Abstract
Background:
Asthma is a chronic respiratory disease that affects millions worldwide. Medication management is the current mainstay of treatment; however, there is evidence to suggest additional benefit with lifestyle changes, particularly with increased physical activity.
Objective:
Our systematic review aims to discover and evaluate the effects of physical activity on asthma outcomes.
Methods:
Systematic search of PubMed, EMBASE, CINAHL, Cochrane Library, Rehabilitation and Sports Medicine Source, Scopus, and Web of Science identified 11,155 results. Thirty-five articles met our inclusion criteria spanning 20 studies. Data extraction was conducted by six independent reviewers, and final results were evaluated by a seventh reviewer and the senior author.
Results:
Wide variation among selected studies, including the heterogeneity of interventions and outcome variables, did not support a meta-analysis. Mixed results of the effects of physical activity on asthma outcomes were found. Most studies suggest that physical activity improves asthma control, quality of life, lung function parameters, and inflammatory serologies, while three found no improvements in any of these outcomes. No studies reported worsening asthma outcomes.
Conclusion:
This review highlights the emerging and promising role of physical activity as a non-pharmacologic treatment for asthma. Additional high-quality randomized controlled trials are needed to overcome the problems of measurement heterogeneity and the dilution of outcome effect size measurement related to physical activity interventions for asthma.
Keywords: Asthma, Physical Activity, Exercise, Quality of Life, Control, Inflammation
Background
Asthma is a chronic respiratory disease that effects over 300 million individuals worldwide.(1) Current treatment guidelines for asthma include primarily medication management with anti-inflammatory medications and long-acting bronchodilators.(2) These therapies help manage symptoms, but despite appropriate prescribing practices, some patient’s asthma symptoms remain uncontrolled. (3) Obtaining optimal control of the disease is complicated by the cost and side-effects of the medications, as well as poor adherence.(3–6) To supplement medication management in many chronic diseases, studies describe the benefits of modifying lifestyle factors, such as physical activity.(7) In patients with asthma, this is more complex, as asthma symptoms can worsen or be triggered by physical activity and can lead to avoidance of physical activity.(8, 9) Low levels of physical activity have been associated with increased asthma symptoms, increase in healthcare utilization, and decreased quality of life.(10–14) Research over decades has demonstrated that lung expansion, as prompted by aerobic exercise, is a bronchodilator.(15) As such, current guidelines recommend that all patients with chronic diseases, including asthma, participate in regular physical activity for overall health benefits.(2, 16) Despite this recommendation, patients with asthma are less physically active than gender matched controls.(12, 13, 17, 18) Describing the risks and benefits of physical activity in asthma patients is necessary to improve and implement recommendations regarding this lifestyle intervention.
Previous studies have evaluated the effects of physical activity on asthma to further define its potential harms and benefits. Systematic reviews of this evidence have shown mixed results and do not include recent studies on physical activity in people living with asthma.(3, 19–21) Studies associate physical activity with improvement in days without asthma symptoms, quality of life, forced expiratory volume in 1 second (FEV1), maximal oxygen consumption, and exercise capacity.(22, 23) A prior systematic review found no statistically significant effects on lung function parameters, but did find a trend toward improved health related quality of life.(19) Other systematic reviews found varying results in mixed adult and pediatric populations, including increased aerobic power, and no change in fractional excretion of nitric oxide or bronchial hyperresponsiveness.(3, 20, 21) New evidence has emerged on the impact of physical activity in adult populations with asthma. Of the two more recent systematic reviews, one focused on adults only, but limited outcome data to asthma control, lung function and airway inflammation.(21, 24) Our study aims to comprehensively review and summarize the evidence of the disease-modifying effects of physical activity on asthma outcomes in adults.
Methods
This is a systematic review conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) and Cochrane guidelines.(25, 26) The protocol is registered in Prospero (registration number: CRD42017058804).
Data Sources
We conducted a comprehensive search on multiple databases for articles in English entered into the datasets from their respective inception dates to November 19, 2019 when the search strategy was implemented: PubMed (1946- ), EMBASE (1947- ), CINAHL (Cumulative Index to Nursing and Allied Health Literature –EBSCOhost, 1937- ), Cochrane Library (1996-), Rehabilitation and Sports Medicine Source (1963- ), Scopus (1788- ), and Web of Science (1970- ). The search strategy was developed by investigators (MK, SN, CC) in collaboration with a clinical librarian (MC) with expertise in systematic search and review (Table E1 in Online Repository).
The search strategy comprised 3 intersecting concept sets: (1) asthmatic and bronchospastic condition concepts, (2) exercise and physical activity interventional concepts, and (3) randomized controlled trials concepts (See Table E1 in the Online Repository for the Pubmed Search Strategy). The search of the electronic databases recalled a total of 11,155 non-unique records. These data were supplemented by manual examination of the reference lists of reviews (identified by a systematic search for reviews) and examination of the reference lists of all the articles that underwent full text review in the selection phase. The results of the electronic and supplemental searches are reported in the PRISMA Flow Diagram.
Study Selection
The study selection occurred over three phases: a screening phase, selection phase and a third data abstraction phase. The screening phase of the review was conducted by four trained reviewers (KW, AS, MK, AD) who screened titles/abstracts. Of the titles/ abstracts reviewed, 91 citations were selected for full-text review. Two independent reviewers (KW, AS, MK, AD) completed a checklist-style form and included articles which met inclusion criteria. The senior author (SN) and independent reviewer (CC) reviewed any discrepancies in the full-text review.
Inclusion criteria for the selection phase included: randomized controlled trials of physical activity interventions evaluating adult subjects (≥18 years old) with a known diagnosis of asthma. Further description of inclusion criteria is available in the online repository.
Data abstraction
Six (KW, SN, VP, MK, AS, IR) independent investigators extracted data from included full-text articles and published abstracts. See details of extracted characteristics in the online repository. An independent investigator (CC) reviewed these characteristics for discrepancies and combined all extracted data into one dataset. Any discrepancies were reviewed with the senior author (SN) and independent investigator (CC). To address the limited data available in published abstracts, we attempted to contact investigators to obtain key study characteristics.
Risk of bias assessment
One independent investigator (SK), with expertise in systematic review methodology evaluated each included study for risk of bias. The principal investigator guided a discussion with the investigator for any discrepancies in assessment of study bias. The independent investigator (SK) used the Cochrane Risk for Bias tool as a guide for his assessment. This tool guided the reviewer in examining random sequence allocation, concealed allocation, blinding of participants and personal, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. The principal investigator reviewed any inconsistencies in data extraction.
Data analysis
Due to heterogeneity of the interventions, outcome measurements, and reporting of outcomes, no meta-analysis was conducted. We exported data by outcome of interest and analyzed results by direction of effect and statistical significance. We employed vote counting to qualitatively evaluate these results of the included studies. Vote counting compares specific outcomes by adding the overall effect reported in the results of various studies. For example, it describes the number of studies that demonstrate positive effect for a particular outcome. Additionally, it counts the number of studies that report a statistically significant result for a given outcome. We report the direction of effect and the statistical significance for each outcome of interest in one of five categories. The direction of effects was defined as: 1) Positive effect with statistical significance; 2) Positive effect without statistical significance; 3) No difference between intervention and control groups 4) Negative effect with statistical significance; 5) Negative effect without statistical significance. In cases where authors did not report an effect size or direction of effect in a qualitative manner and only reported no statistical significance between groups, we coded those as having no difference between the intervention and control groups. Although vote counting is not a universally accepted means of data synthesis, we apply this method to our data, as there were no adequate alternative methods to summarize the diverse data set.(26)
Results
Study Selection
A total of 11,155 citations were retrieved from the searches of the electronic databases (Figure 1). After deduplication, a total of 6051 unique citations remained. After the screening review of titles and abstract, three additional articles were added from the manual review of references and one article published outside of our search range through contact with an author of a trial report. In total, we included 95 full text articles and abstracts for selection phase. Sixty screened-in articles were excluded for the following reasons: not randomized control(14, 27–42), protocol only(43–48), inappropriate study population(49–52), inappropriate control(53–62), inappropriate intervention(63–76), duplicate article(14, 57, 70, 72, 77–79), unable to attain article(80) and recruitment data only(81) (Table E2 in Online Repository). Thirty-five publications from twenty studies met all inclusion criteria and underwent data extraction and synthesis (Figure 1; Table 1).(77–79, 82–113)
Figure 1.
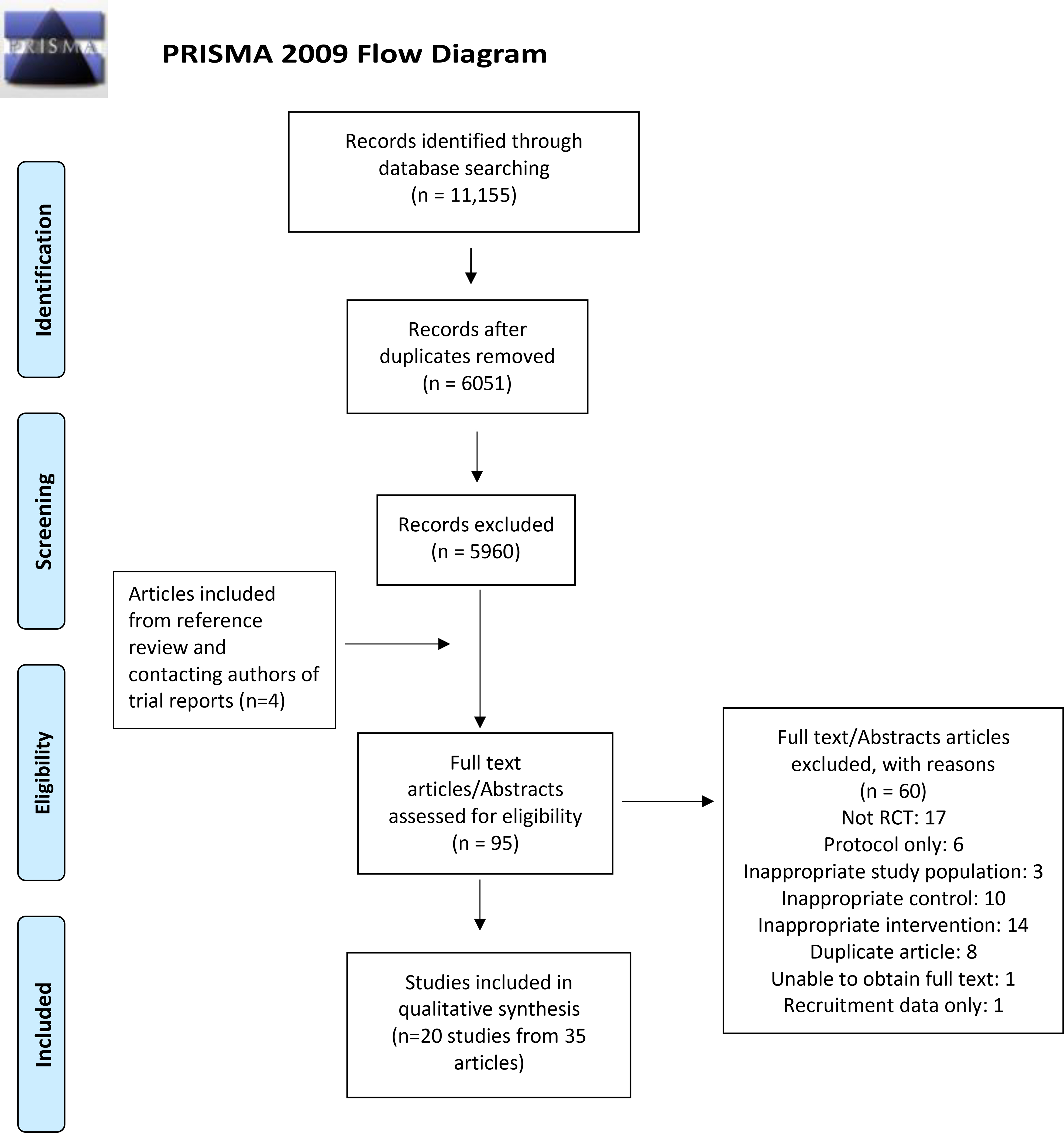
PRISMA Flow Diagram
Table 1.
