Abstract
Few studies have examined the longitudinal trajectory of suicidal ideation (SI) in community samples, particularly during emerging adulthood. Additionally, there is scant data on predictors of longer-term course of SI across this period. We examined multiple domains of adolescent psychosocial and clinical functioning as predictors of SI trajectory and explored whether biological sex moderates those associations. The data came from the Oregon Adolescent Depression Project. Participants completed self-reports of psychosocial and clinical functioning and interviews assessing psychopathology in mid-late adolescence. SI was assessed using up to seven annual mailer assessments spanning ages 19–31. Multilevel growth models found that SI declined across emerging adulthood. Multiple indices of adolescent functioning were associated with higher levels of SI three years later. Few adolescent functioning constructs predicted faster reductions in SI, and no constructs predicted slower longitudinal reductions (or increases) in SI. Similar associations were found when controlling for adolescent SI. Lastly, we found little evidence for sex differences in these associations. This work shows that adolescent functioning is largely associated with initial and enduring levels of SI. Moreover, associations were similar between sexes. Given the modest associations found across long periods of time, future research should focus on proximal risk factors for SI.
Keywords: longitudinal method, suicidal ideation, emerging adulthood, latent growth modeling
Suicide is the second leading cause of death for individuals between 12 and 25 years, and the third leading cause of death for those between 26 and 34 years in the United States (Centers for Disease Control and Prevention [CDC], 2017). Suicidal ideation (SI) frequently precedes suicidal behavior (Bebbington et al., 2010; Victor & Klonsky, 2014). Thus, it is important to understand the factors that influence SI and its course.
A large body of research has examined factors associated with risk for SI using cross-sectional, retrospective designs. For example, in one retrospective study, Kessler and colleagues (1999) compared groups of adolescents and adults aged 15–54 on potential risk factors for suicidal ideation and self-injurious behaviors from the National Comorbidity Survey. The authors found that risk factors for SI, only (relative to making an attempt, having a plan among ideators, making an impulsive attempt without a plan, and planned attempt) were being female, having been previously married (either divorced, separated, or widowed), being less than 25 years old, having lower educational attainment, and being diagnosed with one or more psychiatric disorders. Recent studies have further highlighted additional risk factors for SI in adolescent samples. Several cross-sectional studies find increased risk of SI is linked to difficulties with or insufficient sleep (Goldstein & Frazen, 2020; Li et al., 2016; McKnight-Eily et al., 2011), presence of a mood disorder (Aaltonen et al., 2016; Baldessarini & Tondo, 2003; Kang et al., 2021; Zubrick et al., 2017), family history of psychopathology (Brent et al., 1996; Mars et al., 2019), low socioeconomic status or residing in a single-parent household (Im, Oh, & Suk, 2017; Zubrick et al., 2016), early menarche in female adolescents (Lee et al., 2020), and low self-esteem (Nguyen et al., 2019). While informative, these studies do not address prospective prediction of SI.
There are also a large number of prospective studies examining longitudinal predictors of SI. Franklin et al. (2017) conducted an extensive meta-analysis of longitudinal predictors of self-injurious thoughts and behaviors (STB) among adolescents and adults. The authors found that prior STB, family history of psychopathology or STB, internalizing and externalizing problems, treatment use, and social problems (e.g., experience of abuse, family conflict, stressful life events, or peer problems) were significant predictors of SI. Thus, there is evidence for a wide range of predictors of SI. The authors also found stronger associations with SI within a 6-month follow-up interval than longer follow-up periods. There was considerable variability in the length of follow-up assessments, ranging from 6-months to more than 10 years. However, the length of follow-up for assessing SI (M = 80.72 months, SD = 88.39 months), focusing on risk within a single developmental period. This precluded examining associations across periods, and there was evidence of publication bias for positive findings.
Other studies have examined predictors of the longitudinal course of SI. In these studies, investigators have modelled the course of SI across time and examined predictors of SI trajectories. Studies have primarily focused on identifying group-based trajectories and predictors of membership in those groups (Adrian et al., 2016; Czyz & King, 2015; Giletta et al., 2015; Goldston et al., 2016; Rueter et al., 2008; Wolff et al., 2018). In these studies, typologies generally consist of three groups. In community samples, the largest class includes individuals with consistently low levels of SI. There is frequently a second, smaller, class of initially high but decreasing levels of SI. The third class often varies in shape, with moderate levels or low initial, but increasing, levels of SI. In these group-based trajectory models, higher levels of depressive symptoms, hopelessness, and externalizing problems have been consistently associated with membership in class trajectories with elevated levels of suicidal ideation (Czyz & King, 2015; Giletta et al., 2015; Wolff et al., 2018)
Group-based trajectory models provide appealing descriptions of course for subgroups of individuals. However, there are empirical and interpretational challenges that accompany these models. First, the pattern of results of these studies are consistent with severity classes, such that there are generally low, moderate, and high SI courses identified, which is consistent with observations in the broader literature relying on these methods. The consistency of this pattern across studies varying widely in substantive areas and design characteristics has raised concerns about whether methodological artifacts, rather than substantive trends, drive these results (Sher et al., 2011). Second, the typologies cannot distinguish whether predictors are specifically associated with starting point and/or rate of change. This diminishes the utility of these approaches for understanding exactly what aspects of course these variables predict. Thus, growth curve models describe the sample heterogeneity parsimoniously and permit identifying whether predictors are associated specifically with the intercept or rate of change. Moreover, previous studies have focused on prediction of group membership relying on constructs that were assessed contemporaneous to the start of the trajectories (Czyz & King, 2015; Erausquin et al., 2019; Giletta et al., 2015; Madsen et al., 2016; Prinstein et al., 2008; Wolff et al., 2018). This may inflate the likelihood of finding predictors of the starting points of the trajectories.
Previous studies have also examined sex differences in SI. Multiple studies find that females endorse higher levels of SI (Brownson et al., 2011; Lamis & Lester, 2013; Lewinsohn et al., 2001). However, some studies have found that these sex differences may reverse in late adolescence (Boeninger et al., 2010). Moreover, risk factors for SI may differ between males and females. Cross-sectional studies have found that depression is associated with suicide risk for women, but alcohol problems and poor family support is associated with suicide risk for men (Lamis & Lester, 2013). Others (e.g., Taliaferro & Muehlenkamp, 2014) have reported that increased use of marijuana in males, but depression, sexual abuse, anxiety, running away from home, and engaging in maladaptive behavior in females, are associated with suicidality. Longitudinal studies have also found that higher levels of thwarted belongingness are associated with increased SI in females (Donker et al., 2014). Adrian et al. (2016) found that associations between lower family and peer support, greater externalizing problems, alcohol use and higher likelihood of membership in a high SI trajectory differed between males and females. These findings suggest that there may be sex differences in risk factors for SI during adolescence, but whether these differential associations persist into adulthood is unknown.
The transition between adolescence and adulthood, termed emerging adulthood, is marked by self-discovery, change in education, romantic life, and overall interests (Arnett, 2000). Multiple authors have highlighted that SI persists into emerging adulthood, and contributes to significant distress and impairment in social, occupational, and academic domains (Goldston et al., 2016; Nkansah- Amankra, 2013). During adolescence, SI typically peaks between ages 12 and 17 years (Rueter & Kwon, 2005). Research using data from the National Comorbidity Survey–Adolescent Supplement reported a lifetime prevalence of SI of 12.1% (Nock et al., 2013) and a 12-month prevalence of 3.6% (Husky et al., 2012). Twelve-month prevalence rates for emerging adults between ages 18 to 25 increase, ranging from 6.1% to 8.3% (Han et al., 2018). Rates of 12-month SI decrease modestly in adults between 26–49 years of age (4.0%) and among older adults 50 years and above (2.5%; Han, McKeon, & Gfroerer, 2014). However, few studies have examined the course of SI across developmental periods (Franklin et al., 2017). Given that rates of SI peak in emerging adulthood, this period warrants particular attention with regards to examination of the developmental trajectory and associated correlates of SI over time.
