Abstract
A substantial minority of deployed Gulf War veterans developed posttraumatic stress disorder (PTSD), depression, and several chronic illnesses. Although military combat and exposure to certain nuclear, biological, and chemical agents (NBCs) increase risk for post-deployment health problems, they do not fully explain many Gulf War veteran health diagnoses and are not viable treatment targets. Experiential avoidance (EA; one’s unwillingness to remain in contact with unpleasant internal experiences) is a modifiable psychosocial risk factor associated with PTSD and depression in veterans as well as pain and gastrointestinal diseases in the general population. In this study, we recruited a national sample of deployed Gulf War veterans (N = 454) to test the hypothesis that greater EA would be significantly associated with higher lifetime odds of PTSD, depression, “Gulf War Illness” (GWI/CMI), and other chronic illnesses common in this veteran cohort. Participants completed a self-report battery assessing demographic, military-related, and health-related information. Multivariate analyses showed that after adjusting for age, sex, race, combat exposure, and NBC exposure, worse EA was associated with higher lifetime odds of PTSD, depression, GWI/CMI, gastrointestinal problems, irritable bowel syndrome, arthritis, fibromyalgia, and chronic fatigue syndrome (ORs ranged 1.25 to 2.89; effect sizes ranged small to large), but not asthma or chronic obstructive pulmonary disease. Our findings suggest medical and mental health providers alike should assess for EA and potentially target EA as part of a comprehensive, biopsychosocial approach to improving Gulf War veterans’ health and wellbeing. Study limitations and future research directions are also discussed.
Keywords: Experiential avoidance, Gulf War, veterans, chronic illness, PTSD, depression
Between 1990 and 1991, the United States (U.S.) military participated in Operation Desert Shield, Operation Desert Storm, and Operation Desert Sabre—collectively called the Gulf War or Persian Gulf War. Following Gulf War operations, veterans from the U.S. and other coalition nations reported a wide array of persistent and disabling symptoms including fatigue, musculoskeletal pain, respiratory difficulties, and gastrointestinal complaints (Dursa et al., 2020; Fukuda et al., 1998; Kelsall et al., 2009; Proctor et al., 1998; Unwin et al., 2002; White et al., 2016). Though some of these problems aligned with known medical conditions (e.g., chronic fatigue syndrome), a substantial minority of deployed Gulf War veterans reported an enduring constellation of medically unexplained symptoms, subsequently and collectively referred to as “Gulf War Illness” or “Chronic Multisymptom Illness” (GWI/CMI; Institute of Medicine, 2014). In addition to physical health problems, deployed Gulf War veterans also developed certain psychiatric disorders at higher rates than their non-deployed Gulf War Era veteran counterparts—namely, posttraumatic stress disorder (PTSD) and depression (Toomey et al., 2007).
To better address the medical and mental health needs of Gulf War veterans, investigators have sought to identify reliable risk factors of poor health outcomes in this cohort. One potentially contributing factor is exposure to nuclear, biological, and chemical agents (NBCs). Specifically, Gulf War service members may have encountered NBCs such as hazardous pesticides, oil fire smoke, anti-nerve gas pills, and chemical warfare agents during deployment (Research Advisory Committee on Gulf War Veterans’ Illnesses, 2014; Riegle, 1994; White et al., 2016), and research has documented simple and dose-response relationships between NBC exposure and poor health outcomes in Gulf War veterans (King et al., 2008; Proctor et al., 1998; Wolfe et al., 2002). Another possible contributing factor is combat exposure. Combat exposure is strongly associated with post-deployment psychiatric disorders such as PTSD and depression (Kimbrel et al., 2015, 2014; King et al., 2006; Luxton et al., 2010; Toomey et al., 2007), and it has also been linked to certain medical problems in Gulf War veterans including GWI/CMI, pain, and respiratory issues (e.g., Porter et al., 2019; Sheffler et al., 2016; White et al., 2016).
Although prior research documents associations between military service-related exposures and post-deployment health, these associations do not fully explain medical and mental health outcomes among deployed Gulf War veterans. Moreover, because combat exposure and NBC exposure are both intractable historical factors, their clinical intervention utility is limited. Given the barriers to understanding Gulf War veteran health based on service-related exposures alone, experts have called for adopting a biopsychosocial perspective to better meet Gulf War veteran’s health needs (Ferrari, 2000; Ferrari and Russell, 2001; Wojcik and Lawrie, 2016). Relative to biomedical approaches, the biopsychosocial model takes a more comprehensive approach to conceptualizing physical health complaints by considering the cognitive, affective, and behavioral forces shaping physiological functioning (Engel, 1977). That is not to say certain symptoms cannot have organic (biological) sources according to this framework; rather, it posits that health symptoms can arise from multiple sources and that psychosocial phenomena can both amplify and alleviate physiological symptoms (Ferrari, 2000). The biopsychosocial model has been successfully applied to idiopathic conditions such as chronic pain and irritable bowel syndrome (Bevers et al., 2016; Gatchel et al., 2007; Halpert and Drossman, 2005; Van Oudenhove et al., 2016). It also has clear implications for Gulf War veteran health assessment and intervention and lends itself well to holistic health care (e.g., the Department of Veterans Affairs’ “Whole Health” model; Krejci et al., 2014). As many common Gulf War veteran health problems are chronic and difficult to treat (Porter et al., 2019; Proctor et al., 1998; White et al., 2016), research aimed at identifying modifiable psychosocial influences on post-deployment medical and mental health could meaningfully contribute to Gulf War veteran health theory, research, and practice.
One candidate psychosocial factor is experiential avoidance (EA). EA is the phenomenon whereby a person is unable or unwilling to remain in contact with aversive internal events (e.g., unwanted memories, emotions, and physical sensations) and consequently acts to avoid, alter, or escape their unpleasant internal experiences (Hayes et al., 1996). Though EA might be adaptive in theater or in the immediate aftermath of deployment stress (Bowes et al., 2018; Brockman et al., 2016; Cobb et al., 2017), persistent escape/avoidance of unwanted internal experiences can ironically maintain and even worsen psychiatric symptoms in the long-term (Chawla and Ostafin, 2007; Kashdan, 2010). Indeed, EA has been linked to both PTSD and depression in U.S. military veterans in numerous studies (Avery et al., 2018; Brockman et al., 2016; Bryan et al., 2015; Byllesby et al., 2020; Elliott et al., 2015; Kelly et al., 2019; Meyer et al., 2013, 2019b, 2019c, 2019a, 2018a).
Although most research on EA has focused on EA’s role in the maintenance of mental health disorders, there is also a burgeoning parallel literature on EA in the context of chronic medical conditions. Specifically, studies in patient samples show EA is significantly associated with chronic pain intensity and interference (Cook et al., 2015; Karademas et al., 2017; McCracken and Velleman, 2010; Trainor et al., 2019) as well as irritable bowel syndrome severity and interference (Cassar et al., 2018; Ferreira et al., 2018, 2011; Gillanders et al., 2017). In addition to various pain- and gastrointestinal-related conditions, qualitative research suggests EA is associated with poorer functional adaptation to respiratory conditions like asthma and chronic obstructive pulmonary disease (COPD; Boot et al., 2009). Although one recent study found preliminary evidence for a mediating effect of EA on the relationship between generalized anxiety and asthma outcomes (Michalova et al., 2021), quantitative research linking EA to respiratory disorders is scant and remains an important focus for future research. Taken together, although previous studies suggest EA could meaningfully inform clinical models of chronic illnesses, they were all conducted using relatively small convenience samples. Consequently, it remains unknown whether EA helps explain physical health outcomes among U.S. veterans generally, and Gulf War veterans in particular.
The current study was designed to build upon previous work by investigating the relation of EA to medical and mental health outcomes in a national sample of deployed Gulf War veterans—a veteran cohort with especially high rates of chronic and disabling health concerns, in addition to PTSD and depression (Proctor et al., 1998; Toomey et al., 2007). Previous research has linked EA to PTSD and depression in veteran samples (but not Gulf War veterans) and EA is rarely assessed in research on physical health problems in veterans. Based on the literature reviewed above, we hypothesized that higher (worse) EA would be associated with higher lifetime odds of PTSD and depression, even after adjusting for demographic covariates and military service-related exposures. We additionally hypothesized that after adjusting for demographic covariates and military service-related exposures, higher EA would be associated with higher lifetime odds of GWI/CMI and fatigue-, pain-, respiratory-, and gastrointestinal-related medical diagnoses commonly observed among deployed Gulf War veterans.
