Abstract
Background:
Sexual minority and racial/ethnic minority youth experience a higher burden of asthma. The frameworks of minority stress theory and intersectionality suggest sexual minority and racial/ethnic minority youth may experience disparities in non-remitting asthma.
Objective:
To examine adjusted odds of non-remitting asthma by sexual identity, race/ethnicity, and their intersections, along with their relationship with traditional non-remitting asthma risk factors (weight status and smoking) and victimization (bullying, cyberbullying, and forced sex).
Method:
We utilized data from the Youth Risk Behavior Survey (YRBS) pooled across 41 jurisdiction-years (biennially, 2009–2017), resulting in a sample of 21,789 U.S. youth. The prevalence of non-remitting asthma was examined by sexual identity, race/ethnicity, and their intersections, stratified by sex. Bivariate associations and backward logistic regression models, stratified by sex, were built to examine non-remitting asthma disparities and the effects of selected traditional correlates and victimization variables.
Results:
At the intersections, 8 sexual minority and racial/ethnic minority subpopulations were significantly more likely to have non-remitting asthma compared with White heterosexual sex-matched peers. White gay males and Black lesbian females had the highest odds of non-remitting asthma. Traditional risks of non-remitting asthma and victimization were associated with attenuated odds of non-remitting asthma.
Conclusion:
Many sexual minority and racial/ethnic youth sub-populations are more likely to have non-remitting asthma. Evidence suggests traditional non-remitting asthma risk factors and victimization may partly explain disparities in non-remitting asthma. Asthma management guidelines should be updated to include population health disparities of sexual and racial/ethnic minorities.
Keywords: Asthma, Asthma Remission, Non-remitting Asthma, Disparities, Sexual Minorities, Sexual Identity, Race/Ethnicity, Minority Stress, Intersectionality, Victimization, YRBS, Youth, United States
INTRODUCTION
Asthma is the most common chronic condition among children, affecting 8.4% of youth under 18 years.1,2 Among youth, asthma is a leading cause of hospitalization and is associated with an increased risk for developing diabetes and coronary heart disease in adulthood.3,4 Youth asthma management and surveillance, therefore, remains a top public health priority.2,5,6 Previous asthma surveillance reveals asthma prevalence disparities among youth and adults by sex, sexual identity, and race/ethnicity, as well as those multiply-marginalized by sexual identity and race/ethnicity1,7–16
Despite growing asthma surveillance research, non-remitting asthma is still not well understood. Clinical asthma remission is typically considered as the absence of asthma symptoms without the use of an asthma medication over a period of time (varying from 6 months to 5 years).17,18 In the present study, asthma remission was defined as the self-reported absence of asthma symptoms among those with a prior history of asthma. Most cases of asthma remission occur between ages 14 to 21, and the prevalence of remission has been estimated to be between 33% and 53% among youth under 18.17–19 Among youth and adult populations, there are sex-based differences in asthma remission with more males entering remission than females.18 Correlates of non-remitting asthma have also been identified: persons who smoke, have a body mass index percentile (BMIp) greater than 85, or have more severe asthma tend to have lower rates of remission.18 Notably, sexual minority and/or racial/ethnic minority (SM/REM) youth report a higher prevalence of smoking and elevated weight. 20,21 Additionally, although no studies have investigated asthma severity among sexual minority youth, asthma symptoms have been found to be more severe among racial/ethnic minority youth compared to their White counterparts.18,22 Taken together, the higher prevalence of non-remitting asthma risk factors among SM/REM youth suggests they may experience less asthma remission. Despite the evidence, though, no studies have investigated if such disparities exist by sexual identity. Only one study among youth has examined asthma remission by race/ethnicity, finding White individuals were more likely to experience asthma remission than non-White cohort members.23 Thus, additional surveillance with more precise populations is needed.
