Abstract
This study aimed to assess the predictive performance and establish optimal cut-off points of blood pressure for identifying arteriosclerosis in eastern Chinese adults. Brachial–ankle pulse wave velocity (baPWV) was utilized to evaluate arteriosclerosis. The predictive performance of blood pressure for arteriosclerosis was determined by the area under the curve (AUC) of receiver operating characteristics; the optimal blood pressure cut-off points were determined by Youden’s index. A logistic regression model was used to acquire the odds ratio (OR) of blood pressure for arteriosclerosis. The AUCs of blood pressure for identifying arteriosclerosis were 0.868 (95%CI: 0.860–0.875) for systolic blood pressure (SBP) and 0.835 (95%CI: 0.827–0.843) for diastolic blood pressure (DBP), both p < 0.01. The AUCs of women were higher than that of men (0.903 vs. 0.819 for SBP; 0.847 vs. 0.806 for DBP; Z test p < 0.05). The AUCs in the 18–39.9-years group were higher than that in the 40–59.9-years and 60–84-years groups (0.894 vs. 0.842 and 0.818 for SBP; 0.889 vs. 0.818 and 0.759 for DBP; Z test p < 0.05). The total optimal cut-off points of blood pressure for predicting arteriosclerosis were 123.5/73.5 mmHg (SBP/DBP) overall; 123.5/73.5 and 126.5/79.5 mmHg for women and men, respectively; and 120.5/73.5, 123.5/76.5, and 126.5/75.5 mmHg for 18–39.9-years, 40–59.9-years, and 60–84-years groups, respectively. Blood pressure indexes had a high predictive performance for identifying arteriosclerosis with the optimal cut-off point of 123.5/73.5 mmHg (SBP/DBP) in eastern Chinese adults. Women or the younger population have a higher predictive performance and lower cut-off points to identify arteriosclerosis.
Keywords: blood pressure, brachial-ankle pulse wave velocity, optimal cut-off point, arteriosclerosis
1. Introduction
Cardiovascular diseases (CVD) are the main cause of death across the world. Arteriosclerosis and atherosclerosis are the causes of most cardiovascular diseases, which are both indicators of future cardiovascular events and intervention targets [1,2]. Arteriosclerosis reflects arterial stiffness and function; furthermore, atherosclerosis indicates pathological changes in the arterial structure, which is often associated with cardiovascular events such as arterial rupture and blockage. According to the report “China cardiovascular diseases report 2018”, cardiovascular diseases occupied the leading cause of death, accounting for 44% of all deaths in China [3]. This leads to a heavy burden on medical care resources and the economy in China.
At present, pulse wave velocity is a classic index for the noninvasive detection of arteriosclerosis [4,5]. Brachial–ankle pulse wave velocity (baPWV) is the conduction velocity of the pulse wave at a certain distance from the arterial segment (i.e., pulse wave velocity), which represents the elasticity and compliance of arterial blood vessels [6,7,8,9]. BaPWV has increasingly been used as an epidemiological investigation method for diagnosing arteriosclerosis. Earlier screening and intervention for arteriosclerosis are vital for reducing disability and cardiovascular mortality [10]. Relatively speaking, the measurement of baPWV is complex and expensive. In contrast, blood pressure is easy to measure, and it has consistently been demonstrated that blood pressure is closely associated with arteriosclerosis [11,12,13]. However, what threshold value of blood pressure should be controlled to prevent arteriosclerosis is still unclear.
The predictive performance and accurate warning cut-off point of blood pressure can help patients to take earlier actions to prevent arteriosclerosis. Although we know that there is a close correlation between blood pressure and arteriosclerosis, the predictive performance and appropriate sex- and age-specific cut-off points of blood pressure for identifying arteriosclerosis have not been reported in Chinese adults. Therefore, this study aimed to assess the predictive performance and to develop sex- and age-specific blood pressure cut-off values for identifying arteriosclerosis.
2. Materials and Methods
2.1. Study Population
This study was designed as a cross-sectional study. We collected 9830 medical records from five cities in eastern China (Nanjing, Ningbo, Suzhou, Changzhou, and Taizhou) from 2015 to 2019. Height, weight, age, systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate, smoking and exercise status, and baPWV were the variables of interest. In order to minimize the confounding effects from antihypertensive drugs, we excluded 215 subjects with a hypertension history who currently were taking antihypertensive drugs and with blood pressure controlled to a normal range (SBP < 140 mmHg and DBP < 90 mmHg). Finally, we recruited 9615 qualified subjects aged 18 to 84 years, with 4766 women and 4849 men. This study was conducted in accordance with the Declaration of Helsinki. All the participants in this study signed an informed consent form. This study followed the principles outlined in the Declaration of Helsinki and was approved by the Institutional Review Board of the Faculty of Sports Science, Ningbo University.
2.2. Measurements
Basic information about participants was collected by professionals with questionnaires. The same measurement tools and protocol were adopted in each of the five cities.
Blood pressure measurement: After a 5-min rest, the seated brachial blood pressure of each participant was measured using a mercury sphygmomanometer with standard calibrations. BaPWV measurement: The baPWV was measured using an oscillometer-based device (BP-203RPE; Omron-Colin, Japan) by a trained technician. The subjects rested for at least 5 min in the supine position, with four cuffs wrapped around the upper arm and ankle, and then the arteries of the upper and lower extremity were measured simultaneously via a noninvasive shock pressure wave graph.
