Abstract
Background
It is an incontrovertible fact that the Rhino Orbital Cerebral Mucormycosis (ROCM) upsurge is being seen in the context of COVID-19 in India. Briefly presented is evidence that in patients with uncontrolled diabetes, a dysfunctional immune system due to SARS-COV-2 and injudicious use of corticosteroids may be largely responsible for this malady.
Objective
To find the possible impact of COVID 19 infection and various co-morbidities on occurrence of ROCM and demonstrate the outcome based on medical and surgical interventions.
Methodology.
Prospective longitudinal study included patients diagnosed with acute invasive fungal rhinosinusitis after a recent COVID-19 infection. Diagnostic nasal endoscopy (DNE) was performed on each patient and swabs were taken and sent for fungal KOH staining and microscopy. Medical management included Injection Liposomal Amphotericin B, Posaconazole and Voriconazole. Surgical treatment was restricted to patients with RT PCR negative results for COVID-19. Endoscopic, open, and combined approaches were utilized to eradicate infection. Follow-up for survived patients was maintained regularly for the first postoperative month.
Results
Out of total 131 patients, 111 patients had prior history of SARS COVID 19 infection, confirmed with a positive RT-PCR report and the rest 20 patients had no such history. Steroids were received as a part of treatment in 67 patients infected with COVID 19. Among 131 patients, 124 recovered, 1 worsened and 6 died. Out of 101 known diabetics, 98 recovered and 3 had fatal outcomes. 7 patients with previous history of COVID infection did not have any evidence of Diabetes mellitus, steroid intake or any other comorbidity.
Conclusion
It can be concluded that ROCM upsurge seen in the context of COVID-19 in India was mainly seen in patients with uncontrolled diabetes, a dysfunctional immune system due to SARS-COV-2 infection and injudicious use of corticosteroids.
Keywords: COVID-19, Mucormycosis, Acute invasive fungal sinusitis, Diabetes mellitus
1. Introduction
Rhino Orbital Cerebral mucormycosis (ROCM) is an acute invasive fungal infection which is rare, opportunistic and potentially fatal, which mostly occurs in immunocompromised patients. It is caused by saprophytic and opportunistic fungi of class Phycomycetes, order mucorales, family mucoraceae belonging to genus mucor and rhizopus [1]. Fungal sinusitis can be categorized into non-invasive and invasive groups. While non-invasive fungal sinusitis does not exhibit the penetration of mucosa by hyphae; but in invasive fungal sinusitis hyphae do invade the mucosa [2]. Mucormycosis is manifested by a variety of different syndromes in humans, particularly in immunocompromised patients and those with diabetes mellitus [3].
During the second wave of covid in India there was a rapid rise in mucormycosis cases in patients infected with covid. This rise was attributed to many factors which include steroid intake, diabetes mellitus, oxygen therapy and ventilator/ICU management. There were many reports suggesting the role of industrial oxygen and even use of excessive zinc in etiology of mucor. Literature review regarding association of Invasive Fungal Rhinosinusitis with COVID-19 revealed only isolated case reports.
This is a prospective study done in a large tertiary care hospital to find the possible impact of COVID 19 infection and various co-morbidities on occurrence of ROCM and demonstrate the outcome based on medical and surgical interventions in our institution.
2. Methods
Our institution was declared to be a 2000 bedded fully covid facility after the emergence of Covid 19 infection in New Delhi, India in April 2020 and we have treated more than 21000 Covid patients combined in both first and second waves. After the second wave there was a rapid increase in the number of Covid associated mucor cases (CAM) in the city during April 2021, hence a Mucor surveillance committee was formed by the Dean of the Institution, which included specialists from various departments for diagnosis and management of mucor cases. The ENT wards were converted into a Mucor ward with one ward for Covid positive mucor patients and another ward for Covid negative mucor patients. The present study is a prospective observational study done in the Department of Otorhinolaryngology, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi, India. A total of 131 patients of confirmed Acute Invasive Fungal Rhinosinusitis were included in the study period from 21 May 2021 to 30 June 2021. Patients whose postoperative histopathology did not prove invasive fungal disease were excluded from the study. The study was approved by the Institutional ethical committee of Maulana Azad Medical College vide IEC number no 396.
Data was collected in a proforma and entered in a google sheet. Patient demographics, presenting signs and symptoms, diagnostic investigations including imaging findings, histopathological findings, medical and surgical management approach and clinical outcomes were tabulated and analysed.
2.1. Clinical investigation
Diagnostic nasal endoscopy (DNE) was performed on each patient and swabs using nylon brush were taken from the representative areas and sent for fungal KOH staining and microscopy. We used different sets of endoscopic equipment for covid positive and covid negative mucor cases. The covid positive patients were taken up for nasal endoscopic examination and biopsy under full PPE cover.
