Abstract
Background
To assess the effects of warm compress (WC) on tear film lipid layer, blink pattern and Meibomian gland function in patients with dry eye following femtosecond laser small incision lenticule extraction (SMILE) and laser-assisted subepithelial keratomileusis (LASEK).
Methods
We enrolled 37 eyes of 37 participants, each with dry eye for more than 2 years following SMILE (25 eyes) or LASEK (12 eyes). WC was performed using a spontaneously heating eye mask. Tear film break-up time (TBUT), tear film lipid layer thickness (TFLLT), blink pattern, Meibomian secretory function scores (MGS), visual acuity, spherical equivalent (SE), keratometry, central corneal thickness (CCT) and aberration were assessed before and after WC.
Results
After WC, the following mean values all increased relative to baselines: CCT, SE, minimum (Min-), maximum (Max-) and average (Ave-) TFLLT, TBUT, total MGS (TMGS), number of glands secreting any liquid (MGL), and complete blink rate (CBR) (p values ranging from < 0.001 to 0.042). Partial blink frequency (PBF) and partial blink rate (PBR) decreased (p = 0.002 in both cases). The decrease of PBF was higher in SMILE subgroup than in LASEK (p = 0.030). TBUT variation was positively correlated with that of Ave-TFLLT and TMGS (p = 0.046, 0.028, respectively). Max-TFLLT variation was correlated with that of TMGS (p = 0.020).
Conclusions
WC may temporarily increase tear film thickness and stability, decrease partial blink, and partly augment Meibomian gland function in dry eye patients after corneal refractive surgeries. Future studies are required to investigate long term clinical efficacy and safety.
Keywords: Dry eye, SMILE, LASEK, Warm compress
Background
With the incidence of myopia increasing globally [1], keratorefractive procedures have gained widespread popularity in recent decades. With the benefit of novel techniques, especially the application of femtosecond laser in ophthalmology, keratorefractive procedures are now less invasive and safer, and correct refractive error more accurately than in the past.
Small incision lenticule extraction (SMILE) is the latest keratorefractive procedure. A refractive stromal lenticule is created using a femtosecond laser and extracted through a small peripheral incision, thus modifying the corneal shape and correcting refractive errors [2]. Laser-assisted subepithelial keratomileusis (LASEK) is a surface ablation procedure, which creates an epithelial flap only on the cornea. As both SMILE and LASEK avoid stromal flap creation, fewer corneal nerve fibers are severed, with concomitantly faster regeneration of the corneal nerves and recovery of corneal sensation relative to traditional laser-assisted in situ keratomileusis (LASIK) or femtosecond laser assisted LASIK (FS-LASIK) [3–5].
Nevertheless, as neural damage cannot be avoided completely, post-operative dry eye is still a common complication following SMILE and LASEK. Warm compress (WC) is effective for relieving dry eye syndrome or Meibomian gland dysfunction (MGD) [6, 7]. Here, a novel instrument was employed for assessment of dry eyes to determine the effects of WC on tear film thickness and Meibomian gland function as accurately as possible in post-operative patients.
Methods
Patients
Participants were recruited between July 2017 and October 2017 at the Department of Ophthalmology, Eye and ENT Hospital of Fudan University (Shanghai, China). The study adhered to the tenets of the Declaration of Helsinki and was approved by the Ethical Committee of the Fudan University Eye and ENT Hospital Review Board. All participants were fully informed and gave written consent for publication of this information.
Sample size was calculated by Power and Sample Size Calculators (http://powerandsamplesize.com/Calculators/). Using the data of Tan J, et al. measured by Lipiview [8] and calculation method recommended in the Cochrane Handbook (SDchange=[SD2baseline + SD2final-2 x Corr x SDbaseline x SDfinal]1/2, the correlation between baseline and endpoint was set to 0.5) [9, 10], a sample size of 14 participants was required to detect a treatment effect in TFLLT of 16.90 nm, with a standard deviation (SD) of 22.06 nm, with 80 % power at the 5 % level of statistical significance. Thirty-seven patients were enrolled. Among them, 25 underwent SMILE, and the remaining 12 underwent LASEK. Inclusion criteria were as follows: age ≥ 18 years, reported dry eye syndromes for more than 2 years following refractive surgeries with a tear film break-up time (TBUT) < 10 s. Before refractive surgery, all patients have no complain of dry eye syndrome and the TBUT was longer than 10 s. Exclusion criteria included: the use of topical medications (except ocular lubricants or artificial tears), other dry eye or MGD related therapy at least 1 month prior to the study; active eye inflammation; experienced post-surgical severe ocular or systemic diseases or other long-term complications except dry eye. All patients were instructed to stop using topical medications or wearing contact lenses at least 24 h before examinations, and to avoid skin care products or make-up around the eyes. All patients were routinely screened preoperatively and met the criteria for SMILE or LASEK, and all surgeries went smoothly and were performed by the same experienced surgeon (XTZ).
Surgical procedures
We used the VisuMax femtosecond laser system (Carl Zeiss Meditec, Jena, Germany) to perform SMILE and the Mel-80 excimer laser system (Carl Zeiss Meditec AG, Jena, Germany) to perform LASEK. We previously described these procedures in detail [11, 12].The femtosecond laser settings were as follows: 500 kHz repetition rate, 130 nJ pulse energy, 110 to 120 μm intended cap thickness, 6 to 6.5 mm optical zone, 7.3 to 7.5 mm cap diameter, and a 2 mm side cut at the 12 o’clock position.
Clinical examinations
Study outcome parameters were assessed in the same order before and at 5 min after WC, from least to most invasive: corneal curvature (K1, K2, Km) and central corneal thickness (CCT) measured by Pentacam HR (Oculus GmbH, Wetzlar, Germany), uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA) and spherical equivalent (SE), tear film lipid layer thickness (TFLLT), blink frequency, TBUT, and Meibomian secretary function scores. All examinations were performed between 11:00 am and 17:00 pm in the same room by a single pre-trained and experienced technician. The indoor temperature was set to 22–25 °C.
TBUT was measured using a single fluorescein strip (Jingming New Technology Development Co., Ltd, Tianjin, CHN) to the inferior palpebral conjunctiva after moistening by a drop of normal saline. Time was recorded by digital clock. TBUT was measured three times and the mean was calculated and used in the statistical analyses.
Warm compress
All patients were treated with a warm compress using a spontaneous heating eye mask (Zhenshiming Pharmaceutical Co., Ltd, Fuzhou, Jiangxi, CHN) for 20 min in both eyes according to the manufacturer’s instruction. This eye mask is a standardized, fragrance free, over-the-counter eyeshade, certified after examination and verification by Shanghai Institute of Quality Inspection and Technical Research. At an ambient temperature of 25 ± 2 °C, it takes an average of 3 min to warm up to 35 °C, and maintains temperature over 35 °C for an average of 30 min. The mean temperature was 40.7 °C.
