Abstract
Objective:
Black children and children from low-income communities are disproportionately affected by asthma, attributed partly to pollution exposure. Air purifiers reduce indoor air pollution and improve asthma symptoms in children. In order to implement air purifier interventions, an understanding of patterns of use and potential barriers is necessary.
Methods:
In a home intervention study, 127 children with asthma living in Baltimore were randomized to receive two active or two placebo air purifiers. The 16-week study period included: baseline clinic visit, home visit for air purifier installation (active or placebo) with instruction to use the high or turbo settings, and electronic adherence monitoring of air purifiers. Determinants of adherence were identified using linear regression models.
Results:
Air purifiers were used 80% of the time, and participants demonstrated adherence to high or turbo settings for 60% of the time. In an adjusted model, season was the major determinant of air purifier adherence, with 21% lower use in the winter (p=0.025) attributed to the cold draft generated by the machine.
Conclusion:
In a clinical trial with electronic adherence monitoring, air purifier use was high and participants were adherent to use of high or turbo settings the majority of the time. Addressing practical barriers to consistent use, such as draft during the winter, in addition to financial barriers may improve air purifier adherence among children with asthma living in low-income, urban households.
Keywords: Air purifier, HEPA filter, Environmental control practice, Adherence, Pediatric Asthma, Indoor Air Pollution
Introduction
Asthma is one of the most common chronic diseases of childhood, with a prevalence of 7.5% among US children in 2018. The burden of asthma is disproportionately distributed, with a prevalence as high as 14.3% among Black children, nearly double the prevalence among Caucasian and Hispanic children 1. Furthermore, Black children with asthma living in poor, urban areas carry a disproportionate burden of the disease, with a higher risk for disease associated morbidity 2.
Particulate matter (PM) is a toxic air pollutant found both indoors and outdoors, and fine particulate pollution (PM2.5) has been linked to increased asthma symptoms and reduction in lung function among children with asthma 3,4. Children spend greater than 90% of their time indoors, which emphasizes the importance of improving indoor air quality 5. Indoor PM is increased by common household activities including sweeping, gas stove cooking, frying foods, as well as smoking 6. Indoor PM levels are high among low income households in Baltimore City, with the median PM2.5 levels nearly triple that of the World Health Organization recommended levels, and associated with more severe asthma symptoms and more frequent use of rescue inhalers 7,8. Such differential exposure to pollution has been identified as a contributor to asthma health disparities 9,10.
Measures to reduce indoor air pollution include environmental control practices such as household smoking bans, use of electric heaters in lieu of gas heaters, and use of air purifiers (HEPA filters). Specifically, HEPA filters can reduce concentrations of indoor PM and reduce asthma morbidity 11–14. Prior work investigating the efficacy of air purifiers among children with asthma living in Baltimore City found that the use of home air purifiers reduced indoor PM2.5 by about 50%, and was associated with significantly more symptom free days 13. These findings highlight the health benefit of air purifiers in asthma treatment.
In order to implement air purifiers in asthma treatment, an understanding of patterns of use and predictors of adherence is needed. While there has been a substantial body of work investigating adherence to asthma medications 15,16, there is a gap in the understanding of adherence to environmental interventions. To study the patterns of air purifier use and to measure adherence, it is important to recognize that air purifiers can be used intermittently or continuously, and can be used on different air flow settings.
We hypothesized that characteristics of the individual, the caretaker, the disease (asthma control and severity), and the home environment would be associated with adherence to air purifier use. This investigation is nested within an air purifier intervention study that utilized electronic adherence monitors, and therefore provided an opportunity to evaluate adherence to air purifier use and identify the determinants of air purifier use among a high risk population of predominantly Black children in Baltimore City.
Methods
Study Design
This analysis includes a subset of participants enrolled in AIRWEIGHS, a home intervention study of children with asthma. Enrollment started in September 2018, and all participants who had completed the second home visit by January 2020 were included. The Johns Hopkins Medical Institutional Review Board approved the study, and all participants provided written informed consent before beginning the study.
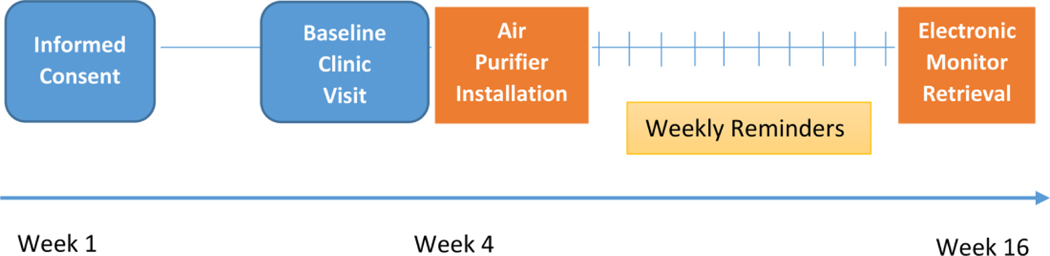
Over the 16-week study period, there was a baseline clinic visit, randomization to the air purifier intervention, a home visit for installation of air purifiers (active or placebo), and electronic adherence monitoring (Figure 1). During the clinic visit, the participant caretakers provided demographic data and completed questionnaires regarding the participant’s asthma symptoms, asthma control, and asthma severity. Participants were provided compensation for their time spent in home visits and clinic visits. Participants were randomized to receive either two active air purifiers containing HEPA filters or two placebos. At the end of the study all participants received two active air purifiers containing HEPA filters.
