Abstract
Objective: To explore the morphological changes of the temporomandibular joint (TMJ) in adult patients with skeletal class II deep overbite before and after orthodontic treatment, and to analyze the effect of the orthodontic treatment. Methods: A total of 40 adult skeletal class II deep overbite patients were recruited as the study cohort. For each subject, the morphology and position of the TMJ were determined using cone beam computed tomography. Results: Compared with before the treatment, the morphology of the condyle changed. The maximum cross-sectional area of the condyle in the axial plane and the condyle neck anteroposterior diameter in the coronal plane were reduced. The condylar apex height in the sagittal plane and the anterior condyle oblique inclination increased with statistically significant differences (all P<0.001). There were more patients who showed their condyles moving forward and their condyles in the middlee after the treatment compared with before the treatment, and with a statistically significant difference (P=0.002). The morphology of the glenoid fossa changed after the treatment. The articular eminence to the FH plane angle in the sagittal plane and the inclination of the posterior glenoid increased. The total height of the fossa increased with statistically significant differences (all P<0.001). Conclusion: TMJs can be adaptive to reconstruction. Orthodontic treatment shows a favorable efficacy in skeletal class ll deep overbite patients.
Keywords: Orthodontic treatment, class II deep overbite, temporomandibular joint, efficacy
Introduction
The skeletal class ll deep overbite is currently one of the most common oral malformations. The most common symptoms are convexity, uncovered teeth, retraction underneath the skeleton, and even upper airway stenosis in severe cases. A disorder of the temporomandibular joint (TMJ) is more apparent in patients with skeletal class ll deep overbites than in normal people, affecting their facial health and appearance [1]. People now pay more attention to facial beauty in work and life, so an increasing number of patients are willing to undergo orthodontic treatment to change the morphology and position of the condyle and the morphology of the temporomandibular fossa [2]. The morphology of the mandibular joint in patients with skeletal class III deep overbite also changes after orthodontic treatment [3,4]. However, there are few studies on the effect of the orthodontic treatment on the morphology of the mandibular joint in adult skeletal class ll deep overbite patients. Therefore, this study aims to evaluate the morphological changes of the mandibular joint in skeletal class ll deep overbite patients after orthodontic treatment using cone-beam computed tomography (CBCT), in order to provide a theoretical basis for the orthodontic treatment of skeletal class ll deep overbite.
Materials and methods
Subjects
A total of 40 patients diagnosed with adult skeletal class ll deep overbite in our hospital from December 2018 to December 2019 were recruited as the study cohort. This study was approved by the Ethics Committee of our hospital (ethical approval number: S2020-133). All the patients signed an informed consent form.
The patients were eligible for the study if they were 18 years old or older, if they showed an ABN angle >4.7° and 22°≤ FMA ≤32°, if they had no history of orthodontics or other facial surgery, if they had no maxillofacial trauma, joint trauma, TMJ dysfunction, or cleft lip and palate, if they were mentally healthy and able to use self-locking braces, and if they participated voluntarily and could actively cooperate with the doctors.
Patients were excluded if they were suffering from systemic diseases, if they were pregnant or lactating, or if they had severe dental caries or abrasions.
Methods
In this retrospective study, the subjects were measured for TMJ morphology-related parameters before and after receiving orthodontic treatment. The details of the orthodontic treatment are as follows. The Damon Q self-locking bracket correction system from Ormco, US, was used to put occlusal plates on and to bond self-locking brackets to all the teeth. Nickel-titanium round wires were used for light traction and for further adjustments to get even mandibular teeth.
Measurement methods and the measured items
CBCT was used to measure the morphology and position of each mandibular joint before and after treatment. In vivo Dental 5 imaging software (Anatomage) was used to reconstruct the scan data. The imaging and measurement were performed in the axial, sagittal, and coronal planes according to the method of Jiang et al. [5].
