Background:
In recent years, the demand for genital plastic procedures has increased. Of those, the reduction of the labia minora has become very popular. Several techniques are described, with all its advantages and disadvantages. The aim of this study is to introduce a novel approach combining de-epithelialization with wedge resection.
Methods:
In this retrospective study, we included patients seen between September 2011 and April 2014 with hypertrophic labia minora. The surgical technique consisted in an integrated approach of de-epithelialization and wedge excision. Patients were examined for early and late postoperative complications. Furthermore, patient satisfaction was evaluated at the final follow-up.
Results:
A total of 17 labioplasties (Franco type II–IV) in 10 patients with a mean age of 29 ± 12 years (range 20–62 y) were performed. Three patients experienced wound-healing problems, requiring surgical revision. After a median follow-up of 39 ± 6 months (range 28–48 mo), a high overall patient satisfaction has been achieved (8.6 ± 1.1). No dyspareunia, hypertrophic scarring, or micturition problems have been reported.
Conclusions:
By using our integrated approach, hereby called the “butterfly technique,” the neurovascular supply remains preserved, and an efficient volume reduction can be achieved with a concealed scar. Nevertheless, suture techniques and suture materials have to be tested to reduce the incidence of wound dehiscence rate.
INTRODUCTION
The number of procedures for labia minora reduction continues to rise worldwide.1 Numerous congenital and acquired anomalies have been associated with hypertrophy of the labia minora, such as hormonal imbalance, excessive manipulation, chronic irritation, urinary incontinence, and myelodysplastic diseases.2,3 Thus, next to aesthetic considerations, indications for labia minora reduction might be foreign body sensation, poor hygiene, chronic infections, ulceration, difficulties in wearing clothes, or psychological impairment.4
Today, no standard techniques for labia minora reduction have been established yet.1,4 Jiang et al1 recently introduced a new modified labiaplasty method, combining wedge de-epithelialization on the medial side and edge resection to meet the needs of more patients and reduce complications. The goals of labioplasty are the reduction of the hypertrophic labia minora, preserving the neurovascular supply and a hidden scar. Edge excision5,6 or elliptical excision2 is fast and easy to perform. However, the results can be unsatisfactory due to overreduction, scar visibility, chronic tenderness of the scars and color mismatch.7–9 Potential complications are wound dehiscence, infection or urinary symptoms.9 In 1998, a new labia minora reduction technique was described by Alter10 using a central wedge or V excision of the most protuberant portion. The aim was to maintain the normal color and contour of the labial edge with minimal tenderness of the scar line. Since then, several modifications have been reported.7,11–15 Murariu et al9 compared straight line excision versus wedge excision in a total of 24 consecutive patients. Based on their observations, they recommend central wedge reduction labioplasty as the method of choice because of better aesthetic outcome. By using this technique, hypopigmentation of the labia minora and pruritus remain minimal.9 Nevertheless, building a superior pedicle by wedge excision potentially can jeopardize sensation7 or can induce distal flap necrosis.8,11,13 To preserve the neurovascular supply, Choi and Kim16 described in 2000 a novel approach by using a bilateral de-epithelialization. This technique also preserves the natural contour and color of the labial edge. Patients with labial hypertrophy of Franco Classification III and IV,17 however, seemed not to have an adequate reduction of the labial volume.8,15,16
To overcome the potential drawbacks of the techniques described above, we developed a combined technique, which integrates the advantages of de-epithelialization and wedge excision. By using our “butterfly technique,” the scar is placed well hidden on the posterior part of the introitus where differences in color and thickness of the labia are less visible.
