Abstract
Objective: To probe into the evidence-based nursing in patients after cataract surgery and its impact on their visual acuity recovery and psychological status. Methods: Ninety-seven patients with cataract who underwent surgery in our hospital were randomly divided into control group (n=48, receiving conventional nursing) and observation group (n=49, receiving evidence-based nursing) for a prospective study. Postoperative visual acuity recovery, incidence of complications, recurrence rate within 1 year, psychological status before and after surgery and quality of life were compared between the two groups. Results: The best corrected visual acuity of the affected eye of patients at 3 and 6 months after surgery in both groups was significantly higher than that before surgery, with the best corrected visual acuity of the same period in the observation group higher than that in the control group (all P<0.05). The incidence of postoperative complications and recurrence rate within 1 year in the observation group were lower than those in the control group (all P<0.05). Three months after operation, the scores of Hamilton Anxiety Scale and Hamilton Depression Scale in the two groups were lower than those before operation, with the scores in the observation group lower than those in the control group (all P<0.05); and the scores of all items in Generic Quality of Life Inventory in the two groups were higher than those before operation, with the scores in the observation group higher than those in the control group (all P<0.05). Conclusion: Evidence-based nursing for patients after cataract surgery can significantly improve the recovery of patients’ postoperative visual acuity, reduce the incidence of postoperative complications as well as the recurrence rate. It also helps to improve the adverse psychological status of patients and their postoperative quality of life.
Keywords: Cataract surgery, evidence-based nursing, visual acuity, psychological status
Introduction
Cataract is a clinical ophthalmic disease with a high incidence. Patients with the disease will have cloudy lens with decreased visual acuity, which can result in blurred vision and even blindness in severe cases [1,2]. Surgery is the main treatment for cataract. However, the incidence of postoperative complications is high, which influences the quality of life of patients [3]. Therefore, it is of significant importance to adopt reasonable, scientific and effective nursing measures to reduce the incidence of postoperative complications and improve patients’ quality of life.
At present, the situation in regard to nursing for patients after cataract surgery still needs improvement in primary hospitals in China. According to surveys, their nursing protocols for patients after cataract surgery mainly focus on eyes and complications [4]. Little attention has been paid to the psychological status and quality of life of patients after surgery. Evidence-based nursing is a new nursing model that includes a variety of nursing measures implemented on the basis of conventional nursing. These measures, whose rationality and effectiveness have been confirmed in a large body of literature and by many evidences, are considered as a more scientific, effective and targeted nursing model than conventional nursing [5,6].
However, evidence-based nursing has been mostly applied to reduce the occurrence of complications in patients after cataract surgery, there are few studies in regard to the influences of evidence-based nursing on patients’ visual acuity recovery and psychological status [7]. So, this study mainly focuses on the effects of evidence-based nursing on postoperative visual acuity recovery and psychological status of patients with cataract.
Materials and methods
General data
This is a prospective study. In the study, 97 cataract patients undergoing cataract surgery in our hospital between December 2018 and December 2019 were randomized into control group (n=48, receiving conventional nursing) and observation group (n=49, receiving evidence-based nursing). This study was approved by the Medical Ethics Committee of our hospital. Patients were eligible if they were aged between 50 and 75; were with only one eye affected; were assessed as grade II to IV by cataract grading system LOCS II [8]; were with the BCVA of the affected eye less than 0.4 [9]; had cataract surgery plan; had signed the informed consent. Patients were excluded if they had other ocular diseases such as keratitis, corneal edema, diabetic retinopathy and age-related macular degeneration; had hematologic abnormality or coagulation disorder and intolerable to surgeries; had malignant tumor or cognitive dysfunction; had participated in other studies etc.
