Key Points
Question
What is the prevalence of decisional conflict for surgical patients during the early phases of the COVID-19 pandemic?
Findings
In this cross-sectional survey study of 182 patients scheduled for otolaryngologic surgery during the pandemic, non-White participants without college education were 10 times more likely to screen positive for decisional conflict compared with college-educated White participants. Concerns about intraoperative and postoperative processes were more prominent than COVID-19 concerns.
Meaning
The results of this survey study suggest the need for health care professionals to converse with patients about patient values, beliefs, and specific concerns about treatment; future studies to elucidate racial health care inequities are warranted.
Abstract
Importance
A patient’s decision to undergo surgery may be fraught with uncertainty and decisional conflict. The unpredictable nature of the COVID-19 pandemic warrants further study into factors associated with patient decision-making.
Objective
To assess decisional conflict and patient-specific concerns for people undergoing otolaryngologic surgery during the pandemic.
Design, Setting, Participants
This prospective cross-sectional survey study was conducted via telephone from April 22 to August 31, 2020. English-speaking adults scheduled for surgery from a single academic surgical center were invited to participate. Individuals who were non-English speaking, lacked autonomous medical decision-making capacity, scheduled for emergent surgery, or had a communication disability were excluded. For race and ethnicity reporting, participants were classified dichotomously as White according to the Behavioral Risk Factor Surveillance System from the Centers for Disease Control and Prevention or non-White as a collective term including Black or African American, American Indian or Alaska Native, Asian, or Pacific Islander race and ethnicity.
Exposures
The SURE Questionnaire (sure of myself, understand information, risks/benefits ratio, and encouragement) was used to screen for decisional conflict, with a total score greater than or equal to 3 indicating clinically significant decisional conflict. Participants were asked to share their specific concerns about having surgery.
Main Outcome and Measures
Decisional conflict and patient demographic data were assessed via bivariate analyses, multivariable logistic regression and conjunctive consolidation. Patient-specific concerns were qualitatively analyzed for summative themes.
Results
Of 444 patients screened for eligibility, 182 (40.9%) respondents participated. The median age was 60.5 years (interquartile range, 48-70 years). The racial and ethnic identity of the participants was classified as binary White (84% [153 of 182]) and non-White (16% [29 of 182]). The overall prevalence of decisional conflict was 19% (34 of 182). Decisional conflict was more prevalent among non-White than White participants (proportion difference 18.8%, 95% CI, 0.6%-37.0% and adjusted odds ratio 3.0; 95% CI, 1.2-7.4). Combining information from multiple variables through conjunctive consolidation, the group with the highest rate of decisional conflict was non-White patients with no college education receiving urgent surgery (odds ratio, 10.8; 95% CI, 2.6-45.0). Intraoperative and postoperative concerns were the most common themes expressed by participants. There was a clinically significant difference in the proportion of participants who screened positive for decisional conflict (30%) and expressed postoperative concerns than those who screened negative for decisional conflict (17%) (proportion difference, 13%; 95% CI, 1%-25%). Among patients reporting concerns about COVID-19, most screened positive for decisional conflict.
Conclusions and Relevance
Results of this cross-sectional survey study suggest that the COVID-19 pandemic was associated with decisional conflict in patients undergoing otolaryngologic surgery. Consistent discussion of risks and benefits is essential. The role of race and ethnicity in decisional conflict warrants further study.
This survey study assesses the prevalence of decisional conflict, patient-specific concerns, and the association between patient factors and decisional conflict in patients undergoing otolaryngologic surgery during the COVID-19 pandemic.
Introduction
The decision to undergo surgery can be burdened with many sources of uncertainty, particularly in patients considering elective surgery or diagnoses with equivocal surgical and nonsurgical treatment options. Even when surgery is clearly the superior treatment, there exist patient concerns about factors surrounding the surgery. Shared decision-making (SDM), a patient-centered process using the best available evidence with the patient’s values and beliefs,1 has been reported to improve clinical outcomes, patient adherence to treatment, and patient feelings of empowerment.2,3 Decisions about surgery are fraught with complex medical considerations, patient concerns, and other psychosocial issues, such as attempting to comprehend the medical situation, recovery time, and associated costs of surgery and hospitalization.3 Each patient and clinical encounter are unique, requiring consideration of patient values, limitations, and treatment goals. One aspect of SDM is decisional conflict (DC), the difficulties patients face when making a decision about their care.4 Unresolved DC has negative consequences, ie, decisional regret or decreased patient satisfaction.5
The COVID-19 pandemic6,7 and efforts to curb disease spread, including social distancing policies, had substantial consequences for medical care and possibly added an additional layer of uncertainty and DC.
Published otolaryngology research reports DC varies between 13% and 43%.4,8,9,10,11,12,13,14 These studies measured DC in cases for which surgery was equivocal: pediatric otologic surgery or adenotonsillectomy,8,9,10,11,12,14 surgical and nonsurgical management of vestibular schwannoma,4 or surgery vs surveillance for indeterminate thyroid nodules.13 A study by Shuman et al15 explored DC in patients treated for laryngeal carcinoma and found, on average, clinically significant DC. These studies of mostly elective surgeries do not include qualitative exploration of patient-specific concerns.
