Abstract
Objective: To explore the advantages of continuous nursing for patients with advanced esophageal cancer after esophageal stent implantation. Methods: A total of 48 patients with advanced esophageal cancer who successfully received esophageal stent implantation in the Department of Oncology, at the First People’s Hospital Affiliated with Shanghai Jiao Tong University were divided into the control group (24 cases, receiving routine discharge guidance) and the experimental group (24 cases, receiving continuous nursing through the issuance of a home nursing instruction handbook, dietary transition guidance after discharge, nutrition and food evaluation, and guidance on daily activities, medication, and prevention of complications, etc.). The quality of life (EORTCQLQ-C30), nutritional status (MNA score and the levels of hemoglobin (Hb), serum total protein (TP) and albumin (Alb)), anxious/depressive mental state (HAMA, HAMD), complications and satisfaction were compared between the two groups. Results: EORTCQLQ-C30, HAMA and HAMD scores of the two groups three months after discharge were lower than those before discharge, and those of the experimental group were lower than those of the control group (all P<0.05). The MNA score and the levels of Hb, TP and Alb in the experimental group three months after discharge had no significant changes compared with those before discharge (all P>0.05), while the MNA score and the levels of Hb, TP and Alb in the control group three months after discharge were lower than those before discharge and those in the experimental group (all P<0.05). The experimental group’s nursing satisfaction was higher than that of the control group (P<0.05). Conclusion: The application of continuous nursing in patients with advanced esophageal cancer after esophageal stent implantation can effectively improve the patients’ adverse mental state, nutritional status and quality of life.
Keywords: Advanced esophageal cancer, esophageal stent implantation, continuous nursing, quality of life, nutritional status
Introduction
The early symptoms of esophageal cancer are not obvious, and most patients are in the middle and late stages when they are diagnosed. Anatomically, the esophageal lymphatic tissue is abundant, and the structure lacks a serous membrane, so patients are more likely to have lymph node metastasis in the early stage and lose the opportunity for surgical resection [1,2]. Patients with esophageal cancer have obvious dysphagia and low nutrient absorption, so alleviating the clinical symptoms and improving the patients’ nutritional status are the main goals for treating advanced esophageal cancer [3]. Currently, esophageal stent implantation is widely used in the treatment of advanced esophageal cancer to improve patients’ dysphagia [4,5]. However, due to the lack of professional care after discharge, patients are prone to nutritional deficiency, and the incidence of complications also increases [6,7].
Continuous nursing refers to the extended out-of-hospital care services that use modern information tools to provide medical care services to patients after discharge [8]. Continuous nursing outside the hospital can ensure that patients receive similar nursing services outside the hospital. Some studies [9] have pointed out that the implementation of continuous nursing for diabetic patients can significantly strengthen blood sugar control and improve patient compliance with medications. However, there is no authoritative guideline on continuous nursing at present, and there is no report on the application of continuous clinical nursing in patients with advanced esophageal cancer after esophageal stent implantation. Therefore, this study examines the effect of continuous nursing in patients with advanced esophageal cancer after esophageal stent implantation, aiming to provide clinical reference.
Material and methods
General information
From May 2019 to May 2020, 48 patients with advanced esophageal cancer who underwent esophageal stent implantation in the Department of Oncology, at the First People’s Hospital Affiliated with Shanghai Jiao Tong University were selected and randomly divided into two groups. Our hospital’s ethics committee approved this study, and all patients signed an informed consent form. Inclusion criteria: Those who were diagnosed with esophageal cancer from the results of relevant clinical examinations and laboratory examinations, and are in the advanced stage; Those who need esophageal stent treatment and the esophageal stent placement is successful; Those who can cooperate with the research and follow-up; Patients and Families members will communicate on WeChat; Those with an estimated survival time >3 months; Those who have signed informed consent. Exclusion criteria: Patients with other serious diseases; Patients with mental illness or communication disorders; Those who participate in other studies simultaneously; Patients who cannot tolerate esophageal stent implantation or have contraindications to surgery; Patients with malignant tumors, etc.
