Abstract
Background: The 2019 coronavirus disease (COVID-19) pandemic has impacted the mental health and well-being of medical personnel, including nursing students. Network analysis provides a deeper characterization of symptom-symptom interactions in mental disorders. The aim of this study was to elucidate characteristics of anxiety and depressive symptom networks of Chinese nursing students during the COVID-19 pandemic.
Method: A total of 932 nursing students were included. Anxiety and depressive symptom were measured using the seven-item Generalized Anxiety Disorder Scale (GAD-7) and two-item Patient Health Questionnaire (PHQ-2), respectively. Central symptoms and bridge symptoms were identified via centrality indices and bridge centrality indices, respectively. Network stability was examined using the case-dropping procedure.
Results: Irritability, Uncontrollable worry, Trouble relaxing, and Depressed mood had the highest centrality values. Three bridge symptoms (Depressed mood, Nervousness, and Anhedonia) were also identified. Neither gender nor region of residence was associated with network global strength, distribution of edge weights or individual edge weights.
Limitations: Data were collected in a cross-sectional study design, therefore, causal relations and dynamic changes between anxiety and depressive symptoms over time could not be inferred. Generalizability of findings may be limited to Chinese nursing students during a particular phase of the current pandemic.
Conclusions: Irritability, Uncontrollable worry, Trouble relaxing, and Depressed mood constituted central symptoms maintaining the anxiety-depression network structure of Chinese nursing students during the pandemic. Timely, systemic multi-level interventions targeting central symptoms and bridge symptoms may be effective in alleviating co-occurring experiences of anxiety and depression in this population.
Keywords: Depression, Anxiety, Nursing students, Network analysis, COVID-19
1. Introduction
The 2019 coronavirus disease (COVID-19) pandemic has become a public health emergency globally (Cucinotta and Vanelli, 2020). The pandemic has posed serious threats to physical health among segments of the general public (Cao et al., 2020; Kılınçel et al., 2021; Li et al., 2020, 2021; Venugopal et al., 2020) and, especially, among healthcare professionals called upon to treat the virus (Lai et al., 2020; Wu et al., 2020). Healthcare personnel have had unique burdens from the pandemic including high levels of interaction with potentially infected persons, workload increases, concerns with inadequate personal equipment, potential demands related to making ethically difficult decisions in the rationing of care, and increased needs to social distance from family and friends as a result of their work (Gu et al., 2021; Pan et al., 2020). Given these stressors, rates of anxiety and depression are substantially higher within healthcare professions compared to population averages (see Pappa et al., 2020 for a review)(Pappa, 2020). For example, Zheng et al. (Zheng, 2021) found rates of depression and anxiety for Chinese nurses caring for COVID-19 patients were 47.1% and 28.4%, respectively. Anxiety and depression may also be prevalent among less experienced trainees including nursing students. For example, one recent study found rates of anxiety and depression were higher among nursing students than students from other disciplines, primarily because of their potentially higher risk for exposure to infection and fear of infection (Savitsky et al., 2020). In order to provide targeted interventions and coping strategies that facilitate prevention and alleviation of clinically significant distress among students entering higher risk occupations such as nursing, it is important to understand mechanisms that increase their risk for anxiety and depression.
Traditional conceptualizations of psychopathology hold that psychiatric disorders are reflected by the assumption that patients' and co-occurring symptoms have related underlying common causes (Borsboom, 2008; Schmittmann et al., 2013). The reflection model and formative interpretation model are two common conceptualizations of psychiatric disorders (Schmittmann et al., 2013). In reflective latent variable models, symptoms are indicators of an underlying latent variable, consistent with the perspective of common causes (Beard et al., 2016). Likewise, when severity of psychopathology is assessed from the sum of item scores for individual symptoms, an underlying assumption is that symptoms and patient presentations are interchangeable (Fried and Nesse, 2015a; Fried and Nesse, 2015b). Notably, however, traditional formulations of psychopathology may obscure important differences between symptoms and relationships among symptoms (Beard et al., 2016). Relevant studies have found that the presence of certain individual symptoms may influence the development of other symptoms (Baglioni et al., 2011). Similarly, alleviating one symptom has the potential to reduce severity of other symptoms (Bringmann et al., 2015). For example, a study on short-term dynamics of depression revealed that changes in one symptom can predict changes in other symptoms, but not in overall symptom severity (Bringmann et al., 2015). This finding suggests that therapies targeting a particular symptom could lead to improvements in other symptoms (Cramer et al., 2010a). Therefore, network theory has emerged and been applied with increasing frequency as a novel approach to understanding the nature and treatment of psychopathology (Rogers et al., 2019).
A key premise of network theory is that psychopathology symptoms are mutually interacting and reinforcing components within a network instead of clusters of underlying latent disorders (Borsboom and Cramer, 2013). To test this contention, network analysis is used to depict relationships within and between disorders (Borsboom and Cramer, 2013; Cramer et al., 2010a). Dynamic and reciprocal relationships between comorbid disorders can be identified in network analysis and address a gap that is not considered with factor analytic approaches (Costantini et al., 2015; McNally, 2016). In network analysis, disorders are viewed as combinations and interactions of symptoms (Nuijten et al., 2016); instead of summing scores of symptoms to describe disorders, network analysis is a symptom-oriented approach that documents the strength and nature of associations among psychiatric symptoms (Beard et al., 2016; Rouquette et al., 2018). This approach can be used to identify central symptoms (i.e., symptoms having strong connections with other symptoms) (Epskamp et al., 2017) as well as bridge symptoms (i.e., symptoms connecting two psychiatric disorders) that can increase the risk of symptoms transferring from one disorder to another (Jones et al., 2019). Using network analysis to understand symptom-symptom interactions is consistent with clinical practice (Belvederi Murri et al., 2020), and is potentially helpful in identifying interventions that are effective in treating individual syndromes and psychiatric comorbidity (McElroy and Patalay, 2019).
