Abstract
Reduced heart rate variability (HRV) in response to stress is a biomarker of emotion dysregulation (ED) and is related to posttraumatic stress disorder (PTSD), yet less is known about its role with dissociation in trauma-exposed adults. The goals of the current study were to examine unique patterns of associations between ED, dissociation, and PTSD with HRV at 15, 30, and 45 minutes (T1, T2, T3) following an acute psychosocial stressor task in a sample of 49 trauma-exposed, urban-dwelling Black women. Associations with baseline psychophysiology measures were also examined. ED and dissociation were assessed using self-report; PTSD was determined using a semi-structured interview. Heart rate (HR) and HRV, indexed with low frequency/high frequency (LF/HF) ratio and respiratory sinus arrhythmia (RSA), were measured with electrocardiogram recordings. ED and dissociation were positively correlated with LF/HF ratio at T3 (p<.05). There were no significant differences between individuals with PTSD versus those without PTSD in HR or HRV following acute stressor; PTSD diagnosis was related to higher HR at baseline. Latent growth modeling revealed that ED was associated with higher LF/HF ratio directly following acute stressor, while dissociation was associated with increase in LF/HF ratio over time. These findings demonstrate that ED is related to higher sympathetic reactivity for a prolonged period of time following stress exposure, while dissociation shows a delayed association with LF/HF ratio, suggesting a distinct impaired parasympathetic activation pattern exists for dissociation.
Introduction
Trauma exposure is ubiquitous (Benjet et al., 2016) but does not affect everyone the same way. Type, timing, and frequency of trauma exposure matters in understanding risk for adverse health outcomes. Interpersonal trauma exposure, child abuse, and exposure to multiple traumas all increase one’s likelihood for negative health outcomes, most notably posttraumatic stress disorder (PTSD) (Briere et al., 2008; Forbes et al., 2011). Certain demographic factors also relate to trauma-related outcomes. Women are twice as likely as men to develop PTSD (Olff et al., 2007). Rates of trauma and PTSD are substantially higher in low-income Black communities with rates of lifetime PTSD as high as 50% (Gluck et al., 2021) as compared to the national average of 6% (Pietrzak et al., 2011). Additionally, high comorbidity exists between PTSD and chronic medical conditions, like diabetes, and trauma exposure and PTSD contribute to worse health outcomes in these populations (Dixon et al., 2020). Thus, examining physiologic responses to stress and factors that influence such responses among trauma-exposed individuals in at-risk groups, such as Black women with diabetes from low-income, urban communities, is necessary to reduce health inequities and improve health outcomes in Black communities.
The adverse health consequences of trauma exposure can be significant, affecting multiple body systems including the autonomic nervous system (ANS). The ANS has a pivotal role in the maintenance of homeostasis and adaptive response to stress. Heart rate variability (HRV), or the fluctuation in the length of intervals between heart beats, reflects the heart’s ability to adapt to external and internal demands and can serve as a measure of ANS balance (Kim et al., 2018). Two commonly used measures of HRV include low frequency/high frequency (LF/HF) ratio and respiratory sinus arrhythmia (RSA or HF-HRV). While HF-HRV is generally reflective of parasympathetic activity and vagal tone, LF/HF ratio includes both SNS and PNS activity (Shaffer and Ginsberg, 2017); high LF/HF ratio is considered to reflect greater sympathetic dominance.
Low RSA and high LF/HF ratio under stress have been consistently associated with PTSD (Schneider and Schwerdtfeger, 2020). Importantly, alterations in HRV observed in adults relates to early life maltreatment or associated psychological factors as opposed to psychological diagnoses (Meyer et al., 2016). Reduced HRV is a biomarker of emotion dysregulation (ED) (Beauchaine, 2015), which is itself a transdiagnostic risk factor for the development of many psychological disorders, including PTSD (Weissman et al., 2019).
ED reflects deficits in the ability to identify, modulate, or manage intense negative emotional states (Gross and Thompson, 2007). ED has been prospectively linked to increased risk for PTSD following trauma exposure (Pencea et al., 2020) and may contribute to maintenance of PTSD symptoms (Powers et al., 2017). Importantly, research has indicated that there may be at least two distinct types of ED in PTSD, which may be associated with different autonomic responses to stress: emotional under-modulation (hyperarousal symptoms characterized by impaired prefrontal inhibition of limbic response) and emotional over-modulation (dissociation characterized by exaggerated prefrontal inhibition of limbic response) (Lanius et al., 2012). Dissociation is a maladaptive form of emotion regulation characterized by disruptions in one’s memory, identity, and self or environment perception, and occurs in response to strong emotions or stress in an effort to manage emotional distress often outside the one’s control (Brière, Weathers, & Runtz, 2005; Powers et al., 2015). Chronic interpersonal trauma and child abuse are associated with increased risk for the development of both ED (Messman-Moore and Bhuptani, 2017) and dissociation (Terock et al., 2016).
Studies on dissociation, PTSD, and HRV in the context of stress exposure are limited. One study found that, compared to controls, patients with dissociative disorders showed higher LF/HF ratio in response to an adult attachment interview (Farina et al., 2015). Another study found state-level dissociation was associated with lower HRV in response to affective cues in trauma-exposed individuals but not healthy controls (Hauschildt et al., 2011). However, there is also evidence of blunted sympathetic response and increased vagal tone in the context of fear cues among individuals with PTSD and dissociation compared to individuals with PTSD and unknown levels of dissociation (Seligowski et al., 2019). This finding fits with prior research showing decreased sympathetic activation to trauma or fear-related cues in individuals with dissociation (d'Andrea et al., 2013), although evidence of no difference in sympathetic response based on dissociation in PTSD+ veterans has also been reported (Kaufman et al., 2002). Limited available research makes it challenging to draw conclusions about how dissociation is related to HRV response in the context of stress among trauma-exposed individuals. Thus, a comprehensive examination of the unique relations between ED, dissociation, and PTSD is warranted.