MATERIALS AND METHODS
General Patient Data and Outcome Evaluation
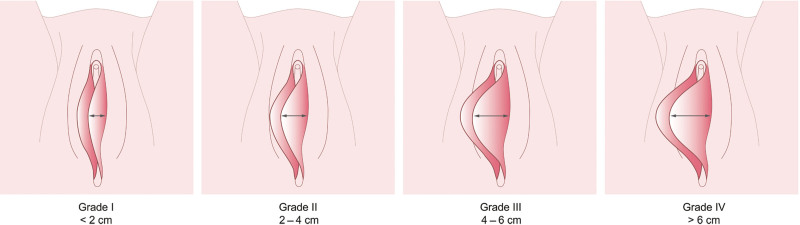
In this retrospective study, we included patients who presented between September 2011 and April 2014 with hypertrophic labia minora. Classification was performed according to Franco into grades I–IV depending on the protrusion of the labia minora through the labia majora: grade I, less than 2 cm; grade II, from 2 to 4 cm; grade III, from 4 to 6 cm; and grade IV, more than 6 cm (Fig. 1).17 Accordingly, there was no Franco grade I, and one patient was diagnosed with labia minora grade IV. Indications for the operative treatment were aesthetic concerns, or discomfort in wearing clothes or during sexual intercourse. Postoperative examinations were performed at 2 days, 2 weeks, and after 6 months. Patients were examined for early postoperative complications such as hematoma, infection, wound dehiscence, and partial flap necrosis. Late complications included problems of scarring and asymmetry. Complications were classified as minor if management was conservative and as major if a reoperation was performed.
Fig. 1.
The Franco’s classification on labial hypertrophy.
The outcome was evaluated at final follow-up. Patients were asked about their overall satisfaction using a Likert scale from 0 to 10 (0 = highly unacceptable, 10 = outstanding, Table 1), whether they would do the surgery again, about their sexual life and dyspareunia. Furthermore, hypertrophic scarring was evaluated. Written informed consent was obtained from all patients.
Table 1.
10-Point Likert Scale
| Likert Scale | Meaning |
|---|---|
| 1 point | Highly unacceptable |
| 2 points | Unacceptable |
| 3 points | Less than acceptable |
| 4 points | Below average |
| 5 points | Average |
| 6 points | Above average |
| 7 points | Good |
| 8 points | Very good |
| 9 points | Excellent |
| 10 points | Outstanding |
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval was obtained by the local ethical committee (Registry of all Projects in Switzerland, Ethikkommission Nordwest- und Zentralschweiz EKNZ, BASEC ID 2017-01243).
Surgical Technique
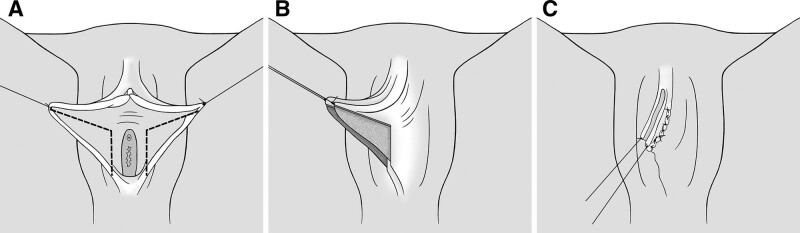
Labioplasties were performed in a lithotomy position under general anesthesia or spinal anesthesia. The most protuberant portion of each labia minora was fixed with a Vicryl 2/0 suture and the wedges to be excised were marked (Fig. 2). Care was be taken to preserve the natural edge of the labia minora. Next, lidocaine 1% with epinephrine 1:100,000 was injected. Then, the marked wedges were de-epithelialized and the neurovascular supply preserved (see Video 1 [online], which demonstrates de-epithelialization of the marked wedges, preserving the subcutaneous tissue and neurovascular supply). The superior pedicled flap was sutured to the posterior border in two layers, subcuticular and interrupted sutures with Vicryl 4/0, hereby preserving the darker corrugated labial edge (Fig. 3). An atraumatic needle was used to prevent tissue damage.
Fig. 2.
Schematic diagram of the surgical technique. The most protuberant portion of each labia minora was fixed with a Vicryl 2/0 suture and the wedges to be excised are marked (A). Then, the marked wedges were de-epithelialized and the neurovascular supply preserved (B). The superior pedicled flap was sutured to the posterior border in two layers, subcuticular and interrupted sutures with Vicryl 4/0, hereby preserving the darker corrugated labial edge (C).