Methods and Materials
Participants and Procedure
Data included in the present analyses were collected as part of a larger Gulf War study focused on the healthcare needs of Gulf War veterans (Grant 1I01HX001682). This project, entitled Gulf War Research and Individual Testimony (Project GRIT; N = 1,153), included a national survey of Gulf War veterans’ healthcare needs, utilization patterns, and associated costs. Participants were eligible for inclusion in the current analysis if they endorsed being deployed to the Persian Gulf region (i.e., Kuwait, Iraq, and Saudi Arabia) any time between August 1990 and July 1991 as part of their U.S. military service.
The Project GRIT survey, conducted January 2019 to August 2020, was administered to a national cohort of deployed Gulf War and non-deployed Gulf War Era U.S. veterans. All study procedures, including consent and HIPAA authorization waivers, were approved by the Institutional Review Boards at the Durham Veterans Affairs (VA) Health Care System and the VA Salt Lake City Health Care System. Potential participants were first identified from a VA administrative database of patients (SPatient file). To be eligible, potential respondents had to have a history of military service during the Gulf War in the administrative record, regardless of whether or not they had deployed, resulting in an initial cohort of 1,098,991 Gulf War Era veterans, including 133,461 women veterans (12.14%). Cohort participants were then categorized into eight geographic regions providing nationwide representation. Stratified random sampling was used to identify a sample of 6,000 veterans (including 750 veterans from each of the 8 geographic regions) to potentially contact for recruitment to complete the Project GRIT survey. Women veterans were oversampled (25%; 1,500/6,000) to ensure sufficient representation in the final sample.
A modified Dillman approach (Dillman et al., 2014) involving multiple and multimethod contacts was used to maximize participant response rate. Eligible veterans were first sent pre-notification letters on VA letterhead describing the purpose and nature of the study, the expected study completion time, and instructions for how to opt out of the study. Eligible veterans were informed in the study information letters that they could complete the survey by telephone, if they preferred, but no participants elected to do so. To incentivize study participation, veterans were also informed that respondents who completed and returned the survey would be entered into a lottery drawing for opportunities to win either $100 or $500 (50 total $100 prizes and 10 total $500 prizes were awarded). To encourage timely study completion, veterans were also informed they would have a greater chance of being selected as a lottery raffle winner if they returned their surveys sooner because they would be considered for a greater number of raffle drawings over time.
One week later, veterans who had not opted out of the study were sent a physical survey copy, another copy of the study information letter describing the project and key elements of informed consent, and a small token of appreciation (a challenge coin with the study name printed on it) along with a pre-paid return envelope. Participants’ consent was inferred from their willingness to complete and return the survey. Approximately two weeks later, a reminder letter was mailed to eligible veterans who had not yet returned their survey. One week after the reminder mailing, non-responders were sent a duplicate packet with another study information sheet, physical survey copy, a complimentary pen, and instructions for how to opt out of the study.
A total of 3,272 veterans were contacted about the survey from the initial pool of 6,000 potential participants. Of the 3,272 surveys that were mailed to prospective participants, 548 surveys were returned to the study site due to incorrect/outdated mailing addresses, resulting in a total 2,724 surveys received by participants. Thirty-two veterans opted out of the study and 1,153 veteran participants completed and returned the survey, resulting in an overall survey response rate of 42.3% (1,153/2,724) and a survey return rate of 35.2% (1,153/3,272). Consistent with our goal of oversampling for women veterans, the final cohort of Project GRIT participants contained a significantly higher number of women veterans than did the national cohort from which we sampled (21.6% vs. 12.1%, p < .001). The mean age of Project GRIT participants (M = 58.8, SD = 7.3) was approximately 0.6 years higher than the mean age of the national cohort in 2020 (the year that most participants completed the survey; M = 58.2, SD = 7.7, z = 2.51, p = .006). Comparing the racial demographics of survey respondents to the population among those with non-missing race data in Veterans Health Administration (VHA) electronic records indicated that the survey sample was similar to the population in the proportion of veterans who identified as White (61.3% vs. 63.1%, z = −1.28, p > .05) or as a racial minority (38.7% vs. 36.9%, z = 1.26, p > .05).
Of the 1,153 Project GRIT survey respondents, n = 454 endorsed being military deployment to the Persian Gulf War region between August 1990 and July 1991 (n = 674 denied, n = 25 responses missing) and were included in the current study’s analyses. Descriptive statistics for the analyzed sample are presented in Table 1. See Figure 1 for an illustration of participant flow.
Table 1.
Characteristics of Deployed Gulf War Veteran Sample (N = 454)
| Characteristic | Missing Data | Observed | ||
|---|---|---|---|---|
| n | % | n | % | |
| Sex | 9 | (1.98) | ||
| Male | 397 | (87.44) | ||
| Female | 48 | (10.57) | ||
| Race | 9 | (1.98) | ||
| White | 243 | (53.52) | ||
| American Indian or Alaska Native | 19 | (4.19) | ||
| Asian | 6 | (1.32) | ||
| Black or African American | 105 | (23.13) | ||
| Native Hawaiian or Pacific Islander | 1 | (0.22) | ||
| Other | 31 | (6.83) | ||
| Hispanic | 15 | (3.30) | 40 | (8.81) |
| Marital status | 9 | (1.98) | ||
| Married, live together | 327 | (72.03) | ||
| Live together, committed relationship | 20 | (4.41) | ||
| Married, separated | 11 | (2.42) | ||
| Divorced | 59 | (13.00) | ||
| Widowed | 6 | (1.32) | ||
| Single, never married | 22 | (4.85) | ||
| VA Service Connected | 13 | (2.86) | 339 | (74.67) |
| Endorsed any combat exposure | 10 | (2.20) | 310 | (68.28) |
| Lifetime mental health diagnoses | ||||
| PTSD | 37 | (8.15) | 173 | (38.11) |
| Depression | 37 | (8.15) | 183 | (40.31) |
| Lifetime medical diagnoses | ||||
| GWI/CMI | 64 | (14.10) | 89 | (19.60) |
| Gastrointestinal problems | 45 | (9.91) | 164 | (36.12) |
| Irritable bowel syndrome | 52 | (11.45) | 92 | (20.26) |
| Arthritis | 36 | (7.93) | 222 | (48.90) |
| Fibromyalgia | 57 | (12.56) | 33 | (7.27) |
| Chronic fatigue syndrome | 54 | (11.89) | 81 | (17.84) |
| Asthma | 57 | (12.56) | 64 | (14.10) |
| COPD or emphysema | 61 | (13.44) | 35 | (7.71) |
Note. All percentages based on the full N = 454 sample; VA = Department of Veterans Affairs; PTSD = posttraumatic stress disorder; GWI/CMI = Gulf War Illness/Chronic Multisymptom Illness; COPD = chronic obstructive pulmonary disease.
Figure 1.
