Abstract
Background: In this case report, we aimed to describe the multimodal imaging characteristics and the successful treatment of idiopathic retinal vasculitis, aneurysms, and neuroretinitis (IRVAN) syndrome in a 39-year-old man. Case presentation: His both eyes were diagnosed with IRVAN syndrome via multimodal imaging, including fundus color photograph, multicolor imaging, infrared ray, fundus autofluorescence, fundus fluorescence angiography and optical coherence tomography angiography. Both eyes were treated with vitrectomy and laser photocoagulation. The treatment was effective. Eighteen months after discharge, the patient had visual acuity of 20/20 in both eyes. Conclusions: This case report demonstrates that vitrectomy and retinal laser photocoagulation can be successful in treating a patient with IRVAN syndrome in both eyes.
Keywords: IRVAN syndrome, multimodal imaging, vitrectomy, retinal laser photocoagulation
Introduction
Kincaid and Schatz were the first to report the association between bilateral retinal arteritis and multiple aneurysmal dilatations in 1983 [1]. It is a retinal disorder without a clear cause. The concept of IRVAN (idiopathic retinal vasculitis, aneurysms, and neuroretinitis) was first proposed in 1995 [2]. The main fundus manifestations of IRVAN include multiple aneurysmal dilatations, retinal vasculitis and neuroretinitis at the bifurcation of arteries and its secondary fundus manifestations are peripheral capillary perfusion disorder, retinal neovascularization and macular exudation [2].
IRVAN syndrome can be classified into five stages. Stage I, macroaneurysms, exudation, neuroretinitis and retinal vasculitis; stage II, capillary non-perfusion, as shown by fluorescein angiography; stage III, posterior segment neovascularization of the disc or elsewhere and/or vitreous hemorrhage; stage IV, anterior segment neovascularization; and stage V, neovascular glaucoma [3]. Existing treatment options include oral glucocorticosteroids, intravitreal VEGF inhibitor, pars plana vitrectomy, and laser panretinal photocoagulation [4,5]. It is generally believed that patients at stage I can be closely observed without treatment. Once there is no perfusion area of peripheral capillaries, laser treatment should be carried out immediately. Patients at stage II and stage III need laser treatment in time, and the treatment effect for patients above stage III is poor. About half of the patients still have severe visual loss after treatment. When vitreous hemorrhage appeared, vitrectomy combined with retinal laser should be used. We have successfully treated a man with IRVAN.