Characteristics of included studies
| Study | Clinical Setting | Participants | Intervention | Comparison Group | Main Outcomes | Time Points Measured |
|---|---|---|---|---|---|---|
| Abd El-Kader et al. (2016)83 | University hospital in Saudi Arabia | 80 obese (BMI 31–37), asthmatic patients aged 41–53 years old whom had been using ICS at least 6 months prior to the start of the study | Treadmill exercise of progressive intensity and frequency 3 times per week for six months | Maintain ordinary lifestyle and medication management for six months | Bone mineral density and serologic inflammatory markers (HDL-c, LDL-c, TNF-alpha, IL-2, IL-4, IL-6, leptin) | All outcomes assessed prior to the intervention and at six months |
| Arandelovic et al. (2007)82 | University of Nis, Departments of the Health Center | 65 adults with mild, persistent asthma (per GINA guidelines) with documented treatment with low dose ICS and short-acting beta-2 agonists | Swimming twice weekly for six months at a local indoor pool, as well as asthma education | Continued treatment with low-dose ICS and short-acting beta-2 agonists | Lung function (spirometry), Lung inflammation (bronchoprovocation test) | All outcomes measured prior to the intervention and after six months |
| Bacon et al. (2015)85* | Not described 2 Hospitals in Montreal, Canada and the Montreal Chest Institute, Montreal, Canada | 66 adults with objectively confirmed asthma and poor asthma control | Cycle, treadmill, or elliptical exercise, three sessions per week for 12 weeks | Usual care | Asthma control (ACQ, and short-acting bronchodilator usage), waist circumference, BMI, depressive symptoms, and FEV1 | All outcomes assessed prior to the intervention and after 12 weeks |
| Boyd et al. (2012)100*, 101 | UAB Lung Health Center in Birmingham, AL | 19 adults ages 19–70 years old with mild-moderate persistent asthma and evidence of reversibility on spirometry | Walking program for 30 minutes, three times weekly, as well as a 30 min coordinator-led educational intervention | 30 min coordinator-led educational intervention | Asthma control (ACQ), lung function (spirometry), serologic and nasal-lavage inflammatory markers (ECP, IL-1beta, IL-4, IL-5, IL-6, IL-13, TNF-alpha and total IgE) | All outcomes assessed prior to intervention and after 12 weeks |
| Evaristo et al (2020)106*,107*, 112*, 113 | University setting in Brazil, not further described | 54 adults with moderate/severe asthma | Intervention consists of 40 minute twice weekly session of treadmill exercises beginning at 60% of the maximum predicted heart rate for 3 months and asthma education (two 2-hour classes/week for 2 weeks) | Breathing exercises (Pranayama Yoga breathing technique) twice a week for three months occurring in 40-minute intervals and asthma education (two 2-hour classes/week for 2 weeks) | Asthma control (ACQ-6), daily asthma symptoms, asthma exacerbations, psychosocial (HAD), health related quality of life (HRQL, AQLQ) exercise capacity (ISWT), airway inflammation (sputum), spirometr and daily physical activity levels (accelerometry) | Outcomes measured at baseline and 3 months (post-intervention) |
| Franca-Pinto et al. (2015)94, 95*, 96*, 97* | Outpatients at a University Hospital in Brazil | 58 adults with severe persistent asthma (GINA guidelines), under the stable care of a pulmonologist, between 20–59 years old | Aerobic training program consisting of 12 weeks of twice weekly indoor treadmill exercise sessions | Yoga breathing group consisting of 12 weeks of twice weekly supervised breathing instruction | Asthma control (ACQ; diary of daily asthma symptoms and exacerbations), health related quality of life (AQLQ), lung function (pulmonary function testing), serologic inflammatory mediators (IL-4, IL-5, IL-6, IL-10, tumor necrosis factor (TNF)-alpha, IL-12p70, IL-8/CXCL-8, MCP-1/CCL2, TANTES/CCL5 and serum IgE) | All outcomes measured over four weeks before and after the 12 weeks of intervention. |
| Freitas et al. (2017)77, 99*, 104*, 110*, 111 | Outpatients at university setting in Brazil, not further described | 55 adults ages 30–60 years old with moderate/severe asthma and a BMI between 35–40 | Aerobic and resistance exercise program twice weekly for three months, as well as a weight-loss program with 12 individual hypocaloric diet counseling sessions | Sham exercises, described as stretching and breathing, two times weekly for three months, as well as a weight-loss program with 12 individual hypocaloric diet counseling sessions. | Asthma control (ACQ), health related quality of life (AQLQ), lung function (spirometry; lung volumes), exercise capacity (CPET), depression/anxiety (HAD), steps/day (accelerometer), body weight/fat (bioelectrical impedance), lung inflammation (FeNO), and serologic inflammatory markers (IL-1, IL-2, IL-4, IL-5, IL-6, IL-10, IL-12, IL-13, TNF-alpha, VEGF, and chemokines) | All outcomes were measured prior to intervention, and after completion of intervention at 3 months |
| Haas et al. (1987)105 | New York University laboratory setting in New York, New York | 22 adults with a diagnosis of asthma and demonstratable EIB (>15% reduction in FEV1 and reversed with bronchodilator). | Aerobic exercise training with early training sessions designed to provide a minimum of 20 minutes of aerobic exercise, and both session length and training heart rate were systematically increased up to 40 minutes and 80% or maximal predicted heart rate. | Not described | Lung function (maximal voluntary ventilation12) and exercise capacity (minute ventilation, oxygen consumption, heart rate) | All outcomes measured before intervention and at 12 weeks. |
| Ma et al. (2015)91 | Kaiser Permanente Medical Centers in Northern California | 330 adults aged 18–70 years old with uncontrolled persistent asthma (confirmed through a multistage screening process), and a BMI greater than or equal to 30 | A lifestyle intervention (targeting modest weight loss and increased physical activity) curriculum spanning 12-months, consisting of 13 in-person weekly meetings, then monthly, then bi-monthly meetings, encouraged throughout for at least 150 minutes per week of moderate-intensity physical activity | Usual care from their physician, as well as receiving a pedometer, a body weight scale, a list of routinely offered weight management services, and an asthma education DVD | Asthma control (ACQ), health related quality of life (mini AQLQ), lung function (spirometry), health care utilization (medical record abstraction of encounters, diagnoses, and pharmacy dispensing), BMI. | All outcomes were measured at baseline, and at 6- and 12-months post-randomization |
| Mendes et al. (2010)98, 78, 93 | University Hospital in Brazil, not further described | 101 adults between ages 20–50 years with asthma diagnosis (based on GINA guidelines), and under medical treatment for greater than or equal to six months | Aerobic training program for 30 minutes per session twice a week, as well as an educational program consisting of two classes once weekly for 2 hours and a breathing exercise program involving 30 min session twice weekly for 3 months | Educational program consisting of two classes once weekly for 2 hours and a breathing exercise program involving 30 min session twice weekly for 3 months | Asthma control (daily diary of symptoms), lung function (spirometry), health related quality of life (HRQoL), depression (Beck Depression Inventory), anxiety (State-Trait Anxiety Inventory), exercise capacity (CPET) | Not specifically defined, but assesses all outcomes prior to and after the intervention |
| Meyer et al. (2015)92 | Hamberg metropolitan area, not further described | 21 adults with asthma diagnosis according to “standard criteria” | Group training session weekly for 12 months | Usual care | Exercise capacity (CPET), lung function (pulmonary function testing), health related quality of life (SF-36 and AQLQ), bronchodilator use | All outcomes were measured at baseline and after 12 months |
| Paul et al. (2013) 87* | University Setting, Kerala, India | 80 adults aged 18–40 years old with “partially controlled” asthma | Brisk walking 30 minutes per day for six months | Usual care | Lung function (spirometry), health related quality of life (AQLQ) | At baseline, one month after the onset of the study, and after 6 months |
