population percent, population with a bachelor’s degree, and heart disease prevalence). Overall, the results in Figure 3 and Supplementary Figure (Supplemental Digital Content 2, http://links.lww.com/MLR/C308) suggest that characteristics expected to differ between urban and rural dwellers do so under varying circumstances, as some demonstrate clear break values that may highlight true differences between urban and rural populations, whereas others such as education, poverty, and health outcomes vary semismoothly across the levels of rurality suggesting binary classifications may not capture the nuances of the differences between rural and urban populations.
FIGURE 3.
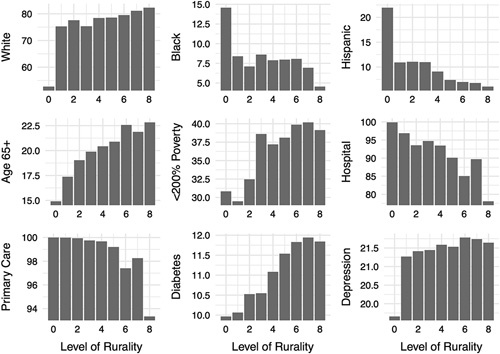
Population characteristics by rurality agreement. The population is total population (millions of people); White, Black, and Hispanic are percent of the population (%); < 200% poverty is the population living in households with incomes < 200% of the federal poverty level; hospital and primary care are people with 30-minute travel time access to an acute care hospital (%); asthma, diabetes, heart disease, and depression are prevalent in the age ±18 population (%).
These patterns are useful in assessing the most appropriate definition of rurality for a characteristic. For example, the biggest differences in race/ethnicity categories tend to be between 0 and 1, suggesting that the broadest rural definitions (eg, UA/UC and CDC) are better suited for capturing differences among groups based on race/ethnicity. Meanwhile, the proximity measures saw the biggest differences between 7 and 8 levels of rurality. This suggests that more restrictive definitions of rural—such as FAR—may be better at identifying the differences based on access to health care. These results are consistent with the takeaways from Table 2.
DISCUSSION
In this analysis, we compared 8 different federal definitions of rural, evaluating the agreement among definitions in which populations were identified as rural as well as the differences in population characteristics among urban and rural dwellers (as defined by each). Notably, the definitions produced massive differences in the number of rural dwellers in the United States, highlighting the difficulties in even enumerating the rural population in the United States.
While the total population of rural dwellers is an important metric, we also found that the characteristics of people and their access to health care services were quite variable from definition to definition, highlighting the discord not only among the size of the US’ rural population but also who are identified as the rural population. We also uncovered large differences in each definition’s ability to distinguish populations that are truly different from one another.
Rurality agreement captured the agreement among rural definitions, which allowed us to evaluate variation in population characteristics across these levels. When mapped, a gradient in the level of agreement was apparent, centered on urban regions and radiating outward through regions that might be considered suburban or exurban (disagreement) before coming back to the agreement in the more remote and least populated regions of the United States. Evaluating the variation in population characteristics across levels of rurality showed that some have well-defined discontinuities and therefore may be more appropriate for use in binary rural-urban classifications, others vary gradually across these levels and do not lend well to this type of classification.
Our findings demonstrate the importance of an appropriate rural definition when considering disparities. Tying policies to efforts to spur rural workforce through recruitment or retention thus should carefully consider the goals of the program and use the most appropriate rurality definition when determining eligibility. Recent evidence on the decreasing density of primary care supply and the contribution to increased mortality supports efforts to increase primary care supply in high need areas.20 But which rural definition best meets the goals of such efforts?
This study should be viewed in the context of some limitations. Although we considered some broad measures of need and access, they are incomplete in capturing the multifactor contributors to health. Unfortunately, current public health data infrastructure limits the public data available at the census tract. The approach here was at the population level, and significant differences could exist across populations within tracts.
