Abstract
Objective:
By definition, restricting (ANR) and binge-eating/purging (ANBP) subtypes of anorexia nervosa (AN) differ in some manifestations of maladaptive eating behavior. This study aimed to determine whether the groups differ in the choices they make about what to eat, and whether there are differences in valuation related to food choice, using an experimental paradigm.
Method:
Inpatients with ANR (n = 40) and ANBP (n = 46) participated in a Food Choice Task. During the task, participants rated 76 food images for healthiness and tastiness, and choice preferences. Groups were compared in percent selection of high-fat and low-fat foods, value ratings of foods, and engagement of self-control in food choice.
Results:
There were no differences between AN subtypes in healthiness or tastiness ratings, or in tendency to limit choice of high-fat foods. There was no difference between the groups in measures of self-control in food choice.
Discussion:
Individuals with ANR and ANBP similarly manifest reduced choices of high-fat foods, with similar tendencies to undervalue the tastiness of high-fat foods. These results suggest that while individuals with ANR and ANBP differ across a range of clinical characteristics, the decision-making process associated with the maladaptive restriction of high-fat foods characteristic of AN is shared by both subtypes.
Keywords: anorexia nervosa, choice, decision-making, eating behavior, eating disorders, subtype
1 |. INTRODUCTION
Since the publication of DSM-IV in 1994, two subtypes of anorexia nervosa (AN) have been formally distinguished: restricting (ANR) and binge-eating/purging (ANBP) (American Psychiatric Association, 2000). Existing research has found, with some consistency, that individuals with ANBP are more impulsive (Peat, Mitchell, Hoek, & Wonderlich, 2009; Waxman, 2009), experience higher rates of suicide attempts, self-injurious behavior, and substance use (Peat et al., 2009; Peterson et al., 2016) and report more severe eating disorder psychopathology (De Young et al., 2013; Ekeroth, Clinton, Norring, & Birgegård, 2013; Lewis et al., 2019; Murao et al., 2017; Reas & Ro, 2018). By definition, the two subtypes also differ in certain manifestations of actual eating behavior. While all individuals with AN (i.e., both subtypes) engage in dietary restriction leading to significantly low weight, individuals with ANBP additionally experience recurrent binge-eating and/or purging episodes.
Examination of actual food choices, and the influence of individualized food valuation ratings on food choice, may help clarify similarities and differences in components of decision-making between the subtypes of AN. In the present study, we used a Food Choice Task previously shown to capture restrictive food choice in individuals with AN (Dalton et al., 2020; Foerde, Steinglass, Shohamy, & Walsh, 2015; Steinglass, Foerde, Kostro, Shohamy, & Walsh, 2015) and relate to actual food intake the following day to examine whether food-based decision-making differs between AN subtypes.
The Food Choice Task used in this study successfully captures the caloric restriction characteristic of AN; in this task, compared with healthy controls, individuals with AN choose high-fat foods less frequently (z = −2.59, p = .009) (Steinglass et al., 2015). Furthermore, food choice in the task predicts actual caloric intake; the tendency to choose high-fat foods in the task is significantly associated with caloric intake in a buffet meal the next day (Foerde et al., 2015; Foerde et al., 2020). In addition, when presented with opportunities that require self-control (to choose a healthy, less tasty food item or to not choose an unhealthy, tasty food item), individuals with AN exhibit more self-control than do controls (Dalton et al., 2020; Foerde et al., 2015).