Methods
The two groups of patients received esophageal stent implantation during hospitalization, and the esophageal stent was successfully placed. Local perfusion chemotherapy was performed 5 to 7 days after stent implantation, including cisplatin 80-100 mg/m2, fluorouracil 750-1000 mg/m2 and pirarubicin 14-25 mg/m2. Four weeks is one treatment cycle and patients needed four consecutive cycles of chemotherapy. Patients in the control group were given routine discharge guidance 3-5 days before discharge. Routine discharge guidance includes explaining the formation of the disease and subsequent treatments, instructing the patients to eat liquid food within one week of discharge, keeping the food at 40°C, and then gradually transiting to normal, eating in a sitting position, standing or sitting for 1 hour after eating, avoiding high intensity exercise, and raising the head of the bed 20-30° while sleeping. Patients in the experimental group were given continuous nursing from 3-5 days before discharge to three months after discharge [10,11]: The continuous nursing group was composed of clinicians and nurses of different levels. WeChat groups and QQ groups were established, and patients and their families were invited to join the group; A home nursing instruction handbook about nursing after an esophageal stent implantation was formulated by the continuous nursing group and was issued to patients before discharge; Focus was on dietary transition, enteral nutrition and food comparasions were explained to patients and their families at the time of discharge; Health education materials were given out on postoperative diet, activities, medication and prevention of complications, all of which were distributed to patients in the WeChat group and QQ groups once every two weeks. Patients’ diet, mental and physical health status were followed up and recorded, and nursing guidance was given according to patients’ actual situation once every two weeks.
Outcome measures
Primary outcome measures
All patients filled out the following scales at the time of discharge and three months after discharge.
Quality of life: The European Organization for Research and Treatment of Cancer Core Quality of Life Scale (EORTCQLQ-C30) was used to assess life quality [12]. The higher the score, the worse the quality of life.
Nutritional status: Mini-Nutritional Assessment Scale (MNA) was used to evaluate patients’ nutritional status [13]. The higher the score, the better the nutritional status. Three ml venous blood was collected at discharge and three months after discharge, respectively. The serum was separated after centrifugation. The levels of hemoglobin (Hb), serum total protein (TP), and albumin (Alb) were measured using an automatic biochemical analyzer (Shenzhen Cooper Biotechnology Co., Ltd., origin: China).
Psychological status: Hamilton Anxiety and Depression Scale (HAMA, HAMD) were used to asses patients [14,15]. The higher the score, the more serious the degree of anxiety and depression.
Secondary outcome measures
Postoperative complications, such as gastroesophageal reflux, esophageal stent displacement, and nutrition loss were recorded and analyzed. The total incidence of adverse reactions = cases of adverse reactions/total cases ×100%.
The self-made satisfaction questionnaire was used to record the satisfaction of the two groups of patients with nursing. The full score of the two groups was 100 points. The patients with more than 90 points were satisfied, the patients with 60-89 points were generally satisfied, and the patients with less than 60 points were dissatisfied. Satisfaction = (satisfied + generally satisfied) cases/total cases ×100%.
Stastical analysis
SPSS 22.0 software was used for data processing, and mean ± standard deviation was used to represent the measurement data. An independent sample t-test was used for comparison between the groups at the same time point. Paired sample t-test was used for comparison within groups at different time points. The count data was expressed as a percentage. Chi-square test or Fisher exact probability methods were adopted. The difference was statistically significant when P<0.05.
Results
Baseline data
There were no patients who died in either group during hospitalization and within three months of follow-up. There was no significant difference in the general information between the two groups (all P>0.05), and as such patients were comparable between the groups. See Table 1.
Table 1.
