Abstract
The purpose of this study was to better understand the number and types of social needs experienced by Medicaid beneficiaries with type 2 diabetes, and how their social needs are associated with key health indictators. Also examined were factors that influence patients’ interest in navigation services for health and social needs to inform future interventions and service delivery. The study expands upon prior research, much of which has focused on only one social need (e.g., food insecurity) or one health outcome. The hypothesis was that among individuals with type 2 diabetes, those with a greater number of social needs would report more health-related problems and be more interested in receiving social needs navigation services. Participants completed a cross-sectional survey by phone (n=95) or online (n=14). Most (85%) reported having at least one social need (M=2.5, SD=2.2), most commonly not having enough money for unexpected expenses (68%) or necessities like food, shelter and clothing (31%), medical costs (24%), and utilities (23%). Results supported our comprehensive conceptual model. Having more social needs was associated with greater perceived stress, diabetes distress, problems with sleep and executive and cognitive functioning, less frequent diabetes self-care activities, more days of poor mental health and activity limitations, worse self-reported health and more hospitalizations. Number of social needs also was positively associated with interest in having a social needs navigator. Social needs were not associated with days of poor physical health, BMI, self-reported A1C, or smoking status. Social needs were associated with a wide range of indicators of poor health and well-being. Participants with the greatest social need burden were most open to intervention.
Keywords: low-income population, social determinants of health, holistic health, type 2 diabetes, patient navigators, health education, health services marketing
Introduction
The self-management burden of type 2 diabetes is significant. Individuals are often overwhelmed with dietary restrictions, self-care responsibilities, and concerns about disease complications (Shirazian et al., 2016).
Self-management of diabetes and related health outcomes are adversely impacted by social needs, including food, shelter, utilities, etc. (Vijayaraghavan, Jacobs, Seligman, & Fernandez, 2011). Most previous research has focused on single needs such as food insecurity, which has been related to greater cost-related medication non-adherence, worse self-reported health (Sattler, Lee, & Bhargava, 2014), depression (Montgomery, Lu, Ratliff, & Mezuk, 2017), poor glycemic control (Berkowitz et al., 2015; Lyles et al., 2013), less fruit and vegetable intake, and lower diabetes self-efficacy (Lyles et al., 2013). However, other studies that report dose-response relationships suggest that it is important to consider how multiple or cumulative needs affect health (Andermann, 2018; Berkowitz et al., 2015; Bisgaier & Rhodes, 2011; Kalousova, Xiao, & Burgard, 2019; Katz et al., 2018; Kreuter et al., In press).
Figure 1 illustrates potential mediating and bi-directional associations between social needs and health-related outcomes. Specifically, Figure 1 shows how social needs can create barriers to effective self-management (e.g., planning, scheduling, follow-through) that impede the performance of health behaviors (e.g., eating healthy, exercising, glucose monitoring, physician visits) that prevent negative health outcomes and quality of life. Although we included diabetes-specific behaviors and outcomes, the model can be applied broadly across other health conditions. A growing number of studies support the benefits of addressing social needs on health behaviors, health outcomes, and healthcare utilization (Bachrach, Pfister, Wallis, & Lipson, 2014; Fitzpatrick-Lewis et al., 2011; Sandberg et al., 2014); however, no single study has tested a comprehensive model.
Figure 1.
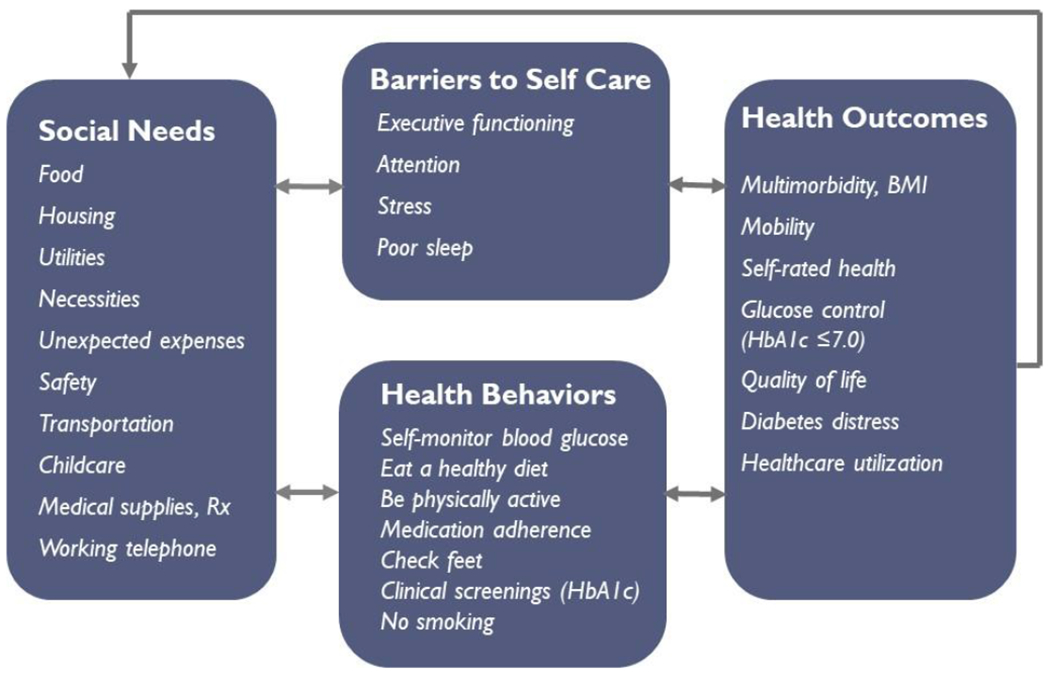
Conceptual model of how social needs impact health outcomes applied to type 2 diabetes