| Razavi et al. (2011)84 | Allergy clinic in Ilam, Iran | 32 women aged 20–30 years old with asthma confirmed by clinical evaluation, pulmonary function test, skin testing for aeroallergens, and a six-minute walk test | 30 minutes weekly of aerobic exercise for 8 weeks, sessions included stretching, walking, and running. | Either vitamin D supplementation or usual care | Lung function (spirometry), exercise capacity via 6MWT | All outcomes were measured prior to the intervention and at 8 weeks |
| Refaat et al. (2015)86 | Respirology Department at the Farwanyia Hospital and Kuwait Physiotherapy center in the State of Kuwait | 68 adults aged 25–65 years old with moderate to severe asthma (based on GINA guidelines) | Supervised physical training three times weekly for six weeks, training involved a 10-minute warm up, 20–30 minutes of an exercise circuit (cycling, step ups, wall squats etc), and a 5 minute cool down | Usual care | Health related quality of life (AQLQ), lung function (pulmonary function testing) | AQLQ was completed prior to study, at the sixth week of the study, and after 3 months, PFTs were completed at initiation of study and after 3 months |
| Scichilone et al. (2012)88 | Pulmonary and Allergy outpatient clinics at the Institute of Respiratory Diseases at the University of Palermo in Palermo, Italy | Nine adults with mild asthma diagnosed by a pulmonologist (based on GINA guidelines) | Two to three weekly sessions of indoor rowing | Usual care | Airway responsiveness (single dose methacholine bronchoprovocation) | For the training group, evaluation was conducted at week 0, week 5 (mid-training), week 10 (post-training), and 4–6 week safter completion, controls underwent testing at week 0 and week 10 |
| Scott et al. (2013)89 | John Hunter Hospital in Australia | 46 overweight and obese (BMI 28–40) adults with asthma, diagnosed by a doctor and documented history of airway hyperresponsiveness | 12-week membership to a gymnasium and a one-hour personal training session once weekly, additionally encouraged to independently attend the gym three times or more weekly | A dietary intervention involved a calorie-restricted diet with two meal replacements daily, as well as weekly counselling with a dietician | Asthma control (ACQ), health related quality of life (AQLQ), lung function (pulmonary function testing), airway inflammation (induced sputum cytology/cell differential) and serologic inflammatory markers (CRP, IL-6, leptin, and adiponectin) | All outcomes measured prior to the intervention and post-intervention (specific timeline not provided) |
| Shaw et al. (2010)102, 103, 79 | South Africa not further described. | 88 adults aged 18–34 years old with moderate-persistent asthma based on NIH guidelines, with daily asthmatic symptoms | Aerobic Exercise Group: Three times weekly exercise program involving 5 minutes warm up, walking or jogging for 30 minutes, and a 5-minute cool down Aerobic Exercise AND Diaphragmatic breathing group: 15 minutes of walking or jogging and a reduced number of breaths during diaphragmatic breathing training | Diaphragmatic breathing group: Three times weekly instructed on breathing technique with practice breathing. Non-exercise control group: Usual care, phoned three times weekly to ensure compliance | Lung function (spirometry), BMI, exercise capacity (VO2 max) | All outcomes measured at baseline and after 8 weeks |
| Toennesen et al. (2018)109 | Copenhagen, Denmark. Academic medical center | 149 non-obese adult asthma patients with at least 1 positive diagnostic test demonstrating variable airflow obstruction (mannitol, methacholine, or reversability test). | Exercise only: High intensity interval training using the “10–20–30” concept on indoor spinning bikes. Diet only: 8-week of 5 group counseling sessions (2–6 patients/group) and 1 individual counseling session with a trained study dietician Exercise + Diet: Received both the exercise and diet interventions |
Usual Care | Asthma control (ACQ), health related quality of life (AQLQ), airway responsiveness (mannitol), serologic inflammatory markers (blood eosinophils, IL-6, hs-CRP), airway inflammatory markers (sputum eosinophils, FeNO), body composition, exercise capacity (CPET), urine urea excretion | Outcomes assessed at baseline and 8 weeks. |
| Turk et al. (2017)108* | The Netherlands, not further described | 31 adults with suboptimal controlled asthma (ACQ>0.75). | Lifestyle intervention program including high intensity interval training occurring three times a week for 3 months. | Control group participants were advised to lose weight and to exercise. | Asthma control (ACQ), asthma exacerbations, weight loss, waist circumference, exercise capacity (6MWT) | Outcomes assessed at baseline and 3 months post intervention. |
| Turner et al. (2011)90 | Australia, not further described | 35 adults older than age 40 with diagnosis of moderate or severe persistent asthma, under the care of a respiratory physician | Three exercise classes weekly for six weeks, that involved walking at different speeds | Usual care | Asthma control (ACQ), health related quality of life (SF-36), exercise capacity (6MWT), anxiety and depression (HADS). | All outcomes measured at baseline, immediately after intervention (6 weeks) and at 3 months following completion of the intervention |
Asthma Control Questionnaire (ACQ), Asthma Quality of Life Questionnaire (AQLQ), chemokine ligand (CCL), C-related protein (CRP), chemokine ligand (CXCL), eosinophil cationic protein (ECP), Forced expiratory volume in one second (FEV1), Forced vital capacity (FVC), high density lipoprotein-c (HDL-c), incremental shuttle walk test (ISWT), interleukin (IL), low density lipoprotein-c (LDL-c), monocyte chemoattractant protein (MCP-1), 36-item short form survey (SF-36), tumor necrosis factor-alpha (TNF-alpha), Global Initiative for Asthma (GINA), Body Mass Index (BMI), Hospital Anxiety and Depression scale (HAD), Health related Quality of life (HRQoL), Six Minute Walk Test (6MWT), High Density Lipoproteins (HDL), Low Density Lipoproteins (LDL)
Indicates abstract
Risk of bias
Many studies did not adequately describe key features required to assess risk of bias. Randomization, allocation concealment, and blinding were difficult to assess in many studies (Figure 2). Most studies described missing data well, and were found to have low risk of selective outcome reporting (Figure 3). Further information regarding bias in this literature is available in the online repository.
Figure 2:
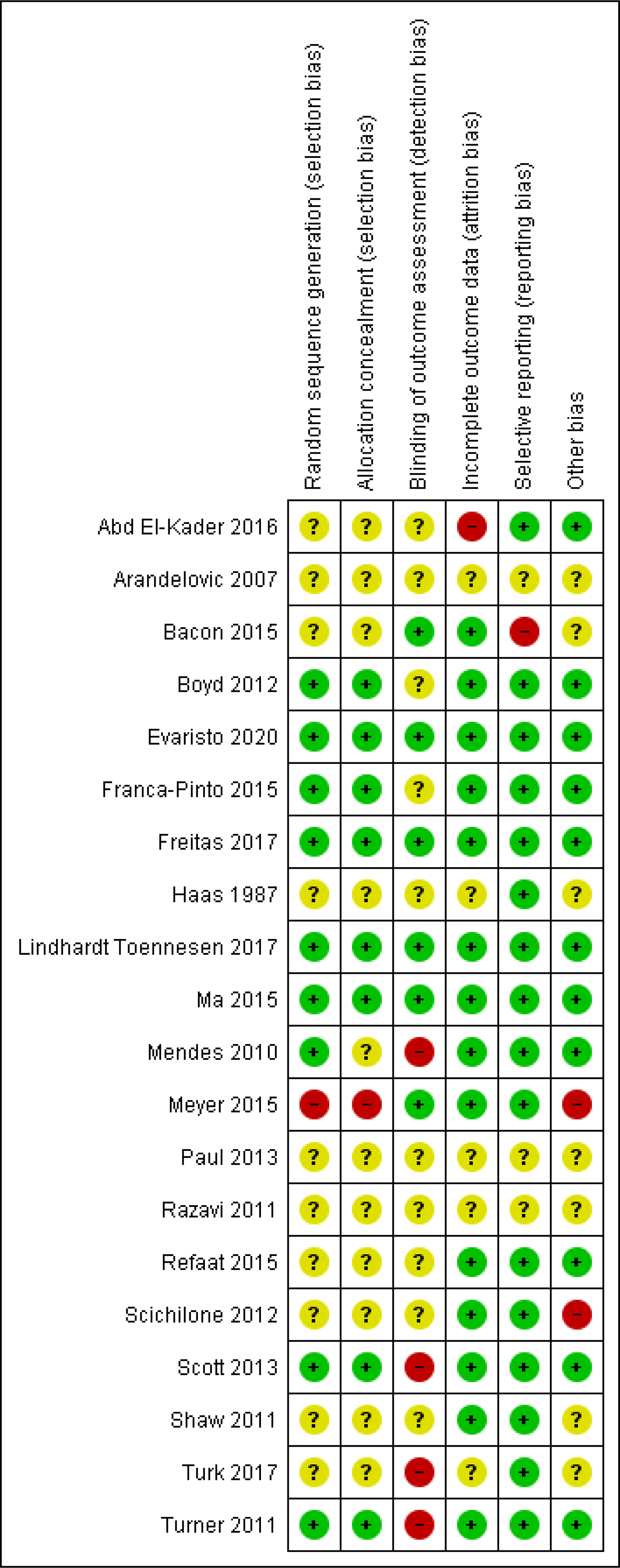
Risk of bias summary- review author’s judgements about each methodological domain for each included study
Figure 3:
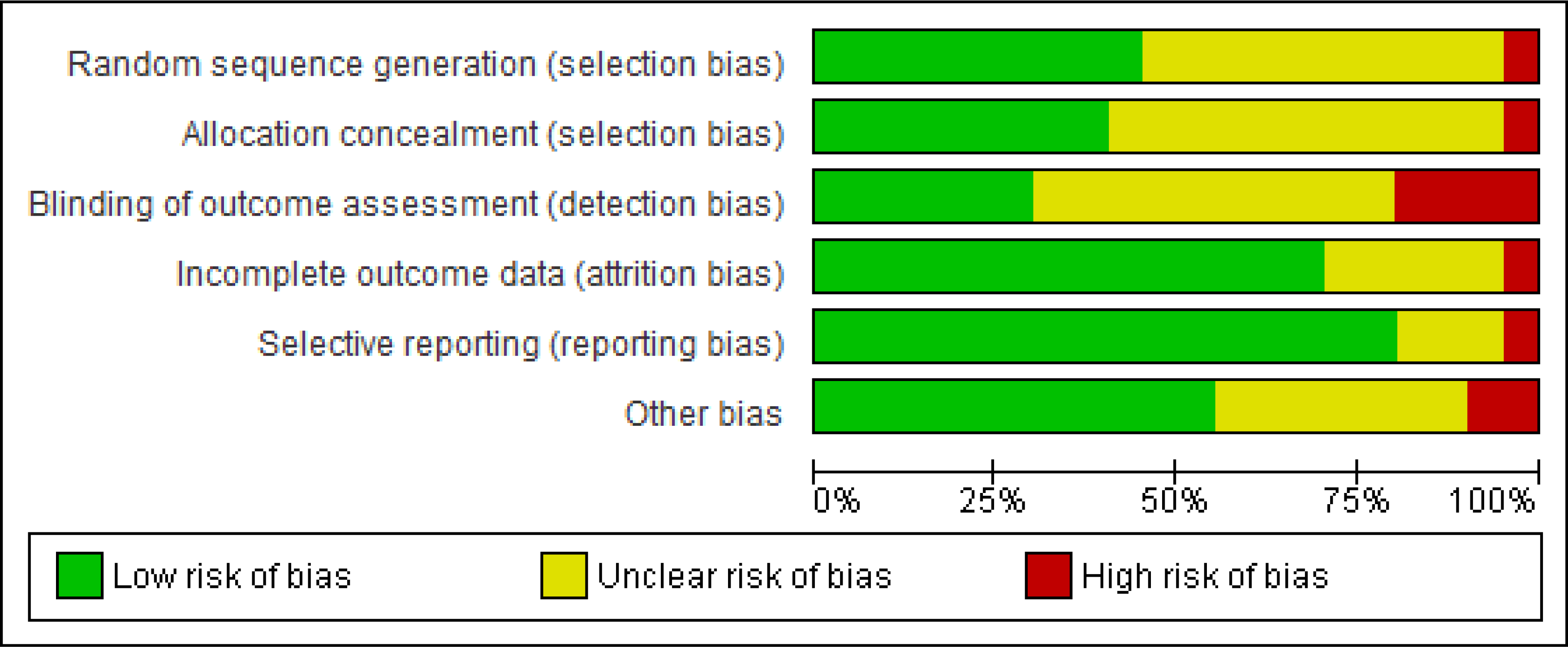
Risk of bias summary graph- review author’s judgments about each methodological domain presented as percentages across all included studies
Population
Table 1 shows the main characteristics of the included studies. The criteria for asthma diagnosis varied considerably, including the regular use of an inhaled corticosteroid or other asthma medication, physician diagnosis, lung function parameters, or meeting the Global Initiative for Asthma (GINA) guidelines.(82, 86, 94, 98) Study size ranged from 19 participants to 330 participants and took place in fourteen different countries. Asthma outcomes varied widely, including lung function parameters, serologic inflammatory markers, health-related quality of life and asthma control measures. Other outcomes assessed included exercise capacity (such as six minute walking distance or incremental shuttle walk test)(84, 90, 108, 113), cardiopulmonary exercise testing including maximum work rates and maximum oxygen uptake(77, 92, 98, 103, 105, 109), weight loss parameters (such as body mass index)(77, 85, 91, 102, 108, 109) and depression/anxiety levels.(77, 85, 90, 98, 113)
Study Interventions
Physical activity interventions varied considerably across studies (Table 1 and Table E3 in the Online Repository). The interventions ranged from walking/running to circuit training or other aerobic and resistance exercises. Nine studies specified that the exercise intervention was supervised.(85, 86, 88, 90, 92, 102, 105, 109, 113) Frequency of physical activity varied from daily to once weekly, and duration varied from six weeks to one year.