The uncertainty of the global pandemic warrants research into how similar large-scale events in the future could affect SDM. Our goal was to measure the prevalence of DC in patients undergoing otolaryngologic surgery during a snapshot in time: the early phases of the COVID-19 pandemic. We sought to build on previous studies by identifying patient-specific factors associated with DC.
Thus, we aimed to determine the prevalence of DC; illuminate patient-specific concerns; and determine the association between patient factors and DC in patients having otolaryngologic surgery during the COVID-19 pandemic. We hypothesized that patients would have specific concerns about their surgery that persist despite the pandemic and that the overall prevalence of DC will be greater in the pandemic setting than that reported in previous literature.
Methods
Context
Patients deciding to undergo surgery experience uncertainty across the spectrum of surgical care, from elective surgery to emergency surgery. The need for physicians to understand patient concerns and engage in SDM is heightened in the setting of a global pandemic.
Study Design and Setting
This survey study was conducted via telephone from April 22 to August 31, 2020, at a single tertiary care academic hospital. All patients were contacted at least 12 hours before their scheduled surgery and screened for eligibility over the telephone. Potential participants were identified from the surgery schedules of 8 surgeons in 3 subspecialties: head and neck surgery, facial plastic and reconstructive surgery, and laryngology. This study has been granted a waiver by the institutional review board of Washington University in St Louis of Health Insurance Portability and Accountability Act of 1996 authorization per section 164.512(i) of the Privacy Rule to allow the research team to use Protected Health Information in the context of this research study.
Patient Selection
Inclusion criteria were English-speaking adults (≥18 years) scheduled to undergo otolaryngologic surgery. Individuals who could not speak English, lacked autonomous medical decision-making capacity, currently admitted or in the emergency department for imminent surgery without an initial outpatient visit, or who had a communication disability precluding telephone interview (ie, profound deafness, aphonia) were excluded.
Demographic data and screening for DC were gathered by close-ended interview and review of the electronic medical record. Patient-specific concerns were obtained by open-ended interview. Study data were collected and managed using the Research Electronic Data Capture tool hosted at Washington University.16,17
Ethical Considerations
Neither the telephone interviewer nor the patient-specific response reviewers were involved in direct patient care at any point. All patients were given the option to decline study participation. Patients were assured their participation and responses would not affect their care. All care clinicians were blinded to patient participation and responses.
Decisional Conflict
The SURE (sure of myself, understand information, risks/benefits ratio, and encouragement) Questionnaire is a 4-item screening tool for DC, scored with a “yes” (1 point) or “no” (0 points).5 A total score greater than or equal to 3 is a positive result (clinically significant DC present); a total score of 4 is a negative result (clinically significant DC absent). The questionnaire was adapted from the Decisional Conflict Scale (DCS)5,18 and both have been used in research studies of surgical patients.4,8,9,10,11,12,13,14,19 The SURE Questionnaire is highly accurate, sensitive, and specific, and minimizes participant burden.5
Patient-Specific Concerns
Patients can be expected to have concerns encompassing disease state or diagnosis, perioperative events, pain, cost, and recovery. In the context of the COVID-19 pandemic, other concerns may also arise, such as fear of contracting the virus, uncertainty about quarantine, and the role of family involvement during inpatient post-surgical recovery, given hospital restrictions on visitor policies. Participants were prompted with the statement “Please list any concerns you have about undergoing your scheduled surgery at this time” to identify particular themes and subthemes of their specific concerns.
Demographic and Clinical Characteristics
Demographic data included age, sex, race and ethnicity, marital status, educational status, type of surgery, date of surgery, medical and surgical histories, and COVID-19 testing information. For analysis, demographic categories were dichotomized. For example, patients who identified as White or Caucasian comprised a single category consistent with the Behavioral Risk Factor Surveillance System from the Centers for Disease Control and Prevention.20 We included patients who identified as American Indian or Alaskan Native, Asian, Black or African American or more than 1 race and ethnicity as a separate collective non-White category. During the study period, surgical scheduling followed the tier structure in guidelines published by the American College of Surgeons.21 Specifically, urgent surgery was structured as Tier 3a (“most cancers, highly symptomatic patient”) and Tier 3b (“high acuity surgery/unhealthy patient”) classifications21; elective surgery was structured as outpatient Tier 2a (“intermediate acuity surgery/healthy patient”) and Tier 2b (“intermediate acuity surgery/unhealthy patient”) classifications.21 Medical comorbidities were graded using the Adult Comorbidity Evaluation-27 (ACE-27) score.22 To assess the COVID-19 pandemic in terms of patient concerns, the date of surgery was dichotomized as “during stay-at home period” or “after stay-at home period,” corresponding to the statewide Missouri stay-at-home order that was in effect until May 4, 2020.23
Statistical Analysis
Descriptive statistics summarized the distribution of demographic variables. Categories were compared between decisional conflict present vs absent groups using χ2 test of independence, unless otherwise indicated. The association between demographic categories or quantities and the primary outcome (present or absent DC) was measured as proportion difference or median difference with the corresponding 95% CI. Conjunctive consolidation, a method of stratifying the data within clusters using cross-table analysis based on statistical isometry, was used post hoc to show the composite effect sizes of combined demographic variables on the primary outcome.24,25 Through this method of stratified analysis, trends in the data are used to assess potential factors associated with high rates of DC. The composite effect size in conjunctive consolidation is a way of exploring interaction outcomes. An interaction outcome can be explored in a multivariable analysis, but its assessment is heavily weighted in statistical significance, and thus associated with sample size. It is not uncommon for important interaction outcomes to be identified as not statistically significant. In conjunctive consolidation, evaluation is based on effect size or the clinical importance of the outcome and not the P values. The C statistic quantified the discriminative power of multivariable models of the staging systems created from the conjunctive consolidation process. Post hoc logistic regression models analyzed potential confounding variables or interaction effects. All statistical analyses were performed at a 2-sided α level of .05. Analyses were conducted using SPSS Statistics, version 27 (IBM Corporation). To our knowledge, this is the first study to date analyzing DC in surgery during the COVID-19 global pandemic, thus we planned to analyze a convenience sample of all eligible patients scheduled for surgery during the study period.
