Abstract
Introduction:
Mental health follow-up after an emergency department (ED) visit for suicide ideation/attempt is a critical component of suicide prevention for young people.
Methods:
We analyzed 2009 to 2012 Medicaid Analytic EXtract for 62,139 treat-and-release ED visits and 30,312 ED-to-hospital admissions for suicide ideation/attempt among patients ages 6 to 17 years. We used mixed-effects logistic regression models to examine associations between patients’ health care utilization prior to the ED visit and likelihood of completing a 30-day mental health follow-up visit.
Results:
Overall, for treat-and-release ED visits, 49% had a 30-day follow-up mental health visit, and for ED-to-hospital admissions, 67% had a 30-day follow-up mental health visit. Having a mental health visit in the 30 days preceding the ED visit was the strongest predictor of completing a mental health follow-up visit (ED treat-and-release: adjusted odds ratio [AOR] 11.01; 95% confidence interval [CI] 9.82–12.35; ED-to-hospital AOR 4.60; 95% CI 3.16–6.68). Among those with no mental health visit in the 30 days preceding the ED visit, only 25% had an ambulatory mental health follow-up visit. Having a general health care visit in the 30 days preceding the ED visit had a much smaller association with completing a mental health follow-up visit (ED treat-and-release: AOR 1.17; 95% CI 1.09–1.24; ED-to-hospital AOR 1.25; 95% CI 1.17–1.34).
Conclusions:
Young people without an existing source of ambulatory mental health care have low rates of mental health follow-up after an ED visit for suicide ideation or attempt, and opportunities exist to improve mental health follow-up for youth with recent general health care visits.
Keywords: adolescents, emergency care, mental health, suicide
Suicide is the second leading cause of death for US adolescents,1 and suicide rates are rising.2 Across US regions, between 2% and 7% of high school students report having attempted suicide.3 Health care services in the period surrounding a suicidal crisis are critical to preventing suicide death. Most adolescents who present to health care settings for suicide ideation or attempt are evaluated in an emergency department (ED)4; some are discharged home and others are hospitalized. The National Strategy for Suicide Prevention, the Zero Suicide initiative, and the Joint Commission recommend close mental health (MH) follow-up when patients are discharged to the community after an ED visit or hospitalization for suicide ideation or attempt.5–7
Attendance at MH follow-up after hospitalization for suicide risk is associated with as much as 75% lower risk of subsequent suicide death.8–10 Overall rates of MH follow-up after acute treatment of suicide attempt are low,11–13 and patient’s MH care utilization postdischarge may vary by patient, hospital, regional, or insurance factors. Children and adolescents may be particularly vulnerable to missing opportunities to engage in MH care, due to longstanding shortages of child and adolescent MH specialists. To inform future suicide prevention efforts, there is a critical need to understand patient and health care utilization characteristics associated with receipt of ongoing MH care after an ED or hospital visit for suicide ideation or attempt.
One important factor in determining whether a young person receives follow-up MH care after a suicidal crisis is whether they previously received MH services. However, little is known about how receipt of MH services before a crisis affects patients’ follow-up. Therefore, we conducted the present study to understand how commonly patients initiate new MH care services after a suicidal crisis. We examined whether patient’s receipt of health care services before a suicide-related ED visit was associated with receipt of MH services after the ED visit. Specifically, we sought to 1) describe patterns of ambulatory visits in the 30 days before and after an ED visit for suicide ideation or attempt; and 2) determine which ambulatory visits and other patient characteristics were associated with completion of a follow-up visit in the 30 days after an ED visit for suicide ideation or attempt.
Methods
Study Design and Data Source
We conducted a retrospective cohort study using claims available in the Medicaid Analytic EXtract (MAX) dataset during the years 2009 to 2012. MAX data include all claims submitted to Medicaid payers in all 50 US states, along with reason for Medicaid eligibility, eligibility periods, service delivery dates (with up to 20 diagnosis codes per encounter), hospital identifiers, provider identifiers, patient demographic characteristics. Medicaid is the largest single payer for MH services for children, and 88% of youth MH service providers nationally accept Medicaid insurance. We limited our study sample to 29 states (AL, AK, AZ, AR, CT, DE, DC, GA, HI, ID, IN, IA, KY, LA, MN, MS, MT, NE, NH, NJ, NY, ND, OK, RI, SD, TN, TX, VA, WY) known to report high-quality, reliable data for children enrolled in all Medicaid fee-for-service and managed care plans available during the study period.14,15 The Children’s Hospital of Philadelphia Institutional Review Board determined that this study did not constitute human subjects research.
Study Sample
We included 6- to 17-year-old children and adolescents who had a treat-and-release ED visit or ED-to-hospital admission with a diagnosis of suicide ideation or suicide attempt. We did not include children younger than 6 because suicide ideation and attempt are rare in this age group and use of claims data to identify these problems in children younger than 6 has not been validated. We did not include adults 18 and older because they can access adult MH services and therefore available treatment options and patterns of care are different from those of children 17 and younger. We excluded individuals not eligible for Medicaid in the 3 months before and one month after the index ED visit in order to ensure that we could capture patient demographic characteristics and ambulatory visits in the 30 days before the ED visit and ambulatory visits in the 30 days after the ED visit and any resulting hospitalization. For each individual represented in the dataset, we included only the first ED visit for suicide ideation or attempt.