There was no one “best” measure of rurality for predicting rural-urban disparities. Although the UIC generally provided the largest disparities, the particular dichotomization of UIC used here was limited to the most rural counties and thus the most rural populations. It is not uncommon for rural-urban disparities to be most pronounced when confining those identified as rural to a narrow population. For example, general surgeon availability per capita in large rural areas was slightly higher than the national average but was nearly 30% below the national average in the small and isolated rural areas.21
We identified some general patterns in which rural definitions identified the largest differences between rural and urban populations. The UIC and CBSA definitions were more predictive for demographics (eg, education, poverty, and population growth). While the UIC also worked well for health measures, the FAR codes were also predictive for the more common health care resources (access to a hospital, dentist, and primary care physician). Thus, one potential takeaway is that when considering access to more common health care resources, the FAR definition may work well. However, less prevalent resources (eg, access to a hospital with at least 100 beds) were better identified using the CBSA definition. Meanwhile, we present additional guidance on which definitions better capture differences (Fig. 3, Supplementary Fig., Supplemental Digital Content 2, http://links.lww.com/MLR/C308); for example, the largest gradient for Black, Asian, and Hispanic percentages—as well as percent with depression—is between 0 rural definitions and 1; this implies the most restrictive definition of urban (UA/UC) is the strongest identifier. Thus, one potential rule of thumb is for race/ethnicity as the outcome, use the broader definitions of rurality (eg, UA/UC), for demographics, use restrictive definitions (eg, UIC or CBSA), and for access to health care resources, use isolation-based measures (eg, FAR). Another interesting finding is that the CDC and UA/UC definitions were generally 2 of the lower performing identifiers of differences between rural and urban populations; for the CDC definition, this should not be surprising, since the CDC’s discussion on this measure focuses on its value in separating large metro central counties from large metro fringe counties.22 However, one conclusion is that the broadest definitions of rural do not adequately capture rural-urban disparities (other than for race/ethnicity); a more restrictive (smaller) definition of rural tends to find larger differences, which underscores the nonlinearity in rural disparities. Although generally, health challenges were increasing in rurality, the tighter the definition, the larger the disparity.
In some cases, the availability of data will guide the definition choice; the RUCA definition is not possible when using county data. But when given the choice, these findings suggest that research designs should carefully consider the measure and context when deciding on the rural definition. A study of access to acute care in the Northeast might use FAR or CBSA; a national study of health insurance rates should probably consider the UIC. These findings, considered as a whole, underscore the importance of careful consideration of the research question and context when deciding on the most appropriate definition for rurality.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.
Footnotes
Supported by Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (HHS) as part of an award totaling $525,465 with 0% financed with nongovernmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement by, HRSA, HHS, or the US Government. For more information, please visit HRSA.gov.
The authors declare no conflict of interest.
Contributor Information
Julianna C. Long, Email: juliacl@live.unc.edu.
Paul L. Delamater, Email: pld@email.unc.edu.
George M. Holmes, Email: mark_holmes@unc.edu.
REFERENCES
- 1.US Census Bureau. What is rural America?. The United States Census Bureau. 2017. Available at: www.census.gov/library/stories/2017/08/rural-america.html. Accessed August 21, 2020.