2.3. Definitions
Arteriosclerosis: Blood vessel elastic function was assessed by baPWV. Arteriosclerosis was defined by a baPWV ≥ 1400 cm/s [14,15,16]; hypertension: participants taking antihypertensive drugs or SBP ≥ 140 mmHg or DBP ≥ 90 mmHg; blood pressure grade: normal blood pressure, with SBP < 120 mmHg and DBP < 80 mmHg; high–normal blood pressure: SBP in the range of 120–139 mmHg and/or DBP in the range of 80–90 mmHg; grade 1 hypertension: SBP in the range of 140–159 mmHg and/or DBP in the range of 90–99 mmHg; grade 2 hypertension: SBP in the range of 160–179 mmHg and/or DBP in the range of 100–109 mmHg; grade 3 hypertension: SBP ≥ 180 mmHg and/or DBP ≥ 90 mmHg [17].
Smoking status: smokers were defined as those who smoked at least one cigarette per day continuously or cumulatively for 6 months [18]; exercise status: exercisers were defined as those who exercised through at least 30 min of moderate-intensity physical activity three times per week (60% to 90% of maximum heart rate reserve or 50% to 85% of maximum oxygen intake) [19,20]; Body Mass Index (BMI) = weight(kg)/height (m)2 [21].
2.4. Statistical Analysis
Statistical analysis was performed with SPSS software (version 25.0). Continuous variables (height, weight, BMI, resting heart rate, SBP, DBP, and baPWV) were presented as the mean ± standard deviation (SD); comparisons among groups were conducted by a one-way ANOVA. Comparisons of rates (arteriosclerosis%, hypertension%, smoker%, and exerciser%) were performed by a chi-square test. The predictive performance of blood pressure was evaluated by the area under the curve (AUC) of receiver operating characteristics (ROC) for identifying arteriosclerosis. Comparisons of AUCs between the two groups were conducted by a Z-test. The optimal cut-off points on the ROC curve were determined by the maximal Youden’s index (sensitivity + specificity − 1). Crude odds ratios (ORs), as well as adjusted ORs, were calculated by a multiple logistic regression model to analyze the association between blood pressure and arteriosclerosis. Adjusted factors included age, sex, resting heart rate, BMI, smoker, and exerciser, among which sex, smoking, and exercise status were treated as categorical variables. The percent attributable risk of the population (PARP) was calculated by the exposure percentage and ORs, based on the optimal cut-off points of blood pressure for identifying arteriosclerosis. The formula is given as follows: PARP = 100 × p (OR − 1)/[p (OR − 1) + 1]%.
3. Results
3.1. Baseline Characteristics of Subjects
A total of 9615 subjects were included in this study. Height, weight, BMI, heart rate, SBP, DBP, baPWV, and smoking and exercise statuses were collected. Of the included participants, 4849 were men, and 4766 were women; their ages ranged from 18 to 84 years. A small portion of the records on smoking and exercise were not collected in the questionnaire, and missing subjects therein were ignored. The Kolmogorov–Smirnov test showed that all the continuous variables (height, weight, BMI, resting heart rate, SBP, DBP, and baPWV) had a normal distribution, all of which were p > 0.05. There were differences in baseline measurements in sex and age groups, p < 0.01 (a one-way ANOVA test for continuous variables; a chi-square test was used for categorical variables). The characteristics of the subjects are shown in Table 1.
Table 1.
Baseline characteristics by sex and age in the subjects.
| Variables | Sex | Age (Yrs) | |||
|---|---|---|---|---|---|
| Women (n = 4766) |
Men (n = 4849) |
18–39.9 (n = 2901) |
40–59.9 (n = 5581) |
60–84 (n = 1133) |
|
| Height, cm | 159.2 ± 5.5 | 170.3 ± 6.1 a | 165.5 ± 8.1 | 165.1 ± 7.9 | 161.9 ± 8.2 a |
| Weight, Kg | 59.0 ± 8.5 | 72.6 ± 10.1 a | 63.4 ± 12.4 | 67.3 ± 11.1 | 65.1 ± 10.7 a |
| BMI, Kg/m2 | 23.3 ± 3.1 | 25.0 ± 3.0 a | 23.0 ± 3.4 | 24.6 ± 3.0 | 24.8 ± 3.1 a |
| HR, beats/min | 72.1 ± 9.8 | 73.0 ± 11.5 a | 72.7 ± 10.4 | 72.5 ± 10.4 | 72.6 ± 11.0 |
| SBP, mmHg | 117.8 ± 17.1 | 127.2 ± 15.3 a | 114.1 ± 13.4 | 124.6 ± 16.1 | 134.2 ± 18.5 a |
| DBP, mmHg | 69.5 ± 10.8 | 77.3 ± 10.7 a | 66.5 ± 9.7 | 76.2 ± 11.0 | 77.5 ± 10.1 a |
| BaPWV, cm/s | 1262.1 ± 242.6 | 1377.8 ± 232.7 a | 1163.3 ± 160.8 | 1343.8 ± 207.6 | 1608.1 ± 283.9 a |
| Arteriosclerosis, % (n) | 22.4 (1067) | 38.7 (1876) b | 7.9 (228) | 33.4 (1862) | 75.3 (853) b |
| Hypertension, % (n) Smoker, % (n) Exerciser, % (n) |
10.8 (514) 2.6 (105) 22.8 (910) |
19.9 (962) b 38.3 (1573) b 18.1 (741) b |
4.1 (119) 15.8 (388) 15.9 (387) |
17.7 (989) 22.7 (1069) 22.0 (1031) |
32.5 (368) b 23.0 (221) b 24.5 (233) b |
Note: values are the means ± SD or % (n); a one-way ANOVA test, p < 0.01; b chi-square test, p < 0.01. Abbreviations: BMI, body mass index; yrs, years; HR, heart rate; SBP, systolic blood pressure; DBP, diastolic blood pressure; baPWV, brachial–ankle pulse wave velocity.
