Abstract
Purpose
The study aims to evaluate the use of face masks on allergic rhinitis symptoms in pollen allergy patients who were compulsorily using face masks due to the covid-19 pandemic.
Materials and methods
A 15-item questionnaire was developed following the study goals by a team experienced in allergic rhinitis. Then the records of patients who underwent allergy tests in our hospital between 2013 and 2019 were retrospectively analyzed. Fifty participants with isolated pollen allergy were included in the study. Patients who agreed to participate in the research answered the questions over the phone.
Results
Of the 50 participants, 30 (60%) were female and 20 (40%) were male, with a mean age of 34.34 ± 9.41 years. While the rate of participants who defined their nasal symptoms as severe-moderate in the pre-pandemic period was 92% (46 patients), this rate decreased to 56% (28 patients) during the pandemic when they used face masks. In ocular symptoms, the same rate decreased from 60% (30 patients) to 32% (16 patients). A statistically significant decrease was found in both nasal and ocular symptoms of patients after mask use (p < 0.001). The most regression in allergy symptoms was observed in sneezing (p = 0.029) and nasal discharge (p = 0.039).
Conclusions
This study observed that the use of face masks reduced both nasal and ocular allergic rhinitis symptoms in individuals with pollen allergy. These results support the hypothesis that the use of face masks would reduce the severity of allergic rhinitis symptoms.
Keywords: Allergens, Allergic rhinitis, Face mask, Pollen
1. Introduction
Allergic rhinitis (AR) is an IgE-mediated inflammation of the nasal mucosa that is characterized by symptoms such as nasal discharge, nasal congestion, nasal itching, and sneezing. With an increasing prevalence worldwide, especially in developed countries, AR is estimated to affect approximately 20–40% of the world population [1]. A recent study assessing 9017 people in Turkey reported the prevalence of AR as 36.7% [2]. AR, if treated inadequately, negatively affects patients' work productivity and academic performance, and causes impaired concentration and sleep disorders, resulting in significant health problems [3]. AR is caused by microparticles in the air that are called aeroallergens. When these microparticles reach the nasal mucosa by inhalation, the type 1 hypersensitivity reaction occurs against these allergens in sensitive individuals. Therefore, allergen avoidance and environmental controls are the first-line treatment of AR, with significant coverage in the treatment guidelines [4].
The goal of environmental controls is to prevent allergens from contacting the respiratory tract mucosa. Preventive methods aim to effectively reduce allergen exposure, thereby increasing the efficacy of medical treatment and improving the quality of life [5]. However, allergen avoidance is a controversial issue due to the difficulty for the patients to fully implement these methods, and the level of evidence is not very high [6]. In addition, controlling contact with outdoor allergens is much more difficult than controlling contact with indoor allergens. Pollens are the most common outdoor allergens, being the most common cause of allergic rhinitis in the population [7]. Pollen, the small male reproductive unit of plants, contains numerous allergenic proteins and can be carried over great distances by the wind. Various methods have been described for pollen avoidance in AR patients with pollen sensitivity, and face mask usage during pollen seasons is one of the recommended avoidance methods [8]. However, there is no explicit study showing that masks protect from allergens.
Due to the COVID-19 pandemic, which started at the end of 2019 and is still continuing, it is required to wear face masks outdoors and non-residential indoors for about one year now in Turkey. Therefore, the pandemic provides a good opportunity to assess the effect of face mask usage on allergy symptoms. The present study aimed to evaluate the effectiveness of face mask usage on allergic rhinitis symptoms using a questionnaire for allergic rhinitis patients with isolated pollen allergy who had to wear face masks due to the pandemic.