LipiView
An interferometer (LipiView, TearScience® Inc, Morrisville, NC) was used for measuring the quantitative TFLLT and blink frequency dynamically by analyzing more than one million tear film data points. TFLLT was calculated using interferometry color described as interferometric color units (ICUs), which is equivalent to 1 nanometer (nm). Patients were instructed to hold their head in a comfortable position and look directly into the camera without deviation of eye position, and to blink freely throughout imaging. Natural light from the source passed through the tear film and was reflected back to the camera. The measurement region was the lower third of the cornea, approximately 1 mm above the inferior tear meniscus. The minimum (Min-), maximum (Max-), average (Ave-) and standard deviation (-std) TFLLT were analyzed automatically within preset 19.1 s. Simultaneously, total (TBF) and partial blink frequency (PBF) were also recorded, and were used to calculate partial blink rate (PBR, calculated by PBF/TBF) and complete blink rate (CBR, calculated by 1-PBR). The upper cut-off of LipiView is 100 ICU; values higher than this are recorded as 100 + ICU. A conformance factor for imaging ≥ 0.7 was considered acceptable, but to ensure quality of our data, only conformance factor ≥ 0.8 were included in the final analysis.
Meibomian gland evaluator
Secretory function of the Meibomian glands was measured by a handheld Meibomian Gland Evaluator (TearScience® Inc, Morrisville, NC) and recorded as Meibomian gland scores. Gentle and blink-stimulated pressure (0.8 g/mm2 − 1.2 g/mm2) was applied to the Meibomian gland openings along the lower eyelid margin. The width of the evaluator covers an average of 5 gland openings. After gentle clean of the lower eyelid using clean cotton swabs, the evaluator was applied 1–2 mm below and in parallel with the eyelid, near the root of the eyelash. The eyelid was gently turned inside out slightly just until the gland opening was clearly visible. Fifteen glands in 3 regions (temporal, central, and nasal) were evaluated, with an average pressing time of 10–15 s. We graded the number and secretion characteristics of glands: 3 points (clear liquid), 2 points (cloudy liquid), 1 point (toothpaste-like), and 0 (no secretion). The following metrics were calculated: the total Meibomian gland secretion score (TMGS) of all 15 glands, ranging from 0 to 45; the number of glands secreting any liquid (MGL, clear or cloudy liquid, grade 2 or 3); and the number of glands secreting clear liquid (MGC, clear liquid, grade 3).
Statistical analysis
Statistical analysis was performed using SPSS ver. 22.0 (SPSS Inc, Chicago, IL, USA). The right eye was selected as the study eye. Variables were described as averages ± SD. The one-sample Kolmogorov-Smirnov test was used to test for normality. Paired t-tests or Wilcoxon tests were then used to analyze the changes from baseline in normal or non-normal distribution parameters, respectively. Variables were compared between SMILE and LASEK using independent sample t-tests or Mann-Whitney U tests. Pearson or Spearman correlation analyses were used to evaluate the linear relationships between different variables. P < 0.05 was considered statistically significant.
Results
We enrolled 37 right eyes of 37 participants (age 29.5 ± 6.3 years, 14 male and 23 female). The mean time interval since refractive surgery was 29.10 ± 2.70 months (range from 23 to 33 months). Before WC, there was no difference in all indicators between surgeries.
TFLLT
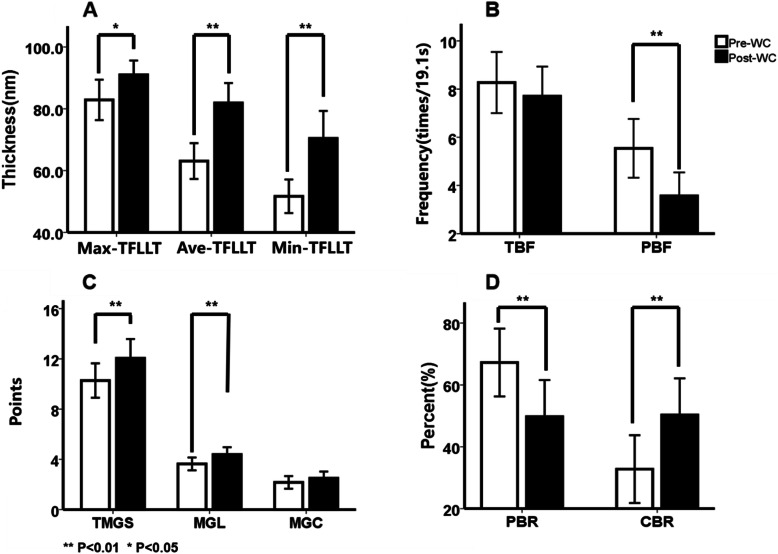
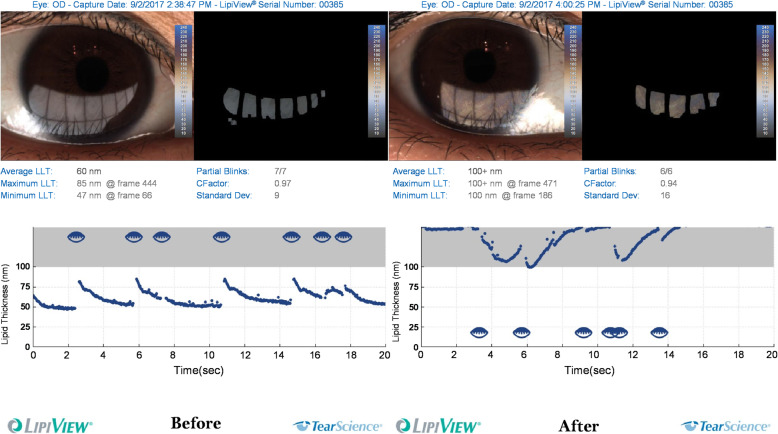
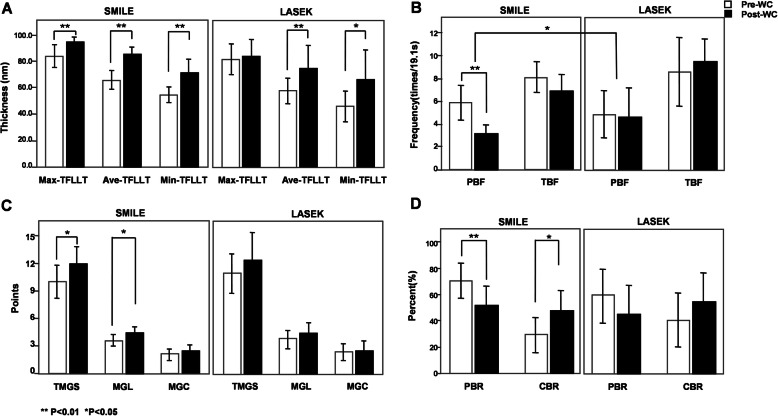
The mean values of Min-, Max- and Ave-TFLLT increased significantly after WC (p < 0.001, p = 0.023, p < 0.001, respectively, Fig. 1A; Table 1), whereas TFLLT-Std did not change. Figure 2 shows the contrast image under the LipiView display window before and after WC. Significant increases of Ave-, Max- and Min-TFLLT were observed in postoperative eyes in the SMILE group (p < 0.001, p = 0.006, p < 0.001, respectively), but only Ave- and Min-TFLLT increased significantly following WC in the LASEK group (p = 0.006 and 0.015, respectively). No significant difference was observed between surgeries (Fig. 3A, Table 2) .
