Abstract
Rates of survival with functional recovery for both in-hospital and out-of-hospital cardiac arrest are notably low. Extracorporeal cardiopulmonary resuscitation (ECPR) is emerging as a modality to improve prognosis by augmenting perfusion to vital end-organs by utilizing extracorporeal membrane oxygenation (ECMO) during conventional CPR and stabilizing the patient for interventions aimed at reversing the aetiology of the arrest. Implementing this emergent procedure requires a substantial investment in resources, and even the most successful ECPR programs may nonetheless burden healthcare systems, clinicians, patients, and their families with unsalvageable patients supported by extracorporeal devices. Non-randomized and observational studies have repeatedly shown an association between ECPR and improved survival, versus conventional CPR, for in-hospital cardiac arrest in select patient populations. Recently, randomized controlled trials suggest benefit for ECPR over standard resuscitation, as well as the feasibility of performing such trials, in out-of-hospital cardiac arrest within highly coordinated healthcare delivery systems. Application of these data to clinical practice should be done cautiously, with outcomes likely to vary by the setting and system within which ECPR is initiated. ECPR introduces important ethical challenges, including whether it should be considered an extension of CPR, at what point it becomes sustained organ replacement therapy, and how to approach patients unable to recover or be bridged to heart replacement therapy. The economic impact of ECPR varies by health system, and has the potential to outstrip resources if used indiscriminately. Ideally, studies should include economic evaluations to inform health care systems about the cost-benefits of this therapy.
Keywords: Cardiac arrest, Extracorporeal cardiopulmonary resuscitation, Extracorporeal membrane oxygenation, OHCA, IHCA
Take-home message
| Emerging data from recent randomized controlled trials offer the most rigorous evidence to date that extracorporeal cardiopulmonary resuscitation (ECPR) may improve survival with neurological and functional recovery in cardiac arrest when performed within highly coordinated healthcare delivery systems. It is important to consider not only the setting and system within which ECPR is employed, but also the ethical and economic implications that may accompany more widespread implementation of ECPR. |
Introduction
The incidence of unexpected cardiac arrest is high, with in-hospital (IHCA) and out-of-hospital cardiac arrests (OHCA) in the United States estimated at 200,000 and 350,000/year, respectively [1]. Survival to hospital discharge after these events is low (IHCA range 6–26% [1–4]; OHCA typically < 10% [1, 5–7]), particularly when resuscitative efforts are prolonged [7–10]. Outcomes are more dismal when restricted to survival with neurological or functional recovery [6–8, 11].
Attempts at improving cardiac arrest outcomes have increasingly included extracorporeal techniques to re-establish circulation [12–15]. The application of venoarterial extracorporeal membrane oxygenation (ECMO) during cardiac arrest is referred to as extracorporeal cardiopulmonary resuscitation (ECPR). Performed under considerable time pressure, ECPR requires a substantial investment of resources—both personnel and equipment—and considerable reorganization of pre-hospital, hospital, and intensive care protocols.
This review will evaluate the impact of ECPR on survival and, perhaps more importantly, neurological and functional recovery in adults suffering cardiac arrest, identify those most likely to benefit, explore the resources required, and address relevant ethical issues.
History and trends in ECPR use
The first published report of successful ECPR in adults was the description by Kennedy of 8 cardiac arrest patients from 1957 to 1965 [16]. Seven were successfully resuscitated, surviving hours to days, with one patient neurologically intact at hospital discharge. Kennedy described the need for readily available teams and equipment, perfusionists’ ability to establish assisted circulation within 30 min, and successful maintenance of portable, primed sterile circuits for > 1 month. Lastly, the author cautioned that extracorporeal techniques should supplement, not replace, conventional CPR.
ECPR has expanded significantly since then. Data from the Extracorporeal Life Support Organization (ELSO) Registry have demonstrated an increase in annual ECPR cases from < 100 in 2009 to > 1500 in 2019 [17]. This increase occurred in the setting of propensity-matched analyses suggesting a survival advantage, with recent randomized controlled trials (RCTs) now providing greater guidance (see below). The concurrent increase in ECMO use during the 2009 Influenza A(H1N1) pandemic also likely contributed to the rise in ECPR, owing to greater availability of ECMO teams and equipment, as well as increased interest in the use of ECMO in general.
Physiology and technical considerations
In venoarterial ECMO, blood is drained from a central vein, pumped through a membrane lung, and returned through an artery, providing both gas exchange and circulatory support [18]. ECPR specifically refers to initiating ECMO during cardiac arrest prior to return of spontaneous circulation (ROSC), setting it apart from venoarterial ECMO for post-cardiac arrest cardiogenic shock. ECPR must be initiated more quickly than any other form of ECMO, typically with incomplete knowledge of the patient’s suitability for extracorporeal support. Often the most challenging issue during evaluation for ECPR is determining the patient’s likelihood of neurological recovery.
ECPR is usually performed via femoral cannulation, resulting in retrograde aortic blood flow. Without left ventricular output, reinfused oxygenated blood should reach the coronary and cerebral vascular beds [19], outperforming conventional CPR (the duration of which is referred to as ‘low-flow time’) which is estimated to be < 25–30% of cardiac output [20, 21]. ECPR stabilizes the patient more effectively, providing time to identify and reverse the underlying aetiology of cardiac arrest.
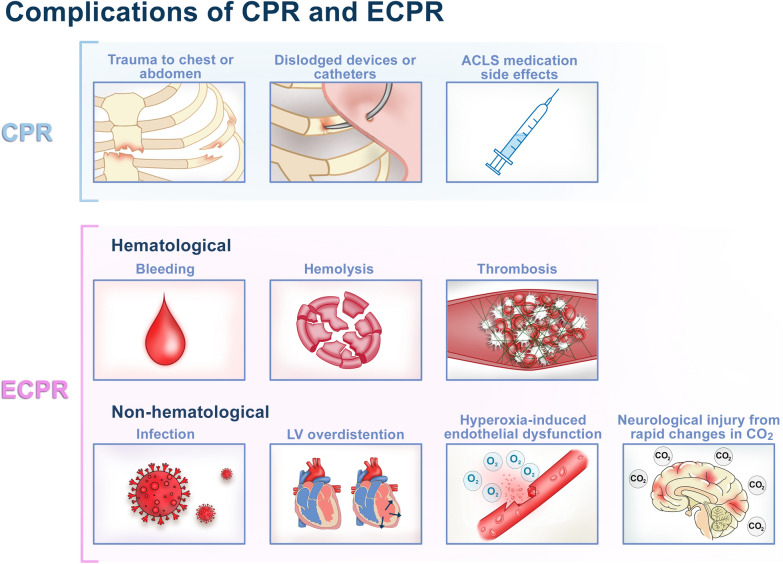
The arterial return cannula occupies most of the cross-sectional area of the femoral artery, posing a risk of distal limb ischemia, which may be mitigated by placing a distal reperfusion cannula [15, 22, 23]. High rates of successful cannulation with minimal vascular complications have been reported at certain experienced centers using ultrasound guidance for percutaneous vascular access combined with fluoroscopic verification of wire positioning [24, 25]. However, rates of vascular complications may still be substantial even at high-volume centers, and providers should anticipate and plan for these potentially serious adverse events [26], especially in the setting of ECPR given the emergent nature of the cannulation (Fig. 1). A recent single-center propensity-score matched analysis of venoarterial ECMO demonstrated that cannula site infections were significantly lower with a percutaneous compared with a surgical approach [27].
Fig. 1.
Complications associated with conventional CPR and ECPR. ACLS advanced cardiac life support, CO2 carbon dioxide, CPR cardiopulmonary resuscitation, ECPR extracorporeal cardiopulmonary resuscitation, LV left ventricle
Understanding outcomes in ECPR
Survival is a universally reported endpoint, but does not sufficiently characterize success of ECPR. Measures of functional status, such as the Cerebral Performance Category (CPC) score or Modified Rankin scale (mRS) are commonly used to assess early post-arrest outcomes. [28]. Beyond survival with functional or neurological recovery, it is important to understand long-term functional status and quality-of-life [29, 30]. The International Liaison Committee on Resuscitation (ILCOR) has recommended the use of both short-term functional assessments (e.g., mRS) and longer-term health-related quality-of-life tools as core outcome measures for cardiac arrest trials [31].
The potential benefit of ECPR over conventional CPR must be weighed against the potential for negative outcomes (including severe neurological and functional disability) [4] and the intensity of resources required. Given the incidence of unexpected cardiac arrest, even small increases in the rates of survival with neurological or functional recovery could justify the expanded use of ECPR because of the absolute numbers involved. However, ECPR should be considered complementary to initial high-quality conventional CPR. It is not clear whether the resources invested in ECPR would yield greater societal benefit if they were used elsewhere, for instance, to improve bystander CPR. This is especially the case given the relatively low rate of potentially appropriate ECPR candidates relative to the total number of arrests [23, 32, 33].
Not surprisingly, higher rates of bystander CPR have been associated with improved 30-day survival in OHCA [34]. Based on data of patients who survived to 30 days post-OHCA from a large Danish registry, 1-year rates of neurological injury, nursing home admission, and death were relatively low—with a high rate of returning to work—and significantly correlated with whether bystander CPR, including defibrillation, was performed [30, 35]. The combination of high-quality CPR and ECPR for those without ROSC within a reasonable timeframe has the potential to maximize short-term survival and, by extension, long-term neurological and functional outcomes.
Evidence for the use of ECPR
In-hospital cardiac arrest
There are no completed prospective RCTs of ECPR for in-hospital cardiac arrest. Single-center, retrospective observational studies have demonstrated that ECPR is feasible in-hospital (Table 1), with registry data showing it is used more commonly in younger patients with fewer, predominantly cardiac, comorbidities [36]. A landmark study by Chen and colleagues reported 34.1% overall survival to hospital discharge (30.3% when restricted to CPC 1 or 2) in 135 patients receiving ECPR after > 10 min of unsuccessful CPR [13]. The average duration from CPR initiation to ECMO was 55.7 ± 27 min, with ~ 10–30 min needed to establish ECMO once the ECPR decision was made. Probability of survival to discharge was ~ 50%, 30%, and 10% for low-flow times of 30, 60, and 90 min, respectively.
Table 1.
