Abstract
Objective: This research was designed to explore the application evaluation of evidence-based nursing (EBN) in pain nursing of patients with advanced lung cancer (LC). Methods: A total of 108 advanced LC patients admitted to our hospital were randomized into a control group and an observation group, each with 54 patients. Those in the control group were given conventional nursing measures and those in the observation group were treated by EBN measures based on the former. The scores of pain levels, sleep quality, and negative emotions (anxiety and depression), quality of life, and nursing satisfaction of the two groups were compared. Results: Compared with the control group, the sleep quality score, quality of life, and nursing satisfaction of patients in the observation group were higher. The scores of pain levels and negative emotions (anxiety and depression) were lower, with statistically marked differences (all P<0.05). Conclusion: EBN has good clinical practicability in the pain of advanced LC, improving patients’ sleep, quality of life after treatment, and nursing satisfaction. It can be recommended in clinical practice.
Keywords: Patients with advanced lung cancer, pain, evidence-based nursing, quality of life, nursing satisfaction
Introduction
Lung cancer (LC) is a common malignancy of the respiratory system, ranking among the first three tumorigenesis. With the deterioration of environment, changes in diet structure, and gradual aggravation of static lifestyle, the morbidity is increasing year by year [1-3]. There is no specific manifestation in the early stage. Patients often lose the opportunity of surgical treatment because they have advanced to the middle and late stage when discovered [4-6].
Pain is the main clinical manifestation of advanced LC, which is attributed to the invasion of local nerves by tumors, causing discomfort to patients. In addition, various adverse reactions of follow-up treatment may lead to depression and anxiety which will lead to the decrease of treatment cooperation and shorten the life cycle of patients. The treatment of pain is one of the important contents of LC [7-9]. Nursing is the main component of clinical work. Active and effective nursing measures can reduce patients’ pain and negative emotions, and improve their quality of life and life cycle [10,11]. Evidence-based nursing (EBN) is a new nursing concept, which provides relevant and effective targeted nursing measures by reading literature and combining relevant professional knowledge. It has achieved good application results in various fields [12]. However, there has been no previous research report on EBN in advanced LC patients. This research applied EBN measures in the treatment of pain in advanced LC and observed the clinical efficacy, to provide more evidence-based basis.
Materials and methods
General data
A total of 108 advanced LC patients admitted to our hospital from January 2019 to December 2020 were prospectively selected and randomized into either a control group or an observation group, each totaling 54 patients. Those in the control group were given conventional nursing measures. Those in the observation group were treated by EBN based on the former. Inclusion criteria were as follows: (1) Those diagnosed with LC by pathological classification; (2) LC stage III-IV; (3) Patients with clinical pain; (4) The estimated life cycle was more than half a year [1].
Exclusion criteria were as follows: (1) Those who could not speak; (2) Patients with nervous system diseases; (3) Insomnia; (4) Those who had a history of depression and anxiety; (5) Those with heart, liver, and kidney insufficiency; (6) There were those with mental disorders that could not be included in the research. Both groups of patients were aware about this research and signed an informed consent form. This research was approved by the Ethics Committee of our hospital.
Treatment methods
After admission, all patients participated in comprehensive treatment measures according to LC classification and staging. The three-step analgesic method could assist for related analgesic treatment.
Conventional nursing methods
Patients participated in conventional nursing measures in the oncology department, including routine publicity and education on LC, dietary guidance, and medication.
EBN methods
Based on conventional nursing, the observation group applied EBN: (1) An EBN group was established and included a head nurse, an associate chief physician, specialist nurses in the oncology department, and charge and bed nurses [12]; Then, they were trained to master EBN methods; The theoretical level of pain-related knowledge and nursing skills was strengthened. (2) Based on the causes and treatment measures of advanced LC pain, the deputy chief physician studied the pathophysiological characteristics of pain and nursing related research hotspots by consulting relevant literature; The nursing staff explored the targeted measures of cancer pain nursing, and finally determined the nursing plan.
It mainly includes: (1) Psychological supported nursing measures: The late stage of LC itself brings anxiety and depression to patients. Pain will aggravate the above-mentioned adverse emotions to a certain extent, and even produce pessimism and world-weariness emotions. At this time, the nursing staff should carry out targeted and personalized nursing measures according to patients’ personal experience, cultural background, and related medical experience, and emphasize the necessity of eye contact, active communication, and implement necessary psychological support to alleviate their pain.