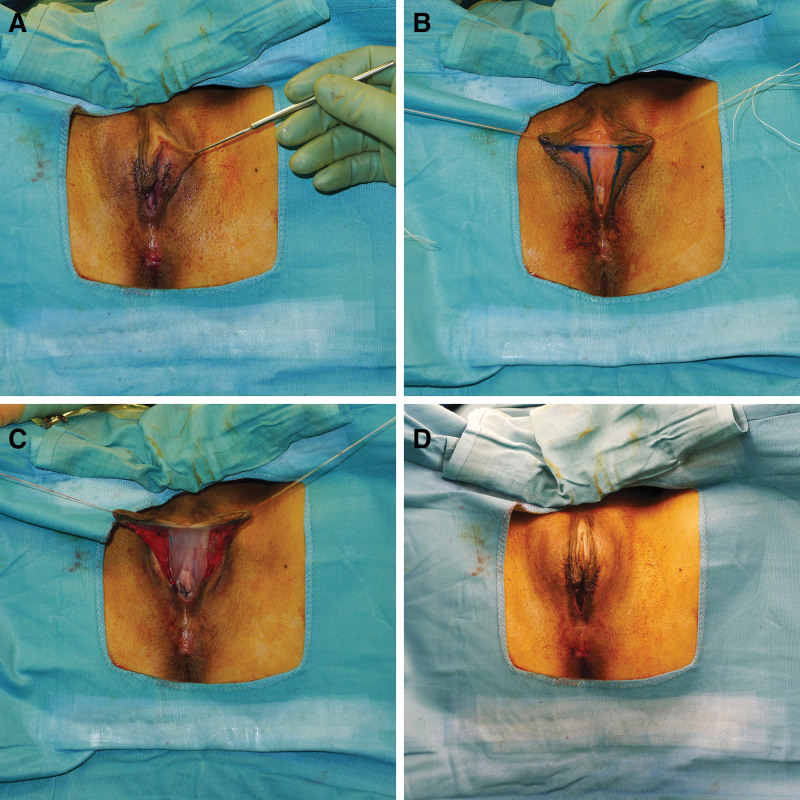
Fig. 3.
Intraoperative steps of the surgical technique. A, Preoperative view. B, Marking of the wedges. C, De-epithelialization of the wedges. D, Postoperative view.
Video 1. Video 1 from “The Butterfly Technique – A Retrospective Study for Labia Minora Reduction using an Integrated Approach.” Video 1 demonstrates de-epithelialization of the marked wedges, preserving the subcutaneous tissue and neurovascular supply.
For postoperative care, patients were instructed to locally disinfect after micturition and defecation. In six of the 10 patients, broad-spectrum antibiotics were prescribed for 5 days. Sexual intercourse was permitted 6 weeks postoperatively.
Statistical Analyses
The values are shown as the mean and SDs /standard error of mean or median and range where appropriate. Analyses were performed using GraphPad Prism version 5.00 for Windows (GraphPad Software, San Diego, Calif.).
RESULTS
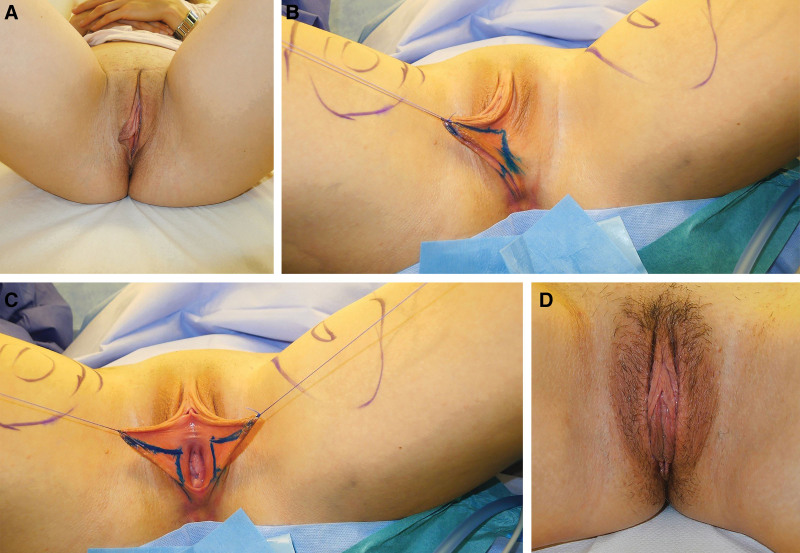
A total of 17 labioplasties in 10 patients with a mean age of 29 ± 12 years (range 20–62 y) were performed. Of those, seven patients underwent bilateral labial reduction (Table 2). The mean surgery time was 73 ± 49 minutes (range 31–179 min). One patient underwent labioplasty combined with liposuction of the abdomen and legs (Fig. 4), whereas another patient underwent simultaneous breast reduction. Three patients experienced wound-healing problems. In one patient, wound dehiscence was observed secondary to an infection, requiring surgical revision. The remaining two patients healed by secondary intention. No flap necrosis occurred during the follow-up period. None of the patients reported of problems with micturition. Scar corrections were performed after seven months for an unsightly scar after a conservatively treated hematoma and after 10 months for asymmetry. We found an overall higher complication and revision rate in patients with prolonged operative duration.
