Background:
There is minimal information describing the common characteristics among patients seeking primary/revision rhinoplasty. Success is traditionally interpreted from the surgeon's viewpoint, without considering the patient's perspective. The study's aims were to (1) identify/compare anatomic and functional characteristics commonly found in patients seeking primary and revision rhinoplasties; (2) assess patient satisfaction using a survey; and (3) explore whether graft choice (auricular cartilage versus rib cartilage) affects patient satisfaction and outcome in revision rhinoplasty.
Methods:
A retrospective review of all rhinoplasties by a single surgeon from June 2016 to January 2020 was performed, focusing on preoperative anatomic/functional characteristics and operative interventions performed. A survey was then used to assess patient satisfaction. Finally, survey outcomes were compared between patients who received auricular and rib cartilage grafts in revision rhinoplasty.
Results:
A total of 102 rhinoplasties (53 primary and 49 revisions) were included. Primary rhinoplasties were noted to have more patients with “big” noses (P = 0.015) or humps (P < 0.010). Patients undergoing revision rhinoplasties more commonly exhibited middle vault collapse (P = 0.022). The survey response rate was 60%. Revision rhinoplasty patients had a higher incidence of dissatisfaction with their outcome
Conclusions:
Several features among patients seeking revision rhinoplasties could have been created in the primary operation. The rhinoplasty surgeon should be careful to not introduce new issues or create worse deformities than those seen following the initial operation. Survey-based outcome analysis demonstrated that revision rhinoplasty patients are more likely to have a greater rate of dissatisfaction following their operation.
INTRODUCTION
Rhinoplasty is a challenging operation relying heavily on the intricate, experienced skill of the surgeon to balance the patient’s desired cosmetic nasal improvements while maintaining proper nasal function.1 Unfortunately, some patients undergo rhinoplasty but remain dissatisfied with either their cosmetic appearance and/or nasal function and ultimately seek future surgery to correct persistent or new deformities from their initial operation.
Minimal research exists examining the specific patient characteristics common among patients undergoing primary and revision procedures. Furthermore, although the rhinoplasty literature focuses on operative techniques and strategies to improve cosmetic and functional outcomes from the surgeon’s perspective, little information exists exploring patient-reported satisfaction.2 Such information is especially useful in the context of revision rhinoplasties, in which a patient is willing to invest in a second operation to improve their nasal appearance and function. Further studying and understanding these motivations would aid surgeons in identifying common pitfalls that motivate patients to undergo revision surgeries.3
Specifically with regards to revision rhinoplasty, the source of cartilage for grafting and the effect the cartilage source has on the functional and cosmetic result of revision rhinoplasty is controversial. To our knowledge, no direct comparison of a single surgeon’s longitudinal results has ever been reported with respect to patient-reported cosmetic and functional outcome.
The primary objective of this study is to identify unique preoperative features in the two patient populations undergoing primary and revision rhinoplasties. Second, we utilize a survey to assess patient satisfaction between primary and revision rhinoplasties. Thirdly, we compare patient-reported aesthetic and functional outcomes in revision rhinoplasty comparing the use of ear cartilage to rib cartilage as donor grafting material.
METHODS
Chart Review
After institutional review board approval (Protocol Number: Pro00024510), a retrospective cohort study was conducted including all patients that underwent a rhinoplasty from June 2016 to January 2020 at Houston Methodist Hospital by a single surgeon.
Inclusion Criteria
Female or male patients, 18 years or older, underwent either functional or cosmetic rhinoplasty procedures with the senior author of this study.
Exclusion Criteria
Patients younger than 18 years old or patients for whom information was incomplete or unavailable were excluded.
Demographic Variables
Patients were grouped into two cohorts based on whether they received a primary or revision rhinoplasty. Pertinent demographic information was collected including gender, race, indication for rhinoplasty, and comorbidities.
Preoperative Evaluation Variables
Each patient underwent a standardized, preoperative written evaluation developed by the senior author assessing anatomic, functional, and cosmetic characteristics. Variables in this evaluation included the following: primary versus secondary rhinoplasty, presence of a septal perforation, history of nasal trauma or intranasal drug use, assessment of skin quality, appearance of the dorsum, nasal bones, middle vault, width of nose, tip structure, tip definition, nasofrontal angle, nasal starting point, nasal length, presence of a dorsal hump, nasal tip projection, alar–columellar relationship, columellar characteristics, nasolabial angle, nasal ptosis, presence of a tension tip, characteristics of the septum and mucosa, presence of inferior turbinate hypertrophy, and presence of either internal or external nasal valve collapse. The surgeon’s primary/overall impression of the nasal appearance was also noted (categorized as “big,” “twisted,” “boxy,” “pinched,” “asymmetric,” “long,” “short,” or having a saddle nose deformity). Patients were excluded if any of these variables were missing from the medical record.
Intraoperative Variables
Intraoperative variables were recorded on a standardized form immediately following completion of the surgical procedure and included operative interventions involving the lateral or medial crura, specific tip refinements, dorsal changes, bony pyramid alterations, or use of grafts (including source of grafting material). All other associated procedures performed at the time of the operation (septoplasty, turbinate resection, internal valve repair, and external valve repair) and operative time were included.
Postoperative Complications
Surgical complications were recorded such as hematoma, infection (defined as any clinical evidence of surgical site infection from superficial stitch abscess to major graft loss), and reinterventions (including surgical reinterventions and in-office procedures such as steroid injections or dorsal rasping).
Outcomes Survey
All patients that met the inclusion criteria were sent an email containing a link to the survey (SDC 1). (See figure, Supplemental Digital Content 1, which displays the survey questions, http://links.lww.com/PRSGO/B770.) The designated target for analysis was a 60% response rate, which was achieved after 16 days from the start of the survey period. Participants were asked to assess their functional and cosmetic satisfaction with their rhinoplasties using a Likert scale.
Subgroup Analysis: Graft Outcomes
Additionally, the difference in satisfaction between the use of rib and auricular cartilage with regards to clinical and patient-reported outcomes was evaluated. In this analysis, only patients who exclusively received either rib or auricular cartilage were included.