Case presentation
The study was approved by the Ethics Committee of the Affiliated Hospital of Weifang Medical College. The informed consent was signed by the patient. A 39-year-old man had progressive painless diminution of vision in right eye over two months. The visual acuity was hand motion in right eye and 20/20 in left eye. The patient had no history of any systemic diseases.
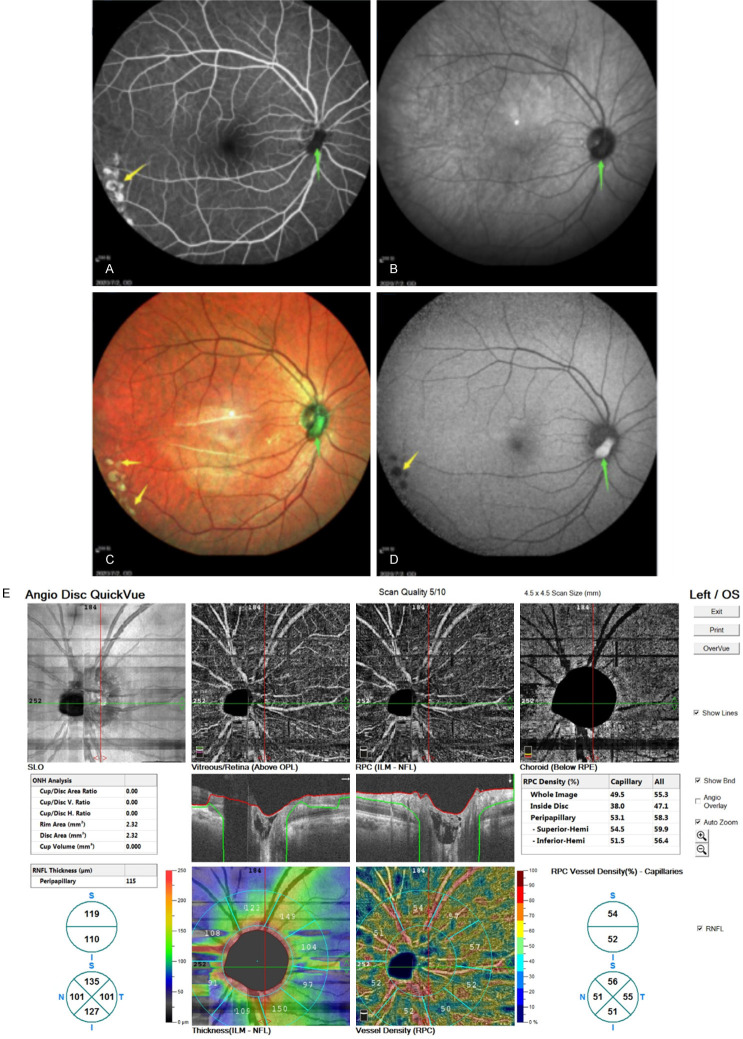
The patients underwent various imaging examinations of his left eye, including fundus color photograph (Figure 1A), multicolor imaging (MCI, Figure 1B), infrared ray (IR, Figure 1C) and fundus autofluorescence (FAF, Figure 1D). They all suggested membranous hyperplasia on the nasal side of the optic disc (green arrows), scattered hemorrhages in retinal posterior pole (red arrows), and multiple aneurysmal dilatations in the superior and inferior temporal retinal arteries of the retina (yellow arrows). The fundus fluorescence angiography (FFA) showed that the intensity of dye leakage through the walls of optic papillae increased proportionally as time progressed, indicating neovascularization membrane on the nasal side of the optic papillae (green arrows), multiple aneurysmal dilatations at the retinal arteries (yellow arrows) and extensive peripheral retinal nonperfusion areas (blue arrows) before the retinal laser photocoagulation (Figure 2). Therefore, the left eye was diagnosed as stage II IRVAN syndrome. The left eye was treated twice with retinal laser photocoagulation. Although no indication of IRVAN syndrome was found in the right eye before operation due to vitreous hemorrhage, superior temporal aneurysms were found during vitrectomy. The right eye was diagnosed as stage III IRVAN syndrome, and it was performed with retinal laser photocoagulation during vitrectomy.
Figure 1.
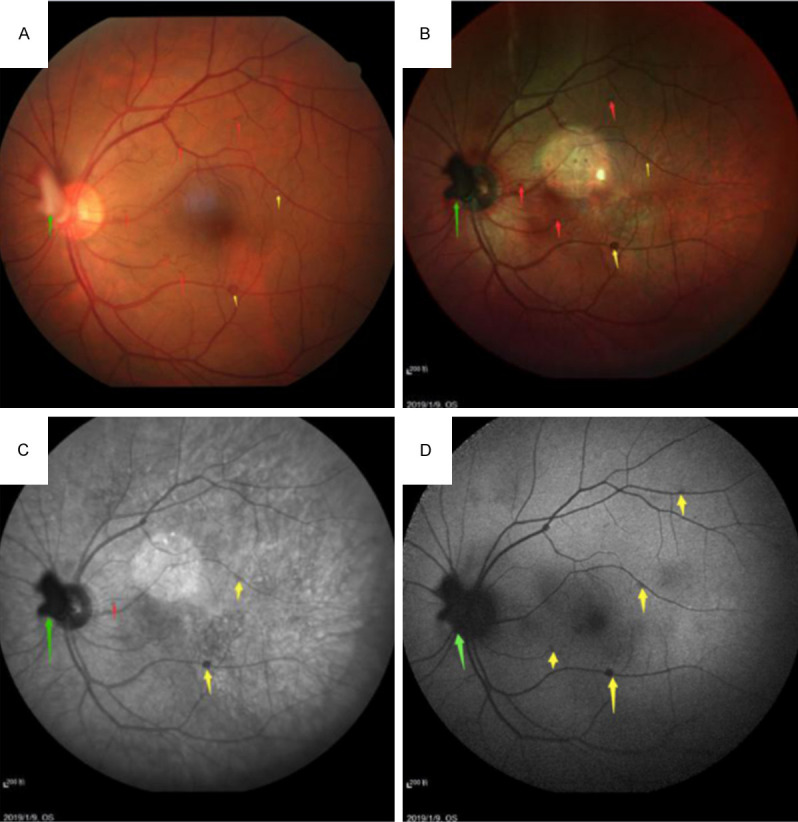
The fundus color photograph (A), MCI (B), IR (C) and FAF (D) of left eye showing presence of membranous hyperplasia (green arrows), hemorrhages (red arrows), multiple aneurysmal dilatations (yellow arrows).