Fig. 1.
Change in TFLLT, blink frequency, meibomian glands scores and blink rate after WC. (A: Min-, Max- and Ave-TFLLT; B: total and partial blink frequency; C: different meibomian glands scores; D: complete and partial blink rate)
Table 1.
Overall differences of indicators from before to after warm compress (WC)
| Pre-WC | Post-WC | P value | |
|---|---|---|---|
| Lipid Layer | |||
| TFLLT-Ave(nm) | 63.08±17.37 | 81.89±19.30 | 0.000* |
| TFLLT-Max(nm) | 82.86±19.62 | 91.00±13.81 | 0.023* |
| TFLLT-Min(nm) | 51.70±16.28 | 70.43±26.60 | 0.000* |
| TFLLT-Std | 5.38±2.60 | 7.84±9.28 | 0.109 |
| TBUT(s) | 5.38±2.19 | 6.38±2.16 | 0.000* |
| Meibomian Gland | |||
| TMGS (0 to 45 points) | 10.28±4.05 | 12.06±4.53 | 0.002* |
| MGL (0 to 15, n) | 3.64±1.51 | 4.39±1.71 | 0.004* |
| MGC (0 to 15, n) | 2.17±1.48 | 2.50±1.58 | 0.139 |
| Blink pattern Parameters | |||
| TBF (times/19.1s) | 8.27±3.81 | 7.70±3.69 | 0.505 |
| PBF (times/19.1s) | 5.54±3.66 | 3.57±2.92 | 0.002* |
| CBR (%) | 32.76±32.89 | 50.28±35.51 | 0.002* |
| PBR (%) | 67.23±32.89 | 49.72±35.51 | 0.002* |
| LogMAR UDVA | -0.05±0.10 | -0.08±0.09 | 0.270 |
| LogMAR CDVA | -0.12±0.07 | -0.13±0.07 | 0.317 |
| SE (Diopter, D) | -0.47±0.52 | -0.34±0.42 | 0.042* |
| K1 | 38.55±2.19 | 38.59±2.22 | 0.953 |
| K2 | 39.44±2.12 | 39.45±2.19 | 0.899 |
| Km | 38.99±2.15 | 39.02±2.19 | 0.816 |
| CCT (um) | 462.47±44.03 | 471.57±49.01 | 0.006* |
| Total HOAs | 0.63±0.51 | 0.85±0.38 | 0.593 |
| Z (4, 0) | 0.30±0.27 | 0.39±0.23 | 0.970 |
| Z (3, 1) | -0.13±0.34 | -0.15±0.34 | 0.101 |
| Z (3, -1) | -0.43±0.46 | -0.42±0.44 | 0.688 |
All data are expressed as the mean ± standard deviations
TFLLT tear film lipid layer thickness, TBUT tear film break-up time, TMGS total Meibomian gland secretion score, MGL glands secreting any liquid, MGC glands secreting clear liquid, TBF total blink frequency, PBF partial blink frequency, PBR partial blink rate, CBR complete blink rate, UDVA uncorrected distance visual acuity, CDVA corrected distance visual acuity, SE spherical equivalent, CCT central corneal thickness, HOAs higher order aberrations
*Significant difference
Fig. 2.
Interference pattern of a patient before (A) and after (B) warm compress under LipiView inspection window
Fig. 3.
Change in TFLLT, blink frequency, meibomian glands scores and blink rate after WC following SMILE and LASEK. (A: Min-, Max- and Ave-TFLLT; B: total and partial blink frequency; C: different meibomian glands scores; D: complete and partial blink rate)
Table 2.
Comparison between SMILE and LASEK before and after WC
| SMILE | P value | LASEK | P value | P value# | |||
|---|---|---|---|---|---|---|---|
| Pre-WC | Post-WC | Pre-WC | Post-WC | ||||
| TFLLT-Ave(nm) | 65.68 ± 18.22 | 85.00 ± 14.67 | 0.000* | 57.67 ± 14.71 | 75.42 ± 26.10 | 0.006* | 0.794 |
| TFLLT-Max(nm) | 83.60 ± 20.46 | 94.16 ± 9.58 | 0.006* | 81.33 ± 18.53 | 84.42 ± 18.81 | 0.694 | 0.666 |
| TFLLT-Min(nm) | 54.48 ± 14.80 | 72.00 ± 22.70 | 0.000* | 45.92 ± 18.31 | 67.17 ± 34.27 | 0.015* | 0.642 |
| TFLLT-Std | 5.56 ± 2.87 | 6.36 ± 3.68 | 0.390 | 5.00 ± 1.95 | 10.92 ± 15.38 | 0.127 | 0.902 |
| TBUT(s) | 5.65 ± 2.12 | 6.26 ± 1.51 | 0.009* | 4.82 ± 2.32 | 6.64 ± 3.20 | 0.008* | 0.772 |
| TMGS (0 to 45 points) | 10.00 ± 4.39 | 11.92 ± 4.67 | 0.011* | 10.91 ± 3.24 | 12.36 ± 4.39 | 0.102 | 0.700 |
| MGL (0 to 15, n) | 3.60 ± 1.55 | 4.40 ± 1.76 | 0.014* | 3.72 ± 1.49 | 4.36 ± 1.69 | 0.142 | 0.710 |
| MGC (0 to 15, n) | 2.08 ± 1.55 | 2.52 ± 1.56 | 0.078 | 2.36 ± 1.36 | 2.45 ± 1.63 | 0.873 | 0.636 |
| TBF (times/19.1s) | 8.12 ± 3.35 | 6.84 ± 3.70 | 0.083 | 8.58 ± 4.78 | 9.50 ± 3.06 | 0.231 | 0.063 |
| PBF (times/19.1s) | 5.88 ± 3.87 | 3.08 ± 2.08 | 0.000* | 4.83 ± 3.24 | 4.58 ± 4.10 | 0.754 | 0.030* |
| CBR (%) | 29.08 ± 33.07 | 48.08 ± 36.30 | 0.012* | 40.43 ± 32.54 | 54.84 ± 34.90 | 0.145 | 0.799 |