Visit Categories
We identified ED visits using claims that listed an ED place of service code (23) or common procedure terminology (CPT) codes 99281–99285, Healthcare Common Procedure Coding System (HCPCS) codes G03880-G0384, and revenue codes 450–459, 981. We identified whether an ED visit included treatment for suicide ideation or attempt using International Classification of Diseases, 9th revision, diagnosis codes: V62.84 for suicide ideation and a previously validated algorithm for suicide attempt.4 We determined whether an ED visit resulted in a hospitalization by identifying claims with a general or psychiatric inpatient unit place of service code within 2 calendar days of the ED visit (in order to allow for ED visits lasting past midnight resulting in hospital admissions on a subsequent day). If any inpatient claim followed the ED visit within 2 calendar days, we classified the visit as an ED-to-hospital admission. If there were no inpatient claims within 2 calendar days, the visit was classified as a treat-and-release ED visit.
We classified ED visits as being for suicide ideation only if the code V62.84 was present during the ED visit, and no codes for suicide attempt were present. We classified visits as being for suicide attempt using an established algorithm for identifying suicide attempt encounters.4 Among suicide attempt visits, we further categorized visits that involved self-poisoning (ie, intentional ingestion) using International Classification of Diseases, 9th revision diagnosis codes 960–989 versus other means of self-harm (including inhalation, firearm injury, laceration, jump or fall, and others).
We identified ambulatory visits 30-days before and after the index ED visit using a combination of CPT, HCPCS, place of service, and diagnosis codes. For ED-to-hospital admissions, the 30-day window began after hospital discharge. Visits were classified as ambulatory MH visits if they were conducted by a psychiatrist, psychologist, or other therapist, had any HCPCS or CPT code for ambulatory MH services, or if they had an ambulatory place of service code (52 or 53) and any psychiatric diagnosis code.16,17 Therefore, some MH visits were conducted with pediatricians, family practitioners, and other medical clinicians, if the medical clinician billed for a MH diagnosis or service. Visits were classified as general ambulatory visits if they had an ambulatory place of service code, were not conducted by a psychiatric provider or nonprescribing psychotherapist, and had no psychiatric diagnosis codes. We identified ED and hospital admissions in the 30 days before and after the index ED visit using the same codes we used to identify the index ED visit.
Covariates
Demographic characteristics (age, sex, race/ethnicity) and utilization characteristics (Medicaid plan type, reason for Medicaid eligibility) were determined from the MAX personal summary files. We identified patient health conditions from diagnoses listed on their index ED visit and hospitalization and any health care encounters preceding those visits. We identified complex chronic physical health conditions (ie, conditions affecting 2 or more organ systems expected to result in significant medical needs) using a well-established algorithm.18 We identified chronic psychiatric conditions using an established pediatric-specific algorithm.16,17
Analysis
All analyses were conducted at the level of an individual ED visit. We described characteristics of the sample of ED visits using frequencies and percentages. We then compared differences in characteristics of treat-and-release ED visits and ED-to-hospital admissions using Chi-squared and Kruskal-Wallis tests. We compared differences in the proportion of patients with visits in the 30 days after the index ED visit stratified on whether they had a visit in the 30 days before the index ED visit using Fisher’s exact test.
We measured the odds of an ambulatory MH visit within 30 days of the index ED visit associated with patient demographic and clinical characteristics using a mixed-effects logistic regression model including as predictors all patient demographic and clinical characteristics (including whether the patient had a health care encounter within the 30 days preceding the ED visit), adjusting for year of visit, with a random effect for state, and using robust standard errors.
Analyses were conducted in SAS version 9.4 (SAS Institute, Cary, NC) for dataset management, Stata 16 (StataCorp LLC, College Station, Tex) for models, and GraphPad Prism 8 (GraphPad Software, San Diego, Calif) and R version 3 (R Foundation, Vienna, Austria) for figures. All statistical tests were 2-sided and P values <.05 were considered statistically significant.
Results
The total study sample included 92,451 unique ED visits for suicide ideation or attempt in 2009 to 12. Among those, 38% had suicide ideation only, and 62% had a suicide attempt. Of suicide attempts, 89% were due to self-poisoning, with the remainder using other means. Median age of included patients was 15 years (interquartile range 12–16 years). The sample had a slight female predominance (54%), and the most common racial/ethnic group was white (46%). Most patients were enrolled in comprehensive managed care (73%); a minority were enrolled in behavioral health managed care (12%) or fee-for-service (15%) plans. The most common reason for Medicaid eligibility was income (75%), followed by disability (15%), or being in foster care (10%). Including diagnoses from all visits prior to the index ED admission (at minimum, in the 3-month eligibility period), we identified that nearly one third of patients had a complex chronic physical health condition (31%), and only 43% had a chronic psychiatric condition (other than suicide ideation or attempt diagnosed during the ED visit). A minority of cases were treated at children’s hospitals (10%).
Table 1 further describes the study sample stratified on treat-and-release ED visits versus ED-to-hospital admissions. In the overall study sample, two thirds of visits (67%) were treat-and-release ED visits and one third (33%) were ED-to-hospital admissions.
Table 1.