Table 2.
Overview of the Patient Characteristics Including Treatment, Complications, and Outcome
| Patient | Sex/Age (y) | Surgery | Surgery time (min) | Anesthesia | Follow-up (mo) | Complications | Revision | Outcome* |
|---|---|---|---|---|---|---|---|---|
| 1 | 32 | Bilateral butterfly | 52 | General | 31 | None | None | 9 |
| 2 | 24 | Bilateral butterfly | 79 | Local | 32 | Infection and wound dehiscence | Yes | 8 |
| 3 | 62 | Bilateral butterfly | 36 | General | 37 | None | None | 10 |
| 4 | 20 | Bilateral butterfly | 38 | General | 39 | None | None | 8 |
| 5 | 27 | Bilateral butterfly | 31 | Local | 44 | None | None | 7 |
| 6 | 24 | Unilateral butterfly | 138 (bilateral breast reduction) | General | 44 | Wound dehiscence | Yes (scar correction) | 7 |
| 7 | 22 | Unilateral butterfly | 32 | General | 44 | None | None | 9 |
| 8 | 25 | Bilateral butterfly | 73 | Local | 39 | Transient edema | None | 10 |
| 9 | 32 | Unilateral butterfly | 75 | Local | 48 | Hematoma and wound dehiscence | Yes (scar correction) | 8 |
| 10 | 23 | Bilateral butterfly | 179 (with liposuction of the abdomen and legs) | Local | 28 | None | None | 10 |
*0 = highly unacceptable, 10 = outstanding.
Fig. 4.
A, Preoperative view. B and C, Intraoperative view with the marked edges. D, Postoperative view after 6 weeks.
After a median follow-up of 39 ± 6 months (range 28–48 mo), a high overall patient satisfaction has been achieved (8.6 ± 1.1, Table 3) and the scar was well hidden. All patients would recommend the procedure to a friend, whereas nine patients would undergo the operation again. Five patients noticed no change in their sex life, whereas four patients reported of an improved sex life. No dyspareunia or micturition problems have been reported.
Table 3.
Follow-up Questionnaire
| Overall satisfaction | |
| Very satisfied | 4 |
| Satisfied | 5 |
| Little satisfied | 0 |
| Not satisfied | 0 |
| Not available | 1 |
| Likert scale 1–10 | |
| 7 | 2 |
| 8 | 3 |
| 9 | 2 |
| 10 | 3 |
| Undergo operation again | |
| Yes | 9 |
| No | 0 |
| Not available | 1 |
| Recommend operation | |
| Yes | 10 |
| No | 0 |
| Sex life | |
| Improved | 4 |
| Equal | 5 |
| Worse | 0 |
| No sex life | 1 |
| Dyspareunia | 0 |
| Micturition problems | 0 |
DISCUSSION
The size and appearance of a woman’s labia are more commonly noticed from both functional and aesthetic standpoints. Thus, there is an increase in the number of women requesting aesthetic surgery of the female genitalia and different techniques have been proposed.6 To date, no single ideal procedure for labia minora reduction has been identified yet.8
By using our integrated approach of de-epithelialization and wedge excision, an acceptable cosmetic result can be achieved with a preserved neurovascular supply and darker corrugated labial edge. Furthermore, an efficient vertical volume reduction can be obtained, and the scar is well hidden on the posterior part of the introitus. Despite a relatively high complication rate in our series, a high overall patient satisfaction was achieved after the final follow-up. An improved sex life was reported in four patients. Shifting the clitoris closer to the vaginal introitus might result in a stronger stimulation of the clitoris during intercourse, leading to an improved sexual excitability.4
In a recent study by Jiang et al,1 a new bilateral labiaplasty procedure was presented, combining wedge de-epithelialization on the medial side with edge resection on the lateral side. The authors concluded that this modified technique is a safe method with low risks, and may result in better sexual sensitivity for the patients.1 However, only patients with stage III labia hypertrophy or higher according to Franco’s classification were included.17 Scarring might be more obvious in this technique, potentially leading to a decrease in sexual sensitivity after labiaplasty. In our