Figure 1.
AIRWEIGHS Study Design. Timeline showing sequence of events.
Participants
The study population included 127 children with asthma living in Baltimore City, a subgroup of the AIRWEIGHS study. Participants were recruited from prior asthma studies, the emergency department, and pediatric pulmonary clinics. Inclusion criteria were: (i) age 8–17 years, (ii) symptomatic asthma, (iii) non-smoker, (iv) spending ≥ 4 nights/week at home, (v) no plans to move during the study. Exclusion criteria were: (i) significant pulmonary or cardiac disease, (ii) home not appropriate candidate due to disrepair, (iii) enrolled in an environmental asthma trial in the previous 12 months, (iv) pregnancy.
Randomization to Air Purifier Use
Two portable air purifiers (Rabbit Air™ Minus A1 Model 700 or 780) were provided to participants (paid for by the study). One purifier (Model 780) was placed in the participant’s bedroom. The second purifier (Model 700) was placed in another room commonly utilized by the participant (typically the common room/family room). Those in the control group received identical placebo air purifiers with internal air filters removed.
Measurement of Air Purifier Adherence
All purifiers had electronic adherence monitors (HOBO model H06-004-02), continuously logging amperage of use. Air purifier use was reported as the percentage of total time (over 12-week time period) that the air purifier was turned on. All purifiers (including placebos) had five settings for filtration: turbo, high, medium, low and silent. Caretakers were instructed to leave the air purifiers on either the high or turbo setting for 12 weeks. These settings were selected for their enhanced air filtration capacity. Air purifier adherence was defined as the percentage of the observation period (12 weeks) that the air purifier was on the high or turbo setting. Air purifier use was defined as the percentage of the observation period (12 weeks) that the air purifier was on. An incentive of $50 was offered as a bonus for those who used the air purifiers >70% of the time. Caretakers received weekly phone calls for 10 weeks after air purifier installation to reinforce adherence to air purifier use. During these phone calls they were asked to identify any barriers to use of the high or turbo settings.
Participant Characterization
Participant caretakers provided demographic data including participant age and race, caretaker education, income and employment, and participant insurance type. Participant caretakers filled out questionnaires regarding asthma symptoms, severity and control. Asthma severity was determined based on the National Asthma Education and Prevention Program (NAEPP) guidelines for classification, which included number of symptomatic days and nights, albuterol use, and FEV1.17 Asthma control was evaluated using the Pediatric/Adolescent Asthma Therapy Assessment Questionnaire (ATAQ)18. Participant caretakers also provided information about the home environment including number of individuals in the home, and presence of smokers in the home. Season was captured based on the date of installation of air purifiers in the home.
Statistical Analysis
Summary statistics (means, medians) were generated for baseline demographic characteristics, air purifier use, and air purifier adherence to the high or turbo settings. Paired t-tests were used to compare air purifier adherence (and total use) between the two air purifiers in the home.
Outcome measures included air purifier adherence and air purifier use. Univariable linear regression models of air purifier adherence and use were fit for the following participant and caretaker characteristics: (i) age (ii) gender (iii) body mass index (BMI) (iv) race (v) education (vi) employment (vii) income (viii) insurance. Caretaker characteristics (education, income and employment) were evaluated for collinearity using variance inflation factors. Univariable linear regression models of air purifier adherence and use were fit for responses to the ATAQ and NAEPP asthma severity. Univariable regression models of air purifier adherence and use were fit for the following home and environmental characteristics: (i) presence of smokers in the home (ii) home occupancy (iii) season of air purifier installation.
Multivariable models were constructed to account for possible confounders and for differences between the treatment groups. Variables with p-values < 0.2 in univariable linear regression models of air purifier adherence were selected for inclusion in the multivariable models. Analyses were performed with Stata statistical software, version 15.0 (Stata Corp, College Station, Texas). Statistical significance was defined as p < 0.05.
Results
Participants were 8 to 17 years old, predominantly Black (86%) and from households of low socioeconomic status (Table1). About 60% of participants had moderate or severe asthma, per NAEPP guidelines 19.
Table 1.
Demographic characteristics of 127 participants from the AIRWEIGHS study.