Demographic and Clinical Characteristics of ED and Hospital Visits for Suicide Ideation or Attempt Among US Adolescents With Medicaid (2009–12)
| ED Treat-and-Release |
ED-to-Hospital Admission |
P Value | |||
|---|---|---|---|---|---|
| Visit Characteristics | n | % | n | % | |
| Total | 62,139 | 67 | 30,312 | 33 | |
| Sex | <.001 | ||||
| Female | 32,416 | 52 | 17,521 | 58 | |
| Male | 29,723 | 48 | 12,791 | 42 | |
| Age, median (IQR) | 14 | 11–16 | 15 | 14–16 | <.001 |
| Age | <.001 | ||||
| Age 6–12 years | 19,661 | 32 | 4907 | 16 | |
| Age 13–17 years | 42,478 | 68 | 25,405 | 84 | |
| Race/ethnicity | <.001 | ||||
| White | 28,203 | 45 | 13,970 | 46 | |
| Black | 12,466 | 20 | 5722 | 19 | |
| Hispanic | 10,761 | 17 | 4534 | 15 | |
| Other | 10,709 | 17 | 6086 | 20 | |
| Type of Medicaid plan | <.001 | ||||
| Comprehensive managed care | 45,558 | 73 | 22,269 | 74 | |
| Behavioral health managed care | 8119 | 13 | 3626 | 12 | |
| Fee for service | 8462 | 14 | 4417 | 15 | |
| Reason for Medicaid eligibility | <.001 | ||||
| Disability | 9269 | 15 | 4720 | 16 | |
| Income | 47,185 | 76 | 21,866 | 72 | |
| Foster care | 5685 | 9 | 3726 | 12 | |
| Chronic health conditions* | |||||
| Complex chronic physical health condition | 17,146 | 28 | 11,118 | 37 | <.001 |
| Chronic psychiatric condition | 13,957 | 23 | 25,284 | 83 | <.001 |
| Reason for visit | <.001 | ||||
| Suicide ideation only | 19,710 | 32 | 14,504 | 48 | |
| Any suicide attempt | 42,429 | 68 | 15,808 | 52 | |
| Poisoning | 38,596 | 62 | 13,492 | 45 | <.001 |
| Other self-injury | 3833 | 6 | 2316 | 8 | <.001 |
| Children’s hospital encounter | 4556 | 7 | 4389 | 15 | <.001 |
| Length of stay in days, median (IQR) | 1 | 1–1 | 6 | 3–8 | <.001 |
CI indicates confidence interval; ED, emergency department; and IQR, interquartile range.
Chronic health condition diagnoses were ascertained from the index SI/SA ED visit and any visits in the eligibility period preceding the ED visit.
Among patients with treat-and-release ED visits, 56% attended any outpatient visit in the 30 days before and 64% attended an outpatient visit in the 30 days after the ED visit (Table 2). Among patients with ED-to-hospital admissions, 67% attended any outpatient visit in the 30 days before the ED visit and 77% attended any outpatient visit in the 30 days after hospital discharge. The most common type of health care encounter in the 30 days after both a treat-and-release ED visit or an ED-to-hospital admission was a MH visit, followed by a general health visit, and the least common was a repeat ED visit or hospitalization.
Table 2.
Characteristics of Visits in the 30 Days Before and After an ED Visit for Suicide Ideation or Attempt Among US Adolescents Using Medicaid
| Visit Types | 30 Days Before Visit |
30 Days After Discharge |
||||||
|---|---|---|---|---|---|---|---|---|
| ED Treat-and-Release |
ED-to-Hospital Admission |
ED Treat-and-Release |
ED-to-Hospital Admission |
|||||
| n | % | n | % | n | % | n | % | |
| Any visit | 34,855 | 56 | 20,122 | 66 | 39,907 | 64 | 23,203 | 77 |
| Outpatient mental health visit | 23,347 | 38 | 15,384 | 52 | 30,210 | 49 | 20,166 | 67 |
| Outpatient general visit | 14,386 | 23 | 7278 | 24 | 14,023 | 23 | 6199 | 20 |
| ED or hospital visit | 8588 | 14 | 5570 | 18 | 8582 | 14 | 4611 | 15 |
| No health care encounter | 27,284 | 44 | 10,190 | 34 | 22,232 | 36 | 7109 | 23 |
ED indicates emergency department.
ED treat-and-release (n = 62,139); ED-to-hospital admission (n = 30,312).
Percentages do not sum to 100% because some patients had visits in more than 1 category (ie, an outpatient mental health visit and an outpatient general visit).
Figure 1 shows rates of 30-day follow-up visits stratified on whether the patient had a health care encounter in the 30 days before the ED visit. For treat-and-release ED visits, Eighty percent of patients with a visit in the 30 days before the ED visit had any follow-up ambulatory visit in the 30 days following discharge. In comparison, only 44% of those without a visit in the 30 days preceding the ED visit had a follow-up ambulatory visit (P < .001). Similarly, MH follow-up was substantially more common among those with a visit in the 30 days before the ED visit (66% vs 25%, P < .001). For ED-to-hospital admissions, 84% with a visit in the 30 days before the ED visit had any 30-day follow-up ambulatory visit. Only 61% of those without a visit in the 30 days preceding the ED-to-hospital admission had an ambulatory follow-up visit (P = .017). Similarly, MH follow-up was substantially more common among those with a visit in the 30 days before the ED-to-hospital admission (75% vs 48%, P < .001).