In this study, we capitalize on a large prospective study beginning in adolescence to examine the associations between adolescent psychosocial and clinical functioning and parental history of depressive, anxiety, and substance use disorders and course of SI. We also explore sex differences in these associations. The trajectories of SI spanned late adolescence into adulthood. We include a multiyear gap between the assessment of risk factors and SI trajectories to ensure that the risk factors temporally precede the SI trajectory. We hypothesized that adolescent psychopathology, low social support, life stressors, and family history of psychopathology would predict trajectories of SI during adulthood. We also hypothesized that associations for depressive and other internalizing symptoms, and life stressors with SI trajectories would be larger for females than males (Lewinsohn et al., 1996; Prinstein et al., 2008), and externalizing symptoms and substance use would be stronger predictors of SI for males than for females.
Method
Participants and Procedure
Data come from the Oregon Adolescent Depression Project (OADP) (Lewinsohn et al., 1993), a longitudinal study of students recruited from nine high schools in Western Oregon in 1987. The OADP sample included 1,709 participants (ages 13–20, Mage = 16.56 years, SD = 1.19 years) (Lewinsohn et al., 1993). Participants were invited to complete seven annual self-report assessments examining SI. Participants differed in age at the start and finish of the mailer assessments, ranging from age 19 at the beginning to age 31 at the end. For the purposes of this study, we only included participants who had completed the T1 assessment and had at least one mailer assessment. The current study sample included 1,417 individuals. Just over half of the sample (54.9%) were female. The sample was predominantly White (91.7%). Nearly half (46.80%) of the participants had at least one parent who graduated with a four year degree. On average, participants completed 5.61 mailer assessments (range: 1–7; SD = 1.69).
Measures
Suicidal Ideation.
Suicidal ideation was assessed using a four-item screener (Lewinsohn et al., 1996). The items included: “I thought about killing myself”, “I had thoughts about death”, “I felt that my family and friends would be better off if I was dead”, and “I felt that I would kill myself if I knew a way”. Participants responded on a 4-point frequency scale. The screener questionnaire had participants respond to the items on a 1–4 scale with higher scores reflecting higher SI (total scores range from 4–16). The presence of SI within the last week was rated as occurring (1 = rarely/none of the time, 2 = some/a little of the time, 3 = occasionally/a moderate amount of time, and 4 = most/all of the time). The screener was administered at T1 (alpha = .81) and in the mailer assessments (mean alpha = .75; range = .68–.80).
Diagnostic Measures.
At T1, all adolescent participants were interviewed, but not a caregiver, with the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS; Orvaschel et al., 1982). This interview was conducted by trained Masters-level clinicians. Diagnoses were reviewed by a senior clinician and adhered to criteria from the Diagnostic and Statistical Manual of Mental Disorders–Third edition Revised (DSM-III-R; American Psychiatric Association, 1980). All interviews were audio or video recorded. A subset of interviews (n = 263) were coded for reliability. Inter-rater reliability was good to excellent for MDD (κ = 0.86), anxiety disorders (κ = 0.60), and substance use disorders (κ = 0.84) (Lewinsohn et al., 2001). Lifetime rates of MDD, anxiety disorders, and substance use disorders (SUD) were 20.39%, 8.32%, and 7.76%, respectively.
Self -Report Measures.
Participants completed an extensive battery of measures to assess multiple psychosocial and clinical constructs at T1. All measures had been previously shown to have good psychometric properties (Lewinsohn et al., 1993). All variables examined were scored so that higher values indicate poorer functioning. We examined depressotypic cognitions, depressotypic attributions, coping skills, emotional reliance, self-esteem, social competence, interpersonal conflict with parents, family support, peer support, minor life stressors, major life stressors, and T1 baseline ideation as adolescent predictors of SI trajectories. Details about the individual instruments administered are provided in the online supplementary materials. Individual measures were standardized and averaged to yield construct scores with coefficient alphas ranging from .59 to .83 (median = .75).
Parental History of Psychopathology.
A subset of OADP participants who were oversampled for a personal history of psychopathology were selected for a family study when the participants were approximately 24 years old (Klein et al., 2001). First-degree family members were interviewed using the Structured Clinical Interview for DSM-IV, non-patient version (SCID-NP; First et al., 1996). In addition, family history data were collected from the original OADP participants and at least one other family member using a modified version of the Family Informant Schedule and Criteria (FISC; Mannuzza & Fyer, 1990), supplemented with items necessary to derive DSM-IV diagnoses. Interviews were conducted without knowledge of offspring diagnoses. Of the 1,417 probands included in this study, diagnostic information was available for 770 mothers (54.3%) and 753 (53.1%) fathers. Of those, direct interviews were conducted with 573 (74.4%) mothers and 350 (46.5%) fathers.
As multiple data sources were available for many parents, we derived lifetime best-estimate DSM-IV diagnoses from all available information (Leckman et al., 1982). Two diagnosticians, from a team of four senior clinicians, independently derived best-estimate diagnoses without knowledge of offspring diagnoses. Disagreements were resolved by consensus. Interrater reliability of the independently derived best-estimate diagnoses prior to the resolution of discrepancies was excellent for MDD (κ = .91), any anxiety disorder (κ = .94), alcohol use disorder (AUD) (κ = .97), and substance use disorder (SUD) (κ = .96).
Data Analysis
We focused on 16 adolescent and three parental predictors of suicidal ideation. Analyses were conducted using multilevel models using the robust maximum likelihood estimator in Mplus 8.3 (Muthén & Muthén 1998–2015). First, we estimated an unconditional growth model to describe the overall trajectory of suicidal ideation from late adolescence into adulthood. Second, as many of the predictor variables covary, we estimated a series of conditional growth models with individual constructs predicting growth parameters of SI trajectories. Third, we examined associations between each construct and SI trajectories when controlling for adolescent self-report of SI. Missing data was accommodated using FIML estimation methods. These analyses examined whether predictors in adolescence were uniquely associated with later course of SI beyond the influence of SI in adolescence. Finally, we examined whether the relationships between psychosocial constructs and trajectories of SI were moderated by sex. Significant interactions were probed using methods from Aiken et al. (1991).
Results
Unconditional Model
The first model examined the normative change in SI across the seven assessment points. Age at mailer assessments was centered at age 20 (fewer than 1% of observations were available earlier than age 19, hence centering at age 19 would lead to estimates based on modest amounts of information) for all analyses to maintain a uniform meaning of the intercept across participants. The estimated average level of SI was 4.49 (SE = 0.038, t = 119.38, p < .001) and the average rate of change in SI was −.016 (SE = .006, t = 2.596, p < .01; Figure 1). There was significant variability in the starting point of SI (variance component = .391, SE = .063, t = 6.155, p < .001); however, there was non-significant variability in rate of change in SI (variance component < 0.001, SE = .002, t = .130, p = .896). This suggests that there is a homogenous trajectory of SI; however, we examined prediction of both the intercept and slopes (Singer & Willett, 2003).
Figure 1.
