Abstract
Odontomas are common benign odontogenic tumors, being often detected on routine radiographs during the first two decades of life. Rarely, odontoma can interfere with jaw movements, causing mouth opening limitation. A 28-year-old male patient was referred complaining of restriction of mouth opening and mandibular movements, which started 6 months ago. Clinical examination revealed a painless increase of volume on the right maxilla, which interfered the mandibular movements, being associated with pain in these attempts. A well-defined, oval radiopaque lesion in close relationship with the impacted maxillary right third molar was detected in tomographic reconstructions. A surgical excision of the lesion was performed, and microscopy revealed complex odontoma. After 4 months of follow-up, the patient achieved adequate mouth opening and recovered mandibular movements. In the current case, the lesion was placed in a difficult access site, which directly interfered with the displacement of coronoid process. Odontoma should be included in the differential diagnosis when assessing causes of restricted mouth opening.
Keywords: odontogenic hamartoma, odontoma, restricted mouth opening, surgical approach
Introduction
Odontoma is the most common odontogenic tumor, representing from 21% to 67% of all odontogenic tumors. Because of their typically indolent behavior, odontomas are best defined as tumor-like malformations (hamartomas), constituted by epithelial and mesenchymal tissues.[1] According to their clinicopathological features, it can be classified as compound odontoma, when the malformation bear similarity to teeth or present as small teeth, or complex odontoma, when an amorphous mass is detected.[1,2] Odontomas are asymptomatic lesions, often detected during routine radiographs in the first two decades of life, without gender predilection.[1] Conservative surgical removal is the choice of treatment, the prognosis is excellent.[2,3]
Mouth opening limitation can have several causes, with most cases involving temporomandibular joint (TMJ) disorders, TMJ osteoarthritis, and masticatory muscle disorders. Moreover, other causes include trauma, radiotherapy, surgery, neoplasm, and autoimmune disease.[4-7]
This report describes an unusual case of a large-sized complex odontoma, located on the right posterior maxilla, restricting the mouth opening in a young male patient.
Case Presentation
A 28-year-old male patient was referred complaining of difficulties in mouth opening, which started 6 months ago. Because of restricted amplitude of mandibular movements, his feeding was limited to soft and small-pieced food. The patient denied any previous history of trauma or surgery. The extraoral examination evidenced symmetric facial proportions and no clinical signs of fractures [Figure 1a].
Figure 1.
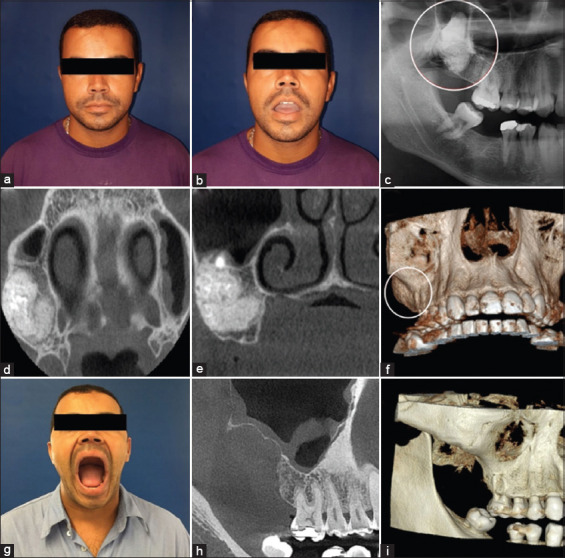
(a) Pre-operatory frontal view. (b) Restriction of the mouth opening. (c) Panoramic radiograph showing a large radiopaque lesion involving the impacted maxillary right third molar (circle) (Panoramic dental X-ray). (d) Axial view evidencing expansion of vestibular cortical bone (cone beam computed tomography [CBCT]). (e) Frontal view and relationship to the maxillary sinus (CBCT). (f) 3-D Reconstruction (CBCT) exhibiting the increased cortical bone expansion (circle). (g) After 4 months of follow-up, frontal view with normal range of mouth opening. (h) After 1 month of follow-up (CBCT), no residual lesion or recurrence. (i) 3-D reconstruction (CBCT) after 1 month of follow-up, without alterations in the lesional area. At the top, notice the pterygoid plate of the sphenoid bone
The mandibular dynamics, associated with pain, were highly restricted. The mouth opening was 25 mm, the left lateral movement was 2 mm, and the protrusion movement was about 1 mm [Figure 1b]. Intraoral examinations revealed an expansion of vestibular cortical bone I on the right maxillary tuberosity, measuring about 1 cm in its largest diameter, with hard consistency; however, the oral mucosa presented without alterations. The maxillary right second and third permanent molars were missing, with the patient reporting extraction of the second permanent molar in the adolescence.
