Colombia exemplifies the complex risk dynamics for COVID-19 transmission where epidemiological, behavioral, and political forces are simultaneously at play. Throughout March to June 2021, Colombia experienced a massive third wave of COVID-19 cases and deaths, surpassing two previous surges (Figure 1). [1] On June 23, 2021, the National Institute of Health (INS) reported Colombia's four millionth COVID-19 case, just two days after recording the 100,000th death. Throughout this period, South America was the global COVID-19 hotspot. [2] Colombia's incidence and mortality rates were among the highest in the world and continued to increase even after the remainder of the continent was trending downward (Figure 2).
Figure 1.
Colombia: 7-day moving average of daily new confirmed COVID-19 cases per million people (by date of report) through June 30, 2021
Figure 2.
Colombia compared to the continents of the world on the 7-day moving average of daily new confirmed COVID-19 cases per million people (by date of report) through June 30, 2021
Colombia's first cases were identified in March 2020, as COVID-19 circumnavigated the globe and the World Health Organization (WHO) declared the outbreak to be a pandemic.[3] During the subsequent 16 months, Colombia experienced three distinct surges in COVID-19 cases (Figure 1). [4] During each successive wave, the peak was higher, surpassing 13,000 daily cases in August 2020; then exceeding 21,000 in mid-January 2021; and later topping 33,000 in June 2021. [1] The protracted surge from March through June 2021 evolved into a two-stage peak-within-a-peak. [1]
Multiple factors may have interacted synergistically to propel this sustained rise in COVID-19 cases, primarily by increasing the likelihood of citizens congregating in shared settings or family gatherings. First, Colombia progressively discontinued pandemic prevention measures even as cases accelerated upward, opting for broad societal “reopening” in hopes of stimulating a battered economy. Pandemic fatigue was ubiquitous, accompanied by public eagerness to end the lockdown. Second, COVID-19 transmission risks were elevated by delayed vaccine acquisition and slow-motion vaccine distribution. Only 21% of the population had received at least a single vaccine dose on the day that cases topped 4 million. [5] Third, genomic testing detected the presence of highly transmissible and pathogenic SARS-CoV-2 variants, particularly gamma (P.1), mu (B.1.621), and currently, Delta (B.1.617.2), for which the most common vaccine administered in Colombia, Sinovac, has lower efficacy. [6] Fourth, COVID-19 testing increased sharply, boosting the number of symptomatic and asymptomatic cases detected. [1,4] Fifth, in late April, protests and transit blockades erupted nationwide, triggered by government policy proposals; these high-visibility demonstrations have been blamed for potentially spreading COVID-19. Sixth, and related to the protests, Idrovo (2021) suggested that there may have been a fundamental shift in risk perception, commenting that, “Colombia is a clear example of a society that fears hunger, absence of work, violence, lack of education, and other social problems more than SARS-CoV-2 infection.” [7]
As we consider how these factors may have played a role, caution is the watchword when interpreting trends. For COVID-19, attributing causation to observed epidemic patterns and predicting future surges has been notoriously uncertain and speculative even for experts. [8]
Colombia's decision to ease COVID-19 containment policies and reopen the economy during May and June 2021 was consequential. Throughout 2020, prior to the availability of COVID-19 vaccines, nations worldwide resorted to using nonpharmacological interventions (NPIs)—population-level policy measures—to curtail the spread of COVID. [9] Such blunt-force measures demonstrably reduced transmission. [9] Colombia first imposed nationwide “quarantine” measures on March 25, 2020. These included school and workplace closures, cancellation of public events, restrictions on gatherings, public transportation shutdowns, stay-at-home orders, internal travel restrictions, international travel controls and border closures, and public information campaigns. Mask mandates were enacted later. Yet by June 2021, after the reopening, only seasonal school closures and some mask mandates remained in effect. [6] Mandate or not, more than 80% of the Colombian population has consistently opted to wear masks when leaving home, dating from the first months of the pandemic. [6] However, no restrictions were in force during the surge related to social distancing or gatherings.[6] Mobility, measured by smartphone apps, briefly dipped by 25% in late May, only to return swiftly to full mobility in mid-June as cases were escalating. [6]