3.2. Prevalence of Arteriosclerosis in Different Blood Pressure Grades
Among the 9615 subjects, 312 subjects with normal blood pressure had arteriosclerosis, with a prevalence of 6.9%. All of the 66 subjects with grade 3 hypertension had arteriosclerosis, with a prevalence of 100%. The prevalence of arteriosclerosis was raised with the increase in the blood pressure grade (p < 0.01). The relationships between blood pressure grades and the prevalence of arteriosclerosis are shown in Table 2.
Table 2.
Prevalence of arteriosclerosis in different blood pressure grades.
| Arteriosclerosis | Normal Blood Pressure |
High–Normal Blood Pressure | Grade 1 Hypertension |
Grade 2 Hypertension |
Grade 3 Hypertension |
|---|---|---|---|---|---|
| Positive, n | 312 | 1441 | 859 | 237 | 64 |
| Negative, n | 4209 | 2185 | 283 | 25 | 0 |
| Prevalence, % | 6.9% | 39.7% a | 75.2% a | 90.5% a | 100% a |
| p value a | - | <0.01 | <0.01 | <0.01 | <0.01 |
Notes: a chi-square test; the normal group was used as a reference, p < 0.01.
3.3. Predictive Performance and the Optimal Blood Pressure Cut-Off Points
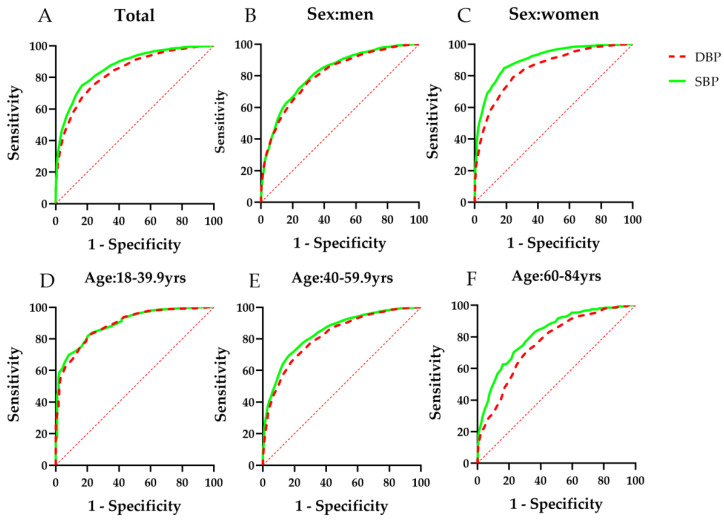
The AUC values of sex- and age-specific blood pressure for identifying arteriosclerosis were 0.868 for SBP and 0.835 for DBP, both of which had effective predictive performance (p < 0.01). The AUC values of both SBP and DBP for women for identifying arteriosclerosis were higher than those for men (Z test, p < 0.01). As age increased, the predictive performance of blood pressure for identifying arteriosclerosis decreased (Z test, p < 0.01). The details are shown in Figure 1 and Table 3.
Figure 1.
ROC curves of blood pressure for identifying arteriosclerosis in Chinese adults. (A) total subjects; (B) subjects in men; (C) subjects in women; (D) subjects aged 18 to 39.9 years; (E) subjects aged 40 to 59.9 years; (F) subjects aged 60 to 84 years; ROC, receiver operating characteristic; SBP, systolic blood pressure; DBP, diastolic blood pressure; yrs, years.
Table 3.
AUC values of sex- and age-specific blood pressure for identifying arteriosclerosis.
| Variables | SBP (95%CI) | DBP (95%CI) |
|---|---|---|
| Total | 0.868 (0.860–0.875) | 0.835 (0.827–0.843) |
| Sex | ||
| Women Men |
0.903 (0.893–0.913) 0.819 (0.807–0.831) a |
0.847 (0.834–0.860) 0.806 (0.793–0.818) a |
| Age(years) | ||
| 18–39.9 yrs | 0.894 (0.875–0.913) | 0.889 (0.869–0.909) |
| 40–59.9 yrs | 0.842 (0.832–0.853) b | 0.818 (0.807–0.829) b |
| 60–84 yrs | 0.818 (0.790–0.846) b | 0.759 (0.728–0.790) b |
Note: a compared with women, Z test, p < 0.05; b compared with 18–39.9 years, Z test, p < 0.05. Abbreviations: SBP, systolic blood pressure; DBP, diastolic blood pressure; yrs, years; AUC, area under the curve.