The goals of the current study were to examine associations of ED, dissociation, and PTSD in relation to HR, RSA, and LF/HF ratio following a laboratory-based social-evaluative psychological stressor, the Trier Social Stress Test (TSST) (Kirschbaum et al., 1993), in a sample of trauma-exposed Black women with diabetes, and to determine how ED and dissociation differentially relate to change in HRV post-TSST. This group is relevant for this research question because of the increased vulnerability to chronic trauma exposure and resulting psychological and medical health consequences in urban Black women (Dixon et al., 2020). Since impaired HRV is already present in individuals with type 2 diabetes mellitus (T2DM) and increases risk for further negative health outcomes (Schroeder et al., 2005), better understanding of the psychological factors associated with low HRV in individuals with T2DM could be helpful in efforts to improve health outcomes in this group. We hypothesized that ED would be related to lower RSA and higher LF/HF ratio at each post-stressor time point (T1 = 15 min, T2=30 min, and T3=45 min). We also hypothesized that dissociation symptoms would be related to higher RSA and lower LF/HF ratio at T1. We evaluated specific associations between PTSD diagnosis and HR, RSA, and LF/HF ratio response post-TSST. We hypothesized that PTSD would be related to lower RSA and higher LF/HF ratio at T1. Finally, regarding change over time, we hypothesized that ED would be related to lower initial levels of RSA and higher initial levels of LF/HF ratio and less change in RSA and LF/HF ratio over time, while dissociation symptoms would be related to higher initial levels of RSA and lower initial levels of LF/HF ratio and greater change in RSA and LF/HF ratio over time. Although the focus of the study is on psychophysiological response to stress, baseline levels of HR, RSA, and LF/HF ratio and their associations with the psychological variables of interest were also included.
Material and Methods
Procedure
Participants were 18-65 year old women with T2DM recruited from an ongoing study of risk factors for the development of PTSD from medical clinic waiting rooms at a publicly funded urban hospital (Dixon et al., 2020). Following eligibility determination, participants underwent clinical interviews, blood draw, and TSST protocol. Participants were excluded from the study if they had been diagnosed with bipolar, psychotic, or autoimmune disorders, were currently receiving systemic treatment with a non-steroidal anti-inflammatory drug, glucocorticoid, or anticonvulsant drug (other than gabapentin), or current treatment with an antipsychotic or benzodiazepine. Informed consent was obtained in accordance with the regulations of the Declaration of Helsinki after the procedure was explained in its entirety. Informed consents were approved by the Emory University Institutional Review Board and Grady Research Oversight Committee.
Participants
Participants included 49 Black women (mean age = 51.80 years, SD = 9.69, range = 23-65). Highest education level obtained for the sample was as follows: 20.4% >12th grade education, 30.6% graduated high school/GED, 30.6% had some college or technical school, and 18.4% were college graduates. Regarding household monthly income, 83.0% endorsed <$2,000 household monthly income and 22.4% were employed.
Psychological Measures
Traumatic Events Inventory (TEI).
The TEI is a 14-item screening assessment for history of traumatic events exposure (Gillespie et al., 2009). For this study, sum of trauma exposure encapsulated the lifetime number of types of traumas witnessed or experienced (excluding child abuse).
Childhood Trauma Questionnaire (CTQ).
The CTQ is a 25-item psychometrically sound self-report instrument assessing childhood physical, sexual, emotional abuse and neglect (Bernstein and Fink, 1998). Internal reliability in the current study was high (α = .94). Child maltreatment severity was calculating by summing all categories of maltreatment.
Difficulties in Emotion Regulation Scale, 18 item (DERS-18).
The DERS-18 is a shortened well-validated version (Victor and Klonsky, 2016) of the DERS (Gratz and Roemer, 2004). The DERS-18 assesses difficulty with awareness and understanding of emotions, acceptance of emotions, the ability to engage in goal-directed behavior and restrain impulsive behavior, and the ability to use emotion regulation strategies appropriately. The 18-item version was validated in an urban sample of Black women (Mekawi et al., 2020a). Items were summed to create an overall level of ED (DERS total), which showed high internal consistency in this sample (α = .93).
Multiscale Dissociation Inventory (MDI).
The MDI is a 30-item well-validated self-report measure of past-month dissociative symptomatology across disengagement, depersonalization, derealization, emotional constriction, memory disturbance, and identity dissociation (Brière, 2002). A total measure of dissociative symptoms (MDI total) was used for this study and showed high internal consistency in this sample (α = .93).
Clinician-Administered PTSD Scale (CAPS).
The CAPS is a well-validated clinician administered measure of current PTSD (Weathers et al., 2013). This study used both the CAPS for DSM-IV (CAPS-IV) and DSM-5 (CAPS-5) due to changing over when CAPS-5 was published. Thirty-four percent (n=19) received the CAPS for DSM-IV and 66% received the CAPS-5. In the study, PTSD symptom severity was calculated by the sum of PTSD symptoms1.
Beck Depression Inventory-II (BDI-II).
The BDI-II is a well-validated 21-item self-report measure of current depressive symptoms (Beck et al., 1996). Items were summed to create an overall depression severity score. Internal reliability of the BDI scale in this sample was high (α = .93).
Stressor Task
Trier Social Stress Test (TSST).
The TSST is a 20-minute standardized acute laboratory psychosocial stressor challenge that induces social-evaluative threat (Allen et al., 2017). Before and after the TSST, participants were seated in a quiet room nearby the room where the stressor challenge occurred. The TSST is a well-validated tool that reliably provokes acute subjective and physiological stress responses in the participant (Allen et al., 2017).
Biological Measures
Heart Rate and Heart Rate Variability.