COVID-19-related economic pressures created powerful impetus for the government to reopen borders, reactivate commerce, and reengage the public. Colombia's GDP plummeted 6.8% in 2020. Four million persons lost their jobs and by year-end 2020, 3-in-8 Colombians (37.5%) lived below the poverty line. Poverty was related to more severe cases of COVID-19 from the earliest months of the pandemic [10] and socioeconomic inequalities were significantly related to COVID-19 mortality. [11]
Half of Colombia's wage earners (48%) work in the informal sector. [12] Informal workers receive no pay when absent, lack personal protective equipment, labor in close proximity to others, and return home to crowded multigenerational households. Precarious work and lack of social protection translate to a brutal reality: social distancing and lockdown measures are incompatible with family economic survival. [10,11] COVID-19 surveillance data reflect elevated risks for the working class with 75% of cases between ages 20 and 59. [1]
Adding to Colombia's economic and health care demands, an estimated two million Venezuelan migrants have transplanted to Colombia over recent years. [13] As the primary receptor nation for the Venezuelan diaspora, the presence of these vulnerable migrants increases the size of the total population inside Colombia needing access to jobs and health care by 4%. Many Venezuelans are clustered in informal settlements, migrant shelters, or on the street. According to the International Labor Organization, 62% of Venezuelan nationals in Colombia are employed in sectors deemed highly impacted by the pandemic, posing overt risks for COVID-19 transmission. [14]
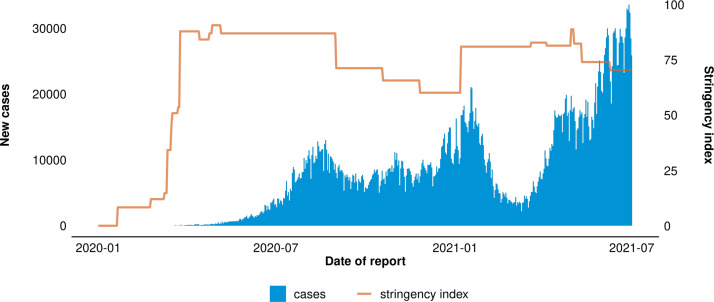
So, did Colombia's choice to boldly reopen the country while COVID-19 cases were climbing sharply influence the course of the pandemic? [5] This cannot be known with certainty, but two metrics provide insights. The Oxford COVID-19 Government Response Tracker monitors NPIs for 180 countries. [15] Each day, for each nation, the Tracker generates a summary metric for all NPIs currently in force—the Stringency Index—ranging from 0 (no restrictions) to 100 (maximal restrictions across all policies). The WHO brilliantly created a graphic that superimposes the Stringency Index on the COVID-19 epidemic curve (Figure 3). [4] It is visually apparent that Colombia eased restrictions, and the corresponding Stringency Index declined, in Fall 2020 and during May and June 2021. Easing restrictions preceded and continued up to the January surge and later, coincided with the peak-on-peak surge during May and June 2021. Declining from a maximum Stringency Index of 91, as of June 30, 2021, the Index stood at 70. [4]
Figure 3.
Colombia: Daily new confirmed COVID-19 cases per million people (by date of report) and corresponding Oxford Stringency Index through June 30, 2021
Another indicator, population mobility, uses smartphone apps to track citizen movement in real time. [6] As NPIs were eased, mobility returned to pre-COVID levels in January, and again in June 2021. [6] While not conclusive, observations based on both indicators are compatible with an explanation that government easing of NPIs contributed to marked upticks in COVID-19 cases.
The proliferation of COVID-19 testing during April through June 2021 may have both captured the startling rise in incident cases and increased the level of case detection (Figure 4). [4] The COVID-19 positivity rate rose above 30%. Increased access to testing facilitated screening for contacts of confirmed cases. The reopening, right at the start of Colombia's short summer vacation season, may have prompted many to seek testing prior to holiday travel, including mandatory testing for international air travelers. The steep rise in asymptomatic cases suggests increased case detection, as more apparently healthy persons were tested.
Figure 4.
Colombia: COVID-19 tests per thousand people by week and percent positive, June 1, 2020 through June 27, 2021
Coordinated nationwide demonstrations commenced on April 28, 2021, opposing proposed fiscal policy reforms that would have raised taxes mid-pandemic, and health system reforms that would have given health insurance companies more influence. Writ large, the protests of 2021 were a resumption of the massive 2019 strikes that focused on poverty, inequality, injustice, climate change, and the piecemeal implementation of the peace accord. The 2021 demonstrations started peacefully and initially garnered support from 73% of the Colombian public. Protests devolved into pandemonium in several cities as police forces launched a violent crackdown on demonstrators. Deaths of protestors climbed to 72 as police violence itself became an accelerant for more protests.