The optimal cut-off points of sex- and age-specific blood pressure for identifying arteriosclerosis were 123.5/75.5 mmHg (SBP/DBP), and the corresponding sensitivity/specificity reached 0.832/0.756 for SBP and 0.768/0.747 for DBP. According to their Youden’s index values, women and young groups had a higher predictive performance. The optimal cut-off points of SBP and DBP for men were higher than those for women; meanwhile, the cut-off points of the older group were slightly higher than those of the younger group (Table 4).
Table 4.
Optimal cut-off points, sensitivity, and specificity for blood pressure to identify arteriosclerosis.
| Variables | Optimal Cut-Off Points (mmHg) | Sensitivity | Specificity | Youden’s Index | ||||
|---|---|---|---|---|---|---|---|---|
| SBP | DBP | SBP | DBP | SBP | DBP | SBP | DBP | |
| Total | 123.5 | 75.5 | 0.832 | 0.768 | 0.756 | 0.747 | 0.588 | 0.515 |
| Sex | ||||||||
| Women | 123.5 | 73.5 | 0.815 | 0.0.758 | 0.848 | 0.790 | 0.663 | 0.548 |
| Men | 126.5 | 79.5 | 0.761 | 0.703 | 0.719 | 0.763 | 0.480 | 0.466 |
| Age(years) | ||||||||
| 18–39.9 yrs | 120.5 | 73.5 | 0.798 | 0.781 | 0.818 | 0.829 | 0.616 | 0.610 |
| 40–59.9 yrs | 123.5 | 76.5 | 0.836 | 0.793 | 0.694 | 0.683 | 0.530 | 0.476 |
| 60–84 yrs | 126.5 | 75.5 | 0.770 | 0.678 | 0.704 | 0.719 | 0.474 | 0.395 |
Abbreviations: SBP, systolic blood pressure; DBP, diastolic blood pressure; yrs, years.
3.4. ORs in the Multiple Logistic Regression Model and PARP on Arteriosclerosis
The AUC values of sex- and age-specific blood pressure for identifying arteriosclerosis were 0.868 for SBP and 0.835 for DBP, both with effective predictive performance (p < 0.01). The multivariate logistic regression model on arteriosclerosis was adjusted by age, sex, resting heart rate, BMI, smoking status, and exercise status. Compared with the subjects below the optimal blood pressure cut-off points (shown in Table 4), the crude OR value of those who had a higher blood pressure was 15.887; meanwhile, the adjusted OR value decreased significantly to 8.845. With regard to the features of sex or age, the relative OR values of women were larger than those of men, while the OR values decreased gradually with an increase in age. According to the adjusted OR and exposure percentage, the total PARP of blood pressure was 70.6% (sex- and age-specific PARP reached 70.1% and 70.0% in women and men, respectively, and 50.2%, 75.8%, and 84.9% in 18–39.9-years, 40–59.9-years, and 60–80-years groups, respectively). The details are listed in Table 5.
Table 5.
ORs (95% CI) in the multiple logistic regression model and PARP of arteriosclerosis based on optimal cut-off points for blood pressure.
| Variables | Crude OR (95%CI) | Adjusted OR (95%CI) | PARP |
|---|---|---|---|
| Total a | 15.887 (14.036–17.981) | 8.845 (7.694–10.168) | 70.6% |
| Sex b | |||
| Women | 20.022 (16.541–24.237) | 11.429 (9.116–14.330) | 70.1% |
| Men | 9.030 (7.837–10.404) | 6.243 (5.340–7.300) | 70.0% |
| Age(years) c | |||
| 18–39.9 yrs | 25.480 (15.152–36.604) | 13.759 (8.379–20.042) | 50.2% |
| 40–59.9 yrs | 12.749 (10.666–15.239) | 10.367 (8.618–12.472) | 75.8% |
| 60–84 yrs | 8.940 (6.449–12.394) | 8.512 (6.294–11.510) | 84.9% |
Notes: a adjusted OR: adjusted for age, sex, resting heart rate, BMI, smoking status, and exercise status; b adjusted OR: adjusted for age, resting heart rate, BMI, smoking status, and exercise status; c adjusted OR: adjusted for sex, resting heart rate, BMI, smoking status, and exercise status. Abbreviations: yrs, years; OR, odds ratio; CI, confidence interval; PARP, population attributable risk proportion.
4. Discussion
Arteriosclerosis measured by baPWV was a strong predictor of cardiovascular mortality [13,22,23]. Thus, the early detection of arteriosclerosis or arterial stiffness could help to assess the risk stratification and reduce the prevalence of cardiovascular events. In the past decade, studies have investigated the relationships between blood pressure and arteriosclerosis or high arterial stiffness, measured by pulse wave velocity in different populations worldwide [24,25]. Studies in Japan found that SBP, mean arterial pressure (MAP), and arterial stiffness are closely related [26,27]; Wang et al. found that increased blood pressure was the main factor affecting arteriosclerosis in Chinese adults [28]. Arteriosclerosis has multiple risk factors, such as age, sex, blood pressure, blood glucose, lifestyle, etc. [26,28]. Due to the convenience of measuring blood pressure, assessing the predictive performance of blood pressure for arteriosclerosis could facilitate screening arteriosclerosis earlier. Therefore, our aims were to assess predictive performance and to establish the optimal cut-off points for blood pressure in identifying arteriosclerosis in the Chinese population. The prevalence of hypertension changes significantly with age and sex. Accordingly, we stratified the data by age and sex and developed the sex- and age-specific predictive performance of blood pressure. We retained samples from all ages so that we could analyze the characteristics of age.