| PBR (%) | 70.91 ± 33.07 | 51.93 ± 36.30 | 0.008* | 59.56 ± 32.54 | 45.14 ± 34.90 | 0.145 | 0.691 |
| LogMAR UDVA | -0.05 ± 0.10 | -0.07 ± 0.09 | 0.556 | -0.05 ± 0.14 | -0.10 ± 0.09 | 0.180 | 0.514 |
| LogMAR CDVA | -0.12 ± 0.06 | -0.13 ± 0.07 | 0.317 | -0.13 ± 0.08 | -0.13 ± 0.08 | 1.000 | 0.733 |
| SE (Diopter, D) | -0.43 ± 0.45 | -0.33 ± 0.41 | 0.200 | -0.56 ± 0.66 | -0.35 ± 0.49 | 0.068 | 0.857 |
| K1 | 38.09 ± 2.04 | 38.08 ± 1.96 | 0.560 | 39.63 ± 2.28 | 39.79 ± 2.45 | 0.491 | 0.263 |
| K2 | 39.01 ± 2.04 | 38.96 ± 1.99 | 0.348 | 40.44 ± 2.06 | 40.58 ± 2.33 | 0.541 | 0.486 |
| Km | 38.56 ± 2.04 | 38.52 ± 1.95 | 0.313 | 40.01 ± 2.17 | 40.19 ± 2.37 | 0.064 | 0.032* |
| CCT (um) | 452.71 ± 35.09 | 458.38 ± 37.04 | 0.072 | 485.22 ± 55.83 | 502.33 ± 61.28 | 0.021* | 0.125 |
| Total HOAs | 0.73 ± 0.52 | 0.89 ± 0.42 | 0.274 | 0.43 ± 0.41 | 0.73 ± 0.21 | 0.735 | 0.228 |
| Z (4,0) | 0.30 ± 0.26 | 0.37 ± 0.21 | 0.510 | 0.28 ± 0.31 | 0.46 ± 0.28 | 0.612 | 0.604 |
| Z (3,1) | -0.11 ± 0.38 | -0.14 ± 0.39 | 0.129 | -0.16 ± 0.22 | -0.21 ± 0.12 | 0.436 | 0.708 |
| Z (3, -1) | -0.57 ± 0.42 | -0.56 ± 0.38 | 0.901 | -0.01 ± 0.32 | 0.02 ± 0.29 | 0.528 | 0.670 |
All data are expressed as the mean ± standard deviations
TFLLT tear film lipid layer thickness, TBUT tear film break-up time, TMGS total Meibomian gland secretion score, MGL glands secreting any liquid, MGC glands secreting clear liquid, TBF total blink frequency, PBF partial blink frequency, PBR partial blink rate, CBR complete blink rate, UDVA uncorrected distance visual acuity, CDVA corrected distance visual acuity, SE spherical equivalent, CCT central corneal thickness, HOAs higher order aberrations
*Significant difference (P < 0.05)
#Comparison between SMILE and LASEK
Blink Pattern
Both PBF and PBR decreased significantly after WC (p = 0.002 in both cases, Fig. 1B, D; Table 1). Following SMILE, significant decreases were observed in PBF (p < 0.001) and PBR (p = 0.008), whereas an increase was observed in CBR (p = 0.012). There was no significant change in the LASEK subgroup. Except for PBF (p = 0.030), there was no significant difference between surgeries. (Fig. 3B, D; Table 2)
TBUT and Meibomian Gland Function
The mean TBUT value increased significantly after WC (p < 0.001, Table 1). The differences were significant in both SMILE (p = 0.009) and LASEK (p = 0.008) subgroups, but not between surgeries (Table 2). There were statistically significant increases in TMGS and MGL (p = 0.002, 0.004, respectively), but not in MGC (Fig. 1C, Table 1). Significant increase of TMGS (p = 0.011) and MGL (p = 0.014) was observed in SMILE subgroup, whereas not in LASEK subgroup or between surgeries (Fig. 3C, Table 2).
Safety and other clinical outcomes
No adverse events were observed during the study. After WC, the mean SE value and CCT increased significantly (p = 0.042, 0.006, respectively), while UDVA, CDVA, K1, K2, Km, total higher order aberrations (HOAs), Z (4, 0), Z (3, 1) and Z (3, -1) remained unchanged (p > 0.05) (Table 1). The increased CCT was significant in eyes following LASEK (P = 0.021), but not in eyes following SMILE (p = 0.072). The difference of Km was only significant between surgeries (p = 0.032) but not within any subgroup. Beyond that, no significant differences of other parameters were observed within either subgroup or between surgeries. (Table 2)
Correlation analysis
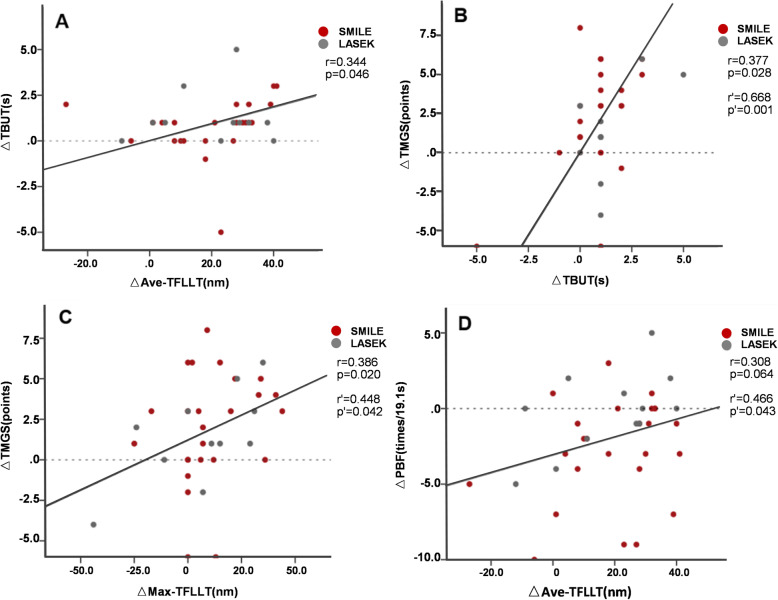
The change in TBUT (△TBUT) was positively correlated with △Ave-TFLLT (Fig. 4A) and △TGMS (Fig. 4B). △Max-TFLLT was positively correlated with △TMGS (Fig. 4C). After adjustment for age, sex and pre-operative SE, △TBUT was still positively correlated with △TMGS (Fig. 4B), also with △MGL (r = 0.649, p = 0.001), △MGC (r = 0.604, p = 0.004) and △TBF (r = 0.487, p = 0.025). △Max-TFLLT was still positively correlated with △TMGS (Fig. 4C), and △Ave-TFLLT was positively correlated with △PBF (Fig. 4D).