Nine studies included other interventions apart from physical activity, either in the control group, intervention group, or both.(77, 84, 89, 91, 94, 98, 103, 109, 113) This ranged from breathing exercises/training (77, 94, 98, 102, 113), a weight loss or dietary component (77, 89, 91, 109) or vitamin supplementation.(84)
One study reported a negative outcome associated with exercise. A participant fell while walking and suffered a fractured wrist.(91) No study attributed any worsening asthma symptoms or exacerbations to the physical activity intervention.
Outcomes
Results of included studies are summarized in Table 2. We recorded all outcomes of included studies for the fullness of the review record, but synthesized results of asthma outcomes. Other outcomes not included in our analysis were weight change, mental health, bone mineral density, aerobic capacity and physical activity levels. Comprehensive study outcomes are described in Table 1. All studies included at least one of the asthma outcomes we evaluated.
Table 2:
Results of Included Studies
| STUDIES |
|||
|---|---|---|---|
| LUNG FUNCTION | ASTHMA CONTROL | HEALTH-RELATED QUALITY OF LIFE | |
| Abd El-Kader et al. (2016) | |||
| Arandelovic et al. (2007) | +* | ||
| Bacon et al. (2015) | N | +* | |
| Boyd et al. (2012) | N | N | |
| Evaristo et al (2020) | N | +* | +* |
| Franca-Pinto et al. (2015) | N | +* | +* |
| Freitas et al. (2017) | N | +* | + |
| Hass et al. (1987) | N | ||
| Ma et al. (2015) | N | N | + |
| Mendes et al. (2010) | N | +* | +* |
| Meyer et al. (2015) | N | N | N |
| Paul et al. (2013) | + | ||
| Razavi et al. (2011) | +* | ||
| Refaat et al. (2015) | +* | +* | |
| Schichilone et al. (2012) | N | ||
| Scott et al. (2013) | +* | N | N |
| Shaw et al. (2010) | +* | ||
| Toennesen et al. (2018) | N | +* | +* |
| Turk et al. (2017) | +* | ||
| Turner et al. (2011) | N | N | +* |
+*: Statistically significant positive effect in variable between intervention and control group
+: Positive effect in variable between intervention and control group
N: No difference between intervention and control groups reported
−: Negative effect in variable between intervention and control group
−*: Statistically significant negative effect in variable between intervention and control group
Blank cell indicates the outcome was not measured
Lung function
All but two studies reported lung function information, primarily with spirometry measurements.(83, 108) Physical activity effects on lung function values varied across studies. Six of twenty-two studies reported improvement in at least one spirometry measurement (forced vital capacity-FVC, forced expiratory volume in 1 second-FEV1, FEV1/FVC or total lung capacity) between the intervention and control groups.(82, 84, 86, 87, 89, 102) Twelve studies showed no between-group differences in any lung function parameter with physical activity. (77, 85, 88, 90–92, 94, 98, 101, 105, 109, 113)
Asthma Control
Twelve studies reported data on asthma control. (77, 85, 89–92, 94, 98, 101, 108, 109, 113) Outcome measures ranged from the Asthma Control Questionnaire (ACQ) scores, to rescue inhaler use, to emergency room visits, to daily diary symptom reports, to number of reported asthma exacerbations. The results of effect of physical activity on asthma control varied across studies. Ten studies assessed participants with the ACQ (77, 85, 89–91, 94, 101, 108, 109, 113) with five studies showed a significant improvement in the ACQ score between groups.(77, 85, 108, 109) One study showed no difference in bronchodilator inhaler use between groups post-intervention,(92) while two showed a significant improvement.(85, 113) Another study showed a significant increase in asthma symptom-free days at 30, 60, and 90 days post-intervention between intervention and control groups.(98) Overall, seven studies showed a statistically significant improvement in at least one outcome measure of asthma control (Table 2).
Health Care Related Quality of Life
Eleven studies reported data regarding asthma-related quality of life. Nine out of eleven studies reported data using the asthma quality of life questionnaire (AQLQ or mini- AQLQ). (77, 86, 87, 89, 91, 92, 94, 109, 113) This is a four-domain questionnaire to evaluate the physical and emotional impact of asthma. The four domains include symptoms, activity limitation, emotional function, and environmental exposure.(114)
Two studies used the asthma-related health care quality of life questionnaire (ARHQoL).(98, 106) This tool assesses four domains of asthma-related quality of life, but rather than the emotional functions and environmental exposure domains, it assesses socioeconomic and psychosocial domains.(115) Two studies additionally reported the 36-item Short Form Survey (SF-36) data.(90, 92)
Of the nine studies that used the AQLQ to assess asthma-related quality of life, five showed a statistically significant improvement with the intervention in the mean AQLQ or at least one domain.(86, 87, 94, 109, 113) Improvement in the activity limitation (77, 86, 91, 94, 113), symptoms (86, 91, 94), and emotional function domains were found.(86)
One study employed the ARHQoL questionnaire and found a statistically significant improvement in the physical limitation and symptom frequency domains.(98) Another study found improvement in the physical component of the SF-36.(90) This between group difference was no longer significant at 3-month follow up. The other study evaluating SF-36 did not publish between group analyses.(92) Nearly half of the studies found some improvement in quality of life, while the remainder showed no statistically significant difference (Table 2).
Serologic Inflammatory Markers (Table 3)
Table 3:
Serologic Inflammatory Markers Results
| STUDIES | Serologic Inflammatory Markers | ||||
|---|---|---|---|---|---|
|
| |||||
| Th2 Inflammation | Th1 Inflammation | TH17 Inflammation | Pro Inflammatory Markers (hormones and IL8) | Other | |
| Abd El-Kader et al. (2016) | ↓IL-4* | ↓IL-2* | ↓Leptin* | ↓LDL-c* | |
| ↓IL-6* | ↓TNF-alpha* | ↓Calcium* | |||
| Boyd et al. (2012) | ↔ECP | ↓IL-1beta | |||
| ↓Eosinophils | |||||
| Franca-Pinto et al. (2015) | ↓FeNO | ↓IL-8 | |||
| ↓MCP-1* | |||||
| ↓IL-6* | |||||
| Freitas et al. (2017) | ↓IL-4* | ↓TNF-alpha* | ↓Leptin* | ↓CCL* | |
| ↓IL-6* | |||||
| Scott et al. (2013) | ↓Leptin* | ||||
| Toennesen et al. (2018) | ↔Eosinophils | ||||
Significant
↓reduction
↔ no change
Six studies examined the effect of physical activity on serologic inflammatory markers.(77, 83, 89, 94, 101, 109) The specific serologic markers varied across studies. Three studies showed a significant reduction in at least one inflammatory marker between the intervention and control group.(77, 83, 94) IL-6 was the only inflammatory marker that was consistently reduced in the intervention groups (reported as statistically significantly reduced between groups in three studies).(77, 83, 94) Three studies found no significant between-group differences in any inflammatory marker.(89, 101, 109)
Discussion
This systematic review aimed to discover and evaluate the available evidence to better understand the effects of physical activity in adults with asthma. Twenty-three randomized controlled trials of varying sizes were included in our analysis. Of our included studies, thirteen articles from seven studies were published abstracts. These were included for the fullness of the record as there is limited research in this area. Similar to other systematic reviews, our findings are limited by the presence and quality of data provided in the included studies. We found heterogeneity in the type, frequency and duration of physical activity interventions as well as the outcomes measures which precluded a meta-analysis. Nonetheless, our qualitative findings suggest that physical activity can improve asthma control, lung function and health care-related quality of life. None of the studies found worsening of asthma control during the physical activity interventions.
Asthma symptom control is an important patient-reported outcome and a key component of assessing asthma control.(116, 117) Of the thirteen studies that reported changes in asthma symptom control, over half found improvements in self-reported outcomes. Asthma control was assessed using different self-reported measures of asthma control with the most commonly used measure being Asthma Control Questionnaire (ACQ). In over half of the included studies, blinding of the outcome assessors was unclear, resulting in a potential threat to the validity of the assessments. Future physical activity interventions in asthma should include asthma control as a core outcome measure, utilize validated instruments and improve reporting of their trial methods, especially blinding of assessors and allocation concealment.(118) This would allow not only for more reliable results, but also ease in future collation of data for meta-analysis.
