Abstract
Although headache attributed to hypothyroidism is coded within The International Classification of Headache Disorders, 3rd edition, an association between headache and thyrotoxicosis (hyperthyroidism) is mentioned only in the appendix. Reports on relevant cases are too scarce to establish a causal relationship. A young man with a history of migraine with aura arrived at our headache clinic with a 10-day history of headache and weight loss. Brain MRI revealed normal findings. Blood tests revealed thyrotoxicosis. A test for thyroid-related antibodies was negative. Thus, the patient was diagnosed with painless thyroiditis. The patient's headache resolved as his thyroid hormone levels decreased. To the best of our knowledge, this is the first reported case of headache exaggerated by painless thyrotoxicosis.
Keywords: thyrotoxicosis, painless thyroiditis, migraine
Introduction
It is well known that hormones such as estrogen and progesterone have effects on headache (1). In contrast, the potential effects of thyroid hormones on headache remain controversial. It is reported that 30% of hypothyroid patients have headache attributed to hypothyroidism (2). Although headache attributed to hypothyroidism is coded in The International Classification of Headache Disorders, 3rd edition (ICHD-3), an association with thyrotoxicosis (hyperthyroidism) is mentioned only in the appendix (2). This is because reports on relevant cases have been too scarce to establish a causal relationship between headache and thyrotoxicosis.
At our headache clinic, we encountered a patient with a unique presentation of migraine with aura. Specifically, his headache worsened in conjunction with painless thyroiditis, which is one subtype of thyrotoxicosis. Thyrotoxicosis is defined as a state of thyroid hormone excess and can be caused by Graves' disease [thyroid-stimulating hormone receptor antibody (TRAb) or thyroid-stimulating antibody (TSAb) positivity], subacute thyroiditis (accompanied by neck pain and fever after viral infection), and painless thyroiditis. It is generally recognized that painless thyroiditis is a transient hyperthyroidism accounting for approximately 0.5-5% of thyrotoxicosis cases (3). There are previous reports of headaches caused by Graves' disease (4-6), but to the best of our knowledge, there is no detailed case report on the occurrence of headache with painless thyrotoxicosis.
Case Report
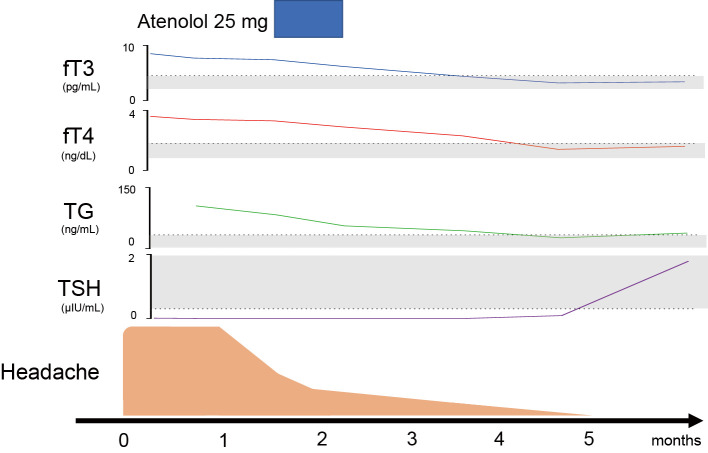
An 18-year-old man presented with a 10-day history of daily headache, which worsened in the morning, and strong stabbing pain in his left parietal area two or three times a day. The pain was accompanied by photophobia, phonophobia, and sometimes nausea, but no autonomic symptoms. Since 13 years of age, the patient had experienced non-throbbing headaches, lasting for 2-3 hours, once or twice a month. He had also experienced scintillation, consistent with migraine aura before the headaches. He had no history of medication overuse. He had experienced 13 kg of weight loss in the past 2 months. He had a family history of migraine with aura. His vital signs, including heart rate (80 bpm), were normal. Other than brisk patellar reflex, neurological examinations were grossly normal, including tremor. His cranial MRI/A findings were normal. His blood test results, including his C-reactive