Two independent reviewers (N.S.W. and S.P.G.) performed summative content analyses of patient-specific concerns using NVivo software, version 12 (QSR International), via line-by-line coding into themes and subthemes. Any remaining discrepancy in coding was resolved by the senior author (J.J.C.).
Results
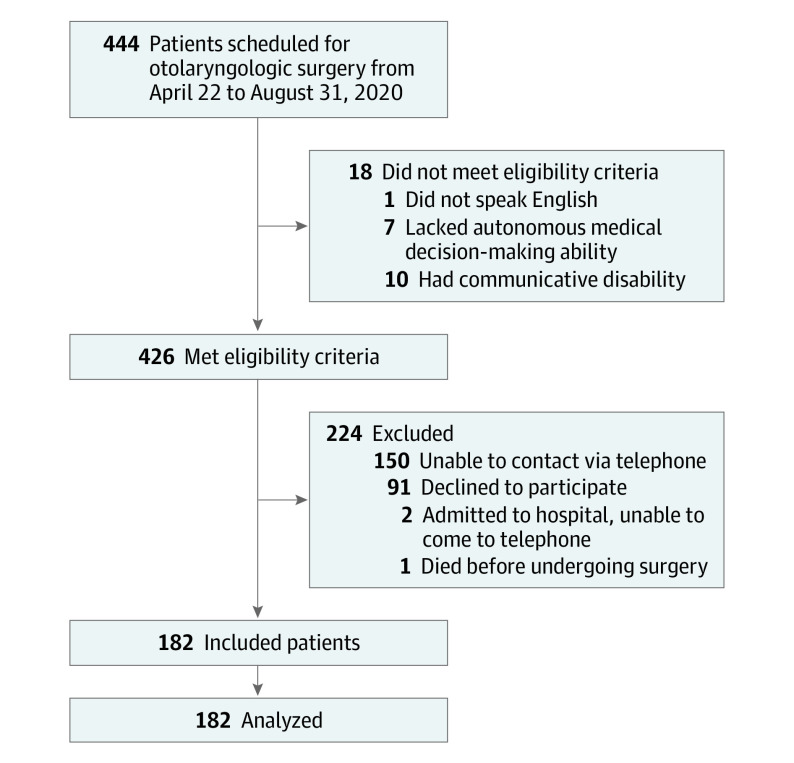
After 444 patients were screened for eligibility, 182 (40.9%) participated (Figure 1). Of the 241 eligible people who did not complete the study, 91 participants (37.8%) declined for various reasons and 150 participants (62.2%) could not be reached via telephone after 3 separate attempts. Table 1 presents the study population demographic characteristics. The median age was 60.5 years (interquartile range, 48-70 years). Most participants were female (92 [50.5%]), White (153 [84.0%]), non-Hispanic (176 [97%]), married (111 [60.1%]) and had at least some college education (138 [75.8%]). Most participants had histories that included medical (76.4% [139 of 182]) and surgical (95.1% [173 of 182]) procedures and mild level of comorbidity per the ACE-27 (43.2% [60 of 139]). Forty-two patients (23.0%) were undergoing a revision or repeated surgery (ie, airway surgery for recurrent respiratory papilloma), and most patients (99 [54.4%]) had elective surgery.
Figure 1. Study Flow Diagram.