These studies identified differences between individuals with AN and healthy control participants; they were not designed to assess differences between subtypes of AN. In the current study, we combined data from two prior studies (Foerde et al., 2015; Foerde et al., 2020) with an additional group of patients with AN to achieve a sample size large enough to compare the behavior of patients with ANBP to that of patients with ANR on the Food Choice Task. Research comparing eating behavior in individuals with ANR and ANBP is limited. However, binge eating in individuals with bulimia nervosa is associated with a specific increase in the intake of dietary fat (Alpers & Tuschen-Caffier,- 2004; Gendall, Sullivan, Joyce, Carter, & Bulik, 1997; Walsh, Kissileff, & Hadigan, 1989) and analysis of loss of control eating in both children (Tanofsky-Kraff et al., 2009) and adults (Hadigan, Kissileff, & Walsh, 1989) reflects increased intake of high-calorie desserts and snack. Given the absence of binge eating (i.e., concurrent loss of control and overeating) among individuals with ANR and the consistent finding of impulsivity among individuals with ANBP, we hypothesized that individuals with ANBP would rate high-fat foods as more tasty, would more frequently choose high-fat foods to eat, and would employ self-control less frequently compared to individuals with ANR.
2 |. METHODS
2.1 |. Participants
All participants were females ≥16 years of age who met criteria for AN at the time of admission for inpatient care at the New York State Psychiatric Institute. Of the 86 participants (ANR: n = 40; ANBP: n = 46), 52 participated in one of two studies which used the Food Choice Task during fMRI scanning (ANR: n = 20; ANBP: n = 32) (Foerde et al., 2015; Foerde et al., 2020). We have pooled data from these participants with data from 34 AN participants (ANR: n = 20; ANBP: n = 14) who completed the task outside of the MRI scanner. Diagnosis was established by Eating Disorders Assessment for DSM-5 (Sysko et al., 2015) or Eating Disorders Examination (Fairburn, 2008). All studies were approved by the NYSPI Institutional Review Board and all participants provided written informed consent (individuals under 18 years of age gave assent and a parent or guardian provided consent).
2.2 |. Food choice task
The Food Choice Task (Steinglass et al., 2015) is comprised of three phases (see Figure S1): Healthiness rating, Tastiness rating, and Choice. In the Healthiness and Tastiness rating phases, participants were shown images of the same 76 food items (38 high-fat, 38 low-fat), presented in predetermined pseudo-random order (different order in each phase); the order of these two phases was randomly assigned. High-fat food items were defined as those with >30% of total calories from fat (NCEP, 2001). Prior to the task, participants were asked to identify the food items to ensure familiarity. Participants rated healthiness and tastiness of the 76 food items on a 5-point scale, on which “3” indicated “neutral.” After the two rating phases, one food item rated as “neutral” on both healthiness and tastiness was selected as a Reference Item to be used in the Choice phase. If no item was rated as “3” on both healthiness and tastiness, an item that had been rated “3” on healthiness and “4” or above on tastiness was used as the Reference Item because a neutral healthy but tasty item would have greater overall value than an unhealthy item for a participant who made decisions based on health information (Foerde et al., 2015; Steinglass et al., 2015). In the Choice phase, the Reference item was presented on the left side of the screen and the trial-unique food item on the right. Participants were asked to indicate their preference to eat the Reference Item or the trial-unique item on a 5-point scale. To incentivize choices reflective of actual preferences, participants were told that one of their chosen food items would be given to them as a snack after the task. Following the task, participants were served a snack-sized portion of one of their (randomly selected) food choices. Task test–retest reliability (Foerde et al., 2018) and validity in relation to actual food intake (Foerde et al., 2015) have been established.
2.3 |. Procedures
All participants completed the Food Choice Task within 1 week of hospital admission, two hours after a standardized lunch of ∼550 kcal. Height and weight were obtained on the day of testing. Eating disorder symptoms were assessed using the Eating Disorder Examination Questionnaire (EDE-Q) (Fairburn, 2008) and the Three Factor Eating Questionnaire (TFEQ) (Stunkard & Messick, 1985).
2.4 |. Data analysis
Demographic and clinical characteristics were compared using independent samples t-test within the IBM SPSS Statistics 26 analysis package. Alpha was set at 0.05. There were no significant differences in task behavior between the 52 patients with AN who performed the Food Choice Task during fMRI scanning and the 34 who performed the task outside the scanner (data available upon request). Therefore, data from all participants was analyzed as a single sample.