The panoramic radiograph (panoramic dental X-ray) evidenced a well-defined radiopaque mass involving the impacted maxillary right third permanent molar [Figure 1c]. Through cone beam computed tomography (CBCT; EAGLE 3D® - Dabi Atlante; On Demand 3D Dental software; 1-mm-thick images), a well-defined hyperdense lesion measuring 24.1 mm × 21.4 mm × 20.3 mm, associated with expansion of the vestibular cortical bone, was observed [Figure 1d-f]. The hyperdense mass was closely related to the maxillary sinus, with 8 mm of bone expansion to the infratemporal fossa. These findings strongly indicated interference of the coronoid process movement.
The surgical procedure was performed under general anesthesia, without complications. The placement of a bite-block device was infeasible due to limited mouth opening. Two linear incisions were performed distal to the first molar, one on the alveolar ridge and another toward to the deep of the vestibular sulcus [Figure 2a and b]. Using electric surgical handpieces, the osteotomy was performed with a taper fissure crosscut carbide no. 701 surgical bur carefully to cut only buccal cortical aiming to preserve palatine bone and avoiding damage the maxillary sinus membrane and structures related to the pterygomaxillary fissure. Excision of the lesion was conducted using manual instruments and edges were just finished using abrasion bur. The surgical area was washed to remove small fragments. The palatine process and the related blood vessels were preserved, and no excessive bleeding was observed. After removal of the lesion, the surrounding soft tissue was used directly to close the oroantral communication, without the need for complex maneuvers. Occlusive 4-0 polyglactin suture was conducted, and ketoprofen 100 mg every 12 h, for 3 days, for post-operative analgesia was indicated. By histopathological analysis, the lesion presented both amorphous calcified deposit (enamel matrix and irregular dentine) and soft tissue (pulp-like tissue) components, being consistent with complex odontoma [Figure 2c and d].
Figure 2.
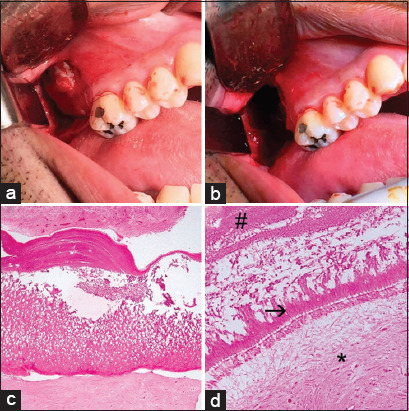
Trans-operatory view. (a) Intraoral access of the lesion. (b) Surgical cavity after removal of the lesion. Histopathological analysis (Hematoxylin and eosin stain). (c) Panoramic view showing cementoid, irregular dentin, and enamel matrix surrounded by fibrous connective tissue (×10 magnification). (d) Microscopical details showing dental pulp tissue (*) and hard tissue composed by irregular tubular dentin (black arrow) and enamel matrix (#) (×40 magnification). Notice the hamartomatous nature of these dental tissues
The patient recovered well [Figure 1g-i], and the mandibular movements were gradually reestablished. Notoriously, it happened after 1 week of the surgical treatment, until the 4th month of follow-up, where the patient recovered the amplitude of mandibular movements. Our service has the support of a multidisciplinary team for all patients with surgical treatment. In the current case, the gradual mandibular movements were controlled and recorded by an experienced professional. The patient was followed up for 1 year, after which he did not return for the scheduled assessments.
Discussion
In the present study, we reported, for the 1st time, a case involving mouth opening limitation due to a complex odontoma. The location of this odontogenic lesion on the right maxillary tuberosity, generating expansion of the vestibular cortical bone, provoked interference with the coronoid process movements, and mandibular dynamics.