Fig. 4.
Correlations between (A) change in Ave-TFLLT and change in tear film break-up time (TBUT); B change in TBUT and change in total Meibomian gland secretion score (TGMS); C change in Max-TFLLT and change in TGMS; D change in Ave-TFLLT and change in partial blink frequency (PBF). R or P-value with superscript indicates result after adjustment for age, sex, and pre-operative SE
Discussion
Dry eye syndrome is one of the most common postoperative complications of corneal refractive surgery (CRS), usually presenting as a transitory phenomenon during the early stages of recovery that naturally resolves several months later. However, complaints of persistent dry eye symptoms cannot be ignored in clinical practice. CRS was reported to be a risk factor for dry eye [13], which in turn increased the risk of refractive regression postoperatively [14]. It is therefore very important to improve the postoperative prognosis and break this vicious cycle by relieving chronic dry eye after CRS. According to previous report, CRS may adversely affect functional meibomian glands, which contributed to chronic tear film dysfunction after CRS [15]. Thermal treatments and eyelid massage are conventional therapy for patients with MGD, but when combined with WC, massage could induce rubbing-related deformation. The risk may be higher for cornea with refractive surgery, which may potentially increase risk of corneal ectasia [16]. So only WC was performed in this study under safety concern. Despite the proven efficacy of WC in various studies, poor compliance can’t be ignored due to time and temperature required [17]. Eyelid thermal pulsation (LipiFlow) therapy was previously reported to improve recalcitrant dry eye syndrome after CRS [18], but it also produced the highest per-treatment cost and was only recommended as second line therapy to MGD patients who were unresponsive to WC [19]. Portable spontaneous heating eye mask has a significant advantage of cost and accessibility over the LipiFlow, and simplify the application of heat therapy, which may improve compliance and make it convenient to use at-home.
Among the different tear layers, the outer lipid layer is thought to retard evaporation and increase stability of the tear film. Changes in distribution and decreased thickness of this layer can lead to dry eye [20], and TFLLT is significantly correlated with other dry eye indicators [21]. As a newly invented ocular surface interferometer, LipiView permits dynamic measurement of the lipid layer thickness with simultaneous recording of the blink pattern. The efficacy and repeatability of this instrument has been previously confirmed [22, 23], and it has been used in the evaluation of dry eye [24], MGD [25] and post-cataract surgery [26]. The repeatability and accuracy of TFLLT measurements with LipiView are superior to another commonly used instrument (Keeler Tearscope-Plus™) [23].
This study showed significant increases in TFLLT and TBUT after WC, and some improvements in Meibomian gland function. One possible explanation is that WC contributes to dilating the Meibomian gland ducts, melting meibum and promoting liquid secretion and thus further reducing the evaporation of tears, and increasing the stability of the tear film. This assumption agree with previous study, which reported that elevated eyelid temperature could unblock the meibomian glands, deliver more meibomian oil and ameliorating dry eye symptoms [27]. Jung et al. reported worse Meibomian gland structure and function in CRS patients following surgery relative to healthy individuals [15]. This being so, it is reasonable to assume that WC will confer greater benefits on postoperative patients than on healthy individuals, a possibility that warrants further investigation. Besides, we observed significant increases in TMGS and MGL but not in MGC, suggesting that the improvement occurred mainly in dysfunctional Meibomian glands by reducing obstruction rather than stimulating secretion. It’s worth noting that the partial recovery time for meibomian gland yielding clear liquid secretion was approximately 2 h in healthy eye [28]. In that case, the nonsignificant change of MGC may be partly related to unrecovered gland function. The recovery time of dysfunctional Meibomian glands was still unclear. Therefore, adequate interval time from baseline evaluation should be preserved in future studies to eliminate this impact.
The increased Ave-TFLLT and Min-TFLLT values were both higher than the upper limits of the deviations for previously repeated measurements (from − 9 to 16 nm) [22], indicating a significant change. The smaller variations of Max-TFLLT relative to Ave-TFLLT and Min-TFLLT may result from limitations of the measurement capability of the former by the LipiView detection range (up to 100 nm), particularly in patients with high Max-TFLLT baseline values. It is worth noting that the dry eye was more prevalent in Asian populations than Australian populations [29, 30]. Moreover, the risk of chronic dry eye after refractive surgery was also significantly higher among Asians [31], suggesting the possibility of ethnic differences in dry eye. Mean Ave-TFLLT was recently measured at 54 nm among Asians [22], which seems significantly lower than previous report in dry eye patients (76 ± 25 nm) [32]. Given that Meibomian gland disease was also more common among patients with low TFLLT (≤ 60 nm) [32], clinicians attending Asian patients should be aware of the risks of post-operative dry eye problems.
Blinking is important for promoting the secretion of lacrimal gland, recoating the cornea with tears, and maintaining good visual acuity. Decreased blinking frequency is an important factor contributing to postoperative tear film instability [31, 33], but the effectiveness of blinking is often overlooked in clinical practice. In our study, both PBF and PBR decreased significantly after WC, indicating improved blink efficiency. TRF appeared unaffected both by WC and by other variables that we measured. It is reasonable to assume that relative to total blinking, partial blinking might have a bigger impact on long-term tear film stability. This conjecture was supported by a previous study, which indicated that extent of blinking rather than total blink rate was the determinant for tear film instability [34]. A possible explanation is that incomplete blinking may cause defects in re-distribution of the mucin and lipid layers, thereby increasing tear evaporation and decreasing lipid layer thickness. Moreover, the impaired corneal innervation and reduced protective blink reflex following CRS may increase partial blinking rate and tear film instability [35]. It is particularly noteworthy that the blinking habit is trainable, and blink efficiency exercises can achieve long-lasting benefits [35, 36]. Methods to modify blinking habits and reduce partial blinking are therefore worth exploring for postoperative patients with chronic dry eye.