- 2.Probst J, Eberth JM, Crouch E. Structural urbanism contributes to poorer health outcomes for rural America. Health Aff (Millwood). 2019;38:1976–1984. [DOI] [PubMed] [Google Scholar]
- 3.Singh GK, Siahpush M. Widening rural–urban disparities in life expectancy, US, 1969–2009. Am J Prev Med. 2014;46:e19–e29. [DOI] [PubMed] [Google Scholar]
- 4.Gong G, Phillips SG, Hudson C, et al. Higher US rural mortality rates linked to socioeconomic status, physician shortages, and lack of health insurance. Health Aff (Millwood). 2019;38:2003–2010. [DOI] [PubMed] [Google Scholar]
- 5.Starfield B, Shi L, Grover A, et al. The effects of specialist supply on populations’ health: assessing the evidence: the evidence suggests that populations do not necessarily benefit from an overabundance of specialists in a geographic area. Health Aff (Millwood). 2005;24(suppl 1):W5-97–W5-107. [DOI] [PubMed] [Google Scholar]
- 6.Kaufman BG, Thomas SR, Randolph RK, et al. The rising rate of rural hospital closures. J Rural Health. 2016;32:35–43. [DOI] [PubMed] [Google Scholar]
- 7.Miller KEM, James HJ, Holmes GM, et al. The effect of rural hospital closures on emergency medical service response and transport times. Health Serv Res. 2020;55:288–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gujral K, Basu A. Impact of Rural and Urban Hospital Closures on Inpatient Mortality. Cambridge, MA: National Bureau of Economic Research; 2019. [Google Scholar]
- 9.Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. Am J Public Health. 2005;95:1149–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bennett KJ, Borders TF, Holmes GM, et al. What is rural? challenges and implications of definitions that inadequately encompass rural people and places. Health Aff (Millwood). 2019;38:1985–1992. [DOI] [PubMed] [Google Scholar]
- 11.Mueller KJ Coburn AF Knudson A, et al. Considerations for defining rural places in health policies and programs. Rural Policy Research Institute; 2020:21.
- 12.Waldorf BS. A continuous multi-dimensional measure of rurality: moving beyond threshold measures. 2006 Annual Meeting, July 23–26. Long Beach, CA: American Agricultural Economics Association (New Name 2008: Agricultural and Applied Economics Association); 2006. Report No.: 21383. Available at: https://ideas.repec.org/P/ags/aaea06/21383.html. Accessed August 21, 2020.
- 13.Waldorf B, Kim A. Defining and Measuring Rurality in the US: From Typologies to Continuous Indices: Workshop on Rationalizing Rural Area Classifications. Washington, DC: The Keck Center; 2015:26. [Google Scholar]
- 14.Randolph RK Thompson KW Thomas SR, et al. Delineating rural areas in the United States. Poster presented at: National Rural Health Association Annual Conference; 2019.
- 15.Streeter RA, Snyder JE, Kepley H, et al. The geographic alignment of primary care Health Professional Shortage Areas with markers for social determinants of health. PLoS One. 2020;15:e0231443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.USDA ERS. Documentation: urban influence codes. 2019. Available at: www.ers.usda.gov/data-products/urban-influence-codes/documentation.aspx. Accessed August 21, 2020.
- 17.PolicyMap. Our Data Directory: PolicyMap and Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System, Health Outcome Estimates and Risk Factor Estimates. Available at: www-policymap-com.libproxy.lib.unc.edu/data/our-data-directory/. Accessed August 21, 2020.
- 18.Garcia MC, Rossen LM, Bastian B. Potentially excess deaths from the five leading causes of death in metropolitan and nonmetropolitan counties—United States, 2010–2017. MMWR Surveill Summ. 2019;68:1–11. [DOI] [PubMed] [Google Scholar]
- 19.ESRI. Service area service with asynchronous execution—ArcGIS REST API. ArcGIS for Developers; 2020. Available at: https://developers.arcgis.com/rest/network/api-reference/service-area-asynchronous-service.htm. Accessed August 21, 2020.
- 20.Basu S, Berkowitz SA, Phillips RL, et al. Association of primary care physician supply with population mortality in the United States, 2005–2015. JAMA Intern Med. 2019;179:506–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thompson MJ, Lynge DC, Larson EH, et al. Characterizing the general surgery workforce in rural America. Arch Surg. 2005;140:74–79. [DOI] [PubMed] [Google Scholar]
- 22.National Center for Health Statistics. Data access—urban rural classification scheme for counties. National Center for Health Statistics Public Use Data files; 2019. Available at: www.cdc.gov/nchs/data_access/urban_rural.htm. Accessed March 25, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.