The prevalence of arteriosclerosis was high in our study because it is more sensitive to diagnosis under the same vessel condition. As blood pressure levels increased, the prevalence of arteriosclerosis also gradually increased. Our result, that there was a positive correlation between blood pressure and arteriosclerosis, is consistent with previous studies [26,27,28]. It is widely known that many factors, such as age, gender, family history of coronary artery disease, hyperlipidemia, smoking, eating habits, etc., can affect both hypertension and arteriosclerosis. Therefore, these factors could be considered potential confounders when studying the association between blood pressure and arteriosclerosis. For example, the percentage of smokers was very different among different sex and age groups in the baseline of this study, which may have led to potential confounding bias in the sex- and age-specific associations between blood pressure and arteriosclerosis. In general, a stratified analysis can be used to deal with confounding bias. When multiple potential confounding factors exist, a multiple logistic regression model is a better statistical method, due to the advantage of controlling the mixed relationship between multiple factors. Therefore, we used a multiple logistic regression model to control the confounding factors of sex, age, BMI, smoking and exercise status for analyzing the association between blood pressure and arteriosclerosis. However, in this study, some CVD risk factors, such as hypercholesterolemia and hyperglycemia, were not considered due to the lack of blood biochemical indicators, which may have overestimated the effects of ORs in the multiple logistic regression model and the effects of PARP. Our main results regarding the predictive performance and optimal cut-off points of blood pressure were relatively less affected by these potential confounding factors because the AUCs of the ROC curve and the cut-off points for identifying arteriosclerosis are stable and independent. In addition, we also considered the effects of hypertension drugs. Pharmacological treatment can affect blood pressure and, thus, would be a confounding factor in a blood pressure study. Wilkinson et al. have suggested that studies should start in youth to minimize the initial confounding effects of arteriosclerosis and pharmacological treatment [29]. In order to minimize the confounding effects of antihypertensive drugs, we excluded 215 subjects with a hypertension history who were currently using antihypertensive drugs and whose blood pressure was controlled in the normal range.
Generally, the predictive performance, which ranges from 0.5–1, is determined by the AUC of the ROC curve. An area that exceeds 0.8 indicates good predictive performance. The results of the AUCs indicated that two kinds of blood pressure indexes have a high predictive performance for arteriosclerosis. The AUCs of SBP and DBP to assess arteriosclerosis were 0.868 and 0.835, respectively. Although blood pressure can predict arteriosclerosis well, it may be more accurate to predict arteriosclerosis when combined with other indicators [6]. The optimal cut-off points of SBP/DBP for predicting arteriosclerosis were 123.5/75.5 mmHg, respectively. The clinical diagnostic standard of hypertension is 140/90 mmHg, while the optimal blood pressure cut-off points calculated in our study for predicting arteriosclerosis were lower than the diagnostic standard. If the clinical diagnostic standard of hypertension is applied to predict arteriosclerosis, many subjects with arteriosclerosis will be erroneously diagnosed. Our results of blood pressure cut-off points were close to the diagnostic values for those with high–normal blood pressure (120/80mmHg for SBP/DBP), which indicates that people with high–normal blood pressure have a higher risk of arteriosclerosis. A cohort study considered a blood pressure cut-off threshold of <122.5/76 mmHg as being optimal for discriminating cardiovascular mortality; meanwhile, the cut-off point of <135/83 mmHg for blood pressure has an independent prognostic value of cardiovascular mortality [30]. Another cohort study recommended 130/80 mmHg as the optimal cut-off threshold in self/home blood pressure measurements [31]. Our research indicates that even if blood pressure does not meet the diagnostic standard for hypertension (140/90 mmHg for SBP/DBP), when the SBP or DBP exceeds 123.5 or 75.5 mmHg, respectively, people also are exposed to the risk of encountering arteriosclerosis.