There were 4 outcome measures. First, the morphology of the condyle was described using the maximum cross-sectional area of the condyle in the axial plane, the condyle neck anteroposterior diameter in the axial plane, the anterior condyle oblique inclination in the sagittal plane, the condylar apex height in the sagittal plane, and the condylar mediolateral diameter in the coronal plane. Second, the position of the condyle was described using the condyle position in the sagittal plane (posterior joint space area/anterior joint space area). Values of -0.25-0.25 indicated that the position of the condyle was in the middle, values >0.25 indicated that the condyle moved forward, and values <-0.25 indicated that the condyle moved backward. Third, the position of the glenoid fossa was described using the articular eminence to the FH plane angle in the sagittal plane, the total height of the fossa in the coronal plane, the anteroposterior width of the articular fossa in the coronal plane, and the inclination of the posterior glenoid in the coronal plane. Finally, the patients’ satisfaction rates after the surgery were evaluated and classified into one of three levels (satisfaction, basic satisfaction and dissatisfaction). The treatment satisfaction rate was defined as: treatment satisfaction rate = (cases of satisfaction + cases of basic satisfaction)/total number of cases * 100%.
Statistical methods
SPSS 22.0 software was used for the statistical analysis. GraphPad Prism 8 was used to plot the figures. The measurement data that met a normal distribution were expressed as the mean ± standard deviation (x̅ ± sd). The TMJ morphological measurements on the different sides were processed using independent sample t-tests, and the TMJ morphological measurements before and after the treatment were processed using paired t-tests. The count data were described using composition ratios and processed using chi-square tests, two-sided α=0.05. P<0.05 was considered statistically significant.
Results
General data
Among the 40 adult patients with skeletal class ll deep overbites, 17 were males and 23 were females, aged 22-36 years old, with an average age of 27.9±4.4 years old. There was no statistically significant differences in the morphology or positions of the mandibular joints on the left and right sides of the patients before and after the treatment (all P>0.05). See Table 1 for details.
Table 1.
General conditions (n=40; x̅ ± sd)*
| Category | Before treatment | After treatment | ||
|---|---|---|---|---|
|
|
|
|||
| Left | Right | Left | Right | |
| Maximum cross-sectional area of condyle (mm2) | 98.84±17.12 | 99.11±15.67 | 76.63±9.08 | 74.05±9.34 |
| Condyle neck anteroposterior diameter (mm) | 7.78±1.21 | 8.12±1.34 | 7.34±1.07 | 7.31±0.98 |
| Anterior condyle oblique inclination (°) | 34.01±2.39 | 32.98±3.27 | 35.02±2.43 | 35.32±3.87 |
| Condylar mediolateral diameter (mm) | 18.68±1.19 | 18.82±1.54 | 17.79±1.68 | 17.60±2.32 |
| Condylar apex height (mm) | 18.06±1.96 | 17.79±1.86 | 17.61±1.97 | 18.04±2.25 |
| Articular eminence to the FH plane angle (°) | 29.26±2.67 | 28.15±2.49 | 32.48±1.85 | 33.56±3.06 |
| Total height of the fossa (mm) | 7.72±0.88 | 7.85±0.98 | 8.23±0.79 | 8.48±0.84 |
| Anteroposterior width of the articular fossa (mm) | 15.47±2.14 | 15.21±2.21 | 15.03±2.48 | 15.31±2.31 |
| Inclination of posterior glenoid (°) | 33.21±2.53 | 31.79±3.23 | 36.02±3.31 | 35.57±2.43 |
indicates measurement data.
Morphology changes of condyle
After the treatment, the maximum cross-sectional areas of the condyle in the axial plane and the condylar mediolateral diameters in the coronal plane decreased; the condylar apex heights in the sagittal plane and the anterior condyle oblique inclinations increased with statistically significant differences (all P<0.001). There were no significant differences in the condyle neck anteroposterior diameters before or after the treatment (P=0.131). See Table 2 and Figure 1.
Table 2.