Statistical Analysis
Mean and SD were used to describe continuous, normally distributed data. Median and interquartile range (IQR) were used to describe nonnormally distributed data. Independent Student’s t test was used to compare normally distributed continuous variables, whereas Mann–Whitney tests were used to compare nonnormally distributed variables. Chi-square and Fisher’s exact tests were used to compare categorical variables between groups. Finally, binary logistic regression analyses were conducted to control for confounders when defining the preoperative characteristics for primary and revision rhinoplasty procedures. Significance was defined at a P value less than 0.05. All statistical analyses were performed using IBM SPSS software (IBM SPSS Statistics for Windows, Version 25.0; IBM Corp, Armonk, N.Y.).
RESULTS
During the study period, a total of 102 rhinoplasty operations were included with complete data available for analysis. Primary rhinoplasties accounted for 52% of cases (53) and revision rhinoplasties accounted for 48% (49 cases).
Demographic Evaluation
The median age of patients that underwent primary and revision rhinoplasty was 37.9 and 50.2 years, respectively (P < 0.001). Women were significantly more likely to undergo a revision rhinoplasty compared to men (P = 0.002). No significant differences were noted with regards to race, comorbidity, or history of nasal trauma (all P > 0.05) (Table 1).
Table 1.
Demographic Information
| Variable | Rhinoplasty Procedures | P | ||
|---|---|---|---|---|
| Primary (n = 53) (%) | Revision (n = 49) (%) | |||
| Median age, y [range] | 37.9 [18–78] | 50.2 [22–70] | 0.0001* | |
| Gender | 0.002* | |||
| Male | 28 (52.8) | 11 (22.4) | ||
| Female | 25 (47.2) | 38 (77.6) | ||
| Race | 0.150 | |||
| Asian | 1 (1.9) | 0 (0.0) | ||
| African American | 0 (0.0) | 2 (4.1) | ||
| Middle Eastern | 4 (7.5) | 3 (6.1) | ||
| White/Caucasian | 46 (86.8) | 37 (75.5) | ||
| Hispanic | 2 (3.8) | 7 (14.3) | ||
| Indication | 0.052 | |||
| Cosmetic | 13 (24.5) | 9 (18.4) | ||
| Functional | 20 (37.7) | 10 (20.4) | ||
| Both | 20 (37.7) | 30 (61.2) | ||
| Comorbidities | Smoking | 3 (5.7) | 4 (8.2) | 0.782 |
| Hypertension | 9 (17.0) | 8 (16.3) | 0.929 | |
| Diabetes | 6 (11.3) | 2 (4.1) | 0.162 | |
| COPD | 0 (0.0) | 0 (0.0) | — | |
| CAD | 1 (1.9) | 0 (0.0) | 0.522 | |
| Coagulopathy | 2 (3.8) | 3 (6.1) | 0.463 | |
| Previous nasal surgeries | 9 (17.0) | 38 (77.6) | 0.0001* | |
| Previous nasal trauma | 7 (13.2) | 14 (28.6) | 0.053 | |
*Significant P value.
CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease.
Preoperative Evaluation
Primary Impression
Having a “big” nose was more prevalent in patients undergoing a primary rhinoplasty (P = 0.015, OR 7.8, 95% confidence interval [CI]: 1.50–41.076), whereas patients who received a revision rhinoplasty were significantly more likely to have asymmetry (P = 0.041, OR 4.36, 95% CI: 1.06–17.96). Features such as a twisted dorsum, boxy or pinched tip appearance, or differences in skin quality were not significantly different between groups (Table 2).
Table 2.
Primary Impression
| Variable | Rhinoplasty Procedures | P * | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|---|
| Primary (n = 53) (%) | Revision (n = 49) (%) | Odds Ratio | 95% Confidence Interval | P | |||
| Primary impression | Big | 14 (26.4) | 3 (6.1) | 0.006† | 7.86 | 1.50–41.07 | 0.015† |
| Twisted | 9 (17.0) | 9 (18.4) | 1.000 | 0.98 | 0.26–3.72 | 0.985 | |
| Boxy | 11 (20.8) | 7 (14.3) | 0.392 | 0.46 | 0.12–1.75 | 0.256 | |
| Pinched | 14 (26.4) | 17 (34.7) | 0.364 | 0.90 | 0.27–2.95 | 0.872 | |
| Asymmetric | 6 (11.3) | 14 (28.6) | 0.028† | 4.36 | 1.06–17.96 | 0.041† | |
| Long | 6 (11.3) | 6 (12.2) | 0.885 | 0.85 | 0.18–4.02 | 0.844 | |
| Short | 2 (3.8) | 4 (8.2) | 0.424 | 1.13 | 0.09–13.28 | 0.921 | |
| Saddle | 2 (3.8) | 10 (20.4) | 0.009† | 5.99 | 0.89–40.28 | 0.066 | |
| Skin quality | Thin | 13 (24.5) | 20 (40.8) | 0.079 | 1.34 | 0.36–4.96 | 0.653 |
| Medium | 14 (26.4) | 8 (16.3) | 0.216 | 0.76 | 0.21–2.65 | 0.664 | |
| Thick | 15 (28.3) | 13 (26.5) | 0.841 | 1.38 | 0.38–4.96 | 0.618 | |
| Sebaceous | 2 (3.8) | 0 (0.0) | 0.496 | 0.00 | — | 0.999 | |
*Chi-square or Fischer’s exact test used.
†Significant P value.
Frontal View Assessment
Middle vault collapse was more prevalent in the revision rhinoplasty group (P = 0.022, OR 8.86, 95% CI: 1.37–57.08). However, the surgeon’s analysis of nasal width, tip characteristics, nasofrontal angle, and nasal starting point were all not significantly different between primary and revision rhinoplasties (Table 3).
Table 3.
