Abstract
Objectives:
The key component of a comprehensive palliative care (PC) unit is provision of a regular and sustainable home-based PC (HBPC) service. This quality improvement project aimed to plan, organise and sustain a regular HBPC service in a government cancer centre in Southeast India. The aim was to regularise and increase the number of home care visits among the patients identified for HBPC services through sustainable interventions.
Materials and Methods:
The A3 methodology with its team-based, structured problem-solving approach was the tool used. The situational process map at baseline was followed up with a sequential cause and effect analysis and team discussions to create sustainable and reliable interventions. These included creating the electronic data system for data collection in PC, allocation of resources and implementation of systems to coordinate HBPC services. The roles and ownership to maintain improvement were established by designation and this requirement has been included in the job description to ensure reliability and sustainability.
Results:
The regularisation of home care services with a consistent increase in the number of home visits from 2/week to over 6/week helped achieve the Specific, Measurable, Achievable, Relevant and Time bound goal. Better documentation, coordination and accountability were also positive outcomes. Working with different departments and teams along the project helped build trust and understanding along with a sound base for collaborative research.
Conclusion:
The A3 way of problem solving through dialogue and consensus helped to organise HBPC services and this methodology can be extended to other areas in future.
Keywords: Palliative care, Home-based palliative care, A3 methodology, Quality improvement
INTRODUCTION
Home-based palliative care (HBPC) is considered a key component of a comprehensive PC service.[1] It enables the care providers to continue the care provided in the acute or subacute setting and ensure seamless transitions to the changing medical, social and spiritual needs at the patient’s home.[2] The existence of a competent home care team provides security in the form of support, prevention and relief of unavoidable suffering[2] along with improved patient satisfaction.[3] The benefits of home PC in lowering the symptom burden of the patient and empowering the caregiver have been well documented.[4-6] In India, 80% of the 1 million cancer cases detected annually are in the advanced stage of the disease. Outside of Kerala, most states lack a network of HBPC provision[7] and Andhra Pradesh is one of them.
The Homi Bhabha Cancer Hospital and Research Centre (HBCHRC) is a tertiary cancer care centre in Andhra Pradesh (Southeast India) with a functional PC unit since its inception 6 years ago. Besides caring for patients on disease-modifying therapy with curative and palliative intent, the PC unit is required to serve patients with advanced disease who are home bound and unable to travel to the centre.
The HBPC services are organised and coordinated in collaboration between the PC unit at HBCHRC and a community-based (non-governmental) organisation (CBO). The PC unit at HBCHRC provides outpatient PC services and the CBO which has been working for geriatric and PC focuses on HBPC in the city.
Although patients with home care needs were being identified, the services lacked planning and organisation which is necessary for care provision, preserving continuity of care and sustainability of the service. The number of patients identified for HBPC within city limits averaged around 25–30 at any given time and the home visits were about 0–3/week and erratic. This was an important gap in the quality of the services and cause for concern.
Thus, when the opportunity for collaborative training with the Stanford PC-PAICE PC – Promoting Assessment and Improvement of Cancer Experience in Quality Improvement was proposed, it was a unanimous decision by HBCHRC and the CBO to choose the poor organisation and coverage of HBPC services as their problem statement and work toward improving it in a disciplined and methodical manner.
MATERIALS AND METHODS
The working group in this QI project included the nurse, social worker, the palliative care physician and an oncologist at HBCHRC along with the coordinating physician and team members of the CBO providing HBPC services.
The A3 methodology with its structured approach was used for quality improvement. The A3 methodology is a systematic team-based problem-solving method incorporating the principles of Plan, Do, Check and Act cycle. The term A3 denotes the size of paper used to outline the steps through the process of problem solving.[8,9] The left side of the A3 includes the background, the problem statement, the Specific, Measurable, Achievable, Relevant and Time bound (SMART) goal and the root cause analysis. Through discussions with the multidisciplinary team and a consensus; the problems are identified and prioritised. Interventions are then accordingly aligned. The envisioned interventions, its practice, sustainability and results make up the right side of the A3 sheet. The run chart tells the story of the project from baseline to completion.
In discussion with the CBO team members, the SMART goal chosen was to regularise and intensify the weekly HBPC visits from 0 to 3 visits per week in November 2017 to six visits per week at the minimum, by June 2018.