2.2. Microbiological investigations
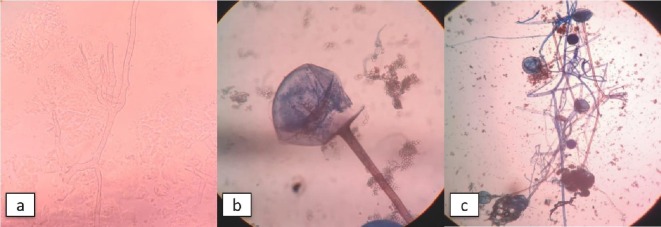
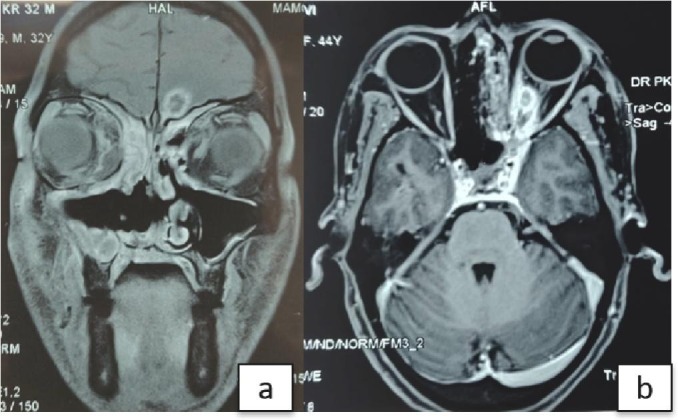
The samples received in the mycology were subjected to direct microscopy i.e., potassium hydroxide mount (KOH) mount to see for fungal hyphae. On KOH microscopy - broad aseptate/pauci septate hyphae with wide angle branching were seen which were suggestive of mucormycosis (Fig. 1 ). All the samples were simultaneously cultured on the fungal culture media (sabouraud's dextrose agar with antibiotics) and were incubated in 37° and 25 °C. The growth of mucormycetes appeared within 7 to 10 days. On culture they showed greyish white cottony growth. After which Lactophenol Cotton Blue mount (LPCB) mount was prepared to see the characteristic morphology of the mucormycetes under the microscope.
Fig. 1.
a) Broad aseptate/pauci septate hyphae on KOH mount suggestive of mucormycosis. b) and c) mucorals on lactophenol cotton blue mount.
2.3. Radiological investigations
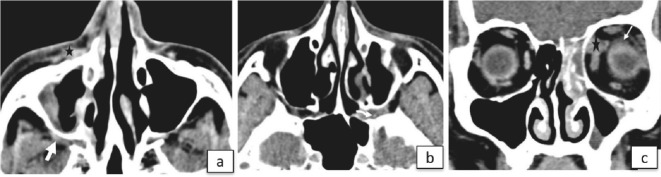
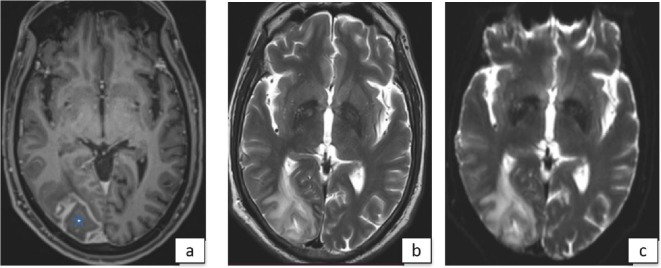
As CECT was used as the initial modality to evaluate a suspected case of COVID associated mucormycosis (CAM). MRI was reserved for patients with orbital apex and intracranial involvement, especially when CT findings were equivocal. Contrast enhanced CT scan of Sino nasal region and orbit was performed after intravenous bolus injection of non- ionic iodinated contrast administered at a dose 1–1.25 ml/kg body weight using thin collimation of 0.63 mm thickness. Multiplanar reconstruction along coronal and sagittal planes from these axial sets of images (Fig. 2 ). Inclusion of the cavernous sinus region was ensured in every case. MR examination of Sino nasal region and orbits was done using T1 weighted, T2 weighted and short tau inversion recovery (STIR) images in multiple planes followed by contrast enhanced T1 W fat saturated images using 3 mm thick slices (Fig. 3 ). MRI of the brain was also done when intracranial extension was suspected using T1 W, T2 W, Fluid attenuated inversion recovery (FLAIR), Diffusion images (DWI) and post contrast T1 W images. MR angiography TOF technique was done to assess the internal carotid artery and its branches (Fig. 4 ). Intracranial and intraorbital involvement on MRI scans are shown in Fig. 5 .
Fig. 2.
(a)Contrast enhanced axial CT scan in soft tissue window in a 61 year old male with mucormycosis shows soft tissue contents in right retro antral region (white arrow) with fat stranding and soft tissue contents in right preantral region (black star) (b)Contrast enhanced axial CT in soft tissue window in in a 33-year-old post COVID male patient with left sided CAM shows soft tissue contents in right sphenopalatine foramen extending to pterygopalatine fossa (curved arrow) (c)Contrast enhanced coronal CT in soft tissue window in a 28-year-old male with rhino ocular mucormycosis shows involvement of left orbit in form of soft tissue contents in superomedial part of extraconal space abutting the superior oblique and medial rectus muscle (black star) and fat stranding in intraconal compartment (white arrow).
Fig. 3.
Post contrast T1 fat saturated coronal(a) and axial image(b) in a 47-year-old male with right rhino-orbito-cerebral mucormycosis shows phlegmonous soft tissue content in right orbital apex (white arrow) encasing the optic nerve and extending into cavernous sinus which shows lack of enhancement and convex lateral margin (black arrow) The right optic nerve appears bulky and shows diffusion restriction suggestive of ischemia (c) (white arrowhead).