Association between tear film, meibomian gland function and blinking pattern has been noticed in many clinical studies [24, 33]. To explore the role of TFLLT, blink pattern and meibomian gland function in tear film stability after CRS, we conducted multiple correlation analyses. We show that variation in TBUT was positively correlated with that of TFLLT and Meibomian gland scores, and the latter two parameters were also positively correlated. These results implied that TFLLT and Meibomian gland function may be a protective factors of tear film stability after CRS. Besides, TFLLT measurement was reported to be affected by demographic factors such as age and sex [24]. After adjustment, the variation in PBF was positively correlated with Ave-TFLLT, suggesting that blinking pattern may also be involved in the increase of TFLLT after WC. This is not surprising as the tear film lipid layer is originated from meibum, secreted from the meibomian gland and spread onto the ocular surface with each blink [37]. TFLLT, Meibomian gland score and blink pattern might also be effective indices for tear film evaluation, like the traditional indicator TBUT.
To further compare benefits between the two surgery types, we analyzed the effects of WC on SMILE and LASEK patients. There was no significant difference between two groups before WC. After WC, TFLLT-Max, CBR and Meibomian gland function improved significantly in the SMILE group, whereas PBF and PBR decreased. No significant changes of any above indicators were observed in the LASEK group, indicating that different surgical procedures may differ in their impact on the recoverability of TFLLT and blink pattern. Previous study reported that the Meibomian gland parameters showed worsening after refractive surgery, more in the SMILE group than LASEK group [15], which agrees with the baseline Meibomian gland evaluation result in our study. In that case, WC may be more beneficial for the SMILE group. Moreover, although SMILE and LASEK are both flapless corneal refractive surgeries with only superficial corneal ablation, the former had worse recovery of corneal sensitivity following surgery, besides, association among the blinking rate, TFLLT, and corneal sensitivity was also noticed [38]. Therefore, the varying degree of postoperative corneal sensitivity recovery may partly explain the different change of TFLLT and blink pattern following SMILE and LASEK. However, at more than 2 years after surgery, we observed no significant difference between surgeries except PBF. Similarly, Chung B, et al. also reported that the decrease in corneal sensitivity recovered to baseline level at 6 months after both SMILE and LASEK [38]. Accordingly, we presumed that the long-term difference between SMILE and LASEK might be slight, which need to be further investigated.
To further assess the safety and other clinical outcomes of this treatment, we measured visual acuity, SE, keratometry, corneal thickness, and aberration but observed no significant differences before and after WC except CCT. According to Niimi J, et al., increased tear osmolarities are associated with thinner corneas, and eye closure can create a hypoosmotic environment by reducing tear evaporation and tear drainage, and lead to increase of CCT [39]. This may partly explain the increase of CCT during eye-closed WC procedure. Besides, the tear evaporation can be further reduced with increased TFLLT during WC, which may also contribute to low tear osmolarity established within a short time. Moreover, thicker cornea was associated with slower deswelling [39], which may be involved in the difference between surgeries, considering the baseline CCT value seems higher in LASEK group. No significant change of keratometry was observed after WC, which indicated this WC method would not cause obvious corneal deformation in CRS patients. The Solomon et al. reported blurred vision and decreased visual acuity after WC [40]. Interestingly, the slight but significant decrease we observed in SE was the opposite of that. Different WC methods and measurement sequences among studies may account for this discrepancy. For example, vision measured immediately after WC might be blurred. At present study, WC went smoothly without adverse effects or complaints of discomfort, demonstrating that short-term WC was safe for post-CRS patients.
There are some limitations to our study. First, both eyes were treated simultaneously and there was a lack of control group. As mentioned above, eye closure itself can influence tear evaporation and drainage, in addition, diurnal variations were detected in both tear flow and corneal thickness [41, 42]. To eliminate bias, nonheated eye mask with similar material could have been applied to the contralateral eye as a control. Second, this study focused exclusively on changes shortly after WC. According to the Tear Film and Ocular Surface Society’s Dry Eye Workshop II (TFOS DEWS II), the TBUT improvement following a single application of WC can last for up to 30 min and repeated eyelid warming achieve a stable improvement on both tear film and meibomian gland function [17]. Studies over a longer time scale and regular WC sessions are needed as a follow-up. Third, the TFOS DEWS II also recommended optimal WC treatment temperature of ≥ 40℃, which refers to temperature on palpebral conjunctiva and the gland, not on the external skin of the eyelids [17]. Immediately after removal of a heated eyebag, the maximal internal eyelid temperature was about 1.5℃ less warm than the mean surface temperature of the eyebag [43]. Considering the mean temperature was 40.7 °C in this study, the actual temperature on palpebral conjunctiva and the gland may be a little inadequate. An infrared thermometer along with the WC device in recommended, for even temperature maintenance and accurate temperature record. Fourth, LipiView only measured the lower part of the cornea and we therefore lacked information about overall corneal condition. This may have increased the likelihood that our analyses exaggerated the role of incomplete blinking on tear thinning, because the consequences of such blinking are localized on the inferior cornea [36]. Finally, the sample size in this study is small, and a larger sample size is expected for further investigations.
Conclusions
In conclusion, our study demonstrated that WC may temporally increase TFLLT and TBUT, decrease incomplete blink and partly improve Meibomian gland function in dry eye patients after SMILE and LASEK. It seems more beneficial for the former. Further investigation of long-term clinical efficacy and safety needs to be performed.
Acknowledgements
Not applicable.
Abbreviations
- WC
Warm compress
- SMILE
Femtosecond laser small incision lenticule extraction
- LASEK
Laser-assisted subepithelial keratomileusis
- LASIK
Laser-assisted in situ keratomileusis
- FS-LASIK
Femtosecond laser-assisted in situ keratomileusis
- TBUT
Tear film break-up time
- TFLLT
Tear film lipid layer thickness
- MGS
Meibomian secretory function scores
- Min-
Minimum
- Max-
Maximum
- Ave-
Average
- TMGS
Total Meibomian secretory function scores
- MGL
Number of glands secreting any liquid
- TBF
Total blink frequency
- MGC
Number of glands secreting clear liquid
- CBR
Complete blink rate
- PBF
Partial blink frequency
- PBR
Partial blink rate
- CCT
Central corneal thickness
- UDVA
Uncorrected distance visual acuity
- CDVA
Corrected distance visual acuity
- SE
Spherical equivalent
- ICUs
Interferometric color units
- std
Standard deviation
- HOAs
Higher order aberrations
- CRS
Corneal refractive surgery
Authors' contributions
XYZ, YS and XTZ: designed study; XYZ, YS, JS: conducted study; XYZ, JS: collected data; XYZ, YS: analyzed and interpreted data; XYZ, wrote the main manuscript text; XYZ, prepared figures and table; all authors reviewed the manuscript; XTZ: final approval of article. The author(s) read and approved the final manuscript.
Funding
Supported by the National Natural Science Foundation of China (Grant No. 81770955), Joint research project of new frontier technology in municipal hospitals (SHDC12018103), Project of Shanghai Science and Technology (Grant No.20410710100), Major clinical research project of Shanghai Shenkang Hospital Development Center (SHDC2020CR1043B) and the Project of Shanghai Xuhui District Science and Technology (2020-015).