The number of HBPC services provided per week became the outcome measure and was documented as a run chart. This run chart depicted the changes in services sequentially with on-going improvement interventions, across the duration of the project.
As this was a QI project with no identifiable and/or individual patient information, a formal ethics review was not sought for. Permission to conduct the project was obtained from the director of the institute.
Situational analysis
The start of problem solving using the A3 methodology was to have a situational analysis to first understand the process and then identify the root causes of the problem in the workflow.
The first tool was the process map to understand the referral patient flow from the outpatient oncology unit to palliative care and the subsequent identification of patients needing HBPC services.
Process map of the HBPC services before the improvement project
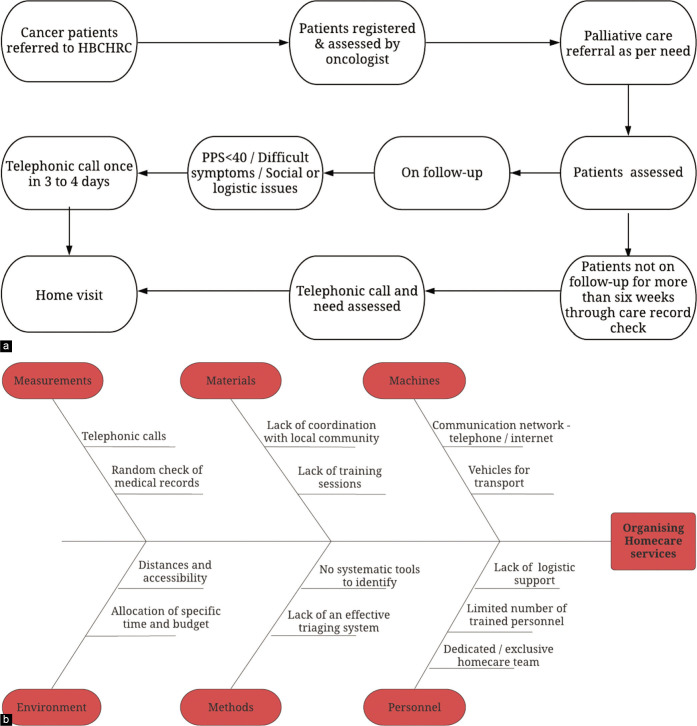
Three categories of patients reported to the outpatient palliative care unit at HBCHRC [Figure 1a].
Figure 1:
(a) Situational analysis – The A3 methodology tools applied sequential for the project. (b) Cause and effect analysis using fishbone diagram. The GEMBA/participant observation technique was used to directly observe the conditions at the workplaces and identify the root causes for the inconsistent homecare services through team consensus.
Patients on cancer-directed therapy needing supportive care
Patients visiting the hospital regularly; either on oral cancer directed therapies or not on any disease directed therapy
Patients unable to travel to the centre due to advanced cancer represented by caregivers.
A HBPC assessment of the patient was made using the palliative performance scale (≤40%); the symptom burden (≥5 on the Edmonton Symptom Assessment Scale) and the social and logistical challenges faced by patients to reach the hospital.
Patients lost to follow-up for over 6 weeks received a phone call and a needs assessment for HBPC was done. Of those identified, patients living within the 40 km radius were earmarked for home care.
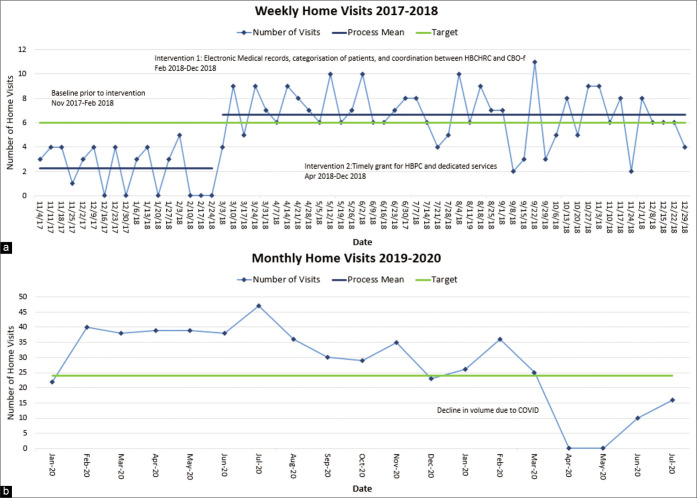
As part of the A3 methodology, the sequential tool – the cause and effect diagram [Figure 1b] was used to identify the contributors to the problem. This analysis was the outcome of the GEMBA walk which is the Japanese term for the ‘real place where the work happens.’ This provided the opportunity to engage with people directly involved at different levels. In this way, through meetings and interactions, root causes for the inconsistent HBPC services at ground level were unveiled. Although HBPC was activated, the visits were erratic and disorganised as seen in the baseline run chart between November 2017 and February 2018 [Figure 2a].