Minority stress theory (MST) and intersectionality are theoretical frameworks that can be applied to investigate health disparities of multiply-marginalized populations.24–26 MST posits that marginalized populations are disparately burdened with stigmatization, discrimination, and oppression that contributes to an overall heightened burden of stress.24 Minority stressors can take the form of proximal (e.g., internalized homophobia) or distal (e.g., prejudiced events such as victimization) stressors. The heightened chronic stress experienced can cause physiological changes, such as immune system dysregulation, which have been associated with the development of asthma.27 Stress-related coping can also manifest as maladaptive health behaviors that increase the prevalence of traditional risks of asthma non-remission, such as smoking and disordered eating that increases risk for a BMIp>95.18,24,28,29 Ultimately, the higher burden of chronic stress and stress-linked coping behaviors can exacerbate both mental and physical health conditions, potentially impacting the likelihood of asthma remission among marginalized populations.24,30,31
Furthermore, applying an intersectional lens expands the contextual scope of MST by specifically considering the health impacts of multiple marginalization.32,33 Intersectionality—a Black feminist framework developed by Crenshaw25 and Collins26—highlights that marginalization can manifest distinctly at the intersections of multiply-marginalized identities. At the person level, the framework emphasizes that individuals hold multiple characteristics (e.g., race/ethnicity and sexual orientation) but experience the world living in a single body. Applied to the present study, marginalization may be manifesting as excess experiences of victimization among SM/REM youth and impacting both maladaptive-stress coping behaviors and physiological stress responses that may disparately drive asthma remission outcomes among SM/REM sub-populations.
Neither the epidemiology of non-remitting asthma among SM/REM youth nor the association between non-remitting asthma and minority stress-related factors have ever been described. In the present study, we aim to advance the field of pediatric asthma remission research by describing patterns of non-remitting asthma within a large and geographically diverse dataset of high school-aged youth. Specifically, we aim to: (1) examine non-remitting asthma disparities among youth by sexual identity, race/ethnicity, and their intersections and (2) explore the impact of selected traditional asthma non-remission factors (weight status and smoking) and—based on MST—victimization (bullied, cyberbullied, and forced sex) on odds of non-remitting asthma.34 Informed by theory and the related background literature, we hypothesize differential prevalence of non-remitting asthma among SM/REM youth. We also expect traditional correlates of non-remitting asthma, as well as experiences of victimization to be associated with increased odds of non-remitting asthma.
METHODS
Data Source
The Youth Risk Behavior Survey (YRBS) is a biennial survey conducted by the Centers for Disease Control and Prevention (CDC) to collect health data on students in grades 9–12.35 We utilized local administrations of the YRBS, pooling data across jurisdictions of states and large, urban school districts. Jurisdictions use a two-stage cluster sample design to identify a representative sample of students.35 A new sample is selected each year the survey is administered. The YRBS data weights adjust for student non-response and distribution of students by grade, sex, and race/ethnicity in each jurisdiction.
Study Design
Local YRBS data were pooled across multiple jurisdictions and years (biennially, 2009–2017). Only jurisdiction-years including sexual identity, lifetime asthma, and current asthma measures were included in the sample, representing 137,107 students. For the present analyses, students were excluded if they were missing any of the primary demographic variables of interest (Sexual Identity, Race/Ethnicity, Age, Region), resulting in 129,196 participants. Finally, only individuals who reported having lifetime asthma and who answered “yes” or “no” to still having asthma were included, leaving a final analytic sample of 21,789 youth across 41 jurisdiction-years.
Measures
The following measures were used: Demographics (Sex, Sexual Identity, Race/Ethnicity, SM/REM Sub-Populations, Age, Region); Traditional Non-remitting Asthma Risk Factors (Obese and Overweight, Smoking Status); the Primary Outcome (Non-remitting Asthma); and Victimization Indicators (Bullied, Cyberbullied, Forced Sex). These victimization variables were selected because prior research has used victimization variables to represent manifestations of stigma that contribute to excess minority stress levels among SM/REM youth.34,36 These specific variables cover a range of social settings (school and non-school), and bullying is the most common form of victimization among SMY.7,34,36–38 Moreover, besides bullying, forced sex is the most common type of victimization experienced by sexual minority females, particularly bisexual women and women of color.7,38 For information on survey questions and classification for measures, see Table I.