Our study suggests that physical activity can improve patients’ quality of life. Most of the studies included used the same standardized quality of life measure, the Asthma Quality of Life Questionnaire. Quality of life is a key factor when considering treatment interventions, as it is meant to provide an assessment of the patient’s perceived wellbeing.(119) It is generally viewed as a more holistic approach for patient assessment.(119) In asthma, the improvement in quality of life is important to note, as prior studies have demonstrated a lack of direct correlation between clinical measures and patients’ measured QoL. (120–122) Our study suggests that physical activity provides an improvement in patients’ perceived wellbeing, as most studies showed an improvement in overall quality of life. This aligns with the findings of a previous systematic review in physical activity training in asthma which found positive effects on the quality of life of asthma patients.(109) Our findings on improvement in quality of life also add to the literature in adults with asthma as the recently published systematic review on PA and asthma in adults did not assess quality of life outcomes.(21)
In our analysis, almost half of the studies showed evidence of improved resting lung function post-intervention. This is consistent with the findings from a review by Avallone and colleagues in 2012 who reported improvements in lung function (e.g., PEF, FEV1, FEF25.(21) Additionally, in the meta-analysis conducted by Hansen et al, lung function slightly increased, in favor of exercise training (Standard Mean Difference: −0.36, −0.72 to 0.00).(21) This suggests physical activity improves lung function parameters, but further research is needed to better define this change/effect.
Our systematic review was unique from prior studies in that it also evaluated systemic markers of inflammation as an outcome of interest. Physical activity’s effect on inflammatory markers could serve as a pathway to better understand the physiological benefit of exercise. Six of the studies included in our analysis assessed for changes in serum inflammatory markers with physical activity. Interleukin-6 (IL-6) was the most frequently measured biomarker and was found to decrease with the physical activity intervention in three studies. IL-6 has been shown to be elevated in obese patients with asthma.(123) Recent studies have also shown that IL-6 levels are associated with severe asthma, and together with the results reviewed here (77, 83, 94), suggest that this marker should be further considered as a target for intervention studies.(124)
This adds to prior data evaluating changes in systemic inflammatory markers with physical activity in asthmatic individuals. When comparing physical activity versus sedentary behavior in asthmatic individuals, one study found no difference in airway inflammation, but found a significant decrease in serologic C-reactive protein levels with increased physical activity.(125) This reinforces the importance of evaluating not only direct lung parameters, but also systemic markers of inflammation. Further studies evaluating changes in IL-6 and other systemic inflammatory markers is needed to better understand this relationship.
Limitations of the studies found in our review include short follow-up intervals, lack of assessment of general physical activity levels and generalizability of results. None of the studies included in our analysis assessed for maintenance of physical activity or outcomes longer than one year. Our study and others suggest these short-term interventions have positive effects on multiple asthma outcomes, but the potential for increased long-term benefits has not been evaluated. Studies in the future should assess the long-term benefits of these physical activity interventions on asthma outcomes.
Only three studies reported physical activity outcomes such as change in steps/day, leisure-time physical activity or total physical activity levels.(77, 89, 91) In order better understand the mechanisms of physical activity on asthma outcomes, overall physical activity measures need to be assessed and reported in studies. Additionally, many studies employed a supervised, gym-based physical activity intervention that may not be feasible or accessible for most asthma patients. These clearly defined interventions suggest physical activity improves asthma outcomes, and future research will need to investigate if this extends to more accessible modes of physical activity, such as lifestyle physical activity.(126)
A limitation related to our review was the inability to conduct a meta-analysis due to the heterogeneity of results. Hansen et al. reported a meta-analysis assessing lung function, asthma control, and airway inflammation.(21) However, deriving a summary effect size for this highly heterogeneous body of literature could be misleading because of the different nature and intensity of the interventions. Instead, we used vote counting synthesis to analyze our findings as we were able to summarize the diverse results across the studies. This method has its known limitations including not being able to determine a small or large effect.(127) Using a vote counting method also allowed us to comprehensively evaluate the role of physical activity in asthma outcomes, so we did not need to limit our outcome measures.
Despite the heterogeneity in design and outcomes, our summative report of literature in physical activity’s effect on asthma found improvements in asthma control, quality of life, lung function and serum inflammatory markers. This aligns with recent observations, which note the growing body of evidence supporting aerobic exercise as a treatment for asthma.(15) Currently, the Global Initiative in Asthma nor the National Heart, Lung, Blood Institute (NHLBI) Asthma Guidelines do not provide specific recommendations for physical training or exercise as a means of asthma control.(2, 128) Even the December 2020 NHLBI update to the asthma management guidelines does not mention the potential benefit of physical activity.(129) Physical training was well tolerated among people with asthma in the included studies. Based on this data, individuals with asthma should be encouraged to participate in regular exercise training to improve asthma outcomes, without fear of symptom exacerbation. More research is needed to optimize these exercise interventions and determine the best methods to incite behavior change.
Supplementary Material
Highlights Box:
What is already known about this topic? Low levels of physical activity are associated with poorer asthma outcomes. Engaging in regular physical activity might have a beneficial impact in adults with asthma.
What does this article add to our knowledge? Physical activity is safe among adults with asthma with varying severity levels. Physical activity favors improvements in lung function, asthma control, quality of life and serologic inflammatory markers.
How does this study impact current management guidelines? Our findings suggest, in addition to the general health benefits of physical activity, regular physical activity may be a potential non-pharmacologic treatment in adults with asthma.
Acknowledgments
Conflict of interest disclosures: MK-No conflicts to disclose, MC- No conflicts to disclose, CC- No conflicts to disclose, VPC- No conflicts to disclose, IR- No conflicts to disclose, AS- No conflicts to disclose, KW- No conflicts to disclose, SK- No conflicts to disclose, SN-Receives funding from NIH (K01HL133370).
Abbreviations
- ACQ
Asthma Control Questionnaire
- AQLQ
Asthma Quality of Life Questionnaire
- CCL
chemokine ligand
- CINAHL
Cumulative Index to Nursing and Allied Health Literature
- CRP
C-related protein
- CXCL
chemokine ligand
- ECP
eosinophil cationic protein
- EMBASE
Excerpta Medica database
- FEV1
Forced expiratory volume in one second
- FVC
Forced vital capacity
- GINA
Global Initiative for Asthma
- HDL-c
high density lipoprotein-c
- IL
interleukin
- LDL-c
low density lipoprotein-c
- MCP-1
monocyte chemoattractant protein
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-analysis
- PTH
parathyroid hormone
- SF-36
36-item short form survey
- TNF-alpha
tumor necrosis factor-alpha
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Masoli M, Fabian D, Holt S, Beasley R. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy. 2004;59(5):469–78. [DOI] [PubMed] [Google Scholar]
- 2.Expert Panel Report 3: Guidelines for the Diganosis and Management of Asthma. Bethesda, MD: National Heart, Lung, and Blood Institute (US); 20072007August. [Google Scholar]
- 3.Pakhale S, Luks V, Burkett A, Turner L. Effect of physical training on airway inflammation in bronchial asthma: a systematic review. BMC pulmonary medicine. 2013;13:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lipworth BJ. Systemic adverse effects of inhaled corticosteroid therapy: A systematic review and meta-analysis. Arch Intern Med. 1999;159(9):941–55. [DOI] [PubMed] [Google Scholar]
- 5.Gamble J, Stevenson M, McClean E, Heaney LG. The prevalence of nonadherence in difficult asthma. Am J Respir Crit Care Med. 2009;180(9):817–22. [DOI] [PubMed] [Google Scholar]
- 6.Holgate ST, Price D, Valovirta E. Asthma out of control? A structured review of recent patient surveys. BMC Pulm Med. 2006;6Suppl 1(Suppl 1):S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nunan D, Mahtani KR, Roberts N, Heneghan C. Physical activity for the prevention and treatment of major chronic disease: an overview of systematic reviews. Syst Rev. 2013;2:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crimi E, Balbo A, Milanese M, Miadonna A, Rossi GA, Brusasco V. Airway inflammation and occurrence of delayed bronchoconstriction in exercise-induced asthma. AM REV RESPIR DIS. 1992;146(2):507–12. [DOI] [PubMed] [Google Scholar]
- 9.Mancuso CA, Sayles W, Robbins L, Phillips EG, Ravenell K, Duffy C, et al. Barriers and facilitators to healthy physical activity in asthma patients. The Journal of asthma : official journal of the Association for the Care of Asthma. 2006;43(2):137–43. [DOI] [PubMed] [Google Scholar]