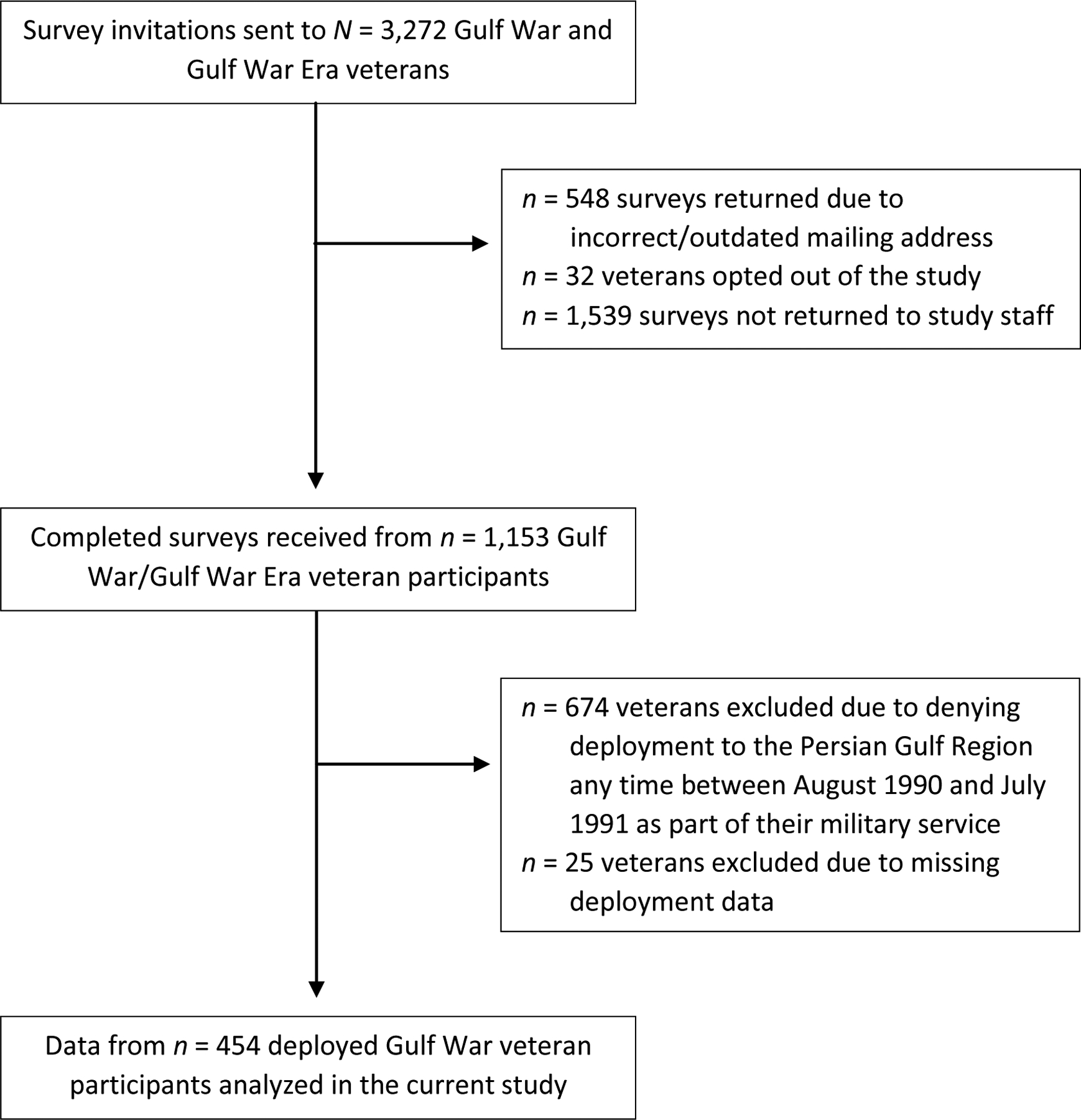
Participant Flow
Measures
Demographic Information.
Veterans reported their age, sex, race, ethnicity, marital status, and Department of Veterans Affairs (VA) service-connection status.
Mental and Medical Health Outcomes.
Veterans reported whether they had ever been diagnosed with the following problems using a yes/no response format: PTSD, depression, GWI/CMI, gastrointestinal problems, irritable bowel syndrome, arthritis, fibromyalgia, chronic fatigue syndrome, asthma, and COPD/emphysema.
Combat Exposure.
Combat exposure was assessed with the 7-item Critical Warzone Experiences Scale (Kimbrel et al., 2014). Respondents rated the frequency to which they experienced each event during combat (e.g., “being directly responsible for the death of an enemy combatant”) using a 5-point Likert scale ranging from 0 (Never) to 4 (10 or more times). Combat exposure was dichotomized as either endorsed (score > 0) or denied (score = 0). The Critical Warzone Experiences Scale has demonstrated a single factor structure, good internal consistency, good test-retest reliability, and good convergent validity with other combat exposure scales (Kimbrel et al., 2015, 2014). Internal consistency in the current sample was good (Cronbach’s α = .84).
NBC Exposure.
NBC exposure was assessed with the Deployment Risk & Resilience Inventory-2 (DRRI-2; Vogt et al., 2012) NBC Exposure subscale (Section F), which includes 13 polytomous items. Respondents rated the extent to which they believed they encountered various NBCs during military deployment, which were scored as 0 (No), 1 (Not sure), or 2 (Yes). The DRRI-2 has demonstrated strong internal consistency and criterion-related validity in previous work (Vogt et al., 2013). Internal consistency in the current sample was excellent (Cronbach’s α = .91).
Experiential Avoidance.
EA was assessed with the Brief Experiential Avoidance Questionnaire (BEAQ; Gámez et al., 2014), a validated 15-item measure derived from the longer Multidimensional Experiential Avoidance Questionnaire (MEAQ; Gámez et al., 2011). Respondents rated the degree to which they agreed with each item (e.g., “I go out of my way to avoid uncomfortable situations”) using a 7-point Likert scale ranging from 0 (Strongly disagree) to 6 (Strongly agree). One item (item 6; “Fear or anxiety won’t stop me from doing something important”) is reverse-scored. The BEAQ has shown good internal consistency, convergent validity, and discriminant validity in previous work (Gámez et al., 2014). Internal consistency in the current sample was excellent (Cronbach’s α = .91).
Data Analytic Plan
Analyses were conducted between February and June 2021 using R Statistical Software Version 4.0.2 (R Foundation for Statistical Computing, 2020). We applied multivariate imputation by chained equations using the “mice” package in R (van Buuren and Groothuis-Oudshoorn, 2011) to handle missing data for all variables other than diagnostic outcome variables. Continuous measure internal consistencies were estimated using all available data prior to multiple imputation. Mean item-level DRRI-2 and BEAQ scores were calculated after multiple imputation procedures to yield easily interpretable measures of overall NBC exposure and EA, respectively.
We first computed descriptive statistics to characterize the sample’s sociodemographic background and health histories. We then conducted chi-square tests of independence to examine bivariate associations between putative health risk factors (i.e., age, sex, race, combat exposure, NBC exposure, and EA) and health outcomes. Continuous measures of participant age (Mdn age = 56 years old), NBC exposure (Mdn = 1.54) and EA (Mdn = 2.73) were dichotomized via median-split in the full sample for chi-square analyses only.
Next, we computed a series of logistic regression models to test our hypotheses regarding the multivariate effects of EA on health outcomes after adjusting for age, sex, race, combat exposure, and NBC exposure. Effect sizes accompany all bivariate (Cranmer’s φ; Kotrlik et al., 2011) and multivariate (Cohen’s d; Chinn, 2000) estimates. For ease of presentation, only EA-related estimates and effect sizes are displayed in the tables; complete output is included in the Supplementary File.
Results
Preliminary Analyses
Visual inspection and quantitative analysis (i.e., skewness and kurtosis) of continuous measure data suggested approximately normal distribution. Our national sample of deployed Gulf War veterans had an average 57.14 years of age (SD = 7.20; ages ranged 47 to 90 years old). Mean item-level scores indicated the overall sample reported moderately high perceived NBC exposure (M = 1.36, SD = 0.61, n = 15 missing) and fairly low (i.e., relatively good) EA (BEAQ: M = 2.86, SD = 1.24, n = 0 missing). Shown in Table 1, our sample was mostly white, married, and VA service-connected. Nearly two-thirds of the sample endorsed combat exposure. Rates of lifetime PTSD and depression in our sample were comparable to each other. The most commonly endorsed medical diagnoses were arthritis, irritable bowel syndrome, and GWI/CMI.
Bivariate Analyses
EA-related findings from chi-square tests of independence are summarized in Table 2 (see Supplementary File for complete results). Higher EA was significantly associated with lifetime diagnoses of PTSD, depression, GWI/CMI, gastrointestinal problems, irritable bowel syndrome, arthritis, fibromyalgia, chronic fatigue syndrome, and asthma (ps ≤ .021; effect sizes ranged small to moderate). EA was not significantly associated with lifetime COPD/emphysema at the bivariate level.
Table 2.