technique, more subcutaneous tissue is preserved, which may result in better sexual sensitivity. That being said, further research is needed with objective measurements. Moreover, Filho et al18 reported of a Butterfly-like approach, where the labia minora were attached temporarily to the internal thigh with stitches, resembling an open butterfly wing. By using this technique with central and inferior wedge resection, evaluation of asymmetry may be facilitated, aiding precision in the treatment.18 Although this method might be suitable especially for asymmetrical labia minora, more subcutaneous tissue might be sacrificed, ultimately affecting sensation. The ultimate goal of labia minora reduction is to preserve the neurovascular supply and to meet the expectations of the patients who anticipated that the labia minora would be completely covered by the labia majora over their entire length, not only in the section below the clitoris.4
When performing the surgery, it is important to have good anesthesia for a safe and comfortable procedure. The surgery can be done under local anesthesia using epinephrine to reduce bleeding, or under epidural or general anesthesia. The decision depends on the extent of the surgery to be performed, and ultimately remains at the discretion of the operating surgeon and the patient, respectively.19
Potential complications after labia minora reduction are problems during micturition, dyspareunia, wound-healing complications, hypertrophic scars, hematoma or secondary bleeding, and suture dehiscence.4 To overcome the limitation of postoperative micturition problems, correction of the clitoral protrusion by means of caudal tightening should be avoided if the urethral orifice is too close to the clitoris.4 If continuous subcutaneous wound closure is performed, hematoma or secondary bleeding remains minimal.4 Infection occurs relatively rarely due to the rich blood supply of the genital tissue and the routine administration of a broad-spectrum antibiotic. Overall, postoperative care varies greatly.19 Either topical (erythromycin, polymyxin B, and bacitracin) or oral antibiotics (first-generation cephalosporins, clindamycin for patients with penicillin allergies) are recommended, whereas several studies are recommending both.13,20,21 Postoperative pain remains minimal and subsides after a couple of days after the surgery and can be well managed with medications.4
Postoperative wound dehiscence is relatively common and is particularly difficult to manage, given the unique physiology of the labia.15 Whether the technique (running versus interrupted, or one or two layers) or suture material (permanent versus resorbable) affects the rate of dehiscence remains unknown, and there is no apparent consensus within the literature.15 In his initial description of the wedge resection, Alter10 described the use of Vicryl sutures (Ethicon, Inc., Somerville, N.J.), whereas Hodgkinson and Hait2 reported on chromic gut and permanent sutures (4-0 Prolene; Ethicon, Inc.) which were removed at 7 days. Recently, Alter7 utilized 5-0 Monocryl (Ethicon, Inc.) sutures placed in at least three layers; vertical mattress sutures were used for the leading labial edge, a running Monocryl was placed for the remainder of the medial edge, and interrupted sutures were inserted for the lateral edge. Regardless of suture type, the ultimate goal is to achieve a tension-free closure to minimize the risk of dehiscence.15 Furthermore, it is most important to recognize that postoperative edema in this friable tissue can confound even the most exacting closure.15 Last, Dermabond (Ethicon, Inc.) has been found to serve as a useful adjunct in maintaining wound edge adherence when issues of wound separation arose.15