For Healthiness and Tastiness phases, mean ratings for high- and low-fat foods were calculated for each participant. For the Choice phase, responses on the five-point scale were converted to binary “Yes” or “No” preferences for the trial-unique food item versus the constant neutral reference item and the proportion of choices of the trial-unique food was calculated for high-fat and low-fat foods separately. Neutral responses were omitted from choice analyses. Summary ratings and choice data were analyzed using mixed ANOVA (2 [subtype] × 2 [high-fat/low-fat]). Summary ratings and choice data were analyzed within IBM SPSS Statistics 26 analysis package.
The influence of healthiness and tastiness ratings on food decisions in the Choice block was examined using multilevel regression models (lme4 linear mixed effects package for R (Bates, Maechler, & Bolker, 2011). Binomial choice data were modeled with multilevel logistic regression, in which participant choice (selection of the trial-unique food item over the reference food) was the dependent variable and z-scored healthiness and tastiness ratings were entered as independent variables. Continuous outcome rating data from the Healthiness and Tastiness phases were modeled using multilevel linear regression. In all analyses, models included by-subject random intercepts and slopes (Barr, Levy, Scheepers, & Tily, 2013).
To examine self-control, trials were first categorized as to whether they presented a conflict between healthiness and tastiness ratings (food items rated tasty and unhealthy or non-tasty and healthy). On these trials, “self-control” was used when choosing a healthy but non-tasty food, or not choosing a tasty but unhealthy food. Trials with neutral responses were omitted. The proportion of trials with an opportunity for self-control (coded 1/0) and use versus nonuse of self-control (coded 1/0) were modeled using multilevel logistic regression entering Diagnosis (ANR/ANBP coded −1/+1) as independent variables.
3 |. RESULTS
3.1 |. Clinical characteristics
Clinical characteristics are summarized in Table 1. ANR and ANBP did not differ significantly in mean age or duration of illness. Mean BMI of the ANBP group was significantly higher than that of the ANR group. Mean scores on the EDE-Q and on the Disinhibition scales of the TFEQ were significantly higher in the ANBP group than the ANR group.
TABLE 1.
Demographic and clinical characteristics
| ANR (n = 40) |
ANBP (n = 46) |
Subtype comparison |
|||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t | df | P | |
| Age (years) | 27.8 | 7.7 | 26.4 | 6.3 | 0.93 | 1,84 | .35 |
| BMI (kg/m2) | 15.6 | 2.1 | 16.9 | 1.7 | −3.2 | 1,84 | .002 |
| Duration of illness (years) | 10.9 | 7.8 | 10.4 | 6.2 | 0.34 | 1,84 | .74 |
| EDE-Q total | 3.7 | 1.4 | 4.7 | 1.1 | −3.7 | 1,81 | <.001 |
| EDE-Q eating concern | 2.9 | 1.6 | 4.1 | 1.1 | −4.3 | 1,82 | <.001 |
| EDE-Q restraint | 3.7 | 1.7 | 4.8 | 1.5 | −2.9 | 1,83 | .005 |
| EDE-Q weight concern | 3.9 | 1.6 | 4.9 | 1.3 | −3.3 | 1,82 | .002 |
| EDE-Q shape concern | 4.2 | 1.4 | 5.1 | 1.1 | −3.3 | 1,82 | .002 |
| TFEQ restraint | 16.3 | 3.3 | 17.7 | 3.5 | −1.8 | 1,84 | .07 |
| TFEQ disinhibition | 3.9 | 3.2 | 6.3 | 4.4 | −2.9 | 1,84 | .005 |
| TFEQ hunger | 4.1 | 3.6 | 4.8 | 3.6 | −0.8 | 1,84 | .42 |
| Race/ethnicity | N | % | N | % | |||
| Asian | 2 | 5.0 | 2 | 4.3 | |||
| Black/African American | 0 | 0 | 2 | 4.3 | |||
| Hispanic/Latino | 3 | 7.5 | 1 | 2.2 | |||
| Caucasian | 35 | 87.5 | 41 | 89.1 | |||
Note: Data are missing for: one ANR and two ANBP for EDE-Q total; two ANBP for EDE-Q eating concern; one ANBP for EDE-Q restraint; one ANR and one ANBP for EDE-Q weight concern; one ANR and one ANBP for EDE-Q shape concern. All statistically significat p values are marked in bold.