Comparison of baseline data between the two groups (x̅ ± sd)
| Indicators | Control group (n=24) | Experimental group (n=24) | χ2/t | P |
|---|---|---|---|---|
| Gender (n) | 0.097 | 0.755 | ||
| Male | 16 | 17 | ||
| Female | 8 | 7 | ||
| Age (year) | 56.8±5.9 | 55.8±6.9 | 0.540 | 0.592 |
| Course of disease (year) | 2.29±1.04 | 2.44±1.19 | 0.465 | 0.644 |
| TNM staging (n) | 0.751 | 0.386 | ||
| Stage III | 13 | 10 | ||
| Stage IV | 11 | 14 | ||
| Tumor location (n) | 0.829 | 0.661 | ||
| Superior segment | 8 | 10 | ||
| Middle piece | 10 | 7 | ||
| Lower part | 6 | 7 | ||
| Stooler grading (n) [16] | 1.778 | 0.182 | ||
| Grade III | 20 | 16 | ||
| Grade IV | 4 | 8 | ||
| Pathological type (n) | 0.772 | 0.680 | ||
| Squamous cell carcinoma | 18 | 20 | ||
| Adenocarcinoma | 4 | 2 | ||
| Adenosquamous carcinoma | 2 | 2 | ||
| Preoperative Hb (g/L) | 88.29±5.50 | 88.54±5.20 | 0.162 | 0.872 |
| Previous treatment history (n) | 1.244 | 0.537 | ||
| None | 4 | 5 | ||
| Chemotherapy | 14 | 16 | ||
| Radiotherapy combined with chemotherapy | 6 | 3 | ||
| Education level (n) | 0.087 | 0.768 | ||
| Junior high school and below | 15 | 14 | ||
| Senior high school and above | 9 | 10 |
Quality of life (EORTCQLQ-C30 score)
Three months after discharge, the EORTCQLQ-C30 scores of the two groups were lower than those before discharge, and those of the experimental group were significanly lower (all P<0.001). See Table 2.
Table 2.
Comparison of the EORTCQLQ-C30 score between the two groups ((x̅ ± sd), points)
| Groups | Before discharge | Three months after discharge | t | P |
|---|---|---|---|---|
| Control group (n=24) | 53.67±2.83 | 42.68±1.98 | 15.588 | <0.001 |
| Experimental group (n=24) | 53.71±2.79 | 36.52±1.56 | 26.345 | <0.001 |
| t | 0.049 | 11.972 | ||
| P | 0.961 | <0.001 |
Note: EORTCQLQ-C30: quality of life.
Nutritional status (MNA score)
Three months after discharge, the MNA scores of the experimental group had no significant changes compared with those before discharge (all P>0.05), and the MNA scores of the control group three months after discharge were lower than those before discharge and those of the experimental group (all P<0.05). See Table 3.
Table 3.
Comparison of the MNA score of nutritional status between the two groups ((x̅ ± sd), points)
| Groups | Time | Nutrition screening | General assessment | Total score |
|---|---|---|---|---|
| Control group (n=24) | Before discharge | 12.67±1.04 | 14.53±1.68 | 27.16±1.59 |
| Three months after discharge | 10.52±0.89* | 12.83±1.37* | 23.66±1.18* | |
| Experimental group (n=24) | Before discharge | 12.71±1.02 | 14.49±1.71 | 27.09±1.62 |
| Three months after discharge | 12.58±0.91# | 14.29±1.64# | 26.71±1.49# |
Note: Compared with the same group before discharge;
P<0.05.
Compared with the control group 3 months after discharge;
P<0.05.
MNA: nutritional status.
Nutrition indicators
The levels of Hb, TP and Alb in the experimental group 3 months after discharge were not significantly changed from those before discharge (all P>0.05), and the Hb, TP and Alb levels in the control group three months after discharge were lower than those before discharge and in the experimental group (all P<0.05), as shown in Table 4.
Table 4.
Comparison of nutritional indicators between the two groups before and after the intervention (g/L, (x̅ ± sd))
| Groups | Time | Hb | TP | Alb |
|---|---|---|---|---|
| Control group (n=24) | Before discharge | 108.29±5.50 | 61.30±5.24 | 38.88±4.22 |
| Three months after discharge | 104.44±5.37* | 57.87±4.22* | 36.07±4.10* | |
| Experimental group (n=24) | Before discharge | 108.54±5.20 | 61.31±5.19 | 38.46±3.96 |
| Three months after discharge | 109.22±5.68# | 61.63±5.56# | 39.23±3.67# |
Note: compared with the same group before discharge;
P<0.05.
Compared with the control group 3 months after discharge;
P<0.05.
Hb: hemoglobin; TP: serum total protein; Alb: albumin.
Psychological state
Three months after discharge, HAMA and HAMD scores of the two groups decreased and those of the experimental group were lower (all P<0.05), as shown in Table 5.
Table 5.