Previous studies have examined the network structure of anxiety and depressive symptom relationships in varied populations including Canadian undergraduate students (Frewen et al., 2013), pregnant women in Singapore (Phua et al., 2020), and American psychiatric patients (Rogers et al., 2019). More recently, other network analysis studies have been conducted during the COVID-19 pandemic in samples comprising adults from China (Wang et al., 2020). However, because patterns and clinical features of depression and anxiety can vary on the basis of sample characteristics such as age, culture, socioeconomic status, presence or absence of medical conditions, and unique stressors (Compton et al., 2006; Kleinman, 2004; Marques et al., 2011), the assumption that network analysis findings from one group are applicable to other groups is not warranted and network structures of anxiety and depressive symptoms should be analyzed separately within particular populations.
Compared to general adult or student samples, nursing students are more likely to experience stressors that reflect effects of pandemics (e.g., limited opportunities for practice-based training during lockdowns and heightened exposure to infected persons, directly witnessing the ravages of an infection, increased fear of infection when lockdowns are lifted) and also trigger increases in anxiety and depression (García-González et al., 2021; Savitsky et al., 2020). Unfortunately, to date, researchers have not utilized network analysis to examine anxiety and depressive symptom relations among nursing students. Therefore, the aim of this study was to characterize the network structure of anxiety and depressive symptoms among nursing students during the COVID-19 pandemic.
2. Methods
2.1. Study settings and participants
This online survey was conducted in nursing school students from four universities in China (Peking University, Jilin University, Lanzhou University, and Capital Medical University) between September 14, 2020 and October 7, 2020. Due to the COVID-19 outbreak, onsite assessments were not adopted. Following previous studies (Sun et al., 2020; Wu et al., 2020), the questionnaire was distributed online using the WeChat-based QuestionnaireStar application. WeChat is a widely used communication application with more than 1.2 billion active users per month in China. Students who met the following selection criteria were included: (1) undergraduate nursing students of the four universities above, (2) age between 15 and 28 years, and (3) ability to understand Chinese and the content of the survey. All nursing students from these universities were WeChat users for teaching reasons. They were consecutively invited to participate in this study during the study period. This study was approved by the Institutional Review Board (IRB) of Beijing Anding Hospital and all the participants provided online written informed consent. For those younger than 18 years, their guardians provided online written informed consent.
2.2. Measurements
Demographic data including age, gender, residence (rural or urban), academic grade, and status as only child in family (“no” versus “yes”), were collected. Anxiety was measured with the Chinese version of the seven-item Generalized Anxiety Disorder Scale (GAD-7) (He et al., 2010; Spitzer et al., 2006). Each item was scored from 0 (not at all) to 3 (nearly every day). GAD-7 total scores range from 0 to 21 with higher scores indicating more severe anxiety symptoms. Depression was measured with the two-item Patient Health Questionnaire (PHQ-2) Chinese version (Kroenke et al., 2003; Yang et al., 2015); each item was scored from 0 (not at all) to 3 (nearly every day) and higher total scores reflected more severe depression. Both the PHQ-9 and GAD-7 have been validated in Chinese populations (He et al., 2010; Yang et al., 2015).
2.3. Statistical analysis
2.3.1. Network estimation
All analyses were conducted using R (Version 4.0.3) (R Core Team, 2020). Following previous studies (Marchetti, 2019; Mullarkey et al., 2019), item informativeness (i.e., standard deviation (SD) of the item) and redundancy (i.e., < 25% of statistically different correlations) were examined by the function describe in R-package psych (Version 2.0.12) (Revelle, 2020) and the function goldbricker in the R-package networktools (Version 1.2.3) (Payton, 2020), respectively. Items must be excluded if they display low informativeness (i.e., 2.5 times their value lower than mean value levels of informativeness for all items in a scale (Marchetti, 2019). As described in the goldbricker function, correlations between two target variables that measure the same underlying construct and all other variables must be calculated; hence at least three items are required to evaluate redundancy in the scale. Consequently, item redundancy was examined only for the GAD-7 in this study.
To establish the depression-anxiety symptom network structure, Extended Bayesian Information Criterion (EBIC) graphical least absolute shrinkage and selection operator (LASSO) network models were used (Epskamp et al., 2012). To estimate and visualize the network, R-package qgraph (Version 1.6.5) (Epskamp et al., 2012) and bootnet (Version 1.4.3) (Epskamp et al., 2018) were used. The association of each pairwise continuous variable (i.e., symptoms) was computed with partial correlation analyses after controlling for all other variables included in the network (Epskamp et al., 2018). In the network analysis, each variable was defined as a node and each pairwise association between variables was defined as an edge. Thicker edges indicate higher correlations. Green and red color edges indicated positive and negative correlations, respectively (Epskamp et al., 2012).
To explore the importance of individual symptoms within the network, three centrality indices were computed: strength (i.e., sum of the absolute edge weights connected to a certain node), closeness (inverse of summing all the shortest path lengths from one node to all other nodes), and betweenness (i.e., the importance of a symptom as a “connecter” to other symptoms based on how frequently a node lies on all the shortest paths between other nodes) (Opsahl et al., 2010). In addition, predictability, which reflects how well a specific node is predicted by all its neighboring nodes, was estimated using R-package mgm (Version 1.2–11) (Haslbeck and Waldorp, 2020). Furthermore, to explore bridge symptoms in the network that played important roles in connecting two or more psychiatric disorders (Cramer et al., 2010b), the bridge function in R-package networktools (Version 1.2.3) was used (Payton, 2020). Bridge centrality indices, including bridge strength, closeness, and betweenness, assessed bridge symptoms. Following previous studies (Garabiles et al., 2019; Jones et al., 2019), bridge symptoms were selected using a bridge strength cutoff of the 80th percentile.