The protests involved mass gatherings where demonstrators did not observe social distancing guidelines and some did not wear masks. Could protests have elevated risks for airborne transmission of COVID-19? This was clearly the invective for politicians who denounced the protests. Notably, during his June 21 commemoration of the tragic loss of 100,000 Colombians to COVID-19, Colombia's President Duque explicitly blamed the protests for causing 10,000 preventable deaths. [16]
Multiple studies were conducted to determine whether the Colombian protests set off super-spreader events. Investigators examined the epidemic curves for metropolitan centers where large demonstrations occurred. [17] The timing of the protests neither matched nor predicted surges in COVID-19 cases. Another team of researchers conducted mathematical analyses, applying two types of modeling procedures to examine epidemic trends in major protest cities. [18] Patterns were diverse across the cities examined, prompting the authors to conclude that the protests had a “heterogeneous effect” on the number and trend of COVID-19 cases. [18]
A just-released preprint authored by investigators from the Colombian Ministry of Health reported an interrupted time series analysis for the entire country and 24 capital cities that showed an estimated increase of 3,360 cases associated with the protests—but did not claim a causal effect. For context, the authors note that 582,000 COVID-19 cases were registered nationwide during the peak of the protests. [19]
These equivocal findings in Colombia were reminiscent of studies conducted in 2020 focusing on worldwide Black Lives Matter protests following the police killing of George Floyd in Minnesota; researchers, using modeling techniques and anonymized cell phone data, failed to definitively link protests to COVID-19 transmission. [20] Nevertheless, outdoor mass gatherings can spread COVID-19 if special conditions are met; Stanford investigators showed how outdoor presidential rallies attended by large audiences of unmasked, cheering supporters sitting close together for hours became super spreader events.
Despite the lack of statistical evidence that Colombian protests amplified COVID-19 spread, another tactic used by the demonstrators may have affected care for COVID-19 patients. Paralyzing transit blockages obstructed access to hospitals and clinics for staff and patients, impeded access to vaccination and testing sites for clients and personnel, and disrupted supply chains for vital equipment and oxygen.
Taken together, Colombia provides a potent case example of complex, multifactorial contributions to steep and sustained surges in COVID-19 cases and deaths. The tapering of the surge and the future trajectory of the pandemic in Colombia will be influenced by policy decisions regarding COVID-19 containment measures, acceleration of the lagging vaccination program, the degree to which dangerous variants propagate, and the unpredictability of the virus.
Contributors
Conceptualization: JMS, RCB, JMU-R, OABA, Review of literature and identification of government reports and online resources: OABA, JMU-R VAPE, RCB, JMS
Desk review: RCB, JAOC, VAPE, OABA, JMU-R
Manuscript writing, review and editing: JMS, RCB, JMU-R, OABA, OM, ZE
Spanish language translation: OM, ZE
Funding
None
Declaration of Competing Interests
None
Acknowledgements
None
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lana.2021.100072.
Contributor Information
James M. Shultz, Email: jshultz1@med.miami.edu.
Ryan C. Berg, Email: RBerg@csis.org.
Oscar Alberto Bernal Acevedo, Email: obernal@uniandes.edu.co.
Jovana Alexandra Ocampo Cañas, Email: ja.ocampo@uniandes.edu.co.
Victoria A. Pinilla Escobar, Email: v.pinillaescobar@med.miami.edu.
Omar Muñoz, Email: omar.munoz@jhsmiami.org.
Zelde Espinel, Email: z.espinel@miami.edu.
José Miguel Uribe-Restrepo, Email: miguel.uribe@gmail.com.
Appendix. Supplementary materials
References
- 1.Instituto Nacional de Salud. Coronavirus (COVID-19 en Colombia). https://www.ins.gov.co/Paginas/Inicio.aspx (accessed August 10, 2021).
- 2.Turkewitz J, Taj M. New York Times; 2021. After a year of loss, South America suffers worst death tolls yet.https://www.nytimes.com/2021/04/29/world/americas/covid-latin-america.html?0p19G=0232 Apr 29. (accessed August 10, 2021) [Google Scholar]
- 3.Shultz JM, Perlin A, Saltzman RG, Espinel Z, Galea S. Coronavirus disease's first wave circumnavigates the globe. Disaster Med Public Health Prep. 2019;14(5):e28–e32. doi: 10.1017/dmp.2020.103. 2020 Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. COVID-19 Explorer. Colombia. 2021 June 23. https://worldhealthorg.shinyapps.io/covid/ (accessed August 10, 2021).
- 5.Our World in Data. Coronavirus (COVID-19) Vaccinations: Colombia. 2021 June 23. https://ourworldindata.org/covid-vaccinations?country=COL (accessed August 10, 2021).
