Abstract
Objective
A salient disturbance in anorexia nervosa (AN) is the persistent restriction of food intake. Eating behavior in AN is thought to be influenced by anxiety. The current study probed associations between mealtime anxiety and food intake among individuals with AN and healthy comparison individuals (HC).
Method
Data were combined across three studies (total of 92 AN and 78 HC) for secondary data analysis. Participants completed a multi-item laboratory buffet meal and visual analogue scale assessments of pre- and post-meal anxiety. Linear regression models assessed the association between mealtime anxiety and calorie and fat intake at the meal, and whether associations differed by diagnostic group.
Results
Among individuals with AN, pre-meal anxiety was significantly associated with reduced calorie intake and reduced consumption of calories from fat at the meal; these associations were not observed among HC. There was no evidence for an association between calorie/fat intake at the meal and post-meal anxiety in either group.
Discussion
Treatments that target mealtime anxiety may improve eating and nourishment among individuals with AN. Interventions like exposure therapy that provide skills in overcoming mealtime anxiety might be enhanced by informing patients that post-meal anxiety is not related to intake.
Keywords: anorexia nervosa, anxiety, eating behavior
Introduction
Anorexia nervosa (AN) is characterized by persistent restriction of food intake (American Psychiatric Association, 2013), with particular restriction of dietary fat (Schebendach et al., 2019), such that a significantly low body weight is maintained. This restrictive eating behavior is extremely resistant to change, and does not normalise following successful inpatient treatment in which weight restoration is achieved (Foerde et al., 2021; Mayer et al., 2012; Schebendach et al., 2011). More restrictive eating at discharge, characterized by limited variety and energy density, is associated with poorer outcomes among individuals with AN (Schebendach et al., 2012; Schebendach et al., 2008; Schebendach et al., 2011). Anxiety around eating is common in AN (Forrest et al., 2018; Hildebrandt et al., 2012), and many have suggested that anxiety perpetuates restrictive eating (Kaye, 2008; (Kaye, 2008; Lloyd et al., 2017; Pallister & Waller, 2008; Steinglass et al., 2011; Strober, 2004; Treasure et al., 2020). Here, data were pooled across studies to create a large dataset of objective, laboratory assessments of intake. Associations were examined between calorie/fat intake, and anxiety before/after the meal, among individuals with AN, as compared with healthy comparison individuals (HC).
While the association between anxiety and eating in AN has long been recognized, there are different considerations about the precise nature of this relationship. Some emphasize the role of fear-based processes, suggesting pre-meal anxiety affects momentary intake, to provide a rationale for addressing pre-meal anxiety within treatment (Steinglass et al., 2011). Pre-meal anxiety is related to food intake amongst individuals with AN (Steinglass et al., 2010). A motivational video encouraging food intake was associated with increased intake and reduced anxiety amongst individuals with AN (Cardi et al., 2011). A pharmacologic intervention targeting pre-meal anxiety failed to reduce anxiety or increase intake (Steinglass, Kaplan, et al., 2014). Others suggest eating stimulates anxiety in AN, and that dietary restriction reduces this anxiety (Hart et al., 2013; Kaye et al., 2003; Kaye, 2008; Nunn et al., 2012). To our knowledge this is unexplored, but if supported would encourage addressing negative reinforcement processes within AN treatment.
The current study extends existing research by examining fear-based and negative reinforcement models, testing the relationship of both pre-meal and post-meal anxiety with calorie and fat intake. We hypothesized that 1) greater pre-meal anxiety would be associated with reduced caloric intake, and reduced consumption of calories from fat, among individuals with AN as compared with HC; and 2) greater caloric intake/proportion of calories consumed from fat, would be associated with greater post-meal anxiety among individuals with AN, relative to HC.
Methods
The current study comprises secondary analysis of data combined across three studies of AN (one ongoing, two completed; (Foerde et al., 2020; Steinglass et al., 2015)) at the New York State Psychiatric Institute (NYSPI). Each study administered a laboratory-based multi-item meal, and mealtime anxiety assessments. Some of the food intake data are published (Foerde et al., 2020; Steinglass et al., 2015), but mealtime anxiety data are not.
Data from seven patients with AN binge-eating/purging subtype were excluded because the meal met criteria for being a binge meal (patient endorsed a binge and consumed an uncharacteristically large amount of food). The exclusion of binge meals was to avoid conflating restrictive and binge eating behaviors, which may be differentially associated with anxiety (Lavender et al., 2013). The small number of binge meals precluded exploring whether binge eating moderates associations between anxiety and intake in AN.