Frontal View Assessment
| Variable | Rhinoplasty Procedures | P * | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|---|
| Primary (n = 53) (%) |
Revision (n = 49) (%) |
Odds Ratio |
95% Confidence Interval |
P | |||
| Dorsum frontal view | Straight | 21 (39.6) | 24 (49.0) | 0.342 | 2.15 | 0.37–12.37 | 0.389 |
| Deviated | 19 (35.8) | 14 (28.6) | 0.432 | 1.53 | 0.22–10.64 | 0.667 | |
| Twisted | 6 (11.3) | 5 (10.2) | 0.856 | 1.11 | 0.17–7.01 | 0.912 | |
| Concave | 23 (43.4) | 22 (44.9) | 0.879 | 1.35 | 0.379–4.82 | 0.641 | |
| Nasal bones frontal view | Short | 10 (18.9) | 14 (28.6) | 0.248 | 0.34 | 0.022–5.44 | 0.453 |
| Normal | 27 (50.9) | 23 (46.9) | 0.686 | 0.22 | 0.01–3.80 | 0.299 | |
| Long | 5 (9.4) | 1 (2.0) | 0.207 | 0.10 | 0.00–3.78 | 0.216 | |
| Middle vault frontal view | Narrow | 36 (67.9) | 33 (67.9) | 0.956 | 1.47 | 0.17–12.35 | 0.718 |
| Normal | 5 (9.4) | 1 (2.0) | 0.207 | 0.13 | 0.00–2.47 | 0.175 | |
| Collapse | 2 (3.8) | 11 (22.4) | 0.005† | 8.86 | 1.37–57.08 | 0.022† | |
| Sublux | 17 (32.1) | 15 (30.6) | 0.874 | 1.40 | 0.36–5.48 | 0.625 | |
| Asymmetrical | 7 (6.9) | 9 (8.8) | 0.474 | 1.06 | 0.22–5.01 | 0.936 | |
| Width frontal view | Narrow | 21 (39.6) | 13 (26.5) | 0.161 | 3.43 | 0.06–1.79 | 0.205 |
| Normal | 4 (7.5) | 6 (12.2) | 0.515 | 3.25 | 0.31–33.42 | 0.321 | |
| Wide | 11 (20.8) | 12 (24.5) | 0.652 | 0.80 | 0.17–3.75 | 0.787 | |
| Tip frontal view | Deviated | 13 (24.5) | 8 (16.3) | 0.306 | 1.01 | 0.244–4.24 | 0.980 |
| Pinched | 13 (24.5) | 16 (32.7) | 0.363 | 2.57 | 0.52–12.75 | 0.246 | |
| Asymmetrical | 10 (18.8) | 9 (18.3) | 0.948 | 0.92 | 0.20–4.15 | 0.916 | |
| Amorphous | 6 (11.3) | 11 (22.4) | 0.132 | 3.51 | 0.75–16.39 | 0.109 | |
| Bulbous | 17 (32.1) | 11 (22.4) | 0.276 | 0.60 | 0.14–2.45 | 0.482 | |
*Chi-square or Fischer’s exact test used.
†Significant P value.
Lateral View Assessment
The presence of a hump (P = 0.0001) on the lateral view was significantly more common in primary rhinoplasty patients (P = 0.010, OR 0.13, 95% CI: 0.03–0.62). Other features such as abnormal nasal projection, acute or obtuse nasolabial angle, and nasal ptosis were not significantly different between groups (Table 4).
Table 4.
Lateral View Assessment
| Variable | Rhinoplasty Procedures | P * | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|---|
| Primary (n = 53) (%) | Revision (n = 49) (%) | Odds Ratio | 95% Confidence Interval | P | |||
| NF angle lateral view | Shallow | 7 (13.2) | 3 (6.1) | 0.323 | — | — | — |
| Deep | 14 (26.4) | 18 (36.7) | 0.262 | — | — | — | |
| Normal | 21 (39.6) | 20 (40.8) | 0.902 | — | — | — | |
| St. Pt lateral view | High | 5 (9.4) | 4 (8.2) | 1.000 | — | — | — |
| Low | 17 (32.1) | 18 (36.7) | 0.620 | — | — | — | |
| Normal | 21 (39.6) | 20 (40.8) | 0.902 | — | — | — | |
| Length lateral view | Normal | 10 (18.9) | 7 (14.3) | 0.535 | 1.16 | 0.24–5.51 | 0.846 |
| Short | 6 (11.3) | 16 (32.7) | 0.009† | 1.65 | 0.22–12.3 | 0.622 | |
| Hump lateral view | Yes | 38 (71.7) | 17 (34.7) | <0.0001† | 0.13 | 0.03–0.62 | 0.010† |
| Projection lateral view | Normal | 5 (9.4) | 5 (10.2) | 1.000 | 0.78 | 0.00–179.94 | 0.931 |
| Over | 20 (37.7) | 11 (22.4) | 0.094 | 0.38 | 0.00–106.98 | 0.742 | |
| Under | 18 (34.0) | 25 (51.0) | 0.081 | 0.49 | 0.00–109.82 | 0.799 | |
| Alar/Col | Normal | 19 (35.8) | 9 (18.4) | 0.048 | 0.72 | 0.06–8.09 | 0.793 |
| Retraction | 7 (13.2) | 16 (32.7) | 0.019† | 8.02 | 0.77–82.90 | 0.080 | |
| Hanging | 14 (26.4) | 16 (32.7) | 0.498 | 4.18 | 0.42–41.58 | 0.222 | |
| Columella | Normal | 11 (20.8) | 8 (16.3) | 0.566 | 0.18 | 0.01–2.34 | 0.194 |
| Hanging | 27 (50.9) | 21 (42.9) | 0.414 | 0.07 | 0.00–0.90 | 0.041 | |
| Retracted | 3 (5.7) | 11 (22.4) | 0.014† | 0.17 | 0.00–3.54 | 0.255 | |
| NL angle | Acute | 30 (56.6) | 24 (49.0) | 0.441 | 1.88 | 0.17–19.99 | 0.598 |
| Obtuse | 7 (13.2) | 12 (24.5) | 0.144 | 3.04 | 0.29–31.73 | 0.353 | |
| Nasal ptosis | Yes | 33 (62.3) | 24 (49.0) | 0.177 | 0.86 | 0.18–4.13 | 0.852 |
| Tension tip | Yes | 20 (37.7) | 9 (18.4) | 0.030† | 0.35 | 0.07–1.74 | 0.203 |
Alar/Col, Alar–Columella relationship; NF, nasofrontal angle; NL, nasolabial; St. Pt, starting point.