Although social needs screening of patients by medical providers and organizations are increasing, there is considerable variability in the measures, procedures, and completion rates (Fraze, Lewis, Rodriguez, & Fisher, 2016; Gottlieb, Garcia, Wing, & Manchanda, 2016). Large Medicaid managed care organizations (MCOs) are especially well-positioned to provide social needs screening and intervention programs to members. Medicaid MCOs have the added benefit of being able to provide services and collect data on members statewide compared to programs delivered through individual clinics or health systems. Medicaid MCOs have models for developing partnerships, applying alternative payment models, and sharing data across systems to address social determinants and impact health, but administrative, financial, and privacy challenges do exist (Daniel-Robinson & Moore, 2019). In addition to physical health care management programs, MCOs may provide navigation services to help address members’ social needs. Building on patient navigation programs that seek to improve patients’ health outcomes (Ali-Faisal, Colella, Medina-Jaudes, & Scott, 2017), social needs navigation seeks to alleviate patients’ social needs by helping patient’s access government or community programs and by providing regular follow-up and counseling to reduce barriers to self-care. Navigation services that resolve social needs facilitate opportunities for members to engage in healthy behaviors and improve health outcomes longer-term (Figure 1). Further, when members are not in a state of acute need, navigators can offer behavioral coaching and coordinate with the member’s physician as needed to address holistic health goals and recommended healthcare visits.
The purpose of this study was to (1) examine the feasibility of assessing social needs among Medicaid beneficiaries outside the point-of-care, and (2) expand previous research that has focused on only one social need (e.g., food insecurity) or one outcome, to better understand the number and types of social needs experienced, and their associations with various health indictators. Also, to inform future interventions and service delivery offered by MCOs, we examined factors that influence patients’ interest in health and social needs navigation services. The authors hypothesized that individuals with type 2 diabetes with a greater number of social needs would also report a variety of negative health-related outcomes and be more interested in receiving navigation services.
Method
Study Design
From June 22 to October 10, 2017, a cross-sectional survey was administered to adult Medicaid beneficiaries from Louisiana Healthcare Connections (LHCC), the state’s largest Medicaid managed care health plan. The goal was to survey 100 members to assess the feasibility of the research team to contact and enroll health plan members with type 2 diabetes into a research study and to inform protocols for conducting a future intervention trial to address social needs and health.
Target population and recruitment.
The health plan identified 10,276 members ages 18-75 with type 2 diabetes (members with type 1 diabetes and pregnant women with gestational diabetes were excluded). The research team selected a random subsample of 2500 LHCC members to recruit by telephone to invite their participation, confirm eligibility, obtain verbal informed consent and complete the survey. To maximize recruitment resources, research staff prioritized initiating new calls over making repeated calls to the same member. Voice messages were left when possible, although few individuals returned the call. Those completing the survey received a $25 gift card.
Limited study resources necessitated the exclusion of anyone who could not complete the survey in English. To minimize participant burden, the survey took less than 30 minutes to complete and participants were allowed to complete the survey online if preferred. All study materials and procedures were approved by the Institutional Review Board (IRB) at Washington University in St. Louis, the State of Louisiana Department of Health and Hospitals IRB, and by the health plan.
Survey respondents.
Interviewers made at least one phone call to 1,761 health plan members. Of those attempted to be reached, 33% had wrong or disconnected phone numbers. A total of 309 members were reached. Of those, four were excluded after reporting they did not have diabetes; 173 expressed interest in the study (56%), and 109 of those interested provided verbal consent and participated in the survey (63%; 102 completed the full survey).
Survey measures.
The selection of constructs to be measured in the survey (Table 1) was informed by the conceptual model in Figure 1. Standard measures of all constructs were used whenever possible. For all aggregate measures, higher scores reflect higher levels of the construct being measured.
Table 1.