Summary of Bivariate (Chi-Square) Tests of Associations between EA and Health Outcomes
| Lifetime Diagnosis | High EA (n = 238) | Low EA (n = 216) | X2 | φ | p | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| PTSD | 138 | (30.40) | 35 | (7.71) | 85.07 | .45 | < .001 |
| Depression | 135 | (29.74) | 48 | (10.57) | 59.07 | .38 | < .001 |
| GWI/CMI | 66 | (14.54) | 23 | (5.07) | 23.62 | .25 | < .001 |
| Gastrointestinal problems | 102 | (22.47) | 62 | (13.66) | 12.90 | .18 | < .001 |
| Irritable bowel syndrome | 64 | (14.10) | 28 | (6.17) | 15.18 | .19 | < .001 |
| Arthritis | 133 | (29.30) | 89 | (19.60) | 9.41 | .15 | .002 |
| Fibromyalgia | 26 | (5.73) | 7 | (1.54) | 10.82 | .17 | .001 |
| Chronic fatigue syndrome | 64 | (14.10) | 17 | (3.74) | 30.23 | .27 | < .001 |
| Asthma | 42 | (9.25) | 22 | (4.85) | 5.36 | < .01 | .021 |
| COPD or emphysema | 18 | (3.96) | 17 | (3.74) | < 0.01 | < .01 | .953 |
Note. Percentages based on the full N = 454 sample; degrees of freedom for all tests = 1; EA = experiential avoidance; φ = phi effect size coefficient, where 0.1, 0.3, and 0.5 signify effects of small, medium, and large magnitude, respectively; see Table 1 for information about missing data for each individual diagnostic outcome variable; see Supplementary File for complete output.
Multivariate Analyses
EA-related logistic regression findings are summarized in Table 3 (see Supplementary File for complete results). Mental health analyses supported study hypotheses. After adjusting for demographic covariates, combat exposure, and NBC exposure, greater (worse) EA was associated with significantly higher odds of lifetime PTSD and depression. Medical health analyses partially supported hypotheses. After adjusting for demographic covariates and military-related exposures, higher EA was associated with significantly higher odds of lifetime GWI/CMI, gastrointestinal problems, irritable bowel syndrome, arthritis, fibromyalgia, and chronic fatigue syndrome, (effect sizes ranged small to large), but not asthma or COPD/emphysema.
Table 3.
Summary of Multivariate (Logistic Regression) Tests of Associations between EA and Health Outcomes
| Multivariate Effect of EA, Adjusting for Age, Sex, Race, Combat Exposure, and NBC Exposure | |||||
|---|---|---|---|---|---|
| Lifetime Mental Health Diagnosis | OR | 95% CI | c | d | |
| Lower | Upper | ||||
| PTSD | 2.89*** | 2.28 | 3.73 | .86 | 0.59 |
| Depression | 2.25*** | 1.83 | 2.80 | .79 | 0.45 |
| Lifetime Medical Diagnosis | OR | 95% CI | c | d | |
| Lower | Upper | ||||
| GWI/CMI | 1.50*** | 1.19 | 1.90 | .78 | 0.22 |
| Gastrointestinal problems | 1.28** | 1.07 | 1.54 | .64 | 0.14 |
| Irritable bowel syndrome | 1.35** | 1.09 | 1.67 | .70 | 0.17 |
| Arthritis | 1.25* | 1.05 | 1.49 | .67 | 0.12 |
| Fibromyalgia | 1.57** | 1.14 | 2.21 | .77 | 0.25 |
| Chronic fatigue syndrome | 1.74*** | 1.39 | 2.22 | .73 | 0.31 |
| Asthma | 1.25 | 0.98 | 1.59 | .65 | 0.12 |
| COPD or emphysema | 1.05 | 0.77 | 1.42 | .64 | 0.03 |
Note: OR = odds ratio; CI = confidence interval; effect size d approximated using procedures described by Chinn (2000), where 0.1, 0.3, and 0.5 signify effects of small, medium, and large magnitude, respectively;
p < .05,
p < .01,
p < .001;
see Supplementary File for complete output.
Discussion
U.S. veterans deployed to the Persian Gulf region in service of 1990–1991 Gulf War military operations have endorsed higher rates of mental health problems such as PTSD and depression than their non-deployed Gulf War Era veteran counterparts (Toomey et al., 2007). Moreover, deployed Gulf War veterans reported chronic, often idiopathic physical symptoms at higher rates than either non-deployed Gulf War Era veterans or veterans deployed to other regions during the same time period (Kang et al., 2009, 2003; Proctor et al., 1998; The Iowa Persian Gulf Study Group, 1997). Despite public and scientific interest in better understanding and optimizing Gulf War veteran health, etiologies for many common Gulf War veteran health problems are unknown and prognosis can be poor (White et al., 2016). The biopsychosocial model (Engel, 1977), which emphasizes the influence of physiological and psychosocial factors on health functioning, could meaningfully improve clinical models and interventions for Gulf War veteran health outcomes. The current study recruited a large national sample of deployed Gulf War veterans to test the hypothesis that EA—a psychosocial risk factor for numerous mental health disorders and certain medical health conditions—would be significantly associated with higher lifetime odds of PTSD, depression, and chronic illnesses commonly observed among deployed Gulf War veterans.
Rates of self-reported health diagnoses in our sample were comparable to previously studied samples of deployed Gulf War veterans (Dursa et al., 2020; Eisen et al., 2005; Karlinsky et al., 2004; Kipen et al., 1999; Tuteja et al., 2019; Zundel et al., 2019), although rates of asthma, COPD/emphysema, and arthritis were slightly higher than in prior studies (Dursa et al., 2020; Eisen et al., 2005; Karlinsky et al., 2004). Bivariate EA associations were strongest for PTSD and depression, but chi-square analyses also detected significant relationships between EA and lifetime diagnoses of GWI/CMI, gastrointestinal problems, irritable bowel syndrome, arthritis, fibromyalgia, chronic fatigue syndrome, and asthma. Logistic regression analyses adjusting for demographic factors and military-related exposures partially supported our hypotheses. Consistent with previous work in other veteran samples (Avery et al., 2018; Brockman et al., 2016; Bryan et al., 2015; Byllesby et al., 2020; Elliott et al., 2015; Kelly et al., 2019; Meyer et al., 2013, 2019b, 2019c, 2019a, 2018a), EA was associated with lifetime histories of PTSD and depression in multivariate analyses. Higher (i.e., worse) EA was also associated with higher odds of lifetime GWI/CMI, gastrointestinal problems, irritable bowel syndrome, arthritis, fibromyalgia, and chronic fatigue syndrome. Effect sizes for the relationship between EA and mental health outcomes were double to triple the magnitude of those found for the relationship between EA and medical health outcomes.
Contrary to hypotheses, EA was not significantly associated with asthma in multivariate analyses or with COPD/emphysema in either bivariate or multivariate analyses. Our results suggest that EA is less relevant to the experience of respiratory conditions than it is to pain, gastrointestinal, and fatigue-related disorders. Although research on EA and other psychosocial variables in the context of asthma and COPD is limited and equivocal (Michalova et al., 2021), it is possible that EA is less relevant to the maintenance of respiratory disorders than other psychosocial variables (e.g., anxiety sensitivity; Avallone et al., 2012; Simon et al., 2006; Witcraft et al., 2021).