2. Materials and methods
In our study, a questionnaire was developed by a team experienced in allergy following the purpose of the study (Fig. 1 ). The 15-item questionnaire consisted of four parts: demographic information of the patients, face mask usage during the pandemic, allergic complaints during the pre-pandemic period, and allergic complaints during the pandemic period. Then, the medical records of the patients who received a skin prick test in the allergy outpatient clinic of our hospital between January 2013 and December 2019 were reviewed retrospectively. Patients with pollen sensitivity identified by the skin-prick test and who were symptomatic during March–April, the study period, were listed. Patients allergic to pollen and also sensitive to indoor allergens such as house-dust mites, fungal spores, animal epithelial materials, and cockroaches were excluded from the study. Ninety patients with isolated pollen allergy were included in the study. Patients were contacted by phone and informed about the purpose and scope of the study. Patients who agreed to participate in the study answered the questions in the questionnaire over the phone. The data were collected in April, the time when seasonal allergens are high in number and took approximately one month. Ethics Committee approval for the study was obtained from the clinical research ethics committee of *** University (60116787–020/21586).
Fig. 1.
Questionnaire form used in the study.
2.1. Statistical analysis
All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) version 25 for Windows (IBM Corp.; Armonk, NY, USA). Continuous variables were presented as mean ± standard deviation, minimum, and maximum values. Categorical variables were presented as numbers and percentages. We used the Wilcoxon paired-sample test and McNemar's test for comparing the groups. For all analyses, a p-value of <0.05 was considered statistically significant.
3. Results
During the approximately one-month period between the start and end of the study, 51 (56.6%) of 90 patients were reached. One patient refused to participate in the study. The study assessed the data of 50 participants. Thirty (60%) of the participants were female and 20 (40%) were male, with a mean age of 34.34 ± 9.41 (min-max: 18–58) years.
During the pandemic, 29 (58%) of the study participants worked from the office regularly, 13 (26%) worked from home, and 8 (16%) did not work. All of the study participants stated that they constantly wore face masks outside of their homes and workplaces, while 86% (43 patients) of the participants used surgical masks, 8% (4 patients) N95 masks, and 6% (3 people) fabric masks.
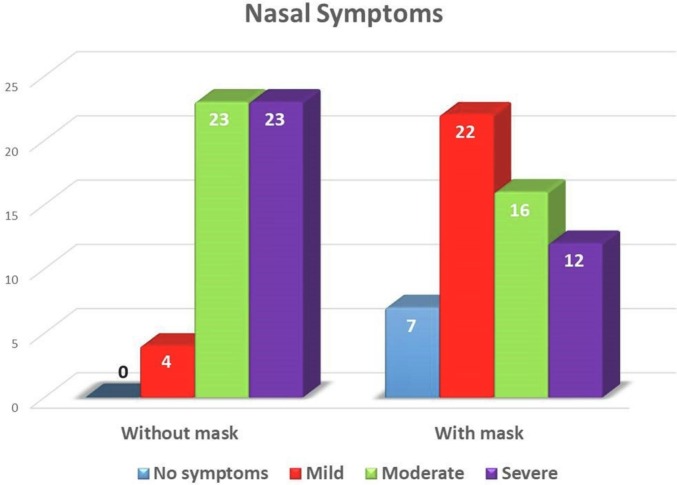
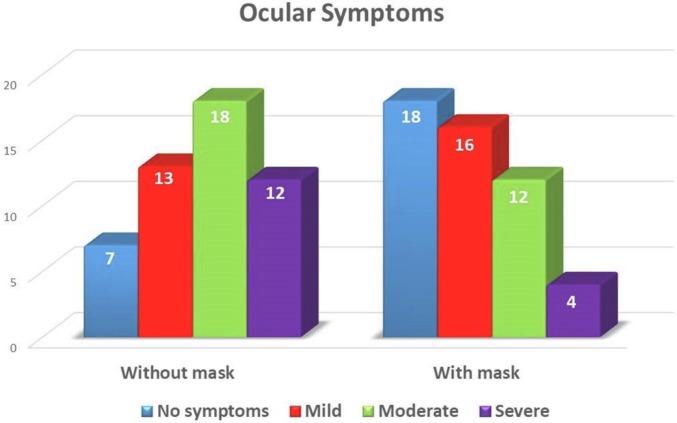
According to the survey results, the rate of participants describing their allergy-related nasal complaints as moderate-severe in the pre-pandemic period was 92% (moderate: 23, severe: 23; total: 46 patients), while the rate declined to 56% (moderate: 16, severe: 12; total: 28 patients) during the pandemic when they used face masks (Fig. 2 ). Our study established a statistically significant reduction in the nasal symptoms of the patients after the mask usage (p < 0.001). Similarly, the rate of participants with severe to moderate allergy-related ocular symptoms decreased from 60% (moderate: 18, severe: 12; total: 30 patients) to 32% (moderate: 12, severe: 4 severe; total 16 patients) (Fig. 3 ). Our study established that the reduction in allergic ocular symptoms was also statistically significant (p < 0.001).