Notable published studies of ECPR
| Type of study | No. of subjects | Outcome measurement | Resultsa | |
|---|---|---|---|---|
| IHCA | ||||
| Chen [14] | Propensity-score matched analysis | 46 matched pairs | Survival to discharge with CPC 1–2 |
ECPR vs CPR 30.4% vs 15.2%; HR 0.51, [0.35–0.74], p < 0.0001b |
| Shin [15] | Propensity-score matched analysis | 60 matched pairs | Two-year survival with minimal neurological impairment |
ECPR vs CPR 20% vs 5%; HR = 0.53, [0.36–0.80], p = 0.002 |
| Ouweneel [37] | Meta-analysis of matched pairs analyses | 195 matched pairs | 30-day survival with CPC 1–2 |
ECPR vs CPR 23% vs 9.7%, RR 0.85,c ARR 13%, [7–20%], p = 0.0001 |
| IHCA and OHCA with in-hospital ECPR | ||||
| Lunz [40] | Multicenter retrospective study |
IHCA: 165 OHCA: 258 |
3-month survival with CPC 1–2 |
IHCA vs OHCA 34.2% vs 9%; RR 0.72,c p < 0.01 |
| OHCA with in-hospital ECPR | ||||
| Choi [32] | Propensity-score matched analysis | 320 matched pairs | Survival to discharge with CPC 1–2 |
ECPR vs CPR 9% vs 6%, OR, 0.94; 95% CI, 0.41–2.14), p = NS |
| Yannopoulos [68] | ECPR protocol compared to historical controls |
ECPR: 62 CPR: 170 |
Survival to discharge with CPC 1–2 |
ECPR vs CPR 41.9% vs 15.3%, OR 4,d [2.08–7.7], p < 0.0001 |
| Yannopoulos [47] | RCT of ECPR or standard ACLS |
ECPR: 15 ACLS: 15 |
Survival to hospital discharge |
ECPR vs ACLS 43% [21.3–67.7] vs 7% [1.6–30.2], risk difference 36% [3.7–59.2], RR 0.61,c posterior probability of ECPR superiority: 0.9861 |
| Ref. [48] | RCT of ECPR or standard ACLS |
ECPR: 124 ACLS: 132 |
6-month survival with CPC 1 or 2 |
ECPR vs ACLS 31.5% vs 22%, RR 0.88,c p = 0.09 |
| Hsu [33] | Pilot trial of expedited transport and ECPR initiation or standard care |
Expedited transport: 12 (ECPR: 5 of 12) Standard: 3 |
ED arrival interval; ECPR initiation interval |
911-to-ED arrival < 30 min: 42% ED arrival-to-ECPR < 30 min: 60% |
| OHCA with pre-hospital or in-hospital ECPR | ||||
| Lamhaut [63] | Observational study comparing ECPR protocols |
Period 1: 114 Period 2: 42 |
Survival with CPC 1 or 2 at ICU discharge or day 28 |
Period 2 vs Period 1e 28.6% vs 7.9%, RR 0.78,c p < 0.001 |
| Bougouin [23] | Population-based registry study |
ECPR: 525 CPR: 12,666 |
Survival to hospital discharge |
ECPR vs CPR 8.4% vs 8.6%, p = 0.91; OR 1.3, [0.8–2.1], p = 0.24f Pre-hospital ECPR vs In-hospital ECPR OR 2.9;d 95% CI 1.5–5.9; p = 0.002 |
ACLS advanced cardiac life support, CPC cerebral performance status, CPR cardiopulmonary resuscitation, ECPR extracorporeal cardiopulmonary resuscitation, HR hazards ratio, IHCA in-hospital cardiac arrest, OHCA out-of-hospital cardiac arrest, OR odds ratio, RCT randomized controlled trial, RR risk ratio intensive care unit
aAll odds ratios, hazards ratios, and risk ratios represent odds or risk of mortality [95% confidence interval] unless otherwise specified
bHazards ratio and p value are for differences in overall survival; p value for survival with CPC 1–2 between groups was 0.09
cRisk ratio calculated based on reported mortality rates, therefore, no 95% confidence interval is provided
dOdds ratio of survival
ePeriod 1: less pre-hospital ECPR (41.4%); Period 2: more pre-hospital ECPR (64.3%)
fOdds ratio and 95% confidence interval after multivariate analysis
To assess potential benefits of ECPR over CPR alone, the same investigators performed a propensity-score matched analysis comparing patients suffering witnessed cardiac arrest of presumed cardiac origin, receiving > 10 min of CPR [14]. Overall survival to discharge with CPC 1 or 2 in ECPR patients (n = 59) was 23.7%, compared to 10.6% for conventional CPR (n = 113), p = 0.02. Among 46 matched pairs, those who underwent ECPR had significantly better survival to discharge (HR 0.51, 95% CI 0.35–0.74, p < 0.0001), which continued out to 1 year. The difference in survival to discharge with CPC 1 or 2 was not statistically significant (Table 1). A higher percentage of ECPR patients underwent subsequent percutaneous coronary intervention (PCI) (17.4% vs 6.5%), which may reflect treatment bias, or the ability of ECPR to sustain patients long enough to facilitate PCI.
A matched-pairs analysis by Shin et al. reported a similar association between ECPR (n = 85) and higher 2-year adjusted survival with minimal functional deficits compared to CPR (n = 321) for IHCA (Table 1) [15]. Younger age, shorter low-flow time, and subsequent cardiac intervention (PCI or cardiac surgery) were associated with more favorable functional outcomes in the ECPR group.
In a meta-analysis of ECPR versus CPR in predominantly IHCA, which incorporated 195 propensity-matched pairs, there was a 13% absolute risk difference in functionally intact 30-day survival favoring ECPR; PCI was much more common in the ECPR group [37].
Out-of-hospital cardiac arrest with in-hospital or pre-hospital ECPR
Patients consistently have better outcomes from ECPR in IHCA compared to OHCA [38–41]. A retrospective study in five European centers (n = 423) demonstrated significantly lower survival with functional recovery using ECPR for OHCA compared with IHCA (9% vs 34%, p < 0.01)[40] despite a lower burden of comorbidities; likely because IHCA subjects had higher rates of witnessed arrest and shorter low-flow times owing to initiation of bystander CPR.
One large population-based retrospective cohort study from South Korea analyzed differences in outcomes between ECPR and CPR for OHCA from 2009 to 2013, controlling for patient demographics, arrest characteristics, and co-interventions [32]. Despite an absolute rate of survival with functional recovery among ECPR recipients (n = 320) of 9%, compared to only 2% among conventional CPR recipients (n = 36,227), there was no significant difference in either multivariable logistic regression or propensity-matched analyses. Of note, only 30% of ECPR recipients had a shockable rhythm or received bystander CPR, suggesting that many patients were poor ECPR candidates [42]. Additionally, no-flow (pre-CPR) time and CPR duration were not considered in the analyses.
The largest study of OHCA, a retrospective registry-based study in the Greater Paris area from 2011 to 2018, analyzed outcomes incorporating pre-hospital and in-hospital ECPR [23]. Despite being younger and having higher rates of bystander CPR and initial shockable rhythms, the ECPR group (n = 525) had a similarly low rate of survival to hospital discharge as conventional CPR (n = 12,666), 8.4% vs 8.6%, without any significant differences in multivariate or propensity-matched analyses. Notably, pre-hospital ECPR, compared with in-hospital ECPR, was among the factors associated with greater odds of hospital survival (OR 2.9; 95% CI 1.5–5.9, p = 0.002), along with an initial shockable rhythm and transient ROSC before ECMO. While these results offer cautious optimism for pre-hospital ECPR, the overall low survival rate highlights the limitations of pre-hospital ECPR for OHCA in a real-world setting, including the complexity of the logistics and the need for better identification of patients likely to benefit [43].
Attempts to improve ECPR outcomes for OHCA have included earlier identification of favorable candidates, with an emphasis on shockable rhythms [44], and more rapid initiation of ECMO upon hospital arrival [24]. A single-center cohort study demonstrated that the combination of carefully selected patients with presumed cardiac aetiology, short no-flow times, high-quality CPR, minimization of low-flow time, and prompt coordination of ECMO, coronary angiography, and PCI, led to improved outcomes [22]. The system within which this study was conducted had a number of features including: identification by the emergency medical service (EMS) of potential ECPR candidates, central dispatch of mobile ECMO transport teams with 24/7 availability, three strategically located ECMO initiation hospitals (with 24/7 cardiac catheterization lab access) where EMS and the mobile ECMO team would come together for the purpose of cannulation, and a centralized ECMO intensive care unit (ICU) for optimized post-resuscitative care of ECPR patents [22, 45]. Development of this system involved stakeholders from four healthcare systems, ten EMS systems, government officials, hospital administrative leadership, and key clinical leaders throughout the greater Minneapolis-St. Paul metropolitan area [45]. The total operational costs of the Minnesota Resuscitation Consortium for a team of ECMO specialists, doctors, and paramedics are approximately 3 to 3.5 million dollars for the team to serve a population of 2 million people, shared between participating health care systems.1
A follow-up study of 160 patients treated with the same ECPR protocol demonstrated higher rates of survival with favorable neurological and functional status with CPR duration < 60 min than observed in a comparable group (n = 654) undergoing conventional CPR as part of an unrelated RCT [24, 46]. The effect of time on survival was prominent. Beyond 30 min, every additional 10 min of CPR decreased survival by 25% in ECPR. Nonetheless, survival of 15–20% was observed after CPR of up to 90 min. In contrast, none of the 218 treated with standard CPR for longer than 40 min survived. The same center recently conducted the first RCT of ECPR versus standard ACLS for refractory OHCA with ventricular fibrillation, using the same coordinated pre- and in-hospital resuscitation protocols [45, 47]. The trial, which was stopped early for prespecified superiority criteria after enrollment of only 30 patients, demonstrated a significantly higher survival to discharge for ECPR compared to standard ACLS (43% vs 7%, risk difference 36.2%, 95% CI 3.7–59.2), and more favorable neurological and functional outcomes at 3 and 6 months. These results offer optimism for ECPR in OHCA, but generalizability of such a carefully orchestrated system (including coordination with paramedic and general medical communities) is yet to be determined [45].