Taken together, our findings suggest that the tendency to avoid, suppress, or otherwise attempt to control unpleasant internal experiences (e.g., thoughts, memories, and physical sensations) is related to many of deployed Gulf War veterans’ chronic medical and mental health problems. Our results align with previous work identifying EA as a prospective risk factor for various health problems (Berghoff et al., 2017; Chawla and Ostafin, 2007; Hildebrandt and Hayes, 2012; Spinhoven et al., 2014) and functional disability in veterans with chronic pain even after accounting for pain intensity and mental health symptoms (Cook et al., 2015). This study’s findings have positive implications for treatment; whereas providers cannot intervene on historical variables tied to poor health outcomes in this cohort (e.g., combat exposure and NBC exposure), psychosocial factors such as EA are modifiable biopsychosocial treatment targets. Though generally considered a stable trait (e.g., Spinhoven et al., 2014), previous clinical trials of psychosocial treatments showed EA was sensitive to change during standard VA inpatient and outpatient PTSD treatment (Byllesby et al., 2020). Other studies have shown that Acceptance and Commitment Therapy (ACT), which purports to exert therapeutic benefit in part by reducing EA, was useful for veterans with comorbid PTSD and alcohol use disorder (Meyer et al., 2018b) as well as Navy recruits with training injury-related acute pain (Udell et al., 2018). Other similar approaches (e.g., mindfulness-based treatment for PTSD, “transdiagnostic” cognitive-behavior therapy for anxiety) have also been shown to reduce EA among veterans (Espejo et al., 2017; Reyes et al., 2020). Understood within this larger literature, our findings suggest that adding acceptance-based, mindfulness-based, or cognitive-behavioral interventions as part of a biopsychosocial treatment plan could incrementally improve Gulf War veteran physical and mental health outcomes. Future research directly testing whether changes in EA during treatment facilitate improvements in symptom severity and/or functioning among Gulf War veterans is warranted.
Our findings also suggest it would be helpful for specialty medical care providers and mental health care professionals alike to assess for biological and psychosocial risk factors such as EA when evaluating patients with complex symptom presentations. This recommendation is consistent with VA’s whole-person approach to health care, which explicitly considers biological, cognitive, affective, social, and environmental factors shaping health functioning (Krejci et al., 2014). It would also be important for providers to communicate to veterans and their caregivers that physical health complaints are not “in someone’s head,” but that the manner in which someone psychologically and behaviorally responds to their symptoms can nevertheless influence symptom presentation and prognosis. Considering growing evidence that certain Gulf War-related health conditions (including GWI/CMI) may also affect military personnel deployed to Iraq and Afghanistan during subsequent conflicts (e.g., the Global War on Terrorism; DeBeer et al., 2017), future studies on the role of EA in the experience and treatment of chronic medical and mental health conditions in other veteran cohorts is needed.
This study had several strengths, such as the use of a large, nationally representative sample of deployed Gulf War veterans reporting diverse health histories and variable levels of EA and service-related exposures. Our study replicated previous research linking EA to post-deployment psychiatric disorders and extended prior work by demonstrating EA’s relationship to several complex, idiopathic medical conditions commonly reported by Gulf War veterans. Regarding external validity, the national sample of Project GRIT Gulf War/Gulf War Era veterans from which current study data were drawn was comparable to the larger population of VHA-enrolled veterans at the time of study completion in terms of age and race, and women veterans were adequately represented in our sample due to deliberate oversampling of women veterans in Project GRIT. At the same time, our findings should be contextualized by study limitations. Because our study of deployed Gulf War veterans did not include a comparison group, for example, our data do not speak to the association between EA and various medical and mental health diagnoses among non-veterans, non-deployed Gulf War veterans, or veterans of other military conflicts.
Additionally, our cross-sectional design precludes drawing causal inferences. Future research incorporating longitudinal design would help to understand prospective relationships between military experiences, EA, and medical and mental health diagnoses among veterans. Our survey also relied on self-reported diagnoses and retrospective assessment of military service-related exposures, which could have been biased by recall error. Nor can we rule out the influence of other medical and mental illness risk factors such as social support (Ren et al., 1999) or somatosensory catastrophizing (Edwards et al., 2016; Seto and Nakao, 2017) on diagnostic outcomes.
Another limiting factor regards how EA was measured in this study. Although EA was originally conceptualized as a general unwillingness to experience a broad set of unpleasant internal states (Hayes et al., 1996), investigators have recently demonstrated that EA can also be specific to certain issues such as substance use (Luoma et al., 2011), psychotic symptoms (Shawyer et al., 2007), body image concerns (Sandoz et al., 2013), obsessive-compulsive symptoms (Jacoby et al., 2018), trichotillomania (Houghton et al., 2014), and social anxiety (MacKenzie and Kocovski, 2010). Thus, although our sample reported fairly low (i.e., adaptive) EA overall, we do not know whether veteran participants would have endorsed higher (i.e., worse) EA if asked to specifically consider their deployment-related experiences when responding. One worthwhile area of future research, therefore, would be to develop military-specific measures of EA to more precisely investigate the associations between military deployment, EA, and post-deployment health outcomes. These limitations notwithstanding, our study provides empirical support for the incremental utility of incorporating transdiagnostic biopsychosocial variables into veteran health case conceptualization and assessment. Future research testing whether holistic treatment approaches lead to superior Gulf War veteran health outcomes–and whether those treatment improvements are driven by reductions in EA—would also be helpful.
Supplementary Material
Highlights.
Many Gulf War veterans have developed chronic, difficult-to-treat illnesses
Biopsychosocial models can improve chronic illness diagnosis and treatment
Experiential avoidance (EA) is a psychosocial mental/medical illness risk factor
EA was associated with PTSD, depression, and several chronic medical illnesses
EA-focused assessment and intervention might improve Gulf War veterans’ health
Acknowledgement
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the United States Government or Department of Veterans Affairs (VA). Preparation of this report was supported by VA grant 1I01HX001682. Dr. Blakey was supported by the Department of Veterans Affairs Office of Academic Affiliations Advanced Fellowship in Mental Illness Research and Treatment. Dr. Beckham was funded by a Senior Research Career Scientist award from VA Clinical Sciences Research and Development (IK6BX00377). Dr. Pugh was funded by a Research Career Scientist Award from VA Health Services Research and Development (IK6HX002608).
Footnotes
Declarations of interest: None.
References
- Avallone KM, McLeish AC, Luberto CM, Bernstein JA, 2012. Anxiety sensitivity, asthma control, and quality of life in adults with asthma. J. Asthma 49, 57–62. 10.3109/02770903.2011.641048 [DOI] [PubMed] [Google Scholar]
- Avery T, Blasey C, Rosen C, Bayley P, 2018. Psychological Flexibility and Set-Shifting among Veterans Participating in a Yoga Program: A Pilot Study. Mil. Med 183, E359–E363. 10.1093/milmed/usy045 [DOI] [PubMed] [Google Scholar]