Characteristics of survey respondents (N=109)
| Sample characteristics | N | % or M (SD) |
|---|---|---|
| Age (range 25-65 years) | 108 | M=50 (SD=10) |
| Female | 73 | 67% |
| Race | ||
| Black/African American | 54 | 50% |
| White | 40 | 37% |
| Other | 10 | 9% |
| Married or living with a partner | 31 | 28% |
| Have any children (age <18) at home | 39 | 36% |
| Education | ||
| Less than high school | 30 | 28% |
| High school graduate | 40 | 37% |
| Advanced training or degree | 34 | 31% |
| Employment status | ||
| Working for pay (part or full time) | 22 | 20% |
| Looking for work | 16 | 15% |
| Disabled | 52 | 47% |
| Other | 15 | 14% |
| Annual pre-tax household income | ||
| <$10,000 | 60 | 55% |
| $10,000-$19,999 | 18 | 17% |
| >$20,000 | 12 | 11% |
| Social needs | ||
| Total number (sum) | 104 | M=2.5 (SD=2.2) |
| Not enough money to deal with unexpected expenses | 74 | 68% |
| Trouble finding or paying for childcare if you need it | 13 | 36%† |
| Not enough money for necessities like food, shelter, and clothing | 34 | 31% |
| Problems paying for your medical care or medicines | 26 | 24% |
| Unable to pay for utilities like gas, water, and electricity | 25 | 23% |
| Unsafe neighborhood | 22 | 20% |
| Not sure self and others in your home will not get enough to eat | 20 | 18% |
| No reliable transportation | 18 | 17% |
| No working phone | 11 | 10% |
| No place to stay | 8 | 7% |
| Not enough space for everyone in your home | 8 | 7% |
| Someone will threaten to hurt you physically | 4 | 4% |
| Body Mass Index | ||
| Underweight/normal weight | 9 | 8% |
| Overweight | 26 | 24% |
| Obese | 64 | 59% |
| Age at diabetes diagnosis | 106 | M=41 (SD=13) |
| Had A1C tested in past year (at least once) | 100 | 92% |
| Most recent A1c test result | ||
| ≤7.0 | 27 | 25% |
| 7.1 – 8.0 | 12 | 11% |
| ≥ 8.0 | 27 | 25% |
| Don’t know | 39 | 36% |
| Diabetes self-care activities (daily, in past 7 days) | ||
| Checked feet | 76 | 70% |
| Checked blood glucose at least once | 70 | 64% |
| Checked blood glucose as recommended | 54 | 50% |
| Followed a healthful eating plan | 45 | 41% |
| Ate 5+ servings of fruit & vegetables | 42 | 39% |
| Participated in 30+ minutes of physical activity | 38 | 35% |
| Checked inside of shoes | 33 | 30% |
| Did not eat high fat foods (red meat, full-fat dairy) | 21 | 19% |
| Participated in a specific exercise session | 19 | 17% |
| Comorbid conditions (M=2.5; SD=1.4) Range 0-6 | 97 | 89% |
| High blood pressure | 82 | 75% |
| Depression | 38 | 35% |
| Heart disease | 26 | 24% |
| Asthma | 29 | 27% |
| Other | 80 | 73% |
| Hearing problems or hearing aids | 16 | 15% |
| Vision problems or glasses/contacts | 68 | 62% |
| Mobility problems or cane/walker | 38 | 35% |
| Overall self-rated health | ||
| Excellent/Very Good | 8 | 7% |
| Good | 22 | 20% |
| Fair | 44 | 40% |
| Poor | 27 | 25% |
| CDC Healthy Days measure (N, % any days) | ||
| Physical illness or injury (M=9; SD=11) | 57 | 52% |
| Mental health problems (M=8; SD=11) | 51 | 47% |
| Interruption of activities (M=9; SD=11) | 38 | 35% |
| Did not get enough sleep (M=12; SD=12) | 69 | 63% |
| Smoking status | ||
| Never | 48 | 44% |
| Former | 29 | 27% |
| Current | 31 | 28% |
| Has a regular doctor | 98 | 90% |
| Any self-reported primary care visits in past year (M=7.9, SD=7.5) | 98 | 90% |
| Any self-reported ED visits in past year (M=1.8, SD=3.3) | 56 | 51% |
| Any self-reported hospitalizations in past year (M=0.7, SD=1.3) | 39 | 36% |
| Perceived stress scale (range 1-5) | 106 | M= 2.5 (SD=1.0) |
| Diabetes distress scale score (range 1-5) | 106 | M= 2.0 (SD=1.1) |
| Cognitive Function problems scale (range 1-4) | 104 | M= 1.7 (SD=0.8) |
| Executive Function problems scale (range 6-24) | 104 | M= 11.2 (SD=5.3) |
Only 13 respondents needed childcare of the 36 who had children under age 18 living at home
Note. Percentages of N=109 may not equal 100 due to rounding and missing data.
Legend. M=Mean, SD=Standard deviation
Social needs were measured with 12 items assessing the likelihood that social needs related to food, housing, transportation, safety, and money for utilities, medications, necessities, unexpected expenses, and childcare would be met in the next month (Kreuter, McQueen, Boyum, & Fu, 2016). All items are listed in Table 1. Although most response options used a 4-point scale (1=very unlikely to 4=very likely), one item assessing space in the home included three response options: not enough space, about the right amount, too much space. For each item, responses were dichotomized as likelihood of being met or unmet, then a sum score (0-12) was created to reflect total social needs.
Diabetes history was measured by age at diagnosis, current use of pills (yes/no) and/or insulin (yes/no) for their diabetes, number of A1C tests in the past year, and value of the latest A1C result (≤7.0, 7.1-8.0, ≥8.1, don’t know).