protein and D-dimer levels were grossly normal, but revealed thyrotoxicosis [free triiodothyronine (T3), 8.5 pg/mL (reference range, 2-4.5 pg/mL); free thyroxine (T4), 3.6 ng/dL (reference range, 0.7-1.8 ng/dL)], decreased thyroid-stimulating hormone [TSH, 0.01 μIU/mL (reference range, 0.3-4.5 μIU/mL)] and elevated thyroglobulin [TG, 105 ng/mL (reference range, 5-30 ng/mL)]. Tests for TRAb, TSAb, TGAb, and thyroid peroxidase antibody (TPOAb) were all negative, and thyroid ultrasonography revealed normal findings. He was diagnosed with painless thyroiditis. His headache started to show some improvement spontaneously one month after the start of symptoms, prior to the administration of medication for thyroiditis. Specifically, approximately 1.5 months after the onset of symptoms (upon presentation to the clinic), we initiated treatment with 25-mg atenolol for 3 weeks for palpitation due to painless thyroiditis, which improved after treatment. His free T3, free T4, and TG levels gradually decreased, and his TSH level gradually increased to the normal range at 5 months after the onset of headache (Figure). There were no adverse events. He was followed up for several years, but this was the only episode of daily headache attacks. His migraine frequency was not significantly affected by the development of painless thyroiditis.
Figure.
The time course of headache and the thyroid function. The light gray shadow indicates the normal range for each hormone. Headaches started to improve at approximately 1 month after the onset of symptoms. Painless thyroiditis was diagnosed at 1.5 months after the onset, and atenolol was used for 3 weeks. The thyroid function improved and reached the normal range at 5 months after the onset of symptoms. fT3: free triiodothyronine, fT4: free thyroxine, TG: thyroglobulin, TSH: thyroid-stimulating hormone
Discussion
To the best of our knowledge, this is the first detailed report on the occurrence of headache with painless thyrotoxicosis. Reports on the association between headache and thyrotoxicosis are scarce. Larner et al., who studied thyroid hormone levels of 13 headache patients, reported that 2 (15%) patients had hypothyroidism but none had thyrotoxicosis (7). We also reviewed eleven cases of thyrotoxicosis in which the chief complaint was headache based on previous case reports (Table) (4-6,8-10). The patients were predominantly female (82%). Of the seven cases for which information on age was available, the mean age was 38 years (range, 15-58 years). The average free T4 level of these patients was 7.5 ng/dL (range, 4.6-10.4 ng/dL). In contrast, our patient was male, young, and had a lower free T4 in comparison to most reported cases. Furthermore, the majority of previously profiled patients had tremor and tachycardia, but our patient did not present either of these symptoms. Regarding the tendon reflex, previous studies have reported both hyperreflexia and hyporeflexia. Our case did not involve thyrotoxicosis, which was typically reported in previous studies; however, weight loss was the key to reaching the diagnosis. Similarly to our case, headache in the context of thyrotoxicosis consistently improved after the successful treatment of thyrotoxicosis, although surgery was necessary in one patient (6).
Table.
Review of Previous Case Reports on Headache with Thyrotoxicosis.