Participants
Participants were females with AN (n=92) and female HC (n=78), aged 13–40 years. Diagnoses were determined by the EDE (Fairburn et al., 1993)/EDA-5 (Sysko et al., 2015)). Exclusion criteria were current psychotropic medication use, psychotic disorder, current substance use disorder, history of a neurological disorder/injury, contraindication to MRI, and pregnancy. Additional exclusion criteria for HC included current/past psychiatric illness, significant medical conditions, and body mass index (BMI) outside of the 18.5–25 kg/m2 range.
Patients with AN were receiving inpatient (n=73) or outpatient (n=19) treatment. 55 individuals with AN had restricting subtype (59.78%). Procedures occurred at the beginning of treatment. HC were recruited from the community. All studies were approved by the NYSPI Institutional Review Board. Participants provided written informed consent (or assent with parental written consent, for participants under 18 years).
Procedures
Laboratory Multi-item Meal (Sysko et al., 2018)
The laboratory meal comprised a 25-item ad-libitum buffet in the eating laboratory at NYSPI. In two studies, the meal occurred at lunchtime and in one the meal was at dinnertime (contents were the same). Participants received a standardized research meal (~300 kcal or ~550 kcal lunch) 5 hours prior to the laboratory meal and asked not to consume anything (except water) between the standardized meal and the laboratory meal. Food items at the laboratory meal ranged in fat content; for example, grilled chicken, fried chicken, fruit salad, Oreo cookies, water and soda (for full list see (Sysko et al., 2018)). Participants were instructed that “This is your lunch/dinner for today. Eat as much or as little as you like. How you determine that is up to you”. Participants had up to one hour to complete the meal, and rang a bell to signal the end of the meal. Food was weighed before and after the meal (Acculab 7200 balance, readability 0.1g), and amount consumed in grams, kcal, and macronutrient content (e.g., % kcal from fat) calculated.
Psychological Assessments
Mealtime anxiety was assessed in the eating laboratory in the presence of the buffet, prior to meal instructions, and again after the participant completed the meal. Participants rated their anxiety using pen and paper visual analogue scales (VAS) anchored by “not at all” and “extremely”. The ratings were converted to numeric values between 0 and 100.
Eating disorder severity was assessed using the EDE-Q (Fairburn & Beglin, 1994), trait anxiety was assessed with the Spielberger Trait Anxiety Inventory (STAI; (Spielberger et al., 1970)), and depression symptoms assessed with the Beck Depression Inventory (Beck et al., 1988).
Data analysis
All analyses were completed in R (R Core Team, 2017).
Linear regression models (including study as a covariate) assessed group differences (AN versus HC) in age, psychological measures, mealtime anxiety, and intake variables (calories and % calories from fat). A multi-level linear regression model, including participant as a random effect, and diagnostic status, time, and their interaction, as fixed effects, assessed whether anxiety changed from pre- to post-meal, and whether this change differed by diagnostic status.
Linear regression models assessed the association of pre-meal anxiety, diagnosis, and their interaction, with intake variables. Linear regression models also assessed the association of intake, diagnosis, and their interaction, with post-meal anxiety; these models were adjusted for pre-meal anxiety. All models included study and age as covariates. Where interactions were supported, the association between anxiety and intake was estimated in AN and HC groups separately. When associations were supported within the patient group, analyses including additional covariates (STAI, BDI, EDEQ, illness duration, BMI) were completed, to minimise the risk of associations reflecting the influence of a third factor (i.e. confounding).
The main analyses probing associations between mealtime anxiety and food intake amongst AN and HC were replicated with adjustment for meal start time and duration rather than adjustment for study. Outcomes are reported in the Supplement.
Results
Demographic and clinical characteristics are presented in Table 1. Individuals with AN had higher scores on clinical measures and ate less at the meal. For a detailed description of participants by study and diagnosis, see the Supplement (Table S1).