A second recently completed RCT, the Prague OHCA Trial, compared a bundle of interventions, including prompt intra-arrest transport, in-hospital ECPR and rapid invasive evaluation and treatment (n = 124), to standard ACLS (n = 132) in OHCA of presumed cardiac cause [48]. The trial, which was terminated based on prespecified subgroup analysis criteria, demonstrated a non-statistically significant difference in the primary outcome of 6-month survival with functional recovery favoring ECPR (31.5% vs 22%, p = 0.09) using an intention-to-treat (ITT) analysis, with 8% of patients crossing over from control to ECPR. Of note, the ECPR group had significantly more patients who underwent CPR for ≥ 45 min (73.4% vs 55.3%) and had worse pH and lactate values on admission, although they also had higher rates of targeted temperature management (95.1% vs 70.1%) and diagnostic angiography (97.6% vs 77%). A subgroup with ECPR patients with CPR duration ≥ 45 min had significantly higher rates of overall 6-month survival and survival with neurological recovery out to 30 days—a notable finding considering that 4 of 6 survivors in the standard ACLS group had crossed over to ECPR, further supporting the concept that ECPR may be successful despite prolonged low-flow times.
Patient-specific factors associated with ECPR outcomes
Across studies, several factors have consistently been identified as portending worse prognosis for ECPR over conventional CPR, including older age, longer duration of low-flow time, and an initial non-shockable rhythm (Table 2) [13, 15, 23, 40, 41, 49–55]. One high-volume center in Taiwan demonstrated that the combination of age > 75 and low-flow time > 60 min resulted in 0% neurological or functional recovery [20]. In a prospective study from Japan, one-month survival with CPC 1 or 2 was > 30% with low-flow time of 40 min in those with shockable rhythms compared to < 15% in non-shockable rhythms [51]. Other retrospective analyses have shown favorable outcomes despite prolonged low-flow time (> 45 min) when restricted to younger patients (≤ 43 years) [56], or when patients exhibit signs of life during CPR [55].
Table 2.
Factors associated with outcomes after ECPR
| Risk factors | Effect on survival with functional recovery | OR for survival | RR or HR for mortality | Modifiable? |
|---|---|---|---|---|
| Pre-arrest | ||||
| Older age | Unfavorable | Age > 60, OR 0.54 [13] | Age ≤ 65, HR 0.46 [15] | No |
| Shockable rhythm | Favorable | OR 1.39–3.93 [13, 23, 41, 51, 53, 55] |
HR 0.58 [14] Asystole, RR 1.36 [56] PEA, RR 1.2 [56] |
No |
| Intra-arrest | ||||
| Shorter no-flow or low-flow time | Favorable |
CPR < 30 min (vs > 30 min), OR 4.13 [13] CPR < 45 min (vs > 45 min), OR 3.53 [13] CPR < 60 min (vs > 60 min), OR 9.82 [13] For every 10 min shorter CPR, OR 1.95 [51] CPR duration per min increase, OR 0.97 [41] CPR < 45 min vs CPR > 58 min, OR 3.66 [52] |
CPR per min increase, HR 1.007 [14] CPR duration ≤ 35 min, HR 0.37 [15] |
Yes |
| High-quality CPR | Favorable | N/A | N/A | Yes |
| Post-arrest | ||||
| Targeted temperature management | Favorable | N/A | N/A | Yes |
| Percutaneous coronary intervention | Favorable | OR 1.52 [13] | HR 0.36 [15] | Yes |
CPR cardiopulmonary resuscitation, N/A not available, PEA pulseless electrical activity
Using a retrospective analysis of an ECPR cohort, Lunz et al. demonstrated how the application of a composite of stringent criteria (age ≤ 65, witnessed cardiac arrest with bystander CPR, no major comorbidity, and the ability to initiate ECMO within 1 h from arrest) could double the rate of survival with favorable functional outcomes (19–38%) [40]. These data, in conjunction with the prospective RCT data, highlight the potential of achieving survival with functional recovery with ECPR in select cases despite extended low-flow time, but such results are likely to have a strong correlation with other patient- and center-specific factors (e.g., comorbidities, reversibility of underlying aetiology, center experience, quality of post-resuscitation care) [24]. A better understanding of the relative contributions of each factor to patient outcomes is essential for optimal patient selection and would benefit from additional prospective, multicenter trials—although even that data will be limited by the selection criteria used for enrollment.
ELSO registry data
Additional real-world evidence is available from the ELSO registry [17]. Despite an increase in age and comorbidity in ECPR recipients, the average survival has remained steady at ~ 30% (predominantly reflecting IHCA case volume), with decreasing ECMO-associated complication rates [17]. The increase in ECPR cases likely represents a combination of expanded use and increased reporting. Unfortunately, conclusions from the ELSO registry are limited because it lacks important cardiac arrest and outcome details including no-flow time, low-flow time, transient ROSC during CPR, location of the arrest, and neurological and functional status of survivors. Revisions to the registry will make such information available in the future [57].
Organizational guidelines for the use of ECPR
ILCOR has incorporated ECPR into guidelines on Advanced Life Support [9, 58–60]. Acknowledging very-low-quality evidence, the committee offered a weak recommendation for ECPR as a rescue strategy for select patients with potentially reversible cardiac arrest etiologies in whom conventional CPR is failing [58, 59]. They also acknowledged that ECPR is complex, requires considerable resources and training, is not universally available, and may facilitate additional treatments such as PCI [9, 58–61]. The 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care emphasize the need for additional investigations to evaluate cost-effectiveness, resource allocation, and ethics surrounding the routine use of ECPR in resuscitation [62]. The European Resuscitation Council’s 2021 Guidelines acknowledge the results of the ARREST trial and suggests the consideration of ECPR as a rescue therapy for selected patients in settings in which it can be implemented [60]. Of note, all of these recommendations were developed before the results of the Prague OHCA trial were known.
Logistical considerations
Timing of initiation
ECPR should be viewed as complementary to high-quality conventional CPR given the association between bystander CPR and favorable long-term outcomes [30, 34, 35]. Indeed, most experienced centers require a minimum time (e.g., 10 min) of failed, high-quality CPR prior to cannulating for ECPR to avoid unnecessary deployment when ROSC might have been achieved by CPR alone [13, 15, 22, 39, 63]. To minimize low-flow time beyond this initial attempt at conventional resuscitation, there is a narrow window to perform cannulation. Providers should activate ECPR teams during cardiac arrest as soon as it is apparent that the patient might be an appropriate ECPR candidate, rather than waiting 10 min or longer to first assess success of CPR, given that the cannulation procedure will require additional time. High-volume ECMO centers have reported a wide range of times from cardiac arrest to establishment of ECMO, from 42.1 ± 25.7 min for IHCA to as long as 87.1 ± 26.9 min for OHCA patients [13, 15, 22, 39, 63], demonstrating the difficulty in limiting low-flow time even with rigorously designed strategies. The recently published Extracorporeal Cardiopulmonary Resuscitation for Refractory Out-of-Hospital Cardiac Arrest (EROCA) trial, a pilot trial assessing the feasibility of achieving a 911 call to emergency department (ED) arrival time of < 30 min and an ED arrival to ECPR initiation time of < 30 min, did not achieve its primary endpoint of 80% success rate for each time target—with actual rates of 42% and 60%, respectively—further highlighting the challenges in limiting low-flow times even under tightly controlled trial conditions [33]. Among other considerations, simulation training may help ensure more rapid cannulation [64].
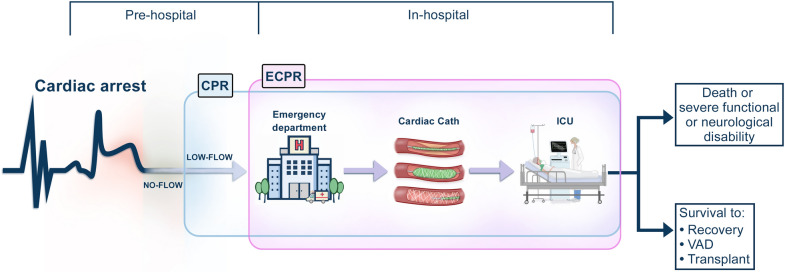
Resource availability and systems design
The resources required to effectively perform ECPR are substantial, including access to essential equipment (e.g., primed circuits), and availability of personnel capable of performing cannulation and managing the patient. The location where ECPR is performed, be it in-hospital (ED, operating room, catheterization laboratory, intensive care unit, or ward) or outside the hospital, will inform staffing and storage of supplies to minimize low-flow time, and may influence whether ECPR is restricted to certain locations within the hospital [65]. A detailed description of recommended personnel and supplies and recommendations for the systems design of cardiac ECMO programs in general, including centralization of resources to experienced, high-volume centers, has previously been published in a position paper [66]. Health systems that perform ECPR for OHCA should have formal plans detailing responsibilities of EMS and receiving hospitals to expedite ECPR on arrival to the ED or catheterization laboratory (Fig. 2) [22, 39, 67]. The relationship may consist of a hub-and-spoke model where local and referral centers initiate ECPR, but transfer patients to the hub for ongoing ECMO management [66].
Fig. 2.
Schematic representation of CPR and ECPR by location. Much like conventional CPR (blue shaded area), locations where ECPR may be initiated (pink shaded area) include: prior to arrival to the hospital (pre-hospital ECPR), emergency department, catheterization laboratory, intensive care unit, or other locations within the hospital where cardiac arrest may occur (e.g., operating room, inpatient ward). CPR cardiopulmonary resuscitation, ECPR extracorporeal cardiopulmonary resuscitation, ICU intensive care unit, IHCA in-hospital cardiac arrest, Low-flow time from initiation of CPR to initiation of ECPR, No-flow time between cardiac arrest and initiation of CPR, OHCA out-of-hospital cardiac arrest, VAD ventricular assist device
Post-resuscitation care
A vital component to any successful ECPR program is post-arrest care after cannulation, as highlighted by both the ARREST and Prague OHCA trials [47, 48]. Given the common occurrence of coronary artery disease as the aetiology of cardiac arrest [68, 69], and the importance of early revascularization on outcomes [70, 71], ECPR should be paired with rapid access to coronary angiography, with PCI as indicated [68]. Targeted temperature management (e.g., avoidance of hyperthermia, with or without hypothermia) should be implemented in ECPR patients, as appropriate, given data demonstrating a benefit on neurological outcomes [72]. This may easily be achieved through the extracorporeal circuit.