Figure 2.
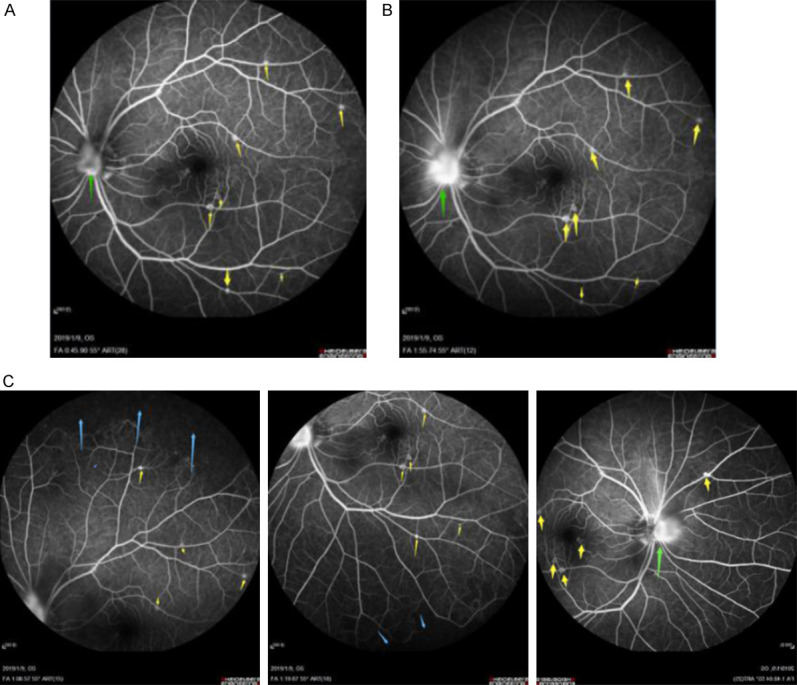
The left eye FFA demonstrates that multiple aneurysmal dilatations (yellow arrows) at retina, the hyperfluorescence leakage (green arrows) is increased compared the early phase (A) and the late phase (B) and non-perfusonareas (blue arows) at peripheral retina (C).
When the patient was discharged from the hospital, the visual acuity of the right eye reached 20/40 and was corrected to 20/20. The FFA of left eye showed that aneurysms had shrunk in the retina (yellow arrows) and the panretinal photocoagulation laser scars were present in the periphery (orange arrows) (Figure 3). However, the patient’s left eye progressed to stage III IRVAN syndrome after a month. There was sudden and vitreous hemorrhage in the vision. We performed vitrectomy and laser photocoagulation of the retina at the left eye during the operation. Its visual acuity reached 20/100 and was corrected to 20/20 when he was discharged.
Figure 3.