Cognitive function was measured with 4-items (α=.86) assessing current difficulty with activities such as “reading and following complex instructions” and “planning for and keeping appointments” (National Institute of Neurological Disorders and Stroke (NINDS), March 2015). Response options ranged from 1=not at all to 4=very much, and a mean score (1-4) is reported. Using the same response options, executive function was measured with 6 items (Buchanan et al., 2010) (α=.92) assessing participants’ usual experience with problems with attention such as “concentrating on a task” and “learning new tasks or instructions;” a sum score (6-24) of responses is reported.
Perceived stress in the past month was measured using Cohen’s 4-item global measure (α=.75) (Cohen, Kamarck, & Mermelstein, 1983). Response options range from 0=never to 5=very often. Diabetes distress in the past month was measured using a 17-item scale (α=.94) where severity is rated 1=not a problem to 6=very serious problem (Polonsky et al., 2005). Mean scores are reported.
Diabetes self-management was measured using the 10-item Diabetes Self-care Activities Scale (Toobert, Hampson, & Glasgow, 2000) assessing the frequency of specific behaviors in the last 7 days (e.g., follow healthy diet, exercise, blood glucose testing, foot care). A mean score is reported.
CDC’s Healthy Days Measure (4 items) assessed self-rated health (poor-excellent), number of days in the past 30 days when physical and mental health was not good, and days that poor physical or mental health restricted usual activities. An additional item measured number of days in the past 30 days of insufficient sleep (Centers for Disease Control and Prevention, 1993).
Using a brief self-report measure of comorbidity (Groll, To, Bombardier, & Wright, 2005), participants were asked whether a doctor had ever told them they had each of 9 specific conditions (e.g., high blood pressure, asthma, cancer, depression) and any “others” they reported. A sum score of chronic conditions was used (0-9). Participants also reported their height and weight, which were used to estimate body mass index (Centers for Disease Control and Prevention).
Several questions were adapted from health plan assessments. One question determined self-reported smoking status as former, current or never. Self-reported healthcare access (having a regular physician, frequency of physician visits, total number of emergency department (ED) visits and hospitalizations in the past year) also was measured.
Additional questions were developed specifically for this study and measured participants’: 1) prior experience with individuals who assisted with their diabetes care (7 job titles were assessed and participants could report “others” in open-ended responses that were recoded into categories); responses were summed across categories then dichotomized to reflect any vs. no help from others for their diabetes care; 2) prior participation in “a class or workshop on how to manage your diabetes yourself”, and 3) interest in having a navigator assist with their health and 4) social needs. Responses for each of these four items were coded yes vs. no/don’t know.
Socio-demographic measures included standard items from national surveys including age, sex, race/ethnicity, marital status, number of children (<18 years) living at home, education, employment status, and annual household income before taxes.
Data analysis.
To better understand the number and types of social needs experienced, descriptive statistics were used to summarize participants’ responses across survey items. Although the recruitment goal was only to survey 100 people for feasibility purposes, power calculations showed that we had over 80% power to detect small (0.25) associations with N=100 (Faul, Erdfelder, Lang, & Buchner, 2007). To examine the variety of associations between social needs and health outcomes, bivariate associations between continuous survey measures were examined with Pearson correlation coefficients. To examine correlates of participants’ interest in navigation for health and social needs, individual bivariate logistic regression analyses were performed. Multivariable analyses were not conducted due to the small sample size and the large number of covariates. Analyses of survey data were conducted with SPSS software (version 24).
Results
Survey results
Table 1 reports sample characteristics. Participants did not differ from non-participants on age or gender, but no further information was collected by the research team about non-participants. Participants ranged in age from 25 to 65 years old. Most were female (67%) and African American (50%) or White (37%); 28% reported less than a high school education and most (55%) reported an income <$10,000.
Over half of participants (58%) reported having 2 or more social needs; only 15% reported none of the 12 social needs. The most commonly reported social need was not having enough money to deal with unexpected expenses (68%), followed by paying for childcare (where applicable), necessities, medical care/medicines, and utilities.
Most participants were obese (59%) or overweight (24%), and many were taking pills (75%) and/or insulin (46%) for their diabetes. Although most reported having their A1C checked in the past year (92%), 36% didn’t know the result. Only one person reported doing all 9 diabetes self-care behaviors each day; median = 3.
Most participants (89%) reported at least one chronic condition in addition to diabetes (Table 1). Most participants reported their health as fair (40%) or poor (25%) and had experienced insufficient sleep (63%) and interruptions of usual activities due to poor mental and/or physical health (55%) in the past 30 days. One in four (28%) were current smokers. Most survey respondents reported having a regular doctor (90%) and had been seen by a doctor in the past year. Participants reported low to moderate stress, diabetes-specific distress, and problems with cognitive function.
Table 2 shows the patterns of association between social needs and health-related variables in the conceptual model, as well as correlations between model variables. Having more social needs was significantly associated with having more problems with cognitive and executive functioning, greater stress, diabetes specific distress, days of poor mental health, activity limitations and sleep problems, worse diabetes self-care, and more hospitalizations.