HAMA and HAMD scores of two groups before and after the intervention (x̅ ± sd)
| Groups | Time | HAMA Score | HAMD Score |
|---|---|---|---|
| Control group (n=24) | Before discharge | 7.83±1.37 | 7.96±1.27 |
| Three months after discharge | 6.43±1.11* | 6.86±1.34* | |
| Experimental group (n=24) | Before discharge | 7.68±1.53 | 8.04±1.56 |
| Three months after discharge | 5.22±1.32*,# | 5.77±1.44*,# |
Note: compared with the same group before discharge;
P<0.05.
Compared with the control group 3 months after discharge;
P<0.05.
HAMA, HAMD: anxious/depressive mental state.
Postoperative complications
There was no significant difference in the incidence of postoperative complications between the two groups (P>0.05). See Table 6.
Table 6.
Comparison of the incidence of postoperative complications between the two groups 3 months after discharge n (%)
| Groups | Gastroesophageal reflux | Esophageal stent displacement | Loss of nutrition | Total incidence |
|---|---|---|---|---|
| Control group (n=24) | 1 (4.17) | 1 (4.17) | 3 (12.50) | 5 (20.83) |
| Experimental group (n=24) | 1 (4.17) | 0 (0.00) | 0 (0.00) | 1 (4.17) |
| χ2 | 0.522 | 0.000 | 1.422 | 1.714 |
| P | 0.470 | 1.000 | 0.233 | 0.190 |
Satisfaction
The patients’ satisfaction with nursing care in the experimental group was 95.83% (18 cases were satisfied, 5 cases were generally satisfied), which was higher than 75.00% (12 cases were satisfied, 6 cases were generally satisfied) of the control group (P<0.05), as shown in Figure 1.
Figure 1.
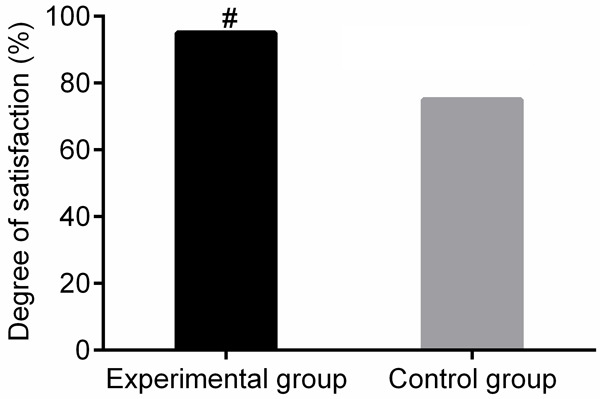
Comparison of satisfaction with nursing of two groups of patients. Compared with the control group, #P<0.05.
Discussion
Surgery is the primary method for treating esophageal cancer, but some patients still have difficulty eating after surgery. The emergence of esophageal stent technology has mostly solved this problem, which can quickly resolve esophagostenosis, restore eating and improve nutritional status [17]. However, due to the influence of many factors, such as severe postoperative complications, patients’ adverse psychological status of being extremely afraid of cancer, the effects of late radiotherapy, catheterization trauma and discomfort caused by catheters, patients will have depression, anxiety and other emotions, which affects the recovery of the disease [18]. Therefore, during the entire treatment and postoperative recovery process, high-quality nursing services are essential to promote postoperative rehabilitation.
Discharge is a very vulnerable period for patients, and more than half of the patients have medical problems during this period [19]. Continuous nursing is a new nursing concept proposed in recent years, as an extended nursing service from the hospital to the family [20]. Continuous nursing has only been carried out for more than ten years. Although domestic continuous nursing research has covered all kinds of clinical system diseases, it is more common in heart disease and respiratory system disease. There are few studies on continuous nursing of esophageal cancer, and it is mainly about the nursing research after radical resection of early esophageal cancer. However, there is no report on the clinical research on continuous nursing after esophageal stent implantation.
This study showed that the MNA scores and Hb, TP, Alb levels of the experimental group did not change significantly three months after discharge compared with those before discharge. The MNA scores and Hb, TP, Alb levels of the control group three months after discharge were lower than those before discharge and those of the experimental group. It was also observed that the EORTCQLQ-C30 score of the experimental group was lower than that of the control group three months after discharge, indicating that continuous nursing can significantly improve the postoperative nutritional status of patients with advanced esophageal cancer and improve the postoperative quality of life. It is speculated that continuous nursing’s specific content is related to the patient’s condition, mainly focusing on diet, patients’ psychological changes, medication, prevention of complications, etc. Members of the continuous nursing group provide patients with post-discharge nursing guidance through telephone, WeChat, etc. The team members have vibrant clinical and nursing experience. They further standardize continuous nursing, carry out individual assessments for different patients, and conduct appropriate intervention, which will help improve the patients’ nutritional status and improve the quality of life of patients [21].