| Characteristic | Values |
|---|---|
| Age [years; mean (range)] | 11 (8–17) |
| Race (%) Black Caucasian Other |
86 9 6 |
| Sex (% male) | 60 |
| BMI Category (%) | |
| Underweight | 2 |
| Normal | 39 |
| Overweight | 20 |
| Obese | 39 |
| Caregiver education level (%) 8th Grade – High School High School Grad Some College College/Grad School |
19 35 26 20 |
| Caregiver Income (%) < $20, 000 $20,000 - $39,999 > $40,000 Unknown |
39 31 20 11 |
| Caregiver Employment (%) Working at Paying Job Retired/Disabled Laid Off/Unemployed Full Time Home Maker Other/ Refused to Answer |
49 20 10 17 5 |
| Health Insurance (%) Private Public Don’t Know |
14 84 2 |
| NAEPP Asthma Severity (%) Intermittent Mild Persistent Moderate Persistent Severe Persistent |
8 31 43 17 |
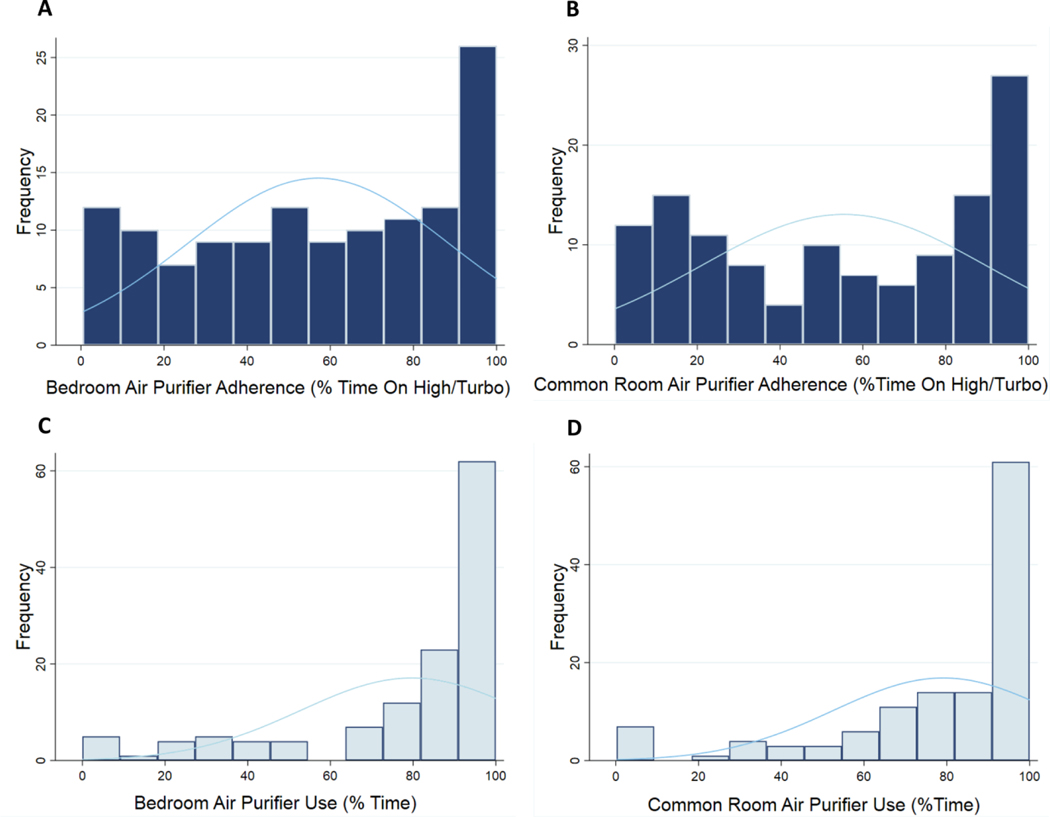
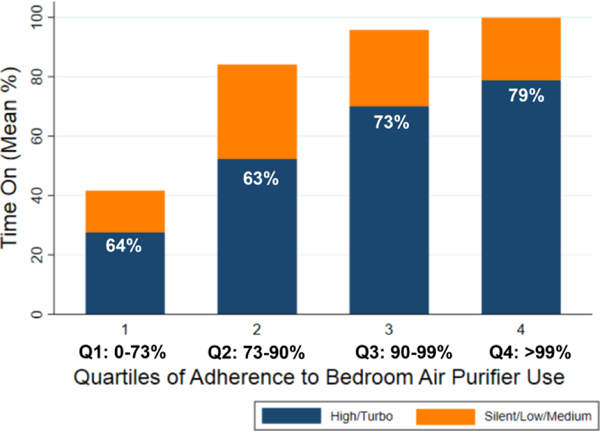
Each participant had one air purifier in the bedroom and one in a common room. Average air purifier use did not vary by location: bedroom use 79.6% of the time (over 12-week interval), common room use 79.1% of the time (paired t-test, p=0.761) (Figure 2). Average air purifier adherence, defined as the percentage of time the air purifier was on the high or turbo setting, also did not vary by location: bedroom adherence: 57.0% of the time, common room: 55.4% of the time (paired t-test, p= 0.523). Given the similarity in average use and average adherence between the bedroom and the common room, the remainder of the analyses were performed for the participant’s bedroom air purifier, since that children typically spent the majority of their time indoors in the bedroom 5. There was no difference in air purifier adherence or use between the treatment groups (Table 2). Almost 70% of the participants used the air purifier greater than 80% of the time. Among those participants with higher air purifier use, there was a greater proportion of total time on that was spent on the high or turbo settings. Participants were stratified into quartiles based on air purifier use, and among those in the highest quartile, average use of the high or turbo setting was 79% of the total time the air purifier was on. This was significantly greater than those in the lowest quartile, who used the high or turbo setting only 64% of the total time that the air purifier was on (95% confidence interval 0.9 to 29%, p= 0.037) (Figure 3).
Figure 2.
Histogram of air purifier use and adherence by location. A. Bedroom air purifier adherence B. Common room air purifier adherence. C. Bedroom air purifier use. D. Common room air purifier use. (Note scales differ.)
Table 2.