ECMO can markedly increase arterial partial pressures of oxygen (PaO2) and decrease carbon dioxide (PaCO2), although there is little data on appropriate oxygenation targets and the safest levels and rates of change in PaCO2. Extreme reductions in PaCO2 (< 30 mmHg) within the first 48 h of ECMO and rapid changes in PaCO2 from pre- to post-cannulation have been implicated in neurological complications [73, 74]. Prospective studies are needed to help determine the optimal gas exchange targets after initiation of ECPR.
Additionally, while the optimal anticoagulation strategy for this patient population is unknown, it is reasonable to apply the same institutional protocol as for conventional venoarterial ECMO, recognizing that some of these patients may be at increased bleeding risk in the setting of concomitant antiplatelet therapy after PCI, and may require early and potentially repeated neuroimaging [75, 76].
Availability of temporary circulatory support and long-term mechanical circulatory support device platforms (with or without access to on-site heart transplantation) are important elements to offer the greatest chance for survival when recovery remains uncertain [77]. Resources to address long-term management and complications in an intensive care setting, including neurological prognostication, are also essential [66].
Ethical considerations
There are a number of ethical dilemmas associated with ECPR [78, 79]. ECPR will invariably increase the number of patients receiving extracorporeal support without a meaningful chance of recovery, the so-called ‘bridge to nowhere’. Whereas use of implantable ventricular assist devices or long-term infusions of inotropic medications are commonly used as a ‘destination’ for patients with heart failure, often affording the patient an opportunity to be discharged home, an ECMO ‘bridge to nowhere’ necessarily confines the patient, who may or may not be awake and sentient, to an intensive care setting without prospect of discharge [78–80]. Conventional CPR can be stopped when efforts are deemed futile. Perhaps, then, ECPR may be considered an extension of CPR and subject to the same discretion, allowing clinicians to unilaterally withdraw ECMO when a meaningful outcome is unattainable. If, instead, ECPR transitions into sustained organ replacement therapy and is no longer classified as an extension of CPR, then one would presumably treat the patient as any other receiving life-sustaining therapies. To our knowledge, a determination of how ECPR should be classified relative to CPR in this regard has not been determined and appears open to interpretation, potentially creating the opportunity for unilateral cessation of ECMO under such circumstances.
Given that ECMO can adequately support end-organ perfusion with no native cardiac function, the relevance of addressing Do-Not-Resuscitate orders may be questioned. Even in the absence of a physiological role of conventional CPR, addressing code status may have symbolic meaning for the family [78]. As ECMO and ECPR become more commonplace, there may be an increasing need to consider ECPR in routine discussions of code status, with a category reserved for Do-Not-ECMO (DNE) [81, 82]. Ideally, healthcare professionals should engage in shared decision-making regarding end-of-life care [79, 81, 83]. Programs offering ECPR should anticipate these dilemmas and have policies and procedures to address them, including early involvement of palliative care services [66, 84].
Another area of controversy is organ donation. ECPR has the potential to increase organ availability. In a systematic review and meta-analysis, the prevalence of brain death was significantly higher with ECPR than CPR (27.9% vs. 8.3%, p < 0.0001), without a significant difference in the rate of organ donation between patients resuscitated with ECPR and CPR (29.4% vs. 59.2% of brain deaths, p = 0.544; 7.6% vs. 4.8% of total deaths, p = 0.471) [85]. This potential for increased availability of brain-dead donors may introduce ethical dilemmas regarding the motivation to initiate and the timing of withdrawal. Whereas organ donation should never be the primary intention of ECPR, it may nonetheless decrease the incidence of donation under uncontrolled circumstances (e.g., Maastricht classification categories II and V) and increase controlled donation upon withdrawal of ECMO (Maastricht category III) [23, 40, 86].
How clinicians approach these complex issues will vary by cultural and religious preference and according to local laws, hospital regulations, and ethical practices [83].
Economic impact
ECPR requires highly specialized equipment and personnel, and is expensive. A Finnish study calculated median cost per quality-adjusted life year (QALY) of 7474–12,642€ for venoarterial ECMO in a mixed cardiogenic shock and cardiac arrest population [87]. This likely represents an overly optimistic estimation given their high survival to discharge (65.7%). A recent cost-effectiveness model of ECPR for IHCA based on varying thresholds of age, Charlson Comorbidity Index, and gender determined that costs range from 8394 to 10,818€ per QALY, with an ECPR-for-all strategy falling within the typical willingness-to-pay threshold in North America and Europe [88].
Kawashima et al. noted that total hospital costs-per-life-saved by ECPR in a single Japanese center were two-fold higher for an initial non-shockable versus shockable rhythm ($213,656 vs $101,669); the cost per QALY for shockable rhythms was < 50% that for non-shockable rhythms ($11,081 vs $29,447), and the incremental cost-effectiveness ratio of ECPR over CPR was $16,246 per QALY [50]. A Canadian study of 692 patients receiving ECMO (43.8% for cardiac failure) over 8-years revealed that most of the costs in the year following admission (median Can $130,157) were incurred during the incident hospitalization (median Can $91,192) [89].
In a robust cost analysis of 62 ECPR patients (40% survival with functional recovery) at two centers in Australia, mean cost per ECPR patient was 50,535€, with ECPR adding an average of three QALYs per patient at 16,890€ per QALY over a 10-year period, or four QALYs per patient at 12,614€ over a 15-year period [90].
Where the optimal cost–benefit ratio lies, and whether the cost justifies marginal improvements in survival over conventional CPR, particularly in certain populations (e.g., pre-hospital ECPR), will vary by hospital, country, and region. It also depends on reliable estimates of ECPR effectiveness, making cost-effectiveness analyses an important part of any future large randomized controlled trial [50, 87, 91]. Of note, all existing economic assessments evaluate cost on a ‘per patient’ basis at centers with existing ECMO programs. These analyses do not take into consideration costs associated with the initiation of an ECMO program, let alone initiation of a de novo ECPR program at a center in which extracorporeal cardiopulmonary support was not previously available. Such start-up costs may make the overall cost per ECPR patient prohibitively expensive, especially in light of the infrequency of appropriate ECPR candidates [23, 32, 33].
Impact of pandemics on ECPR
The coronavirus disease 2019 (COVID-19) pandemic, with large numbers of critically ill patients [92], has raised questions about appropriateness of resource-intensive therapies, including ECPR [93, 94]. The concomitant risks to healthcare workers during resuscitative efforts create additional uncertainty about employing ECPR. In areas most strained during pandemics, it may be reasonable to restrict ECPR to patients highly likely to benefit or not offer it at all [93].
Areas of future research
Two landmark RCTs of ECPR versus conventional CPR for OHCA have now been completed, both of which suggest a clinically meaningful survival benefit, despite premature termination in one trial after reaching only 20% of target enrollment, raising questions about its validity, and a lack of statistical significance in the other [9, 47, 48, 58–60]. Several trials of ECPR versus CPR are ongoing (Table 3), although based on reported trial designs and sample sizes, none are likely to completely resolve existing uncertainty about the role of ECPR, particularly for OHCA.
Table 3.
Ongoing controlled trials of ECPR for out-of-hospital cardiac arrest
| Title | Study design | Sample size | Brief description | Primary outcome(s) |
|---|---|---|---|---|
| Early initiation of extracorporeal life support in refractory OHCA (INCEPTION); NCT03101787 | Multi-center randomized controlled trial | 110 | ECPR versus conventional CPR | 30-day survival with favorable neurological status (CPC 1 or 2) |
| BC ECPR trial for out-of-hospital cardiac arrest; NCT02832752 | Non-randomized, controlled parallel group trial (allocation based on region of treatment) | 420 | Incorporation of ECPR into regional medical system, compared to regions providing usual care | CPC status at hospital discharge |
| CPR, pre-hospital ECMO and early reperfusion (CHEER 3 Trial) for patients in refractory cardiac arrest to improve survival to hospital discharge | Single-center feasibility study | 25 | Implementation of pre-hospital ECPR | CPC status at hospital discharge |
| Pre-hospital ECMO in advanced resuscitation ion patients with refractory cardiac arrest (SUB30); NCT03700125 | Single-center feasibility study | 6 | Implementation of a pre-hospital ECMO-capable cardiac arrest team | Proportion of patients successfully established with pre-hospital ECPR within 30 min of collapse |
CPR cardiopulmonary resuscitation, ECPR extracorporeal cardiopulmonary resuscitation, ECMO extracorporeal membrane oxygenation, CPC cerebral performance status, OHCA out-of-hospital cardiac arrest
There remain substantial challenges to performing large, multicenter RCTs of ECPR, including coordination of healthcare delivery systems, clinical equipoise in expert centers—particularly as more data emerge—and the potential for uncontrolled crossover. We feel that a multicentre phase 3 trial with an accompanying economic analysis could provide vital information to help determine the efficacy of ECPR in OHCA, its generalizability beyond two highly specialized and coordinated healthcare systems (depending on the centers participating and study design), and the cost-effectiveness of the intervention. Ideally, design of such a trial should combine the expertise of those who perform ECPR with clinical trialists, epidemiologists and health economists. Even if such trials were successfully conducted and achieved their endpoints, additional questions would remain, such as how best to deliver ECPR to candidates at an optimal timepoint.
Regardless of future trial results, it is important to acknowledge that ECPR will never be as readily available as conventional CPR. The importance of early, high-quality CPR cannot be overstated and ECPR trials should focus on studying the role of ECPR in complementing resuscitative efforts for highly selected patients who have failed initial, optimal conventional CPR.
Conclusions
ECPR offers the promise of significantly improving the low rates of survival with functional and neurological recovery among patients suffering cardiac arrest. At present, there are sufficient data to support the initiation of ECPR in select individuals with reversible etiologies of cardiac arrest in whom low-flow time is minimized—and even in certain circumstances with more prolonged low-flow time—with greater potential benefit in IHCA than OHCA. These conditions assume that the healthcare system in which ECPR is offered is designed to deliver the intervention efficiently and effectively. Two recent RCTs have demonstrated that ECPR is best implemented in a high-volume, organized system, with extensive training and coordination among departments, including emergency services for OHCA. Future research should further our current understanding of the role of ECPR in cardiac arrest and refine our approach to this complex endeavor.
