Abstract
Background
We aimed to explore the risk profiles attributable to psychosocial and behavioural problems during the coronavirus disease 2019 pandemic. To this end, we created a risk-prediction nomogram model.
Methods
A national multicentre study was conducted through an online questionnaire involving 12,186 children (6-11 years old) and adolescents (12-16 years old). Respondents’ psychosocial and behavioural functioning were assessed using the Achenbach Child Behaviour Checklist (CBCL). Data were analysed using STATA software and R-language.
Results
The positive detection rate of psychological problems within Wuhan was greater than that outside Wuhan for schizoid (P = 0.005), and depression (P = 0.030) in children, and for somatic complaints (P = 0.048), immaturity (P = 0.023), and delinquent behaviour (P = 0.046) in adolescents. After graded multivariable adjustment, seven factors associated with psychological problems in children and adolescents outside Wuhan were parent-child conflict (odds ratio (OR): 4.94, 95% confidence interval (95% CI): 4.27-5.72), sleep problems (OR: 4.05, 95% CI: 3.77-4.36), online study time (OR: 0.41, 95% CI: 0.37-0.47), physical activity time (OR: 0.510, 95% CI: 0.44-0.59), number of close friends (OR: 0.51, 95% CI: 0.44-0.6), time spent playing videogames (OR: 2.26, 95% CI: 1.90-2.69) and eating disorders (OR: 2.71, 95% CI: 2.35-3.11) (all P < 0.001). Contrastingly, within Wuhan, only the first four factors, namely, parent-child conflict (5.95, 2.82-12.57), sleep problems (4.47, 3.06-6.54), online study time (0.37, 0.22-0.64), and physical activity time (0.42, 0.22-0.80) were identified (all P < 0.01). Accordingly, nomogram models were created with significant attributes and had decent prediction performance with C-indexes over 80%.
Limitation
A cross-sectional study and self-reported measures.
Conclusions
Besides the four significant risk factors within and outside Wuhan, the three additional factors outside Wuhan deserve special attention. The prediction nomogram models constructed in this study have important clinical and public health implications for psychosocial and behavioural assessment.
Keywords: Coronavirus disease 2019, Risk factors, Psychosocial and behavioural problems, Children and adolescents
Introduction
Since the coronavirus disease 2019 (COVID-19) outbreak in Wuhan, Hubei Province, China in December 2019 (Liu et al., 2020c; Wang et al., 2020a; WHO, 2020), most governments have temporarily implemented social distancing measures by imposing citywide or nationwide lockdowns (Patrick et al., 2020). This included the temporary closure of schools, which has affected up to 1.4 billion students worldwide (UNESCO, 2020; Viner et al., 2020). In China, a nationwide school closure, implemented as an emergency measure, came into effect on 27 January 2020 and was extended until late April 2020. For practical reasons, measures undertaken to minimise the adverse socio-emotional effects of school closures included increased parent children activities, peer communication and support, reduced academic load, and promotion of healthy habits, such as increased physical activity, balanced diet, regular sleeping pattern, and good personal hygiene, based on national and local guidelines (Ministry of Education of China, Ministry of Industry and Information Technology of China, 2020; Ministry of Education of China, 2020; Ministry of Civil Affairs, 2021). Although public activities were discouraged, children were required to wear a mask and maintain social distancing when going outside during physical activities. A large percentage of children in China live with their extended families in a single household; hence, grandparents often provide childcare during special periods. Measures were implemented online to assist students with mental health issues across cities in China.
Although citywide lockdowns have effectively slowed down the spread of COVID-19 (Pan et al., 2020; Tian et al., 2020), researchers have recognised that the disrupted school routines and long-term home confinement have had a negative impact on children's physical and mental health (Brooks et al., 2020; Miu et al., 2020; Wang et al., 2020b). For instance, 22.6% and 18.9% students reported depressive and anxiety symptoms in a mental health survey during the early period of home confinement in Hubei Province (Xie et al., 2020). Since the majority of data were cross-sectional, Zhang et al. conducted a longitudinal cohort study that investigated psychological symptoms and suicide-related problems among children and adolescents prior to the outbreak (early November 2019) and 2 weeks after school reopened (during the second wave of the pandemic, in mid-May 2020). This study found a significant increase in the prevalence of anxiety, depression, suicidal ideation, and suicide attempts in Anhui Province, China (Zhang et al., 2020).
In the current medical literature, there is considerable interest in the prevalence and potential risk factors attributable to the development of psychosocial and behavioural problems. A large cross-sectional study that enrolled 4,805 female adolescents revealed that short sleep duration and physical inactivity represented independent factors for suffering from depression (Zhou et al., 2020a). Another online study consisting of 8,079 adolescents revealed that women and high school students were at greater risk for depressive and anxiety symptoms (Zhou et al., 2020b). However, results from the previous studies lack consistency as most of them were monocentre studies and focused on only some dimensions of mental health. Therefore, despite many research endeavours (Loades et al., 2020), we are still facing challenges in predicting children and adolescents who are more likely to be mentally ill. The most compelling reason might be due to the lack of experience and complicated processes underlying mental aetiology and pathogenesis. Therefore, it is of great importance to create a robust prediction model by incorporating multiple established risk factors in a multicentre study using a general scale to measure childhood psychosocial and behavioural status during the pandemic.
So far, the available literature on prediction models for mental problems associated with COVID-19 is scarce. To bridge this gap in the literature and generate more information for preventing negative outcomes, we conducted a multicentre investigation to assess multiple contributing factors among children and adolescents (6-16 years old) who were enrolled from 5 geographic regions of China by using a comprehensive scale of childhood psychosocial and behavioural problems. To further enhance the applicability of our findings, we aimed to create risk prediction nomogram models based on promising significant attributes.
Methods
Study design and ethical aspects
This was a multicentre study. An online survey was conducted from 20 May 2020 to 20 July 2020. The study was approved by the Institutional Review Board of the Capital Institute of Paediatrics (Number: SHERLL2020019). Parents or guardians provided informed consent online for all participants.
Study participants
The study was prospectively sponsored by the Subspecialty Group of Developmental and Behavioural Paediatrics, the Society of Paediatrics, and the Chinese Medical Association. This study used a stratified cluster sampling strategy. North, East, West, South and Central geographical regions within mainland China, were selected to form a representative sample. Within each region, the city with the largest population and the city geographically located in the centre of the region were chosen. Therefore, 10 cities were selected from the North (Beijing and Changchun), East (Shanghai and Nanjing), West (Chongqing and Xi'an), South (Guangzhou and Fuzhou), and Central (Wuhan and Zhengzhou) regions. Subsequently, within each city, the district whose average income was closest to the region's median was selected. One primary, one junior, and one high school were chosen from each district based on whether they were medium-sized public schools, had at least 1,000 students, had no more than 60% of their students belonging to the same gender, and were active for more than 10 years. In order to reach the necessary sample size, two classes from each grade were randomly selected from the schools.