Fig. 2.
Distribution of allergic nasal symptom severity of the participants during the periods with and without a face mask.
Fig. 3.
Distribution of allergic ocular symptom severity of the participants during the periods with and without a face mask.
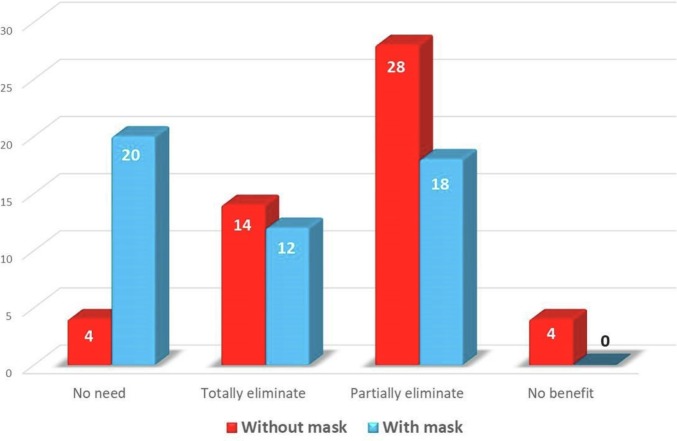
The rate of participants who needed medical treatment due to allergic rhinitis in the pre-pandemic period was 92% (46 patients), while the rate decreased to 60% (30 patients) after mask usage. Similarly, there were 4 (8%) participants expressing that they did not benefit from medical treatment in the pre-pandemic period, while no participant stated that they did not benefit from medical treatment after mask usage (Fig. 4 ). Our study determined that the use of face masks statistically increased the efficacy of medical treatment (p < 0.001).
Fig. 4.
The effect of face mask usage on the medical treatment of allergic rhinitis.
When the effects of face mask usage on allergic symptoms were examined separately, our study observed that there was a 16% reduction in sneezing, 14% in nasal discharge, 8% in nasal itching, and 2% in nasal congestion during the pandemic (Table 1 ). These data showed that mask usage had the greatest effect on sneezing, and a statistically significant reduction was identified in sneezing (p = 0.029) and nasal discharge (p = 0.039).
Table 1.
The effect of face mask usage on allergic rhinitis symptoms.
| Pre-pandemic period n (%) |
Pandemic period n (%) |
p-value | |
|---|---|---|---|
| Sneezing | 31 (%62) | 23 (%46) | p = 0.029⁎ |
| Nasal discharge | 18 (%36) | 11 (%22) | p = 0.039⁎ |
| Nasal itching | 23 (%46) | 19 (%38) | p = 0.289 |
| Nasal congestion | 12 (%24) | 11 (%22) | p = 0.999 |
p < 0.05 the statistical significance level.