Availability of data and materials
Data and materials are available upon request from the corresponding author at doctzhouxingtao@163.com.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the Ethics Committee of the Eye and ENT Hospital Review Board of Fudan University. Written informed consent was obtained from all patients after the nature and possible consequences of the study were explained.
Consent for publication
All participants in this study signed written consent forms for the publication of their relevant clinical data.
Competing interests
The authors declare that there is no competing interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xueyi Zhou and Yang Shen contributed equally to this work and are considered co-first authors.
References
- 1.Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Sekundo W, Kunert KS, Blum M. Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6 month prospective study. Br J Ophthalmol. 2011;95(3):335–339. doi: 10.1136/bjo.2009.174284. [DOI] [PubMed] [Google Scholar]
- 3.Li M, Zhou Z, Shen Y, Knorz MC, Gong L, Zhou X. Comparison of corneal sensation between small incision lenticule extraction (SMILE) and femtosecond laser-assisted LASIK for myopia. J Refract Surg. 2014;30(2):94–100. doi: 10.3928/1081597X-20140120-04. [DOI] [PubMed] [Google Scholar]
- 4.Kobashi H, Kamiya K, Shimizu K. Dry eye after small incision lenticule extraction and femtosecond laser-assisted LASIK: meta-analysis. Cornea. 2017;36(1):85–91. doi: 10.1097/ICO.0000000000000999. [DOI] [PubMed] [Google Scholar]
- 5.Darwish T, Brahma A, O’Donnell C, Efron N. Subbasal nerve fiber regeneration after LASIK and LASEK assessed by noncontact esthesiometry and in vivo confocal microscopy: prospective study. J Cataract Refract Surg. 2007;33(9):1515–1521. doi: 10.1016/j.jcrs.2007.05.023. [DOI] [PubMed] [Google Scholar]
- 6.Arita R, Morishige N, Sakamoto I, Imai N, Shimada Y, Igaki M, Suzuki A, Itoh K, Tsubota K. Effects of a warm compress containing menthol on the tear film in healthy subjects and dry eye patients. Sci Rep. 2017;7:45848. doi: 10.1038/srep45848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olson MC, Korb DR, Greiner JV. Increase in tear film lipid layer thickness following treatment with warm compresses in patients with Meibomian gland dysfunction. Eye Contact Lens. 2003;29(2):96–99. doi: 10.1097/01.ICL.0000060998.20142.8D. [DOI] [PubMed] [Google Scholar]
- 8.Tan J, Ho L, Wong K, La A, Lee S, Park S, Tran L, Stapleton F. The effects of a hydrating mask compared to traditional warm compresses on tear film properties in meibomian gland dysfunction. Cont Lens Anterior Eye. 2018;41(1):83–87. doi: 10.1016/j.clae.2017.09.006. [DOI] [PubMed] [Google Scholar]
- 9.Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
- 10.Pang SP, Chen YT, Tam KW, Lin IC, Loh EW. Efficacy of vectored thermal pulsation and warm compress treatments in Meibomian gland dysfunction: a meta-analysis of randomized controlled trials. Cornea. 2019;38(6):690–697. doi: 10.1097/ICO.0000000000001907. [DOI] [PubMed] [Google Scholar]
- 11.Yao P, Zhao J, Li M, Shen Y, Dong Z, Zhou X. Microdistortions in Bowman’s layer following femtosecond laser small incision lenticule extraction observed by Fourier-Domain OCT. J Refract Surg. 2013;29:668–674. doi: 10.3928/1081597X-20130806-01. [DOI] [PubMed] [Google Scholar]
- 12.Li M, Zhao Y, Xiao Q, Yao P, Piao M, Sun L, Zhou X. Demarcation line in the human cornea after surface ablation observed by optical coherence tomography and confocal microscopy. Eye Contact Lens. 2018;44:S19–S23. doi: 10.1097/ICL.0000000000000459. [DOI] [PubMed] [Google Scholar]
- 13.(No authors listed). The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5(2):75–92. [DOI] [PubMed]
- 14.Albietz JM, Lenton LM, McLennan SG. Chronic dry eye and regression after laser in situ keratomileusis for myopia. J Cataract Refract Surg. 2004;30:675–684. doi: 10.1016/j.jcrs.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 15.Jung JW, Kim JY, Chin HS, Suh YJ, Kim TI, Seo KY. Assessment of meibomian glands and tear film in post-refractive surgery patients. Clin Exp Ophthalmol. 2017;45(9):857–866. doi: 10.1111/ceo.12993. [DOI] [PubMed] [Google Scholar]
- 16.McMonnies C, Korb D, Blackie CA. The role of heat in rubbing and massage-related corneal deformation. Cont Lens Anterior Eye. 2012;35:148–154. doi: 10.1016/j.clae.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 17.Jones L, Downie LE, Korb D, Benitez-Del-Castillo JM, Dana R, Deng SX, Dong PN, Geerling G, Hida RY, Liu Y, Seo KY, Tauber J, Wakamatsu TH, Xu J, Wolffsohn JS, Craig JP. TFOS DEWS II management and therapy report. Ocul Surf. 2017;15(3):575–628. doi: 10.1016/j.jtos.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 18.Schallhorn CS, Schallhorn JM, Hannan S, Schallhorn SC. Effectiveness of an eyelid thermal pulsation procedure to treat recalcitrant dry eye symptoms after laser vision correction. J Refract Surg. 2017;33(1):30–36. doi: 10.3928/1081597X-20161006-05. [DOI] [PubMed] [Google Scholar]
- 19.Lam PY, Shih KC, Fong PY, Chan TCY, Ng AL, Jhanji V, Tong L. A review on evidence-based treatments for Meibomian gland dysfunction. Eye Contact Lens. 2020;46(1):3–16. doi: 10.1097/ICL.0000000000000680. [DOI] [PubMed] [Google Scholar]
- 20.Goto E, Tseng SC. Differentiation of lipid tear deficiency dry eye by kinetic analysis of tear interference images. Arch Ophthalmol. 2003;121:173–180. doi: 10.1001/archopht.121.2.173. [DOI] [PubMed] [Google Scholar]