Our complications are comparable to previous reports. Gress4 recently reported of an overall complication rate of 6.4% of wound-healing problems in 812 patients using the “composite reduction labiaplasty.” Triana and Robledo22 performed direct labia minora excision with or without clitoral hood molding and management of labia majora in 74 patients. Of those, one patient had an infection and one had wound dehiscence. Alter reported in a series of a total of 407 patients an overall reoperation rate of 12 patients (2.9%).7 Hereby, a central wedge or V was removed from the most protuberant portion of each labium minus. To excise redundant lateral labium and excess lateral clitoral hood, the outer portion of the V excision was usually curved lateral and anterior.7 However, a limitation of the study is that only 123 patients were examined after surgery.2
Rouzier et al14 evaluated in a consecutive series of 163 patients the results and complication rate after surgical reduction of labia minora (Franco types III and IV). Eleven patients (7%) underwent a second procedure because of a minimal wound dehiscence resulting in an aesthetic result that was not perfect and warranted improvement.14 Postoperative pain was reported by 64% of the patients and was usually relieved by nonnarcotic analgesic agents and lasted 1–60 days (median, 7 d). Postoperative discomfort was reported by 45% of the patients and 23% complained of entry dyspareunia for 3–90 days (median 28 d).14
Ellsworth et al8 presented a case series of 12 patients using the edge excision technique, the inferior wedge resection technique, or de-epithelialization reduction labioplasty, depending on the protrusion of the labia minora through the labia majora. In their study, three patients experienced minor wound-healing difficulties that resolved spontaneously.8 The authors also proposed an algorithm for pairing the degree of deformity with the optimal surgical procedure.8 They suggest the de-epithelialization technique in patients with the least amount of hypertrophy (Franco type I and II), preserving the natural texture, color, and rich neurovascular supply. Also, it avoids a suture line on the labial edge.2 For patients with labia measuring 4–6 cm or more in width (Franco type III and IV), the edge excision technique or the wedge resection technique with superior pedicle flap closure seems to be most appropriate. However, by using this technique, the naturally darker corrugated edge is amputated. Nevertheless, some patients associate this darker edge aesthetic with an aged appearance and prefer to have it removed.10 Thus, it is most important to identify the patient’s goals before choosing a surgical technique.
It has been reported that the edge excision technique has fewer wound-healing complications, but is associated with a suture line at the periphery, potentially increasing the risk for scar contracture and chronic pain during sexual intercourse.23 Last, it is of paramount importance to avoid the complication of excessive reduction.13
For women with large labia (Franco type IV) preferring to keep the natural aesthetic of the labial edge, the inferior wedge resection with a superior pedicle is suggested to be the procedure of choice.14 This technique preserves the darker corrugated labial edge as well as its neurovascular supply.16 However, fibrosis, scar and labial distortion has been described due a higher risk of tip necrosis of the superior pedicle.10,13,14
Ultimately, our study is limited by a low number of patients compared to other studies.7,10,13,14 Therefore, evaluation of a larger cohort is required to confirm our findings.
CONCLUSIONS
By using our integrated approach, the neurovascular supply remains preserved, an efficient volume reduction can be achieved, and the scar is well hidden on the posterior part of the introitus. Nevertheless, suture techniques and suture materials have to be tested to reduce the wound dehiscence rate.
Footnotes
Published online 13 September 2021.