Morphological changes of the condyle before and after treatment (x̅ ± sd)*
| Variable | Before treatment (n=40) | After treatment (n=40) | t | P |
|---|---|---|---|---|
| Maximum cross-sectional area of condyle | 98.73±17.78 | 80.21±15.79 | 15.68 | <0.001 |
| Condyle neck anteroposterior diameter | 8.01±1.43 | 7.64±1.55 | 1.520 | 0.131 |
| Anterior condyle oblique inclination | 33.03±2.89 | 35.41±3.30 | -8.92 | <0.001 |
| Condylar mediolateral diameter | 18.56±2.32 | 17.25±1.92 | 9.72 | <0.001 |
| Condylar apex height | 3.01±1.15 | 3.44±0.90 | -8.69 | <0.001 |
indicates measurement data.
Figure 1.
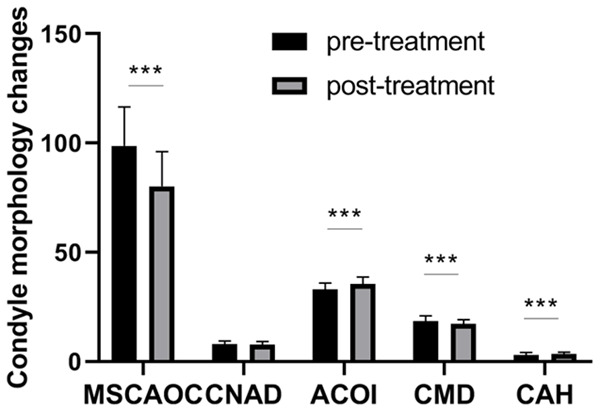
Morphological changes of the condyle before and after treatment. Compared with the pre-treatment morphology, ***P<0.001. MSCAOC: maximum cross-sectional area of the condyle; CNAD: condyle neck anteroposterior diameter; ACOI: anterior condyle oblique inclination; CMD: condylar height mediolateral diameter; CAH: condylar apex height.
Change of condyle position
The positions of the condyle in the sagittal plane changed significantly before and after the treatment. There were more patients who showed a condyle moving forward and a condyle in the middle after the treatment compared with the pre-treatment data (P=0.002). See Table 3 for details.
Table 3.
Changes in the position of the condyle before and after treatment (n=40; n, %)*
| Variable | Before treatment | After treatment | χ2 | P |
|---|---|---|---|---|
| Condyle in the middle | 40 (50.0%) | 51 (63.8%) | 12.019 | 0.002 |
| Condyle moving forward | 8 (10.0%) | 16 (20.0%) | ||
| Condyle moving backward | 32 (40.0%) | 13 (16.2%) |
indicates count data.
Morphological changes of the glenoid fossa
After the treatment, the morphology of the glenoid fossa was significantly changed. The articular eminence to the FH plane angle, the inclination of posterior glenoid in the sagittal plane, and the total height of the fossa in the coronal plane increased with statistically significant differences (all P<0.001). The changes in the total height of the fossa in the coronal plane were not significant after the treatment (P=0.342). See Table 4 and Figure 2 for details.
Table 4.
Morphological changes of the glenoid fossa before and after treatment (x̅ ± sd)*
| Variable | Before treatment (n=40) | After treatment (n=40) | t | P |
|---|---|---|---|---|
| Articular eminence to the FH plane angle | 28.54±2.42 | 32.18±3.07 | -34.55 | <0.001 |
| Inclination of posterior glenoid | 33.35±2.98 | 35.72±2.55 | -23.62 | <0.001 |
| Total height of the fossa | 7.78±0.89 | 8.31±0.95 | -5.56 | <0.001 |
| Anteroposterior width of the articular fossa | 15.34±3.11 | 15.17±2.87 | 0.823 | 0.342 |
indicates measurement data.
Figure 2.