Table 2.
Spearman correlations among continuous survey measures (N=109)
| Needs | Cog | Exec. | Stress | Distress | Phy | Mental | Active | Sleep | Self-care | Health | BMI | Chronic | ED | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Social needs (sum) | ||||||||||||||
| Cognitive function problems | .28*** | |||||||||||||
| Executive function problems | .24* | .70*** | ||||||||||||
| Perceived stress | .36*** | .46*** | .51*** | |||||||||||
| Diabetes distress | .27** | .55*** | .61*** | .49*** | ||||||||||
| Physical health (bad days) | .15 | .39*** | .35*** | .45*** | .35*** | |||||||||
| Mental health (bad days) | .23* | .44*** | .52*** | .57*** | .57*** | .57*** | ||||||||
| Activity limitations | .29* | .52*** | .56*** | .52*** | .40*** | .30* | .58*** | |||||||
| Insufficient sleep (days) | .21* | .44*** | .45*** | .43*** | .40*** | .61*** | .63*** | .43*** | ||||||
| Diabetes self-care | −.30** | −.26** | −.31*** | −.29** | −.37*** | −.13 | −.20* | −.19 | −.18 | |||||
| Health status (poor-excellent) | −.13 | −.32*** | −.45*** | −.44*** | −.52*** | −.34*** | −.51*** | −.24* | −.38*** | .30** | ||||
| BMI score | −.03 | .10 | .18 | .03 | .20* | .05 | .11 | .01 | .16 | −.27** | −.35*** | |||
| Chronic conditions | −.03 | .27** | .33*** | .16 | .27** | .27** | .39*** | .26* | .27** | −.28** | −.43*** | .34*** | ||
| ED visits | .16 | .09 | .13 | −.02 | .16 | .19 | .18 | .18 | .10 | .02 | −.20* | −.03 | .22* | |
| Hospitalizations | .26** | .11 | .13 | .08 | .13 | −.02 | .08 | .38*** | −.04 | .07 | −.12 | −.03 | −.01 | .57*** |
p<0.05
p< 0.01
p < 0.001
Most participants (79%) reported receiving some kind of help with their diabetes. This support was most commonly from a nutritionist (60%), diabetes educator (54%), nurse outside of a doctor’s visit (27%), friends or family (27%), case manager (17%), counselor or psychologist (16%), social worker (13%), lay navigator (6%) or other source (39%).
Many participants were interested in having a navigator to help them with health needs (59%) or social needs (49%); 38% wanted both and 24% wanted neither. Table 3 shows variables that were independently associated with greater interest in having a social needs navigator including having more social needs, problems with cognitive functioning, stress, worse overall health, more days of poor physical and mental health and sleep problems, current smoking, and more ED visits.
Table 3.
Participant interest in navigator services, significant bivariate associations from a series of independent bivariate logistic regression analyses (N=109)
| Want social needs navigator (vs. Not) | Want health navigator (vs. Not) | |||
|---|---|---|---|---|
|
| ||||
| OR | 95% CI | OR | 95% CI | |
| Sum of social needs | 1.52 | 1.19-1.94 | 1.15 | 0.94-1.41 |
| Cognitive function problems | 1.70 | 1.01-2.85 | 2.36 | 1.21-4.60 |
| Executive function problems | 1.08 | 1.00-1.17 | 1.12 | 1.02-1.23 |
| Stress | 1.73 | 1.14-2.62 | 1.88 | 1.19-2.97 |
| Diabetes distress | 1.45 | 0.97-2.15 | 2.32 | 1.33-4.05 |
| Diabetes self-care | 0.80 | 0.59-1.08 | 0.75 | 0.54-1.04 |
| Overall health (poor-excellent) | 0.57 | 0.36-0.89 | 0.59 | 0.38-0.93 |
| Poor physical health days | 1.08 | 1.03-1.13 | 1.03 | 0.99-1.07 |
| Poor mental health days | 1.04 | 1.01-1.08 | 1.04 | 1.00-1.09 |
| Activity limitations | 1.05 | 0.99-1.10 | 1.02 | 0.97-1.08 |
| Poor sleep | 1.04 | 1.00-1.08 | 1.04 | 1.00-1.08 |
| Current smoker vs. non-smoker | 3.11 | 1.21-7.95 | 1.27 | 0.50-3.20 |
| Comorbidity sum | 1.30 | 0.98-1.74 | 1.12 | 0.83-1.50 |
| BMI score | 1.04 | 0.99-1.08 | 1.05 | 1.00-1.10 |
| ED visits | 1.29 | 1.03-1.62 | 0.99 | 0.87-1.12 |
| Hospitalizations | 1.42 | 0.98-2.08 | 1.16 | 0.82-1.64 |
Greater interest in a health navigator was independently associated with greater problems with cognitive and executive functioning, stress, diabetes distress, and poor sleep in a series of bivariate analyses (Table 3). Notably, being in better health was associated with less interest in either a social needs or health navigator. Greater interest in having a health navigator was also related to interest in having a social needs navigator; OR=4.96 (95% CI: 2.03-12.13) p<.001.