Figure 2:
(a) Weekly homecare services recorded as a run chart, across the duration of the project and after completion of the project. (b) Run chart January 2019– July 2020 – monthly HBPC visits done (only physical) target 6/week or 24/month.
The most significant shortcomings identified by the team through a consensus meeting and voting were as follows:
Logistical inability and delay to check the medical records manually
Poor implementation of the triage for HBPC services
Inconsistency in telephonic communication with the patients due to the incomplete manual entries of phone numbers and tele-connectivity issues
Lack of clarity on the staff required to manage the demand for care
Inability to increase capacity with demand for HBPC.
Interventions
To maintain consensus at all stages, the team met and brainstormed to derive the key drivers and interventions to overcome the above contributors [Table 1].
Table 1:
Key drivers and interventions.
| Root cause analysis | Key drivers | Interventions | Responsible team member |
|---|---|---|---|
| Measurements Medical records, phone calls |
Data collection | At HBCHRC Creating an Electronic Medical Record system for PC unit Triage system and code to mark patients needing HBPC By the CBO Creating an electronic database of patients needing HBPC and assigning a unique ID to every patient |
Assigned personnel from HBCHRC PC team Assigned volunteer from the CBO |
| Environment Allocation of specific time and budget, distance Materials Lack of coordination, training |
Planning | Weekly planning of home visits Plan the route, distance and patients to be covered Communication and exchange of information through WhatsApp group and electronic data entry on both sides Team meetings for training and guidance |
Assigned personnel from HBCHRC and CBO |
| Machines Communication, vehicles Methods Tools, implementation of triaging, logistics, personnel Materials Lack of coordination, training |
Resource management | Dedicated home care team availability of transport on designated days coordination between HBCHRC and the home care team Liaising with local community resources |
Assigned personnel from CBO&HBCHRC The timely grant by the Two Worlds Cancer Collaboration to the CBO facilitated this |
| Methods Tools, implementation of triaging, logistics, personnel |
Sustainability | Periodic review Auditing | Assigned personnel from HBCHRC and CBO |
For example, an important problem area was the inadequate medical records which led to inefficient triaging and delays in identification of patients needing HBPC. Accordingly, the key driver was ensuring completeness of the data collected. The team intervened by working with the Information Technology department at HBCHRC to create an electronic medical record system for the palliative care unit to facilitate entries and categorise patients based on their needs. After the triage, those identified for HBPC were given a code ‘A.’ Simultaneously, the CBO digitalised their records and every patient needing HBPC was given a unique ID. The location mapping was also done.
In this way, interventions were planned for the identified problem areas. The team then took up the challenge and initiated the following interventions: [Table 1]
Categorisation of patients seeking PC based on their needs and identifying those needing HBPC to be done on a daily basis (Code A)
Communicating the details of the patients triaged to the CBO at the end of the day
Creation of a master list with a unique identity number for every patient needing HBPC and demarcating them geographically by the CBO volunteers
Coordination between the hospital PC unit and the CBO in organising, regularising and thus increasing the number of HBPC visits systematically. In addition, regular stakeholder feedback was taken for continuous improvement of the QI program
A timely grant directed for HBPC services from the Two Worlds Cancer Collaboration through a memorandum of understanding with the CBO helped fast track the regular HBPC service for the city. Through this grant, personnel and vehicles were allotted for dedicated HBPC.
The interventions used in this project yielded positive results as they were planned in the group discussions and systematically linked based on the problems identified in root cause analysis.