This limitation of the mouth opening imposed serious health implications, including impaired mastication affecting the nutrition, speech difficulties, and compromised oral hygiene. However, after surgical removal of the lesion, the patient recovered the mandibular movements and amplitude of mouth opening.
The most causes of mouth opening limitation often involve anterior disc displacement without reduction of the TMJ, TMJ osteoarthritis, and masticatory muscle disorders, followed by trauma, radiotherapy, surgery third molar extraction, TMJ lesions, among others, autoimmune disease (lupus erythematosus and scleroderma), coronoid hyperplasia, and neoplasm.[4-7] Moreover, infection (odontogenic origin, otitis media, and mastoiditis), burn injury, drug toxicity, ankyloses, and meniscal pathology should be also considered.[6] In head-and-neck cancer, mouth opening limitation can result from local invasion of the primary or metastatic neoplasm into masseter and pterygoid muscles, neural structures, and TMJ tissues.[6,8]
The treatment of limited mouth opening can be by non-surgical conservative approach or surgical approach and, in some cases, a combination of them. Fortunately, the most patients achieve good symptomatic relief with non-invasive management. Regarding the surgical techniques, they can vary from arthroscopic surgery to TMJ prosthesis and distraction osteogenesis.[5] However, the treatment depends exclusively upon detailed clinical evaluation and diagnosis of each patient. Thus, in our case, the surgical removal of the odontoma was sufficient to solve the mouth opening limitation.
Radiopaque lesions of odontogenic origin in the jaws, such as observed in the current case, can be diagnosed as odontoma, calcifying epithelial odontogenic tumor, adenomatoid odontogenic tumor, dentinogenic ghost cell tumor, and calcifying odontogenic cyst. Interestingly, according to the recent WHO classification (2017), ameloblastic fibro-odontoma probably represents immature stages of either compound or complex odontoma.[1] Thus, it was not considered in the differential diagnosis.[9-12]
By histopathology, odontomas are composed by mixed epithelial and mesenchymal tumor-like malformations. Compound odontomas consist of multiple small teeth-like structures presenting dentin, cementum, enamel matrix, and pulp-like tissues. On the other hand, complex odontomas exhibit mature tubular dentine forming a homogeneous mass rounding empty spaces. The etiopathogenesis of odontomas is unknown, with some hypothesis suggesting trauma during primary dentition, as well as hereditary and sporadic genetic mutations. In fact, odontomas can be found in patients with Gardner syndrome, Hermann syndrome, cleidocranial dysplasia, familial colonic adenomatosis, and nevoid basal cell carcinoma syndrome.[2] The current case denied trauma and other possible causes were excluded, including genetic diseases.
The treatment of odontomas basically consists in conservative surgical excision.[3,13] In the current case, significantly, the surgery also aimed at restoring anatomical contours of the maxillary tuberosity to restore the dynamic of the coronoid process movements. The mouth opening gradually recovered, and after 4-month of follow-up, it was stable and comparable to the mandibular movements before detecting the odontoma.
Despite difficulty in accessing the lesion, the surgical procedure was performed through an intraoral approach. Korpi et al.[14] describe a more aggressive technique by performing Le Fort I fracture in the posterior maxilla and those close to maxillary sinus aiming to reduce complications, as face deformities caused by bone defects, oroantral communication, or incomplete removal of the lesion. Our therapeutic approach was based on the surgical management proposed by Gupta and Das,[15] which performed a more conservative access favoring a comfortable and faster recovering of the patient by intraoral access.
Conclusion
In summary, odontoma is an indolent tumor-like proliferation, usually diagnosed on routine radiographs. However, rarely, due to marked cortical expansion, odontoma can cause damages and discomfort of some anatomical structures limiting the mouth opening. In these cases, conservative surgical excision is successful, allowing the mandibular movement restoration.
Authors’ Declaration Statements
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Availability of data and material
The data used in this study are available and will be provided by the corresponding author on a reasonable request.
Conflict of Interest
All authors declare that they have no conflict of interest.
Acknowledgments
The authors are grateful to the Laboratory of Oral Histopathology, School of Dentistry of Ribeirão Preto, University of São Paulo (FORP/USP), for the valuable contribution in the diagnostic procedures.