At the end of survey, a total of 13,593 participants from five geographic regions of China were enrolled in the survey. The city of Zhengzhou was excluded from the survey because it did not reach the necessary sample size (only 122). Questionnaires with abnormal answers (contradictions and/or inconsistencies, e.g. inconsistence/contradictions of age and grade, such as if the children's age was 8 years old while their grade was marked as sixth grade, or if some children were younger than 6 or older than 16 years) were excluded. The remaining questionnaires were carefully reviewed by trained staff, and 12,186 questionnaires were deemed eligible for inclusion. As the city that was first and most severely affected by COVID-19, which also made it the first city responses from the Wuhan group were analysed separately from the rest. Of the total sample, 1,114 children and adolescents belonged to Wuhan, while 11,072 children and adolescents belonged to other regions in China.
Questionnaire design and data collection
Questionnaires were designed to collect data from children's parents/guardians through an online survey conducted through the Wenjuanxing platform (https://dnalab.wjx.cn/jq/75239406.aspx). The questionnaire covered three thematic areas: (1) Demographic information: The demographic variables included students’ age and gender, parental education status (≤ 12 years or > 12 years), whether parents or relatives were infected with COVID-19 (Yes/No), family income status (Decreased/No change/Increased), and post-pandemic parent-child conflict (No change/Decreased or Increased); (2) Psychosocial impact of the pandemic: The variables included homework time (≤ 2 hours, > 2 hours per day), sedentary time (≤ 6 hours, > 6 hours per day), online study time (≤ 4 hours, > 4 hours per day), physical activity time (≤ 1 hour, > 1 hour per day), sleep problems (Yes/No), eating disorders (Yes/No), and the child's number of close friends(≥ 4 or < 4); (3) Psychological problems: The Child Behaviour Checklist score (CBCL), an widely used, empirically based measure widely used to assess psychopathological dimensions and adaptive functioning in children, with a high test-retest reliability and good internal consistency, was administered (Achenbach and Edelbrock, 1981, Achenbach, 1991). This 113-item scale uses a 3-point Likert scale (0 = not true, 1 = somewhat or sometimes true, and 2 = very often or always true) and is completed by parents who rate a wide range of behaviours displayed by the child in the past six months. The Chinese version of the CBCL contains 10 empirically-based syndrome subscales in different age and gender groups that are consistent with clinically diagnosed psychiatric difficulties: anxiety, social withdrawal, depression, somatic complaints, social problems, schizoid, rule-breaking behaviour, hyperactivity, sexual problems, and aggressive behaviour (Xin et al., 1992, Wang et al., 1999). The scoring system has different cut-off points for clinical significance for the various age groups and gender. The presence of a behavioural disorder was indicated when a participant's score exceeded the threshold for clinical significance on any of the subscales (Supplementary Table 1).
Quality control
The survey was anonymised, and a device could be used only once to complete the questionnaire. The questionnaire was designed so it could not be submitted if some of the items were missing. This helped ensure a better completion rate. The questionnaire's settings (e.g. required questions and limited scope of questions) offered the researchers greater control over its administration and prevented respondents from randomly selecting responses or completing the survey in a hurry.
Statistical analyses
The mean and standard deviation (SD) for normal continuous variables and the frequency and percentage per category for categorical variables were calculated to analyse the demographic and psychosocial characteristics of children and adolescents in each group (those who belonged to Wuhan and those who were from outside of Wuhan). Group differences in baseline characteristics were compared using chi-squared (χ2) or t-tests.
First, considering the fact that the score for psychosocial and behavioural problems is continuous in nature, linear regression analyses using the stepwise method were employed to identify factors significantly associated with psychosocial and behavioural problems. Second, the logistic regression analyses were employed to test factors identified through linear regression analyses that were significantly associated with the score on a categorical scale. In linear regression analyses, the independent variables were simultaneously incorporated into the model using the stepwise method, and the outcome was the score for psychosocial and behavioural problems on a continuous scale. Contrastingly, in the logistic regression analyses, the independent variables included the significant variants identified by the linear regression analyses, which were first modelled one by one, and the outcome was the score on a categorical scale. Next, after adjusting for age, gender, and region, and further adjusting for parental career and parental education level, the statistically significant factors were obtained. The significance was calculated using odds ratios (ORs) and at a 95% confidence interval (95% CI). To assess the possibility of non-random measurement error for observations across the cities in this study, the intraclass correlation coefficients (ICCs) were calculated for clustering within regions. In addition, ICCs can be used to assess whether models are not confounded by non-independent observations clustering in multicentre studies (Guthrie, 2012).
To test whether the contribution of significant factors identified by both linear and logistic regression analyses to the risk prediction for psychosocial and behavioural problems was indispensable, two models, i.e. the basic model and the full model were constructed. The basic and the full models were based on a multivariable logistic model. Variables in the basic model included age, gender, region, grade, career, paternal education status, maternal education status, height, weight, weight gain, family income, sedentary time per day, and homework time per day. Besides the above variables in the basic model, four significant factors (parent-child conflict, sleeping problems, online study time per day, and physical activity time per day) were added to the full model for the Wuhan group. Besides the variables in the basic model and the four significant factors mentioned above, number of close friends, videogame time per day, and eating disorders were also included in the full model for the non-Wuhan group. To assess the prediction performance, both calibration and discrimination analyses were performed. In order to calibrate and describe the closeness between the prediction probability and the actual observed risk, the Akaike information criterion (AIC), Bayesian information criterion (BIC), and the -2log likelihood ratio test were used. Alternately, for the discrimination analysis, the net reclassification improvement (NRI) (Pencina et al., 2008; Pencina et al., 2010) and integrated discrimination improvement (IDI) were calculated. Furthermore, the decision curve analyses (Vickers and Elkin, 2006) were also generated. Additionally, a correlation matrix was performed to display the pairwise correlation coefficients between the variables in this study.
Finally, risk prediction nomograms models for psychosocial and behavioural problems among children and adolescents, both within and outside Wuhan, were generated, in which the concordance index (C-index), defined as the area under the receiver operating characteristics curve, was used for reflecting predictive accuracy. In the nomogram, the points were derived based on the significant factors identified from the full prediction model including parent-child conflict, sleeping problems, online study time per day, physical activity time per day, number of close friends, videogame time per day, and eating disorders, as well as some conventional risk factors including age, gender, weight, and family history of COVID-19.