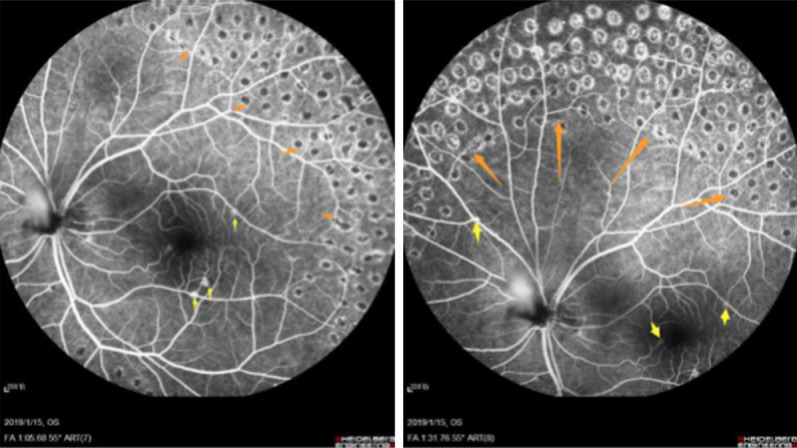
The FFA of left eye showed the aneurysms (yellow arrows) and the panretinal photocoagulation laser scars (orange arrows).
After one year and a half of follow-up, we found that the left eye was in a stable condition by comparing the patient’s optical coherence tomography angiography (OCTA) and FFA (including images taken before the first retinal laser photocoagulation, after the vitrectomy and one and a half year follow-up). We observed that the high blood flow signal of the superficial glomerular vascular membrane in OCTA decreased (Figure 4, yellow arrows) after treatment by three times (Figure 4A). Meanwhile, by comparing the OCTA of superficial and deep retinal blood flow signal, we found that macular aneurysm only existed in the superficial OCTA (Figure 4). The right eye’s last IR (Figure 5B), MCI (Figure 5C), FAF (Figure 5D) and FFA (Figure 5A) showed that the right eye was basically normal except for the membranous hyperplasia (green arrows) of the optic disc and the old laser scars (orange arrows) (Figure 5). And the right eye’s HD OCTA (Figure 5E) showed that the membranous hyperplasia was stable and without the high flow signal after treatment. We compared the FFA of left eye three times (before the first retinal laser photocoagulation, after the vitrectomy and at one and a half year follow-up), and found that the aneurysm had basically disappeared (Figure 6).
Figure 4.
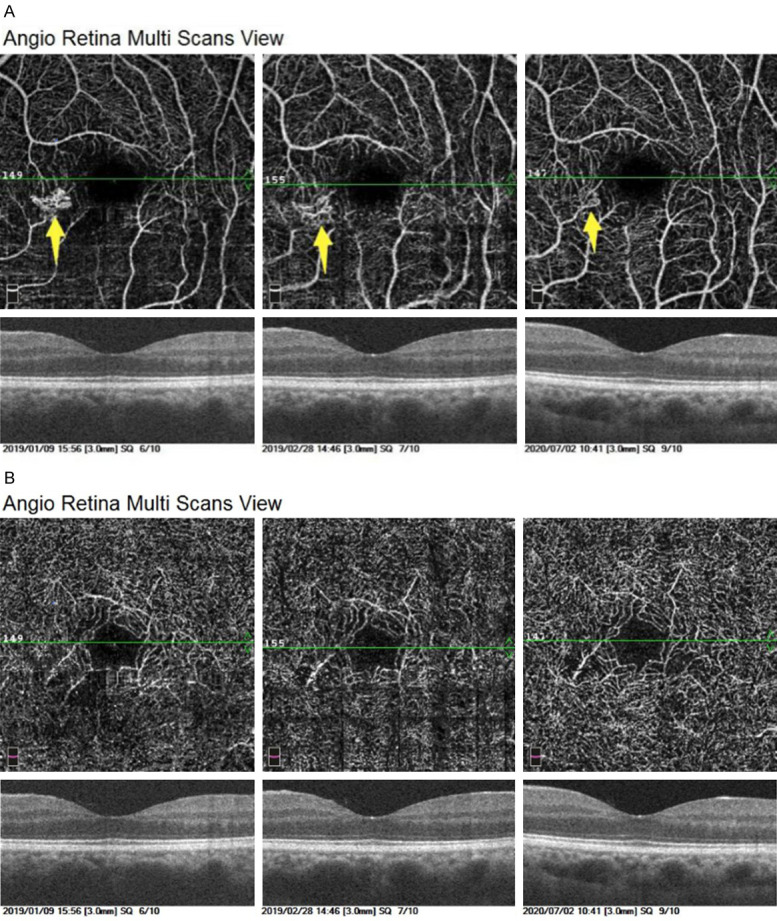
The OCTA’s superficial (A) showed macular aneurysm (yellow arrows) and decreased high blood flow signal of the superficial glomerular vascular membrane. In comparison, OCTA’s deep (B) showed no high blood flow signal.