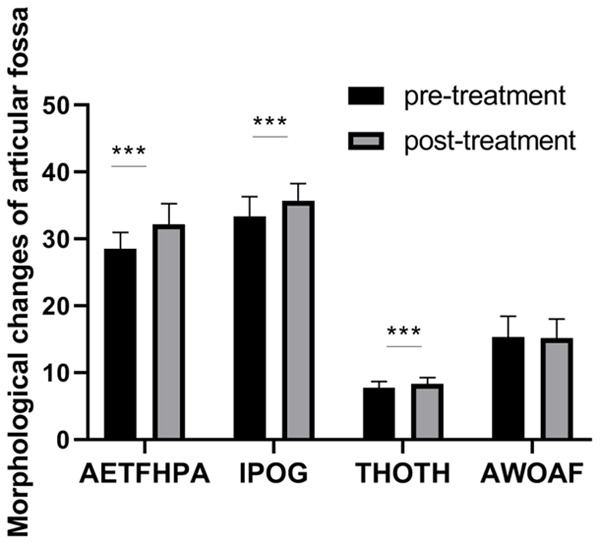
Changes in the glenoid fossa morphology before and after treatment. Compared with before the treatment, ***P<0.001. AETFHPA: articular eminence to the FH plane angle; IOPG: inclination of the posterior glenoid; THOTF: total height of the fossa; AWOAF: anteroposterior width of the articular fossa.
Satisfaction rate
After the treatment, 38 patients were satisfied with the treatment, 1 patient was basically satisfied, and 1 patient was dissatisfied, for a treatment satisfaction rate of 97.5%, indicating a high recognition of the efficacy of the orthodontic treatment.
CBCT before and after the orthodontic treatment
After the orthodontic treatment, the articular eminence to the FH plane angle, the inclination of the posterior glenoid, and the total height of the fossa in the coronal plane increased. The position of the condyle in the glenoid fossa moved from the outer upper back to the middle. So, the patients’ facial appearances improved well, with neatly arranged upper and lower teeth and favorable occlusions. The lateral cephalometric images of the class II malocclusions before and after the orthodontic treatment are shown in Figure 3.
Figure 3.
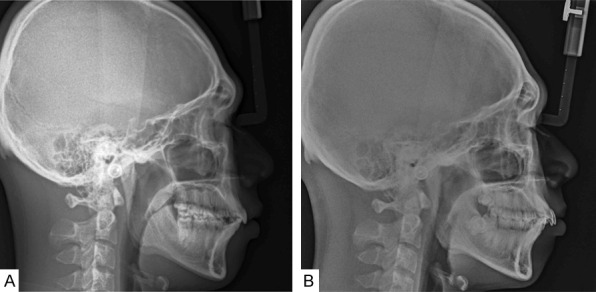
The lateral cephalometric images before and after orthodontic treatment. A: The lateral cephalometric images after the orthodontic treatment; B: The lateral cephalometric images before the orthodontic treatment.
Discussion
Skeletal class ll deep overbite is a common clinical malformation with a complicated pathogenesis. The prevalence of skeletal class ll deep overbite in China is about 20%, and the prevalence in adolescents is 23% [6]. The clinical manifestation of skeletal class ll deep overbite is mandibular retraction, which not only affects the normal function of the mandible but also the appearance. In addition, skeletal class ll deep overbite patients often have posterior upper condyle displacement and are prone to TMJ diseases due to the strong masticatory muscles [7]. One study found that patients with skeletal class ll deep overbites often also suffer from tooth wear and periodontal trauma, which affects chewing and also causes adverse psychological effects on the patients [8]. For adult patients, the main treatment method is orthodontic treatment. Yu et al. found that the patients’ facial morphology improved well, and their quality of life also improved after the orthodontic treatment [9,10].
The indexes involved were all obtained using CBCT. A previous study found that compared with X-ray imaging and traditional spiral CT, CBCT showed a promising feasibility and accuracy in TMJ measurement, and it was able to ensure the accuracy of the research results [11].
This study found no difference in the morphological measurements on the left and right sides of the TMJs, indicating that the orthodontic treatment did not affect the symmetry of the TMJs. This is consistent with previous results [12]. The shapes of the patients’ left and right TMJs are basically symmetrical. One possible reason is that the TMJ is a linked joint, and the left and right sides often have the same movement, so they are often symmetrical.