Statistical analyses were performed using STATA software (version 14.0, Stata Corp, TX), and statistical significance was defined as a two-sided p-value lower than 0.05. The nomogram models were constructed using the ‘rms’ package (Harrell, 2021) implemented in R software (version 4.0.2).
Results
Basic demographic characteristics
The basic demographic characteristics of 12,186 children and adolescents are shown in Table 1 .
Table 1.
Baseline characteristics of children in different area during the COVID-19 pandemic.
| Outside Wuhan (N=11072) | Wuhan (N=1114) | Total (N=12186) | Z/chi-square | P Value | |
| Age (years) | 2.740 | 0.006 | |||
| 6-11 | 9.1(1.33) | 9.3(1.43) | 9.1(1.35) | ||
| 12-16 | 13.9 (1.40) | 13.1 (1.08) | 13.9(1.39) | ||
| Sex | 0.311 | 0.577 | |||
| Boys, N (%) | 5767 (52.1%) | 590 (53.0%) | 6357 (52.2%) | ||
| Girls, N (%) | 5305 (47.9%) | 524 (47.0%) | 5829 (47.8%) | ||
| Family income | 9.903 | 0.007 | |||
| Decrease, N (%) | 5478 (49.5%) | 589 (52.9%) | 6067 (49.8%) | ||
| No change, N (%) | 5510 (49.8%) | 510 (45.8%) | 6020 (49.4%) | ||
| Increase, N (%) | 84 (0.7%) | 15 (1.3%) | 99 (0.8%) | ||
| Parental education status | 90.098 | <0.001 | |||
| ≤12 years, N (%) | 6,633 (59.9%) | 125 (11.2%) | 6,758 (55.5%) | ||
| >12 years, N (%) | 4,439 (40.1%) | 988 (88.8%) | 5,427 (44.5%) | ||
| Maternal education status | 98.929 | <0.001 | |||
| ≤12 years, N (%) | 6,856 (61.9%) | 147 (13.2%) | 7,003 (57.5%) | ||
| >12 years, N (%) | 4,216 (38.1%) | 966 (86.8%) | 5,182 (42.5%) | ||
| Weight gain | 62.960 | <0.001 | |||
| ≤2kg, N (%) | 4194 (37.9%) | 288 (25.9%) | 4482 (36.8%) | ||
| >2kg, N (%) | 6878 (62.1%) | 826 (74.1%) | 7704 (63.2%) | ||
| Parents-child conflict | 63.655 | <0.001 | |||
| Increase, N (%) | 3168 (28.6%) | 460 (40.5%) | 3694 (29.7%) | ||
| No change/decrease, N (%) | 7904 (71.4%) | 676 (59.5%) | 8580 (70.3%) | ||
| Sedentary time per day | 112.81 | <0.001 | |||
| ≤6h, N (%) | 7871 (71.1%) | 621 (55.7%) | 8492 (69.7%) | ||
| >6h, N (%) | 3201 (28.9%) | 493 (44.3%) | 3694 (30.3%) | ||
| Homework time per day | 39.465 | <0.001 | |||
| ≤2h, N (%) | 6429 (58.1%) | 538 (48.3%) | 6967 (57.2%) | ||
| >2h, N (%) | 4643 (41.9%) | 576 (51.7%) | 5219 (42.8%) | ||
| Online study time per day | • | 36.793 | <0.001 | ||
| ≤4h, N (%) | 339 (3.1%) | 53 (4.8%) | 392 (3.2%) | ||
| >4h, N (%) | 10733 (96.9%) | 1061 (95.2%) | 11794 (96.8%) | ||
| Videogames time per day | 20.332 | <0.001 | |||
| ≤1h, N (%) | 3709 (33.5%) | 299 (26.8%) | 4008 (32.9%) | ||
| >1h, N (%) | 7363 (66.5%) | 815 (73.2%) | 8178 (67.1%) | ||
| Physical activity time per day | 58.229 | <0.001 | |||
| ≤1h, N (%) | 5832 (52.7%) | 720 (64.6%) | 6552 (53.8%) | ||
| >1h, N (%) | 5240 (47.3%) | 394 (35.4%) | 5634 (46.2%) | ||
| Sleep problems | 40.930 | <0.001 | |||
| No, N (%) | 7784 (70.3%) | 680 (61.0%) | 8464 (69.5%) | ||
| Yes, N (%) | 3288 (29.7%) | 434 (39.0%) | 3722 (30.5%) | ||
| Eating disorders | 7.629 | <0.001 | |||
| No, N (%) | 7677 (69.3%) | 729 (65.4%) | 8406 (69.0%) | ||
| Yes, N (%) | 3395 (30.7%) | 385 (34.6%) | 3780 (31.0%) | ||
| Number of close friends | 0.3864 | 0.534 | |||
| <4, N (%) | 6,394 (57.8%) | 632 (56.8%) | 7,026 (57.7%) | ||
| ≥4, N (%) | 4,678 (42.3%) | 481 (43.2%) | 5,159 (42.3%) |
Data are expressed as mean (standard deviation) or count (percent). P value was calculated by the rank-sum test or the Chi-squared test where appropriate.
The CBCL score and total positive detection rate
The positive detection rate of psychological problems within Wuhan was greater than that outside Wuhan for schizoid (P = 0.005), depression (P = 0.030), and overall score (P = 0.002) in children, and somatic complaint (P = 0.048), immaturity (P = 0.023), delinquent behaviour (P = 0.046), and overall score (P < 0.001) in adolescents, as shown in Table 2 .
Table 2.
The prevalence of disorders among Wuhan and outside Wuhan in different age groups during the COVID-19 pandemic.