Table 1. Patient Characteristics and Associations With Decisional Conflict.
| Variable | Category (No.)a | No. (%) | Difference between each category for DC present, % (95% CI) | |
|---|---|---|---|---|
| Decisional conflict present (n=34) | Decisional conflict absent (n=148) | |||
| Age, median (range), y | 61.5 (24-85) | 60.0 (18-88) | 1.0 (−6.0 to 4.0)b | |
| Sex | Male (90) | 20 (22.2) | 70 (77.8) | 7.0 (−4.3 to 18.3) |
| Female (92) | 14 (15.2) | 78 (84.8) | NA | |
| Race | White (153) | 24 (15.7) | 129 (84.3) | 18.8 (0.6 to 37.0) |
| Non-White (29)c | 10 (34.5) | 19 (65.5) | NA | |
| Asian (3) | 2 (66.6) | 1 (33.3) | NA | |
| Black or African American (26) | 17 (65.4) | 9 (34.6) | NA | |
| Medical history, ACE-27 category | Yes (139) (mild [60]; moderate [33]; severe [46]) | 26 (18.7) | 113 (81.3) | 0.1 (−13.2 to 13.4) |
| No (43) | 8 (18.6) | 35 (81.4) | NA | |
| Repeated surgery or revision | Yes (42) | 6 (14.3) | 38 (85.7) | 5.7 (−6.8 to 18.2) |
| No (140) | 28 (20.0) | 112 (80.0) | NA | |
| Educational status | No college (44) | 10 (22.7) | 34 (77.3) | 5.3 (−8.6 to 19.2) |
| At least some college (138) | 24 (17.4) | 114 (82.6) | NA | |
| Marital status | Not married (71) | 14 (19.7) | 57 (80.3) | 1.7 (−10 to 13.4) |
| Married (111) | 20 (18.0) | 91 (82.0) | NA | |
| Timing of surgery | Elective (99) | 14 (14.1) | 85 (85.9) | 10 (−1.5 to 21.5) |
| Urgent (83) | 20 (24.1) | 63 (75.9) | NA | |
| Date of surgery | During stay-at-home period (9) | 4 (44.4) | 5 (55.6) | 27.1 (0.8 to 56.4) |
| After stay-at-home period (173) | 30 (17.3) | 143 (82.7) | NA | |
| Type of surgery | Endocrine surgery (7) | 0 (0) | 7 (100) | NA |
| Head and neck cancer without free flap (40) | 6 (15.0) | 34 (85.0) | ||
| Head and neck cancer with free flap (13) | 6 (46.2) | 7 (53.8) | ||
| Facial plastic nasal surgery (21) | 2 (9.5) | 19 (90.5) | ||
| Facial plastic skin cancer reconstruction (27) | 6 (22.2) | 21 (77.8) | ||
| Facial plastic trauma surgery (17) | 5 (29.4) | 12 (70.6) | ||
| Laryngology airway surgery (12) | 1 (8.3) | 11 (91.7) | ||
| Laryngology voice surgery (32) | 5 (15.6) | 27 (84.4) | ||
| Other (13)d | 3 (23.1) | 10 (76.9) | ||
Abbreviations: ACE-27, Adult Comorbidity Evaluation-27; DC, decisional conflict; NA, not applicable.
Categories were compared between decisional conflict present vs absent groups using χ2 test of independence, unless otherwise indicated.
Median difference in age (years).
Non-White participants included 3 participants reporting Asian race and 26 participants reporting Black or African American race.
Other surgeries included anterior skull base surgery (2), anterior cervical discectomy and fusion (1), cosmetic blepharoplasty (1), removal of skin cyst (1), surgery for facial paralysis (1), surgery for swallowing disorders/esophageal dilation (6), and tonsillectomy (1).
The most common types of surgery were head and neck surgery without free flap (40 patients [21.9%]) and voice surgery (32 patients [17.6%]). Almost every patient was tested for COVID-19 preoperatively; 179 patients tested negative and 3 patients had unknown results. Nine patients had surgery during the statewide Missouri stay-at-home period.
Decisional Conflict
The prevalence of DC was 18.7% (34 of 182 patients). In the SURE Questionnaire, the frequency of “no” responses for question 1 (Do you feel sure about the best choice for you?) was 3.3% (6 of 182), for question 2 (Do you know the benefits and risks of each option?) was 17% (30 of 182), for question 3 (Are you clear about which benefits and risks matter most to you?) was 6% (11 of 182), and for question 4 (Do you have enough support and advice to make a choice?) was 1% (2 of 182). Race and ethnicity was the only demographic variable associated with DC, as non-White participants had an adjusted odds ratio of 3.0 (95% CI, 1.2-7.4) for DC compared with White participants, after adjusting for sex, educational status, and timing of surgery. Notably, a higher proportion of participants having surgery during the stay-at-home period had DC (44% [4 of 9]) than those having surgery after the period ended (17% [30 of 173]); however, this study was approved to start shortly before May 4, 2020, and was thus limited by small sample size for the stay-at-home period. A greater proportion of patients having surgery for the first time had DC than patients having repeated or revision surgery (20.0% vs 14.3%; difference: 5.7; 95% CI −6.8 to 18.2).
Oncologic status was a potential confounding variable considered because this population may have a different level of DC than patients without involvement in oncologic care. Seventy-eight (42.9%) participants had surgery for any head and neck cancer, 18 (23.1%) of whom had a positive result for DC. The DC rate was highest in the subgroup who underwent head and neck surgery with a free flap (6 of 13 patients [46.2%]) (Table 1). However, there was no significant interaction effect between oncologic status and either educational status nor timing of surgery.