| Reference number | Age | Sex | PHx of migraine | FHx of migraine | Nausea/ Vommiting |
Heart rate | Papilledema | Tremor | Tendon reflex |
BW loss | fT3 | fT4 | TSH | TRAb | TPOAb | Diagnosis | Treatment | Improvement |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 4 | N/A | F | + | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Graves’ disease | N/A | N/A |
| N/A | F | + | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | ||
| N/A | F | + | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | ||
| N/A | F | + | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Overtreatment of hypothyroidism | N/A | N/A | |
| 5 | 32 | F | - | - | + | 114 bpm | + | + | ↑ | - | >20 | 9.4 | <0.03 | + | - | Graves’ disease | propranolol 120 mg, carbimazole 45 mg | + |
| 6 | 34 | F | +(MO) | - | + | 120 bpm | N/A | + | ↑ | N/A | N/A | 10.3 | <0.05 | + | N/A | Graves’ disease | propranolol 40 mg, carbimazole 60 mg | + |
| 51 | F | - | - | + | N/A | - | + | → | N/A | N/A | 10.4 | <0.05 | + | N/A | Graves’ disease | carbimazole | + | |
| 20 | F | - | - | + | 120 bpm | - | + | → | + | N/A | 4.7 | <0.05 | + | N/A | Graves’ disease | carbimazole→surgery | +(after surgery) | |
| 8 | 58 | F | - | N/A | + | 134 bpm | N/A | N/A | N/A | + | N/A | 5.3 | <0.05 | N/A | N/A | Small multinodular goitre | carbimazole, propranolol | + |
| 9 | 58 | M | N/A | N/A | + | 116 bpm | + | N/A | ↓ | N/A | 7.7 | 4.6 | 0.07 | N/A | - | Thyroid nodule | propylthiouracil 300 mg, propranolol 40 mg, dexamethasone 24 mg | + |
| 10 | 15 | M | - | - | N/A | 105 bpm | N/A | N/A | N/A | N/A | >33 | >7.8 | 0.02 | N/A | N/A | N/A | methimazole | + |
| Current Case | 18 | M | +(MA) | + | + | 70 bpm | - | - | ↑ | + | 8.5 | 3.6 | 0.01 | - | - | Painless thyroditis | atenolol 25mg | + |
Units for fT3, fT4, and TSH are pg/mL, ng/dL, and μIU/mL, respectively. N/A: not available, F: female, M: male, PHx: past history, MA: migraine with aura, MO: migraine without aura, FHx: family history, bpm: beats per minute, BW: body weight, ↑: hyperreflexia, →: normal, ↓: hyporeflexia
In our case, the symptoms worsened in a close temporal relationship with painless thyroiditis. Because there were no abnormalities in thyroid-related antibodies, our case suggests that the cause of headache was the thyroid hormone itself and not the antibodies. Additionally, considering that thyrotoxicosis is transient in painless thyroiditis - in contrast to Graves' disease - a short time course may be enough to cause headaches. Recently, Maggioni et al. reported a case in which headache was induced by replacement treatment with levothyroxine (11). A 65-year-old woman with Hashimoto's thyroiditis presented with a sudden increase in the frequency of migraine with aura attacks when levothyroxine (i.e., thyroid hormone) was taken in gel caps. This method of administration is thought to allow faster intestinal absorption of the hormone in comparison to tablets. The migraine attacks stopped on the day that she stopped taking gel caps (11). As in our case, this report supports that headache is caused by the thyroid hormone itself and not by the antibody.
Not much is known regarding the pathophysiological mechanism through which thyrotoxicosis causes headache. Thyrotoxicosis can cause venous thrombosis, but our patient did not present that clinical finding. Yaka et al. reported on a patient who presented with headache along with thyrotoxicosis and a concurrent increase in intracranial pressure (9). Although we did not perform lumbar puncture, our patient did not have papilledema, which suggested that there was no significant increase in intracranial pressure. Borkum stated the possibility that thyroid hormone may cause enhanced oxidative stress in the brain, modulate cortex excitability by reducing the synthesis of gamma-aminobutyric acid, and promote collagen-induced platelet aggravation (12). Another possible mechanism may be through vasospasms. For example, there is a report on painless thyroiditis causing acute myocardial infarction, possibly through coronary vasospasm (3). Further, thyrotoxicosis is known to coexist with moyamoya disease. Oversensitivity to sympathetic tone in severe thyrotoxicosis may result in vasoconstriction (13). These mechanisms are hypothetical, and future studies are necessary to draw further conclusions about the pathophysiological mechanism through which thyrotoxicosis causes headache.