| Behavior Subscales | Outside Wuhan | Wuhan | Chi-Square | P Value | Outside Wuhan | Wuhan | Chi-Square | P Value |
| Positive rate, N (%) | 6-11years: N=5248 N=666 | 12-16years: N=5824 N=448 | ||||||
| Somatic complaints | 65 (1.24%) | 11 (1.65%) | 0.795 | 0.373 | 86 (1.48%) | 12 (2.68%) | 3.907 | 0.048 |
| Schizoid | 203 (3.87%) | 41 (6.16%) | 7.822 | 0.005 | 237 (4.07%) | 25 (5.58%) | 2.373 | 0.124 |
| Depression | 136 (2.59%) | 27 (4.05%) | 4.717 | 0.030 | NA | NA | NA | NA |
| Social problems | 99 (3.5%) | 17 (4.8%) | 1.563 | 0.211 | 53 (1.8%)/ NA | 11 (4.6%)/ NA | 9.073/NA | 0.007/ NA |
| Compulsive activity | 122 (4.3%)/ NA | 24 (6.8%)/ NA | 4.461/NA | 0.035/ NA | 185 (3.18%) | 21 (4.69%) | 2.990 | 0.084 |
| Hyperactivity | 197 (3.75%) | 19 (2.85%) | 1.363 | 0.243 | 147 (5.0%)/ NA | 25 (10.5%)/ NA | 12.998/NA | <0.001/ NA |
| Aggressive behavior | 106 (2.02%) | 18 (2.70%) | 1.343 | 0.247 | 146 (2.51%) | 18 (4.02%) | 3.730 | 0.053 |
| Delinquent behavior | 87 (1.66%) | 7 (1.05%) | 1.391 | 0.238 | 114 (1.96%) | 15 (3.35%) | 3.995 | 0.046 |
| Social withdrawal | 125 (2.38%) | 12 (1.8%) | 0.879 | 0.349 | NA | NA | NA | NA |
| Immature | NA | NA | NA | NA | 144 (2.47%) | 19 (4.24%) | 5.140 | 0.023 |
| Total positive detection rate, N (%) | 509 (9.7%) | 90 (13.51%) | 9.447 | 0.002 | 669 (11.49%) | 81 (18.08%) | 17.178 | <0.001 |
Data are expressed as mean (standard deviation) or count (percent). And some data are expressed as boys/girls. P value was calculated by the Chi-squared test or the t-test where appropriate.
NA, means that this subscale does not exist in this sex and age subgroup.
The subscales, total CBCL scores, and positive detection rate of disorders within and outside Wuhan in different gender and age groups are shown in supplementary Table 2. For male children (boys), the CBCL score and positive detection rate of psychosocial and behavioural problems were 19.45% and 16.07% within Wuhan, respectively, and 16.2% and 10.6% outside Wuhan, respectively. For female children (girls), the score and rate were 15.16 versus 12.81 and 10.5% versus 8.6% within and outside Wuhan. For adolescent boys, the score and rate were 20.57 versus 14.04 and 20.5% versus 12.4%, and for adolescent girls the score and rate were 15.43 versus 13.34 and 15.3% versus 10.5%.
Identification of significant risk factors
Through linear regression analyses, 13 variables were found to be significant risk factors associated with psychosocial and behavioural problems. These included age, gender, grade, parent-child conflict, weight gain, parental education, career, sleeping problems, the number of friends the child has, online study time per day, videogames time per day, physical activity time per day, and eating disorders (Supplementary Table 3). Subsequently, by conducting logistic regression analyses, eight factors were identified as significant risk factors among children and adolescents, both within and outside Wuhan. After adjusting for parental career and parental education level, the remaining seven factors were still statistically significant among children and adolescents outside Wuhan, namely parent-child conflict (OR: 4.942; 95% CI: 4.27 to 5.72; P < 0.001), sleeping problems (OR: 4.054; 95% CI: 3.77 to 4.36; P < 0.001), number of friends the child has (OR: 0.513; 95% CI: 0.44 to 0.6; P < 0.001), online study time per day (OR: 0.414; 95% CI: 0.37 to 0.47; P < 0.001), videogame time per day (OR: 2.258; 95% CI: 1.9 to 2.69; P < 0.001), physical activity time per day (OR: 0.51; 95% CI: 0.44 to 0.59; P < 0.001), and eating disorders (OR: 2.705; 95% CI: 2.35 to 3.11; P < 0.001).
However, for children and adolescents living in Wuhan, only four factors were identified as significant risk factors, namely parent-child conflict (OR: 5.953; 95% CI: 2.82 to 12.57; P< 0.001), sleeping problems (OR: 4.471; 95% CI: 3.06 to 6.54; P < 0.001), online study time per day (OR: 0.372; 95% CI: 0.22 to 0.64; P < 0.001), and physical activity time per day (OR: 0.416; 95% CI: 0.22 to 0.8; P = 0.009). All results are shown in Table 3 . The ICCs ranged from 0 to 1, and the ICCs of all the significant factors were < 0.05 (Supplementary Table 4), indicating that our models are, at least to some extent, not confounded by non-independent observations.
Table 3.
Identification of significant factors in predicting psychosocial and behavioral problems in different area by using the Logistic regression analyses.
| Variables | Outside Wuhan | Wuhan | |||||
| OR | 95% CI | P | OR | 95% CI | P | ||
| Unadjusted | |||||||
| Age | 1.057 | 1.03 to 1.08 | <0.001 | 1.134 | 1.05 to 1.23 | 0.002 | |
| Sex | 1.216 | 1.06 to 1.39 | 0.006 | 1.801 | 1.23 to 2.63 | 0.002 | |
| Parents-child conflict | 4.535 | 3.94 to 5.23 | <0.001 | 5.4 | 3.57 to 8.17 | <0.001 | |
| Weight gain | 1.005 | 1.00 to 1.01 | 0.020 | 1.018 | 1 to 1.04 | 0.031 | |
| Sleep problems | 3.975 | 3.71 to 4.26 | <0.001 | 3.513 | 2.91 to 4.25 | <0.001 | |
| Number of friends | 0.529 | 0.46 to 0.62 | <0.001 | 0.549 | 0.37 to 0.81 | 0.003 | |
| Online study time per day | 0.406 | 0.36 to 0.45 | <0.001 | 0.331 | 0.25 to 0.45 | <0.001 | |
| Videogames time per day | 2.215 | 1.87 to 2.63 | <0.001 | 1.269 | 0.88 to 1.82 | 0.195 | |
| Physical activity time per day | 0.508 | 0.44 to 0.59 | <0.001 | 0.411 | 0.27 to 0.62 | <0.001 | |
| Eating disorders | 2.701 | 2.35 to 3.10 | <0.001 | 1.909 | 1.33 to 2.75 | 0.001 | |
| Age-, sex-, and region-adjusted | |||||||
| Parents-child conflict | 4.844 | 4.19 to 5.6 | <0.001 | 5.268 | 3.47 to 8.01 | <0.001 | |
| Weight gain | 1.004 | 0.99 to 1.01 | 0.115 | 1.017 | 1 to 1.03 | 0.034 | |
| Sleep problems | 4.025 | 3.75 to 4.32 | <0.001 | 3.737 | 3.06 to 4.57 | <0.001 | |
| Number of friends | 0.52 | 0.45 to 0.6 | <0.001 | 0.525 | 0.35 to 0.78 | 0.001 | |
| Online study time per day | 0.414 | 0.37 to 0.46 | <0.001 | 0.346 | 0.25 to 0.47 | <0.001 | |
| Videogames time per day | 2.239 | 1.89 to 2.66 | <0.001 | 1.244 | 0.86 to 1.80 | 0.248 | |
| Physical activity time per day | 0.512 | 0.44 to 0.59 | <0.001 | 0.433 | 0.28 to 0.66 | <0.001 | |
| Eating disorders | 2.728 | 2.37 to 3.13 | <0.001 | 1.877 | 1.29 to 2.72 | 0.001 | |
| Multivariable adjusted | |||||||
| Parents-child conflict | 4.942 | 4.27 to 5.72 | <0.001 | 5.953 | 2.82 to 12.57 | <0.001 | |
| Weight gain | 1.003 | 0.99 to 1.01 | 0.167 | 1.022 | 1 to 1.05 | 0.11 | |
| Sleep problems | 4.054 | 3.77 to 4.36 | <0.001 | 4.471 | 3.06 to 6.54 | <0.001 | |
| Number of friends | 0.513 | 0.44 to 0.6 | <0.001 | 0.661 | 0.35 to 1.26 | 0.209 | |
| Online study time per day | 0.414 | 0.37 to 0.47 | <0.001 | 0.372 | 0.22 to 0.64 | <0.001 | |
| Videogames time per day | 2.258 | 1.9 to 2.69 | <0.001 | 1.400 | 0.75 to 2.63 | 0.294 | |
| Physical activity time per day | 0.51 | 0.44 to 0.59 | <0.001 | 0.416 | 0.22 to 0.8 | 0.009 | |
| Eating disorders | 2.705 | 2.35 to 3.11 | <0.001 | 1.513 | 0.79 to 2.89 | 0.211 | |
Abbreviations: OR, odds ratio; 95% CI, 95% confidence interval. P values were calculated after adjusting for age of children, sex, region, parental career and parental education.