Methods
Patients in both groups had received cataract surgeries in the outpatient clinics of our hospital. After that, patients in the control group were given conventional nursing, such as regular dressing changes, wearing special eye shields, and were asked not to touch their eyes or wash them within 5 to 7 days; patients in the observation group were given evidence-based nursing, meaning they were treated with corresponding nursing protocols relating to their postoperative performance and complications they presented. These protocols were designed by medical staff after reading a large body of references in the database. The specific nursing measures are as follows [10-12].
(1) Prevention of ocular inflammation: the conjunctival sac of patients was repeatedly washed with 5% povidone-iodine before surgery. After surgery, patients were given antibiotics, such as intraocular injection of cefuroxime right after the operation, to prevent infection. Excipients used for treating the wound were changed regularly and kept in a dry condition; (2) Prevention of hyphema after surgery: hypertension is the main cause of hyphema after cataract surgery. So, for patients with hypertension, antihypertensive drugs were given 1 hour before the surgery to control their blood pressure. Then they were sent into the operating room when their systolic blood pressure remained below 140 mmHg, so as to reduce postoperative hyphema caused by increased blood pressure during surgery. (3) Treatment of corneal edema after surgery: corneal edema is a very common complication after cataract surgery, which could result in blurred vision but could be controlled by local administration of corneal nutrition, anti-infective drugs and so on. However, this complication is able to be alleviated spontaneously in 1 to 2 weeks. (4) Prevention of adverse psychological status after surgery: most patients will have adverse psychological symptoms after cataract surgery, even depression in severe cases. Therefore, after patients were admitted, we communicated with them on a regular base to deliver cataract-related knowledge and treatment protocols with amiable attitude and simple words to increase their trust and help them relax; we also disclosed some previous successful cases, and if possible, arranged them with face-to-face communications with the patients who had a successful surgery with good visual acuity recovery, which had encouraged them greatly; we also informed patients that their surgeons were all veterans with rich clinical experience to help them get rid of their anxiety and fear; during surgery, we talked with patients appropriately to alleviate their nervous.
Outcome measures
Primary outcome measaures
(1) Visual acuity recovery: the best corrected visual acuity (BCVA) of the affected eye was detected before and 3/6 months after surgery using international standard visual acuity chart [13]. (2) Psychological status before and 3 months after surgery: Hamilton Anxiety Scale (HAMA) and Hamilton Depression Scale (HAMD, 17 items) were applied, with the scores of HAMA less than 7 indicating no anxiety in patients and the scores of HAMD (17 items) less than 7 indicating no depression in patients, and higher scores denoting more severe anxiety or depression [14,15].
Secondary outcome measures
(1) Postoperative complications of patients were compared between the two groups. (2) The recurrence rate of patients was compared between the two groups during the one-year follow up. (3) Quality of life of patients before and 3 months after surgery: Generic Quality of Life Inventory (GQOLI-74) was used, in which social, physical and psychological functions were scored from 20 to 100, and material condition of life was scored from 16 to 80, with higher scores indicating better quality of life [16].
Statistical analysis
SPSS 20.0 was used for data analyses. Enumeration data were expressed as n (%), and χ2 test was used for comparison. Measurement data were expressed as x̅±SD. Paired t test was used for within-group comparison before and after surgery. Independent t test was used for between-group comparison. P<0.05 was considered statistically significant.
Results
Comparison of general data between the two groups
The general data in the two groups were comparable, with no statistical difference (all P>0.05). See Table 1.
Table 1.
Comparison of general data between the two groups (n, x̅±sd)
| Indexes | Observation group (n=49) | Control group (n=48) | χ2/t | P |
|---|---|---|---|---|
| Sex (n) | 0.833 | 0.361 | ||
| Male | 22 | 26 | ||
| Female | 27 | 22 | ||
| Age (year) | 63.3±6.4 | 62.8±5.6 | 0.410 | 0.683 |
| Disease duration (year) | 8.83±2.20 | 9.04±2.47 | 0.442 | 0.660 |
| Cataract grading system LOCS II (n) | 0.976 | 0.614 | ||
| Grade II | 20 | 15 | ||
| Grade III | 18 | 20 | ||
| Grade IV | 11 | 13 | ||
| BCVA in the affected eye | 0.23±0.08 | 0.22±0.09 | 0.578 | 0.565 |
Note: BCVA: the best corrected visual acuity.