(2) Medication nursing measures: Nurses master the current three-step analgesic method, skillfully use all levels of analgesics according to the pain degree and position of patients, and avoid the pain aggravated by traumatic medication. They take the initiative to care about the position and nature of patients’ pain and suggest relevant body position guidance, paying attention to the adverse reactions of pre-pain prevention drugs and relevant targeted treatment measures.
(3) Diet nursing measures: patients were encouraged to eat freely. High protein such as chicken, beef, bean products, and fish were chosen first to increase energy intake.
(4) Environmental nursing measures: The light in the ward was adjusted, mainly soft light. The number of accompanying staff in the ward was reduced, and only one family member was chosen to accompany them for 24 h. This can not only increase patients’ sense of security, but also reduce their emotional fluctuation caused by noise. Patients could play their favorite music to shift their attention.
(5) Other measures: Proper exercise was needed, giving priority to not feeling shortness of breath. Centralized medical activities were adopted to avoid disturbing the patient’s relaxation and sleep and the other patients.
Outcome measures
Main outcome measures
The pain changes of the two groups before and after treatment were evaluated by the visual analogue scale (VAS) [13]: A swimming scale with a length of about 10 cm was used, one side was marked with 10 scales; The two ends were “0” and “10” respectively; 0 denoted painlessness and 10 meant the most severe pain that was unbearable.
Sleep quality was assessed by the Pittsburgh Sleep Quality Index, referring to PSQI and QOL scale: It was composed of 19 self-evaluation and 5 other items, with a total score ranging from 0 to 21. The higher the score, the worse the sleep quality of patients was.
The self-rating anxiety scale (SAS) was used before treatment and the day before discharge. It contained 20 items reflecting subjective feelings of anxiety. Each item was divided into four grades according to the frequency of symptoms, including 15 positives and 5 negative scores (with *), and self-rating depression scale (SDS). It included two items of mental-emotional symptoms, eight items of physical disorders, two of psychomotor disorders, and eight of depressive mental disorders. The psychological situation of patients was evaluated [14].
Secondary outcome measures
It mainly includes scoring the quality of life of patients by using their quality of life scoring scale. It also evaluates their nursing satisfaction by referring to the relevant evaluation indexes of the North American Nursing Association (satisfaction = number of satisfied patients/total number ×100%).
Data statistics
The experiment results were evaluated by SPSS22.0 statistical software. The measurement data were expressed by (x̅ ± sd). The data within groups were compared by paired t-test, and those between groups were compared by independent t-test. The counting data were compared by Chi-square test. P<0.05 was statistically remarkable.
Results
This research revealed that there was no marked difference in age, course of disease, clinical stage, and tumor type between the two groups (all P>0.05), which was comparable (Table 1).
Table 1.
Comparison of general information between two groups of patients ((x̅ ± sd)/n)
| Group | Observation group | Control group | χ2/t value | P value |
|---|---|---|---|---|
| Gender | 0.337 | 0.561 | ||
| Male | 32 | 28 | ||
| Female | 22 | 26 | ||
| Age (weeks) | 57.82±5.30 | 58.01±5.10 | 0.189 | 0.851 |
| Duration of disease (months) | 10.21±2.65 | 9.87±2.91 | 0.635 | 0.527 |
| Clinical staging (n) | 0.034 | 0.853 | ||
| Stage III | 29 | 28 | ||
| Stage IV | 25 | 26 | ||
| Pathological type (n) | 0.448 | 0.930 | ||
| Squamous carcinoma | 21 | 19 | ||
| Adenocarcinoma | 29 | 32 | ||
| Small cell lung cancer | 3 | 2 | ||
| Other | 1 | 1 |
Comparison of pain scores between both groups before and after treatment
This research found that there was no obvious difference in pain scores between the two groups before treatment (P>0.05). After treatment, the scores decreased, and the observation group was superior to the control group (P<0.05) (Figure 1).
Figure 1.
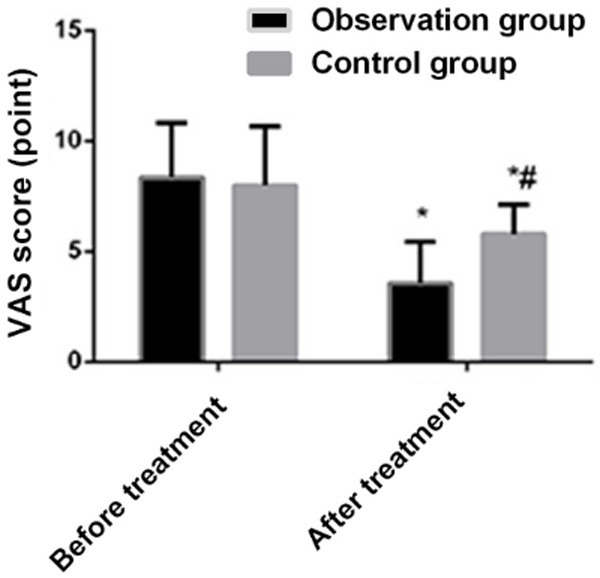
Comparison of pain scores between the two groups of patients before and after treatment. VAS: visual analogue scale. Compared with the before treatment, *P<0.001; comparison between the two groups after treatment, #P<0.001.