2.3.2. Network stability and accuracy
To assess the robustness of the results, the stability and accuracy of the network were assessed using R-package boonet (Version 1.4.3) (Epskamp et al., 2018). First, non-parametric bootstrapping was used to estimate the accuracy of edge-weights by computing confidence intervals (CIs). New datasets based on 95% CIs were created by randomly resampling observations in the data. Second, to assess network stability, a case-dropping bootstrap procedure was performed to compute a correlation stability coefficient (CS-C). CS-C values indicated the maximum proportion of samples that could be removed while correlations between original centrality indices (i.e. strength, closeness, betweenness) and centrality indices based on case-subset network were maintained above 0.7 with a 95% probability (Epskamp et al., 2018). As recommended previously (Epskamp et al., 2018), a CS-C should not be lower than 0.25 and is preferably above 0.5. Finally, differences in network properties (i.e., edge weights, node strengths) were evaluated by bootstrapped difference tests (Epskamp et al., 2018).
2.3.3. Comparisons based on gender and residence
Following previous studies (Lai et al., 2020; Zhang et al., 2020), gender and rural versus urban residence differences in network characteristics were assessed using Network Comparison Test (NCT) in R-package NetworkComparisonTest (Version 2.2.1) (van Borkulo et al., 2017). This test was conducted on subsamples (i.e., females vs males, rural vs urban participants) with 1000 permutations to assess global network strengths (absolute sum of all edge weights) and network structures (distributions of edge weights) between the two networks. In addition, the strength of each edge between the two networks was assessed using Holm-Bonferroni correlations for multiple comparisons.
3. Results
3.1. Study sample
Of the 983 nursing students consecutively invited to participate in this survey, 932 (702 women, 230 men) were included in this study, reflecting a participation rate of 94.8%. The mean age of the sample was 19.78 years (SD:1.42 years). Socio-demographic characteristics of participants are shown in Table 1 . Abbreviations and mean scores of PHQ-2 and GAD-7 items are summarized in Table S1.
Table 1.
Demographic and clinical characteristics of study sample (N = 932).
| Variables | Mean (SD) or N (%) |
| Age | 19.78 (1.42) |
| University | |
| Peking University | 168 (18.03) |
| Jilin University | 394 (42.27) |
| Lanzhou University | 161 (17.27) |
| Capital Medical University | 209 (22.43) |
| School grade | |
| First year | 240 (25.75) |
| Second year | 200 (21.46) |
| Third year | 216 (23.18) |
| Fourth year | 276 (29.61) |
| Male gender | 230 (24.68) |
| Rural residence | 400 (42.92) |
| Only child in family | 385 (41.31) |
SD, standard deviation.
3.2. Network structure and stability
The assessment of item redundancy indicated no GAD-7 items were redundant with other GAD-7 items. Evaluations of item informativeness indicated no items from the GAD-7 (MSD=0.69±0.06) or PHQ-2 (MSD=0.69±0.05) displayed low informativeness. Therefore, all GAD-7 and PHQ-2 items were included in network analyses.
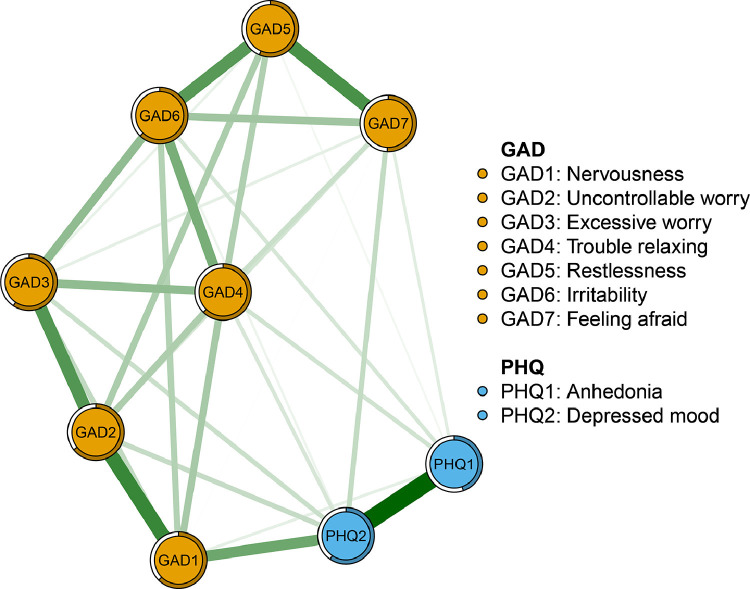
Fig. 1 presents the anxiety and depressive symptom network structure for nursing students. Thirty-one of the 36 edges were above zero, with all connections indicating positive associations. The Anhedonia - Depressed mood edge in depressive symptoms showed a strong connection. Among the anxiety symptoms, the Nervousness – Uncontrollable worry edge showed the strongest connection, followed by edges for Restlessness – Feeling afraid, Uncontrollable worry - Excessive worry, and Restlessness - Irritability. The Nervousness - Depressed mood edge showed the highest connection between anxiety and depressive symptoms within the entire symptom network. Correlation matrices are shown in supplementary material (Table S2). The predictability index indicated that, on average, 58% of the variance in each node could be accounted for by the neighboring nodes (Mpredictability=0.58±0.06). Trouble relaxing (64%), Excessive worry (63%), and Irritability (62%) had the highest predictability indexes within the network (Table S1).
Fig. 1.
Network structure of anxiety and depressive symptoms among nursing students.