Figure 1.
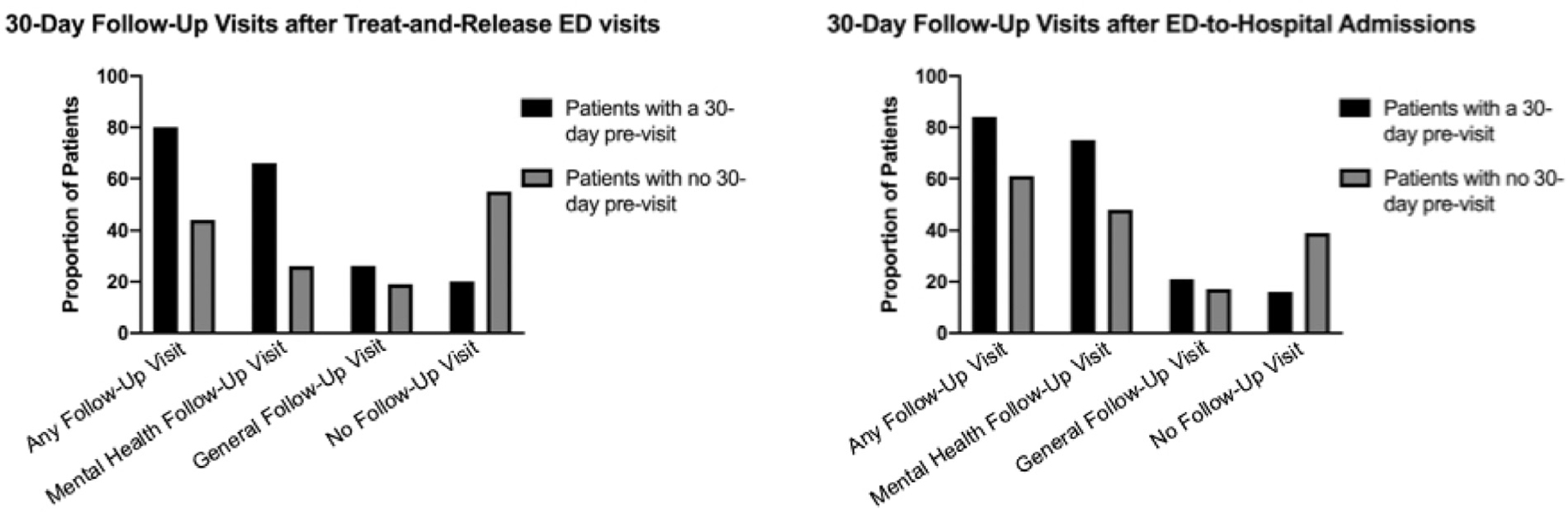
Follow-up visits in the 30 days after an ED visit for suicide ideation or attempt among US adolescents (2009–2012). Note: Treat-and-Release ED visits n = 62,139; ED-to-Hospital Admissions n = 30,312. 30-day previsits included ambulatory encounters for either mental health care or general health care in the 30 days preceding the index ED visit. Mental health follow-up visits included visits with mental health specialists, visits conducted at mental health treatment centers, and any visit with a general clinician that included billing for a mental health diagnosis or procedure. All other ambulatory visits were considered general follow-up visits. ED indicates emergency department.
In adjusted logistic models, we found that the strongest predictor of whether a patient had a MH visit in the 30 days following an ED visit for suicide ideation or attempt was whether the patient had a MH visit in the 30 days preceding the ED visit (ED Treat-and-Release AOR 11.01, 95% confidence interval: 9.82–12.35; ED-to-Hospital Admission AOR 4.60, 95% confidence interval: 3.16–6.68). Other factors associated with completing an ambulatory MH visit in the 30 days after ED visit for suicide ideation or attempt included female sex, having a chronic psychiatric condition, and having a presenting complaint of suicide ideation only (with no suicide attempt). For treat-and-release ED visits, age 13 to 17 years, race other than Black, and having a complex chronic physical health condition, longer ED length of stay, and higher number of ED visits during the study timeframe were also associated with higher odds of completing a follow-up MH visit. Adjusted odds ratios and confidence intervals for all predictors are displayed on Table 3.
Table 3.