Conjunctive consolidation was performed in 2 steps to determine composite variables that stratified participants based on their level of DC (Table 2). First, race and ethnicity and educational status categories were combined. Within each of the 2 levels of race, there was a gradient for rates of DC across educational status. Similarly, within each of the 2 levels of educational status, there was a gradient of the outcome across race categories. This phenomenon is referred to as a double gradient or gradient within a gradient.25 Based on statistical isometry,24,25 different conjoint cells were consolidated to create a 3-category system (A, B, and C) to describe the association of race-educational status with DC rate, from highest to lowest: (A) non-White participants with no college education (60% DC); (B) non-White participants with some college education (21% DC); and (C) White participants at any educational level (16% DC). The absolute difference (95% CIs) in DC rates between groups A and C was 44.4% (95% CI, 10.6%-78.0%). Second, this 3-category system was conjoined with timing of surgery, yielding a double gradient, to devise a new 4-category system (α, β, γ, and δ): (α) non-White participants with no college education having either urgent or elective surgery (60% DC); (β) non-White participants with some college education having urgent surgery or White participants at any educational level having urgent surgery (21% DC); (γ) non-White participants with some college education having elective surgery (17% DC); and (δ) White participants at any educational level undergoing elective surgery (12% DC) (Table 3). The absolute difference between groups α and δ was 47.8% (95% CI, 17.7%-71.6%). In addition, logistic regression analysis of the 4-category system revealed group α had the strongest likelihood of DC (odds ratio, 10.8; 95% CI, 2.6-45.0). The discriminative ability of this model was fair: C statistic 0.64 (95% CI, 0.53-0.74).
Table 2. Conjunctive Consolidation of Race and Educational Status.
| Educational status | Race, No./total No. (%)a | ||
|---|---|---|---|
| Non-Whiteb | White | Total | |
| No college | 6/10 (60)c | 4/34 (12)d | 10/44 (23) |
| Some college | 4/19 (21)e | 20/119 (17)d | 24/138 (17) |
| Total | 10/29 (34) | 24/153 (16) | 34/182 (19) |
The gradient was calculated to represent the difference in percentage value between the category with the highest percent and the lowest percent. For non-White, no college (60%) and White, any education level college (16%), the gradient is calculated as 44%.
Non-White participants included those reporting Asian race and those reporting Black or African American race.
High rate of decisional conflict.
Low rate of decisional conflict.
Intermediate rate of decisional conflict.
Table 3. Conjunctive Consolidation of Race and Educational Status With Timing of Surgery.
| Race and educational status | Timing of surgery, No./total No. (%)a | ||
|---|---|---|---|
| Urgent | Elective | Total | |
| Non-White, no collegeb | 4/5 (80)c | 2/5 (40)c | 6/10 (60) |
| Non-White, some collegeb | 2/7 (29)d | 2/12 (17)e | 4/19 (21) |
| White, any educational level | 14/71 (20)d | 10/82 (12)f | 24/153 (16) |
| Total | 20/83 (24) | 14/99 (14) | 34/182 (19) |
The gradient was calculated to represent the difference in percentage value between the category with the highest percent and the lowest percent. For non-White, no college, either urgent or elective surgery (60% decisional conflict) and White, any education level, elective surgery (12%), the gradient is calculated as 48%.
Non-White participants included those reporting Asian race and those reporting Black or African American race.
High rate of decisional conflict.
Intermediate rate of decisional conflict.
Low rate of decisional conflict.
Very low rate of decisional conflict.
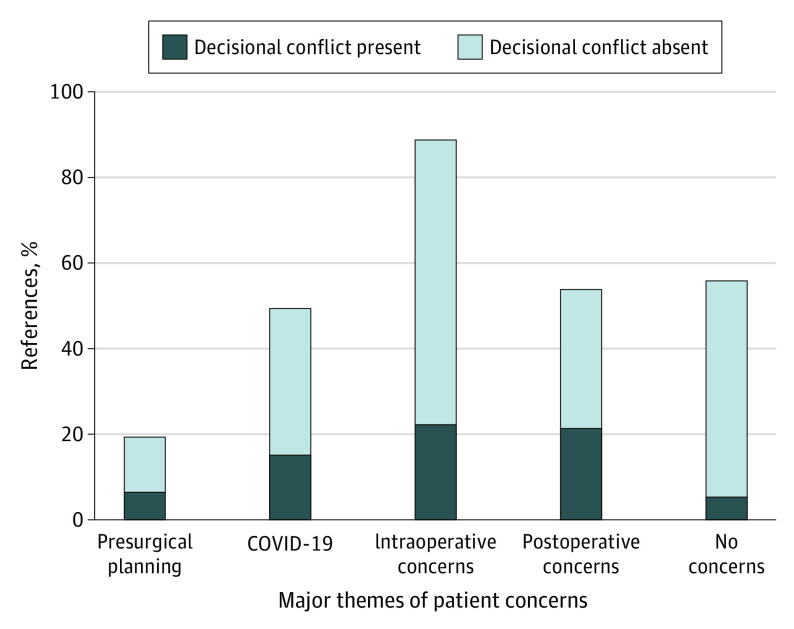
Patient-Specific Concerns
Figure 2 shows prevalent themes and subthemes of the patient-specific concerns. Representative quotations from the entire study cohort stratified by the presence or absence of DC are presented in the eTable in the Supplement. A single statement may include more than 1 subtheme, thus Figure 2 and the eTable in the Supplement report more references (268) than the total number of respondents (182). Initially, there was disagreement on 36% of the items; ultimately, only 2 items required establishment of consensus with the senior author. Most disagreements occurred in the assignment of subtheme codes, not between major themes. For example, a patient who was having a repeated laryngoscopy stated that she remembered “traumatic events in the past, [and] currently feels fearful but hopeful.” This statement was coded under the major theme “Intraoperative concerns.” One reviewer coded the subtheme as “Complications,” the other reviewer coded it as “Confidence in surgery or surgeon.” After discussion, this line was ultimately coded as “Confidence in surgery or surgeon” because it lacked a specific mention of a surgical complication.