RESULTS
The run charts in Figure 2a and b depict the record of the weekly home visits across the 7 months duration of the project and beyond. As may be noted, it shows a distinct improvement in the number of weekly HBC visits from two at baseline to over 6/week. The SMART goal was achieved by the end of the project.
DISCUSSION
Reliability and Sustainability of the project
There were gaps in services when staff was on leave and could not be replaced. Rescheduling of these visits was done over the subsequent weeks. Telephonic calls to bridge these gaps and ensure rescheduling was also done. To ensure reliability of implementing each intervention, a team member was designated specific role and responsibility. The key drivers for improving the processes and responsibility sharing are shown in Tables 1 and 2.
Table 2:
Current process map for reliability and sustainability.
| System | Site | Responsibility | Frequency | Comments |
|---|---|---|---|---|
| Triage and identification of patients needing home care | HBCHRC | D, N, MSW | Daily | Triage and identification: D Data Documentation: N/MSW |
| Communication to the CBO | HBCHRC&CBO | N/MSW at HBCHRC N and Designated Volunteer at CBO |
Daily | Information exchange through WA |
| Planning and coordination of the visit | CBO | N and designated volunteer at CBO | Completed within a week of receipt of information | Geographical mapping Creation of a unique patient ID Home visit plan drawn for the week and visit completed by the team |
| Feedback after completion and documentation | CBO | N and D at CBO N and D at HBCHRC |
On completion of the visits | Communicated by the D/N at CBO to the D/N at HBCHRC and documentation is completed by the N/MSW |
| Special circumstances: In case, the visit is urgent, this information is communicated by the doctor, process is fast tracked and visit is prioritised Daily/weekly exchange of information and reviews by the team are held through WA groups and in person The Google Sheets with the UID and information is accessible to the D/N/MSW at the CBO and HBCHRC to enable continuity of documentation at follow-ups and monitoring the process regular up gradation and communication is on-going between the CBO and HBCHRC | ||||
N: Nurse, D: Doctor, MSW: Medical social worker
To ensure sustainment of the improved processes, the interventions needed to become integrated and implemented at both institutions. The mandated specific roles and ownership required to maintain the improvements were established by designation; to the doctor/nurse/MSW in-charge; rather than choosing specific people [Table 2]. The requirements are now included as part of the job description and this has sustained the improvements even now, 2 years after the project. Indeed, this ensured that the improved processes would continue to flow undisturbed irrespective of changes of members of the team. In fact, the improved processes continue to stay implemented even with two of the members leaving the organisation [Figure 2b].
CONCLUSION
Overall, the QI exercise led to better workflow, which matched with our SMART goal of caring for homebound patients. It helped evolve a dedicated HBPC team with empowered, motivated and confident staff. The processes have become robust with electronic records and streamlining of procedures. The sensitivity and specificity of tracking patients who need HBPC have improved along with enhanced triage, accountability and coordination between the hospital and the CBO teams.
The palliative medicine department and the CBO, with methodology driven planning, could collaborate to understand variances, share vision, resources and systems to implement a crucial service. This helped maximise the outcomes with available minimum resources.
The data entry process is a regular responsibility and mandatory now. Although time consuming, it is being maintained and improvised on mainly due to the enthusiasm from the significant outcomes. Mentoring and ensuring that the interventions continue to be implemented and improve overtime are a challenge. The interventions can change from time to time based on the situation and need. Identification of this dynamic change and sustaining the program will be a major challenge. There is also a need to provide on-going training to expand the congruence and quality of the service. As a framework, the interventions could be generalisable in a similar setting but due to the variation in the provision of home care services in our country, cultural and regional modifications may be needed.
Beyond the project
The hospital administration has identified HBPC as an essential aspect of the continuum for cancer care. The beauty of the QI has been the learning from our mentors and learning through mentoring others. It has also been about building relationships along with the learning. Working with several different departments during the project, helped build trust and understanding, expanded the scope for palliative care along with a sound base for collaborative research activity. QI educational sessions for the staff, the residents and the fellows have been held within the hospital. The paramedical staff; the social workers, nurses, feel encouraged and motivated due to the results of their efforts.
Their participation in the QI project has raised their profile within the institution, impacted their appraisals and has led to publications with their names included as authors,[10] a first for all of them.