4. Discussion
Treatment of individuals with allergic disease consists of allergen avoidance and environmental control, pharmacotherapy, and immunotherapy. Environmental control is generally considered difficult to implement in the treatment of AR patients, but it is indicated for all patients. Informing patients about allergen avoidance is of great importance in terms of achieving and maintaining disease control [9]. However, avoidance of pollens is much more difficult than other allergens because pollination is a global natural phenomenon that occurs periodically, and therefore, source control is not possible. This makes it almost impossible for patients to avoid pollens completely. Among the recommended preventive methods for minimizing allergen exposure in individuals with pollen allergy are avoiding outdoors on dry and windy days during the pollen season, keeping windows closed, and using face masks [10]. However, these recommended preventive methods are mostly based on clinical experience and there are not enough clinical studies assessing the efficacy of these methods. The requirement for face masks during the pandemic has provided a good opportunity to explore the effect of mask usage on allergic symptoms.
The reason for the face mask requirement during the ongoing COVID-19 pandemic is to reduce the spread of saliva and respiratory droplets from infected individuals. The decline of influenza cases during the pandemic supports face mask protection against infections [11]. Standard surgical masks, which are widely used by people, filter particles larger than 3 μm [12], while N95 masks can filter small particles down to 0.04 μm [13]. Among pollen groups, tree pollens have a diameter of 20 to 60 μm, grass pollens are usually 30–40 μm, and grass pollens are about 20 μm in diameter [10]. Therefore, face masks have the potential to reduce the allergen load in the inspired air in addition to protection against infectious agents.
There is limited literature on the effect of face mask usage on allergic rhinitis symptoms. In a placebo-controlled study on 24 patients, Kenney et al. reported that some nasal symptoms were significantly improved in patients using nasal filters, under repeated exposure in an environmental exposure unit. However, the researchers did not establish any significant reduction in the total allergy score [14]. Later, the same researchers conducted another study on 65 patients in a natural setting and during a pollen season and reported a significant reduction in the total allergy score in nasal filter users [15]. Our study observed a significant reduction in the self-reported allergic rhinitis symptoms when individuals with pollen allergy used face masks. The rate of participants who described their nasal complaints as moderate-severe was found to decrease by 36%. Our findings show that face masks are effective in reducing the load of inspiratory particles, including pollens.
The majority of AR patients also experience ocular complaints such as watery and itchy eyes, which is called allergic rhinoconjunctivitis. In their study on 301 nurses with allergic rhinitis symptoms, Dror AA et al. concluded that the use of face masks reduced allergic nasal symptoms but did not affect ocular symptoms [16]. Our study found that the severity of not only nasal symptoms but also ocular symptoms reduced after face mask usage in individuals with pollen allergy. According to the survey results, allergy-related ocular complaints were present in 86% of the participants in the pre-pandemic period, while the rate decreased to 64% during the mask-wearing period. Similarly, the rate of those describing their ocular complaints as moderate-severe decreased from 60% to 32%. The mechanism underlying the development of AR-related ocular symptoms is not fully known. One of the hypotheses on this subject is the nasal-ocular reflex. The nerves providing the parasympathetic innervation to the lacrimal gland are connected with the parasympathetic nerves innervating the nasal cavity. The nasal-ocular reflex is based on the theory that stimulation of the nasal afferent nerves by allergens initiates a neural reflex that produces ocular symptoms by causing an efferent parasympathetic response [17]. It is believed that the positive effect of intranasal steroids used to treat AR on ocular symptoms results from the inhibition of this reflex with an anti-inflammatory effect on the nasal mucosa [18]. In addition, a study by Cömert Ş et al. demonstrated that the use of standard wraparound glasses significantly reduced not only ocular symptoms but also nasal symptoms in patients with allergic rhinoconjunctivitis [19]. This finding suggests a bilateral function of the nasal-ocular reflex arc. The data of our study also support the theory that ocular symptoms can be produced by the nasal-ocular reflex in AR patients and that preventing the contact of allergens with the nasal mucosa can reduce ocular symptoms.