The results of this study showed that the maximum cross-sectional area of the condyle decreased from 98.73 mm2 (before treatment) to 80.21 mm2 (after treatment) in the skeletal class ll deep overbite patients, which is basically consistent with the results from the study of Shi [13]. The inner and outer diameters of the condyle neck decreased from 18.56 mm (before treatment) to 17.25 mm (after treatment), which is in line with the results from the study of Li et al. [14]. The condylar apex height and the anterior condyle oblique inclination increased from 3.01 mm and 33.03° (before treatment) to 3.44 mm and 35.41° (after treatment), respectively, as they did in the study of Zhu et al. [15]. One possible reason is that the adult condyle can still be adapted to remodeling [16]. After the orthodontic treatment, the patient’s occlusion changed, and the condyle underwent adaptive changes. In skeletal class ll deep overbite patients, the articular eminence to the FH plane angle, the total height of the fossa, and the inclination of posterior glenoid increased after the treatment compared with before the treatment. This is basically consistent with the research results from Wang and Qin et al. [17,18]. The increased TMJ load of the patients after the treatment and the reconstruction of the glenoid fossa are possible reasons [19-22]. After the orthodontic treatment, the position of the condyle in the glenoid fossa moved from the outer upper back to the middle. The proportion of the posterior condylar displacement decreased from 40% to 16.2%, and the position in the middle increased from 50.0% to 63.8%, which is consistent with the studies of Carlton et al. and Liu et al. [23,24]. The adaptive reconstruction of the TMJ after the orthodontic treatment is a possible reason.
This study also has certain limitations. The study cohort was small, and the cohort ranged in age from 22 to 36 years old, so there may be a selection bias, which could have a certain influence on the extrapolation of the research results. We plan to continue to recruit patients that meet the selection criteria in the future diagnostic and treatment process to expand the sample size of the study.
In summary, orthodontic treatment for skeletal class ll deep overbite can help the adaptive reconstruction of the TMJ, and the position of the condyle in the glenoid fossa changes from relatively outer and upper to middle, suggesting a favorable clinical effectiveness.
Disclosure of conflict of interest
None.
References
- 1.Dong CM, Yu LF, Zou DR. CBCT research progress of temporomandibular joint in patients with malocclusion. Stomatol. 2020;40:560–564. [Google Scholar]
- 2.Tian LL, Zhang JL, Jiang Y. Soft and hard tissue changes and stability of class ll Division 1 malocclusion treated with T4K appliance. Shanghai J Stom. 2019;28:112–115. [PubMed] [Google Scholar]
- 3.Wang D, Fang MR, Li Q, Ma JQ. Changes of temporomandibular joint in the treatment of skeletal class lll malocclusion. Oral Biomed. 2020;11:176–180. [Google Scholar]
- 4.Rui M, Ting C, Pengqian F, Xinqiao F. Burnout among anaesthetists in Chinese hospitals: a multicentre, cross-sectional survey in 6 provinces. J Eval Clin Pract. 2016;22:387–394. doi: 10.1111/jep.12498. [DOI] [PubMed] [Google Scholar]
- 5.Jiang H, Wang ZW, Liu HC, Hu M, Cao JK, Shi XW. Measurement technology of temporomandibular joint bone structure with dental special CT. Zhonghua Laonian Kouqiang Yixue Zazhi. 2008;6:84–86. [Google Scholar]
- 6.Fu MK, Zhang D, Wang BK, Deng Y, Wang FH, Ye XY. Prevalence of malocclusion in 25392 children and adolescents in China. Chin J Stomatol. 2002;37:371–373. [PubMed] [Google Scholar]
- 7.Guan YX, Liu LX, Wu XP. Effects of different types of malocclusion deformity on the morphology and function of temporomandibular joint. J Stomatol. 2020;40:381–384. [Google Scholar]