Fig. 4.
An irregular area of altered signal intensity is seen in right occipital lobe in the same patient as in Fig. 2. appearing hypointense on axial post contrast T1 fat saturated image (a) (white star) hyperintense on T2 weighted image(b) and showing peripheral diffusion restriction(c) suggestive of subacute infarct.
Fig. 5.
a) Intracranial spread of fungus; b) retrobulbar fungal abscess.
2.4. Histopathological investigations
The samples received in the pathology department were in two forms: formalin fixed tissue for histopathology and smears for cytology. Smears for cytology were prepared either by taking scrapings or from pus discharges along with tissue squashes. For histopathology tissue obtained was fixed in 10% neutral buffered formalin. The tissue received by grossed and processed routinely using a hustokinette for 12 h. Paraffin embedded blocks were prepared and sectioned on slides which in turn were stained with Hematoxylin and Eosin stain. The slides were examined under the microscope for fungal morphology and tissue reaction. Special stains like Silver Methenamine (SM) and Periodic Acid Schiff (PAS) were performed on unstained slides for confirming the diagnosis. Cytology samples were either dry fixed (air dried fixed in methanol) and stained with May Grunwald Giemsa or wet fixed (Ethanol fixed) and stained with Papanicolaou stain for initial screening followed by special staining with SM and PAS.
2.5. Medical and surgical management
Medical management included Injection Liposomal Amphotericin B, Posaconazole and Voriconazole, where the former two were given in histopathological proven mucormycosis and later for aspergillosis respectively.
Surgical intervention included Endoscopic approaches, Open approaches and combined approaches. The various surgeries conducted were Functional Endoscopic Sinus Surgery (FESS), total and partial maxillectomy, endoscopic orbital clearance and open exenteration. Every attempt was made to completely debride the dead tissues and reduce fungal load. Regular suction and clearance were done to clear the residual disease in the postoperative period.
Patients were discharged from the ward once there was no evidence of disease endoscopically with improved clinical features. Once discharged, patients were kept on oral posaconazole with weekly follow up for DNE.
3. Results
A total of 131 patients histopathological proven as invasive fungal rhinosinusitis were included in the study. Mean age was 52.7 ± 12.4 for males and 49.8 ± 10.6 for females. Out of 131 patients, 111 patients had prior history of SARS COVID 19 infection, confirmed with a positive RT-PCR report and the rest 20 patients had no such history. The mean duration for appearance of symptoms was 19 (10–28) days from the time of a COVID positive report. Out of 85 males and 46 females included in the study, 78 males and 33 females had a history of prior COVID infection. Patients' demographic details are depicted in Table 1 .
Table 1.
Demographic data, associated comorbidities, causative organisms, medical and surgical management outlines for the patients admitted for invasive fungal sinusitis.
| Variables | Number | Frequency (%) |
|---|---|---|
| Total cases | 131 | 100 (%) |
| Age (years) (mean ± SD) | 52.7 ± 12.4 (male) | 64.88 |
| 49.8 ± 10.6 (female) | 35.11 | |
| Gender | ||
| Males | 85 | 64.9 |
| Females | 46 | 35.1 |
| COVID status | ||
| Positive for SARS-COV 19 | 111 (33 females; 78 males) | 84.73 |
| Negative for SARS-COV 19 | 20 | 15.26 |
| Diabetes status | ||
| Diabetic | 101 | 77.09 |
| Nondiabetic | 30 | 22.90 |
| Comorbidities (other than diabetes) | ||
| Hypertension | 21 | 16.03 |
| Thyroid dysfunction | 7 | 5.34 |
| Coronary artery disease | 5 | 3.8 |
| Others | 37 | 28.24 |
| Days passed since COVID positive | 19 days (10–28) | – |
| Organism | ||
| Mucor | 122 | 93.12 |
| Aspergillus | 6 | 4.58 |
| Both | 3 | 2.29 |
| Steroid Therapy (only to COVID patients; n = 111) | ||
| Given | 67 | 60.36 |
| Not given | 44 | 39.63 |
| Steroid therapy (n = 67) | ||
| Methylprednisolone | 44 | 65.67 |
| Dexamethasone | 6 | 8.95 |
| Methylprednisolone and dexamethasone combined | 15 | 22.38 |
| Effcorlin | 2 | 2.98 |
| Surgery | ||
| Fess with debridement | 99 | 75.57 |
| Orbital exenteration | 20 | 15.26 |
| Open maxillectomy | 32 | 24.42 |
The most common comorbidity associated with Invasive fungal sinusitis was Diabetes Mellitus followed by Hypertension. A total of 101 patients were already known case of Diabetes whereas 30 patients had no history of diabetes at the time of admission. Out of known diabetics, 85 patients had a history of COVID infection and 16 had no history of COVID infection. Out of 30 patients who had no previous history of diabetes when investigated, 23 were found to have raised blood sugars in diabetic range and hence were included as newly diagnosed Diabetes mellitus. Out of these newly diagnosed Diabetes mellitus patients, 19 patients had COVID infection and 4 patients did not have COVID history.