Table 1:
Demographic and clinical characteristics of participants
| Variable | Mean (SD) | P for between group differencea | |
|---|---|---|---|
| AN (n=92) | HC (n=78) | ||
| Age (years) | 21.53 (7.31) | 21.99 (5.6) | 0.036 |
| Duration Illness (years) | 6.01 (7.08) | NA | NA |
| BMI (kg/m2) | 16.56 (1.77) | 21.29 (1.85) | <0.001 |
| BMI percentile (%) | 7.33 (10.20) | 46.20 (20.70) | <0.001 |
| BAIa | 22.12 (12.02) | 3.71 (5.04) | <0.001 |
| BDIa | 27.08 (12.14) | 1.55 (2.44) | <0.001 |
| STAI (T)a | 60.00 (11.85) | 31.36 (6.78) | <0.001 |
| EDEQ Eating Concernsa | 3.15 (1.65) | 0.14 (0.36) | <0.001 |
| EDEQ Restrainta | 3.92 (1.94) | 0.40 (0.84) | <0.001 |
| EDEQ Shape Concernsa | 4.40 (1.58) | 0.51 (0.65) | <0.001 |
| EDEQ Weight Concernsa | 4.16 (1.7) | 0.43 (0.63) | <0.001 |
| Global EDE Q scorea | 3.92 (1.53) | 0.37 (0.55) | <0.001 |
| Pre-meal anxiety (VAS rating) | 63.79 (32.24) | 11.58 (17.65) | <0.001 |
| Post-meal anxiety (VAS rating) | 70.11 (27.25) | 6.96 (11.44) | <0.001 |
| Caloric intake at meal (kcal) | 386.68 (370.3) | 866.34 (343.8) | <0.001 |
| Fat intake at meal (% total kcal) | 21.26 (14.24) | 37.53 (7.22) | <0.001 |
| Fat intake at meal (g) | 13.09 (17.19) | 37.61 (18.78) | <0.001 |
| Comorbid Anxiety Disorder (n) | 30 | NA | NA |
from linear regression of variable on diagnosis (adjusted for study).
BAI: Beck anxiety inventory, BDI: Beck depression inventory, BMI: Body mass index; EDEQ: Eating disorder examination questionnaire, STAI T: Spielberger state-trait anxiety inventory trait anxiety subscale, SRHI: self-report habit index, VAS: visual analogue scale rating.
The multilevel model indicated that mealtime anxiety was greater amongst individuals with AN compared to HC (B=28.84, 95% CI: 25.68, 32.00, p < 0.001). Across all participants there was a main effect of time, with anxiety decreasing from pre- to post-meal (B=−2.81, 95% CI: −4.55, −0.93, p = 0.003). The diagnostic group by time interaction term was not significant (B=−0.43, 95% CI: −2.24, 1.38, p = 0.646).
Pre-meal anxiety and food intake
Greater pre-meal anxiety was significantly associated with reduced consumption of calories and % calories from fat at the meal, across AN and HC. Diagnostic status by pre-meal anxiety interaction terms were statistically significant: greater anxiety predicted reduced intake among individuals with AN, but not HC. Associations between premeal anxiety and food intake remained amongst patients when including clinical variables in statistical models.
Food intake and post-meal anxiety
There was no significant association between calorie/fat intake and post-meal anxiety among individuals with AN and HC. Terms for the interaction of calorie/fat intake with diagnostic status were not significant.
Outcomes of the main statistical tests were consistent whether adjusting for meal start time and duration, or study (Supplement, Table S2).
Results of analyses assessing the association between meal anxiety and intake are presented in Table 2 and Figure 1 below.
Table 2:
Linear regression model estimates of analyses probing associations between mealtime anxiety and food intake in AN and HC
| Caloric intake on pre-meal anxiety | Fat intakea on pre-meal anxiety | |||
|---|---|---|---|---|
| Variable | B [95% CI] | P Value | B [95% CI] | P Value |
| Pre-meal anxiety | −3.14[−5.62, −0.66] | 0.01 | −0.12[−0.2, −0.04] | <0.001 |
| Diagnostic status | −3.45[−110.34, 103.45] | 0.95 | 0.47[−2.91, 3.85] | 0.79 |
| Pre-meal anxiety: Diagnostic status | −3.35[−5.85, −0.85] | 0.01 | −0.13[−0.21, −0.05] | <0.001 |
| Post-hoc analyses | ||||
| Group | ||||
| AN | −6.49[−9.03, −3.95] | <0.001 | −0.24[−0.32, −0.16] | <0.001 |
| HC | 0.21[−4.08, 4.5] | 1.00 | 0.01[−0.13, 0.14] | 1.00 |
| AN (maximally adjusted modelb) | −4.13[−6.81, −1.46] | <0.001 | −0.17[−0.28, −0.05] |
0.01 |
| Post-meal anxiety on caloric intake | Post-meal anxiety on fat intakea | |||
| B [95% CI] | P Value | B [95% CI] | P Value | |
| Intake | 0.00[−0.01, 0.01] | 0.75 | 0.04[−0.34, 0.42] | 0.83 |
| Diagnosis | 9.79[0.5, 19.09] | 0.04 | 13.84[−1.14, 28.82] | 0.07 |
| Pre-meal anxiety | 0.58[0.42, 0.73] | <0.001 | 0.55[0.4, 0.71] | <0.001 |
| Intake: Diagnostic status | 0.00[−0.01, 0.01] | 0.41 | −0.03[−0.41, 0.36] | 0.89 |
N= 170 (92 AN, 78 HC)
All models adjusted for age and study,
fat intake describes percentage of total calories from fat,
models adjusted for STAI trait, BDI, global EDEQ, illness duration, and BMI, in addition to age and study (N=80).