Adjusted Odds of Health Care Encounters in the 30 Days Following ED Visit for Suicide Ideation or Attempt Among US Adolescents Using Medicaid (2009–2012)
| Visit Characteristics | Treat-and-Release ED Visit Ambulatory Mental Health Visit in 30 Days After Discharge |
ED-to-Hospital Admission Ambulatory Mental Health Visit in 30 Days After Discharge |
||||
|---|---|---|---|---|---|---|
| AOR | 95% LCL | 95% UCL | AOR | 95% LCL | 95% UCL | |
| Female sex | 1.11 | 1.07 | 1.15 | 1.15 | 1.09 | 1.21 |
| Age | ||||||
| Age 6–12 years | Ref | Ref | ||||
| Age 13–17 years | 1.54 | 1.41 | 1.68 | 1.20 | 0.28 | 5.09 |
| Race/ethnicity | ||||||
| Black | Ref | Ref | ||||
| White | 1.46 | 1.34 | 1.59 | 1.29 | 0.81 | 2.05 |
| Hispanic | 1.28 | 1.06 | 1.55 | 1.23 | 0.72 | 2.09 |
| Other | 1.27 | 1.13 | 1.42 | 1.07 | 0.62 | 1.84 |
| Type of Medicaid plan | ||||||
| Behavioral health managed care | Ref | Ref | ||||
| Comprehensive managed care | 1.38 | 0.60 | 3.15 | 1.51 | 0.03 | 90.9 |
| Fee for service | 1.18 | 0.49 | 2.83 | 1.81 | 0.02 | 60.1 |
| Reason for Medicaid eligibility | ||||||
| Disability | Ref | Ref | ||||
| Income | 0.78 | 0.66 | 0.94 | 0.96 | 0.89 | 1.05 |
| Foster care | 1.12 | 0.94 | 1.35 | 1.03 | 0.90 | 1.19 |
| Complex chronic physical health condition | 1.13 | 1.08 | 1.18 | 1.02 | 0.72 | 1.44 |
| Psychiatric Condition | 1.41 | 1.20 | 1.66 | 1.27 | 1.15 | 1.40 |
| Reason for visit | ||||||
| Suicide attempt | Ref | Ref | ||||
| Suicide ideation only | 2.75 | 2.29 | 3.31 | 1.30 | 1.16 | 1.46 |
| Children’s hospital encounter | 1.07 | 0.85 | 1.35 | 0.96 | 0.78 | 1.18 |
| Health care encounters in | ||||||
| 30 days before ED visit | ||||||
| No visits | Ref | Ref | ||||
| ED or inpatient visit | 1.02 | 0.95 | 1.09 | 0.97 | 0.75 | 1.25 |
| General health visit | 1.17 | 1.09 | 1.24 | 1.25 | 1.17 | 1.34 |
| Mental health visit | 11.01 | 9.82 | 12.35 | 4.60 | 3.16 | 6.68 |
| Length of stay | 1.08 | 1.04 | 1.12 | 0.98 | 0.96 | 1.00 |
| Patient number of ED visits during study timeframe | 1.07 | 1.02 | 1.13 | 1.00 | 0.97 | 1.04 |
AOR indicates adjusted odds ratio; CI, confidence interval; ED, emergency department; LCL, lower confidence limit; Ref, reference group; UCL, upper confidence limit.
Model adjusts for all co-variates in table as well as year of visit, includes a random effect for state, and uses a robust standard error.
AORs in bold are statistically significant.
Treat-and-release ED visit n = 30,210; ED-to-hospital admission n = 20,166
Figure 2 provides visual display of individual patients’ patterns of visit completion in the 30 days before and after the index ED visit for suicide ideation or attempt. The figure shows that the majority of patients who completed a MH follow-up visit had a source of MH care in the 30 days before the ED visit; ie, patients did not commonly establish new MH care in the 30 days after the ED visit if they did not already have a source of MH care.
Figure 2.
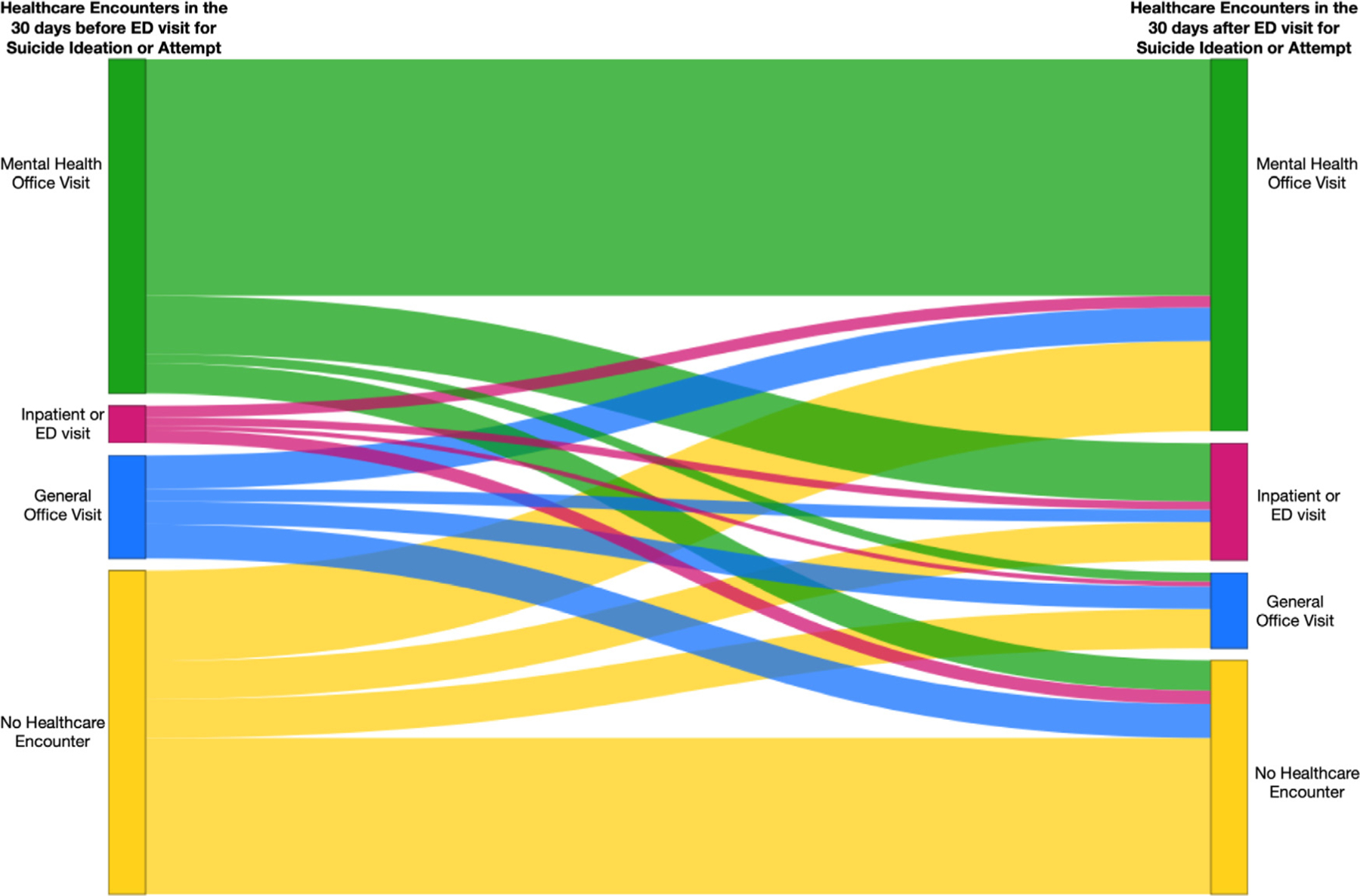
Health care encounters in the 30 days before and after an ED visit for suicide ideation or attempt among US adolescents using Medicaid (N = 92,451). Note: Lines represent individual patients’ trajectories, and line weights are proportional to the number of patients following that trajectory. For patients with ED-to-Hospital admissions, the 30-day follow-up window began after hospital discharge. health care encounter types are mutually exclusive in both the 30-day pre- and post-ED visit periods. If patients had multiple encounters, “Inpatient/ED visits” were represented first. If no inpatient/ED visit occurred, then “Mental Health Office Visits” were represented. If neither an inpatient/ED visit or a mental health office visit occurred, then “General Office Visits” were represented. Finally, “No Health Care Encounter” was represented if no encounters occurred. ED indicates emergency department.