The treatment of AR has a significant economic burden. In the USA, the annual drug cost for AR treatment was reported to be approximately 3.1 billion dollars in 1997 alone [20]. Treatment costs increased further in the 2000s, and it is estimated that the annual cost of antihistamines alone exceeds 3.5 billion dollars, and the total cost of drugs with intranasal corticosteroids exceeds 5 billion dollars per year [21]. Our study observed that the patients' need for medical treatment reduced by 32% during the mask-wearing period. The data further showed that the use of masks increased the efficacy of medical treatment. Considering that the cost of masks is much more affordable than the cost of medical treatment, encouraging AR patients to wear masks during pollen seasons would not only improve the quality of their lives but also contribute significantly to the economy.
The most important limitation of our study is that we did not evaluate the effect of other preventive measures implemented due to the COVID-19 pandemic on allergic rhinitis symptoms. In particular, spending less time outdoors as recommended by health authorities might have reduced the pollen exposure of the participants. However, at the time of the study, there was not a full lockdown in our country, except for the requirement for face masks, and many workplaces, shopping malls, and cafes continued their activities as long as the social distancing was followed. Therefore, COVID-19 preventive measures other than face mask usage were not taken into consideration in our study.
5. Conclusion
This study observed that the use of face masks reduced both nasal and ocular allergic rhinitis complaints in individuals with pollen allergy. This results support the hypothesis that the use of face masks would reduce the severity of allergic rhinitis symptoms. Face mask usage can be considered a preventive measure to minimize allergen exposure in high-risk environments. The data of our study are encouraging for both physicians and patients in terms of informing sensitive individuals about the methods for allergen avoidance and to implement these methods.
Declaration of competing interest
None.
Acknowledgment
The authors thank Ph.D. Hande Senol (Department of Biostatistics, School of Medicine, Pamukkale University) for her assistance and contribution in the statistical analysis of the study.
References
- 1.Bousquet J., Khaltaev N., Cruz A.A., Denburg J., Fokkens W.J., Togias A., et al. Allergic rhinitis and its impact on asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen) Allergy. 2008;63:8–160. doi: 10.1111/j.1398-9995.2007.01620.x. [DOI] [PubMed] [Google Scholar]
- 2.Cingi C., Muluk N.B., Susaman N., et al. The Score for Allergic Rhinitis Study in Turkey, 2020. ENT-Updates. Vol. 11. 2021. pp. 1–7. [Google Scholar]
- 3.Gaudin R.A., Hoehle L.P., Birkelbach M.A., Phillips K.M., Beule A.G., Caradonna D.S., et al. Assoziation zwischen Kontrolle der allergischen Rhinitis und Schlafqualität [The association between allergic rhinitis control and sleep quality] HNO. 2017;65:987–992. doi: 10.1007/s00106-017-0398-9. [DOI] [PubMed] [Google Scholar]
- 4.Seidman M.D., Gurgel R.K., Lin S.Y., Schwartz S.R., Baroody F.M., Bonner J.R., et al. Clinical practice guideline: allergic rhinitis. Otolaryngol Head Neck Surg. 2015;152:S1–43. doi: 10.1177/0194599814561600. [DOI] [PubMed] [Google Scholar]
- 5.Portnoy J., Kennedy K., Sublett J., Phipatanakul W., Matsui E., Barnes C., et al. Environmental assessment and exposure control: a practice parameter–furry animals. Ann Allergy Asthma Immunol. 2012;108(223):e1–15. doi: 10.1016/j.anai.2012.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wise S.K., Lin S.Y., Toskala E., Orlandi R.R., Akdis C.A., Alt J.A., et al. International consensus statement on allergy and rhinology: allergic rhinitis. Int Forum Allergy Rhinol. 2018;8:108–352. doi: 10.1002/alr.22073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lake I.R., Jones N.R., Agnew M., Goodess C.M., Giorgi F., Hamaoui-Laguel L., et al. Climate change and future pollen allergy in Europe. Environ Health Perspect. 2017;125:385–391. doi: 10.1289/EHP2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gautier C., Charpin D. Environmental triggers and avoidance in the management of asthma. J Asthma Allergy. 2017;10:47–56. doi: 10.2147/JAA.S121276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.E Mengi CO Kara Education of patients with allergic rhinitis. In: B Topuz CO Kara editors. Adim adim alerjik rinit [Step by step allergic rhinitis], Istanbul: Logos Yayinevi; 202, p. 144–150.