Abbreviations: ANBP, anorexia nervosa, binge-eating/purging subtype; ANR, anorexia nervosa, restricting subtype; BMI, body mass index; EDE-Q, Eating Disorder Examination Questionnaire; TFEQ, Three-Factor Eating Questionnaire.
3.2 |. Food choice task
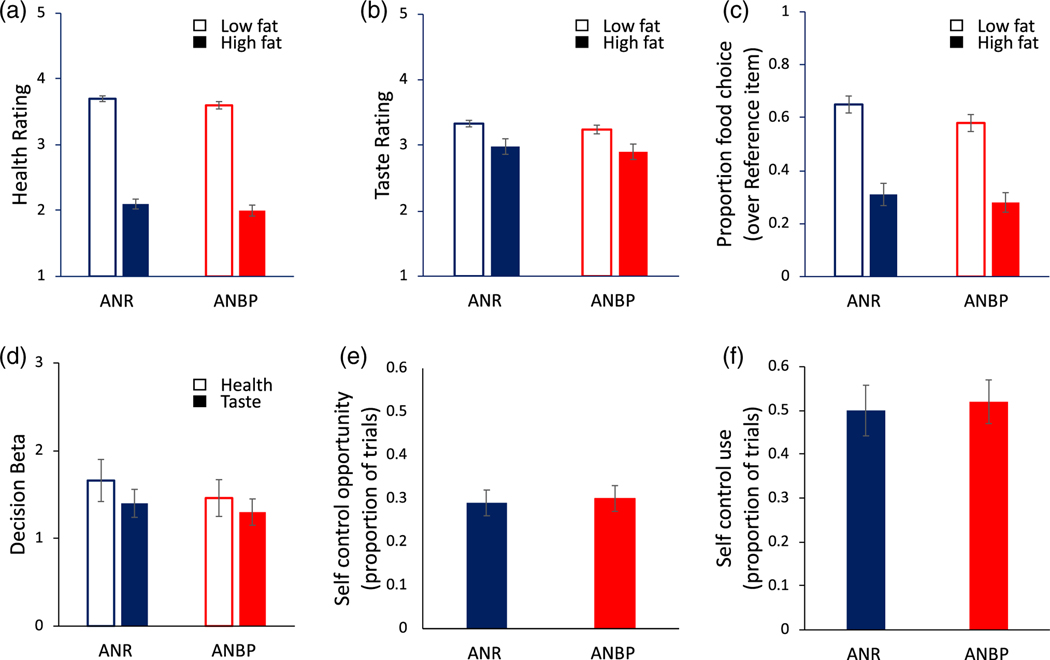
Results of the Food Choice Task are shown in Figure 1. Both AN subtypes rated high-fat foods as less healthy (F[1,84] = 962.2, p < .001) and less tasty than low-fat foods (F[1,84] = 19.2, p < .001). Both ANR and ANBP chose the high-fat food option significantly less often than the low-fat option (F[1,84] = 114, p < .001). There were no differences between the two subtypes in healthiness ratings (p = .13), tastiness ratings (p = .46), percentage of high-fat food choice (p = .57), or in the influence of healthiness (z = 0.64, p = .52) or tastiness (z = 0.37, p = .71) ratings on choice. There were also no differences in the number of choices requiring self-control (z = −0.19, p = .85) or use of self-control (z = −0.24, p = .81).
FIGURE 1.