*Chi-square or Fischer’s exact test used.
†Significant P value.
Base View Assessment
The presence of septal abnormalities such as deviation (P = 0.012, OR 0.07, 95% CI: 0.00–0.56) or spur (P = 0.021, OR 0.16, 95% CI: 0.03–0.76) was significantly associated with the primary rhinoplasty group more commonly compared to revision patients (Table 5).
Table 5.
Base View Assessment and Functional Aspects of the Nose
| Variable | Rhinoplasty Procedures | P * | Odds Ratio | 95% Confidence Interval | P | ||
|---|---|---|---|---|---|---|---|
| Primary [n = 53] (%) | Revision [n = 49] (%) | ||||||
| Septum base view | Deviation | 29 (54.7) | 8 (16.3) | <0.0001† | 0.07 | 0.00–0.56 | 0.012† |
| Spur | 23 (43.4) | 6 (12.2) | <0.0001† | 0.16 | 0.03–0.76 | 0.021† | |
| Caudal deviation base view | Yes | 23 (43.4) | 10 (20.4) | 0.013† | 1.38 | 0.25–7.42 | 0.706 |
| Mucosa | Normal | 21 (39.6) | 34 (69.4) | 0.003† | 3.16 | 0.39–25.22 | 0.276 |
| Edema | 20 (37.7) | 5 (10.2) | 0.001† | 0.11 | 0.00–1.70 | 0.115 | |
| Polyps | 1 (1.9) | 0 (0.0) | 0.334 | — | — | — | |
| Inferior turbinate hypertrophy | Yes | 39 (73.6) | 33 (67.3) | 0.490 | 1.87 | 0.32–10.94 | 0.484 |
| Perforation | Yes | 1 (1.9) | 7 (14.3) | 0.027† | 39.1 | 0.38–4030.6 | 0.121 |
| Nasal valve—internal | Normal | 4 (7.5) | 1 (2.0) | 0.364 | 0.67 | 0.01–46.43 | 0.855 |
| Collapse | 39 (73.6) | 40 (81.6) | 0.331 | 3.85 | 0.38–37.93 | 0.252 | |
| Nasal valve—external | Normal | 11 (20.8) | 2 (4.1) | 0.012† | 0.03 | 0.00–0.367 | 0.005† |
| Collapse | 15 (28.3) | 26 (53.1) | 0.011† | 1.17 | 0.26–5.17 | 0.834 | |
*Chi-square or Fischer’s exact test used.
†Significant P value.
Functional Aspects of the Nose
Although internal nasal valve collapse was a frequently found complaint among both primary and revision populations, the rates were not significantly different between primary and revision populations. However, external nasal valve was more likely to be normal in primary rhinoplasty patients (P = 0.005, OR 0.03, 95% CI 0.00–0.367) (Table 5).
Intraoperative Variables
An open approach was utilized for all the procedures included in the study. Mean operative time was higher for revision rhinoplasty procedures (3.1 h) when compared to primary procedures (2.7 h) (P = 0.021).
Tip Approach
The use of a columellar strut (caudal septal extension graft or free floating medial crural strut) in tip refinement was utilized more frequently in revision rhinoplasties (P = 0.005), whereas a columellar tongue-in-groove stitch was often utilized in primary rhinoplasty (P = 0.013). Additionally, resection of the caudal septum was more likely to be performed in the primary rhinoplasty group (P = 0.012), whereas revision rhinoplasties often required nasal lengthening via a caudal septal extension graft, extended middle vault spreader graft, floating medial crural strut graft or a combination of these maneuvers (P = 0.006) (Table 6).
Table 6.
Surgical Tip Approach
| Variable | Rhinoplasty Procedures | P | ||
|---|---|---|---|---|
| Primary (n = 53) (%) | Revision (n = 49) (%) | |||
| Tip refinements | Columellar strut | 22 (41.5) | 34 (69.4) | 0.005* |
| Columellar TIG | 7 (13.2) | 0 (0.0) | 0.013* | |
| Columellar suture MCF | 34 (64.2) | 26 (53.1) | 0.256 | |
| Suture max crest | 17 (32.1) | 12 (24.5) | 0.396 | |
| Tip graft | 2 (3.8) | 7 (14.3) | 0.084 | |
| Alar spreader graft | 0 (0.0) | 0 (0.0) | — | |
| Resected caudal septum | 11 (20.8) | 2 (4.1) | 0.012* | |
| Alar base resection | 0 (0.0) | 0 (0.0) | — | |
| Tip effect | Increased tip projection | 24 (45.3) | 29 (59.2) | 0.160 |
| Decreased tip projection | 27 (50.9) | 16 (32.7) | 0.062 | |
| Increased tip rotation | 37 (69.8) | 28 (57.1) | 0.184 | |
| Lengthened nose | 13 (24.5) | 25 (51.0) | 0.006* | |
| Altered col–alar relationship | 16 (30.2) | 19 (38.8) | 0.361 | |
| Altered col-labial angle | 39 (73.6) | 33 (67.3) | 0.490 | |
*Significant P value.
MCF, medial crural footplate; TIG, tongue in groove.
Dorsum Approach
Patients who underwent primary rhinoplasties more often required dorsal reduction (P = 0.003), whereas dorsal augmentation was required in revision rhinoplasties (P = 0.001). Furthermore, the use of medial (P = 0.001) and lateral (P < 0.0001) osteotomies were more frequently required when addressing the bony pyramid in primary rhinoplasties (Table 7).
Table 7.