In our case, headache improved before the thyroid hormone levels reached the normal range. Hence, a decline in the thyroid hormone level from the peak value may be sufficient for the relief of headache. One could argue that beta blockers had an effect on our patient's headache. However, considering that the symptoms improved before the initiation of treatment (Figure), it is likely that the headache was worsened by thyroid hormone alone. Lastly, we note that our patient had a past history of migraine with aura, and we could not conclude whether the thyrotoxicosis caused headaches or exacerbated the patient's migraine. Further research and reports are necessary to move the association of headache with thyrotoxicosis (hyperthyroidism) out of the appendix and into the future ICHD guidelines.
In conclusion, we believe that this is the first detailed case report of a patient with headache whose diagnosis turned out to be painless thyrotoxicosis. Because painless thyroiditis, along with other types of thyrotoxicosis, such as Graves' disease (4-6), can worsen headache, it is advisable to measure the thyroid function in patients with headache who present with weight loss or tremor, or those showing changes in the severity or frequency of their usual headache symptoms. An improvement in thyrotoxicosis may lead to suppression of a patient's headache, such as occurred in our case.
The authors state that they have no Conflict of Interest (COI).
Financial Support
The publication of this article was supported by JSPS KAKENHI (grant number 19K16989 to TT).
References
- 1.Martin VT, Behbehani M. Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis - part 2. Headache 46: 365-386, 2006. [DOI] [PubMed] [Google Scholar]
- 2.Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 38: 1-211, 2018. [DOI] [PubMed] [Google Scholar]
- 3.Zheng W, Zhang YJ, Li SY, Liu LL, Sun J. Painless thyroiditis-induced acute myocardial infarction with normal coronary arteries. Am J Emerg Med 33: 983.e5-983.e10, 2015. [DOI] [PubMed] [Google Scholar]
- 4.Thomas DJ, Robinson S, Robinson A, Johnston DG. Migraine threshold is altered in hyperthyroidism. J Neurol Neurosurg Psychiatry 61: 222, 1996. [Google Scholar]
- 5.Herwig U, Sturzenegger M. Hyperthyroidism mimicking increased intracranial pressure. Headache 39: 228-230, 1999. [DOI] [PubMed] [Google Scholar]
- 6.Stone J, Foulkes A, Adamson K, Stevenson L, Al-Shahi Salman R. Thyrotoxicosis presenting with headache. Cephalalgia 27: 561-562, 2007. [DOI] [PubMed] [Google Scholar]
- 7.Larner AJ. Thyroid dysfunction and headache. J Headache Pain 7: 51-52, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ashawesh K, Abdulqawi R, Ahmad S. Hyperthyroidism presenting with persistent vomiting, headache and deranged liver function tests. Eur J Int Med 19: 72, 2008. [DOI] [PubMed] [Google Scholar]
- 9.Yaka E, Cakmur R. Increased intracranial pressure due to hyperthyroidism. Cephalalgia 30: 878-880, 2010. [DOI] [PubMed] [Google Scholar]
- 10.Lai P, Yuan JL, Xue JH, Qiu YQ. Hyperthyroidism with dome-and-dart T wave: A case report: A care-compliant article. Medicine (Baltimore) 96: e6060, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maggioni F, Maggioni G, Mainardi F. Migraine, triggers, and oxidative stress: Be Careful of the pharmacological anamnesis! Headache 56: 782-783, 2016. [DOI] [PubMed] [Google Scholar]
- 12.Borkum JM. Migraine triggers, oxidative stress, and the thyroid. Headache 56: 784-785, 2016. [DOI] [PubMed] [Google Scholar]
- 13.Shen AL, Ryu SJ, Lin SK. Concurrent moyamoya disease and Graves' thyrotoxicosis: case report and literature review. Acta Neurol Taiwan 15: 114-119, 2006. [PubMed] [Google Scholar]