Discussion
Follow-up MH care after a suicide-related hospitalization or ED visit is considered a critical component of suicide prevention care.8 Our study found that 64% of young people discharged from an ED after a visit for suicide ideation or attempt attended any ambulatory health care visit within 30 days after ED discharge, and 49% attended an ambulatory MH visit. For children and adolescents who were hospitalized after their ED visit, Seventy-seven percent completed any follow-up ambulatory visit in 30 days, and 67% completed a follow-up visit addressing their MH. Having an ambulatory MH visit in the 30 days before the ED or hospital visit was the strongest predictor of whether the patient completed a follow-up MH visit within 30 days. Other factors that increased the likelihood of a patient completing a follow-up visit within 30 days after the ED visit included: having a diagnosed chronic psychiatric condition and having an ED visit for suicide ideation only (with no suicide attempt). These findings have several important implications for health services planning.
Nearly half (51%) of young people using Medicaid with a treat-and-release ED visit for suicide ideation or attempt did not receive any ambulatory follow-up MH care within 30 days, and one third (33%) did not receive any ambulatory MH care within 30 days of discharge after a suicide-related hospitalization. These findings are consistent with other research showing lower-than-ideal rates of follow-up for MH care after a crisis hospitalization or ED visit.11,19 Our study advances these findings by showing that having a prior MH visit before the ED visit or hospitalization substantially increases the likelihood that a patient will successfully complete follow-up. This finding suggests that EDs and, to a lesser extent, hospitals are not adequately equipped to ensure that patients attend follow-up MH care if they are not already engaged in MH services. Future quality initiatives to address this problem could offer additional resources for follow-up MH care coordination to patients who did not have an established source of MH care recognizing that even patients with an established source of MH care may need some assistance in arranging follow-up.
Several of our paper’s secondary findings warrant mention because they have important implications for future research or clinical care. First, we found that individuals treated in EDs and hospitals for suicide ideation had higher rates of MH follow-up than those with suicide attempt. We suspect that the most likely explanation for these findings is that documentation of suicidal ideation implies that health care providers have recognized an individual’s suicidal thoughts and are providing treatment for them. For suicide attempts, health care providers may be more focused on the physical injuries than the MH contribution to those injuries. Particularly for the lower-lethality methods of suicide attempt that were common in our sample of children and adolescents, such as medication ingestions, health care providers may not always recognize the risk of subsequent repeat suicide attempt or suicide death. Our findings are consistent with prior research that has shown low rates of recognition of MH conditions among individuals presenting to EDs with self-harm and better outcomes for patients whose MH conditions are recognized in the ED.20 We similarly found that having a chronic psychiatric condition diagnosis other than suicide ideation or attempt was associated with higher likelihood of completing a follow-up ambulatory MH visit. These findings can help guide continuing education initiatives for clinicians working in general ED settings and highlight the importance of universal suicide screening for all patients seeking ED care.