Dorsum Approach and Grafts Utilized
| Variable | Rhinoplasty Procedures | P | ||
|---|---|---|---|---|
| Primary (n = 53) (%) | Revision (n = 49) (%) | |||
| Dorsum | Reduction | 34 (64.2) | 17 (34.7) | 0.003* |
| Augmentation | 7 (13.2) | 21 (42.9) | 0.001* | |
| Augmented NF angle | 4 (7.5) | 6 (12.2) | 0.515 | |
| Depended NF angle | 4 (7.5) | 3 (6.1) | 1.000 | |
| Widened | 23 (43.4) | 13 (26.5) | 0.075 | |
| Spreader grafts | 48 (90.6) | 39 (79.6) | 0.118 | |
| Grafts | 4 (7.5) | 5 (10.2) | 0.735 | |
| Bony pyramid | Medial-oblique osteotomies | 29 (54.7) | 11 (22.4) | 0.001* |
| Lateral osteotomies | 35 (66.0) | 15 (30.6) | <0.0001* | |
| Greenstick osteotomy | 6 (11.3) | 6 (12.2) | 0.885 | |
| Percutaneous osteotomy | 3 (5.7) | 2 (4.1) | 1.000 | |
| Graft-autogenous | Septal | 45 (84.9) | 7 (14.3) | <0.0001* |
| Rib | 5 (9.4) | 21 (42.9) | <0.0001* | |
| Auricular | 11 (20.8) | 33 (67.3) | <0.0001* | |
| Fascia | 5 (9.4) | 17 (34.7) | 0.002* | |
| Associated procedures | NSR | 30 (56.6) | 6 (12.2) | <0.0001* |
| Turbinate resection | 29 (54.7) | 7 (14.3) | <0.0001* | |
| Internal valve repair | 24 (45.3) | 25 (51.0) | 0.562 | |
| External valve repair | 7 (13.2) | 14 (28.6) | 0.055 | |
*Significant P value.
NF, nasofrontal; NSR, nasal septal reconstruction.
Grafts
In primary rhinoplasties, septal cartilage was usually the chosen graft (P < 0.0001). However, in revision procedures, rib (P < 0.0001) or auricular grafts were the favored grafting material (P < 0.0001) (Table 7).
Postoperative Complications
There was no significant difference in the rates of postoperative hematoma formation, infection and reinterventions in both primary/revision rhinoplasty groups (all P > 0.05). The functional and cosmetic satisfaction noted by patients in their first office visit was high in both groups, not significantly different between primary and revision rhinoplasty patients (P = 0.156 and P = 0.066, respectively) (Table 8).
Table 8.
Clinical Postoperative Complications
| Variable | Rhinoplasty | P | |
|---|---|---|---|
| Primary (n = 53) (%) | Revision (n = 49) (%) | ||
| Hematoma | 0 (0.0) | 1 (2.0) | 0.480 |
| Infection | 6 (12.2) | 2 (3.8) | 0.149 |
| Qualitative functional improvement—first postoperative visit | 53 (100.0) | 47 (95.9) | 0.332 |
| Qualitative aesthetic improvement—1-mo postoperative visit | 51 (96.2) | 42 (85.7) | 0.156 |
| Reintervention* | 9 (17.0) | 16 (32.7) | 0.066 |
*Reintervention includes both surgical reinterventions and in-office procedures such as steroid injections or dorsal rasping.
Patient-reported Outcomes: Survey Results
Sixty-one patients completed all parts of the survey (response rate 60%). Of these patients, 34 (55.7%) underwent primary rhinoplasties and 27 (44.3%) underwent revision procedures.
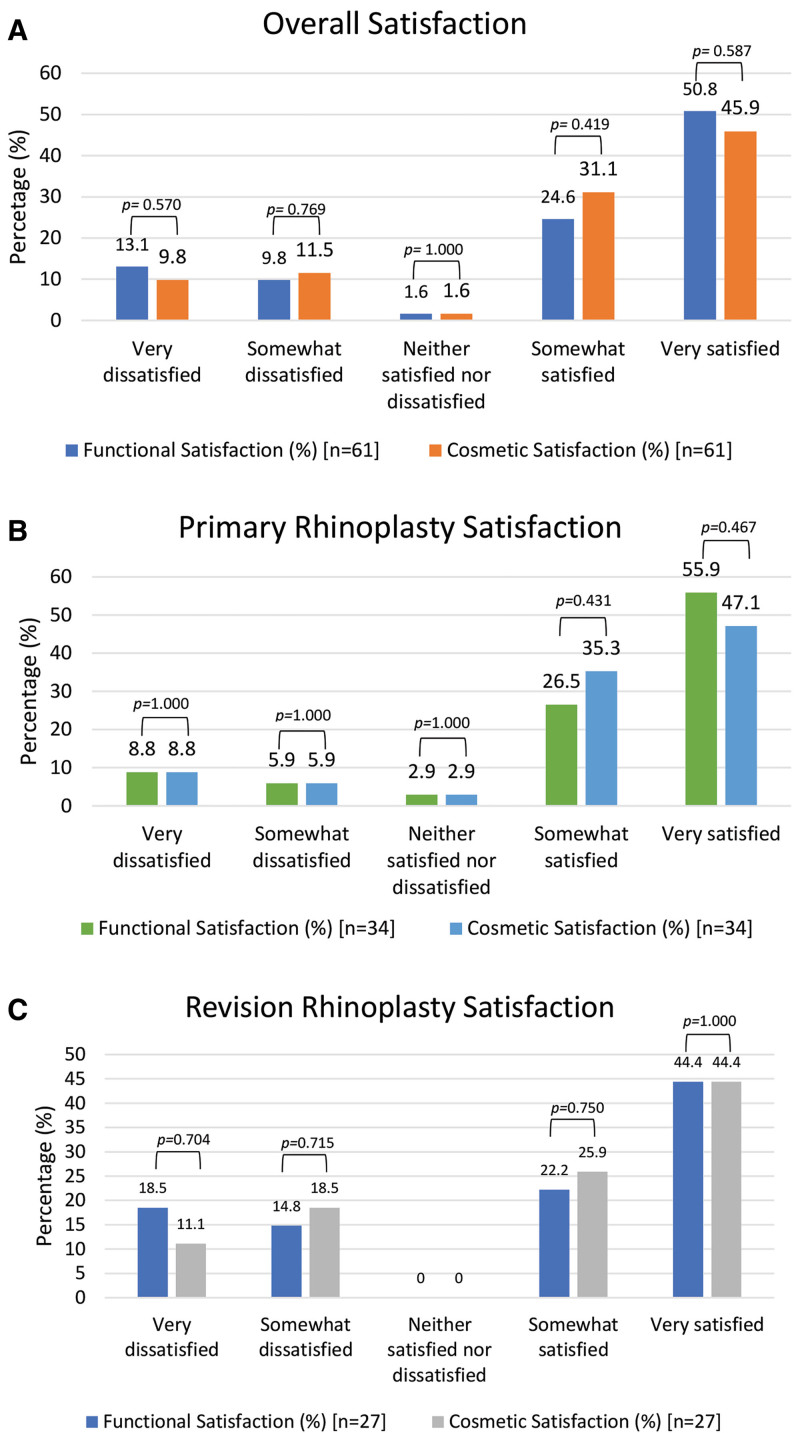
Regarding patient satisfaction, the vast majority of patients in the study were satisfied with their procedure. Overall, patients were similarly satisfied from a functional and cosmetic perspective (all P > 0.05) (Fig. 1A). Patient satisfaction with primary and revision rhinoplasties was then compared. Generally, revision rhinoplasty patients appeared to have higher rates of dissatisfaction and lower rates of satisfaction compared to primary populations (Fig. 1B and C).