- 8.Li D, Shen LH, Du XJ, Cheng HY, Jiang H. Three dimensional finite element analysis of maxillary force exerted by modified vestibular shield. Med Inf. 2018;31:70–73. [Google Scholar]
- 9.Yu X, Yuan LJ, Liu JQ, Fang B, Mao LX, Yang Z, Zhu M, Wu Y, Ma XH, Sun L. Changes of mandibular retrusion with anterior disc displacement after Herbst appliance. Chin J Orthod. 2017;24:204–207. doi: 10.3760/cma.j.issn.1002-0098.2017.03.009. [DOI] [PubMed] [Google Scholar]
- 10.Wen H. Effect of orthodontic treatment on oral health and quality of life of patients with different types of malocclusion. Electronic J Clin Med Lit. 2018;5:79. [Google Scholar]
- 11.Zhou T, Qian Y, Liu WS, Deng D. Application value of CBCT in measurement of bilateral temporomandibular joint in adolescents. Chin J Prosthodontics. 2020;21:282–285. [Google Scholar]
- 12.Rodrigues AF, Fraga MR, Vitral RW. Computed tomography evaluation of the temporomandibular joint in class II division 1 and class III malocclusion patients: condylar symmetry and condyle-fossa relationship. Am J Orthod Dentofacial Orthop. 2009;136:199–206. doi: 10.1016/j.ajodo.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 13.Shi XW. CBCT study on morphological changes of temporomandibular joint in adult patients with skeletal class II deep overbite before and after orthodontic treatment. Dalian Yi Ke Da Xue. 2019 [Google Scholar]
- 14.Li NJ, Zhao CY, Wu K, Ma JQ. Mechanism of twin block appliance in the treatment of angle’s II malocclusion. Stomatol. 2019;39:1082–1084. 1112. [Google Scholar]
- 15.Zhu XY, Hong Y, Ji HN, Zhang J, Mei S, Lu M, Liang YJ, Wang RL. CBCT observation of TMJ morphological changes in children with class II division 1 malocclusion treated with self-locking bracket appliance. Chin J Control Endem Dis. 2019;34:109–110. [Google Scholar]
- 16.Saccucci M, D’Attilio M, Rodolfino D, Festa F, Polimeni A, Tecco S. Condylar volume and condylar area in class I, class II and class III young adult subjects. Head Face Med. 2012;8:34. doi: 10.1186/1746-160X-8-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang K. Effect of orthodontic treatment on temporomandibular joint structure in patients with angle class II division 2 malocclusion. Chin J Mod Drug Appl. 2019;13:57–58. [Google Scholar]
- 18.Qin Q, Yang YF, Qin DC, Zhang L, Zhang Q. Clinical study on the changes of soft and hard tissues before and after extraction of class II^2 malocclusion. J Mod Stomatol. 2018;32:129–133. [Google Scholar]
- 19.Xu XM, Wei XX, Han HL, Li YB, Yang L. Comparison of temporomandibular joint characteristics between adolescents and adults with angle class II division 1 malocclusion. Henan Med Res. 2019;28:1539–1542. [Google Scholar]
- 20.Guan YX, Liu LX, Wu XP. Effects of different types of malocclusion on the morphology and function of temporomandibular joint. Stomatol. 2020;40:381–384. [Google Scholar]
- 21.Park JT, Lee JG, Won SY, Lee SH, Cha JY, Kim HJ. Realization of masticatory movement by 3-dimensional simulation of the temporomandibular joint and the masticatory muscles. J Craniofac Surg. 2013;24:e347–e351. doi: 10.1097/SCS.0b013e31828f2d73. [DOI] [PubMed] [Google Scholar]
- 22.Imamura K, Terajima M, Nakashima A, Takahashi I. A three-dimensional analysis of masticatory muscles in laterognathism. Orthodontic Waves. 2019;78:143–150. [Google Scholar]
- 23.Carlton KL, Nanda RS. Prospective study of posttreatment changes in the temporomandibular joint. Am J Orthod Dentofacial Orthop. 2002;122:486–490. doi: 10.1067/mod.2002.128863. [DOI] [PubMed] [Google Scholar]
- 24.Liu BW, Wang YM, Song F, Liu M, Duan Y, Zhou L. Cone beam CT was used to analyze the changes of temporomandibular joint in angle class II division 1 malocclusion patients before and after twin block treatment. West Chin J Stomatol. 2013;31:610–614. [PubMed] [Google Scholar]