Visual acuity recovery
The BCVA of the affected eye of patients 3/6 months after surgery in both groups was significantly higher than that before surgery, with the BCVA of the same period in the observation group higher than that in the control group (all P<0.05). See Table 2.
Table 2.
The BCVA of the affected eye in the two groups at different time before and after surgery (x̅±sd)
| Group | Before surgery | 3 months after surgery | 6 months after surgery |
|---|---|---|---|
| Observation group (n=49) | 0.23±0.08 | 0.69±0.13*,# | 0.77±0.14*,# |
| Control group (n=48) | 0.22±0.09 | 0.51±0.10* | 0.60±0.16* |
Note: Compared with before surgery;
P<0.05.
Compared with the control group;
P<0.05.
BCVA: the best corrected visual acuity.
Psychological status
The scores of HAMA and HAMD 3 months after surgery in the two groups were lower than those before surgery, with the scores in the observation group lower than those in the control group (all P<0.05). See Table 3.
Table 3.
The scores of HAMA and HAMD before and after surgery in the two groups (x̅±sd)
| Group | Observation group (n=49) | Control group (n=48) | ||
|---|---|---|---|---|
|
|
|
|||
| Time | Before surgery | 3 months after surgery | Before surgery | 3 months after surgery |
| HAMA score | 7.02±1.16 | 5.64±1.10*,# | 6.98±1.06 | 6.12±1.13* |
| HAMD score | 7.50±1.09 | 5.78±1.11*,# | 7.65±1.24 | 6.48±1.16* |
Note: Compared with before surgery;
P<0.05.
Compared with the control group;
P<0.05.
HAMA: Hamilton Anxiety Scale; HAMD: Hamilton Depression Scale.
Complications
The incidence of postoperative complications in the observation group was lower than that in the control group (P<0.05). See Table 4.
Table 4.
Postoperative complications of patients in the two groups (n, %)
| Group | Observation group (n=49) | Control group (n=48) |
|---|---|---|
| Ocular inflammation | 1 (2.04) | 2 (4.17) |
| Hyphema | 0 (0.00) | 2 (4.17) |
| Temporary high intraocular pressure | 1 (2.04) | 2 (4.17) |
| Corneal edema | 1 (2.04) | 4 (8.33) |
| Total incidence rate | 3 (6.12)# | 10 (20.83) |
Note: Compared with the control group;
P<0.05.
Recurrence rate
After 1-year follow-up, the recurrence rate of cataract of the affected eye was 2.04% (1/49) in the observation group, lower than the 12.50% (6/48) in the control group (P<0.05), as shown in Figure 1.
Figure 1.
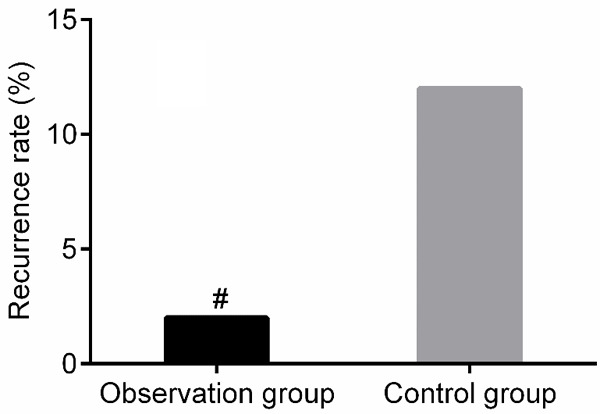
Comparison of the recurrence rate of cataract within 1 year after surgery between the two groups. Compared with the control group, #P<0.05.