Table I:
Measures, Question Wording, Response Options, and Classification, YRBS, 2009–2017
| Measures | Question Wording, Response Options, and Classification |
|---|---|
| Demographics | |
| Sex | Assessed by asking participants, “What is your sex?” Response options: male and female. |
| Sexual Identity (SI) | Assessed by asking participants, “Which of the following best describes you?” Response options: heterosexual (straight); gay or lesbian; bisexual; and not sure. |
| Race/Ethnicity (RE) | Participants were asked if they identified as Hispanic or Latino (yes or no) and to then select all races that applied to them: American Indian or Alaska Native; Asian; Black or African American; Native Hawaiian or Other Pacific Islander; and White. For our analyses, these were joined into 4 racial/ethnic groups: White; Black; Hispanic; and an Additional-race (including multiple-races). |
| SM/REM Sub-Populations | Participants who responded to both sexual identity and race/ethnicity questions were placed into 1 of 16 categories—a combination of (1) heterosexual; (2) gay or lesbian; (3) bisexual; and (4) not sure with (1) White; (2) Black; (3) Hispanic/Latinx; and (4) additional-race. |
| Age | Assessed by asking participants, “How old are you?” Response options ranged from 12 to 18 years old. Students selecting between 12 and 14 years old options were collapsed into “14 years old or younger.” |
| Region | Assessed by grouping jurisdictions together based on U.S. Census regions: Northeast; Midwest; South; and West. |
| Traditional Non-remitting Asthma Correlates 18 | |
| Obese and Overweight | Respondents were classified as obese or overweight based on body-mass index (BMI) calculated using participant-reported age, sex, height, and weight. Individuals with a BMI ≥ 95th percentile were classified as obese, while individuals with a BMI ≥ 85th percentile and < 95th percentile were classified as overweight.65 |
| Smoking Status | Participants were first asked, “Have you ever tried cigarette smoking, even one or two puffs?” Response options: yes and no. Students responding no were classified as (1) never smoked. Participants were then asked, “During the past 30 days, on how many days did you smoke cigarettes?” Response options ranged from 0 to 30 days. Students who selected yes to the first question and 0 days to the second were classified as (2) former smoker; those selecting yes to the first and more than 0 days to the second were classified as (3) current smoker. |
| Victimization Indicators | |
| Bullied | Assessed by asking participants, “During the past 12 months, have you ever been bullied on school property?” Response options: yes and no. |
| Cyberbullied | Assessed by asking participants, “During the past 12 months, have you ever been electronically bullied? (Include being bullied through e-mail, chat rooms, instant messaging, Web sites, or texting.).” Response options: yes and no. |
| Forced Sex | Assessed by asking “Have you ever been physically forced to have sexual intercourse when you did not want to?” Response options: yes and no. |
The primary outcome of non-remitting asthma was formed by first asking, “Has a doctor or nurse ever told you that you have asthma?” Response options: yes; no; and not sure. Participants were then asked, “Do you still have asthma?” Response options: I have never had asthma; yes; no; and not sure. For our analyses, those who responded yes to both questions were considered to have non-remitting asthma. Those who responded yes to the first question but no to the second were classified as in asthma remission. Participants responding differently from above were dropped from all models.
Statistical Analyses
All data cleaning and recoding was conducted in SAS Version 9.4 (SAS Institute, Cary, NC). SAS-Callable SUDAAN Version 11.0.1 (RTI International, Research Triangle Park, NC) was used to appropriately weight estimates and account for the complex sampling design of the YRBS. First, bivariate logistic regressions with traditional non-remitting asthma risk factors and experiences of victimization, stratified by sex, were conducted. Multivariate logistic regressions were used to assess any potential correlates of asthma remission. Predictors were removed in a stepwise manner until only those with p<0.10 (to capture any potential correlate) remained in the model. All adjusted models contained demographics (age, region, race/ethnicity, and sexual identity) and survey year.
RESULTS
The analytic sample (n=21,789) consisted of nearly equal proportions of males (49.2%) and females (50.8%; Table II). The sample predominately identified as heterosexual (87.4%), followed by bisexual (6.9%), not sure (3.2%), and lesbian or gay (2.4%). Slightly over half were White (51.2%)—followed by Black (24.0%), Hispanic or Latinx (17.7%), and additional-race (7.1%). Approximately one-third (33.3%) of respondents had experienced asthma remission. By sex, 40.5% of males experienced remission compared with 26.3% of females (p<0.001), corresponding with prior literature.7,18,19
Table II.