Figure 2. Bar Chart of Major Themes for Patient-Specific Concerns.
Data are recorded as number of references coded and are stratified by presence and absence of decisional conflict.
Overall, intraoperative and postoperative concerns were the most prevalent major themes reported by patients. In fact, there was a clinically significant difference in the proportion of participants who screened positive for DC (30.4% [21 of 69]) and expressed postoperative concerns than those who screened negative for DC (16.6% [33 of 169]) (proportion difference 13%, 95% CI, 1%-25%). While some concerns (ie, logistics about arrival to the surgery center) may not directly change a patient’s decision whether to have the surgery, they may be associated with feelings of uncertainty leading up to surgery.
Of the total responses, 21% (56 of 268 references) were coded as “No concerns.” Between the 2 groups, participants who screened negative for DC reported “no concerns” at a higher rate than participants with DC: proportion difference 19% (95% CI, 10%-28%). Having a repeated or revision surgery possibly affected this response; 39 of 140 participants (28%) having first-time surgery reported “no concerns” vs 17 of 42 patients (40%) having repeated or revision surgery, perhaps because the latter knew what to expect from prior experience. The decision to combine repeated (26 participants) and revision (16 participants) surgical cases in 1 group was made because these patients represent groups comparable to one another, as opposed to patients having first-ever surgery.
Nineteen percent of all responses cited “COVID-19” as a major theme, most of whom screened positive for DC. Most expressed concern about “contracting COVID-19” or uncertainty about “hospital safety or sanitation.”
An unexpected outcome of this survey study was participant gratitude for the opportunity to ask further questions that they may have forgotten to ask during their preoperative clinic visit. Patients were directed to call their surgeon’s office for additional questions. No patient canceled their surgery after completing the survey. There was no missing data.
Discussion
In this survey, the overall prevalence of DC (19%) in patients seeking otolaryngologic surgery during the early months of the COVID-19 pandemic fell within the range cited in the otolaryngology literature (13%-43%).4,8,9,10,11,12,13,14 Non-White race was associated with the presence of DC. The pandemic was a factor in DC in this cohort, as a larger proportion of patients who shared concerns about COVID-19 screened positive on the SURE Questionnaire and patients whose surgery date occurred during the statewide Missouri stay-at-home period had a higher rate of DC than patients who had surgery after the stay-at-home period ended. Intraoperative and postoperative concerns were the most prevalent patient-specific concerns, which may indicate missing elements from preoperative discussions. To our knowledge, this is the largest study of DC in otolaryngology to date, and participants were sampled from multiple subspecialties within the otolaryngology field.
Race and Decisional Conflict
The association between non-White race and DC remained after adjustment for other variables and through conjunctive consolidation, when race was stratified by educational status and timing of surgery. Analysis of open-ended patient-specific concerns of non-White participants varied across all subthemes; thus, the reason for this disparity is unclear. Understanding of racial differences in medical decision-making is hindered by a paucity of research in otolaryngology and other medical specialties addressing the specific topic of race.26,27 Possible explanations are distrust of the medical community27,28 or lack of individual feelings of empowerment experienced by patients communicating with physicians who are ethnically, culturally, and physically different from themselves.27,28 Education about disease state and health literacy are also important issues27,28; in the current study, the group with the highest rate of DC was non-White participants without a college education. In addition, to date, published studies have not compared DC for urgent vs elective surgery. People having elective surgery may have a greater sense of ownership of their decision, whereas people having urgent surgery may feel as if medical decisions occur outside their control. Beyond the actual decision to undergo surgery, sources of DC may arise from other circumstances. For example, patients scheduled for urgent surgery expressed concerns about the recovery period or inpatient stay during the pandemic, thus highlighting the nuances of DC and SDM. More studies explicitly measuring factors associated with race and SDM are warranted to understand this problem and direct efforts toward mitigating the amount of uncertainty experienced by all patients, regardless of racial or ethnic background.
Intraoperative and Postoperative Concerns
A number of factors involving perioperative surgical care may affect SDM. Most patients cited “anesthesia concerns,” or concerns for a “successful outcome,” “recovery,” and “wound and healing.” These qualitative responses align with the finding that the SURE question with the most frequent negative responses addressed risks and benefits. These findings would indicate inconsistency in the discussion of surgical risks and benefits between every surgeon and patient, or with every type of surgery, for reasons that remain unclear. In highlighting these inconsistencies, a potential next step would be for physicians to better understand the tools and instruments informing patients about options, benefits, risks, and adverse effects, as these mechanisms help clarify personal values of treatment outcomes.2,3,27
Concerns Associated With COVID-19
Our hypothesis that patients would have concerns about their surgery that were more prominent than their concerns about COVID-19 did prove to be accurate. Only 19% of the patient responses cited “COVID-19” as a concern. A greater proportion of patients who were concerned about COVID-19 did screen positive for DC, suggesting a negative consequence of the pandemic on patient confidence in choosing to have surgery.