- Berghoff CR, Tull MT, DiLillo D, Messman-Moore T, Gratz KL, 2017. The Role of Experiential Avoidance in the Relation between Anxiety Disorder Diagnoses and Future Physical Health Symptoms in a Community Sample of Young Adult Women. J. Context. Behav. Sci 6, 29–34. 10.1016/j.jcbs.2016.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bevers K, Watts L, Kishino ND, Gatchel RJ, 2016. The biopsychosocial model of the assessment, prevention, and treatment of chronic pain. US Neurol. 12, 98–104. 10.17925/USN.2016.12.02.98 [DOI] [Google Scholar]
- Boot CRL, Van Exel NJA, Van Der Gulden JWJ, 2009. “My lung disease won’t go away, it’s there to stay”: Profiles of adaptation to functional limitations in workers with asthma and COPD. J. Occup. Rehabil 19, 284–292. 10.1007/s10926-009-9185-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowes MA, Ferreira NB, Henderson M, 2018. The influence of psychosocial factors in veteran adjustment to civilian life. Clin. Psychol. Psychother 25, 583–600. 10.1002/cpp.2182 [DOI] [PubMed] [Google Scholar]
- Brockman C, Snyder J, Gewirtz A, Gird SR, Quattlebaum J, Schmidt N, Pauldine MR, Elish K, Schrepferman L, Hayes C, Zettle R, 2016. Relationship of service members’ deployment trauma, PTSD symptoms, and experiential avoidance to postdeployment family reengagement. J. Fam. Psychol 30, 52–62. 10.1037/fam0000152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan CJ, Ray-Sannerud B, Heron EA, 2015. Psychological flexibility as a dimension of resilience for posttraumatic stress, depression, and risk for suicidal ideation among Air Force personnel. J. Context. Behav. Sci 4, 263–268. 10.1016/j.jcbs.2015.10.002 [DOI] [Google Scholar]
- Byllesby BM, Coe LES, Dickstein BD, Chard KM, 2020. Psychometric evaluation of the brief experiential avoidance questionnaire among treatment-seeking veterans with posttraumatic stress disorder. Psychol. Trauma Theory, Res. Pract. Policy 12, 785–789. 10.1037/tra0000581 [DOI] [PubMed] [Google Scholar]
- Cassar GE, Knowles S, Youssef GJ, Moulding R, Uiterwijk D, Waters L, Austin DW, 2018. Examining the mediational role of psychological flexibility, pain catastrophizing, and visceral sensitivity in the relationship between psychological distress, irritable bowel symptom frequency, and quality of life. Psychol. Heal. Med 23, 1168–1181. 10.1080/13548506.2018.1476722 [DOI] [PubMed] [Google Scholar]
- Chawla N, Ostafin B, 2007. Experiential avoidance as a functional dimensional approach to psychopathology: An empirical review. J. Clin. Psychol 63, 871–890. 10.1002/jclp.20400 [DOI] [PubMed] [Google Scholar]
- Chinn S, 2000. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat. Med 19, 3127–3131. [DOI] [PubMed] [Google Scholar]
- Cobb AR, Lancaster CL, Meyer EC, Lee HJ, Telch MJ, 2017. Pre-deployment trait anxiety, anxiety sensitivity and experiential avoidance predict war-zone stress-evoked psychopathology. J. Context. Behav. Sci 6, 276–287. 10.1016/j.jcbs.2017.05.002 [DOI] [Google Scholar]
- Cook AJ, Meyer EC, Evans LD, Vowles KE, Klocek JW, Kimbrel NA, Gulliver SB, Morissette SB, 2015. Chronic pain acceptance incrementally predicts disability in polytrauma-exposed veterans at baseline and 1-year follow-up. Behav. Res. Ther 73, 25–32. 10.1016/j.brat.2015.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeBeer BB, Davidson D, Meyer EC, Kimbrel NA, Gulliver SB, Morissette SB, 2017. The association between toxic exposures and chronic multisymptom illness in veterans of the wars of Iraq and Afghanistan. J. Occup. Environ. Med 59, 54–60. 10.1097/JOM.0000000000000922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillman DA, Smyth JD, Christian LM, 2014. Internet, phone, mail, and mixed-mode surveys: The tailored design method, 4th ed.Wiley, Hoboken, NJ. [Google Scholar]
- Dursa EK, Tadesse BE, Carter CE, Culpepper WJ, Schneiderman AI, Rumm PD, 2020. Respiratory illness among Gulf War and Gulf War era veterans who use the Department of Veterans Affairs for healthcare. Am. J. Ind. Med 63, 980–987. 10.1002/ajim.23172 [DOI] [PubMed] [Google Scholar]
- Edwards RR, Dworkin RH, Sullivan MD, Turk DC, Wasan AD, 2016. The role of psychosocial processes in the development and maintenance of chronic pain disorders. J. Pain 17, T70–T92. 10.1016/j.jpain.2016.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisen SA, Kang HK, Murphy FM, Blanchard MS, Reda DJ, Henderson WG, Toomey R, Jackson LW, Alpern R, Parks BJ, Klimas N, Hall C, Pak HS, Hunter J, Karlinsky J, Battistone MJ, Lyons MJ, 2005. Gulf War veterans’ health: Medical evaluation of a U.S. cohort. Ann. Intern. Med 142, 881–890. [DOI] [PubMed] [Google Scholar]
- Elliott TR, Hsiao YY, Kimbrel NA, Meyer EC, DeBeer BB, Gulliver SB, Kwok OM, Morissette SB, 2015. Resilience, traumatic brain injury, depression, and posttraumatic stress among Iraq/Afghanistan war veterans. Rehabil. Psychol 60, 263–276. 10.1037/rep0000050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel GL, 1977. The need for a new medical model: A challenge for biomedicine. Science (80-.) 196, 129–136. 10.1126/science.847460 [DOI] [PubMed] [Google Scholar]
- Espejo EP, Gorlick A, Castriotta N, 2017. Changes in threat-related cognitions and experiential avoidance in group-based transdiagnostic CBT for anxiety disorders. J. Anxiety Disord 46, 65–71. 10.1016/j.janxdis.2016.06.006 [DOI] [PubMed] [Google Scholar]
- Ferrari R, 2000. The biopsychosocial model: A tool for rheumatologists. Best Pract. Res. Clin. Rheumatol 14, 787–795. 10.1053/berh.2000.0113 [DOI] [PubMed] [Google Scholar]
- Ferrari R, Russell AS, 2001. The problem of Gulf War syndrome. Med. Hypotheses 56, 697–701. 10.1054/mehy.2001.1311 [DOI] [PubMed] [Google Scholar]
- Ferreira NB, Eugenicos M, Morris PG, Gillanders D, 2011. Using acceptance and commitment therapy in irritible bowel syndrome. Gastrointest. Nurs 9, 28–35. [Google Scholar]
- Ferreira NB, Gillanders D, Morris PG, Eugenicos M, 2018. Pilot study of acceptance and commitment therapy for irritable bowel syndrome: A preliminary analysis of treatment outcomes and processes of change. Clin. Psychol 22, 241–250. 10.1111/cp.12123 [DOI] [Google Scholar]
- Fukuda K, Nisenbaum R, Stewart G, Thompson WW, Robin L, Washko RM, Noah DL, Barrett DH, Randall B, Herwaldt BL, Mawle AC, Reeves WC, 1998. Chronic multisymptom illness affecting Air Force veterans of the Gulf War. JAMA 280, 981–988. 10.1001/jama.280.11.981 [DOI] [PubMed] [Google Scholar]
- Gámez W, Chmielewski M, Kotov R, Ruggero C, Suzuki N, Watson D, 2014. The Brief Experiential Avoidance Questionnaire: Development and initial validation. Psychol. Assess 26, 35–45. 10.1037/a0034473 [DOI] [PubMed] [Google Scholar]
- Gámez W, Chmielewski M, Kotov R, Ruggero C, Watson D, 2011. Development of a measure of experiential avoidance: The Multidimensional Experiential Avoidance Questionnaire. Psychol. Assess 23, 692–713. 10.1037/a0023242 [DOI] [PubMed] [Google Scholar]
- Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC, 2007. The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychol. Bull 133, 581–624. 10.1037/0033-2909.133.4.581 [DOI] [PubMed] [Google Scholar]
- Gillanders D, Ferreira NB, Angioni E, Carvalho SA, Eugenicos MP, 2017. An implementation trial of ACT-based bibliotherapy for irritable bowel syndrome. J. Context. Behav. Sci 6, 172–177. 10.1016/j.jcbs.2017.04.006 [DOI] [Google Scholar]
- Halpert A, Drossman D, 2005. Biopsychosocial issues in irritable bowel syndrome. J. Clin. Gastroenterol 39, 665–669. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Follette VM, Strosahl K, 1996. Experimental avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. J. Consult. Clin. Psychol 64, 1152–1168. 10.1037//0022-006x.64.6.1152 [DOI] [PubMed] [Google Scholar]
- Hildebrandt MJ, Hayes SC, 2012. The contributing role of negative affectivity and experiential avoidance to increased cardiovascular risk. Soc. Personal. Psychol. Compass 6, 551–565. 10.1111/j.1751-9004.2012.00448.x [DOI] [Google Scholar]