Adapting to COVID-19
Since March 2020, the pandemic has grounded our HBPC services. This has been a setback for patients but some of the adaptations have revealed that resources could be further optimised. A dedicated telemedicine system set up by the CBO has helped manage patients virtually. The improved data collection has helped to regularly follow-up patients telephonically and provide support. Video calls through the caregivers’ phone have been very useful to provide reassurance and medication. Select HBPC services are being provided using a stricter triage after a telephonic assessment. The way forward could be planning virtual HBPC services on a regular basis and physical home visits only when absolutely needed.
Telemedicine for HBPC could be the collateral benefit and may well be our next QI project!
Acknowledgments
We are grateful to our mentors Jake Mickelsen, Dr. Karl Lorenz and Michelle De Natale from Stanford University, Dr. David Casarett from Duke University and Dr. Nandini Vallath – National Cancer Grid for their mentorship, patience and guidance.
Footnotes
How to cite this article: Viswanath V, Digumarti L, Raju NS, Lokanandi UR, Dasu MR, Bolem SK, et al. Organising home-based palliative care services: A quality improvement project at the Homi Bhabha Cancer Hospital and Research Centre, Vishakhapatnam. Indian J Palliat Care 2021;27(2):197-203.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sepúlveda C, Marlin A, Yoshida T, Ullrich A. Palliative care: The World Health Organization's global perspective. J Pain Symptom Manage. 2002;24:91–6. doi: 10.1016/S0885-3924(02)00440-2. [DOI] [PubMed] [Google Scholar]
- 2.Zhang M, Smith KL, Cook-Mack J, Wajnberg A, DeCherrie L, Soriano TA. In: Evidence Based Practice of Palliative Medicine. Goldstein NE, Morrison RS, editors. Philadelphia, PA: Elsevier Saunders; 2013. How can palliative care be integrated into home based primary care programs? pp. 458–67. [Google Scholar]
- 3.Sarmento VP, Gysels M, Higginson IJ, Gomes B. Home palliative care works: But how? A meta-ethnography of the experiences of patients and family caregivers. BMJ Support Palliat Care. 2017;7:1141. doi: 10.1136/bmjspcare-2016-001141. [DOI] [PubMed] [Google Scholar]
- 4.Brumley R, Enguidanos S, Jamison P, Seitz R, Morgenstern N, Saito S, et al. Increased satisfaction with care and lower costs: Results of a randomized trial of in-home palliative care. J Am Geriatr Soc. 2007;55:993–1000. doi: 10.1111/j.1532-5415.2007.01234.x. [DOI] [PubMed] [Google Scholar]
- 5.Gomes B, Calanzani N, Higginson IJ. Benefits and costs of home palliative care compared with usual care for patients with advanced illness and their family caregivers. JAMA. 2014;311:1060–1. doi: 10.1001/jama.2014.553. [DOI] [PubMed] [Google Scholar]
- 6.Paul A, Fernandes E. Experiences of caregivers in a home-based palliative care model a qualitative study. Indian J Palliat Care. 2020;26:306–11. doi: 10.4103/IJPC.IJPC_154_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Potts M, Cartmell KB, Nemeth LS, Qanungo S. A qualitative evaluation of a home-based palliative care program utilizing community health workers in India. Indian J Palliat Care. 2019;25:181–9. doi: 10.4103/IJPC.IJPC_166_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson PM, Patterson CJ, O'Connell MP. Lean methodology: An evidence-based practice approach for healthcare improvement. Nurse Pract. 2013;38:1–7. doi: 10.1097/01.NPR.0000437576.14143.b9. [DOI] [PubMed] [Google Scholar]
- 9.Lorenz KA, Mickelsen J, Vallath N, Bhatnagar S, Spruyt O, Rabow M, et al. The palliative care promoting assessment and improvement of the cancer experience (pc-paice) project: A multi-site international quality improvement collaborative. J Pain Symptom Manage. 2021;61:190–7. doi: 10.1016/j.jpainsymman.2020.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vemula SR, Dasu MR, Sharma VV, Katta N, Raju NS, Digumarti L, et al. Role of social workers and volunteers in improving the quality of home care services. Indian J Palliat Care. 2019;25:260–357. [Google Scholar]