Univariable linear regression analyses of bedroom air purifier use for 127 participants from the AIRWEIGHS study.
| High/Turbo Air Purifier Adherence | Total Air Purifier Use | |||
|---|---|---|---|---|
| Variable | β [95% CI] | p-value | β [95% CI] | p-value |
| Participant and Caretaker Characteristics | ||||
| Randomization Group | −1.58 [−12.71, 9.55] | 0.779 | −4.36 [−13.83, 5.10] | 0.363 |
| Age | 0.20 [−2.01, 2.42] | 0.856 | 0.32 [−1.56, 2.21] | 0.735 |
| Race 0 = Caucasian/Other 1 = Black |
−6.02 [−21.94, 9.90] | 0.455 | −12.96 [−26.38, 0.46] |
0.058 |
| Gender | 0.79 [−10.56, 12.14] | 0.890 | 0.77 [−8.92, 10.45] | 0.875 |
| BMI | −0.02 [−0.23, 0.18] | 0.834 | −0.11 [−0.28, 0.07] | 0.220 |
| Caretaker Education 0 = High School or less 1 = Beyond High School |
−1.32 [−12.47, 9.84] | 0.816 | 8.87 [−0.52, 18.26] | 0.064 |
| Caretaker Employment 0 = Home-maker/ Retired/Unemployed 1 = Working at paying job |
−2.76 [−13.88, 8.37] | 0.625 | −0.59 [−10.09, 8.90] | 0.902 |
| Income 0 = <$40,000 1 = >/= $40,000 |
10.06 [−4.17, 24.29] | 0.164 | 15.79 [3.63, 27.96] | 0.011 |
| Insurance 0 = Private 1 = Public |
−10.88 [−26.8, 5.03] | 0.178 | −14.18 [−27.68, 0.67] | 0.040 |
| Measures of Asthma Severity and Control | ||||
| NAEPP 0 = Intermittent/Mild 1 = Moderate/Severe |
−2.33 [−16.74, 12.67] | 0.785 | −2.75 [−12.46, 6.95] | 0.576 |
| ATAQ Score | −2.80 [−5.52, −0.08] | 0.044 | −1.45 [−3.80, 0.90] | 0.223 |
| Environmental Characteristics | ||||
| Home Occupancy 0 = 0–4 1 = ≥ 5 |
−9.79 [−21.24, 1.66] | 0.093 | −4.76 [−14.60, 5.08] | 0.340 |
| Smoking in the Home 0 = No 1 = Yes |
1.66 [−11.43, 14.76] | 0.802 | −6.07 [−17.19, 5.06] | 0.283 |
| Winter season 0 = Spring/Summer/Fall 1 = Winter |
−13.53 [−29.69, 2.64] | 0.110 | −10.49 [−24.31, 3.32] |
0.135 |
| Season | 0.355 | 0.463 | ||
| Spring vs. winter | 17.06 [−1.89, 36.00] | 0.077 | 12.94 [−3.26, 29.15] | 0.116 |
| Summer vs. winter | 12.95 [−5.05, 30.95] | 0.157 | 9.22 [−6.18, 4.62] | 0.238 |
| Fall vs. winter | 11.42 [−6.72, 29.56] | 0.215 | 9.95 [−5.57, 25.47] | 0.207 |
Figure 3.
Adherence to Air Purifier Use. Air purifier use, defined as percent of time the air purifier was on, is shown by quartiles. Each stacked bar represents average time the air purifier was on within each quartile, and values listed within each bar represent average proportion of time on high or turbo setting within each quartile.
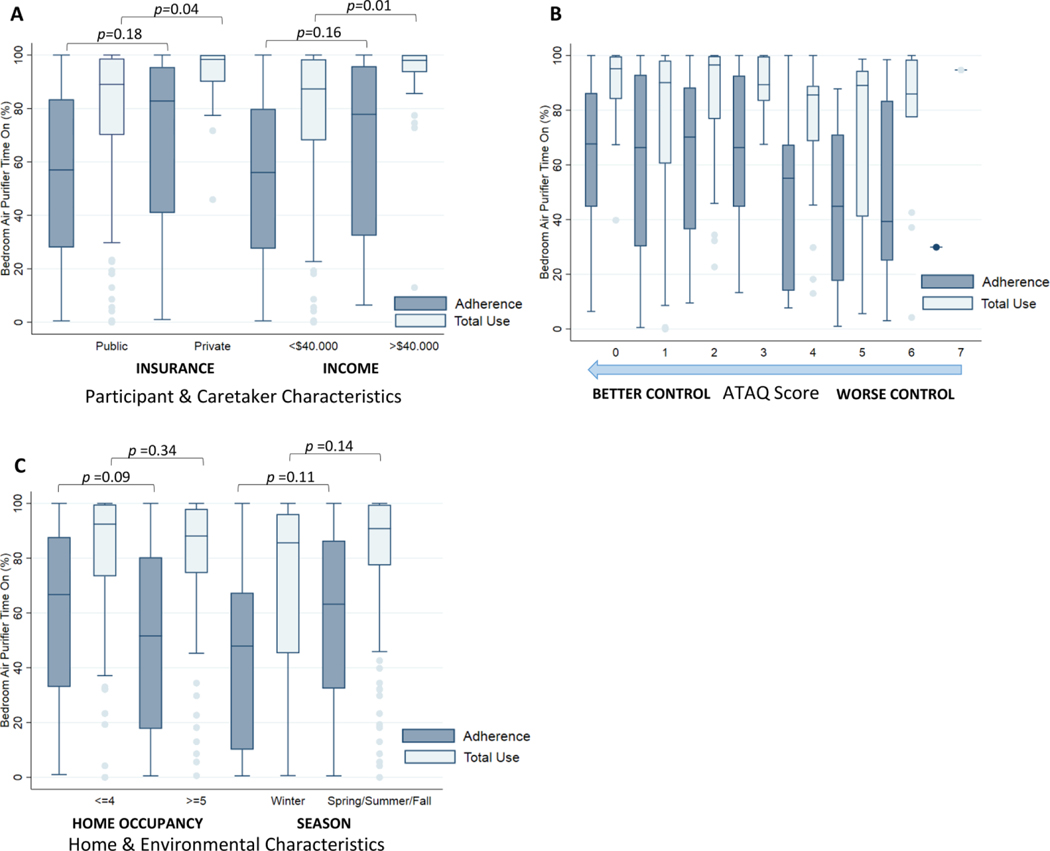
Impact of participant and caretaker characteristics on air purifier adherence and use
Insurance type and caretaker income tended to be associated with air purifier adherence. Average adherence of participants with public insurance was 56% compared to 66% among those with private insurance, and for participants with household income less than $40,000 was 54% compared to 64% among those with income greater than $40,000 (p<0.2 for both) (Table 2). Participants with public insurance used the air purifiers 11% less than those with private insurance (95% confidence interval 51.7 to 28%, p= 0.04). Participants with caretakers with lower incomes (cutoff $40,000 per year) used the air purifiers 16% less than those higher incomes (95% confidence interval 4 to 28%, p= 0.011). (Figure 4A). There was no association with other individual and caretaker characteristics (age, gender, BMI, race, education or employment) with air purifier adherence or use.