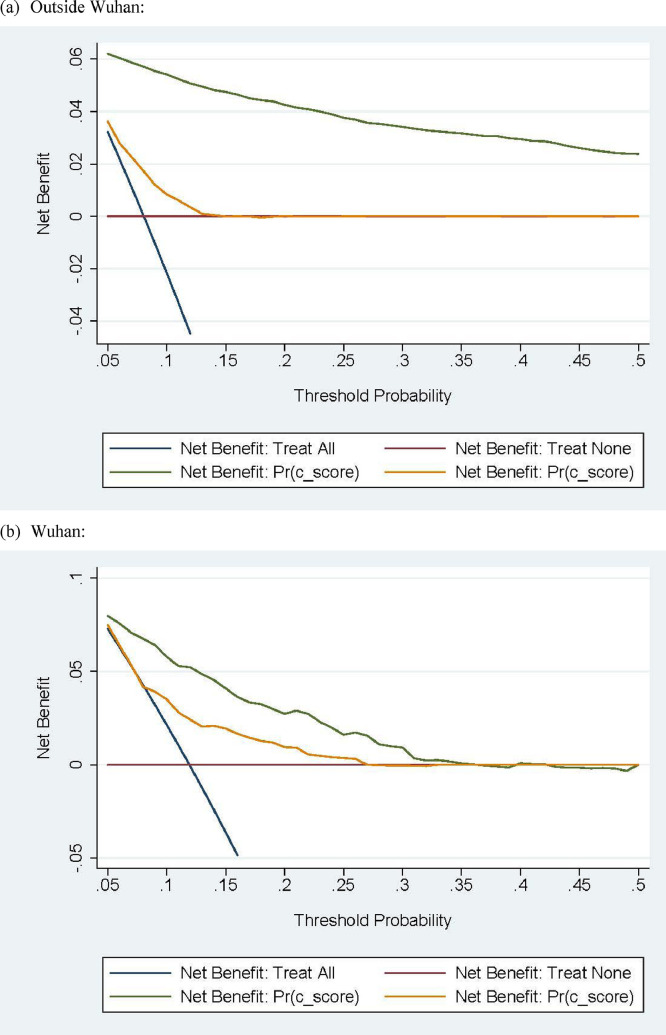
Prediction accuracy assessment
As shown in Table 4 , the basic model and full-model analyses were performed to evaluate the predictive accuracy of the significant factors identified. The full model included all 13 factors identified in the study, while the basic model included all factors, except for the final 7 factors identified for children and adolescents living outside Wuhan and the final 4 factors identified for children and adolescents living in Wuhan. During the analyses, calibration and discrimination statistics were both conducted to evaluate the predictive accuracy obtained by adding the significant factors to the basic model. Further, decision-curve analyses (Vickers and Elkin, 2006) showed that by adding the final significant factors to the basic model, the net benefits gained were obvious among children and adolescents both living in and outside Wuhan (Fig. 1 ).
Table 4.
Prediction accuracy gained by adding the significant factors identified for psychosocial and behavioral problems in different area.
| Statistics | Outside Wuhan | Wuhan | ||
| Basic model | Full model | Basic model | Full model | |
| Calibration | ||||
| AIC | 6043.957 | 3454.593 | 758.702 | 692.339 |
| BIC | 6190.201 | 3681.27 | 872.768 | 831.203 |
| LR test (χ2) | Ref. | 2609.97 | Ref. | 73.52 |
| LR test (P value) | Ref. | <0.0001 | Ref. | <0.0001 |
| Discrimination | ||||
| NRI (P value) | Ref. | <0.0001 | Ref. | 0.0023 |
| IDI (P value) | Ref. | <0.0001 | Ref. | <0.0001 |
| Area under the ROC curve | 0.6396 | 0.9287 | 0.6498 | 0.7719 |
| 95% CI | 0.621 to 0.658 | 0.920 to 0.937 | 0.598 to 0.701 | 0.729 to 0.814 |
| AUROC (P value) | <0.0001 | <0.0001 | ||
Abbreviations: AIC, Akaike information criterion; BIC, Bayesian information criterion; LR, likelihood ratio; NRI, net reclassification improvement; IDI, integrated discrimination improvement; AUROC, area under the receiver operating characteristic; Ref., reference.
Fig. 1.
Decision curve analysis on net benefits gained by significant factors in different areas.
Note: Outside of Wuhan, the factors in the full model (the green solid line) gained better net benefits than those in the basic model (the yellow solid line) across the whole range. In Wuhan, the factors in the full model gained better net benefits than those in the basic model, lower than those in the threshold probabilities of 0.36. ‘C-score’ is the dependent variable of the logistic model, which means the presence of a behavioural disorder when the total score exceeds the cut-off point in the different groups.