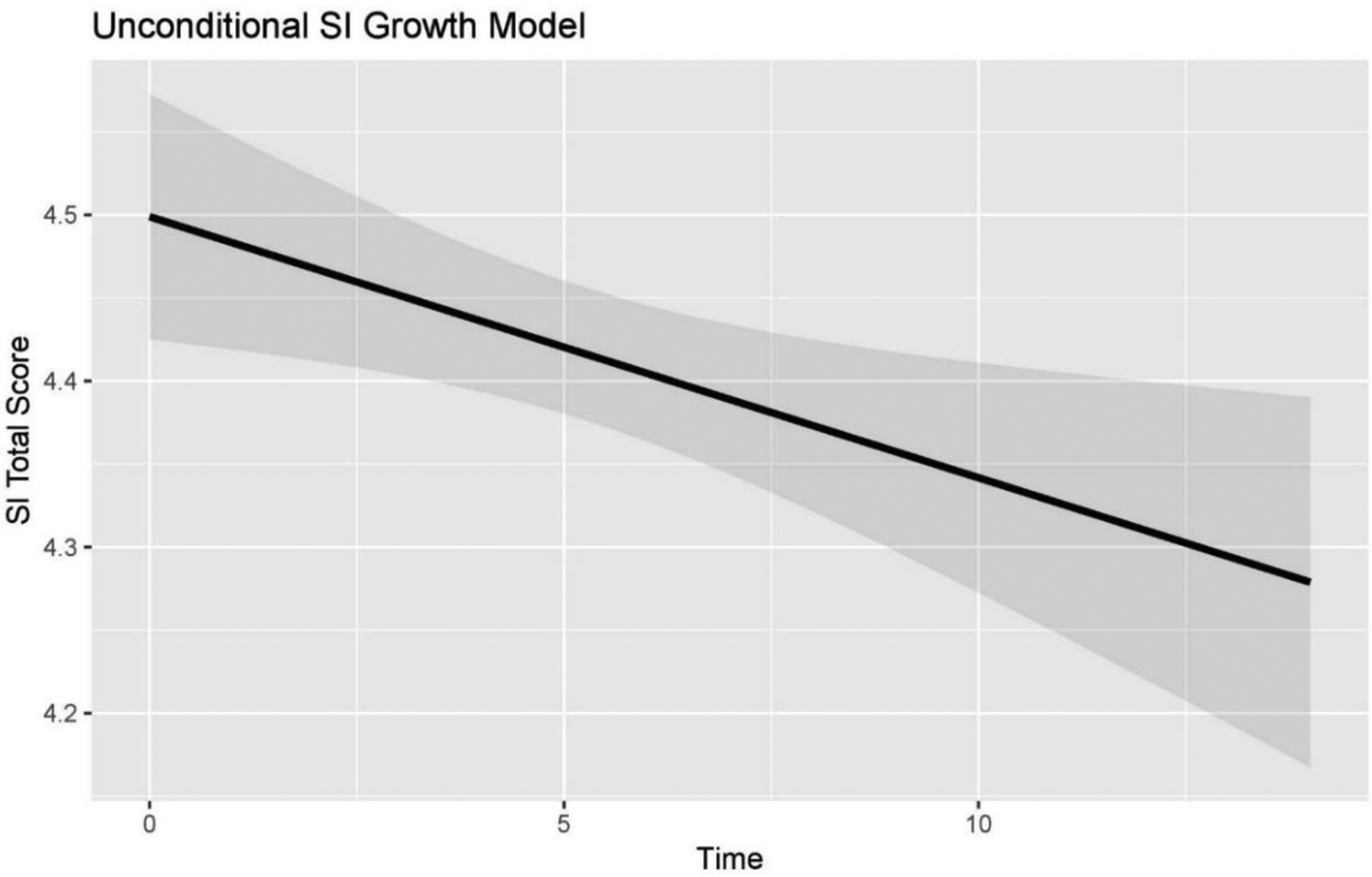
Unconditional SI growth model from age 20–32. Time is reflected in years.
Note: The figure above reflects the overall trajectory of suicidal ideation across time between ages 19–31 years.
Conditional Models
We estimated models with predictors of the intercept and slope parameters in separate analyses. Results are presented in (Table 1, left panel). In these models, we found that higher levels of all constructs, except for adolescent and parent lifetime histories of anxiety, were associated with higher SI intercepts approximately three years after the baseline assessment. We also found that higher depressotypic cognitions, poorer coping skills, parental lifetime depression, more major life stressors, and greater SI at baseline were associated with faster reductions in SI.
Table 1.
Predictors of Suicidal Ideation
| Model 1 Intercept | Model 1 Slope | Model 2 Intercept | Model 2 Slope | |||||
|---|---|---|---|---|---|---|---|---|
| b (SE) | z | b (SE) | z | b (SE) | z | b (SE) | z | |
| Suicidal Ideation at T1 | ||||||||
| T1 Baseline Ideation | .23 (.06)** | 3.64 | −.03 (.01)* | −2.49 | -- | -- | -- | -- |
| Biological Sex | ||||||||
| Male Biological Sex | .23 (.08)** | 3.05 | −.02 (.01) | −1.51 | .31 (.14)* | 2.23 | −.04 (.02) | −1.84 |
| Parental Psychopathology | ||||||||
| Parental Lifetime Depression | .46 (.12)** | 3.75 | −.04 (.02)* | −2.19 | .27 (.22) | 1.26 | .00 (.03) | −0.13 |
| Parental Lifetime Anxiety | .26 (.15) | 1.68 | −.03 (.02) | −1.20 | .21 (.25) | .82 | −.02 (.04) | −0.59 |
| Parental Lifetime Substance Use | .25 (.11)* | 2.34 | −.03 (.02) | −1.86 | .12 (.20) | .61 | .00 (.03) | 0.05 |
| Adolescent Psychopathology | ||||||||
| Lifetime Depression | .40 (.11)** | 3.52 | −.03 (.02) | −1.70 | .41 (.18)* | 2.32 | −.02 (.02) | −.079 |
| Lifetime Anxiety | .22 (.17) | 1.26 | −.01 (.03) | −0.27 | .20 (.23) | .87 | .01 (.03) | 0.29 |
| Lifetime Substance Use | .41 (.18)* | 2.24 | −.03 (.03) | −1.11 | .48 (.31) | 1.58 | −.07 (.04) | −1.64 |
| Depressive Thinking | ||||||||
| Depressotypic Attributions | .23(.06)** | 3.96 | −.02 (.01) | −1.73 | .35 (.10)** | 3.44 | −.03 (.01)* | −2.13 |
| Depressotypic Cognitions | .31 (.08)** | 3.68 | −.02 (.01)* | −1.96 | .41 (.13)** | 3.06 | −.03 (.02) | −1.62 |
| Social Support | ||||||||
| Family Support | .25 (.06)** | 3.83 | −.01 (.01) | −1.00 | .35 (.11)** | 3.09 | −.01 (.02) | −0.82 |
| Peer Support | .28 (.08)** | 3.40 | −.01 (.01) | −0.93 | .33 (.12)** | 2.87 | −.01 (.02) | −0.73 |
| Interpersonal Factors | ||||||||
| Coping Skills | .03 (.01)** | 4.63 | .00 (.00)* | −2.25 | .03 (.01)** | 3.23 | .00 (.00) | −1.63 |
| Emotional Reliance | .02(.01)** | 2.84 | .00(.00) | −1.52 | .02(.01) | 1.50 | .00(.00) | −0.34 |
| Self-Esteem | .17 (.06)** | 2.99 | −.01 (.01) | −1.57 | .23 (.11)* | 2.16 | −.01 (.02) | −0.75 |
| Interpersonal conflict with parents | .16 (.06)** | 2.83 | −.01 (.01) | −1.38 | .18 (.09)* | 2.01 | −.02 (.01) | −1.36 |
| Social Competence | .36 (.11)** | 3.36 | −.02 (.02) | −1.27 | .40 (.16)* | 2.58 | −.01 (.03) | −0.52 |
| Life Stressors | ||||||||
| Minor Life Stressors | .02 (.00)** | 3.73 | .00 (.00) | −1.55 | .02 (.01)* | 2.56 | .00 (.00) | −1.42 |
| Major Life Stressors | .02 (.01)** | 2.91 | .00 (.00)* | −2.11 | .02 (.01) | 1.48 | .00 (.00) | −1.23 |
Note:
p<0.01,
p<0.05.
Model 1: Intercept and slope of predictors associated with SI trajectory. Model 2: Intercept and slope of predictors that were significantly associated with SI trajectory after controlling for T1 baseline ideation. Higher predictor values reflect poorer functioning.