References
- 1.El-Naggar AK, Chan JK, Grandis JR, Takata T, Slootweg PJ. WHO Classification of Head and Neck Tumours. 4th ed. Lyon, FR: International Agency for Research on Cancer; 2017. [Google Scholar]
- 2.Hidalgo-Sánchez O, Leco-Berrocal MI, Martínez-González JM. Metaanalysis of the epidemiology and clinical manifestations of odontomas. Med Oral Patol Oral Cir Bucal. 2008;13:E730–4. [PubMed] [Google Scholar]
- 3.Kämmerer PW, Schneider D, Schiegnitz E, Schneider S, Walter C, Frerich B, et al. Clinical parameter of odontoma with special emphasis on treatment of impacted teeth-a retrospective multicentre study and literature review. Clin Oral Investig. 2016;20:1827–35. doi: 10.1007/s00784-015-1673-3. [DOI] [PubMed] [Google Scholar]
- 4.Kim SM, Lee JH, Kim HJ, Huh JK. Mouth opening limitation caused by coronoid hyperplasia:A report of four cases. Korean Assoc Oral Maxillofac Surg. 2014;40:301–7. doi: 10.5125/jkaoms.2014.40.6.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ashmmam M, Rhab M. Limited mouth opening causes and its treatment modalities among peoples in Al-Khoms, Libya. IOSR J Dent Med Sci. 2018;17:67–70. [Google Scholar]
- 6.Goldstein M, Maxymiw WG, Cummings BJ, Wood RE. The effects of antitumor irradiation on mandibular opening and mobility:A prospective study of 58 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:365–73. doi: 10.1016/s1079-2104(99)70044-2. [DOI] [PubMed] [Google Scholar]
- 7.Poveda-Roda R, Bagán JV, Sanchis JM, Margaix M. Pseudotumors and tumors of the temporomandibular joint. A review. Med Oral Patol Oral Cir Bucal. 2013;18:e392–402. doi: 10.4317/medoral.18799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rapidis AD, Dijkstra PU, Roodenburg JL, Rodrigo JP, Rinaldo A, Strojan P, et al. Trismus in patients with head and neck cancer:Etiopathogenesis, diagnosis and management. Clin Otolaryngol. 2015;40:516–26. doi: 10.1111/coa.12488. [DOI] [PubMed] [Google Scholar]
- 9.Curé JK, Vattoth S, Shah R. Radiopaque jaw lesions:An approach to the differential diagnosis. Radiographics. 2012;32:1909–25. doi: 10.1148/rg.327125003. [DOI] [PubMed] [Google Scholar]
- 10.Dewan HS, Dewan SK, Bahl S, Parekh PT. Cemento-ossifying fibroma of mandible mimicking complex composite odontome. BMJ Case Rep. 2016;2016:216053. doi: 10.1136/bcr-2016-216053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teixeira LR, dos Santos JL, Almeida LY, Nelem-Colturato CB, de Paula RF, Oliveira FR, et al. Residual cementoblastoma:An unusual presentation of a rare odontogenic tumor. J Oral and Maxillof Surg Med and Pathol. 2018;30:187–90. [Google Scholar]
- 12.Kaplan I, Nicolaou Z, Hatuel D, Calderon S. Solitary central osteoma of the jaws:A diagnostic dilemma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e22–9. doi: 10.1016/j.tripleo.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 13.de Vasconcellos Machado C, Knop LA, da Rocha MC, Telles PD. Impacted permanent incisors associated with compound odontoma. BMJ Case Rep. 2015;2015:208201. doi: 10.1136/bcr-2014-208201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Korpi JT, Kainulainen VT, Sandor GK, Oikarinen KS. Removal of large complex odontoma using Le Fort I osteotomy. J Oral Maxillofac Surg. 2010;68:950–1. doi: 10.1016/j.joms.2009.04.105. [DOI] [PubMed] [Google Scholar]
- 15.Gupta M, Das D. Extensive complex odontoma in the maxillary sinus pushing 3rd molar near the orbital floor causing transient diplopia and chronic sinusitis:A rare presentation and surgical management. J Maxillofac Oral Surg. 2015;14:338–40. doi: 10.1007/s12663-013-0561-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used in this study are available and will be provided by the corresponding author on a reasonable request.