Thus, there were in all only 20 patients without any history of COVID. It is important to note that 7 patients with previous history of COVID infection did not have any evidence of Diabetes mellitus, steroid intake or any other comorbidity. All patients were subjected for HbA1C testing which was 10.0 ± 2.0 SD in COVID positive patients and 9.8 ± 2.3 SD in COVID negative patients. Other comorbidities included thyroid dysfunction in 7 patients, coronary artery disease in 5 patients and 37 patients had other miscellaneous diseases not significant for our study (Table 2 ).
Table 2.
Investigation, management and final outcome of COVID associated and non-COVID Invasive fungal sinusitis.
| Variables | COVID positive patients (%) (n = 111) |
COVID negative patients (%) (n = 20) |
|---|---|---|
| HbA1C (mean ± SD) | 10.0 ± 2.0 | 9.8 ± 2.3 |
| Known diabetes | 85 (76.57) | 16 (80) |
| Newly diagnosed diabetes | 19 (17.11) | 4 (20) |
| Non-diabetic | 7 (6.30) | 0 |
| Antifungal therapy | ||
| Amphotericin B | 106 (95.49) | 20 (100) |
| Voriconazole | 5 (4.50) | 0 |
| Kidney function test | ||
| Deranged | 10 (9.0) | 3 (15) |
| Normal | 101 (90.99) | 17 (85) |
| Diagnostic nasal endoscopy | ||
| Pale mucosa | 12 (10.81) | 2 (10) |
| Mucopus | 28 (25.22) | 8 (40) |
| Black crusts | 52 (46.84) | 9 (45) |
| Normal | 19 (17.11) | 1 (5) |
| KOH mount | ||
| Aseptate hyphae | 68 (61.26) | 13 (65) |
| Septate hyphae | 24 (21.62) | 2 (10) |
| Normal | 19 (17.11) | 5 (25) |
| Radiological involvement | ||
| Sinonasal | 34 (30.63) | 5 (25) |
| Rhino orbital | 73 (65.76) | 13 (65) |
| Rhino orbitocerebral | 4 (3.60) | 2 (10) |
| Oxygen support | ||
| Yes | 30 (27.02) | 0 |
| No | 81 (72.97) | 20 (100) |
| Ventilator requirement | ||
| Yes | 6 (5.40) | 0 |
| No | 105 (94.59) | 20 (100) |
| Final outcome | ||
| Recovered | 104 (93.69) | 20 (100) |
| Worsened | 1 (0.90) | 0 |
| Fatal | 6 (5.40) | 0 |
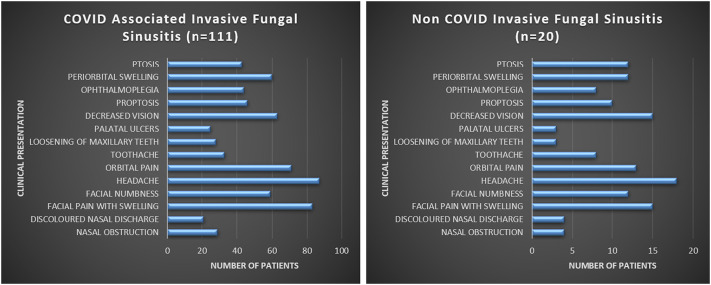
Steroids were received as a part of treatment in 67 patients infected with COVID 19. Among the types of steroids given, Methylprednisolone (MPS) was the most common steroid used in 44 patients followed by MPS and Dexamethasone combined which was given in 15 patients. Among the COVID positives, 30 patients received oxygen supplementation in any form and 6 patients had been admitted in ICU for COVID associated pneumonia. The most common clinical presentation remained Headache in both the groups followed by Facial pain or swelling. The graphical representation of clinical presentations is depicted in Fig. 6 . Some of the clinical pictures are shown in Fig. 7 .
Fig. 6.
Clinical presentation of COVID associated and non-COVID Invasive Fungal Sinusitis.
Fig. 7.
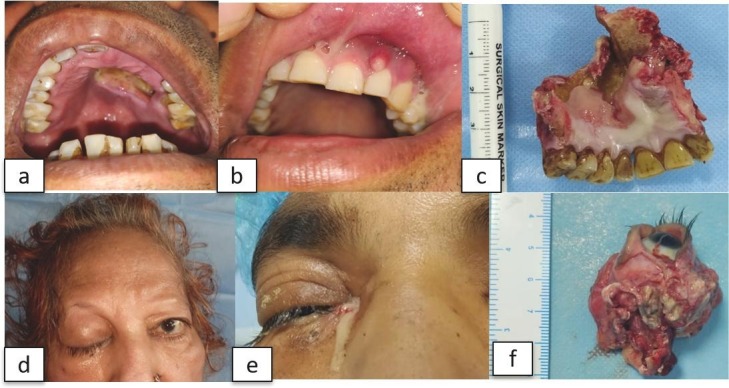
Clinical presentation a) palatal ulceration; b) gingival lesions; c) maxillectomy specimen; d) ptosis; e) orbital abscess; f) orbital exenteration specimen.
Diagnostic nasal endoscopy remained a useful minimally invasive procedure to diagnose invasive fungal sinusitis and obtain samples for fungal KOH testing (Fig. 8 ). Most common findings remained black crusts in 52 patients followed by mucopus in 28 patients in COVID positive group whereas in COVID negative group 9 had black crusts and 8 had mucopus. Comparing COVID positive and negative groups, the normally looking mucosa was in ratio of 19:1.