Comparison of anxiety and depression scores between both groups before and after treatment
This research manifested that there was no obvious difference in anxiety and depression scores between both groups before treatment. After re-evaluation, one day before discharge, the above two scores of patients in the observation group were better than those in the control group (P<0.001). It showed that EBN can reduce the negative emotional scores of patients and alleviate their psychological barriers to a certain extent (Table 2, P<0.001).
Table 2.
SAS and SDS scores of patients in both groups ((x̅ ± sd), score)
| Group | SAS score | SDS score |
|---|---|---|
| Observation group | ||
| Before treatment | 54.37±8.86 | 61.41±6.75 |
| One week after treatment | 35.64±9.55***,### | 43.63±8.29***,### |
| Control group | ||
| Before treatment | 54.63±9.85 | 59.79±7.58 |
| One week after treatment | 48.29±8.28 | 48.75±7.42 |
Note: SAS: Self-Rating Anxiety Scale; SDS: Self-Rating Depression Scale.
Compared with the Before treatment in this group;
P<0.001.
Compared with the control group one week after treatment in this group;
P<0.001.
Comparison of PSQI and QOL scores between both groups before and after treatment
This research discovered that in the sleep quality scale (SQS), there was no marked difference in PSQI and QOL scores between the two groups before treatment (P>0.05). After treatment, the scores decreased, and the observation group was superior to the control group (P<0.05) (Figures 2 and 3).
Figure 2.
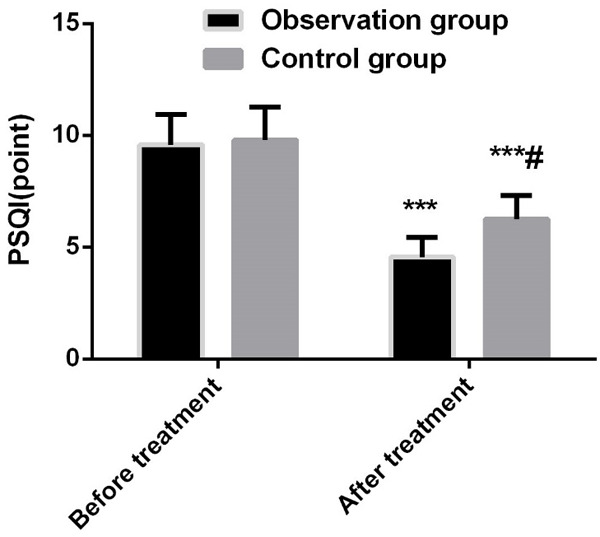
Comparison of PSQI scores between two groups of patients before and after treatment. PSQI: Pittsburgh sleep quality index. Compared with before treatment, ***P<0.001; comparison between the two groups after treatment, #P<0.001.
Figure 3.
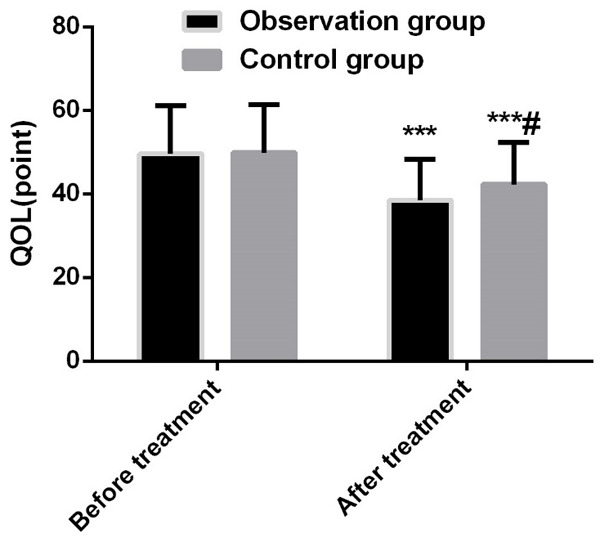
Comparison of QOL scores between two groups of patients before and after treatment. Note: QOL: quality of life. Compared with before treatment, ***P<0.001; comparison between the two groups after treatment, #P<0.001.