In the current study, the predictive performance of blood pressure for identifying arteriosclerosis in sex and age was different. The AUCs for SBP/DBP (0.902/0.846) were higher in women than in men (0.819/0.806), which indicates that the predictive performance for women would be more accurate and also revealed a closer relationship with arteriosclerosis in women. Further analysis through multiple logistic regression showed that the OR value of women (11.4) was greater than that of men (6.2), which was adjusted by age, resting heart rate, BMI, and smoking and exercising status. Although women, in general, have a lower absolute prevalence of arteriosclerosis, when women with a higher blood pressure are defined by the optimal cut-off threshold, they will have a higher relative risk of arteriosclerosis due to the higher OR value. Therefore, we suggest that women should pay attention to the risk of arteriosclerosis as their blood pressure increases. Pertaining to age characteristics, the younger groups showed a higher predictive performance of blood pressure for identifying arteriosclerosis due to higher AUCs. Moreover, as age increased, the adjusted OR values showed a decreasing trend from 13.8 to 10.4 to 8.5, which indicates that young people with high blood pressure have a higher relative risk of arteriosclerosis. It is well known that hypercholesterolemia is one of the main determinants of arteriosclerosis. Thus, it is notable that the above OR values may be overestimated due to the lack of data on the prevalence of hypercholesterolemia and hypertriglyceridemia in the multiple logistic regression model. Tuscarora et al. showed that advanced age and being male are associated with a higher baPWV [32]. Ai et al. found that age has an influence on baPWV, the effect of which is more obvious in women [33]. Although there is compelling evidence to support the fact that being male or aging are significant risk factors for arteriosclerosis [26,27,28,29], the association between blood pressure and arteriosclerosis was stronger in women or the younger population. As a result, women or the younger population might have a higher predictive performance and lower cut-off points for identifying arteriosclerosis. In addition, our study also implied that there may be interaction on arteriosclerosis between blood pressure, age, and sex-based on the sex- and age-specific OR values calculated by the logistic regression analysis. Further multiplicative or additive interaction statistics might contribute to the analysis of the interaction between multiple factors with arteriosclerosis. The results of this study suggest the importance of the early prevention and treatment of hypertension in reducing the risk of arteriosclerosis. The target population for the prevention of arteriosclerosis is not only limited to patients with hypertension. Those who have high–normal blood pressure should also be concerned with the risk of arteriosclerosis. According to the maximal Youden’s index (sensitivity + specificity − 1) of the ROC curve, we determined the corresponding optimal sex- and age-specific cut-off points of blood pressure for identifying arteriosclerosis among adults in China. Women or the younger population have lower cut-off points for both SBP and DBP than men or the older population. Based on these results, we calculated the PARP according to adjusted ORs and exposure percentages. The epidemiological significance of the PARP analysis showed that if intervention measures are taken to control blood pressure below the optimal cut-off points (123.5 mmHg for SBP and 75.5 mmHg for DBP), 70.6% of arteriosclerosis would be prevented across the whole population. If blood pressure is controlled under 123.5/73.5 mmHg for women, 126.5/79.5 mmHg for men, 120.5/73.5 mmHg for 18–39.9 years, and 126.5/75.5 mmHg for 60–84 years, 50.2–84.9% of arteriosclerosis would be prevented.
At present, instruments to measure baPWV are complex and expensive; therefore, this method is mainly applied in large hospitals in China. However, blood pressure can easily be measured in the ordinary population in any primary hospital or community in China. Thus, the application of the predictive performance of blood pressure to identifying arteriosclerosis could help doctors make better decisions and suggestions. Overall, our study showed that blood pressure has a high predictive performance for arteriosclerosis.
5. Conclusions
Blood pressure indexes had a high predictive performance for identifying arteriosclerosis with the optimal cut-off point of 123.5/73.5 mmHg (SBP/DBP) in eastern Chinese adults. Women or the younger population have a higher predictive performance and lower cut-off points to identify arteriosclerosis.
Limitations
There are some limitations to our study. The present study is cross-sectional design, which cannot be used to establish temporal relationship and causality; thus, the validation of optimal cut-off points needs further prospective cohort studies as support. Second, a lack of data on prevalence of hypercholesterolemia and hypertriglyceridemia in the multiple logistic regression model may lead to an overestimation of ORs and PARP. Finally, the subjects were from five cities in eastern China, so the study’s findings cannot necessarily be representative of all Chinese adults.
Acknowledgments