Figure 1: Associations between mealtime anxiety and calorie/fat intake among individuals with anorexia nervosa and healthy controls.
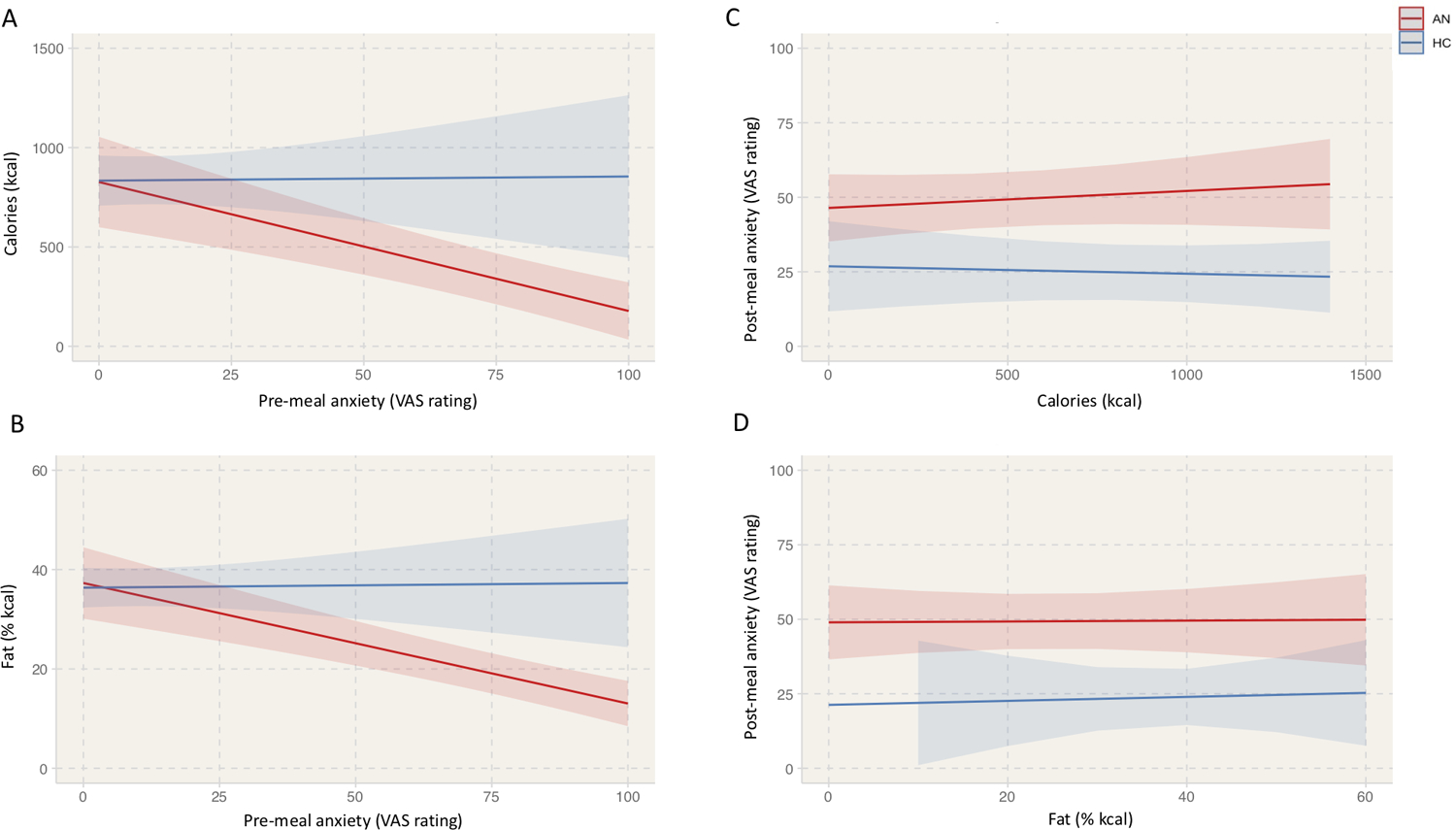
Predicted values of calorie (A) and fat intake (B) from the regression of each outcome on pre-meal anxiety, age, and study, as a function of pre-meal anxiety. Predicted values of post-meal anxiety from the regression of post-meal anxiety on caloric (C) or fat (D) intake, and pre-meal anxiety, age, and study, as a function of calorie/fat intake.