In Fig. 1, the yellow solid line corresponds to the basic model. The green solid line corresponds to the full model. “c_score”, the dependent variable of the logistic model, means the presence of behavioral disorder that total score exceeds the cut-off point in different group. Outside Wuhan, the factors in the full model gained better net benefits than that in the basic model across the whole range. In Wuhan, less than the threshold probabilities of 0.36, the factors in the full model gained better net benefits than that in the basic model. In addition, correlation matrixes were performed to display the pairwise correlation coefficients between the variables in this study (Supplementary Table 5). In detail, this matric was expressed as a lower triangular, with two numbers within each panel. The upper number is the correlation coefficient between the horizontal and vertical variables, and the lower number is the significance level of this coefficient.
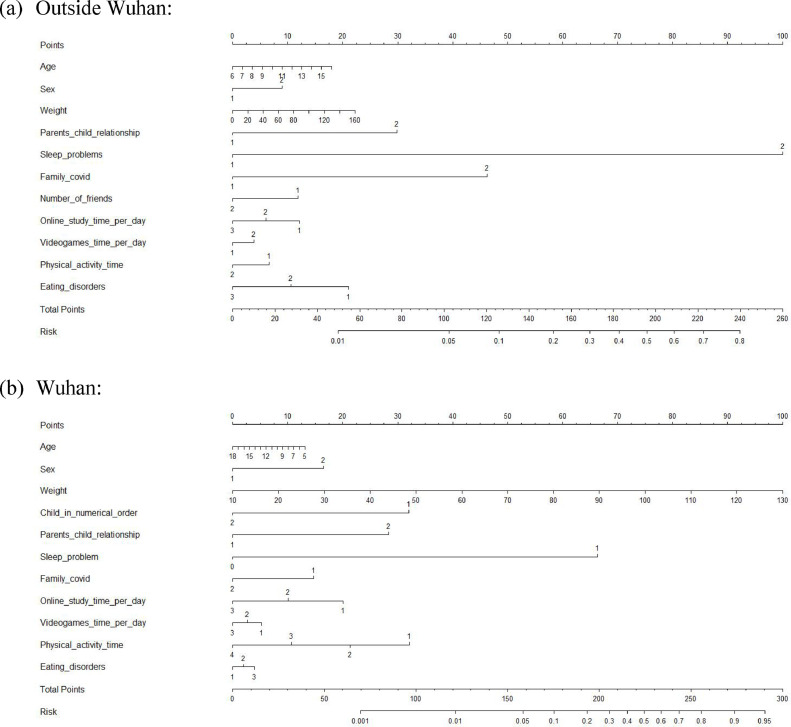
Risk-prediction nomogram model
Based on the significant factors identified from the full prediction model and some conventional risk factors, separate risk prediction nomogram models were created for psychosocial and behavioural problems for children and adolescents living in and outside Wuhan (Fig. 2 ). The C-indexes over 80% indicated that the model's predictive accuracy was good. In addition, the calibration curves also exhibited good predictive accuracy (Supplementary Figure 1).
Fig. 2.
Separate prediction nomograms for psychosocial and behavioural problems for outside Wuhan (the upper panel) and in Wuhan (the lower panel).
An example of the risk-prediction nomogram model outside Wuhan is as follows: assuming a boy (9 points) aged 12 years (11 points), with a weight of 50 kg (7.5 points), with a harmonious parent-child relationship (0 points), with sleeping problems (100 points), with a family member with COVID-19 (47 points), with < 4 close friends (12 points), with ≤ 4 hours of daily study time (0 points), unable to reduce screen time (5 points), with ≤ 1 hours of daily physical activity (7 points), and loss of appetite (22 points); hence, the probability of childhood psychosocial and behavioural problems was estimated to be 69%.
Discussion
This study aimed to assess children and adolescents’ multiple contributing factors associated with psychosocial and behavioural problems caused by long-term home confinement. We created nomogram models to predict the probability of these risk factors. The common key factors within and outside Wuhan were parent-child conflict, sleep problems, online study time and physical activity time. Three additional factors outside Wuhan were number of close friends, videogame time, and eating disorders. To the best of our knowledge, this is the largest study that has explored the difference of risk factors for psychosocial and behavioural problems within and outside Wuhan.
Based on the study's findings, the students’ psychosocial problems were more severe for children and adolescents living in Wuhan than for those living outside Wuhan. These manifestations included greater weight gain, prolonged sedentary time, sleeping problems, prolonged screen exposure time, increased videogame time, as well as physical inactivity or more time spent online studying. Moreover, the positive detection rates in CBCL scores of psychosocial and behavioural problems within Wuhan were significantly higher than those outside Wuhan, such as schizoid and depression in children, as well as somatic complaints, immaturity, and delinquent behaviour in adolescents. These findings were in line with previous studies on somatic and psychological disorders during the pandemic (Liu et al., 2020a; Saurabh and Ranjan, 2020; Xie et al., 2020), which can be attributed to the following reasons: first, the shock resulting from the unexpected announcement of the lockdown in Wuhan city could have probably caused panic, helplessness and concerns about becoming infected (Liu et al., 2020a; Xie et al., 2020), which may have gradually transformed into behavioural problems; second, stress resulting from the higher incidence and rapid spread of COVID-19 infections (Ni et al., 2020). The results showed that the prevalence of COVID-19 in children's family members and relatives in Wuhan was 2.78%, while it was 0.18% for other cities. Children and adolescents were exposed to overwhelming news from the media, which might have added to feelings of fear, distress, and loneliness. Third, the extended duration of home-confinement and consequently, online classes in Wuhan was greater than that of outside Wuhan. Being the centre of the COVID-19 outbreak, Wuhan imposed a lockdown that began on 23 January 2020. Thus, children in Wuhan experienced a longer and stricter quarantine than those outside of Wuhan. The mean length of online study for children in Wuhan was 4.5 months, which was much longer than that for children in other regions (3.3 months). A longer online study duration might have resulted in more negative consequences (Hossain et al., 2020; Lee, 2020).