- Houghton DC, Compton SN, Twohig MP, Saunders SM, Franklin ME, Neal-Barnett AM, Ely L, Capriotti MR, Woods DW, 2014. Measuring the role of psychological inflexibility in Trichotillomania. Psychiatry Res. 220, 356–361. 10.1016/j.psychres.2014.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine, 2014. Chronic Multisymptom Illness in Gulf War veterans: Case definitions reexamined. Washington, DC. 10.17226/18623 [DOI] [PubMed] [Google Scholar]
- Jacoby RJ, Abramowitz JS, Buchholz J, Reuman L, Blakey SM, 2018. Experiential avoidance in the context of obsessions: Development and validation of the Acceptance and Action Questionnaire for Obsessions and Compulsions. J. Obsessive. Compuls. Relat. Disord 19, 34–43. 10.1016/j.jocrd.2018.07.003 [DOI] [Google Scholar]
- Kang HK, Li B, Mahan CM, Eisen SA, Engel CC, 2009. Health of US veterans of 1991 Gulf War: a follow-up survey in 10 years. J. Occup. Environ. Med 51, 401–410. 10.1097/JOM.0b013e3181a2feeb [DOI] [PubMed] [Google Scholar]
- Kang HK, Natelson BH, Mahan CM, Lee KY, Murphy FM, 2003. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among gulf war veterans: A population-based survey of 30,000 veterans. Am. J. Epidemiol 157, 141–148. 10.1093/aje/kwf187 [DOI] [PubMed] [Google Scholar]
- Karademas EC, Karekla M, Flouri M, Vasiliou VS, Kasinopoulos O, Papacostas SS, 2017. The impact of experiential avoidance on the relations between illness representations, pain catastrophising and pain interference in chronic pain. Psychol. Heal 32, 1469–1484. 10.1080/08870446.2017.1346193 [DOI] [PubMed] [Google Scholar]
- Karlinsky JB, Blanchard M, Alpern R, Eisen SA, Kang H, Murphy FM, Reda DJ, 2004. Late prevalence of respiratory symptoms and pulmonary function abnormalities in Gulf War I veterans. Arch. Intern. Med 164, 2488–2491. 10.1001/archinte.164.22.2488 [DOI] [PubMed] [Google Scholar]
- Kashdan TB, 2010. Psychological flexibility as a fundamental aspect of health. Clin. Psychol. Rev 30, 865–878. 10.1016/j.cpr.2010.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly MM, DeBeer BB, Meyer EC, Kimbrel NA, Gulliver SB, Morissette SB, 2019. Experiential avoidance as a mediator of the association between posttraumatic stress disorder symptoms and social support: A longitudinal analysis. Psychol. Trauma Theory, Res. Pract. Policy 11, 353–359. 10.1037/tra0000375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelsall HL, McKenzie DP, Sim MR, Leder K, Forbes AB, Dwyer T, 2009. Physical, Psychological, and Functional Comorbidities of Multisymptom Illness in Australian Male Veterans of the 1991 Gulf War. Am. J. Epidemiol 170, 1048–1056. 10.1093/aje/kwp238 [DOI] [PubMed] [Google Scholar]
- Kimbrel NA, DeBeer BB, Meyer EC, Silvia PJ, Beckham JC, Young KA, Morissette SB, 2015. An examination of the broader effects of warzone experiences on returning Iraq/Afghanistan veterans’ psychiatric health. Psychiatry Res. 226, 78–83. 10.1016/j.psychres.2014.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Evans LD, Patel AB, Wilson LC, Meyer EC, Gulliver SB, Morissette SB, 2014. The Critical Warzone Experiences (CWE) scale: Initial psychometric properties and associations with PTSD, anxiety, and depression. Psychiatry Res. 220, 1118–1124. 10.1016/j.psychres.2014.08.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King LA, King DW, Bolton EE, Knight JA, Vogt DS, 2008. Risk factors for mental, physical, and functional health in Gulf War veterans. J. Rehabil. Res. Dev 45, 395–407. 10.1682/jrrd.2007.06.0081 [DOI] [PubMed] [Google Scholar]
- King LA, King DW, Vogt DS, Knight J, Samper RE, 2006. Deployment Risk and Resilience Inventory: A collection of measures for studying deployment-related Experiences of military personnel and beterans. Mil. Psychol 18, 89–120. 10.1207/s15327876mp1802_1 [DOI] [Google Scholar]
- Kipen HM, Hallman W, Kang H, Fiedler N, Natelson BH, 1999. Prevalence of chronic fatigue and chemical sensitivities in Gulf Registry Veterans. Arch. Environ. Health 54, 313–318. 10.1080/00039899909602493 [DOI] [PubMed] [Google Scholar]
- Kotrlik J, Williams H, Jabor K, 2011. Reporting and interpreting effect size in quantitative agricultural education research. J. Agric. Educ 52, 132–142. 10.5032/jae.2011.01132 [DOI] [Google Scholar]
- Krejci LP, Carter K, Gaudet T, 2014. Whole health: The vision and implementation of personalized, proactive, patient-driven health care for veterans. Med. Care 52, S5–S8. 10.1097/MLR.0000000000000226 [DOI] [PubMed] [Google Scholar]
- Luoma J, Drake CE, Kohlenberg BS, Hayes SC, 2011. Substance abuse and psychological flexibility: The development of a new measure. Addict. Res. Theory 19, 3–13. 10.3109/16066359.2010.524956 [DOI] [Google Scholar]
- Luxton DD, Skopp NA, Maguen S, 2010. Gender differences in depression and PTSD symptoms following combat exposure. Depress. Anxiety 27, 1027–1033. 10.1002/da.20730 [DOI] [PubMed] [Google Scholar]
- MacKenzie MB, Kocovski NL, 2010. Self-reported acceptance of social anxiety symptoms: Development and validation of the Social Anxiety—Acceptance and Action Questionnaire. Int. J. Behav. Consult. Ther 6, 214–232. 10.1037/h0100909 [DOI] [Google Scholar]
- McCracken LM, Velleman SC, 2010. Psychological flexibility in adults with chronic pain: A study of acceptance, mindfulness, and values-based action in primary care. Pain 148, 141–147. 10.1016/j.pain.2009.10.034 [DOI] [PubMed] [Google Scholar]
- Meyer EC, Frankfurt SB, Kimbrel NA, DeBeer BB, Gulliver SB, Morrisette SB, 2018a. The influence of mindfulness, self-compassion, psychological flexibility, and posttraumatic stress disorder on disability and quality of life over time in war veterans. J. Clin. Psychol 74, 1272–1280. 10.1002/jclp.22596 [DOI] [PubMed] [Google Scholar]
- Meyer EC, Kotte A, Kimbrel NA, DeBeer BB, Elliott TR, Gulliver SB, Morissette SB, 2019a. Predictors of lower-than-expected posttraumatic symptom severity in war veterans: The influence of personality, self-reported trait resilience, and psychological flexibility. Behav. Res. Ther 113, 1–8. 10.1016/j.brat.2018.12.005 [DOI] [PubMed] [Google Scholar]
- Meyer EC, La Bash H, DeBeer BB, Kimbrel NA, Gulliver SB, Morissette SB, 2019b. Psychological inflexibility predicts PTSD symptom severity in war veterans after accounting for established PTSD risk factors and personality. Psychol. Trauma Theory, Res. Pract. Policy 11, 383–390. 10.1037/tra0000358 [DOI] [PubMed] [Google Scholar]
- Meyer EC, Morissette SB, Kimbrel NA, Kruse MI, Gulliver SB, 2013. Acceptance and Action Questionnaire-II scores as a predictor of posttraumatic stress disorder symptoms among war veterans. Psychol. Trauma Theory, Res. Pract. Policy 5, 521–528. 10.1037/a0030178 [DOI] [Google Scholar]
- Meyer EC, Szabo YZ, Frankfurt SB, Kimbrel NA, DeBeer BB, Morissette SB, 2019c. Predictors of recovery from post-deployment posttraumatic stress disorder symptoms in war veterans: The contributions of psychological flexibility, mindfulness, and self-compassion. Behav. Res. Ther 114, 7–14. 10.1016/j.brat.2019.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer EC, Walser R, Hermann B, La Bash H, DeBeer BB, Morissette SB, Kimbrel NA, Kwok O-M, Batten SV, Schnurr PP, 2018b. Acceptance and Commitment Therapy for co-occurring posttraumatic stress disorder and alcohol use disorders in Veterans: Pilot treatment outcomes. J. Trauma. Stress 31, 781–789. 10.1002/jts.22322 [DOI] [PubMed] [Google Scholar]
- Michalova L, Dhasmana DJ, Chaudhuri R, Yang JF, Smith SJ, Morris PG, 2021. The role of generalised anxiety in asthma outcomes: Experiential avoidance and self-efficacy as mediators. Thorax 76, A127 LP–A128. 10.1136/thorax-2020-BTSabstracts.220 [DOI] [Google Scholar]
- Porter B, Bonanno GA, Bliese PD, Phillips CJ, Proctor SP, 2019. Combat and trajectories of physical health functioning in U.S. Service Members. Am. J. Prev. Med 57, 637–644. 10.1016/j.amepre.2019.06.015 [DOI] [PubMed] [Google Scholar]
- Proctor SP, Heeren T, White RF, Wolfe J, Borgos MS, Davis JD, Pepper L, Clapp R, Sutker PB, Vasterling JJ, Oznoff D, 1998. Health status of Persian Gulf War veterans: self-reported symptoms, environmental exposures and the effect of stress. Int. J. Epidemiol 27, 1000–1010. 10.1093/ije/27.6.1000 [DOI] [PubMed] [Google Scholar]
- R Foundation for Statistical Computing, 2020. R: A language and environment for statistical computing.