Food ratings and choice across AN subtypes. (a) ANR and ANBP rated low-fat food items as healthier than high-fat food items with no significant differences in healthiness ratings for either low- or high-fat foods between subtypes. (b) Both subtypes rated high-fat foods as less tasty than low-fat foods. Tastiness ratings for low-fat and high-fat foods did not differ between subtypes. (c) ANR and ANBP chose the high-fat food option less often than the low-fat food item, with no difference between subtypes. (d) Food choices among both subtypes were influenced by both healthiness ratings and tastiness ratings, with no group difference in the influence of healthiness or tastiness on choice. (e) ANR and ANBP did not differ in the number of opportunities to use self-control (i.e., when healthiness and tastiness were in conflict) or (f) in the use of self-control (i.e., chose the healthy/not-tasty, did not choose the not-healthy/tasty item). Note: Two AN participants (ANR: n = 1, ANBP: n = 1) did not have any trials with self-control opportunities and were not included in the analysis of self-control use. ANBP, anorexia nervosa, binge-eating/purging subtype; ANR, anorexia nervosa, restricting subtype
4 |. DISCUSSION
Despite differences in eating disorder severity, and contrary to our hypotheses, there were no differences in food-based decision-making between restricting and binge-eating/purging subtypes of AN in the current study. Several studies using the Food Choice Task have shown that decisions about what to eat differ between individuals with eating disorders and healthy volunteers (Dalton et al., 2020; Foerde et al., 2015; Foerde et al., 2020; Gianini et al., 2019; Steinglass et al., 2015). The current negative results are therefore of interest in that they suggest that despite differences in eating disorder psychopathology, ANR and ANBP do not differ in the restriction of high-fat food, the value ratings that influence these choices, or the self-control needed to implement them.
The lack of difference between subtypes seems at first counterintuitive. Several prior studies have reported more severe eating disorder psychopathology, including increased dietary restraint, in individuals with ANBP relative to ANR (De Young et al., 2013; Ekeroth et al., 2013; Reas & Ro, 2018). Yet here, differences in clinical severity, including higher dietary restraint scores in the ANBP group, were not associated with more restrictive food choices (i.e., choice of fewer high-fat foods) or increased need for/use of self-control to make these restrictive food choices on the Food Choice Task. Rather, despite differing across a range of eating disorder symptoms, the two subtypes were equally likely to avoid high-fat food options. These results are consistent with data from a prior study which used ecological momentary assessment to compare the frequency of restrictive eating behaviors in ANR and ANBP (De Young et al., 2013). In that study, individuals with ANBP reported both increased dietary restraint and certain restrictive eating behaviors (e.g., skipping meals, going 8 hr without eating, limiting overall calories at meals), but did not differ from ANR in their limitation of dietary fat (De Young et al., 2013). Taken together, these studies suggest that the avoidance of high-fat foods is a specific and shared behavioral disturbance in AN. The finding that ANR and ANBP did not differ in other aspects of food-based decision-making (e.g., food valuation, influence of health and taste on food choice, use of self-control) further suggests that the decision-making process guiding restrictive food choice is also shared between subtypes.
The strengths of this study include that the population consisted of a relatively large sample of individuals with AN, with approximately equal numbers of individuals with ANR and ANBP, and the methods were standardized such that all patients were studied while underweight, at the initiation of treatment, and using the same task. The study focused on a single, albeit critical, facet of AN—the restriction of food intake. Future studies comparing ANR and ANBP should consider other psychological and behavioral measures to probe differences between these subtypes. For example, targeted manipulations of specific aspects of impulsivity associated with binge eating, such as negative urgency (Culbert et al., 2016; Lavender et al., 2017; Wolz, Granero, & Fernández-Aranda, 2017) or other emotionally negative situations, may elicit differences in high-fat food choice or the engagement of self-control between individuals with and without binge-eating/purging behavior. It is possible that results from this study would not generalize across emotional states. The average duration of illness in this study was long, suggesting a chronically ill patient group. It may be that decision-making about food differs when the onset of illness is more recent.
In summary, this study found that despite differences in clinical severity, there was no evidence of differences between AN subtypes in choices, ratings of healthiness or tastiness, or in engagement of self-control, when individuals with AN were asked to make decisions about what to eat.