Figure 4.
Difference in air purifier adherence (high or turbo use) and total use by (A) insurance type and income (B) asthma control (C) season and home occupancy.
Impact of asthma control and severity on air purifier adherence and use
Each point increase in baseline ATAQ score (indicating less controlled asthma) was associated with a 3% decrease in air purifier adherence to the high or turbo settings (95% confidence interval 0.1 to 6%, p=0.044) (Table 2). Participants with perception of well controlled asthma (ATAQ score 0) used the air purifiers 16% more than those with poorly controlled asthma (ATAQ score 4–7) (95% confidence interval 2 to 29%, p=0.025). (Figure 4B). There was no association between the NAEPP classification of asthma severity and air purifier adherence or use.
Impact of home and the environment on air purifier adherence and use
Home occupancy and season of air purifier installation tended to be associated with air purifier adherence to the high or turbo setting, with relationships approaching statistical significance (Table 2). Participants living in a home with occupancy greater than 4 individuals had a 10% lower average adherence than those with home occupancy less than or equal to 4 individuals (p-value=0.093). Participants who had air purifiers placed in the home during the winter had an average adherence 14% lower than those with purifiers installed in the spring, summer, and fall (p-value= 0.110), and average use was 10% lower than those with purifier installed in the spring, summer, and fall (pvalue=0.135). (Figure 4C).
Barriers to Adherence
On average, about 73 participants responded to phone calls each week, capturing 97% of our participants at least once over the course of 10 weeks. There was no significant relationship between air purifier adherence or use, and the number of phone calls that were answered. Over 20% (27 participants) reported a barrier to use of the high or turbo setting. Among these participants, one-third reported noise as a barrier, one-third reported cold draft, and one-third reported other causes. About 30% (35 participants) reported trouble with the air purifier, the majority (26 participants) of whom reported the purifier reverting to auto settings (independently cycling through air flow settings based on PM concentrations estimated by an internal sensor).
Multivariable models of air purifier adherence
The final linear regression model of predictors of air purifier adherence was adjusted for randomization group, income, insurance type, ATAQ score, home occupancy, and season (Table 3). There was no collinearity among the covariates, evaluated by variance inflation factors. In this multivariable analysis model, winter season was found to be the main driver of adherence to air purifier use. There was a 21% decrease in adherence to air purifier use on the high or turbo settings in the winter, compared to the spring, summer, and the fall (95% confidence interval 3 to 39%, p=0.025).
Table 3.
Multivariable linear regression analyses of bedroom air purifier use for 127 participants from the AIRWEIGHS study.