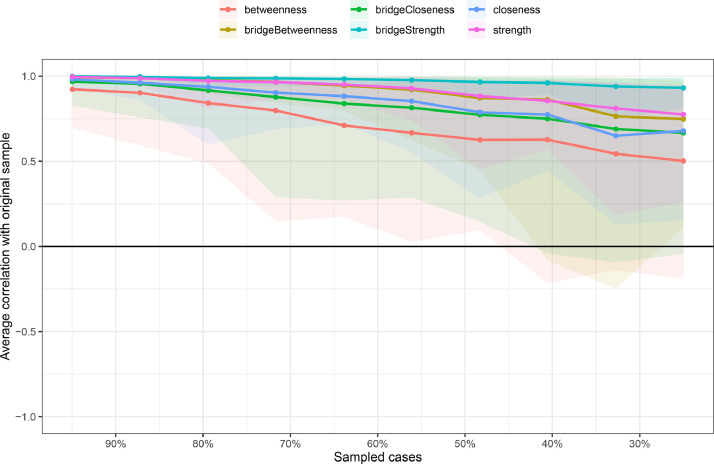
Regarding network stability, the case dropping bootstrap procedure showed that strength and closeness values remained stable after dropping different proportions of the sample (Fig. 2 ). CS-Cs for strength, closeness, and betweenness were 0.594, 0.439, and 0.128, respectively. The index strength showed higher stability: after dropping 59.4% of the sample, results did not change significantly compared to primary results (r = 0.7).
Fig. 2.
The stability of network structure by case dropping subset bootstrap.
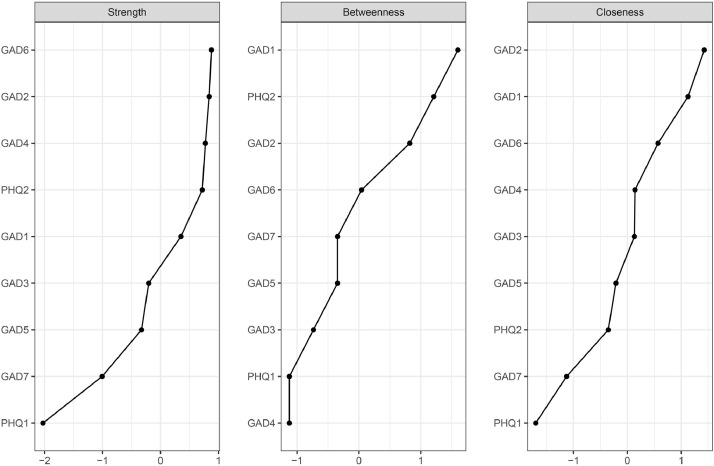
Following previous studies (Epskamp et al., 2018; Forbes et al., 2017; Marchetti, 2019; Shim et al., 2020) in tandem with lower stability of betweenness and closeness, this study focused solely on strength indices. According to centrality indices, the GAD-7 node, Irritability, had the highest strength, followed by Uncontrollable worry, and Trouble relaxing, and the PHQ-2 node Depressed mood. The node with the lowest strength was the PHQ-2 item, Anhedonia (Fig. 3 ). Results of the bootstrap 95% CI for edges and bootstrapped differences tests for edge weights and node strength are shown in supplementary Figure S1-S3.
Fig. 3.
Standardized centrality indices of network structure of anxiety and depressive symptoms (z-scores).
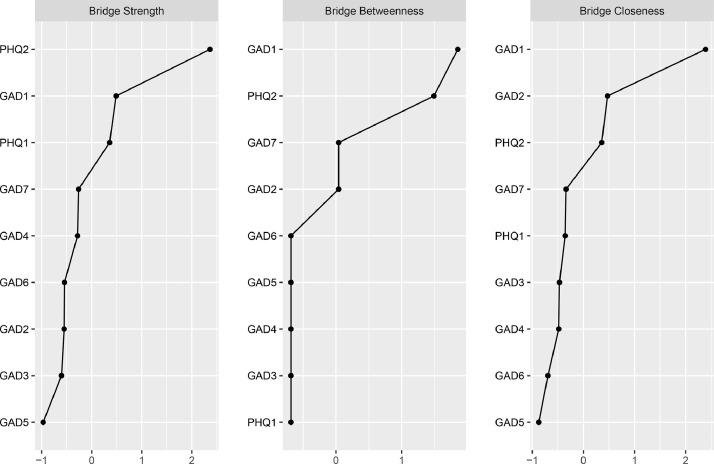
3.3. Bridge symptoms of depression and anxiety
Following previous studies (Garabiles et al., 2019; Jones et al., 2019), bridge strength is the best index identifying nodes in which deactivation could prevent activation spread from one disorder to another and was used to identify bridge symptoms. Depressed mood, Nervousness, and Anhedonia emerged as the three most prominent bridge symptoms (Fig. 4 ).
Fig. 4.
Bridge centrality indices of the anxiety and depressive symptoms among nursing students.
3.4. Comparisons based on gender and residence
There were no significant gender differences in network global strength (females:4.13 vs males:4.14; S = 0.01, p = 0.942), network structure-distribution of edge weights (M = 0.07, p = 0.385), or individual edge weights (all p values >0.05 after Holm-Bonferroni correction). Furthermore, no significant residence differences were found in network global strength (rural:4.16 vs urban:4.07; S = 0.08, p = 0.443), network structure (M = 0.06, p = 0.322), or individual edge weights (all p values >0.05 after Holm-Bonferroni correction). Plots are presented in supplementary materials (figure S4).
4. Discussion
To the best of our knowledge, this was the first study to characterize the anxiety - depressive symptom network of nursing students during the COVID-19 pandemic. In the present study, Irritability was the most central symptom in the entire network, followed by Uncontrollable worry, Trouble relaxing, and Depressed mood. As such, these symptoms were the most likely candidates for triggering or maintaining remaining anxiety and depressive symptoms. Additionally, bridge symptoms linking anxiety and depression in this sample were Depressed mood, Nervousness, and Anhedonia.
Irritability was the most central symptom for Chinese nursing students during the COVID-19 pandemic. Irritability is defined as a person's tendency to experience negative affective states and temper outbursts when faced with stressors (Toohey and DiGiuseppe, 2017). The pandemic is clearly a salient stressor for nursing students. Lockdowns and stay-at-home orders understandably cause irritability among affected persons (Xiang et al., 2020). For instance, long stays at home are related to an increased likelihood of conflict between college students and their family members (Russell et al., 2020). For nursing students, in particular, the pandemic could interfere with progress in applied training during lockdowns. Once lockdowns are lifted, nursing students may face increased risks for personal infection and/or witnessing serious consequences of exposure to COVID-19 infections among patients for whom they care (e.g., death, ongoing symptoms following recovery).