Second, several variables that could affect follow-up were not associated with completion of follow-up MH visits, including hospital length of stay and type of Medicaid plan. The fact that hospital length of stay was not associated with completed MH follow-up visits suggests that more time in hospital is not adequate to improve coordination of follow-up care. Future factors to investigate that might improve rates of follow-up care more than increasing length of hospital stay include availability of specialized discharge planners and other factors related to staffing of MH specialists in the unit where a patient was hospitalized. Similarly, type of Medicaid plan (ie, comprehensive managed care, behavioral health managed care, or fee for service) was not associated with follow-up visit completion. In combination with our findings that diagnoses of suicide ideation, chronic psychiatric conditions, and complex chronic physical health conditions were associated with higher rates of follow-up, this finding suggests that clinical factors affect follow-up visit completion more than health plan organization. Medicaid programs seeking to improve mental health care and outcomes can consider whether investing in clinical resources is more likely to improve patients’ engagement in MH services than health plan organization.
Future research directions include detailed study of ED and hospital processes and staffing models and testing specific models of follow-up care coordination to determine what level of support is effective for ensuring that patients reach ongoing follow-up MH care.
Our findings should be interpreted in the context of several limitations. We used administrative claims data from Medicaid plans in states with high-quality data; however, some services may have been provided without being billed to a patient’s Medicaid plan. We were not able to adjust for detailed clinical factors that might influence a patient’s MH status, such as their home and family environment, recent trauma or stressors, or specific aspects of their suicide risk, such as whether they had a plan for a future suicide attempt. Data are from 2009 to 2012 and therefore do not describe the most recent health care encounters; however, mental health care policies and practices have not substantially changed since that time.21–25 Therefore, we would expect our identified associations to remain consistent in more recent time periods.
Conclusions
Among adolescents with an ED visit or hospitalization for suicide ideation or attempt, one third did not receive ambulatory MH care within 30 days of their ED visit. Future initiatives to increase continuity of MH care after ED visit or hospitalization for young people at risk of suicide may benefit patients if they focus on coordinating follow-up MH services for young people who were not previously engaged in MH care.
What’s New.
Among young people with an emergency department visit for suicide ideation or attempt without an existing source of mental health care, only 25% received mental health follow-up in the month after discharge.
Acknowledgments
Financial statement: This research was supported by grants K23MH115162 (Doupnik) and R01MH107452 (Marcus) from the National Institute of Mental Health. The sponsors had no role in the study’s design, data collection, data analysis or interpretation, writing of the report, or the decision to submit the article for publication.
Footnotes
Conflict of Interest: Dr Marcus reports receiving consulting fees from Allergan and Sage Therapeutics. The other authors have no financial relationships relevant to this article to disclose.
Previous presentation: Findings have not been presented previously.
Contributor Information
Stephanie K. Doupnik, Department of Pediatrics, Center for Pediatric Clinical Effectiveenss, and PolicyLab, Children’s Hospital of Philadelphia, Philadelphia, Pa; The Leonard Davis Institute of Health Economics, The University of Pennsylvania, Philadelphia, Pa.
Molly Passarella, Department of Pediatrics, Center for Pediatric Clinical Effectiveenss, and PolicyLab, Children’s Hospital of Philadelphia, Philadelphia, Pa.
Christian Terwiesch, Wharton School, Philadelphia, Pa; The Leonard Davis Institute of Health Economics, The University of Pennsylvania, Philadelphia, Pa.
Steven C. Marcus, School of Social Policy and Practice and Center for Mental Health, Philadelphia, Pa; The Leonard Davis Institute of Health Economics, The University of Pennsylvania, Philadelphia, Pa.
References
- 1.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. WISQARS fatal injury data, national, 2018. Available at: https://webappa.cdc.gov/sasweb/ncipc/leadcause.html. AccessedMay 20, 2020.
- 2.Curtin S, Warner M, Hedegaard H. Increase in Suicide in the United States, 1999–2014 2016. Hyattsville, Md; http://www.cdc.gov/nchs/data/databriefs/db241.pdf. AccessedMay 20, 2020. [PubMed] [Google Scholar]
- 3.Kann L, McManus T, Harris M, et al. Youth risk behavior surveillance—United States, 2017. Morb Mortal Wkly Rep 2018;67: 1–114. Available at: https://www.cdc.gov/mmwr/volumes/67/ss/ss6708a1.htm. AccessedMay 20, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Callahan ST, Fuchs DC, Shelton RC, et al. Identifying suicidal behavior among adolescents using administrative claims data. Pharmacoepidemiol Drug Saf 2013;22:769–775. 10.1002/pds.3421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Department of Health and Human Services Office of the Surgeon General. National Action Alliance for Suicide Prevention. National Strategy for Suicide Prevention: Goals and Objectives for Action Washington, DC: HHS; 2012.Available at: https://www.ncbi.nlm.nih.gov/books/NBK109917/. AccessedMay 20, 2020. [PubMed] [Google Scholar]
- 6.Zero Suicide Toolkit: Transition Available at: https://zerosuicide.edc.org/toolkit/transition. AccessedMay 20, 2020.