Heart rate (HR) and heart rate variability (HRV) were measured through electrocardiogram (ECG) sensors using the Biopac MP150 for Windows (Biopac Systems, Inc, Goleta, CA) with the BioNomadix wireless ECG amplifier. The wireless amplifier allowed the women to wear the ECG leads continuously during the TSST. Three Ag/AgCl electrodes filled with electrolyte gel were attached to the torso in the lead II position. ECG were sampled at 1000 Hz and analyzed using MindWare HRV module (MindWare Technologies, Ltd, Gahanna, OH). The ECG signal was amplified by a gain of 2000, filtered with a Hamming windowing function, and with a 60-Hz notch filter. HRV was quantified during 1-minute intervals by spectral analysis of the time-sampled inter-beat interval series, according to the methods recommended by the Society for Psychophysiological Research Committee on HRV (Berntson et al., 1997). HF-HRV (RSA) was sampled from 0.12 to 0.40 Hz and was transformed by natural log. HR, RSA, and LF/HF ratio were measured from the 1-min intervals during a baseline pre-stressor time point and at three post-stressor timepoints that were separated by 15-minute intervals. Baseline and post-stressor timepoints T1 (15 min), T2 (30 min), and T3 (45 min) were used in the present study.
Body Mass Index (BMI).
BMI was calculated as: body mass (kg)/(height (m))2. Height and weight were obtained during a physical exam performed by a physician or physician-in-training supervised by a physician prior to the blood draw on the day of the clinical interview.
Hemoglobin A1c.
Whole blood samples were stored at −80°C until the time of assay. Hemoglobin A1c was measured using high performance liquid chromatography by ARUP laboratories (Salt Lake City, Utah).
Data Analysis
Associations between ED, dissociative symptoms, and PTSD with HR, RSA, and LF/HF ratio at baseline and in response to stress in the 45 minutes following the end of the TSST stressor task (T1, T2, T3) were examined. Because depression is related to HRV and trauma load could play a role in these associations, we included these variables in initial correlation analyses. First, we examined distributions of key predictor variables. The level of skewness and kurtosis in this sample fell within acceptable parameters for the sample size on all variables except LF/HF ratio and dissociation (Tabachnick and Fidell, 2001). To reduce high skew for the LF/HF ratio, two outliers were removed for T1, three outliers were removed for T2, and one outlier was removed for T3, which resulted in acceptable levels (Tabachnick and Fidell, 2001). Dissociation was not corrected since dissociation is not normally distributed in the population. Descriptive statistics of the variables of interest were computed (Table 1).
Table 1.
Descriptive characteristics of variables of interest
| Mean (SD, range) | |
|---|---|
| Emotion Dysregulation Total | 28.66 (10.06; 15-53) |
| Dissociation Symptoms | 48.46 (15.21; 30-100) |
| Child Abuse Severity | 37.69 (15.59; 25-100) |
| Overall Trauma Load (no abuse) | 4.74 (2.34; 1-12) |
| PTSD Symptom Severity | 17.66 (13.36; 0-49) |
| Depression Symptom Severity | 14.98 (11.29; 0-44) |
| HR - Baseline | 77.19 (10.98, 56-105) |
| HR – T1 | 81.03 (11.34; 58-107) |
| HR – T2 | 79.61 (12.77; 54-109) |
| HR – T3 | 75.24 (10.27; 55-107) |
| RSA - Baseline | 4.84 (1.66, 2.01-11.19) |
| RSA – T1 | 4.70 (1.37; 1.17-8.07) |
| RSA – T2 | 5.06 (1.61; 1.42-9.73) |
| RSA – T3 | 5.02 (1.58; 1.76-8.96) |
| LF/HF Ratio - Baseline | 2.58 (1.91, 0.16-8.23) |
| LF/HF Ratio – T1 | 2.15 (1.59; 0.26 – 6.71) |
| LF/HF Ratio – T2 | 1.98 (1.66; 0.20-7.82) |
| LF/HF Ratio – T3 | 2.16 (1.68; 0.16-7.36) |
| Body Mass Index | 24.03 (6.74; 18.9-49.8) |
| Hemoglobin A1c | 7.97 (1.95, 4.90-15.40) |
| % (N) | |
| PTSD | 38.8 (19)2 |
N = 49; Note: emotion dysregulation was measured using the DERS; dissociation was measured using the MDI; child abuse severity was measured using the CTQ; trauma load was measured using the TEI; current PTSD diagnosis and symptom severity were measured using the CAPS; current depressive episode was measured using the MINI; current depression symptom severity was measured using the BDI.
Next, bivariate correlations between independent variables of interest (trauma exposure, ED, dissociation, PTSD symptoms, and depression symptoms) and psychophysiological measures (HR, RSA, LF/HF ratio) were examined. Analysis of variance (ANOVA) analyses were run to determine if PTSD diagnosis was associated with mean differences in HR, RSA, and LF/HF ratio at baseline and T1-T3.
Finally, we ran a latent growth curve (LGC) model to assess change specifically in RSA and LF/HF ratio across the timepoints post-TSST to determine how ED and dissociation were related to change in psychophysiological response over time. Compared to only analyzing mean changes in RSA and LF/HF ratio and treating individual differences as error variance, the LGC approach allows us to model observed individual level data in the growth trajectory of RSA and LF/HF ratio over time (Duncan and Duncan, 2009). The intercept was modeled at T1 and, consistent with procedures of assessments which were each 15 minutes apart, we modeled time (across three assessment occasions) as equidistant. Particularly relevant for our research questions, this approach offers the ability to examine the degree to which key predictors (ED and dissociation) exert impact on both the intercept and slope (Curran et al., 2004). Baseline measures of psychophysiology were not included since the goal of this analysis was to examine change in psychophysiological response following the acute stressor. These analyses included 49 total participants, which approaches the recommended minimum sample size of 50 for these analyses (Hamilton et al., 2003). We used the maximum likelihood with robust standard errors (MLR) which is recommended for this type of analysis (Salari et al., 2018). Initial results from bivariate correlation analyses determined other covariates to include in the model at p<.05. Other potential covariates for follow-up analysis were identified based on previous research suggesting associations with RSA and LF/HF ratio: age, income, BMI, and hemoglobin A1c (Antelmi et al., 2004). Due to the small sample size and risk for low power in detecting significant effects, associations between RSA and LF/HF ratio and these potential covariates were assessed to determine if their inclusion was warranted. No significant associations at p<.05 emerged between any of the variables and RSA or LF/HF ratio (see Supplemental Table 1). Collinearity between ED and dissociation was tested and the variance inflation factor (VIF) was 1.74, falling within the normal range. Analyses were conducted with SPSS 26.0 and Mplus Version 8 (Muthén & Muthén, 2017) software packages.