Discussion
This study extends prior work and supports the conceptual model by describing multiple social needs and their associations with a range of health-related outcomes in a sample of adult Medicaid beneficiaries with type 2 diabetes. Most participants (87%) reported at least one social need and 50% reported 3 or more social needs. These rates are comparable to social needs reported by parents of children seen at a safety-net hospital (83% had at least one need; 20% reported 4 or more needs) (Gottlieb, Hessler, et al., 2016). However, the prevalence of social needs are often higher in samples from community health centers (97% had at least one need; Gold et al., 2018) than larger private healthcare systems (34.6% had at least one need; Berkowitz, Hulberg, Standish, Reznor, & Atlas, 2016). Despite the small sample, the authors of this study demonstrate the negative associations of social needs on multiple outcomes: cognitive function, stress, sleep, self-care, and health. These intermediate outcomes may mediate the effects of social needs on health outcomes and should be examined in longitudinal research. Further, a more holistic view of the multiple social needs patients report and their diverse effects on physical and emotional functioning may improve the design of future interventions to address social needs and improve health. Novel interventions are needed because US adults with type 2 diabetes seek to achieve recommended levels of A1C, blood pressure, cholesterol, and smoking abstinence, but only 23% achieve the composite goal (Kazemian, Shebl, McCann, Walensky, & Wexler, 2019).
Implications for intervention.
This study also provides valuable new insights about Medicaid beneficiaries’ interest in social needs navigation. There is a longer history of research on patient navigation programs that typically focus on care coordination, healthcare access, timely treatment, and social support (Ali-Faisal et al., 2017). Although few studies have specifically examined patients’ interest in navigation, some have noted gaps in the uptake of offered services (Schickedanz et al., 2019) or trust in healthcare professionals as a reason for declining navigation (Thygesen, Pedersen, Kragstrup, Wagner, & Mogensen, 2012). In a qualitative study, recently hospitalized patients were more likely to decline navigation, whereas their caregivers desired navigation services (Ursan et al., 2016). As noted in this study, there may be some differences in who accepts navigation for health vs. social needs. Nearly half of participants were interested in having a social needs navigator. People who had more social needs, smoked, and had poorer health were more interested in having a social needs navigator.
Prior research has documented the value of social needs navigation interventions for connecting low-income adults to needed health services (Gottlieb, Hessler, et al., 2016; Kreuter et al., 2016; Schickedanz et al., 2019). However, in a recent survey of Medicaid Managed Care Organizations, 91% reported assessing social needs and 93% reported linking members to social services to address identified needs, but far fewer offered navigation-type services to help members actually access and use available resources (Artiga & Hinton, May 10, 2018). A triage model of self-reported need and interest in navigation would be helpful for delivering navigation services within healthcare organizations, which may prevent social or health crises from emerging. Although healthcare organizations would need to provide training and resources to offer social needs navigation programs, many like Louisiana Healthcare Connections already offer comprehensive care management services to some members. It is possible that providing navigation services may only require shifting and refining existing efforts rather than developing a new program with new resources.
Limitations.
Cross-sectional survey results do not support inferences of temporal associations, and the small sample size may underestimate the magnitude of these associations. Larger studies could use latent variable modeling to examine clustering of social needs and test mediating and moderating pathways of influence from social needs to health outcomes.
Reaching Medicaid beneficiaries by phone was difficult. Despite drawing from a random sample of members with diabetes, it seems likely that those we reached and surveyed could be different from those we could not reach or whose phone service was no longer active. Additionally, many (47%) of the respondents reported they were not working due to a disability. Future studies and health plan outreach activities will benefit from improvements in tracking changes in members’ contact information and using multiple modes of communication (e.g., email, text messages). Although the small sample provided ample power to detect significant associations between social needs and many hypothesized health-related correlates, the small sample may not generalize to the Medicaid population in Louisiana and it is unknown whether the Louisiana Medicaid population is representative of the US Medicaid population.
Future studies with larger samples should attempt to replicate these findings and explore potential differences in health outcomes by the number or types of social needs. Health outcomes could also be examined using administrative claims data or medical record data. Such findings would inform the design of future interventions to be more efficient and effective in addressing social needs. For example, research might identify a threshold level for social needs (e.g., 2+) above which health outcomes are most compromised, or a particular cluster of needs that are more prevalent among patients with certain conditions like type 2 diabetes (Kreuter et al., In press). The authors will attempt to examine these questions in an upcoming intervention trial offering social needs navigation to Medicaid beneficiaries with type 2 diabetes (1R01DK115916-01).
Conclusions.
As more organizations seek to provide social needs referrals and navigation services for members with chronic diseases, attention needs to be paid to the inter-related mix of needs, chronic conditions, and health behaviors that impact healthcare utilization and health outcomes. Future intervention trials can test mediated and moderated effects of social needs on various health behaviors and health outcomes, and compare effects by types or clusters of social needs.
What is known about this topic?
Among adults with type 2 diabetes, food insecurity has been related to poor glucose control; however, this association is inconsistent across studies
Patient navigation programs show promise for improving healthcare access and utilization
What this paper adds:
Participants reported multiple social needs.