A second set of analyses was conducted to examine whether adolescent and parental predictors of SI accounted for additional variance beyond SI in adolescence after controlling for baseline SI. We repeated the same set of analyses and included T1 baseline ideation as a covariate in each of the models (Table 1, right panel). When controlling for SI at T1, adolescent lifetime history of depression, greater depressotypic attributions and depressotypic cognitions, poorer coping skills, lower self-esteem, greater interpersonal conflict with parents, poorer family support, peer support, and social competence, and more minor life stressors were associated with higher SI approximately three years after the baseline assessment. We also found that males had higher SI intercepts than females. Only higher levels of depressotypic attributions were associated with a more rapid rate of decline in SI (Figure 2).
Figure 2.
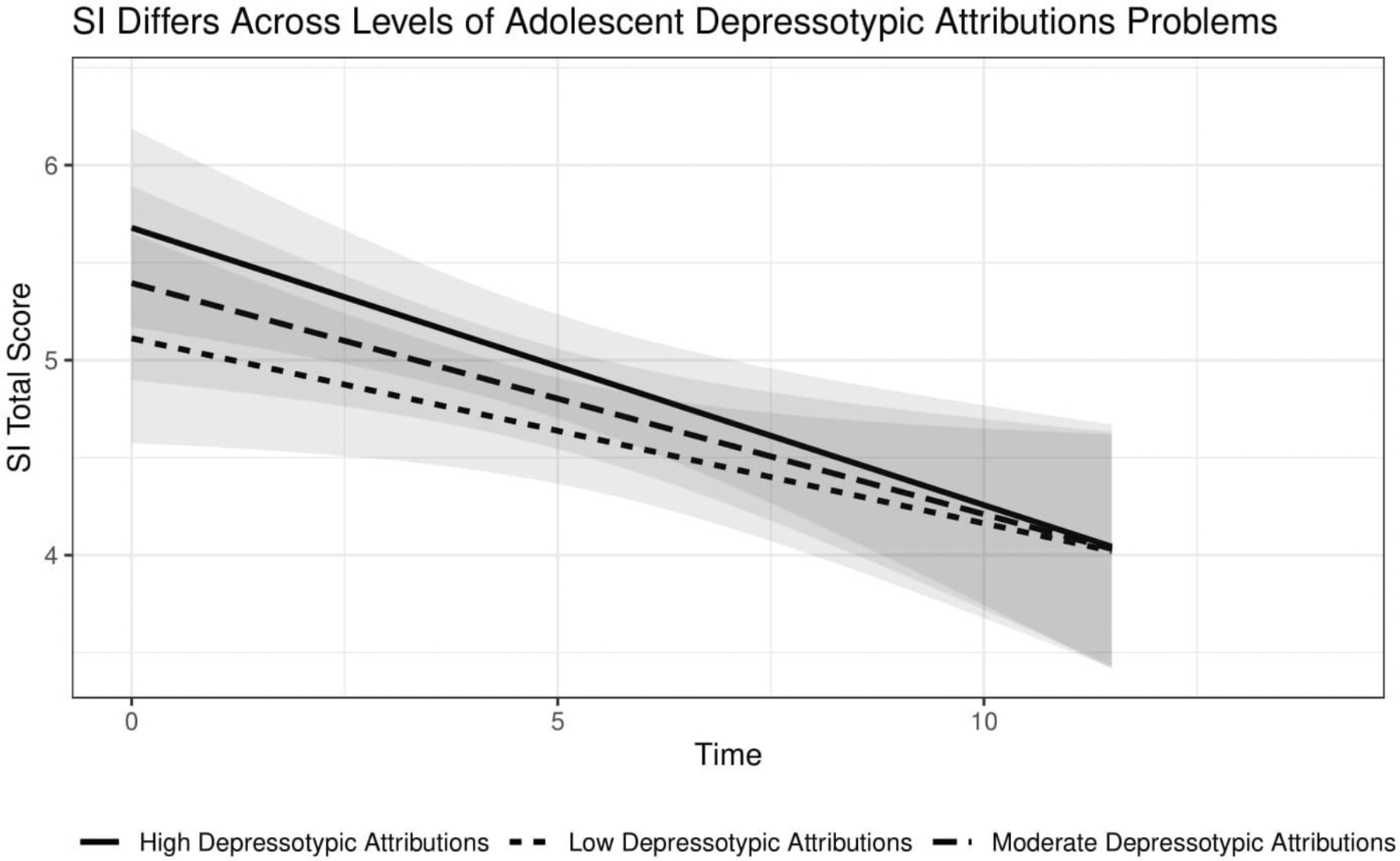
Conditional growth model of SI for Depressotypic attributions.
Note: The time X depressogenic attributions interaction was significant. The rate of change in SI across time was also significant at low (β= −.095, SE= .044, z = −2.142, p < 0.05), moderate (β= .119, SE= .043, z = −2.763, p < 0.01), and high (β= −.142, SE= .044, z = −3.207, p < 0.01) levels of depressotypic attributions
Moderation by Sex
Finally, we examined differences in sex specific predictors of SI (Table 2). In these models, we found no significant interactions between sex and any adolescent psychosocial or clinical construct, adolescent psychopathology, or parental psychopathology and SI three years later. However, interactions between sex and parental lifetime anxiety (β = −.11, SE = .051, p < .05) and adolescent minor life stressors (β = .002, SE = .001, p < .05) were associated with the SI slope. Comparisons of simple slopes analyses found that males with positive parental history of anxiety disorders (β = −.115, SE = .041, p < .05) experienced faster declines in ideation than males without parental history of anxiety (β = −.021, SE = .011, p = .065) and females with (β = .003, SE = .024, p = .915) and without (β = −.013, SE = .013, p = .300) a parental history of anxiety (Figure 3). Similarly, comparisons of simple slopes analyses found that adolescent males with a higher number of minor life stressors (β = −.024, SE = .010, p < .05), males with fewer minor life stressors (β = −.028, SE = .010, p < .05) and females with a higher number of minor life stressors (β = −.019, SE = .011, p = .079) had steeper declines in SI across time than adolescent females with fewer minor life stressors (β = .002, SE = .007, p = .746; Figure 4). No other significant interactions were identified.
Table 2.
Sex Moderating the Influence of Predictors on Suicidal Ideation
| Intercept | Slope | |||||
|---|---|---|---|---|---|---|
| Predictor | Sex | Predictor × Sex | Predictor | Sex | Predictor × Sex | |
| Variable | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) |
| Suicidal Ideation at T1 | ||||||
| T1 Baseline Ideation | .16 (.03)** | .26 (.08)** | .01 (.07) | −.01 (.01)* | −.02 (.01) | .00 (.01) |
| Parental Psychopathology | ||||||
| Parental Lifetime Depression | .46 (.12)** | .20 (.11) | −.03 (.25) | −.04 (.02)* | −.03 (.02) | .00 (.04) |
| Parental Lifetime Anxiety | .30 (.16) | .19 (.11) | .62 (.32) | −.04 (.03) | −.03 (.02) | −.11 (.05)* |
| Parental Lifetime Substance Use | .25 (.11)* | .21 (.11) | −.23 (.22) | −.03 (.02) | −.03 (.03) | .03 (.03) |
| Adolescent Psychopathology | ||||||
| Lifetime Depression | .50 (.14)** | .32 (.08)** | .12 (.29) | −.03 (.02) | −.02 (.01) | .05 (.04) |
| Lifetime Anxiety | .28 (.15) | .25 (.08)** | .00 (.30) | −.02 (.02) | −.02 (.01) | −.03 (.05) |
| Lifetime Substance Use | .44 (.19)* | .24 (.08)** | .15 (.39) | −.03 (.03) | −.02 (.01) | .01 (.06) |
| Depressive Thinking | ||||||
| Depressotypic Attributions | .22 (.05)** | .24 (.08)** | −.10 (.11) | −.01 (.01) | −.02 (.01) | .02 (.02) |
| Depressotypic Cognitions | .30 (.08)** | .23 (.08)** | −.12 (.17) | −.02 (.01) | −.02 (.01) | .02 (.03) |
| Social Support | ||||||
| Family Support | .26 (.06)** | .24 (.08)** | .15 (.13) | −.01 (.01) | −.02 (.01) | −.03 (.02) |
| Peer Support | .27 (.08)** | .21 (.08)* | −.12 (.17) | −.01 (.01) | −.02 (.01) | .03 (.03) |
| Interpersonal Factors | ||||||
| Coping Skills | .03 (.01)** | .23 (.08)** | .00 (.01) | .00 (.00)* | −.02 (.01) | .00 (.00) |
| Emotional Reliance | .02 (.01)** | .27 (.08)** | .02 (.01) | .00 (.00) | −.02 (.01) | .00 (.00) |
| Self-Esteem | .25 (.07)** | .34 (.09)** | .06 (.13) | −.02 (.01)* | −.03 (.01)* | −.01 (.02) |
| Interpersonal conflict with parents | .17 (.06)** | .25 (.08)** | −.04 (.11) | −.01 (.01) | −.02 (.01) | .00 (.02) |
| Social Competence | .35 (.11)** | .21 (.08)* | −.08 (.21) | −.02 (.02) | −.02 (.01) | .01 (.03) |
| Life Stressors | ||||||
| Minor Life Stressors | .02 (.00)** | .23 (.08)** | −.01 (.01) | .00 (.00) | −.02 (.01) | .00 (.00)* |
| Major Life Stressors | .03 (.01)** | .26 (.08)** | .02 (.02) | .00 (.00)* | −.02 (.01) | .00 (.00) |
Note:
p<0.01,
p<0.05.