Results
We first calculated Pearson correlation coefficients between ED, dissociation, PTSD symptom severity, trauma load, and depression symptoms. All variables of interest were significantly correlated with one another (r’s = .29-.76, p’s <.05; see Supplemental Table 2). Next, we examined bivariate correlations between variables of interest and psychophysiological measures (HR, RSA, and LF/HF ratio) across baseline and T1-T3. As shown in Table 2, ED and dissociation were significantly positively associated with LF/HF ratio at T3 (p<.05). Child abuse severity was positively associated with HR at baseline and RSA at T3 (p<.05). Depression symptoms was positively associated with RSA at T3 (p<.05). Next, one-way ANOVA tests examined mean differences in HR, RSA, and LF/HF ratio by PTSD status (No PTSD, PTSD) at baseline and each post-stressor time point. PTSD was associated with higher levels of HR at baseline (p<.05). There were no significant mean differences across RSA or LF/HF ratio at any time point by PTSD diagnosis (See Table 3).
Table 2.
Bivariate Pearson’s correlations (r) between variables of interest and HR, RSA, and LF/HF ratio
| Baseline | T1 | T2 | T3 | Baseline | T1 | T2 | T3 | Baseline | T1 | T2 | T3 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | HR | HR | HR | RSA | RSA | RSA | RSA | LF/HF | LF/HF | LF/HF | LF/HF | |
| ED total | .10 | .02 | −.04 | .13 | −0.04 | −.24 | −.22 | −.29 | −.21 | .29 | .26 | .38** |
| Dissociation total | −.06 | −.15 | −0.15 | −.08 | −.02 | −.12 | .01 | −.28 | −.09 | .11 | .10 | .35* |
| Child abuse severity | .31* | .24 | .20 | .19 | −.06 | −.22 | −.18 | −.36* | −.19 | −.03 | .05 | .15 |
| Other trauma exposure | .12 | .04 | .11 | .12 | −.07 | −.06 | .17 | −.15 | .05 | .22 | .09 | .18 |
| PTSD symptom severity | .25 | .26 | .15 | .10 | .03 | −.13 | .12 | −.20 | −.10 | .13 | −.15 | .01 |
| Depression symptom severity | .19 | .14 | .06 | .10 | −.10 | −.24 | .03 | −.36* | −.12 | .19 | −.07 | .18 |
N=49
p < 0.05
p ≤ 0.01
p < 0.001
Note: Emotion dysregulation (ED) was measured using the DERS, dissociation symptom severity was measured using the MDI, child abuse severity was measured using the CTQ, and trauma exposure was measured using the TEI, PTSD symptom severity was measured using the CAPS, and depression symptom severity was measured using the BDI.
Table 3.
Means, Standard Deviations, and One-Way ANOVA for HR, RSA, and LF/HF Ratio over Time by PTSD Status
| Measure | No PTSD | PTSD | ANOVA | ||||
|---|---|---|---|---|---|---|---|
| n=30 (61.2%) | n=19 (38.8%) | ||||||
| M | SD | M | SD | F | p | df | |
| HR | |||||||
| Baseline | 74.63 | 9.79 | 81.80 | 11.82 | 4.46 | .04 | 1,40 |
| T1 | 78.44 | 10.74 | 85.33 | 11.36 | 3.70 | .06 | 1,38 |
| T2 | 77.20 | 11.83 | 84.23 | 13.70 | 2.71 | .11 | 1,36 |
| T3 | 74.52 | 10.25 | 76.75 | 10.60 | 0.38 | .54 | 1,35 |
| RSA | |||||||
| Baseline | 4.84 | 1.81 | 4.84 | 1.43 | 0.00 | .89 | 1,47 |
| T1 | 4.74 | 1.32 | 4.65 | 1.49 | 0.04 | .84 | 1,46 |
| T2 | 4.87 | 1.42 | 5.33 | 1.86 | 0.89 | .35 | 1,42 |
| T3 | 5.13 | 1.32 | 4.83 | 1.98 | 0.27 | .55 | 1,42 |
| LF/HF ratio | |||||||
| Baseline | 2.61 | 1.90 | 2.53 | 1.99 | 0.02 | .89 | 1,45 |
| T1 | 2.14 | 1.65 | 2.17 | 1.54 | 0.01 | .97 | 1,44 |
| T2 | 2.25 | 1.88 | 1.56 | 1.20 | 1.72 | .20 | 1,39 |
| T3 | 2.32 | 1.75 | 1.83 | 1.52 | 0.81 | .37 | 1,40 |
Finally, we ran two unconditional LGC models predicting change in RSA and LF/HF ratio. First, we ran an unconditional LGC model with DERS total (ED), MDI total (dissociation), child abuse severity, and depression symptoms entered as time-invariant predictors of the intercept and slope characterizing the trajectory of RSA. For the intercept and slope, none of the parameters were statistically significant (see Supplemental Table 3). Next, we ran an unconditional LGC model with ED and dissociation entered as time-invariant predictors of the intercept and slope characterizing the trajectory of LF/HF ratio. For the intercept, the parameter for ED was statistically significant and positive (βint=0.06, SE=.03, p=.02), whereas for dissociation, it was not statistically significant (βint= −0.02, SE =.02, p=.27). We found the opposite pattern for the slope, such that the parameter was statistically significant and positive for dissociation (βslope=0.02, SE=.01, p=.02) and not statistically significant for ED (βslope=−0.01, SE=.01, p=.69), see Figure 1. Thus, higher ED was related to higher initial LF/HF ratio independent of change over time while higher dissociation was related to LF/HF ratio increase over time.