- 7.The Joint Commission. Detecting and treating suicide ideation in all settings Sentinel Event Alert, 2016. Available at: https://www.jointcommission.org/assets/1/18/SEA_56_Suicide.pdf. AccessedMay 20, 2020. [PubMed] [Google Scholar]
- 8.Knesper DJ. American Association of Suicidology and Suicide Prevention Resource Center. Continuity of Care for Suicide Prevention and Research: Suicide Attempts and Suicide Deaths Subsequent to Discharge from the Emergency Department or Psychiatry Inpatient Unit Newton, Mass: Education Development Center, Inc. Available at: http://www.sprc.org/sites/default/files/migrate/library/continuityofcare.pdf. AccessedMay 20, 2020. [Google Scholar]
- 9.While D, Bickley H, Roscoe A, et al. Implementation of mental health service recommendations in England and Wales and suicide rates, 1997–2006: A cross-sectional and before-and-after observational study. Lancet 2012;379:1005–1012. 10.1016/S0140-6736(11)61712-1. [DOI] [PubMed] [Google Scholar]
- 10.Bickley H, Hunt IM, Windfuhr K, et al. Suicide within two weeks of discharge from psychiatric inpatient care: a case-control study. Psychiatr Serv 2013;64:653–659. 10.1176/appi.ps.201200026. [DOI] [PubMed] [Google Scholar]
- 11.Bridge JA, Marcus SC, Olfson M. Outpatient care of young people after emergency treatment of deliberate self-harm. J Am Acad Child Adolesc Psychiatry 2012;51:213–222. 10.1016/j.jaac.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Bridge JA, Horowitz LM, Fontanella CA, et al. Prioritizing research to reduce youth suicide and suicidal behavior. Am J Prevent Med 2014;47:S229–S234. 10.1016/j.amepre.2014.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marino L, Wissow LS, Davis M, et al. Predictors of outpatient mental health clinic follow-up after hospitalization among Medicaid-enrolled young adults: outpatient follow-up in young adults. Early Interv Psychiatry 2016;10:468–475. 10.1111/eip.12206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Byrd VLH, Dodd AH. Assessing the usability of encounter data for enrollees in comprehensive managed care 2010–2011. Mathematic Policy Research; Brief 22, 2015. Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Computer-Data-and-Systems/MedicaidDataSourcesGenInfo/Downloads/MAX_Encounter_Brief_2010_2011.pdf. AccessedMay 20, 2020. [Google Scholar]
- 15.Nysenbaum J, Morris E, Desantis R, et al. Assessing the usability of 2011 behavioral health organization Medicaid encounter data 2016Available at: https://www.medicaid.gov/medicaid/managed-care/downloads/guidance/assessing-the-usability-of-2011.pdf. AccessedJuly 28, 2017.
- 16.Zima B, Rodean J. Child and Adolescent Mental Health Disorders Classification System (CAMHD-CS) Available at: https://www.childrenshospitals.org/Research-and-Data/Pediatric-Data-and-Trends/2019/Mental-Health-Disorder-Codes. AccessedMay 20, 2020.
- 17.Zima BT, Gay JC, Rodean J, et al. Classification system for International Classification of Diseases, Ninth Revision, Clinical Modification and Tenth Revision Pediatric Mental Health Disorders. JAMA Pediatr 2020:e200037. 10.1001/jamapediatrics.2020.0037. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feinstein JA, Russell S, DeWitt PE, et al. R package for pediatric complex chronic condition classification. JAMA Pediatr 2018; 172:596. 10.1001/jamapediatrics.2018.0256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bardach NS, Doupnik SK, Rodean J, et al. ED visits and readmissions after follow-up for mental health hospitalization. Pediatrics 2020;145. 10.1542/peds.2019-2872. [DOI] [PubMed] [Google Scholar]
- 20.Olfson M, Marcus SC, Bridge JA. Emergency department recognition of mental disorders and short-term outcome of deliberate self-harm. Am J Psychiatry 2013;170:1442–1450. 10.1176/appi.ajp.2013.12121506. [DOI] [PubMed] [Google Scholar]
- 21.American Academy of Child and Adolescent Psychiatry: Children’s mental health workforce shortage must be addressed 2017. Available at: https://www.aacap.org/App_Themes/AACAP/docs/resources_for_primary_care/workforce_issues/workforce_factsheet_updated_2018.pdf. AccessedApril 13, 2021.
- 22.Kim WJ. The American Academy of Child and Adolescent Psychiatry Task Force on Workforce Needs. Child and Adolescent Psychiatry Workforce: a critical shortage and national challenge. Acad Psychiatry 2003;27:277–282. [DOI] [PubMed] [Google Scholar]
- 23.Kennedy-Hendricks A, Epstein AJ, Stuart EA, et al. Federal parity and spending for mental illness. Pediatrics 2018;142:e20172618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barry CL, Chien AT, Normand SL, et al. Parity and out-of-pocket spending for children with high mental health or substance abuse expenditures. Pediatrics 2013;131:e903–e911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Olfson M, Wall M, Barry CL, et al. Effects of the affordable care act on private insurance coverage and treatment of behavioral health conditions in young adults. Am J Public Health 2018;108:1352–1354. [DOI] [PMC free article] [PubMed] [Google Scholar]