- 10.Yawn BPR, Matthew A.: Bertram Susan L.: Wollan Peter C. Obesity, low levels of physical activity and smoking present opportunities for primary care asthma interventions: an analysis of baseline data from The Asthma Tools Study. Npj Primary Care Respiratory Medicine. 2015;25:15058-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Strine TW, Mokdad AH, Dube SR, Balluz LS, Gonzalez O, Berry JT, et al. The association of depression and anxiety with obesity and unhealthy behaviors among community-dwelling US adults. Gen Hosp Psychiatry. 2008;30(2):127–37. [DOI] [PubMed] [Google Scholar]
- 12.Avallone KM, McLeish AC. Asthma and aerobic exercise: a review of the empirical literature. J Asthma. 2013;50(2):109–16. [DOI] [PubMed] [Google Scholar]
- 13.Ford ES, Mannino DM, Redd SC, Moriarty DG, Mokdad AH. Determinants of quality of life among people with asthma: Findings from the Behavioral Risk Factor Surveillance System. Journal of Asthma. 2004;41(3):327–36. [DOI] [PubMed] [Google Scholar]
- 14.Dogra S, Kuk JL, Baker J, Jamnik V. Exercise is associated with improved asthma control in adults. The European respiratory journal. 2011;37(2):318–23. [DOI] [PubMed] [Google Scholar]
- 15.Bacon SL, Platts-Mills TAE. Is It Time for Aerobic Exercise to be Included in Asthma Treatment Guidelines? The Journal of Allergy and Clinical Immunology: In Practice. 2020;8(9):2997–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The Physical Activity Guidelines for Americans. Jama. 2018;320(19):2020–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teramoto M, Moonie S. Physical Activity Participation among Adult Nevadans with Self-Reported Asthma. Journal of Asthma. 2011;48(5):517–22. [DOI] [PubMed] [Google Scholar]
- 18.Reznik M, Islamovic F, Choi J, Leu CS, Rowlands AV. Factors associated with in-school physical activity among urban children with asthma. J Asthma. 2018;55(5):492–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carson KVC MG: Picot J: Brinn MP: Esterman AJ: Smith BJ Physical training for asthma. The Cochrane database of systematic reviews. 2013;(9):CD001116. doi(9):CD001116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ram FSF, Robinson SM, Black PN, Ram FS, Robinson SM, Black PN. Effects of physical training in asthma: a systematic review...The Cochrane Collaboration and the Cochrane Airways Group. British Journal of Sports Medicine. 2000;34(3):162–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hansen ESH, Pitzner-Fabricius A, Toennesen LL, Rasmusen HK, Hostrup M, Hellsten Y, et al. Effect of aerobic exercise training on asthma in adults: a systematic review and meta-analysis. Eur Resp J. 2020;56(1):2000146. [DOI] [PubMed] [Google Scholar]
- 22.Eichenberger PD, Stephanie Kofmehl, Christina Reto: Spengler. Effects of Exercise Training on Airway Hyperreactivity in Asthma: A Systematic Review and Meta-Analysis. Sports Medicine. 2013;43(11):1157–70. [DOI] [PubMed] [Google Scholar]
- 23.Heikkinen SAM, Quansah R, Jaakkola JJK, Jaakkola MS. Effects of regular exercise on adult asthma. European Journal of Epidemiology. 2012;27(6):397–407. [DOI] [PubMed] [Google Scholar]
- 24.Carson KV, Chandratilleke MG, Picot J, Brinn MP, Esterman AJ, Smith BJ. Physical training for asthma. The Cochrane database of systematic reviews. 2013;9:Cd001116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gptzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Julian Higgins JT. Cochrane Handbook for Systematic Reviews fo Interventions In: Jacqueline Chandler MC, Li Tianjing, Page Matthew, Welch Vivian editor. 6.1 ed2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Del Giacco SRG-L V Aerobic exercise training reduces bronchial hyper-responsiveness and serum pro-inflammatory cytokines in patients with asthma. Evidence-Based Medicine. 2016;21(2):70. [DOI] [PubMed] [Google Scholar]
- 28.Lingner H, Ernst S, Grofehennig A, Djahangiri N, Scheub D, Wittmann M, et al. Asthma control and health-related quality of life one year after inpatient pulmonary rehabilitation: The ProKAR Study . J Asthma. 2015;52(6):614–21. [DOI] [PubMed] [Google Scholar]
- 29.Majewski MD G: Pawik M: Rozek K Evaluation of a Home-Based Pulmonary Rehabilitation Program for Older Females Suffering from Bronchial Asthma. Advances in clinical and experimental medicine : official organ Wroclaw Medical University. 2015;24(6):1079–83. [DOI] [PubMed] [Google Scholar]
- 30.Porsbjerg C, Lange P, Ulrik CS. Lung function impairment increases with age of diagnosis in adult onset asthma. Respiratory Medicine. 2015;109(7):821–7. [DOI] [PubMed] [Google Scholar]
- 31.Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scandinavian Journal of Medicine & Science in Sports. 2015;25:1–72. [DOI] [PubMed] [Google Scholar]
- 32.Onur STY, Didem Arzu. Immunomodulatory Effect of Exercise in Patients with Asthma. Eurasian Journal of Pulmonology. 2017;19(1):30–3. [Google Scholar]
- 33.Miyamoto NS H: Tanaka T: Asai M: Yanagita Y: Yano Y: Nishinakagawa T: Kotaki K: Kitagawa C: Rikitomi N: Kozu R: Honda S Pulmonary rehabilitation improves exercise capacity and dyspnea in air pollution-related respiratory disease. Tohoku Journal of Experimental Medicine. 2014;232(1). [DOI] [PubMed] [Google Scholar]
- 34.Renolleau-Courtois D, Lamouroux-Delay A, Delpierre S, Badier M, Lagier-Tessonnier F, Palot A, et al. Home-based respiratory rehabilitation in adult patients with moderate or severe persistent asthma. J Asthma. 2014;51(5):552–8. [DOI] [PubMed] [Google Scholar]
- 35.Saguil AO N Physical training for patients with asthma. American Family Physician. 2013;87(5):313–4. [PubMed] [Google Scholar]
- 36.Hildenbrand KN, Freson Sara, Timothy S: Becker Bruce E. Development of an Aquatic Exercise Training Protocol for the Asthmatic Population. International Journal of Aquatic Research & Education. 2010;4(3):278–99. [Google Scholar]
- 37.Dogra S, Jamnik V, Baker J. Control and adherence - Self-directed exercise improves perceived measures of health in adults with partly controlled asthma. J Asthma. 2010;47(9):972–7. [DOI] [PubMed] [Google Scholar]
- 38.Juvonen R, Bloigu A, Peitso A, Silvennoinen-Kassinen S, Saikku P, Leinonen M, et al. Training improves physical fitness and decreases CRP also in asthmatic conscripts. The Journal of asthma : official journal of the Association for the Care of Asthma. 2008;45(3):237–42. [DOI] [PubMed] [Google Scholar]
- 39.Klansky AI, Morrison-Taylor Charlie, Ahlstrand Adriane, Labrie Sarah, Haverkamp Danielle, Christian Hans. No effect of elevated operating lung volumes on airway function during variable workrate exercise in asthmatic humans. Journal of applied physiology. 2016;121(1):89–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Emtner M, Herala M, Stalenheim G. High-intensity physical training in adults with asthma. A 10-week rehabilitation program. Chest. 1996;109(2):323–30. [DOI] [PubMed] [Google Scholar]
- 41.Emtner M, Finne M, Stalenheim G. A 3-year follow-up of asthmatic patients participating in a 10-week rehabilitation program with emphasis on physical training. Archives of Physical Medicine and Rehabilitation. 1998;79(5):539–44. [DOI] [PubMed] [Google Scholar]
- 42.Freeman AT, Geale R, Bali S, Gove K, Cellura D, Burke H, et al. P105 High intensity intermittent exercise training in poorly controlled asthma: preliminary clinical trial results. Thorax. 2018;73(Suppl 4):A159. [Google Scholar]
- 43.Bacon SLL KL: Bourbeau J: Ernst P: Maghni K: Gautrin D: Labrecque M: Pepin V: Pedersen BK The effects of a multisite aerobic exercise intervention on asthma morbidity in sedentary adults with asthma: the Ex-asthma study randomised controlled trial protocol. BMJ open. 2013;3(6): 10.1136/bmjopen-2013-003177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bruton A, Kirby S, Arden-Close E, Taylor L, Webley F, George S, et al. The BREATHE study: Breathing REtraining for Asthma Trial of Home Exercises. A protocol summary of a randomised controlled trial. Prim Care Respir J. 2013;22(2):PS1–PS7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ma JS P: Camargo CA Jr: Xiao L: Ayala E: Gardner CD: Buist AS: Haskell WL: Lavori PW: Wilson SR The Breathe Easier through Weight Loss Lifestyle (BE WELL) Intervention: A randomized controlled trial. BMC Pulmonary Medicine. 2010;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schultz KS H: Jelusic D: Wagner R: Wittmann M: Faller H: Nowak D: Schuler M Effectiveness of pulmonary rehabilitation for patients with asthma: study protocol of a randomized controlled trial (EPRA). BMC pulmonary medicine. 2017;17(1):49–017-0389–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Evaristo KB, Saccomani MG, Martins MA, Cukier A, Stelmach R, Rodrigues MR, et al. Comparison between breathing and aerobic exercise on clinical control in patients with moderate-to-severe asthma: protocol of a randomized trial. BMC pulmonary medicine. 2014;14:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Freitas PD, Ferreira PG, da Silva A, Trecco S, Stelmach R, Cukier A, et al. The effects of exercise training in a weight loss lifestyle intervention on asthma control, quality of life and psychosocial symptoms in adult obese asthmatics: protocol of a randomized controlled trial. BMC pulmonary medicine. 2015;15:124-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Parsons JP, Baran CP, Phillips G, Jarjoura D, Kaeding C, Bringardner B, et al. Airway Inflammation in Exercise-Induced Bronchospasm Occurring in Athletes Without Asthma. J Asthma. 2008;45(5):363–7. [DOI] [PubMed] [Google Scholar]
- 50.Farid R, Azad FJ, Atri AE, Rahimi MB, Khaledan A, Talaei-Khoei M, et al. Effect of aerobic exercise training on pulmonary function and tolerance of activity in asthmatic patients. Iranian journal of allergy, asthma, and immunology. 2005;4(3):133–8. [PubMed] [Google Scholar]
- 51.Majd S, Singh S, Bradding P, Hewitt S, Apps L, Murphy A, et al. Exercise training and airway inflammation in severe-asthma: Results from a feasibility study. European Respiratory Journal. 2018;52. [Google Scholar]
- 52.Pollart SM, Elward KS, Platts-Mills TAE. Improvements in quality of life measures in a structured exercise program for persistent asthma. Journal of Allergy and Clinical Immunology. 2012;129(2):AB60. [Google Scholar]