Uncontrollable worry was another central symptom that emerged in this study. Because nursing students are required to engage in e-learning during lockdowns from the pandemic (Gao et al., 2021), the fear of making mistakes in clinical placements (Liu et al., 2015; Parveen and Inayat, 2017), and graduating as incompetent nurses due to finite knowledge and poor quality of clinical training received from online courses (Masha'al et al., 2020) are major stressors for nursing students. In addition, Trouble relaxing, and Depressed mood were central symptoms in this study. This finding was partially consistent with the emergence of Depressed mood and Uncontrollable worry as the most central symptoms of depression and anxiety observed in a large German inpatient sample (Kaiser et al., 2021). One hypothesis that follows from this overlap between samples is that depressed mood and uncontrollable worry, in particular, characterize distress experienced by groups with increased risk for direct exposure to the virus and/or its consequences (i.e., medical personnel, students in training to be medical practitioners, hospital in-patients).
Clinically, bridge symptoms can be viewed as transdiagnostic and targeted interventions may be effective for both disorders (Kaiser et al., 2021). In a meta-analysis involving 66 longitudinal studies with 88,336 persons, Jacobson and Newman (Jacobson and Newman, 2017) investigated prospective relations between anxiety and depression at both symptom and disorder levels; they found that anxiety symptoms could predict depressive symptoms and vice versa, a finding that provides a basis for considering bridge symptoms within anxiety-depressive symptom networks. The strongest bridge symptoms between anxiety and depression we found in this study included Depressed mood, Nervousness, and Anhedonia, which reflect reductions in motivation, interest and consummatory pleasure, as well as reinforcement learning deficits (Der-Avakian and Markou, 2012; Treadway and Zald, 2011). Our findings are consistent with previous research (Garabiles et al., 2019) in which Depressed mood and Anhedonia were bridge symptoms between anxiety and depression among migrant Filipino domestic workers and Nervousness was a bridge symptom between depression and anxiety for pregnant women (Phua et al., 2020). Given that these study samples were markedly different in sociodemographic characteristics and relevant life stressors, the above symptoms are plausible candidates as hallmark bridge symptoms that contribute to comorbidity of anxiety and depression.
Select recent studies have focused on the mental health sequalae of the COVID-19 pandemic (Kumar and Nayar, 2020) and have found that public health measures including quarantine, isolation and lockdowns may increase mood-related problems including anxiety and depression (WHO, 2020). In general samples and among students, the pandemic has resulted in loss of control, uncertainty, and distress (Savitsky et al., 2020). In view of the crucial roles of high centrality symptoms in a network reported from previous studies (Hayes et al., 2015; Levinson et al., 2017), our findings may have utility in tailoring and testing interventions to reduce co-occurring anxiety and depression among nursing students during pandemics. For example, information and strategies for soliciting and managing concerns of students (Savitsky et al., 2020) should be explicitly incorporated within nursing school curriculum (e.g., additional support and alternative avenues for gaining practice-based experience during lockdowns, additional emphasis upon onsite safety precautions and support for trainees when lockdowns are lifted) to reduce irritability and uncontrollable worry. Emphasis on maintaining self-care (e.g., exercise, healthy diet, sufficient sleep) and improving communication between students and significant others in their social networks, outside of classroom and practicum settings are also recommended to alleviate students’ negative mood symptoms (Hammami et al., 2020).
Despite these possible applied implications, several limitations of this study should be acknowledged. First, because data were collected in a cross-sectional study design, causal relations and dynamic changes between anxiety and depressive symptoms over time could not be inferred (Garabiles et al., 2019; Wang et al., 2020). Second, generalizability of our findings may be limited to Chinese nursing students during a particular phase of the current pandemic. Hence, it is possible that data collected during a different time and/or within different groups of students training as healthcare providers could generate different network structures. Third, because a consecutive sampling method was used in this study, generalizability of the findings to the overall population of nursing students may be limited. On a related note, potential exposure of participants to COVID-19 patients was not directly assessed. However, only 26 participants mentioned that there were confirmed cases in their neighborhoods so results may not extend to nursing student samples in which direct exposure to COVID-19 patients is common. Fourth, depressive symptoms were measured using the two-item PHQ-2. As such, a detailed picture of COVID-19 related depressive symptoms was not provided in the assessment.
In conclusion, this network analysis revealed Irritability, Uncontrollable worry, Trouble relaxing, and Depressed mood as the most central anxiety and depressive symptoms of nursing students in training during the COVID-19 pandemic. As such, these may constitute core symptoms for the development and/or maintenance of co-occurring anxiety and depression within this group. Timely, multilevel interventions targeting bridge symptoms (Depressed mood, Nervousness, Anhedonia) may help to alleviate the anxiety and depression in this population.
Contributors
Study design: Wei Bai, Feng-Rong An, Yu-Tao Xiang.
Data collection, analysis and interpretation: Wei Bai, Qianqian Zhu, Zhiwen Wang, Lin Han, Pan Chen, Hong Cai, Rui Liu, Yan-Jie Zhao, Li Chen, Zong-Mei Ge, Mengmeng Ji, Hongyan Zhang, Teris Cheung, Bing-Xiang Yang, Hai-Tao Xi, Shuo Liu.
Drafting of the manuscript: Wei Bai, Yi-Lang Tang, Yu-Tao Xiang.
Critical revision of the manuscript: Todd Jackson.
Approval of the final version for publication: all co-authors.
Role of the funding source
The funding sources were not involved in the study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Acknowledgments
Acknowledgements
None.
Funding
The study was supported by the National Science and Technology Major Project for investigational new drug (2018ZX09201–014), the Beijing Municipal Science & Technology Commission (No. Z181100001518005), the 2020 Higher Education Teaching Achievement Cultivation Project of Gansu Province, the Fundamental Research Funds for the Central Universities (2020YJ065) and the University of Macau (MYRG2019–00066-FHS).