Author contributions
All authors provided substantial contributions to the conception or design of the work. DA and DB drafted the work, all authors revised it critically for important intellectual content. All authors have given final approval of the version to be published and agree to be accountable for all aspects of the work.
Funding
None.
Declarations
Conflicts of interest
DA reports serving as an at-large member of the Steering Committee for the Extracorporeal Life Support Organization (ELSO). GM reports serving as a member of the board of directors for ELSO. RL reports personal fees from Medtronic and LivaNova, outside the submitted work; member of advisory boards of Eurosets and PulseCath; advisor to the board of directors of ELSO and a past president of the European chapter of ELSO (EuroELSO). DY receives NIH grant support for resuscitation and ECPR and a Helmsley Philanthropic Trust grant for Mobile ECPR Implementation. LV receives consulting fees from Medtronic, outside the submitted work. JB is the current president of EuroELSO. FST reports personal fees from BARD, outside the submitted work. KS receives research support from Metro North Hospital and Health Service, outside the submitted work, and is the research lead of the ELSO Education Task Force (ECMOed) and member of the steering and educational committees for the Asia–Pacific chapter of ELSO (APELSO). ARG is a member of the advisory board for Abbott. JET was supported by a career development award (K23HL141596) from the National Heart, Lung, And Blood Institute (NHLBI) of the National Institutes of Health (NIH), received speakers fees and travel compensation from LivaNova relevant to cardiac arrest, outside the submitted work, speaker fees and travel compensation from Philips Healthcare, outside the submitted work, and is Chair of the Scientific Oversight Committee for ELSO. JSJ is an at-large member of the Steering Committee for the Asia–Pacific chapter of APELSO. YSC is the past chair and current conference committee chair of APELSO. ASS and AC report grants and personal fees from MAQUET, Xenios, and Baxter. AC was a past president of EuroELSO. DB receives research support from ALung Technologies, has been on the medical advisory boards for Baxter, Abiomed, Xenios, and Hemovent, and is the President-elect and member of the board of directors for ELSO. SP, NA, KT, and NU have no disclosures to report.
Footnotes
Personal communication (Demetri Yannopoulos, director of University of Minnesota’s Center for Resuscitation Medicine).
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Arthur S. Slutsky, Alain Combes, and Daniel Brodie are co-senior authors
References
- 1.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Shay CM, Spartano NL, Stokes A, Tirschwell DL, VanWagner LB, Tsao CW, American Heart Association Council on E, Prevention Statistics C, Stroke Statistics S Heart disease and stroke statistics-2020 update: a report from the American heart association. Circulation. 2020;141:e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 2.Schluep M, Gravesteijn BY, Stolker RJ, Endeman H, Hoeks SE. One-year survival after in-hospital cardiac arrest: a systematic review and meta-analysis. Resuscitation. 2018;132:90–100. doi: 10.1016/j.resuscitation.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Thompson LE, Chan PS, Tang F, Nallamothu BK, Girotra S, Perman SM, Bose S, Daugherty SL, Bradley SM, American Heart Association's Get With the Guidelines-Resuscitation I Long-term survival trends of medicare patients after in-hospital cardiac arrest: insights from get with the guidelines-resuscitation((R)) Resuscitation. 2018;123:58–64. doi: 10.1016/j.resuscitation.2017.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS, American Heart Association Get with the Guidelines-Resuscitation I Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB, American Heart Association Statistics C, Stroke Statistics S Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131:322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 6.Chan PS, McNally B, Tang F, Kellermann A, Group CS. Recent trends in survival from out-of-hospital cardiac arrest in the United States. Circulation. 2014;130:1876–1882. doi: 10.1161/CIRCULATIONAHA.114.009711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McNally B, Robb R, Mehta M, Vellano K, Valderrama AL, Yoon PW, Sasson C, Crouch A, Perez AB, Merritt R, Kellermann A. Out-of-hospital cardiac arrest surveillance—cardiac arrest registry to enhance survival (CARES), United States, October 1, 2005–December 31, 2010. MMWR Surveill Summ. 2011;60:1–19. [PubMed] [Google Scholar]
- 8.Malta Hansen C, Kragholm K, Pearson DA, Tyson C, Monk L, Myers B, Nelson D, Dupre ME, Fosbol EL, Jollis JG, Strauss B, Anderson ML, McNally B, Granger CB. Association of bystander and first-responder intervention with survival after out-of-hospital cardiac arrest in North Carolina, 2010–2013. JAMA. 2015;314:255–264. doi: 10.1001/jama.2015.7938. [DOI] [PubMed] [Google Scholar]
- 9.Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, Neumar RW, O'Neil BJ, Paxton JH, Silvers SM, White RD, Yannopoulos D, Donnino MW. Part 7: adult advanced cardiovascular life support: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S444–464. doi: 10.1161/CIR.0000000000000261. [DOI] [PubMed] [Google Scholar]
- 10.Reynolds JC, Frisch A, Rittenberger JC, Callaway CW. Duration of resuscitation efforts and functional outcome after out-of-hospital cardiac arrest: when should we change to novel therapies? Circulation. 2013;128:2488–2494. doi: 10.1161/CIRCULATIONAHA.113.002408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ebell MH, Jang W, Shen Y, Geocadin RG. Development and validation of the good outcome following attempted resuscitation (GO-FAR) score to predict neurologically intact survival after in-hospital cardiopulmonary resuscitation. JAMA Intern Med. 2013;173:1872–1878. doi: 10.1001/jamainternmed.2013.10037. [DOI] [PubMed] [Google Scholar]
- 12.Richardson AS, Schmidt M, Bailey M, Pellegrino VA, Rycus PT, Pilcher DV. ECMO cardio-pulmonary resuscitation (ECPR), trends in survival from an international multicentre cohort study over 12-years. Resuscitation. 2017;112:34–40. doi: 10.1016/j.resuscitation.2016.12.009. [DOI] [PubMed] [Google Scholar]
- 13.Chen YS, Yu HY, Huang SC, Lin JW, Chi NH, Wang CH, Wang SS, Lin FY, Ko WJ. Extracorporeal membrane oxygenation support can extend the duration of cardiopulmonary resuscitation. Crit Care Med. 2008;36:2529–2535. doi: 10.1097/CCM.0b013e318183f491. [DOI] [PubMed] [Google Scholar]
- 14.Chen YS, Lin JW, Yu HY, Ko WJ, Jerng JS, Chang WT, Chen WJ, Huang SC, Chi NH, Wang CH, Chen LC, Tsai PR, Wang SS, Hwang JJ, Lin FY. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet. 2008;372:554–561. doi: 10.1016/S0140-6736(08)60958-7. [DOI] [PubMed] [Google Scholar]
- 15.Shin TG, Jo IJ, Sim MS, Song YB, Yang JH, Hahn JY, Choi SH, Gwon HC, Jeon ES, Sung K, Lee YT, Choi JH. Two-year survival and neurological outcome of in-hospital cardiac arrest patients rescued by extracorporeal cardiopulmonary resuscitation. Int J Cardiol. 2013;168:3424–3430. doi: 10.1016/j.ijcard.2013.04.183. [DOI] [PubMed] [Google Scholar]
- 16.Kennedy JH. The role of assisted circulation in cardiac resuscitation. JAMA. 1966;197:615–618. [PubMed] [Google Scholar]
- 17.https://www.elso.org/Portals/0/Files/Reports/2020_January/International%20Summary%20January%202020_page1.pdf. Accessed 26 June 2021
- 18.Abrams D, Combes A, Brodie D. Extracorporeal membrane oxygenation in cardiopulmonary disease in adults. J Am Coll Cardiol. 2014;63:2769–2778. doi: 10.1016/j.jacc.2014.03.046. [DOI] [PubMed] [Google Scholar]
- 19.Belohlavek J, Mlcek M, Huptych M, Svoboda T, Havranek S, Ost'adal P, Boucek T, Kovarnik T, Mlejnsky F, Mrazek V, Belohlavek M, Aschermann M, Linhart A, Kittnar O. Coronary versus carotid blood flow and coronary perfusion pressure in a pig model of prolonged cardiac arrest treated by different modes of venoarterial ECMO and intraaortic balloon counterpulsation. Crit Care. 2012;16:R50. doi: 10.1186/cc11254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu HY, Wang CH, Chi NH, Huang SC, Chou HW, Chou NK, Chen YS. Effect of interplay between age and low-flow duration on neurologic outcomes of extracorporeal cardiopulmonary resuscitation. Intensive Care Med. 2019;45:44–54. doi: 10.1007/s00134-018-5496-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barsan WG, Levy RC. Experimental design for study of cardiopulmonary resuscitation in dogs. Ann Emerg Med. 1981;10:135–137. doi: 10.1016/s0196-0644(81)80377-0. [DOI] [PubMed] [Google Scholar]