- 53.Coelho CM, Reboredo MM, Carvalho EV, Gomes EP, Valle FM, Malaguti C, et al. Effects of an unsupervised pedometer-based physical activity program on adults with moderate to severe asthma. American Journal of Respiratory and Critical Care Medicine. 2015;191.25932660 [Google Scholar]
- 54.Da Silva RA, Rocco PGL, Mazzucatto F, Cukier A, Stelmach R, Martins MA, et al. High intensity interval training increases daily life physical activity and quality of life in patients with moderate and severe asthma. European Respiratory Journal. 2016;48. [Google Scholar]
- 55.Mancuso CAC TN: Westermann H: Wenderoth S: Wells MT: Charlson ME Improvement in asthma quality of life in patients enrolled in a prospective study to increase lifestyle physical activity. The Journal of asthma : official journal of the Association for the Care of Asthma. 2013;50(1):103–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mancuso CAW S: Wells MT: Charlson ME Increasing Lifestyle Physical Activity in Asthma Patients: A Randomized Trial. American Journal of Respiratory and Critical Care Medicine. 2009;179.19029000 [Google Scholar]
- 57.Bundgaard A, Bach-Mortensen N, Schmidt A. The effect of sodium cromoglycate delivered by Spinhaler and by pressurized aerosol on exercise- induced asthma in children. Clin Allergy. 1982;12(6):601–5. [DOI] [PubMed] [Google Scholar]
- 58.Da Silva RA, Rocco PGL, Mazzucato F, Fernandes T, Cukier A, Stelmach R, et al. High intensity interval training increases aerobic fitness, health related quality of life and clinical control in patients from moderate to severe asthma. European Respiratory Journal. 2017;50. [Google Scholar]
- 59.Mancuso CA, Choi TN, Westermann H, Wenderoth S, Wells MT, Charlson ME. Improvement in asthma quality of life in patients enrolled in a trial to increase lifestyle physical activity. European Respiratory Journal. 2012;40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Saxer S, Schneider S, Appenzeller P, Bader P, Lichtblau M, Furian M, et al. Asthma rehabilitation at high vs. low altitude: Randomized controlled parallel-group trial. European Respiratory Journal. 2017;50. [Google Scholar]
- 61.Saxer S, Schneider S, Lichtblau M, Bader P, Appenzeller P, Estebesova B, et al. Asthma rehabilitation at high vs. low altitude and its impact on exhaled nitric oxide and sensitization patterns: Randomized parallel-group trial. European Respiratory Journal. 2018;52. [DOI] [PubMed] [Google Scholar]
- 62.Aparecido da Silva R, Rocco PGL, Mazzucatto F, Cukier A, Stelmach R, Martins MA, et al. High intensity interval training increases the clinical control, aerobic fitness and decreases dyspnea in severe asthmatics. Eur Resp J. 2016;48(suppl 60):PA1560. [Google Scholar]
- 63.Astafieva NK D: Gamova I: Perfilova I: Udovichenko E Physical rehabilitation in asthma management. European Respiratory Journal. 2011;38. [Google Scholar]
- 64.Awopeju OFE GE: Adedoyin RA A comparison of myocardial oxygen consumption during three modes of sub-maximal exercise testing among patients with asthma [Astmalidotless hastalarda submaksimal egzersiz testinin üç modu sidotlessrasidotlessnda miyokardiyal oksijen tüketiminin karÅŸidotlesslaÅŸtidotlessrmasidotless]. TAF Preventive Medicine Bulletin. 2012;11(5):559–64. [Google Scholar]
- 65.Bruno AU CG: Insalaco G: Barazzoni R: Ballacchino A: Gjomarkaj M: Pace E Nutritional status and physical inactivity in moderated asthmatics: A pilot study . Medicine (United States). 2016;95(31). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pokladnikova JS-K I Effectiveness of a Comprehensive Lifestyle Modification Program for Asthma Patients: A Randomized Controlled Pilot Trial. J Asthma. 2013;50(3):318–26. [DOI] [PubMed] [Google Scholar]
- 67.O’Neill CB K: Sanchez O: Dogra S The acute response to interval and continuous exercise in adults with confirmed airway hyper-responsiveness. Journal of science and medicine in sport. 2017. [DOI] [PubMed] [Google Scholar]
- 68.Scott HAL JR: Callister R: Pretto JJ: Baines K: Saltos N: Upham JW: Wood LG Acute exercise is associated with reduced exhaled nitric oxide in physically inactive adults with asthma. Annals of Allergy, Asthma & Immunology : Official Publication of the American College of Allergy, Asthma, & Immunology. 2015;114(6):470–9. [DOI] [PubMed] [Google Scholar]
- 69.Anderson SD, Pearlman DS, Rundell KW, Perry CP, Boushey H, Sorkness CA, et al. Reproducibility of the airway response to an exercise protocol standardized for intensity, duration, and inspired air conditions, in subjects with symptoms suggestive of asthma. Respir Res. 2010;11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gomieiro LT, Nascimento A, Tanno LK, Agondi R, Kalil J, Giavina-Bianchi P. Respiratory exercise program for elderly individuals with asthma. Clinics (Sao Paulo). 2011;66(7): 1163–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Scott H, Wood L, Upham J. A single bout of moderate-intensity exercise reduces eosinophilic airway inflammation in inactive adults with asthma, while vigorous-intensity exercise has no effect. Respirology. 2018;23:33. [Google Scholar]
- 72.Scott HA, Gibson PG, Garg ML, Pretto JJ, Morgan PJ, Callister R, et al. Clinical asthma outcomes are improved after body fat reduction in overweight and obese asthmatics. American Journal of Respiratory and Critical Care Medicine. 2011;183(1). [Google Scholar]
- 73.Scott HA, Gibson PG, Garg ML, Pretto JJ, Morgan PJ, Callister R, et al. Determinants of weight loss success utilizing a meal replacement plan and/or exercise, in overweight and obese adults with asthma. Respirology. 2015;20(2):243–50. [DOI] [PubMed] [Google Scholar]
- 74.Zietkowski Z, Bodzenta-Lukaszyk A, Tomasiak MM, Skiepko R, Mroczko B, Szmitkowski M. Changes in RANTES and β-thromboglobulin after intensive exercise in patients with allergic asthma. Int Arch Allergy Immunol. 2008;148(1):31–40. [DOI] [PubMed] [Google Scholar]
- 75.Zietkowski Z, Skiepko R, Tomasiak MM, Bodzenta-Lukaszyk A. Soluble CD40 ligand and soluble P-selectin in allergic asthma patients during exercise-induced bronchoconstriction. J Invest Allergol Clin Immunol. 2008;18(4):272–8. [PubMed] [Google Scholar]
- 76.Silva RAd, De Freitas PD, Rocco PGL, Saccomani M, Grandi A, Evaristo KB, et al. Comparison among different instruments to evaluate the clinical control in asthmatic patients submitted to aerobic training. Eur Resp J. 2015;46(suppl 59):PA3712. [Google Scholar]
- 77.Freitas PDF, Silva Palmira G., Stelmach Aline G., Carvalho-Pinto Rafael, Fernandes Regina M., Mancini Frederico L. A., Sato Marcia C., Martins Maria N., Carvalho Milton A., Celso RF The Role of Exercise in a Weight-Loss Program on Clinical Control in Obese Adults with Asthma A Randomized Controlled Trial. American Journal of Respiratory and Critical Care Medicine. 2017;195(1):32–42. [DOI] [PubMed] [Google Scholar]
- 78.Rodrigues Mendes FAA, Cukier Francine Maria, Stelmach Alberto, Jacob-Filho Rafael, Martins Wilson, Fernandes Carvalho Milton A., Ricardo Celso. Effects of Aerobic Training on Airway Inflammation in Asthmatic Patients. Medicine and science in sports and exercise. 2011;43(2):197–203. [DOI] [PubMed] [Google Scholar]
- 79.Shaw BSS I Pulmonary function and abdominal and thoracic kinematic changes following aerobic and inspiratory resistive diaphragmatic breathing training in asthmatics. Lung. 2011;189(2):131–9. [DOI] [PubMed] [Google Scholar]
- 80.Alison J Physical training improves asthmatic subjects’ cardiopulmonary function. Australian Journal of Physiotherapy. 2000;46(4):315. [Google Scholar]
- 81.Lowe A GDO A, Stern DA, Gerald LB, Bime C Feasibility of a Home-Based Exercise Intervention with RemoteGuidance for Obese Asthmatics. Am J Respir Crit Care Med 2018. (197):A4843. [Google Scholar]
- 82.Arandelovi MS I: Nikoli M Swimming and persons with mild persistant asthma. Thescientificworldjournal. 2007;7:1182–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Abd El-Kader SMA-J OH: Ashmawy EM: Gaowgzeh RAM Treadmill walking exercise modulates bone mineral status and inflammatory cytokines in obese asthmatic patients with long term intake of corticosteroids. African Health Sciences. 2016;16(3):798–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Razavi MN, Hanachi Parichehr, Parichehr. The effect of an exercise programme and consumption of vitamin D on performance and respiratory indicators in patients with asthma. Sport Sciences for Health. 2011;6(2):89–92. [Google Scholar]
- 85.Bacon S, Lavoie K, Bourbeau J, Lemiere C, Pepin V, Beland M. Impact of a 12-week supervised aerobic exercise program on asthma control in adult patients with asthma: Preliminary results from the EX-ASTHMA behavioral RCT. Chest. 2015;148(4). [Google Scholar]
- 86.Refaat AG M Effect of physical training on health-related quality of life in patients with moderate and severe asthma. Egyptian Journal of Chest Diseases and Tuberculosis. 2015;64(4):761–6. [Google Scholar]
- 87.Paul DM P The effect of regular brisk walking on quality of life and lung function in partially controlled adult asthmatics. European Respiratory Journal. 2013;42. [Google Scholar]
- 88.Scichilone NM, Zangla Giuseppe, Arrigo Daniele, Cardillov Rita, Bellia Irene, Bonsignore Vincenzo, Rosaria Maria. Effects of exercise training on airway closure in asthmatics. Journal of applied physiology. 2012;113(5):714–8. [DOI] [PubMed] [Google Scholar]
- 89.Scott HAG PG: Garg ML: Pretto JJ: Morgan PJ: Callister R: Wood LG Dietary restriction and exercise improve airway inflammation and clinical outcomes in overweight and obese asthma: a randomized trial. Clinical and experimental allergy : journal of the British Society for Allergy and Clinical Immunology. 2013;43(1):36–49. [DOI] [PubMed] [Google Scholar]
- 90.Turner SE P: Cook A: Jenkins S Improvements in symptoms and quality of life following exercise training in older adults with moderate/severe persistent asthma. Respiration; international review of thoracic diseases. 2011;81(4):302–10. [DOI] [PubMed] [Google Scholar]