Quality of life
The scores of all items in GQOLI-74 at 3 months after surgery in the two groups were higher than those before surgery, with the scores in the observation group higher than those in the control group (all P<0.05). See Table 5.
Table 5.
The scores of all items in GQOLI-74 before and after surgery in the two groups (x̅±sd)
| Group | Observation group (n=49) | Control group (n=48) | ||
|---|---|---|---|---|
|
|
|
|||
| Time | Before surgery | 3 months after surgery | Before surgery | 3 months after surgery |
| Material condition of life | 58.60±4.85 | 69.97±5.43*,# | 58.11±6.40 | 63.33±5.69* |
| Social function | 72.20±5.66 | 79.49±6.13*,# | 71.84±5.86 | 75.04±5.40* |
| Physical function | 74.44±5.81 | 82.22±6.46*,# | 74.15±5.04 | 78.48±5.86* |
| Psychological function | 70.07±6.59 | 76.66±6.30*,# | 69.70±5.52 | 73.38±5.93* |
Note: Compared with before surgery;
P<0.05.
Compared with the control group;
P<0.05.
GQOLI-74: generic quality of life inventory.
Discussion
Although surgery is the primary treatment for cataract patients, it may be accompanied with many postoperative complications, such as ocular inflammation, hyphema, temporary high intraocular pressure, corneal edema and so on, which may result in blurred vision [17,18]. Therefore, high-quality nursing after surgery plays a critical role in reducing the occurrence of complications and promoting patients’ visual acuity recovery.
In this study, visual acuity recovery in patients who received either conventional nursing or evidence-based nursing after cataract surgery were compared. The results showed that the BCVA of the affected eye 3/6 months was significantly higher in the two groups after surgery than that before surgery, with the BCVA of the same period in the observation group higher than that in the control group. Meanwhile, the total occurrence rate of postoperative complications and recurrence rate of cataract during the 1-year follow-up in the observation group were lower than those in the control group, indicating that evidence-based nursing in cataract patients could markedly improve their visual acuity recovery and decrease the occurrence of complications as well as long-term recurrence rate of cataract. Kaur et al. reported that cataract patients who had received surgery had faster visual acuity recovery when treated with evidence-based nursing, and Lundström et al. also reported that with the application of evidence-based nursing, the occurrence of complications in patients after cataract surgery can be markedly reduced [19,20]. This is because nursing measures adopted during evidence-based nursing have been proved to be more scientific, effective and targeted in lowering the occurrence of complications after cataract surgery than those during conventional nursing, so they are conducive to decreasing the occurrence of complications in patients after cataract surgery [21,22]. For example, in evidence-based nursing, antihypertensive drugs are given to patients with hypertension 1 hour before surgery to control their blood pressure, so as to reduce hyphema, which demonstrates that evidence-based nursing is more targeted than conventional nursing.
Most patients will have adverse psychological symptoms after cataract surgery, even depression in severe cases. Hence, timely psychological counseling for patients undergoing cataract surgery is helpful to improve their adverse psychological symptoms [23]. In this study, the HAMA and HAMD scores 3 months after surgery were all lower in the observation group than those in the control group, suggesting evidence-based nursing could significantly improve the adverse psychological status, including anxiety and depression in patients undergoing cataract surgery. Also, the study by Haripriya et al. showed that psychological status of patients could be significantly improved with evidence-based nursing, owing to that adverse psychological status in cataract patients were primarily caused by their concerns for postoperative visual acuity recovery, but delivering previous successful cases to them before cataract surgery or letting them have face-to-face communications with patients who had undergone successful cataract surgery with good visual acuity recovery was helpful to inspire them and gain their trust, thus preparing them with the best mental status to receive cataract surgery [24,25]. Besides, the differences in quality of life of patients before and 3 months after surgery in the two groups were compared in the study, and the result showed that the scores of all items in GQOLI-74 3 months after surgery were higher in the observation group than in the control group, suggesting evidence-based nursing is conducive to improving the life of quality of patients undergoing cataract surgery.