We would like to thank the doctors of the Affiliated Hospital of Ningbo University and Jiangsu Research Institute of Sports Science for the helpful support they provided to us.
Abbreviations
| ROC | receiver operating characteristic |
| AUC | area under the curve |
| OR | odds ratio |
| PARP | percent attributable risk of population |
| SBP | systolic blood pressure |
| DBP | diastolic blood pressure |
| baPWV | brachial–ankle pulse wave velocity |
| yrs | years |
| HR | heart rate |
| CI | confidence interval |
| BMI | body mass index |
Author Contributions
Study concept and design, L.Y. and H.H.; data acquisition, analysis, and interpretation, L.Y. and J.Y.; preparation of the manuscript and figures, Y.G., H.H. and C.Y.; provided data sources, H.H. and A.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Social Science Foundation of China, grant number (grant 18BTY100).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of the Faculty of Sports Science, Ningbo University (NO.2018RAGH1025).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jacques B., Roland A., Saliha D., Gerard M.L., Michel E.S. Aortic Pulse Wave Velocity as a Marker of Cardiovascular Risk in Hypertensive Patients. Hypertension. 1999;33:1111–1117. doi: 10.1161/01.hyp.33.5.1111. [DOI] [PubMed] [Google Scholar]
- 2.Lonn E., Yusuf S., Dzavik V., Doris C., Yi Q., Smith S., Moore-Cox A., Bosch J., Riley W., Teo K. Effects of ramipril and vitamin E on atherosclerosis: The study to evaluate carotid ultrasound changes in patients treated with ramipril and vitamin E (SECURE) Circulation. 2001;103:919–925. doi: 10.1161/01.CIR.103.7.919. [DOI] [PubMed] [Google Scholar]
- 3.Ma L.Y., Chen W.W., Gao R.L., Liu L.S., Zhu M.L., Wang Y.J., Wu Z.S., Li H.J., Gu D.F., Yang Y.J., et al. China cardiovascular diseases report 2018: An updated summary. J. Geriatr. Cardiol. 2020;17:1–8. doi: 10.11909/j.issn.1671-5411.2020.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sung J., Cho S.J., Hong K.P. Relationship between fitness and arterial stiffness according to hypertensive state. Clin. Exp. Hypertens. 2019;41:733–738. doi: 10.1080/10641963.2018.1545849. [DOI] [PubMed] [Google Scholar]
- 5.Ohkuma T., Ninomiya T., Tomiyama H., Kario K., Hoshide S., Kita Y., Inoguchi T., Maeda Y., Kohara K., Tabara Y., et al. Brachial-Ankle Pulse Wave Velocity and the Risk Prediction of Cardiovascular Disease: An Individual Participant Data Meta-Analysis. Hypertension. 2017;69:1045–1052. doi: 10.1161/HYPERTENSIONAHA.117.09097. [DOI] [PubMed] [Google Scholar]
- 6.Takami T., Shigemasa M. Efficacy of various antihypertensive agents as evaluated by indices of vascular stiffness in elderly hypertensive patients. Hypertens. Res. 2003;26:609–614. doi: 10.1291/hypres.26.609. [DOI] [PubMed] [Google Scholar]
- 7.Munakata M., Nagasaki A., Nunokawa T., Sakuma T., Kato H., Yoshinaga K., Toyota T. Effects of valsartan and nifedipine coat-core on systemic arterial stiffness in hypertensive patients. Am. J. Hypertens. 2004;17:1050–1055. doi: 10.1016/j.amjhyper.2004.06.028. [DOI] [PubMed] [Google Scholar]
- 8.Uchida H., Nakamura Y., Kaihara M., Sugimoto T., Norii H., Sasaki M., Sato H., Makino H. Practical efficacy of telmisartan for decreasing morning home blood pressure and pulse wave velocity in patients with mild-to-moderate hypertension. Hypertens. Res. 2004;27:545–550. doi: 10.1291/hypres.27.545. [DOI] [PubMed] [Google Scholar]
- 9.Mancia G., Fagard R., Narkiewicz K., Redon J., Zanchetti A., Böhm M., Christiaens T., Cifkova R., De Backer G., Dominiczak A., et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur. Heart J. 2013;34:2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 10.Boutouyrie P., Tropeano A.I., Asmar R., Gautier I., Benetos A., Lacolley P., Laurent S. Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: A longitudinal study. Hypertension. 2002;39:10–15. doi: 10.1161/hy0102.099031. [DOI] [PubMed] [Google Scholar]
- 11.Roderjan C.N., Cardoso C.R., Ferreira M.T., Muxfeldt E.S., Salles G.F. Correlates of aortic stiffness progression in patients with resistant hypertension: Importance of clinic and ambulatory blood pressure changes. J. Hypertens. 2015;33:827–835. doi: 10.1097/HJH.0000000000000491. [DOI] [PubMed] [Google Scholar]
- 12.Sheng C.S., Li Y., Li L.H., Huang Q.F., Zeng W.F., Kang Y.Y., Zhang L., Liu M., Wei F.F., Li G.L., et al. Brachial-Ankle pulse wave velocity as a predictor of mortality in elderly Chinese. Hypertension. 2014;64:1124–1130. doi: 10.1161/HYPERTENSIONAHA.114.04063. [DOI] [PubMed] [Google Scholar]
- 13.Maeda Y., Inoguchi T., Etoh E., Kodama Y., Sasaki S., Sonoda N., Nawata H., Shimabukuro M., Takayanagi R. Brachial-Ankle pulse wave velocity predicts all-cause mortality and cardiovascular events in patients with diabetes: The Kyushu Prevention Study of Atherosclerosis. Diabetes Care. 2014;37:2383–2390. doi: 10.2337/dc13-1886. [DOI] [PubMed] [Google Scholar]
- 14.Imanishi R., Seto S., Toda G., Yoshida M., Ohtsuru A., Koide Y., Baba T., Yano K. High brachial-ankle pulse wave velocity is an independent predictor of the presence of coronary artery disease in men. Hypertens. Res. 2004;27:71–78. doi: 10.1291/hypres.27.71. [DOI] [PubMed] [Google Scholar]