Declaration of competing Interest
The authors declare no conflict of interest.
Footnotes
Running head: Network of depression and anxiety
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.07.072.
Appendix. Supplementary materials
References
- Baglioni C., Battagliese G., Feige B., Spiegelhalder K., Nissen C., Voderholzer U., Lombardo C., Riemann D. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J. Affect Disord. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Beard C., Millner A.J., Forgeard M.J., Fried E.I., Hsu K.J., Treadway M.T., Leonard C.V., Kertz S.J., Björgvinsson T. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol. Med. 2016;46:3359–3369. doi: 10.1017/S0033291716002300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belvederi Murri M., Amore M., Respino M., Alexopoulos G.S. The symptom network structure of depressive symptoms in late-life: results from a European population study. Mol. Psychiatry. 2020;25:1447–1456. doi: 10.1038/s41380-018-0232-0. [DOI] [PubMed] [Google Scholar]
- Borsboom D. Psychometric perspectives on diagnostic systems. J. Clin. Psychol. 2008;64:1089–1108. doi: 10.1002/jclp.20503. [DOI] [PubMed] [Google Scholar]
- Borsboom D., Cramer A.O. Network analysis: an integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Bringmann L.F., Lemmens L.H., Huibers M.J., Borsboom D., Tuerlinckx F. Revealing the dynamic network structure of the Beck Depression Inventory-II. Psychol. Med. 2015;45:747–757. doi: 10.1017/S0033291714001809. [DOI] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton W.M., Conway K.P., Stinson F.S., Grant B.F. Changes in the prevalence of major depression and comorbid substance use disorders in the United States between 1991 and 1992 and 2001-2002. Am. J. Psychiatry. 2006;163:2141–2147. doi: 10.1176/ajp.2006.163.12.2141. [DOI] [PubMed] [Google Scholar]
- Costantini G., Epskamp S., Borsboom D., Perugini M., Mõttus R., Waldorp L.J., Cramer A.O.J. State of the aRt personality research: a tutorial on network analysis of personality data in R. J. Res. Pers. 2015;54:13–29. [Google Scholar]
- Cramer A.O., Waldorp L.J., van der Maas H.L., Borsboom D. Comorbidity: a network perspective. Behav. Brain Sci. 2010;33 doi: 10.1017/S0140525X09991567. 137-150; discussion 150-193. [DOI] [PubMed] [Google Scholar]
- Cramer A.O.J., Waldorp L.J., van der Maas H.L.J., Borsboom D. Complex realities require complex theories: refining and extending the network approach to mental disorders. Behav. Brain Sci. 2010;33:178–193. [Google Scholar]
- Cucinotta D., Vanelli M. WHO Declares COVID-19 a Pandemic. Acta bio-medica: Atenei Parmensis. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Der-Avakian A., Markou A. The neurobiology of anhedonia and other reward-related deficits. Trends Neurosci. 2012;35:68–77. doi: 10.1016/j.tins.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Borsboom D., Fried E.I. Estimating psychological networks and their accuracy: a tutorial paper. Behav. Res. Methods. 2018;50:195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Cramer A.O.J., Waldorp L.J., Schmittmann V.D., Borsboom D. qgraph: network Visualizations of Relationships in Psychometric Data. J. Stat. Softw. 2012;1:1–18. [Google Scholar]
- Epskamp S., Kruis J., Marsman M. Estimating psychopathological networks: be careful what you wish for. PLoS ONE. 2017;12 doi: 10.1371/journal.pone.0179891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes M.K., Wright A.G.C., Markon K.E., Krueger R.F. Evidence that psychopathology symptom networks have limited replicability. J. Abnorm. Psychol. 2017;126:969–988. doi: 10.1037/abn0000276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frewen P.A., Schmittmann V.D., Bringmann L.F., Borsboom D. Perceived causal relations between anxiety, posttraumatic stress and depression: extension to moderation, mediation, and network analysis. Eur. J. Psychotraumatol. 2013;4 doi: 10.3402/ejpt.v4i0.20656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried E.I., Nesse R.M. Depression is not a consistent syndrome: an investigation of unique symptom patterns in the STAR*D study. J. Affect. Disord. 2015;172:96–102. doi: 10.1016/j.jad.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried E.I., Nesse R.M. Depression sum-scores don't add up: why analyzing specific depression symptoms is essential. BMC Med. 2015;13:72. doi: 10.1186/s12916-015-0325-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao H., Ou Y., Zhang Z., Ni M., Zhou X., Liao L. The Relationship Between Family Support and e-Learning Engagement in College Students: the Mediating Role of e-Learning Normative Consciousness and Behaviors and Self-Efficacy. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.573779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garabiles M.R., Lao C.K., Xiong Y., Hall B.J. Exploring comorbidity between anxiety and depression among migrant Filipino domestic workers: a network approach. J. Affect. Disord. 2019;250:85–93. doi: 10.1016/j.jad.2019.02.062. [DOI] [PubMed] [Google Scholar]
- García-González J., Ruqiong W., Alarcon-Rodriguez R., Requena-Mullor M., Ding C., Ventura-Miranda M.I. Healthcare 9; 2021. Analysis of Anxiety Levels of Nursing Students Because of E-Learning During the COVID-19 Pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu Y., Zhu Y., Xu F., Xi J., Xu G. Factors associated with mental health outcomes among patients with COVID-19 treated in the Fangcang shelter hospital in China. Asia Pac. Psychiatry. 2021;13:e12443. doi: 10.1111/appy.12443. [DOI] [PubMed] [Google Scholar]