Fig. 8.
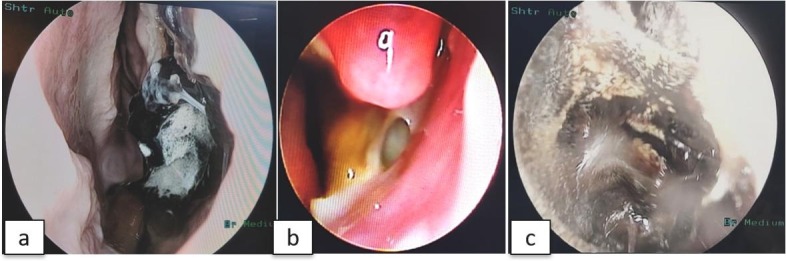
DNE a) Black crust middle turbinate; b) mucopus middle meatus; c) black crust, lateral nasal wall.
Radiological investigations classified the disease into 3 types among which 73 patients had rhino-orbital involvement, 34 had Sino nasal disease and 4 had Rhino-orbito-cerebral involvement in COVID positive group whereas this data was 13, 5 and 2 respectively in COVID negative group.
The administration of medical management depended on the histopathological report. The morphology of fungi was similar in both cytology and histology samples. The mucor has broad (typically 6- to 25-μm diameter), irregular, ribbonlike, non-septate (or sparsely septate) hyphae with irregular broad/right branching. (Fig. 9a and b) These findings were better highlighted on special stains. (Fig. 9c and d). The tissue reaction consisted of neutrophil infiltration, vessel invasion (Fig. 9e) and tissue infarction. Granulomatous reactions were also noted in a few cases. The aspergillus has narrow (typically 2.5 to 4.5-μm diameter) dichotomous branching hyphae at acute angle nearly 45° with frequent septations. Similar tissue reactions were noted as in mucor. Cases with dual infections included mucor with Aspergillus (Fig. 9f) and or sometimes Candida. The dominant species identified in histopathology was Mucorales in 122 patients and Aspergillus species in 6 patients while aspergillus and mucor species coexisted in 3 patients. Interestingly, in contradiction to histopathology report KOH mount presented a different story with aseptate hyphae in 81 patients, septate hyphae in 26 patients while 24 patients reported no fungal elements on KOH mount (Fig. 1).
Fig. 9.
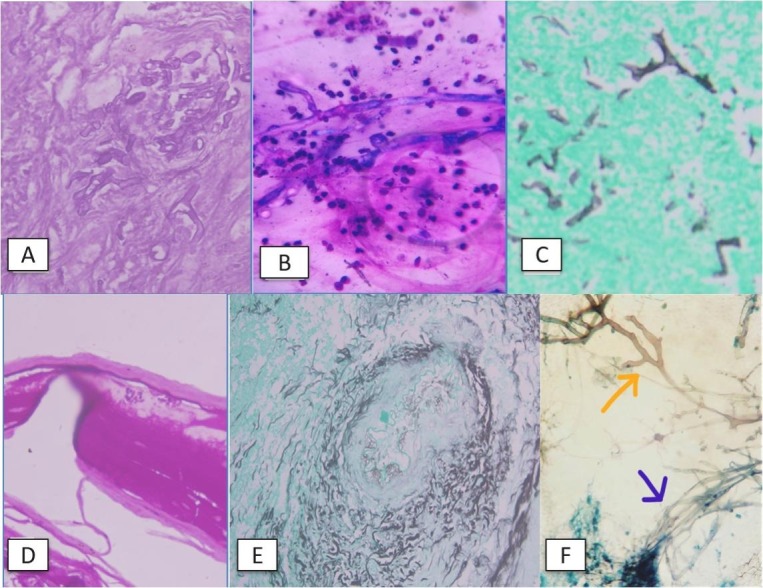
A): Histopathology image showing hyphae of mucor. Stain Hematoxylin and eosin, power 400×; B): Cytology image showing hyphae of mucor along with neutrophilic infiltrate. Stain MayGraunwald Giemsa, power 1000×; C): Histopathology image showing hyphae of mucor in Silver methenamine stain, power 400×; D): Histopathology image showing hyphae of mucor in PAS stain. Power 400×; E): Histopathology image showing vascular invasion. Stain SM power 400×; F): Cytology image showing dual infection; orange arrow mucor, blue arrow Aspergillus. Stain Papanicolaou; power 1000×. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
The medical management was started based on histopathology report. 125 patients received Liposomal Amphotericin B injections while 6 patients diagnosed with isolated aspergillosis received Voriconazole. Noteworthy point is that 3 patients with both the species coexisting received Liposomal Amphotericin only. We started Liposomal Amphotericin B empirically in all cases with clinical and DNE findings suggestive of invasive fungal sinusitis without waiting for a biopsy report or microscopy report. There was an acute shortage of Liposomal AMB during initial days when lipid complex AMB was used intermittently. Some of the patients developed severe drug reactions with lipid complex AMB when it was withdrawn. During the course of treatment all patients were monitored for kidney function, blood sugar levels and electrolytes.