Figure 1.
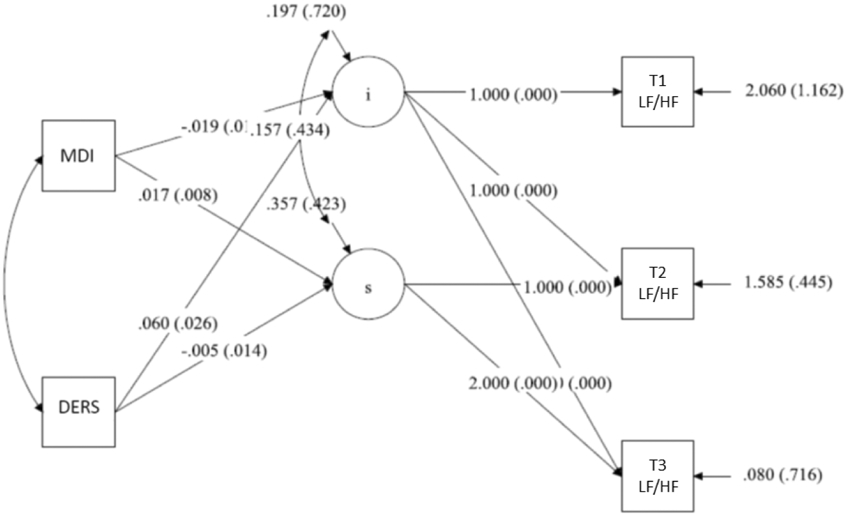
Latent growth model results showing change in LF/HF ratio over first 45 minutes post-stressor and the unique effects of emotion dysregulation (DERS) on initial level of LF/HF ratio and dissociation (MDI) on change in LF/HF ratio over time, standardized betas represented.
Discussion
Impaired autonomic function in the form of low HRV is a known biomarker of PTSD in response to stress exposure (Schneider and Schwerdtfeger, 2020). However, the unique associations of ED and dissociation as transdiagnostic factors involved in PTSD with HRV are less well studied. The current study examined these effects in urban-dwelling trauma-exposed Black women with T2DM, who already are at increased risk for autonomic dysfunction and adverse health outcomes (Dixon et al., 2020), in part due to exposure to chronic trauma and stress in the context of limited socioeconomic resources and racial discrimination (Sibrava et al., 2019). We found significant associations between ED and dissociation with higher LF/HF ratio at 45 minutes post-stressor. In contrast to our hypothesis, we did not find an association between dissociation and higher RSA or lower LF/HF ratio directly following TSST. We also did not find an association between PTSD and RSA or LF/HF ratio in the post-stressor period. It may be that in women with chronic trauma exposure and diabetes, a co-occurring medical condition already characterized by compromised autonomic function, the variability in HRV is better explained by transdiagnostic psychological factors rather than diagnostic symptoms since comorbidity across PTSD and depression is so common. We also did not find any association between psychological symptoms or diagnosis and baseline RSA or LF/HF ratio, although PTSD was associated with higher baseline HR.
In order to examine the impact of ED and dissociation on changes in vagal tone and sympatho-vagal balance over time during the post-TSST recovery, we tested LGC models using RSA and the LF/HF ratio over three post-stressor time points. LGC results showed, in support of our hypothesis, that higher ED predicted higher initial LF/HF ratio post-TSST and that higher LF/HF ratio remained consistent over time. We found a different pattern for dissociation that also partially fit with our hypothesis; dissociation was not associated with initial status of the LF/HF ratio post-TSST, but it did influence the trajectory over time. Specifically, we found that higher dissociation predicted a greater rate of change in LF/HF ratio over time, such that individuals higher on dissociation showed higher LF/HF ratio at later time points from the stressor task compared to those lower on dissociation. Thus, whereas ED predicted higher initial status of LF/HF ratio, dissociation predicted increases in the rate of LF/HF ratio over time. This differential impact of ED and dissociation was only observed in LF/HF ratio and not RSA, but considering the small sample size, more research utilizing larger sample sizes would be beneficial to further examine these effects. The association between ED and higher LF/HF ratio is consistent with prior research suggesting HRV as a biomarker of emotion regulation (Beauchaine, 2015). With ED showing a relatively consistent high LF/HF ratio over time, it suggests that sympathetic dominance may be especially prolonged in individuals who have difficulty regulating emotion.
Overall, the current findings demonstrate the necessity to target trauma-related symptoms in medical populations, including women with diabetes. Trauma exposure and PTSD are related to worse glycemic control and may increase risk for long-term T2DM complications (Dixon et al., 2020). Addressing factors that influence autonomic function in order to improve sympatho-vagal balance could be vital for improving health outcomes in medically ill patients. Although not a focus of the present study, it is critical to acknowledge that race-related stress also contributes to deterioration of physiological and stress-response systems in Black women (Goosby et al., 2018) and ED is a relevant psychological factor to consider in the context of racial discrimination and PTSD within the Black community (Mekawi et al., 2020b). Emotion regulation skills-based interventions adapted for medical settings (Jain et al., 2020) or mindfulness-based interventions (Hopwood and Schutte, 2017) could be promising approaches for addressing ED and dissociation in trauma-exposed medical patients. Regardless of the approach chosen, ensuring that clinicians are trauma-informed and culturally responsive in the implementation of the behavioral health interventions in medical settings is crucial.