- 10.Oh J.W. Springer Nature Singapore Pte Ltd.; Singapore: 2018. Pollen allergy in a changing world. [Google Scholar]
- 11.Chiu N.C., Chi H., Tai Y.L., Peng C.C., Tseng C.Y., Chen C.C., et al. Impact of wearing masks, hand hygiene, and social distancing on influenza, enterovirus, and all-cause pneumonia during the coronavirus pandemic: retrospective National Epidemiological Surveillance Study. J Med Internet Res. 2020;22 doi: 10.2196/21257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Santarsiero A., Ciambelli P., Donsì G., Quadrini F., Briancesco R., D'Alessandro D., et al. Face masks. technical, technological and functional characteristics and hygienic-sanitary aspects related to the use of filtering mask in the community. Ann Ig. 2020;32:472–520. doi: 10.7416/ai.2020.2371. [DOI] [PubMed] [Google Scholar]
- 13.Lee S.A., Grinshpun S.A., Reponen T. Respiratory performance offered by N95 respirators and surgical masks: human subject evaluation with NaCl aerosol representing bacterial and viral particle size range. Ann Occup Hyg. 2008;52:177–185. doi: 10.1093/annhyg/men005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kenney P., Hilberg O., Pedersen H., Nielsen O.B., Sigsgaard T. Nasal filters for the treatment of allergic rhinitis: a randomized, double-blind, placebo-controlled crossover clinical trial. J Allergy Clin Immunol. 2014;133(1477–80):1480.e1-13. doi: 10.1016/j.jaci.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 15.Kenney P., Hilberg O., Laursen A.C., Peel R.G., Sigsgaard T. Preventive effect of nasal filters on allergic rhinitis: a randomized, double-blind, placebo-controlled crossover park study. J Allergy Clin Immunol. 2015;136:1566–1572.e5. doi: 10.1016/j.jaci.2015.05.015. [DOI] [PubMed] [Google Scholar]
- 16.Dror A.A., Eisenbach N., Marshak T., Layous E., Zigron A., Shivatzki S., et al. Reduction of allergic rhinitis symptoms with face mask usage during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020;8:3590–3593. doi: 10.1016/j.jaip.2020.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baroody F.M., Foster K.A., Markaryan A., deTineo M., Naclerio R.M. Nasal ocular reflexes and eye symptoms in patients with allergic rhinitis. Ann Allergy Asthma Immunol. 2008;100:194–199. doi: 10.1016/S1081-1206(10)60442-5. [DOI] [PubMed] [Google Scholar]
- 18.Baroody F.M., Shenaq D., DeTineo M., Wang J., Naclerio R.M. Fluticasone furoate nasal spray reduces the nasal-ocular reflex: a mechanism for the efficacy of topical steroids in controlling allergic eye symptoms. J Allergy Clin Immunol. 2009;123:1342–1348. doi: 10.1016/j.jaci.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 19.Comert S., Karakaya G., Kalyoncu A.F. Wraparound eyeglasses improve symptoms and quality of life in patients with seasonal allergic rhinoconjunctivitis. Int Forum Allergy Rhinol. 2016;6:722–730. doi: 10.1002/alr.21737. [DOI] [PubMed] [Google Scholar]
- 20.Stempel D.A., Thomas M. Treatment of allergic rhinitis: an evidence-based evaluation of nasal corticosteroids versus nonsedating antihistamines. Am J Manag Care. 1998;4:89–96. [PubMed] [Google Scholar]
- 21.Stempel D.A., Woolf R. The cost of treating allergic rhinitis. Curr Allergy Asthma Rep. 2002;2:223–230. doi: 10.1007/s11882-002-0023-0. [DOI] [PubMed] [Google Scholar]