Participant Demographics and Non-remitting Asthma among High School Youth, YRBS, 2009–2017
| Total | Male | Female | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Demographics | 21,789 | -- | 10,323 | 49.21 | 11,466 | 50.79 |
| Sexual Identity (SI) | ||||||
| Heterosexual | 19,076 | 87.43 | 9,521 | 92.62 | 9,555 | 82.41 |
| Lesbian/Gay | 533 | 2.43 | 236 | 1.93 | 297 | 2.92 |
| Bisexual | 1,494 | 6.91 | 282 | 2.54 | 1,212 | 11.15 |
| Not Sure | 686 | 3.22 | 284 | 2.91 | 402 | 3.52 |
| Race/Ethnicity (RE) | ||||||
| White | 11,100 | 51.15 | 5,198 | 50.98 | 5,902 | 51.31 |
| Black | 2,920 | 24.02 | 1,376 | 23.91 | 1,544 | 24.12 |
| Hispanic/Latinx | 4,105 | 17.73 | 1,944 | 17.97 | 2,161 | 17.5 |
| Additional-Race | 3,664 | 7.10 | 1,805 | 7.14 | 1,859 | 7.07 |
| Age, years | ||||||
| 14 or younger | 2,941 | 10.55 | 1,342 | 10.63 | 1,599 | 10.47 |
| 15 | 5,627 | 24.89 | 2,637 | 25.03 | 2,990 | 24.76 |
| 16 | 5,732 | 26.98 | 2,762 | 26.93 | 2,970 | 27.04 |
| 17 | 5,077 | 24.14 | 2,363 | 22.83 | 2,714 | 25.1 |
| 18 or older | 2,412 | 13.44 | 1,219 | 14.58 | 1,193 | 12.33 |
| Region | ||||||
| Northeast | 9,306 | 5.49 | 4,354 | 5.48 | 4,952 | 5.5 |
| Midwest | 3,169 | 32.52 | 1,469 | 31.58 | 1,700 | 33.43 |
| South | 4,928 | 51.90 | 2,376 | 52.81 | 2,552 | 51.01 |
| West | 4,386 | 10.09 | 2,124 | 10.13 | 2,262 | 10.05 |
| SI and RE Intersections | ||||||
| Heterosexual | ||||||
| White | 9,906 | 45.52 | 4,871 | 47.95 | 5,035 | 42.97 |
| Black | 2,546 | 20.88 | 1,265 | 22.03 | 1,281 | 19.76 |
| Hispanic/Latinx | 3,484 | 15.17 | 1,757 | 16.27 | 1,727 | 14.1 |
| Additional-Race | 3,140 | 5.97 | 1,628 | 6.37 | 1,512 | 5.58 |
| Lesbian/Gay | ||||||
| White | 208 | 0.92 | 89 | 0.65 | 119 | 1.19 |
| Black | 103 | 0.8 | 41 | 0.56 | 62 | 1.04 |
| Hispanic/Latinx | 124 | 0.55 | 54 | 0.56 | 70 | 0.55 |
| Additional-Race | 98 | 0.16 | 52 | 0.17 | 46 | 0.14 |
| Bisexual | ||||||
| White | 691 | 3.14 | 116 | 0.92 | 575 | 5.3 |
| Black | 184 | 1.74 | 42 | 0.86 | 142 | 2.59 |
| Hispanic/Latinx | 339 | 1.34 | 63 | 0.37 | 276 | 2.28 |
| Additional-Race | 280 | 0.69 | 61 | 0.39 | 219 | 0.98 |
| Not Sure | ||||||
| White | 295 | 1.66 | 122 | 1.47 | 173 | 1.86 |
| Black | 87 | 0.6 | 28 | 0.47 | 59 | 0.73 |
| Hispanic/Latinx | 158 | 0.67 | 70 | 0.77 | 88 | 0.58 |
| Additional-Race | 146 | 0.28 | 64 | 0.21 | 82 | 0.36 |
| OUTCOME | ||||||
| Non-remitting Asthma | ||||||
| Yes | 14,849 | 66.71 | 6,323 | 59.5 | 8,526 | 73.69 |
| No | 6,940 | 33.29 | 4,000 | 40.5 | 2,940 | 26.31 |
Bivariate Associations with Non-remitting Asthma
Across sexual identity and race/ethnicity separately, gay (odds ratio [OR]: 2.71; 95% confidence interval [CI]: 1.51–7.84), Black (OR:1.80; 95% CI:1.38–2.34), and additional-race (OR:1.30; 95% CI:1.01–1.69) male students were significantly more likely to have non-remitting asthma compared with heterosexual or White, sex-matched students (Table III). Among females, only Black respondents (OR:1.52; 95% CI:1.20–1.92) were significantly more likely to have non-remitting asthma compared with White female respondents. Hispanic/Latinx females were less likely to have non-remitting asthma (OR:0.68; 95% CI:0.56–0.83) than White females.