- 22.Yannopoulos D, Bartos JA, Martin C, Raveendran G, Missov E, Conterato M, Frascone RJ, Trembley A, Sipprell K, John R, George S, Carlson K, Brunsvold ME, Garcia S, Aufderheide TP. Minnesota resuscitation consortium's advanced perfusion and reperfusion cardiac life support strategy for out-of-hospital refractory ventricular fibrillation. JAHA. 2016 doi: 10.1161/JAHA.116.003732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bougouin W, Dumas F, Lamhaut L, Marijon E, Carli P, Combes A, Pirracchio R, Aissaoui N, Karam N, Deye N, Sideris G, Beganton F, Jost D, Cariou A, Jouven X, Sudden Death Expertise Center Extracorporeal cardiopulmonary resuscitation in out-of-hospital cardiac arrest: a registry study. Eur Heart J. 2020;41:1961–1971. doi: 10.1093/eurheartj/ehz753. [DOI] [PubMed] [Google Scholar]
- 24.Bartos JA, Grunau B, Carlson C, Duval S, Ripeckyj A, Kalra R, Raveendran G, John R, Conterato M, Frascone RJ, Trembley A, Aufderheide TP, Yannopoulos D. Improved survival with extracorporeal cardiopulmonary resuscitation despite progressive metabolic derangement associated with prolonged resuscitation. Circulation. 2020;141:877–886. doi: 10.1161/CIRCULATIONAHA.119.042173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bartos JA, Carlson K, Carlson C, Raveendran G, John R, Aufderheide TP, Yannopoulos D. Surviving refractory out-of-hospital ventricular fibrillation cardiac arrest: Critical care and extracorporeal membrane oxygenation management. Resuscitation. 2018;132:47–55. doi: 10.1016/j.resuscitation.2018.08.030. [DOI] [PubMed] [Google Scholar]
- 26.Inoue A, Hifumi T, Sakamoto T, Kuroda Y. Extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest in adult patients. J Am Heart Assoc. 2020;9:e015291. doi: 10.1161/JAHA.119.015291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Danial P, Hajage D, Nguyen LS, Mastroianni C, Demondion P, Schmidt M, Bougle A, Amour J, Leprince P, Combes A, Lebreton G. Percutaneous versus surgical femoro-femoral veno-arterial ECMO: a propensity score matched study. Intensive Care Med. 2018;44:2153–2161. doi: 10.1007/s00134-018-5442-z. [DOI] [PubMed] [Google Scholar]
- 28.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D'Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D, International Liaison Committee on R, American Heart A, European Resuscitation C, Australian Resuscitation C, New Zealand Resuscitation C, Heart, Stroke Foundation of C, InterAmerican Heart F, Resuscitation Councils of Southern A, Arrest ITFoC, Cardiopulmonary Resuscitation O Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 29.Spangenberg T, Schewel J, Dreher A, Meincke F, Bahlmann E, van der Schalk H, Kreidel F, Frerker C, Stoeck M, Bein B, Kuck KH, Ghanem A. Health related quality of life after extracorporeal cardiopulmonary resuscitation in refractory cardiac arrest. Resuscitation. 2018;127:73–78. doi: 10.1016/j.resuscitation.2018.03.036. [DOI] [PubMed] [Google Scholar]
- 30.Kragholm K, Wissenberg M, Mortensen RN, Fonager K, Jensen SE, Rajan S, Lippert FK, Christensen EF, Hansen PA, Lang-Jensen T, Hendriksen OM, Kober L, Gislason G, Torp-Pedersen C, Rasmussen BS. Return to work in out-of-hospital cardiac arrest survivors: a nationwide register-based follow-up study. Circulation. 2015;131:1682–1690. doi: 10.1161/CIRCULATIONAHA.114.011366. [DOI] [PubMed] [Google Scholar]
- 31.Haywood K, Whitehead L, Nadkarni VM, Achana F, Beesems S, Bottiger BW, Brooks A, Castren M, Ong ME, Hazinski MF, Koster RW, Lilja G, Long J, Monsieurs KG, Morley PT, Morrison L, Nichol G, Oriolo V, Saposnik G, Smyth M, Spearpoint K, Williams B, Perkins GD. COSCA (core outcome set for cardiac arrest) in adults: an advisory statement from the international liaison committee on resuscitation. Circulation. 2018;137:e783–e801. doi: 10.1161/CIR.0000000000000562. [DOI] [PubMed] [Google Scholar]
- 32.Choi DS, Kim T, Ro YS, Ahn KO, Lee EJ, Hwang SS, Song SW, Song KJ, Shin SD. Extracorporeal life support and survival after out-of-hospital cardiac arrest in a nationwide registry: a propensity score-matched analysis. Resuscitation. 2016;99:26–32. doi: 10.1016/j.resuscitation.2015.11.013. [DOI] [PubMed] [Google Scholar]
- 33.Hsu CH, Meurer WJ, Domeier R, Fowler J, Whitmore SP, Bassin BS, Gunnerson KJ, Haft JW, Lynch WR, Nallamothu BK, Havey RA, Kidwell KM, Stacey WC, Silbergleit R, Bartlett RH, Neumar RW. Extracorporeal cardiopulmonary resuscitation for refractory out-of-hospital cardiac arrest (EROCA): results of a randomized feasibility trial of expedited out-of-hospital transport. Ann Emerg Med. 2021;78:92–101. doi: 10.1016/j.annemergmed.2020.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hasselqvist-Ax I, Riva G, Herlitz J, Rosenqvist M, Hollenberg J, Nordberg P, Ringh M, Jonsson M, Axelsson C, Lindqvist J, Karlsson T, Svensson L. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372:2307–2315. doi: 10.1056/NEJMoa1405796. [DOI] [PubMed] [Google Scholar]
- 35.Kragholm K, Wissenberg M, Mortensen RN, Hansen SM, Malta Hansen C, Thorsteinsson K, Rajan S, Lippert F, Folke F, Gislason G, Kober L, Fonager K, Jensen SE, Gerds TA, Torp-Pedersen C, Rasmussen BS. Bystander efforts and 1-year outcomes in out-of-hospital cardiac arrest. N Engl J Med. 2017;376:1737–1747. doi: 10.1056/NEJMoa1601891. [DOI] [PubMed] [Google Scholar]
- 36.Tonna JE, Selzman CH, Girotra S, Presson AP, Thiagarajan RR, Becker LB, Zhang C, Keenan HT, American Heart Association's Get With the Guidelines-Resuscitation I Patient and institutional characteristics influence the decision to use extracorporeal cardiopulmonary resuscitation for in-hospital cardiac arrest. J Am Heart Assoc. 2020;9:e015522. doi: 10.1161/JAHA.119.015522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ouweneel DM, Schotborgh JV, Limpens J, Sjauw KD, Engstrom AE, Lagrand WK, Cherpanath TGV, Driessen AHG, de Mol B, Henriques JPS. Extracorporeal life support during cardiac arrest and cardiogenic shock: a systematic review and meta-analysis. Intensive Care Med. 2016;42:1922–1934. doi: 10.1007/s00134-016-4536-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kagawa E, Inoue I, Kawagoe T, Ishihara M, Shimatani Y, Kurisu S, Nakama Y, Dai K, Takayuki O, Ikenaga H, Morimoto Y, Ejiri K, Oda N. Assessment of outcomes and differences between in- and out-of-hospital cardiac arrest patients treated with cardiopulmonary resuscitation using extracorporeal life support. Resuscitation. 2010;81:968–973. doi: 10.1016/j.resuscitation.2010.03.037. [DOI] [PubMed] [Google Scholar]
- 39.Stub D, Bernard S, Pellegrino V, Smith K, Walker T, Sheldrake J, Hockings L, Shaw J, Duffy SJ, Burrell A, Cameron P, de Smit V, Kaye DM. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial) Resuscitation. 2015;86:88–94. doi: 10.1016/j.resuscitation.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 40.Lunz D, Calabro L, Belliato M, Contri E, Broman LM, Scandroglio AM, Patricio D, Malfertheiner M, Creteur J, Philipp A, Taccone FS, Pappalardo F. Extracorporeal membrane oxygenation for refractory cardiac arrest: a retrospective multicenter study. Intensive Care Med. 2020;46:973–982. doi: 10.1007/s00134-020-05926-6. [DOI] [PubMed] [Google Scholar]
- 41.Wengenmayer T, Rombach S, Ramshorn F, Biever P, Bode C, Duerschmied D, Staudacher DL. Influence of low-flow time on survival after extracorporeal cardiopulmonary resuscitation (eCPR) Crit Care. 2017;21:157. doi: 10.1186/s13054-017-1744-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cho YH, Jung JS. Outcomes of extracorporeal life support in out-of-hospital cardiac arrest (OHCA): patient selection is crucial. Resuscitation. 2016;106:e13. doi: 10.1016/j.resuscitation.2016.01.041. [DOI] [PubMed] [Google Scholar]
- 43.MacLaren G, Masoumi A, Brodie D. ECPR for out-of-hospital cardiac arrest: more evidence is needed. Crit Care. 2020;24:7. doi: 10.1186/s13054-019-2722-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pozzi M, Koffel C, Armoiry X, Pavlakovic I, Neidecker J, Prieur C, Bonnefoy E, Robin J, Obadia JF. Extracorporeal life support for refractory out-of-hospital cardiac arrest: should we still fight for? A single-centre, 5-year experience. Int J Cardiol. 2016;204:70–76. doi: 10.1016/j.ijcard.2015.11.165. [DOI] [PubMed] [Google Scholar]
- 45.Bartos JA, Frascone RJ, Conterato M, Wesley K, Lick C, Sipprell K, Vuljaj N, Burnett A, Peterson BK, Simpson N, Ham K, Bruen C, Woster C, Haley KB, Moore J, Trigger B, Hodgson L, Harkins K, Kosmopoulos M, Aufderheide T, Tolar J, Yannopoulos D. The Minnesota mobile extracorporeal cardiopulmonary resuscitation consortium for treatment of out-of-hospital refractory ventricular fibrillation: Program description, performance, and outcomes. EClinicalMedicine. 2020 doi: 10.2139/ssrn.3719070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kudenchuk PJ, Brown SP, Daya M, Rea T, Nichol G, Morrison LJ, Leroux B, Vaillancourt C, Wittwer L, Callaway CW, Christenson J, Egan D, Ornato JP, Weisfeldt ML, Stiell IG, Idris AH, Aufderheide TP, Dunford JV, Colella MR, Vilke GM, Brienza AM, Desvigne-Nickens P, Gray PC, Gray R, Seals N, Straight R, Dorian P, Resuscitation Outcomes Consortium I Amiodarone, lidocaine, or placebo in out-of-hospital cardiac arrest. N Engl J Med. 2016;374:1711–1722. doi: 10.1056/NEJMoa1514204. [DOI] [PubMed] [Google Scholar]