Surgical treatment was aimed at debridement of dead necrotic tissues with removal of fungal debris. Surgical approach was planned after meticulous inter departmental discussions with radiology, ophthalmology and neurosurgery. Endoscopic debridement as a part of Functional Endoscopic sinus surgery was done in 99 patients. The difficult decision of orbital exenteration was taken only after the ophthalmology team advised to do so in order to clear the disease in an already blind eye. A total of 20 orbital exenterations were performed. Open maxillectomies included total, subtotal and partial maxillectomies in order to clear the disease and it was done in 32 patients. It is noteworthy that some patients did need combined procedures mentioned above in order to eradicate the disease.
Among 131 patients, 124 recovered, 1 worsened and 6 died. Out of 101 known diabetics, 98 recovered and 3 had fatal outcomes. Out of 23 newly diagnosed diabetics, 19 recovered, 1 worsened and 3 died. The 7 patients who were non diabetic with no COVID history recovered. The p value of Diabetes status with final outcome is 0.04 which is statistically significant. A total of 67 patients had a history of steroid intake out of which 64 recovered and 3 had fatal outcomes. 64 patients did not receive any form of steroid and 60 patients recovered, 1 worsened and 3 patients succumbed to the disease. The p value for the correlation between steroid intake and outcome was 0.555 which was statistically insignificant (Table 3 ).
Table 3.
Correlation of diabetes status and steroid intake with final outcome of the patients admitted for invasive fungal sinusitis.
| Final outcome |
Total | p-value | ||||
|---|---|---|---|---|---|---|
| Recovered | Worsened | Fatal | ||||
| Diabetes status | Present | 98 | 0 | 3 | 101 | 0.040 |
| Absent | 26 | 1 | 3 | 30 | ||
| Total | 124 | 1 | 6 | 131 | ||
| Steroid intake | Present | 64 | 0 | 3 | 67 | 0.555 |
| Absent | 60 | 1 | 3 | 64 | ||
| Total | 124 | 1 | 6 | 131 | ||
4. Discussion
The epidemiology of mucormycosis in India is different from European countries and the United States. Uncontrolled diabetes mellitus is the predominant risk factor in India and over- shadows other risk factors including haematological malignancy and organ transplantation which are major risk factors in developed countries [4], [5], [6]. Our study reveals that 94.65% of total Invasive Fungal sinusitis patients were diagnosed with Diabetes mellitus. This reinforces the fact that Diabetes is indeed the most common comorbidity associated with Invasive Fungal sinusitis. Indian population is more susceptible to develop Diabetes mellitus which is augmented by rapid socioeconomic development has caused explosive increase in number of Diabetes cases making India an epicentre of global diabetes pandemic [7]. There is a rise in cases of invasive fungal sinusitis globally but the rise is sharp in Indian Subcontinents India [8].
The percentage of Diabetics who acquired Invasive fungal sinusitis remained similar in COVID 19 infected and non-infected patients but startling observation was the occurrence of Invasive Fungal sinusitis in 7 non diabetic patients who had history of mild COVID19 infection, received no steroid as treatment without any other comorbidity. This is a very important observation which points towards the possible role of COVID19 infection in causing Invasive Fungal Sinusitis. The inhaled fungal spores are dealt by mature neutrophil but in COVID 19 infection a raised immature neutrophil count is unable to eliminate fungal spores thereby causing them the settle down and germinate into hyphae [9]. Recent studies also stressed on the fact that COVID 19 infection leads to an incompetent innate immune system [10], [11].
Long-term prospective studies, notably the Diabetes Control and Complications Trial (DCCT), the UK prospective Diabetes Study Group (UKPDS), and the Epidemiology of Diabetes Interventions and Complications (EDIC) study, have provided definite evidence that diabetic complications are directly related to mean glycemia value, as measured by the HbA1c concentration [12]. In this study, the average HbA1c values remained similar in both COVID19 infected and uninfected groups correlating with the similar percentage of diabetics in both the groups. The HbA1c values remained deranged in both the groups and were averaging around 10 indicating poorly controlled glycaemic control in these patients.
Critically ill COVID-19 patients have higher pro-inflammatory (IL-1, IL-2, IL-6, tumour necrosis alpha) and anti-inflammatory (IL-4, IL-10) cytokine levels, less CD4 interferon-gamma expression, and fewer CD4 and CD8 cells.9,37 This severe clinical situation increases the risk of invasive fungal infections [9].