Presented at the 49th Annual Meeting of the Swiss Society of Plastic, Reconstructive and Aesthetic Surgery, 2013, Lugano.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Jiang X, Chen S, Qu S, et al. A new modified labiaplasty combined with wedge de-epithelialization on the medial side and edge resection. Aesthetic Plast Surg. 2021; 45:1869–1876. [DOI] [PubMed] [Google Scholar]
- 2.Hodgkinson DJ, Hait G. Aesthetic vaginal labioplasty. Plast Reconstr Surg. 1984;74:414–416. [DOI] [PubMed] [Google Scholar]
- 3.Kato K, Kondo A, Gotoh M, et al. Hypertrophy of labia minora in myelodysplastic women. Labioplasty to ease clean intermittent catheterization. Urology. 1988;31:294–299. [DOI] [PubMed] [Google Scholar]
- 4.Gress S. Composite reduction labiaplasty. Aesthetic Plast Surg. 2013;37:674–683. [DOI] [PubMed] [Google Scholar]
- 5.Capraro VJ. Congenital anomalies. Clin Obstet Gynecol. 1971;14:988–1012. [DOI] [PubMed] [Google Scholar]
- 6.Felicio Yde A. Labial surgery. Aesthet Surg J. 2007;27:322–328. [DOI] [PubMed] [Google Scholar]
- 7.Alter GJ. Aesthetic labia minora and clitoral hood reduction using extended central wedge resection. Plast Reconstr Surg. 2008;122:1780–1789. [DOI] [PubMed] [Google Scholar]
- 8.Ellsworth WA, Rizvi M, Lypka M, et al. Techniques for labia minora reduction: an algorithmic approach. Aesthetic Plast Surg. 2010;34:105–110. [DOI] [PubMed] [Google Scholar]
- 9.Murariu D, Jackowe DJ, Parsa AA, et al. Comparison of wedge versus straight-line reduction labioplasty. Plast Reconstr Surg. 2010;125:1046–1047. [DOI] [PubMed] [Google Scholar]
- 10.Alter GJ. A new technique for aesthetic labia minora reduction. Ann Plast Surg. 1998;40:287–290. [DOI] [PubMed] [Google Scholar]
- 11.Alter GJ. Labia minora reconstruction using clitoral hood flaps, wedge excisions, and YV advancement flaps. Plast Reconstr Surg. 2011;127:2356–2363. [DOI] [PubMed] [Google Scholar]
- 12.Giraldo F, González C, de Haro F. Central wedge nymphectomy with a 90-degree Z-plasty for aesthetic reduction of the labia minora. Plast Reconstr Surg. 2004;113:1820–1825. [DOI] [PubMed] [Google Scholar]
- 13.Munhoz AM, Filassi JR, Ricci MD, et al. Aesthetic labia minora reduction with inferior wedge resection and superior pedicle flap reconstruction. Plast Reconstr Surg. 2006;118:1237–1247. [DOI] [PubMed] [Google Scholar]
- 14.Rouzier R, Louis-Sylvestre C, Paniel BJ, et al. Hypertrophy of labia minora: experience with 163 reductions. Am J Obstet Gynecol. 2000;182(1 Pt 1):35–40. [DOI] [PubMed] [Google Scholar]
- 15.Tepper OM, Wulkan M, Matarasso A. Labioplasty: anatomy, etiology, and a new surgical approach. Aesthet Surg J. 2011;31:511–518. [DOI] [PubMed] [Google Scholar]
- 16.Choi HY, Kim KT. A new method for aesthetic reduction of labia minora (the deepithelialized reduction of labioplasty). Plast Reconstr Surg. 2000;105:419–422. [DOI] [PubMed] [Google Scholar]
- 17.Franco T, Franco D. Hipertrofia de Ninfas. J Brasileiro Ginecol. 1993;103:163–165. [Google Scholar]
- 18.Filho OP, Ely JB, Lee KH, et al. Labiaplasty with stable labia minora retraction-butterfly-like approach. Plast Reconstr Surg Glob Open. 2020;8:e2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Motakef S, Rodriguez-Feliz J, Chung MT, et al. Vaginal labiaplasty: current practices and a simplified classification system for labial protrusion. Plast Reconstr Surg. 2015;135:774–788. [DOI] [PubMed] [Google Scholar]
- 20.Solanki NS, Tejero-Trujeque R, Stevens-King A, et al. Aesthetic and functional reduction of the labia minora using the Maas and Hage technique. J Plast Reconstr Aesthet Surg. 2010;63:1181–1185. [DOI] [PubMed] [Google Scholar]
- 21.Cao YJ, Li FY, Li SK, et al. A modified method of labia minora reduction: the de-epithelialised reduction of the central and posterior labia minora. J Plast Reconstr Aesthet Surg. 2012;65:1096–1102. [DOI] [PubMed] [Google Scholar]
- 22.Triana L, Robledo AM. Refreshing labioplasty techniques for plastic surgeons. Aesthetic Plast Surg. 2012;36:1078–1086. [DOI] [PubMed] [Google Scholar]
- 23.Fitzpatrick L. Plastic Surgery below the Belt. New York, N.Y.: TIME Magazine. 2008. [Google Scholar]