Table presents unstandardized regression coefficients. Higher predictor values reflect poorer functioning.
Figure 3.
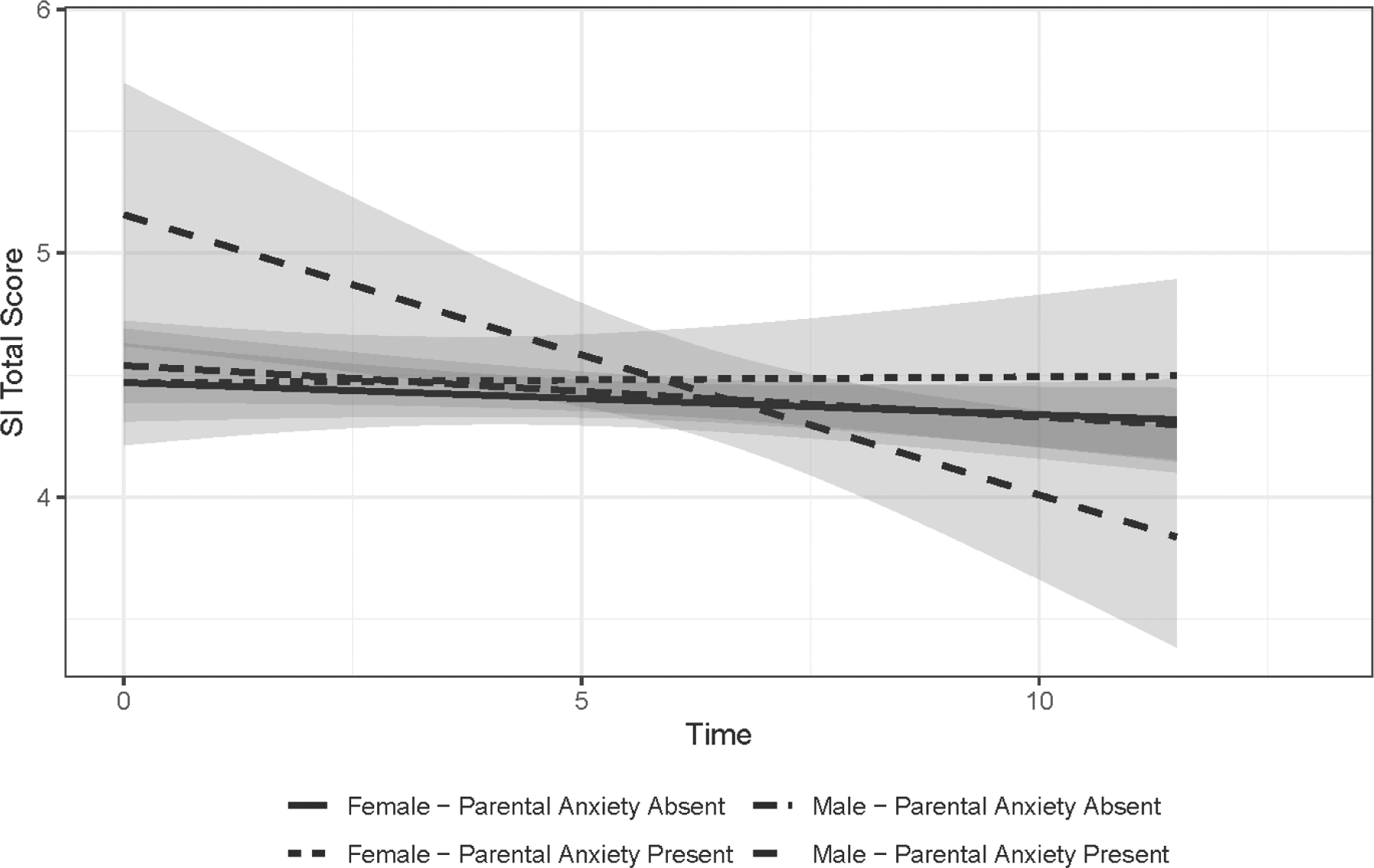
Interactions between biological sex and parental anxiety.
Note: The time X Sex X Parental Anxiety interaction was significant. We found significant associations between the predictor and SI for the slope such that rate of change in SI across time was faster for males with parental history of anxiety (β = −.115, SE = .041, z = −2.820 p < 0.05) than males without parental history of anxiety (β = −.021, SE = .011, z = −1.848 p = .065) and females with (β = .003, SE = .024, z = .107 p = .915) and without (β = −.013, SE = .013, z = 1.037, p = .300) parental history of anxiety.
Figure 4.