- 47.Yannopoulos D, Bartos J, Raveendran G, Walser E, Connett J, Murray TA, Collins G, Zhang L, Kalra R, Kosmopoulos M, John R, Shaffer A, Frascone RJ, Wesley K, Conterato M, Biros M, Tolar J, Aufderheide TP. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet. 2020;396:1807–1816. doi: 10.1016/S0140-6736(20)32338-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.https://www.radcliffecardiology.com/ACC%2021-Prague-OCHA-Study. Accessed 28 Aug 2021
- 49.Ko RE, Ryu JA, Cho YH, Sung K, Jeon K, Suh GY, Park TK, Lee JM, Song YB, Hahn JY, Choi JH, Choi SH, Gwon HC, Carriere KC, Ahn J, Yang JH. The differential neurologic prognosis of low-flow time according to the initial rhythm in patients who undergo extracorporeal cardiopulmonary resuscitation. Resuscitation. 2020;148:121–127. doi: 10.1016/j.resuscitation.2020.01.015. [DOI] [PubMed] [Google Scholar]
- 50.Kawashima T, Uehara H, Miyagi N, Shimajiri M, Nakamura K, Chinen T, Hatano S, Nago C, Chiba S, Nakane H, Gima Y. Impact of first documented rhythm on cost-effectiveness of extracorporeal cardiopulmonary resuscitation. Resuscitation. 2019;140:74–80. doi: 10.1016/j.resuscitation.2019.05.013. [DOI] [PubMed] [Google Scholar]
- 51.Matsuyama T, Irisawa T, Yamada T, Hayakawa K, Yoshiya K, Noguchi K, Nishimura T, Ishibe T, Yagi Y, Kiguchi T, Kishimoto M, Shintani H, Hayashi Y, Sogabe T, Morooka T, Sakamoto H, Suzuki K, Nakamura F, Nishioka N, Okada Y, Matsui S, Sado J, Shimazu T, Ohta B, Iwami T, Kitamura T, Investigators CSG. Impact of low-flow duration on favorable neurological outcomes of extracorporeal cardiopulmonary resuscitation after out-of-hospital cardiac arrest: a multicenter prospective study. Circulation. 2020;141:1031–1033. doi: 10.1161/CIRCULATIONAHA.119.044285. [DOI] [PubMed] [Google Scholar]
- 52.D'Arrigo S, Cacciola S, Dennis M, Jung C, Kagawa E, Antonelli M, Sandroni C. Predictors of favourable outcome after in-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation: a systematic review and meta-analysis. Resuscitation. 2017;121:62–70. doi: 10.1016/j.resuscitation.2017.10.005. [DOI] [PubMed] [Google Scholar]
- 53.Beyea MM, Tillmann BW, Iansavichene AE, Randhawa VK, Van Aarsen K, Nagpal AD. Neurologic outcomes after extracorporeal membrane oxygenation assisted CPR for resuscitation of out-of-hospital cardiac arrest patients: a systematic review. Resuscitation. 2018;130:146–158. doi: 10.1016/j.resuscitation.2018.07.012. [DOI] [PubMed] [Google Scholar]
- 54.Debaty G, Babaz V, Durand M, Gaide-Chevronnay L, Fournel E, Blancher M, Bouvaist H, Chavanon O, Maignan M, Bouzat P, Albaladejo P, Labarere J. Prognostic factors for extracorporeal cardiopulmonary resuscitation recipients following out-of-hospital refractory cardiac arrest. A systematic review and meta-analysis. Resuscitation. 2017;112:1–10. doi: 10.1016/j.resuscitation.2016.12.011. [DOI] [PubMed] [Google Scholar]
- 55.Mork SR, Stengaard C, Linde L, Moller JE, Jensen LO, Schmidt H, Riber LP, Andreasen JB, Thomassen SA, Laugesen H, Freeman PM, Christensen S, Greisen JR, Tang M, Moller-Sorensen PH, Holmvang L, Gregers E, Kjaergaard J, Hassager C, Eiskjaer H, Terkelsen CJ. Mechanical circulatory support for refractory out-of-hospital cardiac arrest: a Danish nationwide multicenter study. Crit Care. 2021;25:174. doi: 10.1186/s13054-021-03606-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Aubin H, Petrov G, Dalyanoglu H, Saeed D, Akhyari P, Paprotny G, Richter M, Westenfeld R, Schelzig H, Kelm M, Kindgen-Milles D, Lichtenberg A, Albert A. A suprainstitutional network for remote extracorporeal life support: a retrospective cohort study. JACC Heart failure. 2016;4:698–708. doi: 10.1016/j.jchf.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 57.Lorusso R, Alexander P, Rycus P, Barbaro R. The extracorporeal life support organization registry: update and perspectives. Ann Cardiothorac Surg. 2019;8:93–98. doi: 10.21037/acs.2018.11.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Callaway CW, Soar J, Aibiki M, Bottiger BW, Brooks SC, Deakin CD, Donnino MW, Drajer S, Kloeck W, Morley PT, Morrison LJ, Neumar RW, Nicholson TC, Nolan JP, Okada K, O'Neil BJ, Paiva EF, Parr MJ, Wang TL, Witt J. Part 4: advanced life support: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015;132:S84–145. doi: 10.1161/CIR.0000000000000273. [DOI] [PubMed] [Google Scholar]
- 59.Brooks SC, Anderson ML, Bruder E, Daya MR, Gaffney A, Otto CW, Singer AJ, Thiagarajan RR, Travers AH. Part 6: alternative techniques and ancillary devices for cardiopulmonary resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S436–443. doi: 10.1161/CIR.0000000000000260. [DOI] [PubMed] [Google Scholar]
- 60.Soar J, Bottiger BW, Carli P, Couper K, Deakin CD, Djarv T, Lott C, Olasveengen T, Paal P, Pellis T, Perkins GD, Sandroni C, Nolan JP. European resuscitation council guidelines 2021: adult advanced life support. Resuscitation. 2021;161:115–151. doi: 10.1016/j.resuscitation.2021.02.010. [DOI] [PubMed] [Google Scholar]
- 61.Tonna JE, Johnson NJ, Greenwood J, Gaieski DF, Shinar Z, Bellezo JM, Becker L, Shah AP, Youngquist ST, Mallin MP, Fair JF, 3rd, Gunnerson KJ, Weng C, McKellar S, Extracorporeal RCRG. Practice characteristics of emergency department extracorporeal cardiopulmonary resuscitation (eCPR) programs in the United States: the current state of the art of emergency department extracorporeal membrane oxygenation (ED ECMO) Resuscitation. 2016;107:38–46. doi: 10.1016/j.resuscitation.2016.07.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Panchal AR, Bartos JA, Cabanas JG, Donnino MW, Drennan IR, Hirsch KG, Kudenchuk PJ, Kurz MC, Lavonas EJ, Morley PT, O'Neil BJ, Peberdy MA, Rittenberger JC, Rodriguez AJ, Sawyer KN, Berg KM, Adult B. Part 3: adult basic and advanced life support: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142:S366–S468. doi: 10.1161/CIR.0000000000000916. [DOI] [PubMed] [Google Scholar]
- 63.Lamhaut L, Hutin A, Puymirat E, Jouan J, Raphalen JH, Jouffroy R, Jaffry M, Dagron C, An K, Dumas F, Marijon E, Bougouin W, Tourtier JP, Baud F, Jouven X, Danchin N, Spaulding C, Carli P. A pre-hospital extracorporeal cardio pulmonary resuscitation (ECPR) strategy for treatment of refractory out hospital cardiac arrest: an observational study and propensity analysis. Resuscitation. 2017;117:109–117. doi: 10.1016/j.resuscitation.2017.04.014. [DOI] [PubMed] [Google Scholar]
- 64.Whitmore SP, Gunnerson KJ, Haft JW, Lynch WR, VanDyck T, Hebert C, Waldvogel J, Havey R, Weinberg A, Cranford JA, Rooney DM, Neumar RW. Simulation training enables emergency medicine providers to rapidly and safely initiate extracorporeal cardiopulmonary resuscitation (ECPR) in a simulated cardiac arrest scenario. Resuscitation. 2019;138:68–73. doi: 10.1016/j.resuscitation.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 65.Kane DA, Thiagarajan RR, Wypij D, Scheurer MA, Fynn-Thompson F, Emani S, del Nido PJ, Betit P, Laussen PC. Rapid-response extracorporeal membrane oxygenation to support cardiopulmonary resuscitation in children with cardiac disease. Circulation. 2010;122:S241–248. doi: 10.1161/CIRCULATIONAHA.109.928390. [DOI] [PubMed] [Google Scholar]
- 66.Abrams D, Garan AR, Abdelbary A, Bacchetta M, Bartlett RH, Beck J, Belohlavek J, Chen YS, Fan E, Ferguson ND, Fowles JA, Fraser J, Gong M, Hassan IF, Hodgson C, Hou X, Hryniewicz K, Ichiba S, Jakobleff WA, Lorusso R, MacLaren G, McGuinness S, Mueller T, Park PK, Peek G, Pellegrino V, Price S, Rosenzweig EB, Sakamoto T, Salazar L, Schmidt M, Slutsky AS, Spaulding C, Takayama H, Takeda K, Vuylsteke A, Combes A, Brodie D, International EN, The Extracorporeal Life Support O Position paper for the organization of ECMO programs for cardiac failure in adults. Intensive Care Med. 2018;44:717–729. doi: 10.1007/s00134-018-5064-5. [DOI] [PubMed] [Google Scholar]
- 67.Tonna JE, Selzman CH, Mallin MP, Smith BR, Youngquist ST, Koliopoulou A, Welt F, Stoddard KD, Nirula R, Barton R, Fair JF, 3rd, Fang JC, McKellar S. Development and implementation of a comprehensive, multidisciplinary emergency department extracorporeal membrane oxygenation program. Ann Emerg Med. 2017;70:32–40. doi: 10.1016/j.annemergmed.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 68.Yannopoulos D, Bartos JA, Raveendran G, Conterato M, Frascone RJ, Trembley A, John R, Connett J, Benditt DG, Lurie KG, Wilson RF, Aufderheide TP. Coronary artery disease in patients with out-of-hospital refractory ventricular fibrillation cardiac arrest. J Am Coll Cardiol. 2017;70:1109–1117. doi: 10.1016/j.jacc.2017.06.059. [DOI] [PubMed] [Google Scholar]