Despite its strengths, the current study has limitations that should be kept in mind. First, although a semi-experimental design of the TSST was used to assess autonomic response to stress, assessment of psychological symptoms was cross-sectional, making it impossible for us to determine causality among our variables of interest. Dissociation was measured using a self-report questionnaire. A lack of insight of one’s own dissociative experiences could have underestimated the severity of dissociation within the women studied. Regarding measurement of HRV, LF/HF ratio has received criticism for its use as a measure of sympatho-vagal balance given the complex relation between sympathetic and parasympathetic activity captured in LF (Billman, 2013). Because LF is not simply a reflection of SNS activity, interpretations of LF/HF ratio need to be used with caution (Shaffer and Ginsberg, 2017). The small sample size means that we may not have had enough power to detect small, yet clinically important associations between our variables of interest. We did not correct for multiple testing and thus there is an increased chance of Type I errors making it important to be cautious in the interpretation of our results without replication. We also did not measure nicotine use or physical activity level, both of which can impact psychophysiological activity. Additionally, because our sample was very specific, the findings may be less generalizable to trauma-exposed populations at large. Future studies with the inclusion of non-trauma exposed and non-T2DM control groups may be helpful in disentangling effects and contributors. However, the potential limitation of generalizability is counter-balanced by the public health importance of studying contributors to autonomic dysfunction among Black individuals with high rates of trauma exposure and comorbid mental and physical health problems. Health inequities in low-income Black communities remain high while behavioral health resources are limited. Given high comorbidity between trauma-related disorders and medical conditions in chronically trauma-exposed Black communities, greater access to behavioral health resources in urban medical clinics is critical.
Conclusions
ED and dissociation were related to increased LF/HF ratio during recovery from stress exposure within this sample, suggesting that addressing the transdiagnostic factors of ED and dissociation through behavioral health treatment may be particularly valuable in improving autonomic dysregulation associated with psychological symptoms in medically ill populations. The use of integrated behavioral health interventions to improve outcomes in diabetic patients continues to grow, yet the focus of interventions are most often on depression (Busetto et al., 2016). There remains limited awareness of trauma exposure and PTSD in medical patients, particularly in low-income Black urban communities, and efforts toward improvements in integrated care and connecting patients to relevant resources need to include a focus on trauma-informed care.
Supplementary Material
Highlights.
Trauma impacts physiological function and response to stress
Psychophysiological response to stress was measured in trauma-exposed Black women
Emotion dysregulation was related to sustained sympathetic response to stress
Dissociation was related to a delayed sympathetic response to stress
In this sample, PTSD was not associated with psychophysiological response to stress
Emotion dysregulation must be considered as a treatment target in medical settings
Acknowledgements
We would like to thank Rebecca Hinrichs, MA, Angelo Brown, and all the Grady Trauma Project staff and volunteers for their assistance in data collection and making this research possible. We would also like to thank all the participants for their time and participation.
This work was primarily supported by the National Institute of Mental Health (MH102890 for Powers, MH099211 for Gillespie), the National Institute of Child Health and Human Development (HD071982 for Bradley), the National Heart, Lung, and Blood Institute (T32HL130025 for Kim), and the National Center for Complementary & Integrative Health (K23AT009713 for Powers). Support also included Emory and Grady Memorial Hospital General Clinical Research Center, NIH National Centers for Research Resources (M01 RR00039).
Footnotes
Conflicts of Interest
There are no conflicts of interest to disclose for any of the authors.
In order to combine CAPS-IV and CAPS-5 severity scores together, all scores were weighted to balance the number of items (17 for CAPS-IV and 20 for CAPS-5) and factor in that scoring of frequency and intensity was separate in the CAPS-IV but combined in the CAPS-5.
The majority of women with PTSD had comorbid MDD (58%, n = 11).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allen AP, Kennedy PJ, Dockray S, Cryan JF, Dinan TG, Clarke G, 2017. The trier social stress test: principles and practice. Neurobiology of Stress 6, 113–126. 10.1016/j.ynstr.2016.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antelmi I, De Paula RS, Shinzato AR, Peres CA, Mansur AJ, Grupi CJ, 2004. Influence of age, gender, body mass index, and functional capacity on heart rate variability in a cohort of subjects without heart disease. The American Journal of Cardiology 93(3), 381–385. 10.1016/j.amjcard.2003.09.065 [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, 2015. Respiratory sinus arrhythmia: A transdiagnostic biomarker of emotion dysregulation and psychopathology. Current Opinion in Psychology 3, 43–47. 10.1016/j.copsyc.2015.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A, Steer R, Brown G, 1996. Manual for the Beck Depression Inventory-II. Psychological Corporation, San Antonio, TX. [Google Scholar]