- 15.Koji Y., Tomiyama H., Ichihashi H., Nagae T., Tanaka N., Takazawa K., Ishimaru S., Yamashina A. Comparison of ankle-brachial pressure index and pulse wave velocity as markers of the presence of coronary artery disease in subjects with a high risk of atherosclerotic cardiovascular disease. Am. J. Cardiol. 2004;94:868–872. doi: 10.1016/j.amjcard.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 16.Tanaka H., Munakata M., Kawano Y., Ohishi M., Shoji T., Sugawara J., Tomiyama H., Yamashina A., Yasuda H., Sawayama T., et al. Comparison between carotid-femoral and brachial-ankle pulse wave velocity as measures of arterial stiffness. J. Hypertens. 2009;27:2022–2027. doi: 10.1097/HJH.0b013e32832e94e7. [DOI] [PubMed] [Google Scholar]
- 17.Writing Group of 2018 Chinese Guidelines for the Management of Hypertension. Chinese Hypertension League. Chinese Society of Cardiology. Chinese Medical Doctor Association Hypertension Committee. Hypertension Branch of China International Exchange and Promotive Association for Medical and Health Care. Hypertension Branch of Chinese Geriatric Medical Association China Guidelines for Prevention and Treatment of Hypertension (2018 Revised Edition) Chin. J. Cardiovasc. Dis. 2019;24:24–56. [Google Scholar]
- 18.He Q., Gao Y. Definitions of several terms on smoking. Chin. J. Tuberc. Respir. Med. 2009;1:26. (In Chinese) [Google Scholar]
- 19.Bureau of Disease Control and Prevention, Ministry of Health of the People’s Republic of China Chinese adult physical activity guide (excerpt) Acta Nutr. Sin. 2012;34:105–110. (In Chinese) [Google Scholar]
- 20.Garber C.E., Blissmer B., Deschenes M.R., Franklin B.A., Lamonte M.J., Lee I.-M., Nieman D.C., Swain D.P. American College of Sports Medicine position stand. Quantity and Quality of Exercise for Developing and Maintaining Cardiorespiratory, Musculoskeletal, and Neuromotor Fitness in Apparently Healthy Adults. Med. Sci. Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 21.Zhou B. Coorperative Meta-Analysis Group Of China Obesity Task Force:Predictive values of body mass index and waist circumference to risk factors of related diseases in Chinese adult population. Zhonghua Liu Xing Bing Xue Za Zhi. 2002;23:5–10. [PubMed] [Google Scholar]
- 22.Bönner G., Gysan D.B., Sauer G. Prevention of arteriosclerosis. Importance of the treatment of arterial hypertension. Z. Kardiol. 2005;94:III56–III65. doi: 10.1007/s00392-005-1308-9. [DOI] [PubMed] [Google Scholar]
- 23.Jiang Y., Fan F., Jia J., Li J., Xia Y., Zhou J., Huo Y., Zhang Y. Brachial-Ankle Pulse Wave Velocity Predicts New-Onset Hypertension and the Modifying Effect of Blood Pressure in a Chinese Community-Based Population. Int. J. Hypertens. 2020;2020:9075636. doi: 10.1155/2020/9075636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adriaan C., Grzegorz D., Jason A., Adam W., Pierre N., Krzysztof A., Joris D., Elisa K. Comparison between multi-channel LDV and PWI for measurement of pulse wave velocity in distensible tubes: Towards a new diagnostic technique for detection of arteriosclerosis. J. Opt. Lasers Eng. 2017;97:41–51. [Google Scholar]
- 25.Tsuneo T., Kenji K., Hiromichi S. Pulse wave velocity as an indicator of arteriosclerosis in hemodialysis patients. J. Atheroscler. 2004;176:405–409. doi: 10.1016/j.atherosclerosis.2004.05.024. [DOI] [PubMed] [Google Scholar]
- 26.Sheng S. Mean arterial pressure and arterial stiffness in Japanese population: A secondary analysis based on a cross-sectional study. Blood Press. Monit. 2020;25:310–317. doi: 10.1097/MBP.0000000000000471. [DOI] [PubMed] [Google Scholar]
- 27.Ishida A., Fujisawa M., Del Saz E.G., Okumiya K., Kimura Y., Manuaba I.I.B., Kareth M.F., Rantetampang A.L., Ohya Y., Matsubayashi K. Arterial stiffness, not systolic blood pressure, increases with age in native Papuan populations. Hypertens. Res. 2018;41:539–546. doi: 10.1038/s41440-018-0047-z. [DOI] [PubMed] [Google Scholar]
- 28.Wang A.X., Su Z.P., Liu X.X., Yang Y.L., Chen S.H., Wang S.L., Luo Y.X., Guo X.H., Zhao X.Q., Wu S.L. Brachial-Ankle pulse wave velocity and metabolic syndrome in general population: The APAC study. BMC Cardiovasc. Disord. 2016;16:228. doi: 10.1186/s12872-016-0409-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilkinson I.B., McEniery C.M., Cockcroft J.R. Arteriosclerosis and atherosclerosis: Guilty by association. Hypertension. 2009;54:1213–1215. doi: 10.1161/HYPERTENSIONAHA.109.142612. [DOI] [PubMed] [Google Scholar]
- 30.Sega R., Facchetti R., Bombelli M., Cesana G., Corrao G., Grassi G., Mancia G. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population. Follow-Up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111:1777–1783. doi: 10.1161/01.CIR.0000160923.04524.5B. [DOI] [PubMed] [Google Scholar]
- 31.Coll-de-Tuero G., Saez M., Rodriguez-Poncelas A., Bayó-Llibre J., Beltran-Vilella M., Reyes-Negre C., Dalfó-Baqué A., Barceló M. What is the optimal cut-off threshold in self-home blood pressure measurement? Medicine. 2019;98:e14817. doi: 10.1097/MD.0000000000014817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tsuchikura S., Shoji T., Kimoto E., Shinohara K., Hatsuda S., Koyama H., Emoto M., Nishizawa Y. Brachial-Ankle pulse wave velocity as an index of central arterial stiffness. J. Atheroscler. Thromb. 2010;17:658–665. doi: 10.5551/jat.3616. [DOI] [PubMed] [Google Scholar]
- 33.Ai Z.S., Li J., Liu Z.M., Fan H.M., Zhang D.F., Zhu Y., Zhang L.J., Zhu W.Q., Bao Y. Reference value of brachial-ankle pulse wave velocity for the eastern Chinese population and potential influencing factors. Braz. J. Med. Biol. Res. 2011;44:1000–1005. doi: 10.1590/s0100-879x2011007500108. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.