Fig. 1.
Patient satisfaction. A, Overall patient satisfaction. B, Patient satisfaction in primary rhinoplasty. C, Patient satisfaction in revision rhinoplasty.
Subgroup Analysis: Graft Outcomes
Only revision rhinoplasty patients were included in this analysis given primary rhinoplasty patients usually received a septal cartilage graft, whereas the graft choices in revision procedures were more varied. A total of 34 patients were included in this subgroup analysis, of which 20 patients (58.8%) received auricular cartilage, and 14 patients (41.2%) received rib cartilage.
When analyzing postoperative complications in the nose, zero cases of hematoma were noted in both cohorts, whereas there were four cases of infection in the rib cartilage group and one in the auricular cartilage group (all P > 0.05). All patients in both groups reported functional improvement 1-month postsurgery in their clinical visit (P = 1.000). Furthermore, 85% of patients in the rib cartilage group and 80% of patients in the auricular cartilage groups reported aesthetic improvement in their first clinical visit (P = 0.842) (SDC 2). (See table, Supplemental Digital Content 2, which displays the rib versus auricular cartilage clinical postoperative complications, http://links.lww.com/PRSGO/B771.) Donor site morbidity was very limited, with only one patient who underwent an auricular graft complaining of ecchymosis at the donor site (which resolved at later postoperative visits).
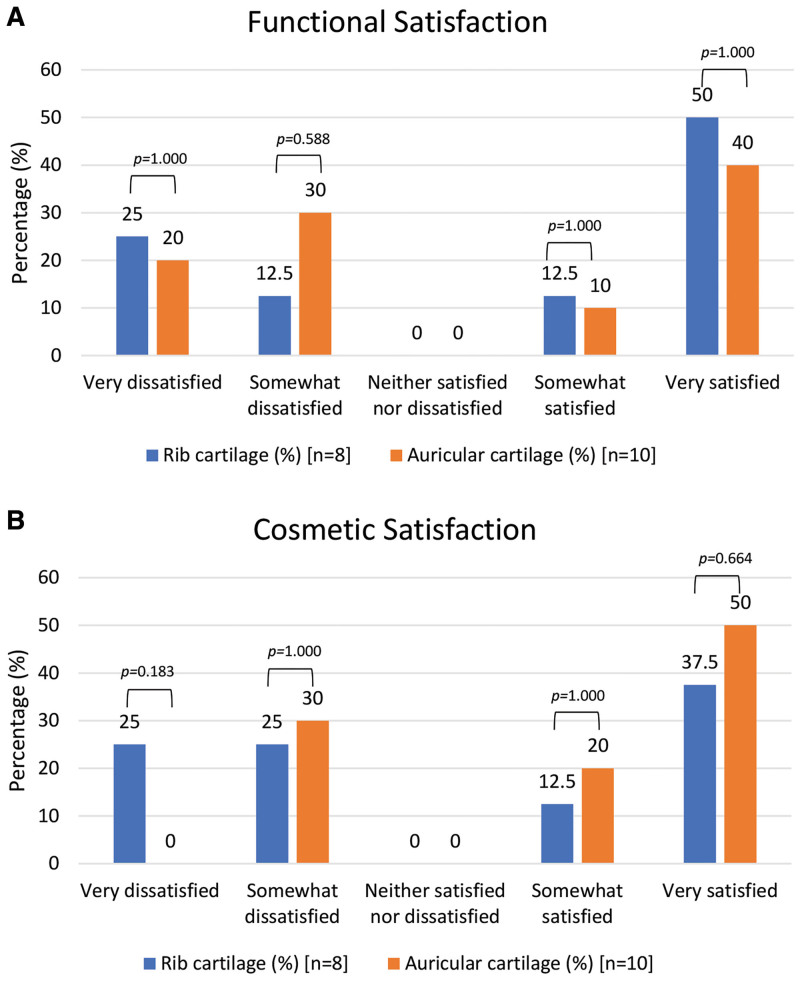
Of the 34 patients included in the subgroup analysis, 18 responded to the survey (a response rate of 53%). With regards to functional and cosmetic satisfaction, the majority of patients were very satisfied with their outcomes in both groups, and no significant differences were noted between cohorts (all P > 0.05) (Fig. 2).
Fig. 2.
Functional and cosmetic satisfaction. A, Functional satisfaction rib versus auricular cartilage. B, Cosmetic satisfaction rib versus auricular cartilage.