Despite the small sample size, needs were significantly associated with a range of cognitive, psychosocial, and health behavior factors that impact mental and physical health outcomes
Not all patients will engage with patient navigators; this paper documents factors associated with interest in having a navigator address health and social needs. Perceiving oneself in worse health, being more stressed, distressed, cognitively challenged, and reporting poor sleep all increased interest in navigation.
Acknowledgements
This research was supported by a pilot grant award (PI: McQueen) from the Washington University Center for Diabetes Translation Research (P30DK092950 PI: Haire-Joshu) and subsequent grant 1R01DK115916-01 (MPI: McQueen & Kreuter). Special thanks go to our participants who shared their time and to our survey interviewers Vineet Raman, Erika Halsey, Paulina Flores Jimenez, and Elle Warshaw. The study benefited from collaborators from Washington University partnerships with the Centene Center for Health Transformation (Karyn Quinn, Lisa Gibson), Centene Corporation (Ginny Barr, Scott Lantz), and Louisiana Healthcare Connections (Kendra Case, Delanie Bachman). Analytic support with claims data was received from Matthew Keller and Margaret Olsen at the Center for Administrative Data Research at Washington University, which is supported by ICTS grant UL1 TR002345 and AHRQ grant R24 HS19455. Procedures and preliminary findings were presented at the annual Society of Behavioral Medicine conference April 2018, New Orleans LA.
Footnotes
Conflict of interest
The authors have no conflicts of interest to report.
Data availability and data sharing
Raw data is not publicly available due to privacy restrictions, but aggregate results are available on request from the corresponding author.
References
- Ali-Faisal SF, Colella TJF, Medina-Jaudes N, & Scott LB (2017). The effectiveness of patient navigation to improve healthcare utilization outcomes: A meta-analysis of randomized controlled trials. Patient Education & Counseling, 100, 436–448. [DOI] [PubMed] [Google Scholar]
- Andermann A (2018). Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Public Health Reviews, 39(19), 17p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Artiga S, & Hinton E (May 10, 2018). Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity. Available at https://www.kff.org/disparities-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/.
- Bachrach D, Pfister H, Wallis K, & Lipson M (2014). Addressing patients’ social needs. An emerging business case for provider investment. Commonwealth Fund publication 1749. Available online http://www.commonwealthfund.org/~/media/files/publications/fund-report/2014/may/1749_bachrach_addressing_patients_social_needs_v2.pdf. [Google Scholar]
- Berkowitz SA, Hulberg AC, Standish S, Reznor G, & Atlas SJ (2016). Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med, 177(2), 244–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkowitz SA, Meigs JB, DeWalt D, Seligman HK, Barnard LS, Bright OM, Schow M, Atlas SJ, & Wexler DJ (2015). Material need insecurities, control of diabetes mellitus, and use of health care resources. Results of the Measuring Economic Insecurity in Diabetes Study. JAMA Internal Medicine, 175(2), 257–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisgaier J, & Rhodes KV (2011). Cumulative adverse financial circumstances: associations with patient health status and behaviors. Health and Social Work, 36(2), 129–137. [DOI] [PubMed] [Google Scholar]
- Buchanan T, Heffernan TM, Parrott AC, Ling J, Rodgers J, & Scholey AB (2010). A short self-report measure of problems with executive function suitable for administration via the Internet. Behavior Research Methods, 42(3), 709–714. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. About adult BMI. How is BMI calculated? Available online at https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html.
- Centers for Disease Control and Prevention. (1993). CDC HRQOL-14 Healthy Days Measure. Available at: http://www.cdc.gov/hrqol14_measure.htm.
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. [PubMed] [Google Scholar]
- Daniel-Robinson L, & Moore JE (2019). Innovation and opportunities to address social determinants of health in Medicaid managed care. Available online at http://healthystudentspromisingfutures.org/wp-content/uploads/2019/07/2019-IMI-Social_Determinants_of_Health_in_Medicaid-Report.pdf.