| High/Turbo Air Purifier Adherence | Total Air Purifier Use | |||
|---|---|---|---|---|
| Variable | β [95% CI] | p-value | β [95% CI] | p-value |
| Participant and Caretaker Characteristics | ||||
| Randomization Group | −5.05 [−16.94, 6.85] | 0.402 | −5.91 [−16.28, 4.44] | 0.260 |
| Income | 5.97 [−12.01, 23.94] | 0.655 | 10.97 [−4.69, 26.63] | 0.168 |
| Insurance | −8.49 [−28.91, 11.94] | 0.412 | −9.17 [ −26.96, 8.62] | 0.309 |
| Measures of Asthma Severity and Control | ||||
| ATAQ Score | −0.43 [−3.53, 2.68] | 0.786 | −0.53 [−3.24, 2.17] | 0.696 |
| Environmental Characteristics | ||||
| Home Occupancy | −10.57 [−22.80, 1.66] | 0.090 | −5.51 [−16.16, 5.14] | 0.307 |
| Winter season | −20.66 [−38.70, −2.61] | 0.025 | −12.49 [−28.21, 3.23] | 0.118 |
coding of variables is the same as Table 2
Discussion
In an air purifier intervention trial of children with asthma living in low-income, urban households, we report that participants used the air purifiers 80% of the time, and were adherent to use of high or turbo settings as instructed 60% of the time. This is the first study to report air purifier adherence with an electronic sensor technology that provides objective evidence of air purifier use and detail regarding settings. Participants who utilized their air purifier did so as instructed (using high or turbo setting) 75% of the time. These findings in the setting of a controlled clinical trial suggest that children with asthma will use air purifiers the majority of the time, and typically as directed.
The 2020 update to the NHBLI guidelines for asthma treatment addresses indoor environmental interventions targeting allergens, and recommends a multi-modal approach to allergen mitigation in sensitized individuals. Air purifiers have often been studied in the context of multi-modal interventions, and have been shown to improve the indoor environment 12,20–23 and to impact asthma morbidity. Notably, there is variability between study findings: some studies demonstrate benefit of air purifier containing interventions on asthma morbidity12,22,24 and others do not 20,21. The allergen reduction systematic review generated for the 2020 NHBLI guidelines describes a lack of evidence regarding adherence to environmental interventions, and notes that this may contribute to the heterogeneity between study findings. The need to study adherence to environmental interventions, including HEPA air purifiers, is outlined as a future research opportunity in this recent update and these findings directly address this research gap.
In the present study, participants used the high or turbo setting 60% of the time, as instructed. This level of air purifier adherence is as high or higher compared to previous reports of medication adherence, considering that at least half of the studies with electronic measures of ICS adherence in childhood asthma report adherence rates less than 50%.25,26 Adherence to air purifier use is in many ways simpler than asthma medication adherence, without a need to remember the dose, the frequency, or refills. Once the purifier is turned on, and placed on the correct setting, no further action is required.
Similar to studies of medication adherence, we found that adherence to air purifier use can be multi-factorial. Our analysis showed that income, insurance status, asthma control, and home occupancy contribute to adherence, with the overall driver being season. Our multivariable model, which adjusted for the aforementioned variables, demonstrates that season is a significant predictor of air purifier adherence, with significantly lower use in the winter compared to other seasons. This is in contrast to medication adherence, where prior work has demonstrated a relative decrease in refills in the summer months, suggesting that seasonal exacerbations may affect medication adherence 27.
Interestingly, adherence to this environmental control practice seems to have a seasonal pattern that may be driven by a cold draft generated by the equipment. The noise associated with use of the high and turbo settings was an anticipated barrier to use; however reports of the cold draft were not only unexpected but also seemed to be quite impactful on adherence given the 20% decrease in adherence during the winter months. These findings suggest that participant feedback regarding inconveniences or drawbacks of air purifier use can help to successfully implement air purifier adherence. Similar to how counseling about a new medication involves a review of potential side effects, moving forward, anticipatory guidance about the secondary effects of cold draft and noise could allow for strategic placement of the purifier away from seating area or bed, or compensatory heating strategies with central or portable heating to overcome these barriers and encourage strong adherence.
This study demonstrated another notable difference between determinants of air purifier adherence and medication adherence based on previous reports 25,26. Studies of medication adherence in adolescents, using electronic medication monitors attached to ICS canisters, had demonstrated a decrease in adherence with increasing age 25,28. However, our study did not find an association between air purifier adherence and age. Perhaps this is because the air purifier intervention can be carried out by the supervising adult, and doesn’t require the engagement of an adolescent.
Patients with asthma coming from disadvantaged backgrounds have been shown to have poor medication adherence 29. Our results in univariable analysis also demonstrated trends of lower air purifier adherence among participants with low income and participants with public insurance. This trend was not supported by the multivariable model. It is likely that outside the setting of a clinical trial, this trend could be exaggerated. The particular air purifier model used for this study is no longer available for retail, but a similar model costs approximately $550, with other similar products ranging from $80-$800. The average cost of running each air purifier during this study was approximately $1.50/month. In the setting of a clinical trial, the individual was not responsible for the cost of the air purifier, and financial incentives for participation and use were provided. Similar to how insurance companies have established first tier coverage of asthma medications, coverage of air purifiers would overcome part of the financial barrier that many patients with low income may face. Implementation and sustainability of environmental interventions is challenging in real-world settings, particularly in low-income communities. In addition to third party payer coverage, community level programs, such as the IMPACT DC asthma clinic which provides resources to cover costs of environmental interventions for low-income patients in urban communites30, may provide a means to support implementation.
Prior studies of medication adherence have demonstrated that patients with better controlled asthma and those with less severe asthma were more likely to be adherent to medications 28,31. Similarly, we found in univariable analysis that those with more controlled asthma (lower ATAQ scores) were more adherent to air purifier use. This relationship between adherence and asthma control may be bidirectional. Those who have less controlled asthma may be more symptomatic due to poor self-management, which includes lack of adherence to asthma medications or other environmental control practices. This would suggest that perhaps the same behaviors that drive medication adherence may also drive air purifier adherence.