Table III:
Prevalence and Unadjusted Odds Ratios for Non-remitting Asthma by Sexual Identity (SI), Race/Ethnicity (RE), and their Intersections, YRBS, 2009–2017.
| Male | Female | |||||||
|---|---|---|---|---|---|---|---|---|
| Non-remitting Asthma (weighted %) | N/Total | OR | 95% CI | Non-remitting Asthma (weighted %) | N/Total | OR | 95% CI | |
| Selected Demographics | ||||||||
| Sexual Identity | ||||||||
| Heterosexual | 58.80 | 5776/9521 | REF | -- | 73.19 | 7026/9555 | REF | -- |
| Lesbian/Gay | 78.63 | 162/236 | 2.71 | (1.51, 4.84) | 80.66 | 236/297 | 1.37 | (0.87, 2.18) |
| Bisexual | 63.68 | 192/282 | 1.17 | (0.66, 2.06) | 75.84 | 956/1212 | 1.09 | (0.78, 1.52) |
| Not Sure | 65.39 | 193/284 | 1.48 | (0.85, 2.58) | 72.72 | 308/402 | 0.99 | (0.61, 1.61) |
| Race/Ethnicity | ||||||||
| White | 55.94 | 3159/5198 | REF | -- | 73.68 | 4471/5902 | REF | -- |
| Black | 69.44 | 949/1376 | 1.80 | (1.38, 2.34) | 81.14 | 1237/1544 | 1.52 | (1.20, 1.92) |
| Hispanic/Latinx | 55.37 | 1127/1944 | 0.97 | (0.80, 1.17) | 65.68 | 1483/2161 | 0.68 | (0.56, 0.83) |
| Additional-Race | 62.06 | 1088/1805 | 1.30 | (1.01, 1.69) | 68.18 | 1335/1859 | 0.81 | (0.61, 1.06) |
| Age, years | ||||||||
| 14 or younger | 68.46 | 898/1342 | REF | -- | 76.96 | 1215/1599 | REF | -- |
| 15 | 60.07 | 1681/2637 | 0.86 | (0.63, 1.16) | 74.09 | 2247/2990 | 0.86 | (0.63, 1.16) |
| 16 | 59.50 | 1680/2762 | 0.93 | (0.68, 1.26) | 75.61 | 2217/2970 | 0.93 | (0.68, 1.26) |
| 17 | 56.91 | 1388/2363 | 0.79 | (0.59, 1.05) | 72.41 | 1980/2714 | 0.79 | (0.59, 1.05) |
| 18 or older | 56.07 | 676/1219 | 0.65 | (0.46, 0.93) | 68.52 | 867/1193 | 0.65 | (0.46, 0.93) |
| Region | ||||||||
| Northeast | 63.04 | 2758/4353 | REF | -- | 76.48 | 3811/4952 | REF | -- |
| Midwest | 62.58 | 943/1469 | 0.98 | (0.82, 1.17) | 76.05 | 1313/1700 | 0.98 | (0.82, 1.16) |
| South | 57.18 | 1367/2376 | 0.78 | (0.67, 0.92) | 72.01 | 1798/2552 | 0.79 | (0.67, 0.94) |
| West | 60.1 | 1255/2124 | 0.88 | (0.70, 1.12) | 72.83 | 1604/2262 | 0.82 | (0.67, 1.01) |
| SI and RE Intersections | ||||||||
| Heterosexual | ||||||||
| White | 54.82 | 2922/4871 | REF | -- | 74.62 | 3790/5035 | REF | -- |
| Black | 69.75 | 876/1265 | 1.94 | (1.48, 2.54) | 79.36 | 1012/1281 | 1.27 | (0.98, 1.64) |
| Hispanic/Latinx | 50.24 | 999/1757 | 0.97 | (0.79, 1.18) | 63.41 | 1156/1727 | 0.58 | (0.46, 0.72) |
| Additional-Race | 62.62 | 979/1628 | 1.40 | (1.07, 1.83) | 65.10 | 1068/1512 | 0.66 | (0.49, 0.88) |
| Lesbian/Gay | ||||||||
| White | 93.36 | 68/89 | 17.65 | (6.98, 44.67) | 67.7 | 93/119 | 0.60 | (0.31, 1.16) |
| Black | 76.77 | 28/41 | 2.67 | (0.98, 7.24) | 95.07 | 55/62 | 7.07 | (2.01, 24.77) |
| Hispanic/Latinx | 61.31 | 33/54 | 1.20 | (0.46, 3.14) | 84.86 | 53/70 | 1.79 | (0.63, 5.11) |