DISCUSSION
Characteristics of Primary versus Revision Rhinoplasties
Rhinoplasty is a technically challenging operation. Achieving a satisfactory outcome requires that the surgeon work together with the patient to identify features of the nose that can be altered to provide the desired cosmetic appearance while maintaining appropriate functional characteristics. However, despite extensive surgical planning, some patients are dissatisfied with their outcome, and up to 20% of patients seek a revision rhinoplasty.4 Previous studies have focused on intraoperative variables and surgical techniques to improve functional and cosmetic outcomes in an effort to reduce revision rates.5–8 However, there is a scarcity of literature comparing specific preoperative characteristics among patients undergoing primary and revision procedures. This is valuable information that would help individual surgeons develop adequate preoperative planning, recognize correctable deficits, and refine operative steps to decrease revision procedure rates and increase patient satisfaction.
Dissatisfaction with rhinoplasty has previously been noted to stem from either introduction of a new deformity or failure to correct a preexisting one.9 In the current study, patients sought revision rhinoplasties most commonly for cosmetic features such as dorsal asymmetry or middle vault collapse—deformities that could have been created as a result of over resection of nasal cartilage or bony structure during the primary operation (SDC 3). (See figure, Supplemental Digital Content 3, which displays the lateral, base, and frontal views of two revision rhinoplasty patients, a 48-year-old woman (A–F) and 34-year-old woman (G–L), each with previous overresection, before (A, C, E, G, I, K) and after (B, D, F, H, J, L) dorsal augmentation and correction of nasal valve collapse. Costal cartilage was used in both cases for dorsal onlay and extended middle vault spreader grafts. Patient 1 (48-year-old woman, A–F) also required additional alar batten grafts and a double layer of temporoparietal fascia on the dorsum due to loss of proper lower lateral cartilage convexity and thin skin, respectively. Both patients reported cosmetic and functional improvement, http://links.lww.com/PRSGO/B772.)
Patients were also more likely to require some form of nasal lengthening during revision surgery, which could be due to over resection of the septum and failure to recognize the need for septal extension during the primary procedure. Other reviews evaluating common reasons for revision rhinoplasty have shown similar findings, pointing to the difficulty in determining the appropriate amount of cartilage to resect from the nose to achieve the proper cosmetic and functional result.4,10,11
The lead author’s approach to preventing revision surgery in his own patients is based on an extensive preoperative planning process that includes in depth documentation of all physical characteristics outlined in Tables 2–8. Furthermore, the surgeon spends a significant amount of time with the patient to come up with shared goals for the surgery. Intraoperatively, the primary surgeon performs every procedure in the same order, proceeding from dorsal or septal work to osteotomies to aesthetic adjustments like grafting or tip work. This way, the maximum foundational support is preserved while still achieving the desired cosmetic result and minimizing the risk for over resection, which often necessitates future revisions.
Furthermore, in the current study, women were noted to undergo revision rhinoplasties more frequently than men. The reason for this difference is unclear. Previously, it has been noted that female rhinoplasty patients are more likely to be able to articulate the exact reasons for their dissatisfaction with the procedure.12 This may have been the reason why female patients in the current cohort were more likely to undergo revision rhinoplasties. Being able to appropriately state why they were dissatisfied with the procedure may have motivated female patients to seek out a revision surgery.
Knowing the features that are most likely to result in a patient seeking a revision rhinoplasty is valuable in the preoperative planning process. Understanding these aspects allows the surgeon to develop a standardized and comprehensive approach to preoperative analysis to determine the functional and aesthetic needs of the individual patient. In revision rhinoplasties, an ideal cosmetic appearance is far more difficult to achieve, given scar tissue formation and unpredictable healing.13 Furthermore, overresection of the structural support of the nose in rhinoplasty can lead to destabilization of the nasal architecture and of the loss of functional characteristics of the nose.
As we noted in our study, these issues can be challenging to manage, and often require the use of grafts from areas other than the nose to create appropriate support. Therefore, it is imperative that the rhinoplasty surgeon cautiously approaches the primary procedure, taking care to avoid creating features that are most often associated with a revision surgery.
A Survey-based Approach to Assessing Patient Satisfaction
The success of a rhinoplasty is determined in large part by the patient’s satisfaction with the procedure. Generally, patient satisfaction with rhinoplasty is evaluated in a clinical setting with an in-person encounter with the surgeon. Such an environment might make patients uncomfortable with expressing their dissatisfaction or disappointment with the outcome. In the present study, we assessed patient satisfaction with an online survey, hypothesizing that patients may be more willing to express dissatisfaction outside of the clinical setting face to face with their surgeon. One of the key findings of the current study is that the satisfaction rates documented by the surgeon in the medical record were higher than the satisfaction rates reported in the survey. Therefore, assessing satisfaction in a conventional clinical setting may fail to identify patients that are otherwise dissatisfied with their outcome. Surgeons may consider utilizing similar strategies to identify patients in their practice that may ultimately be dissatisfied with their clinical outcomes but are reluctant to voice their concerns in an in-person setting.
Auricular versus Autologous Rib Cartilage Grafting and Impact on Patient Satisfaction
Revision rhinoplasties often require the use of alternative sources of cartilage to reconstruct the nose.14,15 Although septal cartilage is prioritized as a primary cartilage source, there is limited consensus on the optimal choice for cartilage if septal cartilage is unavailable.16 Previously, surgeons have pointed to the intrinsic curvature, elasticity, and thickness of auricular cartilage as a limiting factor in its utility. Similarly, rib cartilage has been criticized for its reported donor site pain, scar from harvest and greater potential risk to the patient in graft harvest. However, neither of these observations have been rigorously evaluated in the literature.17 After analyzing a small subgroup of patients that underwent revision rhinoplasty, we did not find significant differences in postoperative clinical complications or functional/cosmetic satisfaction between patients who received rib or auricular cartilage.