The results of this study showed that the HAMA and HAMD scores of the experimental group were lower than those of the control group three months after discharge, and the nursing satisfaction of the experimental group was higher than that of the control group, suggesting that continuous nursing can significantly improve the unhealthy mood of patients with advanced esophageal cancer after discharge, and improve the nursing satisfaction. Maybe it is because continuous nursing guarantees the continuity of nursing work. Patients after discharge can still receive nursing services similar to those during their stay in the hospital, which helps patients increase their confidence in overcoming disease and is, therefore, conducive to improving patients’ unhealthy psychology. Wimberly et al. also pointed out that the implementation of continuous nursing can improve patients’ unhealthy psychology regarding malignant tumors [22]. In terms of complications, the experimental group’s complication rate was slightly lower than that in the control group, indicating that continuous nursing can reduce the complication rate in patients with advanced esophageal cancer after esophageal stent implantation to a certain extent. However, there was no difference with conventional out-of-hospital guidance, which may be related to this study’s small sample size. In the later stage, it is still necessary to expand the sample size and adopt more in depth multi-center clinical research to confirm the application advantages of continuous nursing in patients with advanced esophageal cancer after esophageal stent implantation.
In conclusion, the application of continuous nursing in patients with advanced esophageal cancer after esophageal stent implantation can effectively improve patients’ poor mental state and nutritional status after discharge and improve their quality of life.
Acknowledgements
This work was supported by the Natural Science Research Key Project of Anhui Provincial Department of Education (KJ2019A1272).
Disclosure of conflict of interest
None.
References
- 1.Domper Arnal MJ, Ferrández Arenas Á, Lanas Arbeloa Á. Esophageal cancer: risk factors, screening and endoscopic treatment in Western and Eastern countries. World J Gastroenterol. 2015;21:7933–7943. doi: 10.3748/wjg.v21.i26.7933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Short MW, Burgers KG, Fry VT. Esophageal cancer. Am Fam Physician. 2017;95:22–28. [PubMed] [Google Scholar]
- 3.Jordan T, Mastnak DM, Palamar N, Kozjek NR. Nutritional therapy for patients with esophageal cancer. Nutr Cancer. 2018;70:23–29. doi: 10.1080/01635581.2017.1374417. [DOI] [PubMed] [Google Scholar]
- 4.Zhang Y, Zhou M, Bai L, Han R, Lv K, Wang Z. Radiofrequency ablation combined with esophageal stent in the treatment of malignant esophageal stenosis: a single-center prospective study. Oncol Lett. 2018;16:3157–3161. doi: 10.3892/ol.2018.9046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ziaja D, Stasiów B, Sznapka M, Domalik J, Kuczmik W, Ziaja K, Chudek J. Adaptation of endovascular technique of self-expandable metal esophageal stent implantation in palliative treatment of malignant dysphagia in the course of esophageal and bronchial cancers: a one-center study. Adv Clin Exp Med. 2020;29:1363–1366. doi: 10.17219/acem/111810. [DOI] [PubMed] [Google Scholar]
- 6.Borggreve AS, Kingma BF, Domrachev SA, Koshkin MA, Ruurda JP, van Hillegersberg R, Takeda FR, Goense L. Surgical treatment of esophageal cancer in the era of multimodality management. Ann N Y Acad Sci. 2018;1434:192–209. doi: 10.1111/nyas.13677. [DOI] [PubMed] [Google Scholar]
- 7.Kelly RJ. Emerging multimodality approaches to treat localized esophageal cancer. J Natl Compr Canc Netw. 2019;17:1009–1014. doi: 10.6004/jnccn.2019.7337. [DOI] [PubMed] [Google Scholar]