- 21.Blackie CA, Solomon JD, Scaffidi RC, Greiner JV, Lemp MA, Korb DR. The relationship between dry eye symptoms and lipid layer thickness. Cornea. 2009;28:789–794. doi: 10.1097/ICO.0b013e318191b870. [DOI] [PubMed] [Google Scholar]
- 22.Zhao Y, Tan CLS, Tong L. Intra-observer and inter-observer repeatability of ocular surface interferometer in measuring lipid layer thickness. BMC Ophthalmology. 2015;15(1):53. doi: 10.1186/s12886-015-0036-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Markoulli M, Duong TB, Lin M, Papas E. Imaging the Tear Film: A Comparison Between the Subjective Keeler Tearscope-PlusTM and the Objective Oculus® Keratograph 5 M and LipiView® Interferometer. Curr Eye Res. 2018;43(2):1–8. [DOI] [PubMed]
- 24.Jung JW, Park SY, Kim JS, Kim EK, Seo KY, Kim TI. Analysis of factors associated with the tear film lipid layer thickness in normal eyes and patients with dry eye syndrome. Invest Ophthalmol Vis Sci. 2016;57:4076–4083. doi: 10.1167/iovs.16-19251. [DOI] [PubMed] [Google Scholar]
- 25.Ji YW, Lee J, Lee H, Seo KY, Kim EK, Kim TI. Automated measurement of tear film dynamics and lipid layer thickness for assessment of non-sjögren dry eye syndrome with Meibomian gland dysfunction. Cornea. 2016;36(2):176–182. doi: 10.1097/ICO.0000000000001101. [DOI] [PubMed] [Google Scholar]
- 26.Kim JS, Lee H, Choi S, Kim EK, Seo KY, Kim TI. Assessment of the tear film lipid layer thickness after cataract surgery. Semin Ophthalmol. 2016;4:231–236. doi: 10.1080/08820538.2016.1208764. [DOI] [PubMed] [Google Scholar]
- 27.Borchman D. The optimum temperature for the heat therapy for meibomian gland dysfunction. Ocul Surf. 2019;17(2):360–364. doi: 10.1016/j.jtos.2019.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blackie CA, Korb DR. Recovery time of an optimally secreting meibomian gland. Cornea. 2009;28(3):293–297. doi: 10.1097/ICO.0b013e31818913b4. [DOI] [PubMed] [Google Scholar]
- 29.Jie Y, Xu L, Wu YY, Jonas JB. Prevalence of dry eye among adult Chinese in the Beijing Eye Study. Eye (Lond) 2009;23:688–693. doi: 10.1038/sj.eye.6703101. [DOI] [PubMed] [Google Scholar]
- 30.McCarty CA, Bansal AK, Livingston PM, Stanislavsky YL, Taylor HR. The epidemiology of dry eye in Melbourne Australia. Ophthalmology. 1998;105:1114–1119. doi: 10.1016/S0161-6420(98)96016-X. [DOI] [PubMed] [Google Scholar]
- 31.Albietz JM, Lenton LM, McLennan SG. Dry eye after LASIK: comparison of outcomes for Asian and Caucasian eyes. Clin Exp Optom. 2005;88(2):89–96. doi: 10.1111/j.1444-0938.2005.tb06673.x. [DOI] [PubMed] [Google Scholar]
- 32.Finis D, Pischel N, Schrader S, Geerling G. Evaluation of lipid layer thickness measurement of the tear film as a diagnostic tool for Meibomian gland dysfunction. Cornea. 2013;32(12):1549–1553. doi: 10.1097/ICO.0b013e3182a7f3e1. [DOI] [PubMed] [Google Scholar]
- 33.Chen Q, Li M, Yuan Y, Yu Y, Shi G, Wang X, Ke B. Effects of tear film lipid layer thickness and blinking pattern on tear film instability after corneal refractive surgery. Cornea. 2017;36(7):810–815. doi: 10.1097/ICO.0000000000001207. [DOI] [PubMed] [Google Scholar]
- 34.Hirota M, Uozato H, Kawamorita T, Shibata Y, Yamamoto S. Effect of incomplete blinking on tear film stability. Optom Vis Sci. 2013;90(7):650–657. doi: 10.1097/OPX.0b013e31829962ec. [DOI] [PubMed] [Google Scholar]
- 35.Mcmonnies CW. Incomplete blinking: exposure keratopathy, lid wiper epitheliopathy, dry eye, refractive surgery, and dry contact lenses. Cont Lens Anterior Eye. 2007;30(1):37–51. doi: 10.1016/j.clae.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 36.McMonnies Charles W. Blink efficiency: a neglected area of ocular surface disease management? Invest Ophthalmol Vis Sci. 2011;52(7):4484. doi: 10.1167/iovs.11-7751. [DOI] [PubMed] [Google Scholar]
- 37.Willcox MDP, Argüeso P, Georgiev GA, Holopainen JM, Laurie GW, Millar TJ, Papas EB, Rolland JP, Schmidt TA, Stahl U, Suarez T, Subbaraman LN, Uçakhan OÖ, Jones L. TFOS DEWS II Tear Film Report. Ocul Surf. 2017;15(3):366–403. doi: 10.1016/j.jtos.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chung B, Choi M, Lee KY, Kim EK, Seo KY, Jun I, Kim KY, Kim TI. Comparing dry eye disease after small incision lenticule extraction and laser subepithelial keratomileusis. Cornea. 2020;39(4):501–507. doi: 10.1097/ICO.0000000000002240. [DOI] [PubMed] [Google Scholar]
- 39.Niimi J, Tan B, Chang J, Zhou Y, Ghanekar A, Wong M, Lee A, Lin MC. Diurnal pattern of tear osmolarity and its relationship to corneal thickness and deswelling. Cornea. 2013;32(10):1305–1310. doi: 10.1097/ICO.0b013e31829b21d1. [DOI] [PubMed] [Google Scholar]
- 40.Solomon JD, Case CL, Greiner JV, Blackie CA, Herman JP, Korb DR. Warm compress induced visual degradation and Fischer Schweitzer polygonal reflex. Optom Vis Sci. 2007;84(7):580–587. doi: 10.1097/OPX.0b013e3180dc99d5. [DOI] [PubMed] [Google Scholar]
- 41.Shen M, Wang J, Qu J, Xu S, Wang X, Fang H, Lu F. Diurnal variation of ocular hysteresis, corneal thickness, and intraocular pressure. Optom Vis Sci. 2008;85(12):1185–1192. doi: 10.1097/OPX.0b013e31818e8abe. [DOI] [PubMed] [Google Scholar]
- 42.Harper CL, Boulton ME, Bennett D, Marcyniuk B, Jarvis-Evans JH, Tullo AB, Ridgway AE. Diurnal variations in human corneal thickness. Br J Ophthalmol. 1996;80(12):1068–1072. doi: 10.1136/bjo.80.12.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bilkhu PS, Naroo SA, Wolffsohn JS. Effect of a commercially available warm compress on eyelid temperature and tear film in healthy eyes. Optom Vis Sci. 2014;91(2):163–170. doi: 10.1097/OPX.0000000000000134. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data and materials are available upon request from the corresponding author at doctzhouxingtao@163.com.