Limitations
Findings in DC and other SDM components in this study may be considered preliminary and include limitations. The response rate was 41%, limiting generalizability of the findings. The survey design and inclusion of an English-speaking, voluntary, convenience sample of patients with telephone access and no communication disability may indicate selection bias. Although the SURE Questionnaire is a validated instrument in primary care settings and has been used in surgical studies, further validation studies in surgical patients is needed.5 Because of institutional policies governing the types of surgical procedures permissible during certain phases of the COVID-19 pandemic, some participants were likely receiving urgent surgery (ie, for treatment of head and neck cancer or trauma), limiting generalizability to other types of elective otolaryngologic surgery, in which decision-making is arguably more imperative. Participants were encouraged to list their concerns in an open-ended fashion, but in some cases, answers were vague and subject to the reviewers’ interpretation. Independent coding by reviewers and consensus with the senior author was used to mitigate bias in interpretation. Though this was a preliminary analysis with a moderate response rate, this study identified potential patient groups at-risk of experiencing DC that warrant further study. For example, although our results indicate an association between race and DC, the overall number of non-White patients (16%) was much smaller than the number of White patients (84%), and the 95% CIs around our estimates are quite wide. The grouping of all subgroups of racial and ethnic minority individuals as non-White limits understanding of how these findings apply to those individuals. Additionally, exploration of patient perceptions about receiving care from surgeons who differ ethnically, culturally, and physically from themselves may serve as an important first step to learn about race and factors associated with DC.
Despite these limitations, this is to our knowledge the largest study of DC in otolaryngology and the first to sample participants from different clinical environments (ie, multiple clinical sites at 1 academic hospital system), thus the results suggest the incidence of DC across the spectrum of medical care. Although SDM is a growing research topic,2,3,27 there may be some hesitancy on the part of the surgeon in delving into SDM. One concern was that in performing this survey, patients would cancel surgery out of trepidation. However, there were no cancellations among the participants who completed the study, suggesting the utility of conversations about risks, benefits, and SDM in terms of patient health literacy and feelings of empowerment.
Conclusions
In attempting to assess DC during the specific circumstances of a pandemic, this survey study helped to identify populations potentially at-risk of poor SDM outcomes. Race was associated with DC, and the variables that were factors in this this association were low educational status and urgent timing of surgery. Despite the pandemic setting, participants overwhelmingly shared concerns about intraoperative and postoperative processes, suggesting a need for health care professionals to converse with patients about patient values, beliefs, and specific concerns about treatment. Future studies of racially diverse groups undergoing urgent surgery, including qualitative assessment of these disparities, are warranted.
eTable. Themes and Sub-Themes of Open-ended Patient-Specific Concerns
References
- 1.Politi MC, Street RL Jr. The importance of communication in collaborative decision making: facilitating shared mind and the management of uncertainty. J Eval Clin Pract. 2011;17(4):579-584. doi: 10.1111/j.1365-2753.2010.01549.x [DOI] [PubMed] [Google Scholar]
- 2.Chi JJ. Reflections on shared decision making. Otolaryngol Head Neck Surg. 2018;159(5):809-810. doi: 10.1177/0194599818792212 [DOI] [PubMed] [Google Scholar]
- 3.Chi JJ, Rosenberg A, Hahn S, et al. Patient concerns about nasal reconstruction after Mohs surgery and implications for shared decision making. JAMA Otolaryngol Head Neck Surg. 2018;144(12):1180-1181. doi: 10.1001/jamaoto.2018.2368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Graham ME, Westerberg BD, Lea J, et al. Shared decision making and decisional conflict in the management of vestibular schwannoma: a prospective cohort study. J Otolaryngol Head Neck Surg. 2018;47(1):52. doi: 10.1186/s40463-018-0297-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferron Parayre A, Labrecque M, Rousseau M, Turcotte S, Légaré F. Validation of SURE, a four-item clinical checklist for detecting decisional conflict in patients. Med Decis Making. 2014;34(1):54-62. doi: 10.1177/0272989X13491463 [DOI] [PubMed] [Google Scholar]