- Benjet C, Bromet E, Karam E, Kessler R, McLaughlin K, Ruscio A, Shahly V, Stein DJ, Petukhova M, Hill E, 2016. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychological medicine 46(2), 327–343. 10.1017/s0033291715001981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein D, Fink L, 1998. Manual for the childhood trauma questionnaire. New York: The Psychological Corporation. [Google Scholar]
- Berntson GG, Thomas Bigger J Jr, Eckberg DL, Grossman P, Kaufmann PG, Malik M, Nagaraja HN, Porges SW, Saul JP, Stone PH, 1997. Heart rate variability: origins, methods, and interpretive caveats. Psychophysiology 34(6), 623–648. 10.1111/j.1469-8986.1997.tb02140.x [DOI] [PubMed] [Google Scholar]
- Billman GE, 2013. The LF/HF ratio does not accurately measure cardiac sympatho-vagal balance. Frontiers in Physiology 4, 26. 10.3389/fphys.2013.00026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brière J, 2002. MDI, Multiscale dissociation inventory: Professional manual. Psychological Assessment Resources, Incorporated. [Google Scholar]
- Brière J, Weathers F, Runtz M, 2005. Is dissociation a multidimensional construct? Data from the Multiscale Dissociation Inventory. Journal of Traumatic Stress, 18, 221–231. [DOI] [PubMed] [Google Scholar]
- Briere J, Kaltman S, Green BL, 2008. Accumulated childhood trauma and symptom complexity. Journal of Traumatic Stress 21(2), 223–226. 10.1002/jts.20317 [DOI] [PubMed] [Google Scholar]
- Busetto L, Luijkx KG, Elissen AMJ, Vrijhoef HJM, 2016. Intervention types and outcomes of integrated care for diabetes mellitus type 2: a systematic review. Journal of Evaluation in Clinical Practice 22(3), 299–310. 10.1111/jep.12478 [DOI] [PubMed] [Google Scholar]
- Curran PJ, Bauer DJ, Willoughby MT, 2004. Testing main effects and interactions in latent curve analysis. Psychological Methods 9(2), 220. 10.1037/1082989x.9.2.220 [DOI] [PubMed] [Google Scholar]
- d'Andrea W, Pole N, DePierro J, Freed S, Wallace DB, 2013. Heterogeneity of defensive responses after exposure to trauma: Blunted autonomic reactivity in response to startling sounds. International Journal of Psychophysiology 90(1), 80–89. 10.1016/j.ijpsycho.2013.07.008 [DOI] [PubMed] [Google Scholar]
- Dixon HD, Michopoulos V, Gluck RL, Mendoza H, Munoz AP, Wilson JG, Powers A, Schwartz AC, Umpierrez GE, Gillespie CF, 2020. Trauma exposure and stress-related disorders in African-American women with diabetes mellitus. Endocrinology, Diabetes & Metabolism 3(2), e00111. 10.1002/edm2.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC, 2009. The ABC’s of LGM: An introductory guide to latent variable growth curve modeling. Social and Personality Psychology Compass 3(6), 979–991. 10.1111/j.1751-9004.2009.00224.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farina B, Speranza AM, Imperatori C, Quintiliani MI, Marca GD, 2015. Change in heart rate variability after the adult attachment interview in dissociative patients. Journal of Trauma & Dissociation 16(2), 170–180. 10.1080/15299732.2014.975309 [DOI] [PubMed] [Google Scholar]
- Forbes D, Fletcher S, Parslow R, Phelps A, O’Donnell M, Bryant RA, McFarlane A, Silove D, Creamer M, 2011. Trauma at the hands of another: longitudinal study of differences in the posttraumatic stress disorder symptom profile following interpersonal compared with noninterpersonal trauma. The Journal of Clinical Psychiatry 73(3), 372–376. 10.4088/jcp.10m06640 [DOI] [PubMed] [Google Scholar]
- Gillespie C, Bradley B, Mercer K, Smith A, Conneely K, Gapen M, Ressler K, 2009. 9Trauma exposure and stress-related disorders in inner city primary care patients. General Hospital Psychiatry 31, 505–514. 10.1016/j.genhosppsych.2009.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gluck R, Hartzell G, Dixon HD, Michopoulos V, Powers A, Stevens J, Fani N, Carter S, Schwartz A, Jovanovic T, Ressler K, Bradley B, Gillespie CF, 2021. Trauma exposure and stress-related disorders in a large, urban, predominantly African American female sample. Archives of Women's Mental Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goosby BJ, Cheadle JE, Mitchell C, 2018. Stress-related biosocial mechanisms of discrimination and African American health inequities. Annual Review of Sociology 44, 319–340. 10.1146/annurev-soc-060116-053403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz K, Roemer L, 2004. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment 26(1), 41–54. 10.1023/b:joba.0000007455.08539.94 [DOI] [Google Scholar]
- Gross JJ, Thompson RA, 2007. Emotion regulation: Conceptual foundations. [Google Scholar]
- Hamilton J, Gagne PE, Hancock GR, 2003. The Effect of Sample Size on Latent Growth Models. Multivariate Behavioral Research 44, 396–406. [Google Scholar]
- Hauschildt M, Peters MJ, Moritz S, Jelinek L, 2011. Heart rate variability in response to affective scenes in posttraumatic stress disorder. Biological Psychology 88(2), 215–222. 10.1016/j.biopsycho.2011.08.004 [DOI] [PubMed] [Google Scholar]
- Hopwood TL, Schutte NS, 2017. A meta-analytic investigation of the impact of mindfulness-based interventions on post traumatic stress. Clinical Psychology Review 57, 12–20. 10.1016/j.cpr.2017.08.002 [DOI] [PubMed] [Google Scholar]
- Jain S, Ortigo K, Gimeno J, Baldor DA, Weiss BJ, Cloitre M, 2020. A Randomized Controlled Trial of Brief Skills Training in Affective and Interpersonal Regulation (STAIR) for Veterans in Primary Care. Journal of Traumatic Stress. 10.1002/jts.22523 [DOI] [PubMed] [Google Scholar]
- Kaufman ML, Kimble MO, Kaloupek DG, McTeague LM, Bachrach P, Forti AM, Keane TM, 2002. Peritraumatic dissociation and physiological response to trauma-relevant stimuli in Vietnam combat veterans with posttraumatic stress disorder. The Journal of Nervous and Mental Disease 190(3), 167–174. 10.1097/00005053-200203000-00005 [DOI] [PubMed] [Google Scholar]