- Ren XS, Skinner K, Lee A, Kazis L, 1999. Social support, social selection and self-assessed health status: Results from the veterans health study in the United States. Soc. Sci. Med 48, 1721–1734. 10.1016/S0277-9536(99)00069-6 [DOI] [PubMed] [Google Scholar]
- Research Advisory Committee on Gulf War Veterans’ Illnesses, 2014. Gulf War Illness and the health of Gulf War veterans: Resarch update and recommendations, 2009–2013 Washington, DC. [Google Scholar]
- Reyes AT, Bhatta TR, Muthukumar V, Gangozo WJ, 2020. Testing the acceptability and initial efficacy of a smartphone-app mindfulness intervention for college student veterans with PTSD. Arch. Psychiatr. Nurs 34, 58–66. 10.1016/j.apnu.2020.02.004 [DOI] [PubMed] [Google Scholar]
- Riegle DW, 1994. U.S. Chemical and Biological Warfare-Related Dual Use Exports to Iraq and their Possible Impact on the Health Consequences of the Gulf War Washington, DC. [Google Scholar]
- Sandoz EK, Wilson KG, Merwin RM, Kate Kellum K, 2013. Assessment of body image flexibility: The Body Image-Acceptance and Action Questionnaire. J. Context. Behav. Sci 2, 39–48. 10.1016/j.jcbs.2013.03.002 [DOI] [Google Scholar]
- Seto H, Nakao M, 2017. Relationships between catastrophic thought, bodily sensations and physical symptoms. Biopsychosoc. Med 11, 1–8. 10.1186/s13030-017-0110-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shawyer F, Ratcliff K, Mackinnon A, Farhall J, Hayes SC, Copolov D, 2007. The Voices Acceptance and Action Scale (VAAS): Pilot data. J. Clin. Psychol 63, 593–606. 10.1002/jclp.20366 [DOI] [PubMed] [Google Scholar]
- Sheffler JL, Rushing NC, Stanley IH, Sachs-Ericsson NJ, 2016. The long-term impact of combat exposure on health, interpersonal, and economic domains of functioning. Aging Ment. Health 20, 1202–1212. 10.1080/13607863.2015.1072797 [DOI] [PubMed] [Google Scholar]
- Simon NM, Weiss AM, Kradin R, Evans KC, Reese HE, Otto MW, Oppenheimer JE, Smoller JW, Zalta A, Worthington JJ, Pollack MH, 2006. The relationship of anxiety disorders, anxiety sensitivity and pulmonary dysfunction with dyspnea-related distress and avoidance. J. Nerv. Ment. Dis 194, 951–957. 10.1097/01.nmd.0000249062.25829.53 [DOI] [PubMed] [Google Scholar]
- Spinhoven P, Drost J, de Rooij M, van Hemert AM, Penninx BW, 2014. A longitudinal study of experiential avoidance in emotional disorders. Behav. Ther 45, 840–850. 10.1016/j.beth.2014.07.001 [DOI] [PubMed] [Google Scholar]
- The Iowa Persian Gulf Study Group, 1997. Self-reported illness and health status among Gulf War veterans: A population-based study. JAMA 277, 238–245. [PubMed] [Google Scholar]
- Toomey R, Kang HK, Karlinsky J, Baker DG, Vasterling JJ, Alpern R, Reda DJ, Henderson WG, Murphy FM, Eisen SA, 2007. Mental health of US Gulf War veterans 10 years after the war. Br. J. Psychiatry 190, 385–393. 10.1192/bjp.bp.105.019539 [DOI] [PubMed] [Google Scholar]
- Trainor H, Baranoff J, Henke M, Winefield H, 2019. Functioning with fibromyalgia: The role of psychological flexibility and general psychological acceptance. Aust. Psychol 54, 214–224. 10.1111/ap.12363 [DOI] [Google Scholar]
- Tuteja AK, Talley NJ, Stoddard GJ, Samore MH, Verne GN, 2019. Risk factors for upper and lower functional gastrointestinal disorders in Persian Gulf War Veterans during and post-deployment. Neurogastroenterol. Motil 31, 1–13. 10.1111/nmo.13533 [DOI] [PubMed] [Google Scholar]
- Udell CJ, Ruddy JL, Procento PM, 2018. Effectiveness of Acceptance and Commitment Therapy in increasing resilience and reducing attrition of injured US Navy Recruits. Mil. Med 183, e603–e611. 10.1093/milmed/usx109 [DOI] [PubMed] [Google Scholar]
- Unwin C, Hotopf M, Hull L, Ismail K, David A, Wessely S, 2002. Women in the Persian Gulf: lack of gender differences in long-term health effects of service in United Kingdom Armed Forces in the 1991 Persian Gulf War. Mil. Med 167, 406–413. [PubMed] [Google Scholar]
- van Buuren S, Groothuis-Oudshoorn K, 2011. Mice: Multivariate imputation by chained equations in R. J. Stat. Softw 45, 1–67. 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- Van Oudenhove L, Levy RL, Crowell MD, Drossman DA, Halpert AD, Keefer L, Lackner JM, Murphy TB, Naliboff BD, 2016. Biopsychosocial aspects of functional gastrointestinal disorders: How central and environmental processes contribute to the development and expression of functional gastrointestinal disorders. Gastroenterology 150, 1355–1367.e2. 10.1053/j.gastro.2016.02.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt DS, Smith BN, King DW, King LA, 2012. Manual for the Deployment Risk & Resilience Inventory-2 (DRRI-2): A collection of measures for studying deployment-related experiences of military veterans.
- Vogt DS, Smith BN, King LA, King DW, Knight J, Vasterling JJ, 2013. Deployment Risk and Resilience Inventory-2 (DRRI-2): An updated tool for assessing psychosocial risk and resilience factors among service members and veterans. J. Trauma. Stress 26, 710–717. https://doi.org/10.1002.jts.21868 [DOI] [PubMed] [Google Scholar]
- White RF, Steele L, O’Callaghan JP, Sullivan K, Binns JH, Golomb BA, Bloom FE, Bunker JA, Crawford F, Graves JC, Hardie A, Klimas N, Knox M, Meggs WJ, Melling J, Philbert MA, Grashow R, 2016. Recent research on Gulf War illness and other health problems in veterans of the 1991 Gulf War: Effects of toxicant exposures during deployment. Cortex 74, 449–475. 10.1016/j.cortex.2015.08.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witcraft SM, Dixon LJ, Leukel P, Lee AA, 2021. Anxiety sensitivity and respiratory disease outcomes among individuals with chronic obstructive pulmonary disease. Gen. Hosp. Psychiatry 69, 1–6. 10.1016/j.genhosppsych.2020.12.004 [DOI] [PubMed] [Google Scholar]
- Wojcik W, Lawrie SM, 2016. Towards a biopsychosocial model of Gulf War Illness? EBioMedicine 3, 6–7. 10.1016/j.ebiom.2015.12.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe J, Proctor SP, Erickson DJ, Hu H, 2002. Risk Factors for Multisymptom Illness in US Army Veterans of the Gulf War. J. Occup. Environ. Med 44, 271–281. [DOI] [PubMed] [Google Scholar]
- Zundel CG, Krengel MH, Heeren T, Yee MK, Grasso CM, Janulewicz Lloyd PA, Coughlin SS, Sullivan K, 2019. Rates of chronic medical conditions in 1991 Gulf war veterans compared to the general population. Int. J. Environ. Res. Public Health 16, 1–16. 10.3390/ijerph16060949 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