- Faul P, Erdfelder E, Lang A, & Buchner A (2007). G*Power: A flexible statistical power analysis for the social, behavioral, and biomedical sciences Behavior Research Methods, 39(2), 175–191. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick-Lewis D, Ganann R, Krishnaratne S, Ciliska D, Kouyoumdjian F, & Hwang S (2011). Effectiveness of interventions to improve the health and housing status of homeless people: a rapid systematic review. BMC Public Health, 11, 638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraze T, Lewis VA, Rodriguez HP, & Fisher ES (2016). Housing, transportation, and food: how ACOs seek to improve population health by addressing nonmedical needs of patients. Health Affairs, 35(11), 2109–2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold R, Bunce A, Cowburn S, Dambrun K, Dearing M, Middendorf M, Mossman N, Hollombe C, Mahr P, Melgar G, Davis J, Gottlieb L, & Cottrell E (2018). Adoption of social determinants of health EHR tools by community health centers. Annals of Family Medicine, 16, 399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb L, Garcia K, Wing H, & Manchanda R (2016). Clinical interventions addressing nonmedical health determinants in Medicaid managed care. American Journal of Managed Care, 22(5), 370–376. [PubMed] [Google Scholar]
- Gottlieb LM, Hessler D, Long D, Laves E, Burns AR, Amaya A, Sweeney P, Schudel C & Adler NE (2016). Effects of social needs screening and in-person service navigation on child health: A randomized clinical trial. JAMA Pediatr, 170(11), e162521. [DOI] [PubMed] [Google Scholar]
- Groll DL, To T, Bombardier C, & Wright JG (2005). The development of a comorbidity index with physical function as the outcome. Journal of Clinical Epidemiology, 58(6), 595–602. [DOI] [PubMed] [Google Scholar]
- Kalousova L, Xiao B, & Burgard SA (2019). Material hardship and sleep: results from the Michigan Recession and Recovery Study. Sleep Health, 5(2), 113–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz A, Chateau D, Enns JE, Valdivia J, Taylor C, Walld R, & McCulloch S (2018). Association of the social determinants of health with quality of primary care. Annals of Family Medicine, 16(3), 217–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazemian P, Shebl FM, McCann N, Walensky RP, & Wexler DJ (2019). Evaluation of the cascade of diabetes care in the United States, 2005-2016. JAMA Intern Med, 179(10), 1376–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreuter MW, Garg RC, Li L, McNulty L, Thompson T, McQueen A, & Luke AA (In press). How do social needs cluster among low-income individuals? Population Health Management. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreuter MW, McQueen A, Boyum S, & Fu Q (2016). Unmet basic needs and health intervention effectiveness in low-income populations. Preventive Medicine, 91, 70–75. doi: 10.1016/j.ypmed.2016.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyles CR, DeWalt D, Wolf MS, Dahlke AR, Schillinger D, Curtis L, Davis TC, & Seligman HK (2013). Food insecurity in relation to changes in hemoglobin A1c, self-efficacy, and fruit/vegetable intake during a diabetes educational intervention. Diabetes Care, 36, 1448–1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery J, Lu J, Ratliff S, & Mezuk B (2017). Food insecurity and depression among adults with diabetes: Results from the National Health and Nutrition Examination Survey (NHANES). Diabetes Educator, 43(3), 260–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Neurological Disorders and Stroke (NINDS). (March 2015). Quality of life in neurological disorders (Neuro-QoL) measures. Version 2.0. Cognition Function-Short form. Available online http://www.healthmeasures.net/administrator/components/com_instruments/uploads/15-09-01_02-09-32_Neuro-QOLv2.0-CognitiveFunctionSF_09-8-2014.pdf. [Google Scholar]
- Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullen J, & Jackson RA (2005). Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care, 28, 626–631. [DOI] [PubMed] [Google Scholar]
- Sandberg SF, Erikson C, Owen R, Vickery KD, Shimotsu ST, Linzer M, Garrett NA, Johnsrud KA, Soderlund DM, & DeCubellis J (2014). Hennepin health: A safety-net accountable care organization for the expanded Medicaid population. Health Affairs, 33(11), 1975–1984. [DOI] [PubMed] [Google Scholar]
- Sattler ELP, Lee JS, & Bhargava V (2014). Food insecurity and medication adherence in low-income older Medicare beneficiaries with type 2 diabetes. Journal of Nutrition in Gerontology and Geriatrics, 33, 401–417. [DOI] [PubMed] [Google Scholar]
- Schickedanz A, Sharp A, Hu YR, Shah NR, Adams JL, Francis D, & Rogers A (2019). Impact of social needs navigation on utilization among high-utilizers in a large integrated health system: a quasi-experimental study. Journal of General Internal Medicine, 34, 2382–2389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirazian S, Crnosija N, Weinger K, Jacobson AM, Park JF, Tanenbaum ML, … Hammock AC (2016). The self-management experience of patients with type 2 diabetes and chronic kidney disease: A qualitative study. Chronic Illness, 12(1), 18–28. [DOI] [PubMed] [Google Scholar]
- Thygesen MK, Pedersen BD, Kragstrup J, Wagner L, & Mogensen O (2012). Gynecological cancer patients’ differentiated use of help from a nurse navigator: A qualitative study. BMC Health Services Research, 12, 168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toobert DJ, Hampson SE, & Glasgow RE (2000). The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care, 23, 943–950. [DOI] [PubMed] [Google Scholar]
- Ursan ID, Krishnan JA, Pickard AS, Calhoun E, DiDomenico R, Prieto-Centurion V, Sullivan JB, Valentino L, Williams MV, & Joo M (2016). Engaging patients and caregivers to the design transitional care management services at a minority serving institution. Journal of Health Care for the Poor and Underserved, 27(1), 352–365. [DOI] [PubMed] [Google Scholar]
- Vijayaraghavan M, Jacobs EA, Seligman H, & Fernandez A (2011). The association between housing instability, food insecurity, and diabetes self-efficacy in low-income adults. Journal of Health Care for the Poor and Underserved, 22(4), 1279–1291. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Raw data is not publicly available due to privacy restrictions, but aggregate results are available on request from the corresponding author.