- Hammami A., Harrabi B., Mohr M., Krustrup P. Physical activity and coronavirus disease 2019 (COVID-19): specific recommendations for home-based physical training. Managing Sport and Leisure. 2020:1–6. [Google Scholar]
- Haslbeck J.M.B., Waldorp L.J. mgm: estimating Time-Varying Mixed Graphical Models in High-Dimensional Data. J. Stat. Softw. 2020;1:1–49. [Google Scholar]
- Hayes A.M., Yasinski C., Ben Barnes J., Bockting C.L. Network destabilization and transition in depression: new methods for studying the dynamics of therapeutic change. Clin. Psychol. Rev. 2015;41:27–39. doi: 10.1016/j.cpr.2015.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He X.Y., Li C.B., Qian J., Cui H.S., Wu W.Y. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatients (in Chinese) Shanghai Arch Psychiatry. 2010:200–203. [Google Scholar]
- Jacobson N.C., Newman M.G. Anxiety and depression as bidirectional risk factors for one another: a meta-analysis of longitudinal studies. Psychol. Bull. 2017;143:1155–1200. doi: 10.1037/bul0000111. [DOI] [PubMed] [Google Scholar]
- Jones P.J., Ma R., McNally R.J. Bridge Centrality: a Network Approach to Understanding Comorbidity. Multivariate Behav. Res. 2019:1–15. doi: 10.1080/00273171.2019.1614898. [DOI] [PubMed] [Google Scholar]
- Kaiser T., Herzog P., Voderholzer U., Brakemeier E.L. Unraveling the comorbidity of depression and anxiety in a large inpatient sample: network analysis to examine bridge symptoms. Depress Anxiety. 2021;38:307–317. doi: 10.1002/da.23136. [DOI] [PubMed] [Google Scholar]
- Kılınçel Ş., Kılınçel O., Muratdağı G., Aydın A., Usta M.B. Factors affecting the anxiety levels of adolescents in home-quarantine during COVID-19 pandemic in Turkey. Asia Pac. Psychiatry. 2021;13:e12406. doi: 10.1111/appy.12406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinman A. Culture and depression. N. Engl. J. Med. 2004;351:951–953. doi: 10.1056/NEJMp048078. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med. Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Kumar A., Nayar K.R. COVID 19 and its mental health consequences. J. Mental Health. 2020;30:1–2. doi: 10.1080/09638237.2020.1757052. [DOI] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA network open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson C.A., Zerwas S., Calebs B., Forbush K., Kordy H., Watson H., Hofmeier S., Levine M., Crosby R.D., Peat C., Runfola C.D., Zimmer B., Moesner M., Marcus M.D., Bulik C.M. The core symptoms of bulimia nervosa, anxiety, and depression: a network analysis. J. Abnorm. Psychol. 2017;126:340–354. doi: 10.1037/abn0000254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H.Y., Cao H., Leung D.Y.P., Mak Y.W. The Psychological Impacts of a COVID-19 Outbreak on College Students in China: a Longitudinal Study. Int. J. Environ. Res. Public Health. 2020;17:3933. doi: 10.3390/ijerph17113933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Zhao J., Ma Z., McReynolds L.S., Lin D., Chen Z., Wang T., Wang D., Zhang Y., Zhang J., Fan F., Liu X. Mental Health Among College Students During the COVID-19 Pandemic in China: a 2-Wave Longitudinal Survey. J. Affect. Disord. 2021;281:597–604. doi: 10.1016/j.jad.2020.11.109. [DOI] [PubMed] [Google Scholar]
- Liu M., Gu K., Wong T.K.S., Luo M.Z., Chan M.Y. Perceived stress among Macao nursing students in the clinical learning environment. Int. J. Nursing Sci. 2015;2:128–133. [Google Scholar]
- Marchetti I. Hopelessness: a Network Analysis. Cognit. Ther. Res. 2019;43:611–619. [Google Scholar]
- Marques L., Robinaugh D.J., LeBlanc N.J., Hinton D. Cross-cultural variations in the prevalence and presentation of anxiety disorders. Expert. Rev. Neurother. 2011;11:313–322. doi: 10.1586/ern.10.122. [DOI] [PubMed] [Google Scholar]
- Masha'al D., Rababa M., Shahrour G. Distance Learning-Related Stress Among Undergraduate Nursing Students During the COVID-19 Pandemic. J. Nurs. Educ. 2020;59:666–674. doi: 10.3928/01484834-20201118-03. [DOI] [PubMed] [Google Scholar]
- McElroy E., Patalay P. In search of disorders: internalizing symptom networks in a large clinical sample. J. Child Psychol. Psychiatry. 2019;60:897–906. doi: 10.1111/jcpp.13044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally R.J. Can network analysis transform psychopathology? Behav. Res. Ther. 2016;86:95–104. doi: 10.1016/j.brat.2016.06.006. [DOI] [PubMed] [Google Scholar]
- Mullarkey M.C., Marchetti I., Beevers C.G. Using Network Analysis to Identify Central Symptoms of Adolescent Depression. J. Clin. Child & Adolescent Psychol. 2019;48:656–668. doi: 10.1080/15374416.2018.1437735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuijten M.B., Deserno M.K., Cramer A.O.J., Borsboom D. Mental disorders as complex networks: an introduction and overview of a network approach to psychopathology. Clin. Neuropsychiatry: J. Treatment Eval. 2016;13:68–76. [Google Scholar]
- Opsahl T., Agneessens F., Skvoretz J. Node centrality in weighted networks: generalizing degree and shortest paths. Soc. Networks. 2010;32:245–251. [Google Scholar]
- Pan X., Xiao Y., Ren D., Xu Z.M., Zhang Q., Yang L.Y., Liu F., Hao Y.S., Zhao F., Bai Y.H. Prevalence of mental health problems and associated risk factors among military healthcare workers in specialized COVID-19 hospitals in Wuhan, China: a cross-sectional survey. Asia Pac Psychiatry. 2020:e12427. doi: 10.1111/appy.12427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parveen A., Inayat S. Evaluation of factors of stress among Nursing Students. Advanced Practices in Nursing. 2017;2:136. [Google Scholar]
- Payton J. 2020. Tools For Identifying Important Nodes in Networks.https://cran.r-project.org/web/packages/networktools/index.html Assessed by. [Google Scholar]