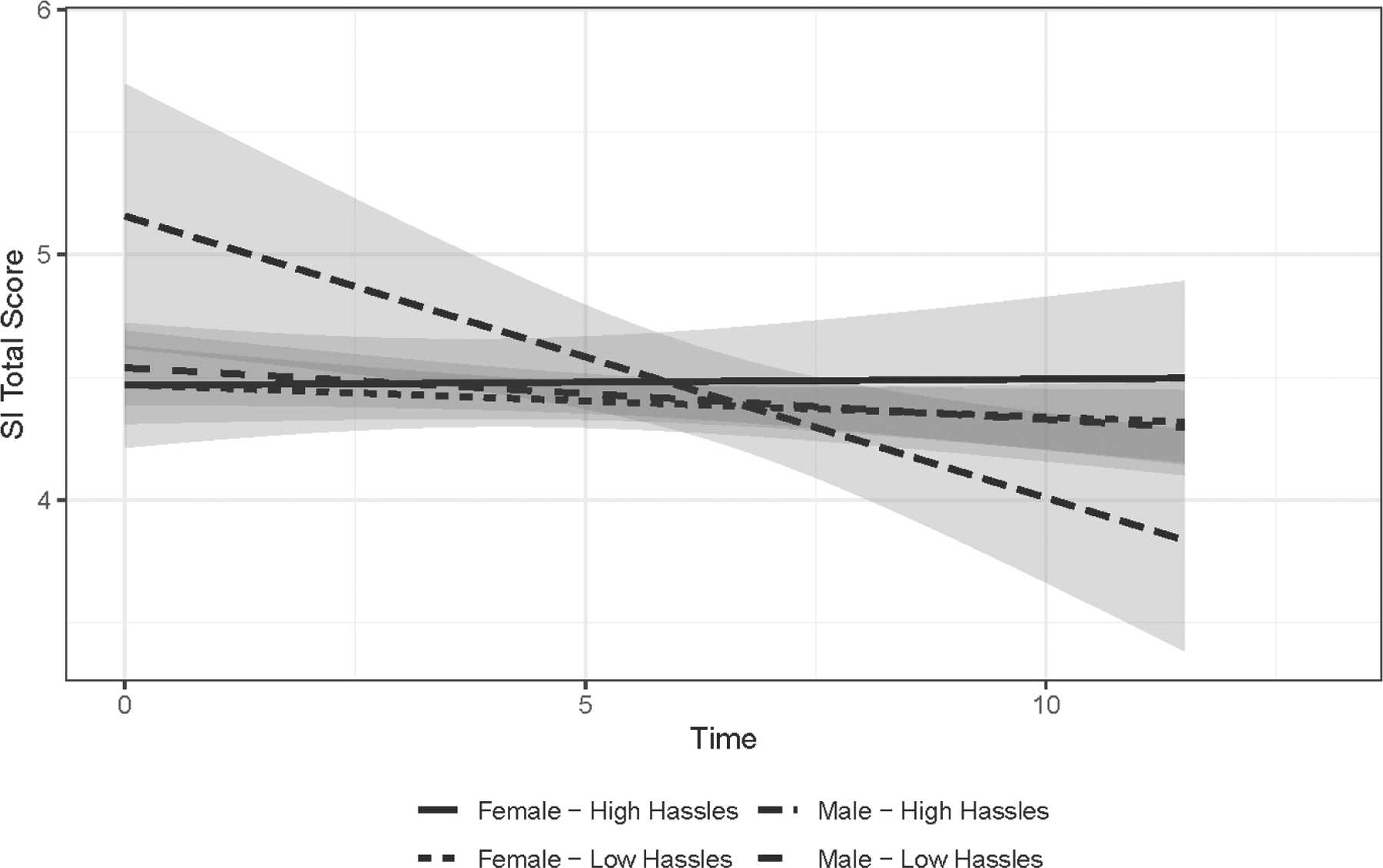
Interactions between biological sex and minor life stressors
Note: The time X Sex X Hassles interaction was significant. We found significant associations between the predictor and SI for the slope such that rate of change in SI across time was faster for males with a higher number of minor life stressors/hassles (β = −.024, SE = .010, z = −2.325, p < .05), males with low minor life stressors/ hassles (β = −.028, SE = .010, z = −2.873, p < .05), and females with a higher number of minor life stressors/ hassles (β = −.019, SE = .011, z = −1.756, p = .079), than females with low minor life stressors/ hassles (β = .002, SE = .007, z = .324, p = .746).
Discussion
SI is a serious mental health concern for adolescents and young adults (Law & Shek, 2016; Prinstein et al., 2008) as it is associated with risk to escalation for suicidal behaviors. This study examined adolescent predictors of SI trajectory in emerging and early adulthood and explored whether sex moderated associations between focal predictors and SI trajectory. We found that the normative pattern of SI was characterized by a declining trajectory from emerging to early adulthood. Further, when controlling for SI, multiple measures of adolescent functioning were associated with higher levels of SI approximately three years later, but there were few associations with rates of change in SI. Lastly, we found limited support for sex differences in the associations between adolescent functioning and SI course.
We estimated models with and without controlling for baseline SI in adolescence. Overall, we found that most independent variables continued to predict higher SI intercepts in both models. This suggests that a wide range of risk factors (e.g., depressotypic cognitions, depressotypic attributions, social competence, interpersonal conflict with parents, family support, peer support, and male biological sex) are associated with greater SI approximately three years later. Many of these predictors were also previously identified in studies of risk for SI in adolescence (Goldston et al., 2016; Prinstein et al., 2008). However, those previous studies, integrated by Franklin et al. (2017), consisted of studies that largely relied on predictions within a single developmental period. Here, we show that these variables continued to predict level of SI into emerging and early adulthood.
However, we found fewer associations between adolescent functioning and change in SI than for the SI intercept. When not controlling for adolescent SI, T1 SI, parental lifetime depression, depressotypic cognitions, coping skills, and major life stressors were associated with more rapid reductions in SI. Thus, these results are consistent with individuals with higher initial levels of SI returning to normative levels with time.
When controlling for adolescent SI, nearly all association between predictors and the slope were no longer statistically significant. In these analyses, only higher depressotypic attributions in adolescence predicted a more rapid decrease in SI levels in emerging adulthood. We cannot rule out that this was a spurious finding. This finding contrasts with previous longitudinal research in adolescents that found that negative attributional styles were prospectively associated with increases in SI over time even after controlling for baseline depression and SI rates (Abramson et al., 1989; Burke et al., 2016; Joiner & Rudd, 1995; Priester & Clum, 1992). Moreover, both cross-sectional (Schwartz et al., 2000; Wagner et al., 2000) and longitudinal (Kleiman et al., 2012) studies with adolescents have found associations between a positive attributional style and reductions in SI. However, these previous studies have been conducted over shorter periods of time than the present study. Nonetheless, the association between depressotypic attributions and course of SI when controlling for adolescent SI should be interpreted with caution.
In contrast to the majority of the literature on SI (Becker, Holdaway, & Luebbe, 2018; Brownson et al., 2011; Kann et al., 2018; Lamis & Lester, 2013; Lewinsohn et al., 2001; Turecki & Brent, 2016), we found that males had higher levels of SI than females in emerging adulthood. However, this is consistent with some studies reporting higher levels of SI in males in this period ((Boeninger et al., 2010; Ibrahim et al., 2017). We also examined sex differences in the relationships between adolescent functioning, parental lifetime history of psychopathology and trajectories of SI in emerging adulthood. We hypothesized that the associations between course of SI and depressive symptoms, internalizing symptoms, and life stressors would be stronger for girls, whereas relationships with externalizing problems, alcohol, and substance use behaviors would be stronger for boys. Contrary to our hypotheses, we found no sex differences in the prediction of SI at age 20. However, we found some interactions that predicted the slope. These interactions showed that there were declines in SI across time for male participants with a family history of anxiety and with higher levels of minor life stressors, but these factors did not influence SI trajectory for females or males without a family history of anxiety or with low levels of minor life stressors. However, given the exploratory nature of these analyses we cannot rule out the possibility that they are due to chance.
The current study of SI trajectory has implications for prevention. When controlling for T1 baseline ideation, most factors (e.g., coping skills, biological sex, minor life stressors, interpersonal conflict with parents) were associated with higher levels of SI multiple years following the initial assessments. Thus, a number of these constructs may be targets of intervention. Coping skills could be developed or enhanced; responses to minor stressors could be addressed; or conflict with parents could be targeted in interventions. However, only some of these factors were also associated with more rapid decline in SI. Thus, these influences appear to be reflecting levels of SI that persist across the surveillance period. Our findings suggest that multiple factors, including depressotypic cognitions and attributions, family and peer functioning, and coping skills, could be prevention targets in adolescence to reduce the longer-term experience of SI in emerging adulthood.
The study benefitted from a large cohort with longitudinal assessments of SI in emerging adulthood. We also assessed multiple domains of potential risk factors for SI. However, these findings should also be interpreted in the context of a number of limitations. First, levels of SI were modest. Thus, we describe normative changes for a community sample, but are not able to speak to longitudinal changes for more severe populations. Second, the sample had modest racial and ethnic diversity. As prior research has suggested that trajectory of SI differs across race and ethnicity, it may limit the generalizability of our findings (Erausquin et al., 2019). Third, although we had longitudinal assessments of SI, we did not examine measures of other near-neighbor constructs, including non-suicidal self-injury (NSSI) and suicidal gestures and attempts (May & Klonsky, 2016; Taliaferro & Muehlenkamp, 2014). Thus, we cannot speak to how the constructs examined here are implicated in severe suicidal and self-injurious behaviors. Future longitudinal research including measures assessing associated self-injurious behavior and outcomes will allow us to understand and better isolate specific markers associated with SI trajectory.