However, this is a single-center study with a small sample size and relatively short-term follow-up. More in-depth studies need to be conducted to explore the long-term effects of evidence-based nursing on visual acuity of patients undergoing cataract surgery.
In summary, evidence-based nursing in patients undergoing cataract surgery can substantially improve their visual acuity recovery and decrease the occurrence and recurrence of postoperative complications. It is also conducive to improving adverse psychological status in cataract patients and their quality of life in clinical settings.
Disclosure of conflict of interest
None.
References
- 1.Lee CM, Afshari NA. The global state of cataract blindness. Curr Opin Ophthalmol. 2017;28:98–103. doi: 10.1097/ICU.0000000000000340. [DOI] [PubMed] [Google Scholar]
- 2.Khairallah M, Kahloun R, Bourne R, Limburg H, Flaxman SR, Jonas JB, Keeffe J, Leasher J, Naidoo K, Pesudovs K, Price H, White RA, Wong TY, Resnikoff S, Taylor HR Vision Loss Expert Group of the Global Burden of Disease Study. Number of people blind or visually impaired by cataract worldwide and in world regions, 1990 to 2010. Invest Ophthalmol Vis Sci. 2015;56:6762–9. doi: 10.1167/iovs.15-17201. [DOI] [PubMed] [Google Scholar]
- 3.Roberts HW, Day AC, O’Brart DP. Femtosecond laser-assisted cataract surgery: a review. Eur J Ophthalmol. 2020;30:417–429. doi: 10.1177/1120672119893291. [DOI] [PubMed] [Google Scholar]
- 4.Wang SY, Blachley TS, Andrews CA, Ayanian JZ, Lee PP, Stein JD. Hospitalization after cataract surgery in a nationwide managed-care population. PLoS One. 2016;11:e0149819. doi: 10.1371/journal.pone.0149819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shuman CJ, Powers K, Banaszak-Holl J, Titler MG. Unit leadership and climates for evidence-based practice implementation in acute care: a cross-sectional descriptive study. J Nurs Scholarsh. 2019;51:114–124. doi: 10.1111/jnu.12452. [DOI] [PubMed] [Google Scholar]
- 6.Gattinoni L, Carlesso E, Santini A. Physiology versus evidence-based guidance for critical care practice. Crit Care. 2015;19(Suppl 3):S7. doi: 10.1186/cc14725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Babu BSG, Ravilla TD. Evidence-based management of eye care delivery. Community Eye Health. 2018;31:S15–S16. [PMC free article] [PubMed] [Google Scholar]
- 8.Gali HE, Sella R, Afshari NA. Cataract grading systems: a review of past and present. Curr Opin Ophthalmol. 2019;30:13–18. doi: 10.1097/ICU.0000000000000542. [DOI] [PubMed] [Google Scholar]
- 9.Esaka Y, Kojima T, Dogru M, Hasegawa A, Tamaoki A, Uno Y, Nishida T, Nakamura T, Hara S, Ichikawa K. Prediction of best-corrected visual acuity with swept-source optical coherence tomography parameters in keratoconus. Cornea. 2019;38:1154–1160. doi: 10.1097/ICO.0000000000002043. [DOI] [PubMed] [Google Scholar]
- 10.Haripriya A. Antibiotic prophylaxis in cataract surgery - an evidence-based approach. Indian J Ophthalmol. 2017;65:1390–1395. doi: 10.4103/ijo.IJO_961_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kessel L, Erngaard D, Flesner P, Andresen J, Tendal B, Hjortdal J. Cataract surgery and age-related macular degeneration. An evidence-based update. Acta Ophthalmol. 2015;93:593–600. doi: 10.1111/aos.12665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Galvis V, Tello A, Camacho PA, Rey JJ. Comment on: antibiotic prophylaxis in cataract surgery - an evidence-based approach. Indian J Ophthalmol. 2018;66:603. doi: 10.4103/ijo.IJO_1309_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pishnamaz MR, Ostadimoghaddam H. Striped circle visual acuity chart; a novel visual acuity chart based on the landolt-c chart. Med Hypothesis Discov Innov Ophthalmol. 2018;7:22–24. [PMC free article] [PubMed] [Google Scholar]