Supplementary Material
Acknowledgments
Funding information
Hilda and Preston Davis Foundation; National Institute of Mental Health, Grant/Award Numbers: K24 MH113737, R01 MH105452, T32 MH096679
Footnotes
DATA AVAILABILITY STATEMENT
The data that support findings from this study are available upon request from the corresponding author.
SUPPORTING INFORMATION
Additional supporting information may be found online in the Supporting Information section at the end of this article.
CONFLICT OF INTEREST
Dr. Steinglass receives royalties from UpToDate. Dr. Walsh receives royalties and honoraria from Guilford Press, McGraw-Hill, Oxford University Press, UpToDate, British Medical Journal, John Hopkins Press, and Guidepoint Global. Drs. Foerde, Shohamy, Uniacke, and Ms. Slattery report no conflicts of interest.
REFERENCES
- Alpers G, & Tuschen-Caffier B. (2004). Energy and macronutrient intake in bulimia nervosa. Eating Behaviors, 5(3), 241–249. 10.1016/j.eatbeh.2004.01.013 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: American Psychiatric Association Press. [Google Scholar]
- Barr DJ, Levy R, Scheepers C, & Tily HJ (2013). Random effects structure for confirmatory hypothesis testing: Keep it maximal. Journal of Memory and Language, 68(3), 255–278. 10.1016/j.jml.2012.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates D, Maechler M, & Bolker B. (2011). Technical Report. [Google Scholar]
- Culbert KM, Lavender JM, Crosby RD, Wonderlich SA, Engel SG, Peterson CB, … Fischer S. (2016). Associations between negative affect and binge/purge behaviors in women with anorexia nervosa: Considering the role of negative urgency. Comprehensive Psychiatry, 66, 104–112. 10.1016/j.comppsych.2016.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton B, Foerde K, Bartholdy S, McClelland J, Kekic M, Grycuk L, … Steinglass JE (2020). The effect of repetitive transcranial magnetic stimulation on food choice-related self-control in patients with severe, enduring anorexia nervosa. The International Journal of Eating Disorders, 53(8), 1326–1336. 10.1002/eat.23267 [DOI] [PubMed] [Google Scholar]
- De Young KP, Lavender JM, Steffen K, Wonderlich SA, Engel SG, Mitchell JE, … Crosby RD (2013). Restrictive eating behaviors are a nonweight-based marker of severity in anorexia nervosa. The International Journal of Eating Disorders, 46(8), 849–854. 10.1002/eat.22163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekeroth K, Clinton D, Norring C, & Birgegård A. (2013). Clinical characteristics and distinctiveness of DSM-5 eating disorder diagnoses: Findings from a large naturalistic clinical database. Journal of Eating Disorders, 1, 31. 10.1186/2050-2974-1-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG (2008). Cognitive behavior therapy and eating disorders. New York: Guilford Press. [Google Scholar]
- Foerde K, Gianini L, Wang Y, Wu P, Shohamy D, Walsh BT, & Steinglass JE (2018). Assessment of test-retest reliability of a food choice task among healthy individuals. Appetite, 123, 352–356. 10.1016/j.appet.2018.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foerde K, Schebendach J, Davis L, Daw N, Walsh BT, Shohamy D, & Steinglass JE (2020). Restrictive eating across a spectrum from healthy to unhealthy—Behavioral and neural mechanisms. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foerde K, Steinglass JE, Shohamy D, & Walsh BT (2015). Neural mechanisms supporting maladaptive food choices in anorexia nervosa. Nature Neuroscience, 18(11), 1571–1573. 10.1038/nn.4136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gendall KA, Sullivan PE, Joyce PR, Carter FA, & Bulik CM (1997). The nutrient intake of women with bulimia nervosa. The International Journal of Eating Disorders, 21(2), 115–127. [DOI] [PubMed] [Google Scholar]