This study highlights that SI declines through emerging adulthood. Poorer psychosocial and clinical functioning in adolescence was associated with higher levels of SI three years later and continuing over a seven year follow-up period, even when controlling for adolescent SI. However, we did not find any associations with increased slopes of SI beyond the effects of adolescent SI, and only a few variables predicted reductions in SI over time. Moreover, we found modest evidence for sex differences in the relationships between psychosocial and clinical functioning in adolescence and SI in early adulthood.
Supplementary Material
Acknowledgement:
We extend our gratitude to Dr. Lewinsohn for his work on the Oregon Adolescent Depression Project.
Role of Funding:
This publication was supported by the following grants: National Institute of Mental Health Grants R01MH66023 (Dr. Klein), R01 MH40501, R01 MH50522, R01 MH52858, and R01 DA012951 (Dr. Peter M. Lewinsohn), and R01 MH107495 (Dr. Olino).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Daniel N. Klein, Stony Brook University
John R. Seeley, University of Oregon & Oregon Research Institute
References
- Aaltonen K, Näätänen P, Heikkinen M, Koivisto M, Baryshnikov I, Karpov B, … Joffe G (2016). Differences and similarities of risk factors for suicidal ideation and attempts among patients with depressive or bipolar disorders. Journal of Affective Disorders, 193, 318–330. [DOI] [PubMed] [Google Scholar]
- Abramson LY, Metalsky GI, & Alloy LB (1989). Hopelessness depression: A theory-based subtype of depression. Psychological review, 96(2), 358–372. [Google Scholar]
- Adrian M, Miller AB, McCauley E, & Vander Stoep A (2016). Suicidal ideation in early to middle adolescence: sex- specific trajectories and predictors. Journal of Child Psychology and Psychiatry, 57(5), 645–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (1980). Diagnostic and Statistical Manual of Mental Disorders (3rd edition). Author. [Google Scholar]
- Aiken LS, West SG, & Reno RR (1991). Multiple regression: Testing and interpreting interactions.
- Arnett JJ (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55(5), 469–480. [PubMed] [Google Scholar]
- Baldessarini RJ, & Tondo L (2003). Suicide risk and treatments for patients with bipolar disorder. JAMA, 290(11), 1517–1519. [DOI] [PubMed] [Google Scholar]
- Bebbington PE, Minot S, Cooper C, Dennis M, Meltzer H, Jenkins R, & Brugha T (2010). Suicidal ideation, self-harm and attempted suicide: results from the British psychiatric morbidity survey 2000. European Psychiatry, 25(7), 427–431. [DOI] [PubMed] [Google Scholar]
- Becker SP, Holdaway AS, & Luebbe AM (2018). Suicidal behaviors in college students: Frequency, sex differences, and mental health correlates including sluggish cognitive tempo. Journal of Adolescent Health, 63(2), 181–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boeninger DK, Masyn KE, Feldman BJ, & Conger RD (2010). Sex differences in developmental trends of suicide ideation, plans, and attempts among European American adolescents. Suicide and Life-Threatening Behavior, 40(5), 451–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Bridge J, Johnson BA, & Connolly J (1996). Suicidal behavior runs in families: a controlled family study of adolescent suicide victims. Archives of General Psychiatry, 53(12), 1145–1152. [DOI] [PubMed] [Google Scholar]
- Brownson C, Drum DJ, Smith SE, & Burton Denmark A (2011). Differences in suicidal experiences of male and female undergraduate and graduate students. Journal of College Student Psychotherapy, 25(4), 277–294. [Google Scholar]
- Burke TA, Connolly SL, Hamilton JL, Stange JP, Abramson LY, & Alloy LB (2016). Cognitive risk and protective factors for suicidal ideation: A two year longitudinal study in adolescence. Journal of Abnormal Child Psychology, 44(6), 1145–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czyz EK, & King CA (2015). Longitudinal trajectories of suicidal ideation and subsequent suicide attempts among adolescent inpatients. Journal of Clinical Child & Adolescent Psychology, 44(1), 181–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donker T, Batterham PJ, Van Orden KA, & Christensen H (2014). Gender-differences in risk factors for suicidal behaviour identified by perceived burdensomeness, thwarted belongingness and acquired capability: cross-sectional analysis from a longitudinal cohort study. BMC psychology, 2(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erausquin JT, McCoy TP, Bartlett R, & Park E (2019). Trajectories of suicide ideation and attempts from early adolescence to mid-adulthood: associations with race/ethnicity. Journal of Youth and Adolescence, 48(9), 1796–1805. [DOI] [PubMed] [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, … Nock MK (2017). Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychological Bulletin, 143(2), 187–232. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1996). Structured clinical interview for DSM-IV axis I disorders, clinician version (SCID-CV). Washington, DC: American Psychiatric Press. [Google Scholar]
- Giletta M, Prinstein MJ, Abela JR, Gibb BE, Barrocas AL, & Hankin BL (2015). Trajectories of suicide ideation and nonsuicidal self-injury among adolescents in mainland China: Peer predictors, joint development, and risk for suicide attempts. Journal of Consulting and Clinical Psychology, 83(2), 265–279. [DOI] [PubMed] [Google Scholar]
- Goldstein TR, & Franzen PL (2020). Sleep difficulties and suicidality in youth: current research and future directions. Current Opinion in Psychology, 34, 27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldston DB, Erkanli A, Daniel SS, Heilbron N, Weller BE, & Doyle O (2016). Developmental trajectories of suicidal thoughts and behaviors from adolescence through adulthood. Journal of the American Academy of Child & Adolescent Psychiatry, 55(5), 400–407. e401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Compton WM, Blanco C, Colpe L, Huang L, & McKeon R (2018). National trends in the prevalence of suicidal ideation and behavior among young adults and receipt of mental health care among suicidal young adults. Journal of the American Academy of Child & Adolescent Psychiatry, 57(1), 20–27. e22. [DOI] [PubMed] [Google Scholar]
- Han B, McKeon R, & Gfroerer J (2014). Suicidal ideation among community-dwelling adults in the United States. American Journal of Public Health, 104(3), 488–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husky MM, Olfson M, He JP, Nock MK, Swanson SA, & Merikangas KR (2012). Twelve-month suicidal symptoms and use of services among adolescents: Results from the National Comorbidity Survey. Psychiatric Services, 63(10), 989–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim N, Amit N, Din NC, & Ong HC (2017). Gender differences and psychological factors associated with suicidal ideation among youth in Malaysia. Psychology Research and Behavior Management, 10, 129–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Im Y, Oh W-O, & Suk M (2017). Risk factors for suicide ideation among adolescents: five-year national data analysis. Archives of Psychiatric Nursing, 31(3), 282–286. [DOI] [PubMed] [Google Scholar]
- Joiner TE Jr, & Rudd MD (1995). Negative attributional style for interpersonal events and the occurrence of severe interpersonal disruptions as predictors of self- reported suicidal ideation. Suicide and Life- Threatening Behavior, 25(2), 297–304. [PubMed] [Google Scholar]
- Kang C, Zheng Y, Yang L, Wang X, Zhao N, Guan TF, … Hu J (2021). Prevalence, risk factors and clinical correlates of suicidal ideation in adolescent patients with depression in a large sample of Chinese. Journal of Affective Disorders, 290, 272–278. [DOI] [PubMed] [Google Scholar]
- Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, … Thornton J (2018). Youth risk behavior surveillance—United States, 2017. MMWR Surveillance Summaries, 67(8), 1–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Borges G, & Walters EE (1999). Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry, 56(7), 617–626. [DOI] [PubMed] [Google Scholar]