- 14.Zimmerman M, Martin J, Clark H, McGonigal P, Harris L, Holst CG. Measuring anxiety in depressed patients: a comparison of the Hamilton anxiety rating scale and the DSM-5 anxious distress specifier interview. J Psychiatr Res. 2017;93:59–63. doi: 10.1016/j.jpsychires.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 15.Raimo S, Trojano L, Spitaleri D, Petretta V, Grossi D, Santangelo G. Psychometric properties of the Hamilton depression rating scale in multiple sclerosis. Qual Life Res. 2015;24:1973–80. doi: 10.1007/s11136-015-0940-8. [DOI] [PubMed] [Google Scholar]
- 16.Zhou Y, Zhou R, Li W, Lin Y, Yao J, Chen J, Shen T. Controlled trial of the effectiveness of community rehabilitation for patients with schizophrenia in Shanghai, China. Shanghai Arch Psychiatry. 2015;27:167–74. doi: 10.11919/j.issn.1002-0829.215026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glick P, Luoto J, Orrs MS, Oliva MS, Tabin GC, Sanders DS, Thomas BJ, Ruit S, Belachew T, Tasfaw AK. The individual and household impacts of cataract surgery on older blind adults in Ethiopia. Ophthalmic Epidemiol. 2019;26:7–18. doi: 10.1080/09286586.2018.1504310. [DOI] [PubMed] [Google Scholar]
- 18.Ellis EM, Lee JE, Saunders L, Haw WW, Granet DB, Heichel CW. Complication rates of resident-performed cataract surgery: impact of early introduction of cataract surgery training. J Cataract Refract Surg. 2018;44:1109–1115. doi: 10.1016/j.jcrs.2018.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaur A, Gupta V, Christopher AF, Malik MA, Bansal P. Nutraceuticals in prevention of cataract - an evidence based approach. Saudi J Ophthalmol. 2017;31:30–37. doi: 10.1016/j.sjopt.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lundström M, Barry P, Henry Y, Rosen P, Stenevi U. Evidence-based guidelines for cataract surgery: guidelines based on data in the European registry of quality outcomes for cataract and refractive surgery database. J Cataract Refract Surg. 2012;38:1086–93. doi: 10.1016/j.jcrs.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 21.Kessel L, Andresen J, Erngaard D, Flesner P, Tendal B, Hjortdal J. Indication for cataract surgery. Do we have evidence of who will benefit from surgery? A systematic review and meta-analysis. Acta Ophthalmol. 2016;94:10–20. doi: 10.1111/aos.12758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kohnen T. Evidence-based treatment for macular edema after lens-based surgery. J Cataract Refract Surg. 2017;43:151–152. doi: 10.1016/j.jcrs.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 23.Zhang D, Fan Z, Gao X, Huang W, Yang Q, Li Z, Lin M, Xiao H, Ge J. Illness uncertainty, anxiety and depression in Chinese patients with glaucoma or cataract. Sci Rep. 2018;8:11671. doi: 10.1038/s41598-018-29489-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haripriya A, Chang DF. Intracameral antibiotics during cataract surgery: evidence and barriers. Curr Opin Ophthalmol. 2018;29:33–39. doi: 10.1097/ICU.0000000000000445. [DOI] [PubMed] [Google Scholar]
- 25.Prata TS, Ushida M, Dorairaj S. Cataract surgery alone cannot be considered an IOP-lowering procedure for open-angle glaucoma patients: an evidence-based perspective. Arq Bras Oftalmol. 2015;78:V–VI. doi: 10.5935/0004-2749.20150072. [DOI] [PubMed] [Google Scholar]