Given the response rates to our survey, the sample size limits our ability to conclusively state that rib and auricular cartilage perform similarly in revision rhinoplasty. Future study is required to further investigate the impact that the type of graft utilized has on patient satisfaction. In choosing which cartilage donor site to use in revision rhinoplasty, the senior author takes into account the following parameters: (1) the volume and length of cartilage needed; (2) the need for the recipient site to be straight or curved; (3) the strength, rigidity, and length of the cartilage needed; and (4) the risk and potential effect of long term warping. Ultimately, in the individual patient, the need for longer length of cartilage, straighter cartilage, larger volume, greater rigidity, and support favor choosing rib cartilage over ear cartilage as the appropriate donor cartilage in revision rhinoplasty. This approach and framework was utilized in the current study in the choice of graft for each patient. Our results suggest that when adopting this framework, patient satisfaction is similar between the use of rib or auricular cartilage. Future study should attempt to further compare satisfaction rates between rib and auricular cartilage, focusing on controlling for various factors such as indication or graft size.
Furthermore, the current study focused on autologous rib grafts. It should be noted that other options exist for grafting rib cartilage, including cadaveric rib or MTF biologic alternatives. Generally, the lead author prefers to use autologous rib compared to these alternative sources unless the patient specifically seeks to avoid the extra incision associated with the autologous rib graft. Future study could seek to compare patient satisfaction and outcomes between these graft choices as well.
Study Limitations
This study is not without limitations. A retrospective analysis is always at risk of under or overestimation of the results, and the existence of possible confounding variables. One important limitation of our subgroup analysis is that although the initial patient cohorts included a significant number of participants (102 patients included), when performing our subgroup graft analysis our patient population decreased significantly due to response rates, decreasing the power of our study and therefore its potential reproducibility. Furthermore, the current study could have failed to identify important characteristics/trends in the patients that chose to not respond to the survey.
CONCLUSIONS
Patients that undergo revision rhinoplasties often do so for features that may have been introduced in the primary operation. The rhinoplasty surgeon should be cautious to not introduce these deformities when performing the primary procedure to reduce rates of reintervention. Furthermore, although both primary and revision rhinoplasty patients appear to have improved functional and cosmetic satisfaction as a result of their procedures, the rate of dissatisfaction is higher in patients who received a revision surgery.
ACKNOWLEDGMENT
This study had institutional review board approval and was conducted following the principles outlined by the Declaration of Helsinki.
Supplementary Material
Footnotes
Published online 13 September 2021.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Loyo M, Wang TD. Revision rhinoplasty. Clin Plast Surg. 2016;43:177–185. [DOI] [PubMed] [Google Scholar]
- 2.Hellings PW, Nolst Trenité GJ. Long-term patient satisfaction after revision rhinoplasty. Laryngoscope. 2007;117:985–989. [DOI] [PubMed] [Google Scholar]
- 3.Neaman KC, Boettcher AK, Do VH, et al. Cosmetic rhinoplasty: revision rates revisited. Aesthet Surg J. 2013;33:31–37. [DOI] [PubMed] [Google Scholar]
- 4.East C, Kwame I, Hannan SA. Revision rhinoplasty: what can we learn from error patterns? An analysis of revision surgery. Facial Plast Surg. 2016;32:409–415. [DOI] [PubMed] [Google Scholar]
- 5.Fagundes MS, Moreira AT, Tambara EM, et al. Objective assessment of surgical technique in rotation and nasal projection variation. Braz J Otorhinolaryngol. 2016;82:47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee LN, Boahene KD. A novel technique for sculpting costal cartilage in microtia repair and rhinoplasty. JAMA Facial Plast Surg. 2013;15:349–351. [DOI] [PubMed] [Google Scholar]
- 7.Atighechi S, Dadgarnia M, Vaziribozorg S, et al. The effect of lateral crural overlay surgical technique on elasticity of nasal ala. Eur Arch Otorhinolaryngol. 2018;275:1235–1237. [DOI] [PubMed] [Google Scholar]
- 8.Atolini N, Jr, Lunelli V, Lang GP, et al. Septum pyramidal adjustment and repositioning - a conservative and effective rhinoplasty technique. Braz J Otorhinolaryngol. 2019;85:176–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Constantian MB. What motivates secondary rhinoplasty? A study of 150 consecutive patients. Plast Reconstr Surg. 2012;130:667–678. [DOI] [PubMed] [Google Scholar]
- 10.Chauhan N, Alexander AJ, Sepehr A, et al. Patient complaints with primary versus revision rhinoplasty: analysis and practice implications. Aesthet Surg J. 2011;31:775–780. [DOI] [PubMed] [Google Scholar]
- 11.Bagheri SC, Khan HA, Jahangirnia A, et al. An analysis of 101 primary cosmetic rhinoplasties. J Oral Maxillofac Surg. 2012;70:902–909. [DOI] [PubMed] [Google Scholar]
- 12.Khansa I, Khansa L, Pearson GD. Patient satisfaction after rhinoplasty: a social media analysis. Aesthet Surg J. 2016;36:NP1–NP5. [DOI] [PubMed] [Google Scholar]
- 13.Kamer FM, McQuown SA. Revision rhinoplasty: analysis and treatment. Arch Otolaryngol Neck Surg. 1988;114:257–266. [DOI] [PubMed] [Google Scholar]
- 14.Lee LN, Quatela O, Bhattacharyya N. The epidemiology of autologous tissue grafting in primary and revision rhinoplasty. Laryngoscope. 2019;129:1549–1553. [DOI] [PubMed] [Google Scholar]
- 15.Spataro E, Piccirillo JF, Kallogjeri D, Branham GH, et al. Revision rates and risk factors of 175 842 patients undergoing septorhinoplasty. JAMA Facial Plast Surg. 2016;18:212–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abbas OL. Revision rhinoplasty: measurement of patient-reported outcomes and analysis of predictive factors. Springerplus. 2016;5:1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ho TT, Sykes K, Kriet JD, et al. Cartilage graft donor site morbidity following rhinoplasty and nasal reconstruction. Craniomaxillofac Trauma Reconstr. 2018;11:278–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.