We recognize there are limitations to this study. Specifically, in the clinical trial setting, the responsibility of treatment initiation was not placed on the participant. The clinical trial included a placebo group but the resulted indicated there was no difference in adherence by treatment group. The air purifiers were provided and installed in the homes, and participants received weekly reminders and incentives. The number of phone calls answered by participants did not significantly change adherence, suggesting that weekly phone calls are not required to achieve these high levels of adherence. Adherence could be monitored at follow-up visits, and with current electronic health record (EHR) systems and the use of applications on cellular devices, it would be feasible to create a reminder system with monthly notifications for patients with air purifiers at home. Implementation may be limited by the size of a practice and the features of the EHR. We acknowledge there is a lack of generalizability due to the homogeneity of the participant population. This was a study of predominantly Black children with asthma living in low-income urban communities; however, notably this is a group that is at high risk for morbidity from asthma 9,10, and this study demonstrates that it is feasible to achieve high adherence to air purifier use even among this community. There may be a role for third party payers to offer partial coverage in order to mitigate the impact of the financial burden. The feedback from participants regarding barriers to adherence suggests there may be value in providing anticipatory guidance regarding the cold draft and the noise associated with air purifier use. In real world implementation, it may be necessary to provide additional reminders in the winter, with suggestions for air purifier placement to mitigate the cold draft.
Conclusion:
In summary, air purifiers have been shown to improve indoor air quality and asthma symptoms 11–13. In order to achieve maximal benefit, it is critical to understand adherence to this intervention. With the novel method of monitoring electronic current within air purifiers, this study provided a gold standard approach to assessing air purifier use and whether air purifiers were used as directed (adherence). These findings among a disadvantaged population demonstrate that adherence to an air purifier intervention can be comparable or better than medication adherence. Barriers that have been elucidated in the current study should be considered in efforts to deploy air purifiers in real world settings or in future studies evaluating broad implementation of air purifiers as an effort to reduce childhood asthma morbidity.
Acknowledgments
Funding: This work was supported by the National Institute of Environmental Health Sciences (NIEHS) under grant number P50ES018176 and the U.S. Environmental Protection Agency under grant number 83615201.
Footnotes
Disclosure of Interest: The authors report no conflict of interest.
Clinical Trials Registry Number: NCT02763917.
References
- 1.CDC. Most Recent National Asthma Data. https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm. Accessed October 12, 2019.
- 2.Keet CA, Matsui EC, McCormack MC, Peng RD. Urban residence, neighborhood poverty, race/ethnicity, and asthma morbidity among children on Medicaid. J Allergy Clin Immunol. 2017;140(3):822–827. doi: 10.1016/j.jaci.2017.01.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koenig JQ, Mar TF, Allen RW, et al. Pulmonary effects of indoor- and outdoor-generated particles in children with asthma. Environ Health Perspect. 2005;113(4):499–503. doi: 10.1289/ehp.7511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Delfino RJ, Quintana PJE, Floro J, et al. Association of FEV1in asthmatic children with personal and microenvironmental exposure to airborne particulate matter. Environ Health Perspect. 2004;112(8):932–941. doi: 10.1289/ehp.6815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klepeis NE, Nelson WC, Ott WR, et al. The National Human Activity Pattern Survey (NHAPS): A resource for assessing exposure to environmental pollutants. J Expo Anal Environ Epidemiol. 2001;11(3):231–252. doi: 10.1038/sj.jea.7500165 [DOI] [PubMed] [Google Scholar]
- 6.Breysse PN, Diette GB, Matsui EC, Butz AM, Hansel NN, McCormack MC. Indoor Air Pollution and Asthma in Children. Proc Am Thorac Soc. 2010;7(2):102–106. doi: 10.1513/pats.200908-083RM [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCormack MC, Breysse PN, Matsui EC, et al. In-home particle concentrations and childhood asthma morbidity. Environ Health Perspect. 2009;117(2):294–298. doi: 10.1289/ehp.11770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Breysse PN, Diette GB, Matsui EC, Butz AM, Hansel NN, McCormack MC. Indoor Air Pollution and Asthma in Children. Proc Am Thorac Soc. 2010;7(2):102–106. doi: 10.1513/pats.200908-083RM [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matsui EC, Hansel NN, McCormack MC, Rusher R, Breysse PN, Diette GB. Asthma in the Inner City and the Indoor Environment. Immunol Allergy Clin North Am. 2008. doi: 10.1016/j.iac.2008.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Lung Association. State of the Air.; 2019. [Google Scholar]