Since children are more vulnerable to environmental risks, a great deal of effort has been made to curb the processing of mental illness, such as through the creation of online services to cope with mental health issues in most cities (Liu et al., 2020b). Meanwhile, the causes for childhood psychosocial and behavioural problems have been exhaustively investigated, yet the results are not often reproducible; however, a large multicentre study data on outbreak-associated psychosocial and behavioural problems and morbidity of children during long-term confinement and online study are not available. To bridge this gap, we explored the risk factors for psychosocial and behavioural problems among 12,186 children and adolescents in this large-scale multicentre study during long-term home confinement. Parent-child conflicts, sleeping problems, online study time per day, and physical inactivity time per day were significant risk factors that were common for both children and adolescents living within and outside Wuhan. This was partially in line with some previous studies, which also identified sleeping problems and physical inactivity as risk factors. For instance, Ghosh and colleagues deemed that the lack of outdoor activity and aberrant sleeping habits could alter neuropsychiatric manifestations (Ghosh et al., 2020). In this study we identified that parent-child conflict and online studying time (> 4 hours per day) were additional key factors contributing to psychological problems. Parent-child relationships play a vital role in children's lives during times of hardship (Cluver et al., 2020). Dalton and colleagues reported that effective communication can protect the psychological health of children, such as listening to what children believe about COVID-19 transmission and providing them with accurate explanations that are meaningful, which will ensure that they do not feel unnecessarily frightened or guilty (Dalton et al., 2020). Conversely, parent-child conflict leading to less effective communication between parents/caregivers and children may increase the possibility of psychological problems. Prolonged online study time was another key factor contributing to psychological problems. Although online courses are helpful to ensure that school learning is largely uninterrupted, prolonged online study contributed to much longer screen time, which reduced their physical activity (Wang et al., 2020). Besides, online learning produced anxiety and depressive symptoms because of the stressful workload required (Fawaz and Samaha, 2021).
Furthermore, children's number of close friends, videogame time, and eating disorders have also been identified as risk factors for psychological problems in children outside Wuhan but not in those living in Wuhan. There may be several reasons for this result. As the centre of the outbreak, children and adolescents in Wuhan suffered the most severe psychological stress caused by the pandemic, compared with the rest of China, which exacerbated several risk factors as shown by the OR ratios between Wuhan and the rest of China. Another possible reason was the sample size. Having a large sample size that represents all of China, the statistical power of our model allows the detection of small factors, such as screen-time per day, number of friends, and eating disorders.
The risk prediction nomogram models were created for psychosocial and behavioural problems among children and adolescents. The model reflected good predictive accuracy for both groups. To the best of our knowledge, this is the first study to create a model to predict risk probability for psychosocial and behavioural problems in children and adolescents as a result of the COVID-19 pandemic.
Limitations
The present study has a few limitations. First, random sampling was not used to recruit the sample. Therefore, the extent to which this sample was nationally representative is uncertain. Second, while this study employed a multicentre design, a longitudinal approach might be more suitable and helpful in verifying whether the psychosocial and behavioural problems identified in this study improve in the future as regular schooling progresses. Third, although ICCs have been reported to assure the models were not confounded by non-independent observations clustering in this multicentre study, our observations from the same class/school were most likely not independent. Finally, the basic demographic characteristics of children in and outside Wuhan did not match perfectly, which made it difficult to make a fair comparison of the psychological results in the two groups.
Conclusions
The psychological and behavioural symptoms of children and adolescents in Wuhan were more severe than in other regions of China. Parent-child conflict, sleeping problems, online study time per day, and physical inactivity time per day were common significant risk factors for children and adolescents both within and outside Wuhan during the home confinement and online study period. Furthermore, the risk prediction nomogram models created this study can be used for accurately predicting psychological and behavioural symptoms in children and adolescents.
These models are beneficial in identifying children who are at significant risk for developing psychosocial problems in the event of social isolation. These findings also suggest that besides virus control, health and education administrators need to address the challenges faced by children and adolescents. This requires attention from schools, families, mental health providers, and policy-makers- jointly explore how children's mental health can be protected and any long-term consequences resulting from the COVID-19 pandemic. Since children's physical health, mental health, and productivity in adult life are deeply rooted in their early experiences (Clark et al., 2020; Cluver et al., 2020), further research is necessary to include the voices of children and their families when addressing these emergency issues and to develop comprehensive strategies to protect the well-being of future generations.
Author contribution
T.L., L.W. and X.K. designed the study, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. L.W., Y.Z., L.C., F.J., X.S. and T.L. drafted the paper. F.L., Y.H., H.D., J.Z., L.H., S.F., Q.X., L.X., H.G., W.W., J.S., F.L., Y.Q., X.W., L.W., Y.Z., L.C., F.J., X.S., X.K., and T.L. the data analysis, and all authors critically revised the manuscript for important intellectual content and gave final approval for the version to be published. L.W., C.T., J.W., Y.Y., X.W., L.Z., X.L., F.J., L.S., Y.Z., W.W., X.K., L.X., L.C., J.S., J.Z., H.D. and L.H. collected the data from 8 cities. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors read and approved the final manuscript prior to submission.
Funding
This research was supported by the General Program of National Natural Science Foundation of China (NSFC no.81771223), the Key Research and Development Project of Social Livelihood of Science Innovation and Application Demonstration Project of Chongqing Municipal Science and Technology Commission (no.cstc2018jscx-mszdX0023), the Public Service Development and Reform Pilot Project, the Beijing Municipal Health Commission (BMR2019-11), and the Capital's Funds for Health Improvement and Research (2020-2-2104). The sponsors had no role in the collection, management, analysis, and interpretation of the data, in the preparation, review, or approval of the manuscript, or in the decision to submit the manuscript for publication.
Declaration of Competing Interest
The authors declare no conflicts of interest.
Acknowledgments
We would like to thank all healthcare workers and the educational institution's staff involved in the recruitment stage. We would also like to thank the parents of the students who participated in the survey. We express our appreciation to Mary Margaret Gleason (Children's Hospital of the King's Daughters, New Orleans, LA, USA) and Xinyin Chen (Graduate School of Education, University of Pennsylvania, Philadelphia, PA, USA) for their guidance in the study design, interpretation of the results, and review of the manuscript.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.06.077.
Appendix. Supplementary materials
References
- Ministry of Civil Affairs of the People's Republic of China. Notice on Improving Rescue and Protection for Children Lacking Effective Guardianship. http://www.mca.gov.cn/article/xw/tzgg/202002/20200200024310.shtml (accessed Jan 11, 2021).