- 69.Kagawa E, Dote K, Kato M, Sasaki S, Nakano Y, Kajikawa M, Higashi A, Itakura K, Sera A, Inoue I, Kawagoe T, Ishihara M, Shimatani Y, Kurisu S. Should we emergently revascularize occluded coronaries for cardiac arrest? Rapid-response extracorporeal membrane oxygenation and intra-arrest percutaneous coronary intervention. Circulation. 2012;126:1605–1613. doi: 10.1161/CIRCULATIONAHA.111.067538. [DOI] [PubMed] [Google Scholar]
- 70.Camuglia AC, Randhawa VK, Lavi S, Walters DL. Cardiac catheterization is associated with superior outcomes for survivors of out of hospital cardiac arrest: review and meta-analysis. Resuscitation. 2014;85:1533–1540. doi: 10.1016/j.resuscitation.2014.08.025. [DOI] [PubMed] [Google Scholar]
- 71.Dumas F, Bougouin W, Geri G, Lamhaut L, Rosencher J, Pene F, Chiche JD, Varenne O, Carli P, Jouven X, Mira JP, Spaulding C, Cariou A. Emergency percutaneous coronary intervention in post-cardiac arrest patients without ST-segment elevation pattern: insights from the PROCAT II registry. JACC Cardiovasc Interv. 2016;9:1011–1018. doi: 10.1016/j.jcin.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 72.Dankiewicz J, Cronberg T, Lilja G, Jakobsen JC, Levin H, Ullen S, Rylander C, Wise MP, Oddo M, Cariou A, Belohlavek J, Hovdenes J, Saxena M, Kirkegaard H, Young PJ, Pelosi P, Storm C, Taccone FS, Joannidis M, Callaway C, Eastwood GM, Morgan MPG, Nordberg P, Erlinge D, Nichol AD, Chew MS, Hollenberg J, Thomas M, Bewley J, Sweet K, Grejs AM, Christensen S, Haenggi M, Levis A, Lundin A, During J, Schmidbauer S, Keeble TR, Karamasis GV, Schrag C, Faessler E, Smid O, Otahal M, Maggiorini M, Wendel Garcia PD, Jaubert P, Cole JM, Solar M, Borgquist O, Leithner C, Abed-Maillard S, Navarra L, Annborn M, Unden J, Brunetti I, Awad A, McGuigan P, Bjorkholt Olsen R, Cassina T, Vignon P, Langeland H, Lange T, Friberg H, Nielsen N, TTMT Investigators Hypothermia versus normothermia after out-of-hospital cardiac arrest. N Engl J Med. 2021;384:2283–2294. doi: 10.1056/NEJMoa2100591. [DOI] [PubMed] [Google Scholar]
- 73.Cashen K, Reeder R, Dalton HJ, Berg RA, Shanley TP, Newth CJL, Pollack MM, Wessel D, Carcillo J, Harrison R, Dean JM, Tamburro R, Meert KL, Eunice Kennedy Shriver National Institute of Child H, Human Development Collaborative Pediatric Critical Care Research N Hyperoxia and hypocapnia during pediatric extracorporeal membrane oxygenation: associations with complications, mortality, and functional status among survivors. Pediatr Crit Care Med. 2018;19:245–253. doi: 10.1097/PCC.0000000000001439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Luyt CE, Brechot N, Demondion P, Jovanovic T, Hekimian G, Lebreton G, Nieszkowska A, Schmidt M, Trouillet JL, Leprince P, Chastre J, Combes A. Brain injury during venovenous extracorporeal membrane oxygenation. Intensive Care Med. 2016;42:897–907. doi: 10.1007/s00134-016-4318-3. [DOI] [PubMed] [Google Scholar]
- 75.Cartwright B, Bruce HM, Kershaw G, Cai N, Othman J, Gattas D, Robson JL, Hayes S, Alicajic H, Hines A, Whyte A, Chaikittisilpa N, Southwood TJ, Forrest P, Totaro RJ, Bannon PG, Dunkley S, Chen VM, Dennis M. Hemostasis, coagulation and thrombin in venoarterial and venovenous extracorporeal membrane oxygenation: the HECTIC study. Sci Rep. 2021;11:7975. doi: 10.1038/s41598-021-87026-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Le Guennec L, Cholet C, Huang F, Schmidt M, Brechot N, Hekimian G, Besset S, Lebreton G, Nieszkowska A, Leprince P, Combes A, Luyt CE. Ischemic and hemorrhagic brain injury during venoarterial-extracorporeal membrane oxygenation. Ann Intensive Care. 2018;8:129. doi: 10.1186/s13613-018-0475-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Combes A, Price S, Slutsky AS, Brodie D. Temporary circulatory support for cardiogenic shock. Lancet. 2020;396:199–212. doi: 10.1016/S0140-6736(20)31047-3. [DOI] [PubMed] [Google Scholar]
- 78.Abrams DC, Prager K, Blinderman CD, Burkart KM, Brodie D. Ethical dilemmas encountered with the use of extracorporeal membrane oxygenation in adults. Chest. 2014;145:876–882. doi: 10.1378/chest.13-1138. [DOI] [PubMed] [Google Scholar]
- 79.Abrams D, Curtis JR, Prager KM, Garan AR, Hastie J, Brodie D. Ethical considerations for mechanical support. Anesthesiol Clin. 2019;37:661–673. doi: 10.1016/j.anclin.2019.08.001. [DOI] [PubMed] [Google Scholar]
- 80.Mulaikal TA, Nakagawa S, Prager KM. Extracorporeal membrane oxygenation bridge to no recovery. Circulation. 2019;139:428–430. doi: 10.1161/CIRCULATIONAHA.118.036304. [DOI] [PubMed] [Google Scholar]
- 81.Brodie D, Curtis JR, Vincent JL, Bakker J, Brown CE, Creteur J, Papazian L, Sladen RN, Ranieri VM. Treatment limitations in the era of ECMO. Lancet Respir Med. 2017;5:769–770. doi: 10.1016/S2213-2600(17)30263-1. [DOI] [PubMed] [Google Scholar]
- 82.Simons J, Suverein M, van Mook W, Caliskan K, Soliman O, van de Poll M, Delnoij T, Maessen J, Mees B, Lorusso R. Do-(not-)mechanical-circulatory-support orders: should we ask all cardiac surgery patients for informed consent for post-cardiotomy extracorporeal life circulatory support? J Clin Med. 2021;10:383. doi: 10.3390/jcm10030383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Abrams D, Pham T, Burns KEA, Combes A, Curtis JR, Mueller T, Prager KM, Serra A, Slutsky AS, Brodie D, Schmidt M. Practice patterns and ethical considerations in the management of venovenous extracorporeal membrane oxygenation patients: an international survey. Crit Care Med. 2019;47:1346–1355. doi: 10.1097/CCM.0000000000003910. [DOI] [PubMed] [Google Scholar]
- 84.Bein T, Brodie D. Understanding ethical decisions for patients on extracorporeal life support. Intensive Care Med. 2017;43:1510–1511. doi: 10.1007/s00134-017-4781-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sandroni C, D'Arrigo S, Callaway CW, Cariou A, Dragancea I, Taccone FS, Antonelli M. The rate of brain death and organ donation in patients resuscitated from cardiac arrest: a systematic review and meta-analysis. Intensive Care Med. 2016;42:1661–1671. doi: 10.1007/s00134-016-4549-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Thuong M, Ruiz A, Evrard P, Kuiper M, Boffa C, Akhtar MZ, Neuberger J, Ploeg R. New classification of donation after circulatory death donors definitions and terminology. Transpl Int. 2016;29:749–759. doi: 10.1111/tri.12776. [DOI] [PubMed] [Google Scholar]
- 87.Jaamaa-Holmberg S, Salmela B, Suojaranta R, Lemstrom KB, Lommi J. Cost-utility of venoarterial extracorporeal membrane oxygenation in cardiogenic shock and cardiac arrest. Eur Heart J. 2020;9:333. doi: 10.1177/2048872619900090. [DOI] [PubMed] [Google Scholar]
- 88.Gravesteijn BY, Schluep M, Voormolen DC, van der Burgh AC, Dos Reis MD, Hoeks SE, Endeman H. Cost-effectiveness of extracorporeal cardiopulmonary resuscitation after in-hospital cardiac arrest: a Markov decision model. Resuscitation. 2019;143:150–157. doi: 10.1016/j.resuscitation.2019.08.024. [DOI] [PubMed] [Google Scholar]
- 89.Fernando SM, Qureshi D, Tanuseputro P, Fan E, Munshi L, Rochwerg B, Talarico R, Scales DC, Brodie D, Dhanani S, Guerguerian AM, Shemie SD, Thavorn K, Kyeremanteng K. Mortality and costs following extracorporeal membrane oxygenation in critically ill adults: a population-based cohort study. Intensive Care Med. 2019;45:1580–1589. doi: 10.1007/s00134-019-05766-z. [DOI] [PubMed] [Google Scholar]
- 90.Dennis M, Zmudzki F, Burns B, Scott S, Gattas D, Reynolds C, Buscher H, Forrest P, Sydney ERIG. Cost effectiveness and quality of life analysis of extracorporeal cardiopulmonary resuscitation (ECPR) for refractory cardiac arrest. Resuscitation. 2019;139:49–56. doi: 10.1016/j.resuscitation.2019.03.021. [DOI] [PubMed] [Google Scholar]
- 91.Bharmal MI, Venturini JM, Chua RFM, Sharp WW, Beiser DG, Tabit CE, Hirai T, Rosenberg JR, Friant J, Blair JEA, Paul JD, Nathan S, Shah AP. Cost-utility of extracorporeal cardiopulmonary resuscitation in patients with cardiac arrest. Resuscitation. 2019;136:126–130. doi: 10.1016/j.resuscitation.2019.01.027. [DOI] [PubMed] [Google Scholar]
- 92.Cummings MJ, Baldwin MR, Abrams D, Jacobson SD, Meyer BJ, Balough EM, Aaron JG, Claassen J, Rabbani LE, Hastie J, Hochman BR, Salazar-Schicchi J, Yip NH, Brodie D, O'Donnell MR. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. 2020;395:1763–1770. doi: 10.1016/S0140-6736(20)31189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Abrams D, Lorusso R, Vincent JL, Brodie D. ECMO during the COVID-19 pandemic: when is it unjustified? Crit Care. 2020;24:507. doi: 10.1186/s13054-020-03230-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.MacLaren G, Fisher D, Brodie D. Preparing for the most critically ill patients with COVID-19: the potential role of extracorporeal membrane oxygenation. JAMA. 2020;323:1245–1246. doi: 10.1001/jama.2020.2342. [DOI] [PubMed] [Google Scholar]