- 8.Capasso J. Continuing care for older adults through and beyond a pandemic. Front Health Serv Manage. 2020;37:20–26. doi: 10.1097/HAP.0000000000000097. [DOI] [PubMed] [Google Scholar]
- 9.Turcotte LA, Perlman CM, Fries BE, Hirdes JP. Clinical predictors of protracted length of stay in ontario complex continuing care hospitals. BMC Health Serv Res. 2019;19:218. doi: 10.1186/s12913-019-4024-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kelly P, Deane F, Baker A, Byrne G, Degan T, Osborne B, Townsend C, McKay J, Robinson L, Oldmeadow C, Lawson K, Searles A, Lunn J. Study protocol the continuing care project: a randomised controlled trial of a continuing care telephone intervention following residential substance dependence treatment. BMC Public Health. 2020;20:107. doi: 10.1186/s12889-020-8206-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rubinsky AD, Ellerbe LS, Gupta S, Phelps TE, Bowe T, Burden JL, Harris AHS. Outpatient continuing care after residential substance use disorder treatment in the US Veterans Health Administration: facilitators and challenges. Subst Abus. 2018;39:322–330. doi: 10.1080/08897077.2017.1391923. [DOI] [PubMed] [Google Scholar]
- 12.Carcamo M, Campo V, Behrmann D, Celedón C, Alvear Á, Vásquez P, Araya C. Head and neck cancer: validation of the QLQ-H&N35 quality of life questionnaire. Rev Med Chil. 2018;146:578–584. doi: 10.4067/s0034-98872018000500578. [DOI] [PubMed] [Google Scholar]
- 13.Soysal P, Veronese N, Arik F, Kalan U, Smith L, Isik AT. Mini nutritional assessment scale-short form can be useful for frailty screening in older adults. Clin Interv Aging. 2019;14:693–699. doi: 10.2147/CIA.S196770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zimmerman M, Martin J, Clark H, McGonigal P, Harris L, Holst CG. Measuring anxiety in depressed patients: a comparison of the Hamilton anxiety rating scale and the DSM-5 anxious distress specifier interview. J Psychiatr Res. 2017;93:59–63. doi: 10.1016/j.jpsychires.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 15.Raimo S, Trojano L, Spitaleri D, Petretta V, Grossi D, Santangelo G. Psychometric properties of the hamilton depression rating scale in multiple sclerosis. Qual Life Res. 2015;24:1973–1980. doi: 10.1007/s11136-015-0940-8. [DOI] [PubMed] [Google Scholar]
- 16.Huang FL, Yu SJ. Esophageal cancer: risk factors, genetic association, and treatment. Asian J Surg. 2018;41:210–215. doi: 10.1016/j.asjsur.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 17.Steenhagen E, van Vulpen JK, van Hillegersberg R, May AM, Siersema PD. Nutrition in peri-operative esophageal cancer management. Expert Rev Gastroenterol Hepatol. 2017;11:663–672. doi: 10.1080/17474124.2017.1325320. [DOI] [PubMed] [Google Scholar]
- 18.Wang TY, Chen VC, Yang YH, Chen CY, Lee CP, Wu SI. The effects of anxiety on the receipt of treatments for esophageal cancer. Psychooncology. 2019;28:31–38. doi: 10.1002/pon.4903. [DOI] [PubMed] [Google Scholar]
- 19.Passetti LL, Godley MD, Kaminer Y. Continuing care for adolescents in treatment for substance use disorders. Child Adolesc Psychiatr Clin N Am. 2016;25:669–684. doi: 10.1016/j.chc.2016.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grant M. Continuing care. Am J Nurs. 2019;119:10. doi: 10.1097/01.NAJ.0000580172.58441.7c. [DOI] [PubMed] [Google Scholar]
- 21.Su X, Zhong MH, Ye XM, Zhen L, Yin XX, Qin F, Zhu ML, Kuang YY, Wang HZ. Effects of evidence-based continuing care bundle on health outcomes in rectal cancer patients with temporary stomas: a multicenter randomized controlled trial. Cancer Nurs. 2021;44:223–234. doi: 10.1097/NCC.0000000000000762. [DOI] [PubMed] [Google Scholar]
- 22.Wimberly AS, Hyatt JM, McKay JR. Effect of continuing care for people with cocaine dependence on criminal justice sentences. Behav Sci Law. 2018;36:116–129. doi: 10.1002/bsl.2330. [DOI] [PMC free article] [PubMed] [Google Scholar]