- Gianini L, Foerde K, Walsh BT, Riegel M, Broft A, & Steinglass JE (2019). Negative affect, dietary restriction, and food choice in bulimia nervosa. Eating Behaviors, 33, 49–54. 10.1016/j.eatbeh.2019.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadigan CM, Kissileff HR, & Walsh BT (1989). Patterns of food selection during meals in women with bulimia. The American Journal of Clinical Nutrition, 50(4), 759–766. 10.1093/ajcn/50.4.759 [DOI] [PubMed] [Google Scholar]
- Lavender JM, Goodman EL, Culbert KM, Wonderlich SA, Crosby RD, Engel SG, … Peterson CB (2017). Facets of impulsivity and compulsivity in women with anorexia nervosa. European Eating Disorders Review, 25(4), 309–313. 10.1002/erv.2516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis YD, Gilon Mann T, Enoch-Levy A, Dubnov-Raz G, Gothelf D, Weizman A, & Stein D. (2019). Obsessive–compulsive symptomatology in female adolescent inpatients with restrictive compared with binge–purge eating disorders. European Eating Disorders Review, 27(3), 224–235. 10.1002/erv.2638 [DOI] [PubMed] [Google Scholar]
- Murao E, Sugihara G, Isobe M, Noda T, Kawabata M, Matsukawa N, … Noma S. (2017). Differences in neural responses to reward and punishment processing between anorexia nervosa subtypes: An fMRI study. Psychiatry and Clinical Neurosciences, 71(9), 647–658. 10.1111/pcn.12537 [DOI] [PubMed] [Google Scholar]
- NCEP. (2001). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Final Report. 01–3670, 40. [PubMed] [Google Scholar]
- Peat C, Mitchell JE, Hoek HW, & Wonderlich SA (2009). Validity and utility of subtyping anorexia nervosa. The International Journal of Eating Disorders, 42(7), 590–594. 10.1002/eat.20717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson CB, Pisetsky EM, Swanson SA, Crosby RD, Mitchell JE, Wonderlich SA, … Crow SJ (2016). Examining the utility of narrowing anorexia nervosa subtypes for adults. Comprehensive Psychiatry, 67, 54–58. 10.1016/j.comppsych.2016.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reas DL, & Ro O. (2018). Less symptomatic, but equally impaired: Clinical impairment in restricting versus binge-eating/purging subtype of anorexia nervosa. Eating Behaviors, 28, 32–37. 10.1016/j.eatbeh.2017.12.004 [DOI] [PubMed] [Google Scholar]
- Steinglass J, Foerde K, Kostro K, Shohamy D, & Walsh BT (2015). Restrictive food intake as a choice-A paradigm for study. The International Journal of Eating Disorders, 48(1), 59–66. 10.1002/eat.22345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stunkard AJ, & Messick S. (1985). The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. Journal of Psychosomatic Research, 29(1), 71–83. [DOI] [PubMed] [Google Scholar]
- Sysko R, Glasofer DR, Hildebrandt T, Klimek P, Mitchell JE, Berg KC, … Walsh BT (2015). The eating disorder assessment for DSM-5 (EDA-5): Development and validation of a structured interview for feeding and eating disorders. The International Journal of Eating Disorders, 48(5), 452–463. 10.1002/eat.22388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, McDuffe J, Yanovski S, Merel K, Schvey N, Shomaker L, … Yanovski J. (2009). Laboratory assessment of the food intake of children and adolescents with loss of control eating. The American Journal of Clinical Nutrition, 89, 738–745. 10.3945/ajcn.2008.26886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh BT, Kissileff H, & Hadigan CM (1989). Eating behavior in Bulimia. Annals of the New York Academy of Sciences, 575, 446–454. 10.1111/j.1749-6632.1989.tb53265.x [DOI] [PubMed] [Google Scholar]
- Waxman SE (2009). A systematic review of impulsivity in eating disorders. European Eating Disorders Review, 17(6), 408–425. 10.1002/erv.952 [DOI] [PubMed] [Google Scholar]
- Wolz I, Granero R, & Fernández-Aranda F. (2017). A comprehensive model of food addiction in patients with binge-eating symptomatology: The essential role of negative urgency. Comprehensive Psychiatry, 74, 118–124. 10.1016/j/comppsych.2017.01.012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.