- Kleiman EM, Miller AB, & Riskind JH (2012). Enhancing attributional style as a protective factor in suicide. Journal of Affective Disorders, 143(1–3), 236–240. [DOI] [PubMed] [Google Scholar]
- Klein DN, Lewinsohn PM, Seeley JR, & Rohde P (2001). A family study of major depressive disorder in a community sample of adolescents. Archives of General Psychiatry, 58(1), 13–20. [DOI] [PubMed] [Google Scholar]
- Lamis DA, & Lester D (2013). Gender differences in risk and protective factors for suicidal ideation among college students. Journal of College Student Psychotherapy, 27(1), 62–77. [Google Scholar]
- Law BM, & Shek DT (2016). A 6-year longitudinal study of self-harm and suicidal behaviors among Chinese adolescents in Hong Kong. Journal of Pediatric and Adolescent Gynecology, 29(1), S38–S48. [DOI] [PubMed] [Google Scholar]
- Leckman JF, Sholomskas D, Thompson D, Belanger A, & Weissman MM (1982). Best estimate of lifetime psychiatric diagnosis: a methodological study. Archives of General Psychiatry, 39(8), 879–883. [DOI] [PubMed] [Google Scholar]
- Lee D, Ahn I-Y, Park C-S, Kim B-J, Lee C-S, Cha B, … Choi J-W (2020). Early menarche as a risk factor for suicidal ideation in girls: The Korea youth risk behavior web-based survey. Psychiatry Research, 285, 112706. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, & Andrews JA (1993). Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III—R disorders in high school students. Journal of Abnormal Psychology, 102(1), 133–144. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, & Seeley JR (1996). Adolescent suicidal ideation and attempts: prevalence, risk factors, and clinical implications. Clinical Psychology: Science and Practice, 3(1), 25–46. [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, & Baldwin CL (2001). Gender differences in suicide attempts from adolescence to young adulthood. Journal of the American Academy of Child & Adolescent Psychiatry, 40(4), 427–434. [DOI] [PubMed] [Google Scholar]
- Li SX, Lam SP, Zhang J, Yu MWM, Chan JWY, Chan CSY, … Wing Y-K (2016). Sleep disturbances and suicide risk in an 8-year longitudinal study of schizophrenia-spectrum disorders. Sleep, 39(6), 1275–1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madsen T, van Spijker B, Karstoft KI, Nordentoft M, & Kerkhof AJ (2016). Trajectories of Suicidal Ideation in People Seeking Web-Based Help for Suicidality: Secondary Analysis of a Dutch Randomized Controlled Trial. Journal of medical Internet research, 18(6), e178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannuzza S, & Fyer AJ (1990). Family informant schedule and criteria (FISC), July 1990 revision Anxiety Disorders Clinic, New York State Psychiatric Institute: New York. [Google Scholar]
- Mars B, Heron J, Klonsky ED, Moran P, O’Connor RC, Tilling K, … Gunnell D (2019). What distinguishes adolescents with suicidal thoughts from those who have attempted suicide? A population- based birth cohort study. Journal of Child Psychology and Psychiatry, 60(1), 91–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May AM, & Klonsky ED (2016). What distinguishes suicide attempters from suicide ideators? A meta- analysis of potential factors. Clinical Psychology: Science and Practice, 23(1), 5–20. [Google Scholar]
- McKnight-Eily LR, Eaton DK, Lowry R, Croft JB, Presley-Cantrell L, & Perry GS (2011). Relationships between hours of sleep and health-risk behaviors in US adolescent students. Preventive Medicine, 53(4–5), 271–273. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2015). Mplus user’s guide (7th ed.). Los Angeles: Muthén & Muthén. [Google Scholar]
- Nguyen DT, Wright EP, Dedding C, Pham TT, & Bunders J (2019). Low self-esteem and its association with anxiety, depression, and suicidal ideation in Vietnamese secondary school students: a cross-sectional study. Frontiers in Psychiatry, 10, 698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nkansah- Amankra S (2013). Adolescent suicidal trajectories through young adulthood: Prospective assessment of religiosity and psychosocial factors among a population-based sample in the United States. Suicide and Life- Threatening Behavior, 43(4), 439459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, & Kessler RC (2013). Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry, 70(3), 300–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orvaschel H, Puig-Antich J, Chambers W, Tabrizi MA, & Johnson R (1982). Retrospective assessment of prepubertal major depression with the Kiddie-SADS-E. Journal of the American Academy of Child Psychiatry, 21(4), 392–397. [DOI] [PubMed] [Google Scholar]
- Priester MJ, & Clum GA (1992). Attributional style as a diathesis in predicting depression, hopelessness, and suicide ideation in college students. Journal of Psychopathology and Behavioral Assessment, 14(2), 111–122. [Google Scholar]
- Prinstein MJ, Nock MK, Simon V, Aikins JW, Cheah CS, & Spirito A (2008). Longitudinal trajectories and predictors of adolescent suicidal ideation and attempts following inpatient hospitalization. Journal of Consulting and Clinical Psychology, 76(1), 92–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossom RC, Coleman KJ, Ahmedani BK, Beck A, Johnson E, Oliver M, & Simon GE (2017). Suicidal ideation reported on the PHQ9 and risk of suicidal behavior across age groups. Journal of Affective Disorders, 215, 77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rueter MA, Holm KE, McGeorge CR, & Conger RD (2008). Adolescent suicidal ideation subgroups and their association with suicidal plans and attempts in young adulthood. Suicide and Life-Threatening Behavior, 38(5), 564–575. [DOI] [PubMed] [Google Scholar]
- Rueter MA, & Kwon HK (2005). Developmental trends in adolescent suicidal ideation. Journal of Research on Adolescence, 15(2), 205–222. [Google Scholar]
- Schwartz JA, Kaslow NJ, Seeley J, & Lewinsohn P (2000). Psychological, cognitive, and interpersonal correlates of attributional change in adolescents. Journal of Clinical Child Psychology, 29(2), 188–198. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Jackson KM, & Steinley D (2011). Alcohol use trajectories and the ubiquitous cat’s cradle: Cause for concern? Journal of Abnormal Psychology, 120(2), 322–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer JD, & Willett JB (2003). Applied longitudinal data analysis: Modeling change and event occurrence. Oxford University Press. [Google Scholar]
- Taliaferro LA, & Muehlenkamp JJ (2014). Risk and protective factors that distinguish adolescents who attempt suicide from those who only consider suicide in the past year. Suicide and Life- Threatening Behavior, 44(1), 6–22. [DOI] [PubMed] [Google Scholar]
- Turecki G, & Brent DA (2016). Suicide and suicidal behaviour. The Lancet, 387(10024), 1227–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor SE, & Klonsky ED (2014). Correlates of suicide attempts among self-injurers: A meta-analysis. Clinical Psychology Review, 34(4), 282–297. [DOI] [PubMed] [Google Scholar]
- Wagner KD, Rouleau M, & Joiner T (2000). Cognitive factors related to suicidal ideation and resolution in psychiatrically hospitalized children and adolescents. American Journal of Psychiatry, 157(12), 2017–2021. [DOI] [PubMed] [Google Scholar]
- Wolff JC, Davis S, Liu RT, Cha CB, Cheek SM, Nestor BA, … Spirito A (2018). Trajectories of suicidal ideation among adolescents following psychiatric hospitalization. Journal of Abnormal Child Psychology, 46(2), 355–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zubrick SR, Hafekost J, Johnson SE, Lawrence D, Saw S, Sawyer M, … Buckingham WJ (2016). Suicidal behaviours: prevalence estimates from the second Australian Child and Adolescent Survey of Mental Health and Wellbeing. Australian & New Zealand Journal of Psychiatry, 50(9), 899–910. [DOI] [PubMed] [Google Scholar]
- Zubrick SR, Hafekost J, Johnson SE, Sawyer MG, Patton G, & Lawrence D (2017). The continuity and duration of depression and its relationship to non-suicidal self-harm and suicidal ideation and behavior in adolescents 12–17. Journal of Affective Disorders, 220, 49–56. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