Apart from diabetes mellitus, the impact of COVID 19 and its management on etiology of invasive fungal sinusitis makes this a unique study. Beginning in December 2019, a novel coronavirus (SARS-CoV-2) has caused an international outbreak of acute respiratory illness termed COVID-19 [1]. The severity of COVID-19 symptoms is highly variable, ranging from unnoticeable to life-threatening illness. Severe illness is more likely in elderly COVID-19 patients, as well as those who have certain underlying medical conditions. Patients with severe COVID-19 can develop a systemic inflammatory response that can lead to lung injury and multisystem organ dysfunction. It has been proposed that the potent anti-inflammatory effects of corticosteroids might prevent or mitigate these deleterious effects. According to recovery trial there is potential benefits of low-dose corticosteroids treatment in a subset of critically ill patients with COVID-19 pneumonia [2]. Thus, a short course of methylprednisolone in moderate to severe cases of COVID 19 has potential benefit in survival outcome and there is no role in mild cases [13]. In our study of 111 COVID 19 positive patients, 60.36% patients received steroids as a part of treatment. These patients were already diabetic and addition of steroids as a desperate measure during COVID pandemic may have put the patients in prolonged hyperglycaemic states predisposing them to invasive fungal sinusitis. It is a well-known fact that glucocorticoids can cause unanticipated hyperglycemia thus causing adverse metabolic effects [14]. The most common steroid received by patients was methylprednisolone followed by prednisolone and effcorlin combined. There is no controlled study comparing methylprednisolone with dexamethasone but efficacy is believed to be similar [15]. The overuse of high-dose glucocorticoids and the administration of highly immunosuppressive drugs such as inhibitors of the Janus kinase inhibitors or IL-6 receptor inhibitors to treat patients with the coronavirus disease 2019 (COVID-19) are responsible in part for the increasing number of life-threatening opportunistic infections identified in this patient population [16]. The second wave of covid in India was like a tsunami and the health infrastructure in many cities were overwhelmed with no beds or oxygen available. In sheer desperation of avoiding the need of hospitalization covid positive patients started steroids even for very mild or asymptomatic disease. With little regulatory control on prescription practices or disbursement of drugs in India there was overuse of many medicines without any definite indications in covid. There were many prescriptions freely circulated on social media. Patients with asymptomatic or mild covid symptoms, took a combination of 7–8 drugs including ivermectin, doxycycline, azithromycin, zinc, favipiravir and steroids just to avoid hospitalization and oxygen requirement. Classically, uncontrolled diabetes mellitus, neutropenia, and corticosteroid therapy are known risk factors for mucormycosis. There is an urgent need to reconsider the careful use of steroids drugs in patients with severe COVID-19 due to the high prevalence of underlying comorbidities in these patients, including diabetes mellitus, haematological malignancies, end-stage kidney disease, and organ transplant recipients [16]. In this study, the most common clinical presentation in both the COVID19 infected and non-infected groups remained headache followed by facial pain and swelling. It implied the fact that the nature of disease remained the same clinically in both the groups. Frank symptoms like palatal discoloration/ulceration, palatal perforation, diplopia, proptosis, ophthalmoplegia and ptosis are clear indications for starting antifungal therapy without histopathological report.
DNE followed by nasal swabs for KOH mount was done for every patient which showed aseptate hyphae in 61.83%, septate hyphae in 19.84% and normal in 18.32% patients. There are many cases where KOH microscopy could not detect the fungus but histopathology could demonstrate the presence of fungal elements. This is mainly due to inadequate fungal hyphae, trapped fungal hyphae in mucosa preventing it to come in contact with stains, inter observer variability and improper sampling technique [17].
Black crusts in the nasal cavity were the dominant finding on DNE in both the groups followed by mucopus in middle meatus. The finding of mucopus was slightly higher in COVID 19 non infected group of 40% compared to 25.22% in COVID infected group while it remained the same for black crusts in both the groups. The presence of dark necrotic mucosa and mucopus are one of the most common finding on DNE [3].
There are many cases where KOH microscopy could not detect the fungus but histopathology could demonstrate the presence of fungal elements. This is mainly due to inadequate fungal hyphae on surface of mucosa, trapped fungal hyphae in mucosa preventing it to come in contact with sampling brush and improper sampling technique [17].
Considering this fact, the medical treatment was tailored based on the histopathology report rather than KOH microscopy. The role of KOH microscopy remained only as augmentation of clinical, radiological and histopathological diagnosis. 93.12% patients were diagnosed with mucormycosis who received injection liposomal AMB while 4.58% had aspergillosis who were treated with voriconazole. It is noteworthy that 2.29% i.e., 3 patients out of 131 patients had both the species on histopathology and these patients received Liposomal AMB.
For decades, amphotericin B deoxycholate has been the standard therapy for invasive aspergillosis [18]. Now various studies have suggested that Voriconazole is drug of choice for aspergillosis but it lacks anti mucormycosis activity [19].
Rhino orbital involvement being the most commonly classified variant in radiological scans suggests the early involvement of orbit in invasive fungal sinusitis. When COVID positive and negative groups were compared we did not find any change in disease classification. The history of oxygen support and ICU admission did not relate to the occurrence of invasive fungal sinusitis or outcome of the disease in this study.
93.69% patients recovered in COVID positive group and 100% recovered in COVID negative group. 6 patients died who belonged to COVID positive group. The mortality of invasive fungal sinusitis mainly mucormycosis approaches 50% which makes it a devastating disease [12]. It is worth mentioning that we started Liposomal aAMB early if there was a strong suspicious of invasive fungal sinusitis clinically or radiologically. We did not wait for histopathology report for tissue samples taken before surgery and based on clinical and radiological evidence patients were taken for surgery urgently. These factors might have improved the clinical outcome in favour of patient survival.
4.1. Limitations
There was limited data to establish the role of isolated COVID19 infection in invasive fungal sinusitis. The exact dose of steroid received by the patients during covid illness could not be found due to lack of prescriptions and any documentation.