- Wang XD, Wang XL, Ma H. Chinese Mental Health Journal; Beijing: 1999. Mental Health Asesment Scale (revised edition) p. 4552. [Google Scholar]
- Achenbach T.M., Edelbrock C.S. Behavioral problems and competencies reported by parents of normal and disturbed children aged four through sixteen. Monogr. Soc. Res. Child Dev. 1981;46:1–82. [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet (London, England) 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark H., Coll-Seck A.M., Banerjee A., Peterson S., Dalglish S.L., Ameratunga S., Balabanova D., Bhan M.K., Bhutta Z.A., Borrazzo J., Claeson M., Doherty T., El-Jardali F., George A.S., Gichaga A., Gram L., Hipgrave D.B., Kwamie A., Meng Q., Mercer R., Narain S., Nsungwa-Sabiiti J., Olumide A.O., Osrin D., Powell-Jackson T., Rasanathan K., Rasul I., Reid P., Requejo J., Rohde S.S., Rollins N., Romedenne M., Singh Sachdev H., Saleh R., Shawar Y.R., Shiffman J., Simon J., Sly P.D., Stenberg K., Tomlinson M., Ved R.R., Costello A. A future for the world's children? A WHO-UNICEF-Lancet Commission. Lancet (London, England) 2020;395:605–658. doi: 10.1016/S0140-6736(19)32540-1. [DOI] [PubMed] [Google Scholar]
- Cluver L., Lachman J.M., Sherr L., Wessels I., Krug E., Rakotomalala S., Blight S., Hillis S., Bachman G., Green O., Butchart A., Tomlinson M., Ward C.L., Doubt J., McDonald K. Parenting in a time of COVID-19. Lancet (London, England) 2020;395:e64. doi: 10.1016/S0140-6736(20)30736-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton L., Rapa E., Stein A. Protecting the psychological health of children through effective communication about COVID-19. Lancet Child Adolesc. Health. 2020;4:346–347. doi: 10.1016/S2352-4642(20)30097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fawaz M., Samaha A. E-learning: Depression, anxiety, and stress symptomatology among Lebanese university students during COVID-19 quarantine. Nurs. Forum. 2021;56:52–57. doi: 10.1111/nuf.12521. [DOI] [PubMed] [Google Scholar]
- Ghosh R., Dubey M.J., Chatterjee S., Dubey S. Impact of COVID -19 on children: special focus on the psychosocial aspect. Minerva Pediatr. 2020;72:226–235. doi: 10.23736/S0026-4946.20.05887-9. [DOI] [PubMed] [Google Scholar]
- Guthrie LB, O.E. Sterne JA, Gillman MW, Patel R, Vilchuck K, et al. Ongoing monitoring of data clustering in multicenter studies. BMC Med. Res. Methodol 2012. 2012;12:29. doi: 10.1186/1471-2288-12-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell F.E, 2021. Package 'rms'. https://cran.r-project.org/web/packages/rms/rms.pdf, accessed on March 31, 2021.
- Hossain M.M., Sultana A., Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: a systematic umbrella review of the global evidence. Epidemiol. Health. 2020;42 doi: 10.4178/epih.e2020038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc. Health. 2020;4:421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Liu Y., Liu Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: a cross-sectional survey. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Yang L., Zhang C., Xiang Y.T., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. The lancet. Psychiatry. 2020;7:e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W., Zhang Q., Chen J., Xiang R., Song H., Shu S., Chen L., Liang L., Zhou J., You L., Wu P., Zhang B., Lu Y., Xia L., Huang L., Yang Y., Liu F., Semple M.G., Cowling B.J., Lan K., Sun Z., Yu H., Liu Y. Detection of Covid-19 in Children in Early January 2020 in Wuhan, China. N. Engl. J. Med. 2020;382:1370–1371. doi: 10.1056/NEJMc2003717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loades M.E., Chatburn E., Higson-Sweeney N., Reynolds S., Shafran R., Brigden A., Linney C., McManus M.N., Borwick C., Crawley E. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry. 2020;59 doi: 10.1016/j.jaac.2020.05.009. 1218-1239 e1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miu A., Cao H., Zhang B., Zhang H. Review of Mental Health Response to COVID-19, China. Emerg. Infect. Dis. 2020;26:2482–2484. doi: 10.3201/eid2610.201113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni M.Y., Yang L., Leung C.M.C., Li N., Yao X.I., Wang Y., Leung G.M., Cowling B.J., Liao Q. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China: cross-sectional survey. JMIR Ment. Health. 2020;7:e19009. doi: 10.2196/19009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan A., Liu L., Wang C., Guo H., Hao X., Wang Q., Huang J., He N., Yu H., Lin X., Wei S., Wu T. Association of public health interventions with the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA. 2020;323:1915–1923. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick K., Stanbrook M.B., Laupacis A. Social distancing to combat COVID-19: We are all on the front line. CMAJ : Can. Med. Assoc. J. = journal de l’Association medicale canadienne. 2020;192 doi: 10.1503/cmaj.200606. E516-E517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pencina M.J., D’Agostino R.B., Sr., D’Agostino R.B., Jr., Vasan R.S. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat. Med. 2008;27:157–172. doi: 10.1002/sim.2929. discussion 207-112. [DOI] [PubMed] [Google Scholar]
- Pencina M.J., D’Agostino R.B., Vasan R.S. Statistical methods for assessment of added usefulness of new biomarkers. Clin. Chem. Lab. Med. 2010;48:1703–1711. doi: 10.1515/CCLM.2010.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saurabh K., Ranjan S. Compliance and psychological impact of quarantine in children and adolescents due to Covid-19 pandemic. Indian J. Pediatr. 2020;87:532–536. doi: 10.1007/s12098-020-03347-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian H., Liu Y., Li Y., Wu C.H., Chen B., Kraemer M.U.G., Li B., Cai J., Xu B., Yang Q., Wang B., Yang P., Cui Y., Song Y., Zheng P., Wang Q., Bjornstad O.N., Yang R., Grenfell B.T., Pybus O.G., Dye C. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science (New York, N.Y.) 2020;368:638–642. doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vickers A.J., Elkin E.B. Decision curve analysis: a novel method for evaluating prediction models. Med. Decis. Making. 2006;26:565–574. doi: 10.1177/0272989X06295361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viner R.M., Russell S.J., Croker H., Packer J., Ward J., Stansfield C., Mytton O., Bonell C., Booy R. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc. Health. 2020;4:397–404. doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet (London, England) 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G., Zhang Y., Zhao J., Zhang J., Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet (London, England) 2020;395:945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. Geneva: WHO Characterizes COVID-19 as a Pandemic.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen March 11. [Google Scholar]
- Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., Song R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020;174:898–900. doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xin R., Cai X., Li B. Investigate on 24013 city children’s behavioral problems in 26 units of 22 provinces. Shanghai Arch. Psychiatry. 1992;4:47–55. [Google Scholar]
- Zhang L., Zhang D., Fang J., Wan Y., Tao F., Sun Y. Assessment of mental health of chinese primary school students before and after school closing and opening during the COVID-19 pandemic. JAMA Network Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.21482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J., Yuan X., Qi H., Liu R., Li Y., Huang H., Chen X., Wang G. Prevalence of depression and its correlative factors among female adolescents in China during the coronavirus disease 2019 outbreak. Global Health. 2020;16:69. doi: 10.1186/s12992-020-00601-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S.J., Zhang L.G., Wang L.L., Guo Z.C., Wang J.Q., Chen J.C., Liu M., Chen X., Chen J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry. 2020;29:749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.