Comparison of nursing satisfaction between both groups
Research found that the nursing satisfaction of patients in the observation group was better than that in the control group (P<0.05), which indicated that EBN measures could improve the nursing quality and promote the sound development of medical-nursing relationship (Table 3).
Table 3.
Comparison of patient care satisfaction between both groups (n)
| Group | Very Satisfied | More Satisfied | Satisfied | Fair | Total satisfaction |
|---|---|---|---|---|---|
| Observation group | 12 | 22 | 18 | 2 | 52/54 |
| Control group | 10 | 18 | 16 | 10 | 44/54 |
| χ2 value | 4.594 | ||||
| P value | 0.032 | ||||
Discussion
LC is a familiar malignancy of the respiratory system. Its early clinical symptoms are fever, chest pain, chest tightness, and cough, which easily lead to misdiagnosis and missed diagnosis. Thus, most patients are found in the late stage when the tumor invades the peripheral nerve of the lung tissue and presents severe cancer pain [15]. Cancer pain will not only have a great impact on their health, but also aggravate their emotions of depression and anxiety, affecting their quality of life and sleep. In the end, it may lead to unbearable pain, affect patients’ treatment compliance, and release therapy and life cycle. Good nursing measures helping to reduce cancer pain is of great significance to improve the diagnosis and treatment of advanced LC patients [16,17].
This research revealed that after taking EBN measures, the cancer pain scores of LC patients in the observation group were lower than those in the control group. This may be combined with the previous research data with the content of EBN and their psychological characteristics. It effectively makes up for the universality of conventional nursing and improves the nursing measures. There were similar research reports in the past, which confirmed that EBN could improve the pain of cancer patients [18,19]. We believe that this was relevant to the application of professionals with solid theoretical knowledge and nursing skills in EBN.
SAS and SDS are two outcome measures to evaluate patients’ negative emotions, which can directly reflect their psychological state. The scores of negative emotions in the observation group were lower than those in the control group, which confirmed the effect of EBN in relieving negative emotions and actively improving the psychological state of advanced LC patients [20]. EBN has special psychological support nursing measures, nurses can implement necessary psychological support for patients and relieve their negative emotions.
As to the efficacy of EBN on sleep and quality of life of LC patients with cancerous pain, this research showed that the two in the observation group were better than those in the observation group. It may be related to EBN measures that can actively and effectively reduce pain scores and adopt a variety of nursing measures to promote patients’ sleep. It improves the treatment compliance, sleep, and quality of life of patients, confirming the previous research results [21].
Nursing satisfaction is a crucial index to assess nursing work. EBN measures strengthen communication with patients, reduce their negative emotions, and carry out omni directional personalized intervention from the ward environment, diet, and drugs. The effect of nursing, positive and effective communication was achieved, the feelings between nurses and patients were enhanced, barriers were reduced, and finally the harmony of nurse-patient relationship was promoted. Our research results also suggested that the nursing satisfaction of patients in the observation group was higher than that in the control group. There are similar research reports abroad [22].
This research also had some shortcomings. First of all, the sample size of this research was small and it was a single center study, which may lead to certain bias. During the follow-up period, the related effects after long-term nursing of patients still needs further research.
In general, the application of EBN measures in nursing of advanced LC patients with cancerous pain can effectively reduce the pain scores, relieve their negative emotions, and improve the quality of sleep and life. It can be widely used in clinical practice. However, the number of individuals was small. It was a single center study, which needs to be further confirmed by a multi-center prospective randomized controlled study with a large sample. In addition, the evaluation of the efficacy of EBN measures on advanced LC was also a vital supplement to improve clinical effectiveness.
Disclosure of conflict of interest
None.