Figure 5.
The FFA (A), last IR (B), MCI (C), and FAF (D) of right eye showed that the membranous hyperplasia (green arrows) of the optic disc and the old laser scars (orange arrows). And HD OCTA (E) of the right eye showed that the membranous hyperplasia was stable and without the high flow signal after treatment.
Figure 6.
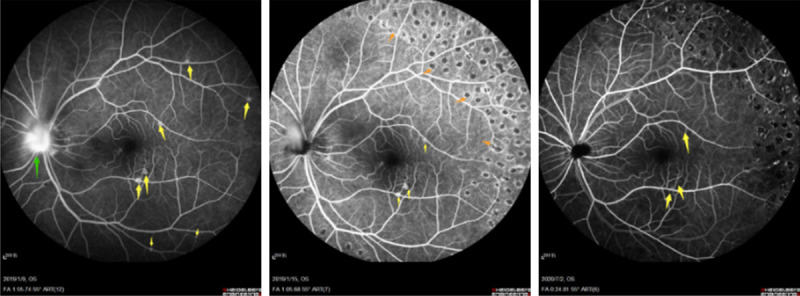
We compared the left eye’s FFA three times (before the first retinal laser photocoagulation, after the vitrectomy and at one and a half year follow-up) and found that the aneurysm had basically disappeared.
Discussion
IRVAN syndrome is a rare retinal vasculitis. It is rare with the characteristics of general vasculitis features, including retinal vasculitis, irregular vessel diameter, perivascular sheath, etc. [6]. IRVAN syndrome is a rare idiopathic entity (especially in Asia) that most commonly presents in adults and most often in young healthy women [7].
Many treatments have been used for IRVAN syndrome, and their efficacies are different. Intravitreal injections of anti-VEGF agents, bevacizumab and ranibizumab, have achieved favorable results [5,8]. Samuel et al. have found that neovascularization and subsequent vitreous hemorrhage and neovascular can be prevented by panretinal photocoagulation when there is widespread ischemia of the retina [3,9]. Laser photocoagulation is an effective treatment to control macroanurysm and ischemia, especially for patients above stage II [3,10]. Photocoagulation of the photoreceptors allows more oxygen to diffuse from the choroid to the inner retina [11].
In this case, the patient’s condition was complicated. At first, the right eye of the patient underwent vitrectomy and retinal laser photocoagulation because of vitreous hemorrhage, and at the same time, we found that the retina of the left eye also showed IRVAN syndrome, so we gave the left eye two times of panretinal laser photocoagulation. Unfortunately, vitreous hemorrhage also occurred in the left eye shortly after discharge, so we had to perform vitrectomy and retinal laser photocoagulation in the left eye. Although the final binocular visual acuity of the patient was 20/20 and was maintained for one and a half year after treatment, vitreous hemorrhage may not occur if sufficient retinal laser treatment had been given to the left eye at an early stage.