Discussion
This study tested relationships between mealtime anxiety and meal consumption among individuals with AN, as compared with HC. As expected, mealtime anxiety was higher among individuals with AN. This large combined study confirmed that greater anxiety prior to a meal was associated with lower intake of calories and dietary fat amongst individuals with AN. Fat is the most energy dense of macronutrients, and previous studies report a particular avoidance of fat by individuals with AN (Schebendach et al., 2019), which likely contributes to malnourishment, challenges with weight restoration, and risk of relapse (Schebendach et al., 2012; Schebendach et al., 2008). One additional, new, finding emerged, which was that post-meal anxiety was not related to calorie or fat intake, amongst individuals with AN and HC.
The findings have implications for strategies to help patients with AN improve nutritional intake. The pre-meal findings support the utility of treatments such as exposure and response prevention, which target pre-meal anxiety (Steinglass et al., 2011). Exposure therapy teaches patients to confront, rather than avoid, feared stimuli, by guiding patients through eating feared foods, while refraining from engaging in ritualised safety behaviors (e.g., tearing food into small pieces). Two studies have shown that exposure therapy can increase food intake in AN (Levinson et al., 2015; Steinglass, Albano, et al., 2014). The absence of an association between amount consumed and post-meal anxiety is important for the psychoeducational component of treatment. That is, despite patients’ beliefs, consuming fewer calories or less fat will not help in alleviating anxiety. The best predictor of anxiety following a meal was pre-meal anxiety, supporting the necessity of addressing pre-meal anxiety in treatment. There was a slight decrease in anxiety from pre- to post-meal across all participants, though the effect of time was fairly minimal relative to that of diagnosis.
Strengths of this study include the large and generalizable sample (including restricting and binge-eating/purging subtypes, inpatients and outpatients, adolescents and adults), and the objective assessment of food intake. Nonetheless, conclusions should be considered in light of several limitations. This study did not experimentally alter anxiety or amount consumed at the meal, and therefore cannot speak to causal relationships. Secondly, inferences about the association between mealtime anxiety and intake can only be made at the between-participant level. Existing data from ecological momentary assessment studies suggest that greater levels of daily anxiety are associated with greater restrictive eating on the same day within an individual (Haynos et al., 2015; Lavender et al., 2013); future studies may adopt a more granular approach, to determine how pre- and post-meal anxiety are associated with meal calorie/fat content at the within-person level. Such studies could consider a wider range of emotions, to evaluate the relative importance of anxiety in predicting food intake, or in negative reinforcement processes, in AN. The focus on anxiety to the exclusion of other factors is a limitation of the current study. Finally, findings apply only to non-binge meals, and we were unable to address whether the association between anxiety and intake differs at binge meals amongst individuals with AN. This could provide further information concerning how anxiety may affect disordered eating behavior.
The current study confirms the association between pre-meal anxiety and lower intake among individuals with AN, whilst adding that intake is not associated with post-meal anxiety. Outcomes support the importance of pre-meal anxiety in maintaining restrictive eating behavior in AN, and use of therapies that encourage overcoming pre-meal anxiety.
Supplementary Material
Acknowledgements and Conflicts of Interest
Funding information:
NIMH MH11445 (R01), MH105452 (R01), MH113737 (K24), Global Foundation for Eating Disorders.