References
- 1.McGonigle N. Lung cancer. Surgery (Oxford) 2020;38:249–254. [Google Scholar]
- 2.Kim SJ, Park CK. Impact of smoking and decreased lung function on the prognosis of female lung cancer: analysis of the Korean association of lung cancer registry. Chest. 2020;157:A243. [Google Scholar]
- 3.Lee Y, Jeon JH, Goh SH, Roh H, Yun JY, Kwon NJ, Choi JH, Yang HC, Kim MS, Lee JM, Lee GK, Han JY. The clinical impact of family history of cancer in female never-smoker lung adenocarcinoma. Lung Cancer. 2019;136:15–22. doi: 10.1016/j.lungcan.2019.07.031. [DOI] [PubMed] [Google Scholar]
- 4.Götschke J, Kahnert K, Tufman A. Die personalisierte therapie des Lungenkarzinoms. Der Pneumologe. 2019;16:69–75. [Google Scholar]
- 5.Hoy H, Lynch T, Beck M. Surgical treatment of lung cancer. Crit Care Nurs Clin North Am. 2019;31:303–313. doi: 10.1016/j.cnc.2019.05.002. [DOI] [PubMed] [Google Scholar]
- 6.Shah DR, Masters GA. Precision medicine in lung cancer treatment. Surg Oncol Clin N Am. 2020;29:15–21. doi: 10.1016/j.soc.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 7.Gül ŞK, Tepetam H, Gül HL. Duloxetine and pregabalin in neuropathic pain of lung cancer patients. Brain Behav. 2020;10:e01527. doi: 10.1002/brb3.1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mercadante S, Masedu F, Valenti M, Aielli F. Breakthrough pain in patients with lung cancer. A secondary analysis of IOPS MS study. J Clin Med. 2020;9:1337. doi: 10.3390/jcm9051337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nurwidya F, Syahruddin E, Yunus F. Pain management in lung cancer. Adv Respir Med. 2016;84:331–336. doi: 10.5603/ARM.2016.0043. [DOI] [PubMed] [Google Scholar]
- 10.Antic M, Aguinaga SR, Bloomer J. Painful fingers and toes reveal a case of non-small cell lung cancer. Chest. 2020;158:A1503–A1504. [Google Scholar]
- 11.El Meziane A, Laarej H. P3.07-08 pain management in lung cancer. J Thorac Oncol. 2018;13:S936. [Google Scholar]
- 12.Twycross A, Smith J. Have you seen the evidence-based nursing blog? Evidence-based nursing blogs: highlighting contemporary issues in nursing. Evid Based Nurs. 2017;20:29–32. doi: 10.1136/eb-2016-102563. [DOI] [PubMed] [Google Scholar]
- 13.Chander NG. Visual analog scale in prosthodontics. J Indian Prosthodont Soc. 2019;19:99–100. doi: 10.4103/jips.jips_94_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu JJ, Zhang YX, Du WS, Jiang LD, Jin RF, Yu HY, Liu JM, Han M. Effect of Qigong on self-rating depression and anxiety scale scores of COPD patients: a meta-analysis. Medicine (Baltimore) 2019;98:e15776. doi: 10.1097/MD.0000000000015776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Malinowska K. The relationship between chest pain and level of perioperative anxiety in patients with lung cancer. Pol Przegl Chir. 2018;90:23–27. doi: 10.5604/01.3001.0011.7490. [DOI] [PubMed] [Google Scholar]
- 16.He Y, Sun LY, Peng KW, Luo MJ, Deng L, Tang T, You CX. Sleep quality, anxiety and depression in advanced lung cancer: patients and caregivers. BMJ Support Palliat Care. 2020 doi: 10.1136/bmjspcare-2018-001684. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Chabowski M, Polański J, Jankowska-Polańska B, Janczak D, Rosińczuk J. Is nutritional status associated with the level of anxiety, depression and pain in patients with lung cancer? J Thorac Dis. 2018;10:2303–2310. doi: 10.21037/jtd.2018.03.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoder C, Holtzclaw A, Sarkar S. The unique role of lung cancer nurse navigators in elderly lung cancer patients. Current Geriat Rep. 2020;9:40–46. [Google Scholar]
- 19.Wang HQ, An BY, Zhou GL, Ma DY, Xin L. Study on the relieving effect of evidence-based nursing model on pain nursing of patients after liver transplantation. Minerva Med. 2020 doi: 10.23736/S0026-4806.20.06581-7. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 20.Huang F, Yi L, Xu LW, Wang L. Evidence-based nursing versus routine nursing in preventing surgical incision infection. Int J Clin Exp Med. 2019;12:8863–8870. [Google Scholar]
- 21.Kalmbach DA, Sen S, Drake CL. Poor sleep is a health crisis for physicians and nurses. Sleep Medicine. 2020;67:256–257. doi: 10.1016/j.sleep.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 22.Zhang HS, Chen CX. Study on the effect of evidence-based nursing model on quality of life and nursing satisfaction of patients with severe acute pancreatitis. Panminerva Med. 2020 doi: 10.23736/S0031-0808.20.03914-2. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]