- 6.Institute for Health Metrics and Evaluation. COVID-19 Results Briefing: Colombia. 2021 June 24. http://www.healthdata.org/sites/default/files/covid_briefs/125_briefing_Colombia.pdf (accessed August 10, 2021).
- 7.Idrovo AJ. More social discontent than pandemic-related risk perception in Colombia. Lancet. 2021;398(10296):211. doi: 10.1016/S0140-6736(21)01239-3. Jul 17Epub 2021 Jun 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Recchia G, Freeman ALJ, Spiegelhalter D. How well did experts and laypeople forecast the size of the COVID-19 pandemic? PLoS One. 2021;16(5) doi: 10.1371/journal.pone.0250935. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0250935 May 5. (accessed August 10, 2021) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ayouni I, Maatoug J, Dhouib W, Zammit N, Fredj SB, Ghammam R, Ghannem H. Effective public health measures to mitigate the spread of COVID-19: a systematic review. BMC Public Health. 2021;21(1):1015. doi: 10.1186/s12889-021-11111-1. May 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moreno-Montoya J, Ballesteros SM, Idrovo AJ. COVID-19 distribution in Bogotá, Colombia: effect of poverty during the first 2 months of pandemic. J Epidemiol Community Health. 2021 doi: 10.1136/jech-2020-214579. Jun 30:jech-2020-214579Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 11.Cifuentes MP, Rodriguez-Villamizar LA, Rojas-Botero ML, Alvarez-Moreno CA, Fernández-Niño JA. Socioeconomic inequalities associated with mortality for COVID-19 in Colombia: a cohort nationwide study. J Epidemiol Community Health. 2021 doi: 10.1136/jech-2020-216275. Mar 4:jech-2020-216275Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 12.Departamento Administrativo Nacional de Estadística (DANE). Empleo informal y seguridad social. 2021 June 11. https://www.dane.gov.co/index.php/estadisticas-por-tema/mercado-laboral/empleo-informal-y-seguridad-social (accessed August 10, 2021).
- 13.Espinel Z, Chaskel R, Berg RC, Florez HJ, Gaviria SL, Bernal O, Berg K, Muñoz C, Larkin MG, Shultz JM. Venezuelan migrants in Colombia: COVID-19 and mental health. Lancet Psychiatry. 2020;7(8):653–655. doi: 10.1016/S2215-0366(20)30242-X. Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.International Labour Organization. COVID-19 Pandemic in the World of Work: ILO Monitor: COVID-19 and the world of work. 7th edition. 2021 Jan 25. https://www.ilo.org/global/topics/coronavirus/impacts-and-responses/WCMS_767028/lang–en/index.htm (accessed August 10, 2021).
- 15.Hale T, Angrist N, Goldszmidt R, Kira B, Petherick A, Phillips T, et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat Hum Behav. 2021 Apr; 5(4):529-538. doi: 10.1038/s41562-021-01079-8 [DOI] [PubMed]
- 16.Suesca L. Sin aglomeraciones hubiéramos podido prevenir 10.000 muertes: Duque [Internet]. Colombia: Caracol radio. 2021 June 21. https://caracol.com.co/radio/2021/06/22/politica/1624317519_266206.html (accessed August 10, 2021).
- 17.Michelsen MI. No hay suficiente evidencia para culpar al paro por las muertes del tercer piso [Internet]. Colombia: La Silla Vacía. 2021 June 16. https://lasillavacia.com/historias/silla-nacional/no-hay-suficiente-evidencia-para-culpar-al-paro-por-las-muertes-del-tercer-pico (accessed August 10, 2021).
- 18.Moreno-Montoya J, Rodriguez-Villamizar LA, Idrovo AJ. Cold Spring Harbor Laboratory Press; 2021. Massive social protests amid the pandemic in selected Colombian cities: Did they increase COVID-19 cases?” MedRxiv.https://www.medrxiv.org/content/10.1101/2021.06.16.21258989v1 June 18. (accessed August 10, 2021) [Google Scholar]
- 19.Fernández-Niño JA, Peña-Maldonado C. Potential effects of social protests in Colombia on the transmission of COVID-19. SSRN.com. August 4, 2021. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3899602 (accessed August 10, 2021).
- 20.Neyman G, Dalsey W. Black Lives Matter protests and COVID-19 cases: relationship in two databases. J Public Health (Oxf) 2021;43(2):225–227. doi: 10.1093/pubmed/fdaa212. Jun 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.