- 91.Ma JS P: Xiao L: Lavori PW: Camargo CA Jr.: Wilson SR: Gardner CD: Buist AS: Haskell WL: Lv N Behavioral weight loss and physical activity intervention in obese adults with asthma. A randomized trial. Annals of the American Thoracic Society. 2015;12(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Meyer AG S: Volmer T: Taube K: Baumann HJ A 12-month, moderate-intensity exercise training program improves fitness and quality of life in adults with asthma: A controlled trial. BMC Pulmonary Medicine. 2015;15(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gonçalves RC: Nunes MPT: CR A, Stelmach Martins M. A.: Carvalho CRF Effects of an aerobic physical training program on psychosocial characteristics, quality-of-life, symptoms and exhaled nitric oxide in individuals with moderate or severe persistent asthma. Brazilian Journal of Physical Therapy / Revista Brasileira de Fisioterapia. 2008;12(2):127–35. [Google Scholar]
- 94.França-Pinto AM FAR: De Carvalho-Pinto RM: Agondi RC: Cukier A: Stelmach R: Saraiva-Romanholo BM: Kalil J: Martins MA: Giavina-Bianchi P: Carvalho CRF Aerobic training decreases bronchial hyperresponsiveness and systemic inflammation in patients with moderate or severe asthma: A randomised controlled trial. Thorax. 2015;70(8):732–9. [DOI] [PubMed] [Google Scholar]
- 95.Pinto AM F: Agondi R: Saraiva-Romanholo B: Stelmach R: Cukier A: Martins M: Kalil J: Carvalho C: Giavina-Bianchi P Effect of aerobic exercise training on bronchial hyperresponsiveness, airway inflammation and health related quality of life in asthmatic patients: A pilot study. European Respiratory Journal. 2012;40. [Google Scholar]
- 96.Mendes FF-P, Cukier Andrezza, Stelmach Alberto, Agondi Rafael, Martins Rosana, Kalil Milton A., Giavina-Bianchi Jorge, Carvalho Pedro, Celso RF Aerobic training decreases bronchial hyperresponsiveness, serum chemokines and symptoms in asthmatic patients: Randomized controlled trial. European Respiratory Journal. 2013;42. [Google Scholar]
- 97.Carvalho CRFF-P, Mendes Andrezza, Stelmach Felipe A. R., Cukier Rafael, Agondi Alberto, Martins Rosana C., Saraiva-Romanholo Milton A., Kalil Beatriz M., Giavina-Bianchi Jorge, Pedro. Aerobic training decrease bronchial hyperresponsiveness and systemic inflammation in patients with moderate or severe asthma: A randomized controlled trial. European Respiratory Journal. 2014;44. [DOI] [PubMed] [Google Scholar]
- 98.Mendes FARG, Raquel C: Nunes Maria P. T.: Saraiva-Romanholo Beatriz M.: Cukier, Stelmach Alberto, Jacob-Filho Rafael, Martins Wilson, Carvalho Milton A., Celso RF Effects of Aerobic Training on Psychosocial Morbidity and Symptoms in Patients With Asthma A Randomized Clinical Trial. Chest. 2010;138(2):331–7. [DOI] [PubMed] [Google Scholar]
- 99.Freitas PF PG: Silva AG: Stelmach R: Carvalho-Pinto R: Fernandes FLA: Martins MA: Mancini MC: Sato MN: Carvalho CRF Mechanisms underlying the role of exercise training as part of a weight loss program on asthma control in obese asthmatics. European Respiratory Journal. 2016;48. [Google Scholar]
- 100.Boyd AW, Estell K, Dransfield M, Schwiebert L. The effect of aerobic exercise on asthma-related responses in adults. Journal of Allergy and Clinical Immunology. 2011;127(2):AB223. [Google Scholar]
- 101.Boyd AY, Estell Celeste T., Tuggle Kim, Gerald Craig M. S., Dransfield Lynn B., Bamman Mark, Bonner Marcas, Atkinson James, Schwiebert Prescott, Lisa M Feasibility of exercising adults with asthma: a randomized pilot study. Allergy Asthma and Clinical Immunology. 2012;8:13-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Shaw IS BS: Brown GA Role of diaphragmatic breathing and aerobic exercise in improving pulmonary function and maximal oxygen consumption in asthmatics. Science & Sports. 2010;25(3):139–45. [Google Scholar]
- 103.Shaw BSS I Static standing posture and pulmonary function in moderate- persistent asthmatics following aerobic and diaphragmatic breathing training. Pakistan Journal of Medical Sciences. 2011;27(3):549–52. [Google Scholar]
- 104.Freitas PD, Ferreira PG, Silva AG, Cukier A, Pinto RC, Salge JM, et al. Exercise training associated with a weight-loss lifestyle program improves daily physical activity in obese asthmatics. European Respiratory Journal. 2014;44. [Google Scholar]
- 105.Haas F, Pasierski S, Levine N, Bishop M, Axen K, Pineda H, et al. Effect of aerobic training on forced expiratory airflow in exercising asthmatic humans. Journal of Applied Physiology. 1987;63(3):1230–5. [DOI] [PubMed] [Google Scholar]
- 106.Saccomani M, Evaristo K, Cukier A, Stelmach R, Carvalho M, Carvalho C. Comparison between the effects of aerobic and breathing exercises in the clinical and psychosocial factors in asthmatic patients. European Respiratory Journal. 2013;42. [Google Scholar]
- 107.Saccomani M, Evaristo K, Rojo M, Santaella DF, Cukier A, Stelmach R, et al. Comparison between the effects of aerobic and breathing exercises on clinical and psychosocial morbidity in asthmatic patients. European Respiratory Journal. 2014;44. [Google Scholar]
- 108.Turk Y, Van Huisstede A, Van Der Geijn GJ, Hiemstra P, Taube C, Braunstahl GJ. Effect of a high intensity life style program on asthma control in obese patients with asthma. European Respiratory Journal. 2017;50. [DOI] [PubMed] [Google Scholar]
- 109.Toennesen LL MH, Hostrup M, Geiker NRW, Jensen CB, Porsbjerg C, Astrup A, Bangsbo J, Parker D, Backer V. Effects of exercise and diet in non-obese asthma patients– a randomised controlled trial. Journal of Allergy and Clinical Immunology-In Practice. 2017;Accepted for publication. [DOI] [PubMed] [Google Scholar]
- 110.Freitas PD, Ferreira PG, Analuci S, Stelmach R, Pinto RC, Sage JM, et al. Effects of exercise training in a weight loss lifestyle intervention on clinical control, quality of life and psychosocial symptoms in obese asthmatics: A RCT. Eur Resp J. 2014;44(Suppl 58):1710. [Google Scholar]
- 111.Freitas PD, Ferreira PG, Silva AG, Cukier A, Stelmach R, Carvalho-Pinto R, et al. Exercise training is a determinant of weight-loss and improvement on asthma control, airway inflammation and psychosocial morbidity in obese asthmatics: A RCT. Eur Resp J. 2015;46(suppl 59):PA734. [Google Scholar]
- 112.Evaristo KB, Saccomani MG, Cukier A, Stelmach R, Carvalho-Pinto R, Santaella DF, et al. Effects of aerobic and breathing exercises on clinical control and airway inflammation in persistent asthma. Eur Resp J. 2017;50(suppl 61):OA2919. [Google Scholar]
- 113.Evaristo KB, Mendes FAR, Saccomani MG, Cukier A, Carvalho-Pinto RM, Rodrigues MR, et al. Effects of Aerobic Training Versus Breathing Exercises on Asthma Control: A Randomized Trial. The Journal of Allergy and Clinical Immunology: In Practice. 2020;8(9):2989–96.e4. [DOI] [PubMed] [Google Scholar]
- 114.Juniper E, Guyatt G, Cox F, Ferrie P, King D. Development and validation of the Mini Asthma Quality of Life Questionnaire. Eur Resp J. 1999;14(1):32–8. [DOI] [PubMed] [Google Scholar]
- 115.De Oliveira MA, Barbiere A, Santos LA, Faresin SM, Fernandes AL. Validation of a simplified quality-of-life questionnaire for socioeconomically deprived asthma patients. The Journal of asthma : official journal of the Association for the Care of Asthma. 2005;42(1):41–4. [DOI] [PubMed] [Google Scholar]
- 116.Reddel HK, Bateman ED, Becker A, Boulet LP, Cruz AA, Drazen JM, et al. A summary of the new GINA strategy: a roadmap to asthma control. The European respiratory journal. 2015;46(3):622–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gaston MH, Porter GK, Thomas VG. Prime Time Sister Circles: evaluating a gender-specific, culturally relevant health intervention to decrease major risk factors in mid-life African-American women. Journal of the National Medical Association. 2007;99(4):428–38. [PMC free article] [PubMed] [Google Scholar]
- 118.Krishnan JA, Lemanske RF Jr., Canino GJ, Elward KS, Kattan M, Matsui EC, et al. Asthma outcomes: symptoms. J Allergy Clin Immunol. 2012;129(3 Suppl):S124–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.“Well-being Concepts “ Health-Related Quality of Life (HRQOL) 2018. [Available from: https://www.cdc.gov/hrqol/wellbeing.htm.
- 120.Juniper EF, Jenkins C, Price MJ, James MH. Impact of inhaled salmeterol/fluticasone propionate combination product versus budesonide on the health-related quality of life of patients with asthma. Am J Respir Med. 2002;1(6):435–40. [DOI] [PubMed] [Google Scholar]
- 121.Rutten-van Molken MP, Custers F, van Doorslaer EK, Jansen CC, Heurman L, Maesen FP, et al. Comparison of performance of four instruments in evaluating the effects of salmeterol on asthma quality of life. Eur Respir J. 1995;8(6):888–98. [PubMed] [Google Scholar]
- 122.Rowe BH, Oxman AD. Performance of an asthma quality of life questionnaire in an outpatient setting. Am Rev Respir Dis. 1993;148(3):675–81. [DOI] [PubMed] [Google Scholar]
- 123.Dixon AE, Holguin F, Sood A, Salome CM, Pratley RE, Beuther DA, et al. An official American Thoracic Society Workshop report: obesity and asthma. Proceedings of the American Thoracic Society. 2010;7(5):325–35. [DOI] [PubMed] [Google Scholar]
- 124.Peters MC, McGrath KW, Hawkins GA, Hastie AT, Levy BD, Israel E, et al. Plasma interleukin-6 concentrations, metabolic dysfunction, and asthma severity: a cross-sectional analysis of two cohorts. The Lancet Respiratory medicine. 2016;4(7):574–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Cordova-Rivera L, Gibson PG, Gardiner PA, McDonald VM. A Systematic Review of Associations of Physical Activity and Sedentary Time with Asthma Outcomes. The journal of allergy and clinical immunology In practice. 2018;6(6):1968–81.e2. [DOI] [PubMed] [Google Scholar]
- 126.Nyenhuis SM, Dixon A, Ma J “Impact of Lifestyle Interventions Targeting Healthy Diet, Physical Activity and Weight Loss on Asthma in Adults: What is the evidence?”. Journal of Allergy and Clinical Immunology: In Practice. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Cochrane Handbook for Systematic Reviews of Interventions. 2020.
- 128.Global Strategy for Asthma Management and Prevention. 2018.
- 129.Cloutier MM, Baptist AP, Blake KV, Brooks EG, Bryant-Stephens T, DiMango E, et al. 2020 Focused Updates to the Asthma Management Guidelines: A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group. Journal of Allergy and Clinical Immunology. 2020;146(6):1217–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