In conclusion, multimodal imaging features of IRVAN syndrome observed in this case report may help practitioners in the field gain deeper understanding and obtain more accurate diagnosis of this elusive disease. In addition, the patient’s stable condition in both eyes after one and a half year follow-up suggests that vitrectomy and retinal laser photocoagulation could be successful in treating patients with IRVAN syndrome.
Disclosure of conflict of interest
None.
References
- 1.Kincaid J, Schatz H. Bilateral retinal arteritis with multiple aneurysmal dilatations. Retina. 1983;3:171–178. doi: 10.1097/00006982-198300330-00005. [DOI] [PubMed] [Google Scholar]
- 2.Chang TS, Aylward GW, Davis JL, Mieler WF, Oliver GL, Maberley AL, Gass JD. Idiopathic retinal vasculitis, aneurysms, and neuro-retinitis. Retinal vasculitis study. Ophthalmology. 1995;102:1089–1097. doi: 10.1016/s0161-6420(95)30907-4. [DOI] [PubMed] [Google Scholar]
- 3.Samuel MA, Equi RA, Chang TS, Mieler W, Jampol LM, Hay D, Yannuzzi LA. Idiopathic retinitis, vasculitis, aneurysms, and neuroretinitis (IRVAN): new observations and a proposed staging system. Ophthalmology. 2007;114:1526–1529. e1. doi: 10.1016/j.ophtha.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 4.Venkatesh P, Verghese M, Davde M, Garg S. Primary vascular occlusion in IRVAN (idiopathic retinal vasculitis, aneurysms, neuroretinitis) syndrome. Ocul Immunol Inflamm. 2006;14:195–196. doi: 10.1080/09273940600657710. [DOI] [PubMed] [Google Scholar]
- 5.Karagiannis D, Soumplis V, Georgalas I, Kandarakis A. Ranibizumab for idiopathic retinal vasculitis, aneurysms, and neuroretinitis: favorable results. Eur J Ophthalmol. 2010;20:792–794. doi: 10.1177/112067211002000425. [DOI] [PubMed] [Google Scholar]
- 6.Wang GL, Lu N, Wang MY. Clinical feature and treatment of IRVAN syndrome. Ophthalmic Res. 2006:191–194. [Google Scholar]
- 7.Singh R, Sharma K, Agarwal A, Dogra M, Gupta V, Sharma A, Dogra MR. Vanishing retinal arterial aneurysms with anti-tubercular treatment in a patient presenting with idiopathic retinal vasculitis, aneurysms, and neuroretinitis. J Ophthalmic Inflamm Infect. 2016;6:8. doi: 10.1186/s12348-016-0074-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marin-Lambies C, Gallego-Pinazo R, Salom D, Navarrete J, Diaz-Llopis M. Rapid regression of exudative maculopathy in idiopathic retinitis, vasculitis, aneurysms and neuroretinitis syndrome after intravitreal ranibizumab. Case Rep Ophthalmol. 2012;3:251–257. doi: 10.1159/000341821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rouvas A, Nikita E, Markomichelakis N, Theodossiadis P, Pharmakakis N. Idiopathic retinal vasculitis, arteriolar macroaneurysms and neuroretinitis: clinical course and treatment. J Ophthalmic Inflamm Infect. 2013;3:21. doi: 10.1186/1869-5760-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saatci AO, Ayhan Z, Takes O, Yaman A, Bajin FM. Single bilateral dexamethasone implant in addition to panretinal photocoagulation and oral azathioprine treatment in IRVAN syndrome. Case Rep Ophthalmol. 2015;6:56–62. doi: 10.1159/000375481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eris E, Perente I, Vural E, Yasa D, Ozkaya A. Assessment of focal laser photocoagulations’ early effect on polypoidal choroidal vasculopathy with optical coherence tomography angiography. Lasers Med Sci. 2018;33:1833–1835. doi: 10.1007/s10103-018-2463-3. [DOI] [PubMed] [Google Scholar]