Conflicts of interest:
Dr. Steinglass reports receiving royalties from UpTo Date. Dr. Walsh reports receiving royalties and honoraria from McGraw-Hill, Oxford University Press, UpToDate, British Medical Journal, Johns Hopkins University Press and Guidepoint Global. Dr Lloyd, Dr Schebendach, Dr Posner and Ms Powell have no conflicts of interest to report.
Data availability statement:
The data that support the findings of this study are available upon request from the corresponding author.
References
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub. [Google Scholar]
- Beck AT, Steer RA, & Carbin MG (1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical psychology review, 8(1), 77–100. [Google Scholar]
- Cardi V, Kan C, Roncero M, Harrison A, Lounes N, Tchanturia K, … Treasure J (2011). Mealtime support in anorexia nervosa: A within-subject comparison study of a novel vodcast intervention [JournalPeer Reviewed Journal]. Psychotherapy and Psychosomatics Vol, 81(1), 54–55. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, & Beglin SJ (1994). Assessment of eating disorders: Interview or self‐report questionnaire? International journal of eating disorders, 16(4), 363–370. [PubMed] [Google Scholar]
- Fairburn CG, Wilson GT, & Schleimer K (1993). Binge eating: Nature, assessment, and treatment. Guilford Press; New York. [Google Scholar]
- Foerde K, Schebendach JE, Davis L, Daw N, Walsh BT, Shohamy D, & Steinglass JE (2020). Restrictive eating across a spectrum from healthy to unhealthy: behavioral and neural mechanisms. Psychological Medicine, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foerde K, Walsh BT, Dalack M, Daw N, Shohamy D, & Steinglass JE (2021). Changes in brain and behavior during food-based decision-making following treatment of anorexia nervosa. J Eat Disord, 9(1), 48. 10.1186/s40337-021-00402-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest LN, Jones PJ, Ortiz SN, & Smith AR (2018). Core psychopathology in anorexia nervosa and bulimia nervosa: A network analysis. Int J Eat Disord, 51(7), 668–679. 10.1002/eat.22871 [DOI] [PubMed] [Google Scholar]
- Hart M, Wilcken B, Williams LT, Sibbritt D, & Nunn KP (2013). Tyrosine supplementation as an adjunct treatment in anorexia nervosa–a noradrenergic repletion hypothesis. In (Vol. 1, pp. 161–168). Advances in Eating Disorders. [Google Scholar]
- Haynos AF, Crosby RD, Engel SG, Lavender JM, Wonderlich SA, Mitchell JE, … Le Grange D (2015). Initial test of an emotional avoidance model of restriction in anorexia nervosa using ecological momentary assessment. J Psychiatr Res, 68, 134–139. 10.1016/j.jpsychires.2015.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildebrandt T, Bacow T, Markella M, & Loeb KL (2012). Anxiety in anorexia nervosa and its management using family-based treatment. European Eating Disorders Review, 20(1), e1–e16. 10.1002/erv.1071 [DOI] [PubMed] [Google Scholar]
- Kaye, Barbarich, Putnam, Gendall, Fernstrom, Fernstrom, … Kishore. (2003). Anxiolytic effects of acute tryptophan depletion in anorexia nervosa. International Journal of Eating Disorders, 33(3), 257–267. 10.1002/eat.10135 [DOI] [PubMed] [Google Scholar]
- Kaye W (2008). Neurobiology of anorexia and bulimia nervosa. Physiol Behav, 94(1), 121–135. 10.1016/j.physbeh.2007.11.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavender JM, De Young KP, Wonderlich SA, Crosby RD, Engel SG, Mitchell JE, … Le Grange D (2013). Daily Patterns of Anxiety in Anorexia Nervosa: Associations With Eating Disorder Behaviors in the Natural Environment. Journal of Abnormal Psychology, 122(3), 672–683. 10.1037/a0031823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson CA, Rodebaugh TL, Fewell L, Kass AE, Riley EN, Stark L, … Lenze EJ (2015). D-cycloserine facilitation of exposure therapy improves weight regain in patients with anorexia nervosa: A pilot randomized controlled trial. The Journal of Clinical Psychiatry, 76(6), e787–e793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd EC, Frampton I, Verplanken B, & Haase AM (2017). How extreme dieting becomes compulsive: A novel hypothesis for the role of anxiety in the development and maintenance of anorexia nervosa. Medical Hypotheses, 108(Supplement C), 144–150. 10.1016/j.mehy.2017.09.001 [DOI] [PubMed] [Google Scholar]