- Phua D.Y., Chen H., Chong Y.S., Gluckman P.D., Broekman B.F.P., Meaney M.J. Network Analyses of Maternal Pre- and Post-Partum Symptoms of Depression and Anxiety. Front. Psychiatry. 2020;11:785. doi: 10.3389/fpsyt.2020.00785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Core Team R. R Foundation for Statistical Computing; Vienna, Austria: 2020. R: A language and Environment For Statistical Computing. [Google Scholar]
- Revelle W. 2020. Procedures For Psychological, Psychometric, and Personality Research.https://cran.r-project.org/web/packages/psych/index.html Assessed by. [Google Scholar]
- Rogers M.L., Hom M.A., Joiner T.E. Differentiating acute suicidal affective disturbance (ASAD) from anxiety and depression Symptoms: a network analysis. J. Affect. Disord. 2019;250:333–340. doi: 10.1016/j.jad.2019.03.005. [DOI] [PubMed] [Google Scholar]
- Rouquette A., Pingault J.-.B., Fried E.I., Orri M., Falissard B., Kossakowski J.J., Vitaro F., Tremblay R., Cote S.M., Borsboom D. Emotional and Behavioral Symptom Network Structure in Elementary School Girls and Association With Anxiety Disorders and Depression in Adolescence and Early Adulthood: a Network Analysis. JAMA Psychiatry. 2018;75:1173–1181. doi: 10.1001/jamapsychiatry.2018.2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell B.S., Hutchison M., Tambling R., Tomkunas A.J., Horton A.L. Initial Challenges of Caregiving During COVID-19: caregiver Burden, Mental Health, and the Parent-Child Relationship. Child Psychiatry Hum. Dev. 2020;51:671–682. doi: 10.1007/s10578-020-01037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savitsky B., Findling Y., Ereli A., Hendel T. Anxiety and coping strategies among nursing students during the covid-19 pandemic. Nurse Educ. Pract. 2020;46 doi: 10.1016/j.nepr.2020.102809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmittmann V.D., Cramer A.O.J., Waldorp L.J., Epskamp S., Kievit R.A., Borsboom D. Deconstructing the construct: a network perspective on psychological phenomena. New Ideas Psychol. 2013;31:43–53. [Google Scholar]
- Shim E.J., Ha H., Park J.E., Kim B.S., Chang S.M., Hong J.P., Cho M.J., Hahm B.J. Gender-based examination of the association between individual symptoms of alcohol use disorder, major depressive disorder, and suicidal behaviors: a network analysis of data from the Korean Epidemiologic Catchment Area Study. J. Affect. Disord. 2020;272:432–439. doi: 10.1016/j.jad.2020.03.162. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Sun D., Yang D., Li Y., Zhou J., Wang W., Wang Q., Lin N., Cao A., Wang H., Zhang Q. Psychological impact of 2019 novel coronavirus (2019-nCoV) outbreak in health workers in China. Epidemiol. Infect. 2020;148:e96. doi: 10.1017/S0950268820001090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toohey M.J., DiGiuseppe R. Defining and measuring irritability: construct clarification and differentiation. Clin. Psychol. Rev. 2017;53:93–108. doi: 10.1016/j.cpr.2017.01.009. [DOI] [PubMed] [Google Scholar]
- Treadway M.T., Zald D.H. Reconsidering anhedonia in depression: lessons from translational neuroscience. Neurosci. Biobehav. Rev. 2011;35:537–555. doi: 10.1016/j.neubiorev.2010.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Borkulo C.D., Boschloo L., Kossakowski J.J., Tio P., Schoevers R.A., Borsboom D., Waldorp L.J. A permutation test; 2017. Comparing Network Structures On Three Aspects. [DOI] [PubMed] [Google Scholar]
- Venugopal V.C., Mohan A., Chennabasappa L.K. Status of mental health and its associated factors among the general populace of India during COVID-19 pandemic. Asia Pac Psychiatry. 2020:e12412. doi: 10.1111/appy.12412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Hu Z., Feng Y., Wilson A., Chen R. Changes in network centrality of psychopathology symptoms between the COVID-19 outbreak and after peak. Mol. Psychiatry. 2020;25:3140–3149. doi: 10.1038/s41380-020-00881-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. Mental Health and COVID-19.https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/publications-and-technical-guidance/noncommunicable-diseases/mental-health-and-covid-19 Assessed by. [Google Scholar]
- Wu W., Zhang Y., Wang P., Zhang L., Wang G., Lei G., Xiao Q., Cao X., Bian Y., Xie S., Huang F., Luo N., Zhang J., Luo M. Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy. J. Med. Virol. 2020;92:1962–1970. doi: 10.1002/jmv.25914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang Y.T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The lancet. PsychiatryPsychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang W.H., Li L., Xiao L.H., Peng F., Liu H.H. Screening for depressive disorder in adolescents: validity of Chinese version of the Patients Health Questionnaire 2-Item. Chin. J. Clin. Psychol. 2015;023:937–943. [Google Scholar]
- Zhang W.R., Wang K., Yin L., Zhao W.F., Xue Q., Peng M., Min B.Q., Tian Q., Leng H.X., Du J.L., Chang H., Yang Y., Li W., Shangguan F.F., Yan T.Y., Dong H.Q., Han Y., Wang Y.P., Cosci F., Wang H.X. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother. Psychosom. 2020;89:242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng R., Zhou Y., Fu Y., Xiang Q., Cheng F., Chen H., Xu H., Fu L., Wu X., Feng M., Ye L., Tian Y., Deng R., Liu S., Jiang Y., Yu C., Li J. Prevalence and associated factors of depression and anxiety among nurses during the outbreak of COVID-19 in China: A cross-sectional study. Int. J. Nurs. Stud. 2021;114:103809. doi: 10.1016/j.ijnurstu.2020.103809. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.