- Kim H-G, Cheon E-J, Bai D-S, Lee YH, Koo B-H, 2018. Stress and heart rate variability: A meta-analysis and review of the literature. Psychiatry Investigation 15(3), 235. 10.30773/pi.2017.08.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirschbaum C, Pirke K-M, Hellhammer DH, 1993. The ‘Trier Social Stress Test’–a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology 28(1-2), 76–81. 10.1159/000119004 [DOI] [PubMed] [Google Scholar]
- Lanius RA, Brand B, Vermetten E, Frewen PA, Spiegel D, 2012. The dissociative subtype of posttraumatic stress disorder: Rationale, clinical and neurobiological evidence, and implications. Depression and Anxiety 29(8), 701–708. 10.1002/da.21889 [DOI] [PubMed] [Google Scholar]
- Mekawi Y, Watson-Singleton NN, Dixon HD, Fani N, Michopoulos V, Powers A, 2020a. Validation of the difficulties with emotion regulation scale in a sample of trauma-exposed Black women. Journal of Clinical Psychology. 10.1002/jclp.23036 [DOI] [PubMed] [Google Scholar]
- Mekawi Y, Watson-Singleton NN, Kuzyk E, Dixon HD, Carter S, Bradley B, Fani N, Michopoulos V, Powers A, 2020b. Racial discrimination and posttraumatic stress: Examining emotion dysregulation as a mediator in an African American community sample. European Journal of Psychotraumatology. 10.1080/20008198.2020.1824398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messman-Moore TL, Bhuptani PH, 2017. A review of the long-term impact of child maltreatment on posttraumatic stress disorder and its comorbidities: An emotion dysregulation perspective. Clinical Psychology: Science and Practice 24(2), 154–169. 10.1111/cpsp.12193 [DOI] [Google Scholar]
- Meyer P-W, Müller LE, Zastrow A, Schmidinger I, Bohus M, Herpertz SC, Bertsch K, 2016. Heart rate variability in patients with post-traumatic stress disorder or borderline personality disorder: relationship to early life maltreatment. Journal of Neural Transmission 123(9), 1107–1118. 10.1007/s00702-016-1584-8 [DOI] [PubMed] [Google Scholar]
- Olff M, Langeland W, Draijer N, Gersons BP, 2007. Gender differences in posttraumatic stress disorder. Psychological Bulletin 133(2), 183. 10.1037/0033-2909.133.2.183 [DOI] [PubMed] [Google Scholar]
- Pencea I, Munoz AP, Maples-Keller J, Fiorillo D, Schultebraucks K, Galatzer-Levy I, Rothbaum BO, Ressler KJ, Stevens J, Michopoulos V, Powers A, 2020. Emotion dysregulation is associated with increased prospectie risk for chronic PTSD development. Journal of Psychiatric Research 121, 222–228. 10.1016/j.jpsychires.2019.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF, 2011. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders 25(3), 456–465. 10.1016/j.janxdis.2010.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers A, Cross D, Fani N, Bradley B, 2015. PTSD, emotion dysregulation, and dissociative symptoms in a highly traumatized sample. Journal of Psychiatric Research 61, 174–179. 10.1016/j.jpsychires.2014.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers A, Fani N, Carter S, Cross D, Bradley B, 2017. Differential predictors of DSM-5 PTSD and ICD-11 complex PTSD among African American women. European Journal of Psychotraumatology. 10.1016/j.jpsychires.2014.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari M, Kazemnejad A, Zayeri F, Daneshvar R, 2018. Comparison of different estimation methods in growth curve models for categorical data: A simulation study. Communications in Statistics-Simulation and Computation 47(6), 1811–1830. 10.1080/03610918.2017.1324982 [DOI] [Google Scholar]
- Schneider M, Schwerdtfeger A, 2020. Autonomic dysfunction in posttraumatic stress disorder indexed by heart rate variability: a meta-analysis. Psychological Medicine 50(12), 1937–1948. 10.1017/s003329172000207x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroeder EB, Chambless LE, Liao D, Prineas RJ, Evans GW, Rosamond WD, Heiss G, 2005. Diabetes, glucose, insulin, and heart rate variability: the Atherosclerosis Risk in Communities (ARIC) study. Diabetes Care 28(3), 668–674. 10.2337/diacare.28.3.668 [DOI] [PubMed] [Google Scholar]
- Seligowski AV, Lebois LA, Hill SB, Kahhale I, Wolff JD, Jovanovic T, Winternitz SR, Kaufman ML, Ressler KJ, 2019. Autonomic responses to fear conditioning among women with PTSD and dissociation. Depression and Anxiety 36(7), 625–634. 10.1002/da.22903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer F, Ginsberg J, 2017. An overview of heart rate variability metrics and norms. Frontiers in Public Health 5, 258. 10.3389/fpubh.2017.00258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibrava NJ, Bjornsson AS, Pérez Benítez ACI, Moitra E, Weisberg RB, Keller MB, 2019. Posttraumatic stress disorder in African American and Latinx adults: Clinical course and the role of racial and ethnic discrimination. American Psychologist 74(1), 101. 10.1037/amp0000339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS, 2001. Using multivariate statistics. [Google Scholar]
- Terock J, Van der Auwera S, Janowitz D, Spitzer C, Barnow S, Miertsch M, Freyberger HJ, Grabe H-J, 2016. From childhood trauma to adult dissociation: the role of PTSD and alexithymia. Psychopathology 49(5), 374–382. 10.1159/000449004 [DOI] [PubMed] [Google Scholar]
- Victor SE, Klonsky ED, 2016. Validation of a brief version of the difficulties in emotion regulation scale (DERS-18) in five samples. Journal of Psychopathology and Behavioral Assessment 38(4), 582–589. 10.1007/s10862-016-9547-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F, Blake D, Schnurr P, Kaloupek D, Marx B, Keane T, 2013. The Clinician Administered PTSD Scale for DSM-5 (CAPS-5)[Measurement Instrument]. [Google Scholar]
- Weissman DG, Bitran D, Miller AB, Schaefer JD, Sheridan MA, McLaughlin KA, 2019. Difficulties with emotion regulation as a transdiagnostic mechanism linking child maltreatment with the emergence of psychopathology. Development and Psychopathology, 1–17. 10.1017/s0954579419000348 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