- 6.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507-513. doi: 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McMichael TM, Currie DW, Clark S, et al. ; Public Health–Seattle and King County, EvergreenHealth, and CDC COVID-19 Investigation Team . Epidemiology of covid-19 in a long-term care facility in King County, Washington. N Engl J Med. 2020;382(21):2005-2011. doi: 10.1056/NEJMoa2005412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chorney J, Haworth R, Graham ME, Ritchie K, Curran JA, Hong P. Understanding shared decision making in pediatric otolaryngology. Otolaryngol Head Neck Surg. 2015;152(5):941-947. doi: 10.1177/0194599815574998 [DOI] [PubMed] [Google Scholar]
- 9.Hong P, Gorodzinsky AY, Taylor BA, Chorney JM. Parental decision making in pediatric otoplasty: the role of shared decision making in parental decisional conflict and decisional regret. Laryngoscope. 2016;126(suppl 5):S5-S13. doi: 10.1002/lary.26071 [DOI] [PubMed] [Google Scholar]
- 10.Hong P, Maguire E, Purcell M, Ritchie KC, Chorney J. Decision-making quality in parents considering adenotonsillectomy or tympanostomy tube insertion for their children. JAMA Otolaryngol Head Neck Surg. 2017;143(3):260-266. doi: 10.1001/jamaoto.2016.3365 [DOI] [PubMed] [Google Scholar]
- 11.Manning AM, Duggins AL, Tiemeyer KA, et al. Characterizing decisional conflict for caregivers of children with obstructive sleep apnea without tonsillar hypertrophy. J Clin Sleep Med. 2018;14(5):849-855. doi: 10.5664/jcsm.7122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ritchie KC, Chorney J, Hong P. Parents’ decisional conflict, self-determination and emotional experiences in pediatric otolaryngology: a prospective descriptive-comparative study. Int J Pediatr Otorhinolaryngol. 2016;86:114-117. doi: 10.1016/j.ijporl.2016.04.034 [DOI] [PubMed] [Google Scholar]
- 13.Taylor BA, Hart RD, Rigby MH, Trites J, Taylor SM, Hong P. Decisional conflict in patients considering diagnostic thyroidectomy with indeterminate fine needle aspirate cytopathology. J Otolaryngol Head Neck Surg. 2016;45:16. doi: 10.1186/s40463-016-0130-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Graham ME, Haworth R, Chorney J, Bance M, Hong P. Decisional conflict in parents considering bone-anchored hearing devices in children with unilateral aural atresia. Ann Otol Rhinol Laryngol. 2015;124(12):925-930. doi: 10.1177/0003489415592000 [DOI] [PubMed] [Google Scholar]
- 15.Shuman AG, Larkin K, Thomas D, et al. Patient reflections on decision making for laryngeal cancer treatment. Otolaryngol Head Neck Surg. 2017;156(2):299-304. doi: 10.1177/0194599816683377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris PA, Taylor R, Minor BL, et al. ; REDCap Consortium . The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15(1):25-30. doi: 10.1177/0272989X9501500105 [DOI] [PubMed] [Google Scholar]
- 19.Hwang R, Lambrechts S, Liu H, et al. Decisional conflict among patients considering treatment options for lumbar herniated disc. World Neurosurg. 2018;116:e680-e690. doi: 10.1016/j.wneu.2018.05.068 [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention . Behavioral Risk Factor Surveillance System. July 2021. Accessed August 10, 2021. https://www.cdc.gov/brfss/questionnaires/pdf-ques/2020-BRFSS-Questionnaire-508.pdf
- 21.American College of Surgeons . COVID-19: Guidance for triage of non-emergent surgical procedures. Published March 17, 2020. Accessed February 12, 2021. https://www.facs.org/covid-19/clinical-guidance/triage
- 22.Kallogjeri D, Piccirillo JF, Spitznagel EL Jr, Steyerberg EW. Comparison of scoring methods for ACE-27: simpler is better. J Geriatr Oncol. 2012;3(3):238-245. doi: 10.1016/j.jgo.2012.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Governors Association. Coronavirus state actions. July 31, 2020. Accessed September 29, 2020. https://www.nga.org/coronavirus-state-actions-all/
- 24.Feinstein AR, Wells CK, Walter SD. A comparison of multivariable mathematical methods for predicting survival—I: introduction, rationale, and general strategy. J Clin Epidemiol. 1990;43(4):339-347. doi: 10.1016/0895-4356(90)90120-E [DOI] [PubMed] [Google Scholar]
- 25.Neely JG, Lieu JE, Sequeira SM, et al. Practical guide to understanding multivariable analyses, Part B: conjunctive consolidation. Otolaryngol Head Neck Surg. 2013;148(3):359-365. doi: 10.1177/0194599812471500 [DOI] [PubMed] [Google Scholar]
- 26.Harris VC, Links AR, Walsh J, et al. A systematic review of race/ethnicity and parental treatment decision-making. Clin Pediatr (Phila). 2018;57(12):1453-1464. doi: 10.1177/0009922818788307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ikeda AK, Hong P, Ishman SL, Joe SA, Randolph GW, Shin JJ. Evidence-based medicine in otolaryngology, part 8: shared decision making-impact, incentives, and instruments. Otolaryngol Head Neck Surg. 2018;159(1):11-16. doi: 10.1177/0194599818763600 [DOI] [PubMed] [Google Scholar]
- 28.Peek ME, Wilson SC, Gorawara-Bhat R, Odoms-Young A, Quinn MT, Chin MH. Barriers and facilitators to shared decision-making among African-Americans with diabetes. J Gen Intern Med. 2009;24(10):1135-1139. doi: 10.1007/s11606-009-1047-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Themes and Sub-Themes of Open-ended Patient-Specific Concerns