- Mayer LE, Schebendach J, Bodell LP, Shingleton RM, & Walsh BT (2012). Eating behavior in anorexia nervosa: before and after treatment. Int J Eat Disord, 45(2), 290–293. 10.1002/eat.20924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunn K, Frampton I, & Lask B (2012). Anorexia nervosa--a noradrenergic dysregulation hypothesis. Med Hypotheses, 78(5), 580–584. 10.1016/j.mehy.2012.01.033 [DOI] [PubMed] [Google Scholar]
- Pallister E, & Waller G (2008). Anxiety in the eating disorders: understanding the overlap. Clin Psychol Rev, 28(3), 366–386. 10.1016/j.cpr.2007.07.001 [DOI] [PubMed] [Google Scholar]
- Schebendach J, Mayer LE, Devlin MJ, Attia E, & Walsh BT (2012). Dietary energy density and diet variety as risk factors for relapse in anorexia nervosa: a replication. Int J Eat Disord, 45(1), 79–84. 10.1002/eat.20922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schebendach JE, Mayer LE, Devlin MJ, Attia E, Contento IR, Wolf RL, & Walsh BT (2008). Dietary energy density and diet variety as predictors of outcome in anorexia nervosa. Am J Clin Nutr, 87(4), 810–816. [DOI] [PubMed] [Google Scholar]
- Schebendach JE, Mayer LE, Devlin MJ, Attia E, Contento IR, Wolf RL, & Walsh BT (2011). Food choice and diet variety in weight-restored patients with anorexia nervosa [Journal Article Research Support, N.I.H., Extramural]. Journal of the American Dietetic Association, 111(5), 732–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schebendach JE, Uniacke B, Walsh BT, Mayer LE, Attia E, & Steinglass J (2019). Fat preference and fat intake in individuals with and without anorexia nervosa. Appetite, 139, 35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, & Lushene RE (1970). Manual for the state-trait anxiety inventory.
- Steinglass J, Foerde K, Kostro K, Shohamy D, & Walsh BT (2015). Restrictive food intake as a choice-A paradigm for study [Journal Peer Reviewed Journal]. International Journal of Eating Disorders. Vol., 48(1), 59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinglass JE, Albano AM, Simpson HB, Wang YJ, Zou JJ, Attia E, & Walsh BT (2014). Confronting Fear Using Exposure and Response Prevention for Anorexia Nervosa: A Randomized Controlled Pilot Study. International Journal of Eating Disorders, 47(2), 174–180. 10.1002/eat.22214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinglass JE, Kaplan SC, Liu Y, Wang Y, & Walsh BT (2014). The (lack of) effect of alprazolam on eating behavior in anorexia nervosa: a preliminary report. Int J Eat Disord, 47(8), 901–904. 10.1002/eat.22343 [DOI] [PubMed] [Google Scholar]
- Steinglass JE, Sysko R, Glasofer D, Albano AM, Simpson HB, & Walsh BT (2011). Rationale for the application of exposure and response prevention to the treatment of anorexia nervosa. Int J Eat Disord, 44(2), 134–141. 10.1002/eat.20784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strober M (2004). Pathologic fear conditioning and anorexia nervosa: On the search for novel paradigms. International Journal of Eating Disorders, 35(4), 504–508. 10.1002/eat.20029 [DOI] [PubMed] [Google Scholar]
- Sysko R, Glasofer DR, Hildebrandt T, Klimek P, Mitchell JE, Berg KC, … Walsh BT (2015). The eating disorder assessment for DSM-5 (EDA-5): Development and validation of a structured interview for feeding and eating disorders. The International journal of eating disorders, 48(5), 452–463. 10.1002/eat.22388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sysko R, Steinglass J, Schebendach J, Mayer LE, & Walsh BT (2018). Rigor and reproducibility via laboratory studies of eating behavior: A focused update and conceptual review. International Journal of Eating Disorders, 51(7), 608–616. [DOI] [PubMed] [Google Scholar]
- Team, R. C. (2017). R: A Language and Environment for Statistical Computing. In R Foundation for Statistical Computing. https://www.R-project.org/ [Google Scholar]
- Treasure J, Willmott D, Ambwani S, Cardi V, Clark Bryan D, Rowlands K, & Schmidt U (2020). Cognitive interpersonal model for anorexia nervosa revisited: the perpetuating factors that contribute to the development of the severe and enduring illness. Journal of Clinical Medicine, 9(3), 630. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available upon request from the corresponding author.