- 11.Reisman RE, Mauriello PM, Davis GB, Georgitis JW, DeMasi JM. A double-blind study of the effectiveness of a high-efficiency particulate air (HEPA) filter in the treatment of patients with perennial allergic rhinitis and asthma. J Allergy Clin Immunol. 1990;85(6):1050–1057. doi: 10.1016/0091-6749(90)90050-E [DOI] [PubMed] [Google Scholar]
- 12.Eggleston PA, Butz A, Rand C, et al. Home environmental intervention in inner-city asthma: A randomized controlled clinical trial. Ann Allergy, Asthma Immunol. 2005;95(6):518–524. doi: 10.1016/S1081-1206(10)61012-5 [DOI] [PubMed] [Google Scholar]
- 13.Butz AM, Matsui EC, Breysse P, et al. A randomized trial of air cleaners and a health coach to improve indoor air quality for inner-city children with asthma and secondhand smoke exposure. Arch Pediatr Adolesc Med. 2011. doi: 10.1001/archpediatrics.2011.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lanphear BP, Hornung RW, Khoury J, Yolton K, Lierl M, Kalkbrenner A. Effects of HEPA air cleaners on unscheduled asthma visits and asthma symptoms for children exposed to secondhand tobacco smoke. Pediatrics. 2011;127(1):93–101. doi: 10.1542/peds.2009-2312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gray WN, Netz M, McConville A, Fedele D, Wagoner ST, Schaefer MR. Medication adherence in pediatric asthma: A systematic review of the literature. Pediatr Pulmonol. 2018;53(5):668–684. doi: 10.1002/ppul.23966 [DOI] [PubMed] [Google Scholar]
- 16.Drotar D, Bonner MS. Influences on adherence to pediatric asthma treatment: A review of correlates and predictors. J Dev Behav Pediatr. 2009;30(6):574–582. doi: 10.1097/DBP.0b013e3181c3c3bb [DOI] [PubMed] [Google Scholar]
- 17.Highlights of the National Asthma Education and Prevention Program Expert Panel Report 3 : Guidelines for the Diagnosis and Management of Asthma Full Report 2007. Children. 2007. [Google Scholar]
- 18.Skinner EA, Diette GB, Algatt-Bergstrom PJ, et al. The asthma therapy assessment questionnaire (ATAQ) for children and adolescents. Dis Manag. 2004;7(4):305–313. doi: 10.1089/dis.2004.7.305 [DOI] [PubMed] [Google Scholar]
- 19.Diette GB, Sajjan S, Skinner EA, Weiss TW, Wu AW, Markson LE. Using the pediatric asthma therapy assessment questionnaire to measure asthma control and healthcare utilization in children. Patient. 2009;2(4):233–241. doi: 10.2165/11313820-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 20.Matsui EC, Perzanowski M, Peng RD, et al. Effect of an integrated pest management intervention on asthma symptoms among mouse-sensitized children and adolescents with asthma a randomized clinical trial. JAMA - J Am Med Assoc. 2017;317(10):1027–1036. doi: 10.1001/jama.2016.21048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DiMango E, Serebrisky D, Narula S, et al. Individualized Household Allergen Intervention Lowers Allergen Level But Not Asthma Medication Use: A Randomized Controlled Trial. J Allergy Clin Immunol Pract. 2016;4(4). doi: 10.1016/j.jaip.2016.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. Pediatrics. 2005;116(2):543. doi: 10.1542/peds.2005-0698Q [DOI] [PubMed] [Google Scholar]
- 23.Bernstein JA, Levin L, Crandall MS, Perez A, Lanphear B. A pilot study to investigate the effects of combined dehumidification and HEPA filtration on dew point and airborne mold spore counts in day care centers. Indoor Air. 2005;15(6):402–407. doi: 10.1111/j.1600-0668.2005.00379.x [DOI] [PubMed] [Google Scholar]
- 24.Takaro TK, Krieger J, Song L, Sharify D, Beaudet N. The Breathe-Easy home: The impact of asthma-friendly home construction on clinical outcomes and trigger exposure. Am J Public Health. 2011;101(1):55–62. doi: 10.2105/AJPH.2010.300008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaplan A, Price D. Treatment adherence in adolescents with asthma. J Asthma Allergy. 2020;13:39–49. doi: 10.2147/JAA.S233268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morton RW, Everard ML, Elphick HE. Adherence in childhood asthma: The elephant in the room. Arch Dis Child Educ Pract Ed. 2014;99(10):949–953. doi: 10.1136/archdischild-2014-306243 [DOI] [PubMed] [Google Scholar]
- 27.Turi KN, Gebretsadik T, Lee RL, et al. Seasonal patterns of Asthma medication fills among diverse populations of the United States. J Asthma. 2018. doi: 10.1080/02770903.2017.1362426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McQuaid EL, Kopel SJ, Klein RB, Fritz GK. Medication adherence in pediatric asthma: Reasoning, responsibility, and behavior. J Pediatr Psychol. 2003;28(5):323–333. doi: 10.1093/jpepsy/jsg022 [DOI] [PubMed] [Google Scholar]
- 29.Louisias M, Phipatanakul W. Managing Asthma in Low-Income, Underrepresented Minority, and Other Disadvantaged Pediatric Populations: Closing the Gap. Curr Allergy Asthma Rep. 2017;17(10). doi: 10.1007/s11882-017-0734-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Teach SJ, Crain EF, Quint DM, Hylan ML, Joseph JG. Improved Asthma Outcomes in a High-Morbidity Pediatric Population. Arch Pediatr Adolesc Med. 2006;160(5):535. doi: 10.1001/archpedi.160.5.535 [DOI] [PubMed] [Google Scholar]
- 31.Burgess S, Sly P, Devadason S. Adherence with preventive medication in childhood asthma. Pulm Med. 2011;2011. doi: 10.1155/2011/973849 [DOI] [PMC free article] [PubMed] [Google Scholar]