5. Conclusion
It can be concluded that ROCM upsurge seen in the context of COVID-19 in India was mainly seen in patients with uncontrolled diabetes, a dysfunctional immune system due to SARS-COV-2 infection and injudicious use of corticosteroids. Diabetes mellitus is the most common comorbidity associated with ROCM. COVID 19 itself causes immune dysregulation which predispose to fungal infections but in combination with diabetes mellitus the risk increases many folds. Also, we cannot find any significant role of oxygen therapy or ICU admission as one of the etiological factors for mucor. Strict blood sugar control, early anti-fungal administration and prompt surgical intervention do reduce the mortality and improve survival outcome as seen in this study which is our ultimate goal.
Acknowledgements
We acknowledge the support received from all the residents of ENT department of Maulana Azad Medical College, New Delhi, India and Dr. Sonal Katyal, Senior Research Fellow, All India Institute of Medical Sciences, for statistical analysis and writing.
References
- 1.Singh V.P., Bansal C., Kaintura M. Sinonasal Mucormycosis: A to Z. Indian J Otolaryngol Head Neck Surg. 2019;(s3):1962–1971. doi: 10.1007/s12070-018-1384-6. [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ismaiel W.F., Abdelazim M.H., Eldsoky I., Ibrahim A.A. 2020. Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID- 19 . The COVID-19 resource centre is hosted on Elsevier Connect , the company ’ s public news and information. (January) [Google Scholar]
- 3.Bond S. These organisms are. 2021. The genera in the order Mucorales cause most human infection; pp. 1–34. [Google Scholar]
- 4.Skiada A., Pagano L., Groll A., Zimmerli S., Dupont B., Lagrou K., et al. Zygomycosis in Europe: analysis of 230 cases accrued by the registry of the european Confederation of Medical Mycology (ECMM) working group on zygomycosis between 2005 and 2007. Clin Microbiol Infect. 2011;17(12):1859–1867. doi: 10.1111/j.1469-0691.2010.03456.x. [DOI] [PubMed] [Google Scholar]
- 5.Kontoyiannis D.P., Yang H., Song J., Kelkar S.S., Yang X., Azie N. Prevalence, clinical and economic burden of mucormycosis-related hospitalizations in the United States: a retrospective study. BMC Infect Dis. 2016;16:1–6. doi: 10.1186/s12879-016-2023-z. [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chakrabarti A., Singh R. Mucormycosis in India: unique features. Mycoses. 2014;57(s3):85–90. doi: 10.1111/myc.12243. [DOI] [PubMed] [Google Scholar]
- 7.Unnikrishnan R., Anjana R.M., Mohan V. Diabetes mellitus and its complications in India. Nat Rev Endocrinol. 2016;12(6):357–370. doi: 10.1038/nrendo.2016.53. [DOI] [PubMed] [Google Scholar]
- 8.Prakash H., Chakrabarti A. Global epidemiology of mucormycosis. J Fungi. 2019;5(1) doi: 10.3390/jof5010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta A., Sharma A., Chakrabarti A. The emergence of post-COVID-19 mucormycosis in India: can we prevent it? Indian J Ophthalmol. 2021;69(7):1645–1647. doi: 10.4103/ijo.IJO_1392_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schulte-Schrepping J., Reusch N., Paclik D., Baßler K., Schlickeiser S., Zhang B., et al. Severe COVID-19 is marked by a dysregulated myeloid cell compartment. Cell. 2020;182(6):1419–1440. doi: 10.1016/j.cell.2020.08.001. e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parackova Z., Zentsova I. Disharmonic inflammatory signatures in COVID-19. Cells. 2020;2:1–17. doi: 10.3390/cells9102206. (December 2019) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weykamp C. HbA1c: a review of analytical and clinical aspects. Ann Lab Med. 2013;33(6):393–400. doi: 10.3343/alm.2013.33.6.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fadel R., Morrison A.R., Vahia A., Smith Z.R., Chaudhry Z., Bhargava P., et al. Early short-course corticosteroids in hospitalized patients with COVID-19. Clin Infect Dis. 2020;71(16):2114–2120. doi: 10.1093/cid/ciaa601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hwang J.L., Weiss R.E. Steroid-induced diabetes: a clinical and molecular approach to understanding and treatment. Diabetes Metab Res Rev. 2014;30(2):96–102. doi: 10.1002/dmrr.2486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prakash H., Ghosh A.K., Rudramurthy S.M., Singh P., Xess I., Savio J., et al. A prospective multicenter study on mucormycosis in India: epidemiology, diagnosis, and treatment. Med Mycol. 2019;57(4):395–402. doi: 10.1093/mmy/myy060. [DOI] [PubMed] [Google Scholar]
- 16.Soiza R.L., Donaldson A.I.C., Myint P.K. Vaccine against arteriosclerosis: an update. Ther Adv Vaccines. 2018;9(6):259–261. doi: 10.1177/2042098618769568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singh A.K., Gupta P., Verma N., Khare V., Ahamad A., Verma V. Fungal rhinosinusitis: microbiological and histopathological perspective. J Clin Diagn Res. 2017;11(7) doi: 10.7860/JCDR/2017/25842.10167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Virchow-klinikum C., Hutchinson F., Diego S., State W., Diseases I, Hospital G . Of invasive aspergillosis. 347(6) 2007. pp. 408–415. [Google Scholar]
- 19.Samsonova M.V., Chernyayev A.L., Lebedin Y.S., Mikhaylichenko K.Y., Polivanova A.E. Pulmonary mucormycosis. Pulmonologiya. 2018;28(2):243–247. [Google Scholar]