| Additional-Race | 85.61 | 33/52 | 4.79 | (1.74, 13.18) | 67.89 | 35/46 | 0.75 | (0.17, 3.38) |
| Bisexual | ||||||||
| White | 71.44 | 76/116 | 1.95 | (0.76, 5.01) | 71.21 | 456/575 | 0.77 | (0.46, 1.29) |
| Black | 55.40 | 28/42 | 0.95 | (0.35, 2.63) | 86.04 | 118/142 | 2.03 | (1.03, 4.01) |
| Hispanic/Latinx | 71.83 | 44/63 | 1.80 | (0.61, 5.32) | 71.58 | 211/276 | 0.83 | (0.52, 1.34) |
| Additional-Race | 56.00 | 44/61 | 1.01 | (0.33, 3.15) | 83.76 | 171/219 | 1.84 | (0.92, 3.68) |
| Not Sure | ||||||||
| White | 66.27 | 93/122 | 1.86 | (0.83, 4.15) | 62.94 | 132/173 | 0.57 | (0.29, 1.14) |
| Black | 71.80 | 17/28* | 1.61 | (0.39, 6.71) | 91.94 | 52/59 | 3.52 | (0.96, 12.92) |
| Hispanic/Latinx | 67.44 | 51/70 | 2.16 | (0.91, 5.16) | 79.42 | 63/88 | 1.45 | (0.66, 3.19) |
| Additional-Race | 36.87 | 32/53 | 0.61 | (0.19, 1.98) | 73.41 | 61/82 | 0.91 | (0.34, 2.42) |
| Selected Variables | ||||||||
| Smoking Status | ||||||||
| Never smoked | 61.39 | 2265/3629 | REF | -- | 75.18 | 3199/4274 | REF | -- |
| Former smoker | 59.66 | 673/1134 | 0.93 | (0.70, 1.24) | 79.71 | 1047/1366 | 1.30 | (1.01, 1.66) |
| Current smoker | 58.78 | 448/705 | 0.90 | (0.65, 1.25) | 79.46 | 542/685 | 1.28 | (0.83, 1.96) |
| Obese | ||||||||
| Yes | 64.07 | 1232/1893 | 1.29 | (1.03, 1.61) | 77.51 | 1019/1288 | 1.28 | (0.95, 1.72) |
| No | 58.08 | 4730/7882 | REF | -- | 72.97 | 6891/2473 | REF | -- |
| Overweight | ||||||||
| Yes | 55.87 | 931.1563 | 0.85 | (0.67, 1.08) | 74.46 | 1479/1967 | 1.06 | (0.83, 1.35) |
| No | 59.82 | 5031/8212 | REF | -- | 73.35 | 6431/8685 | REF | -- |
| Bullied | ||||||||
| Yes | 64.34 | 1261/1868 | 1.29 | (1.03, 1.62) | 79.55 | 2199/2754 | 1.54 | (1.23, 1.92) |
| No | 58.3 | 4937/8258 | REF | -- | 71.65 | 6153/8494 | REF | -- |
| Cyberbullied | ||||||||
| Yes | 65.25 | 699/1017 | 1.34 | (0.95, 1.88) | 78.28 | 1818/2295 | 1.39 | (1.10, 1.76) |
| No | 58.34 | 4602/7736 | REF | -- | 72.12 | 5348/7362 | REF | -- |
| Forced Sex | ||||||||
| Yes | 65.93 | 381/524 | 1.30 | (0.88, 1.90) | 79.97 | 990/1244 | 1.49 | (1.13, 1.97) |
| No | 59.9 | 4912/8026 | REF | -- | 72.82 | 6016/8149 | REF | -- |
Boldface indicates statistical significance (p<0.05)
Analyses performed with small sub-population
Among males, a BMIp>95 (OR:1.29; 95% CI:1.03–1.61) and being bullied (OR:1.29; 95% CI:1.03–1.62) were significantly associated with increased odds of non-remitting asthma. Among females, being a former smoker (OR:1.30; 95% CI:1.01–1.66), being bullied (OR:1.54; 95% CI:1.23–1.92), being cyberbullied (OR:1.39; 95% CI:1.10–1.76), and experiencing forced sex (OR:1.49; 95% CI:1.13–1.97) were associated. Unadjusted models for SM/REM subpopulations across males and females are included in Table III.
Sex-Stratified SM/REM Analyses
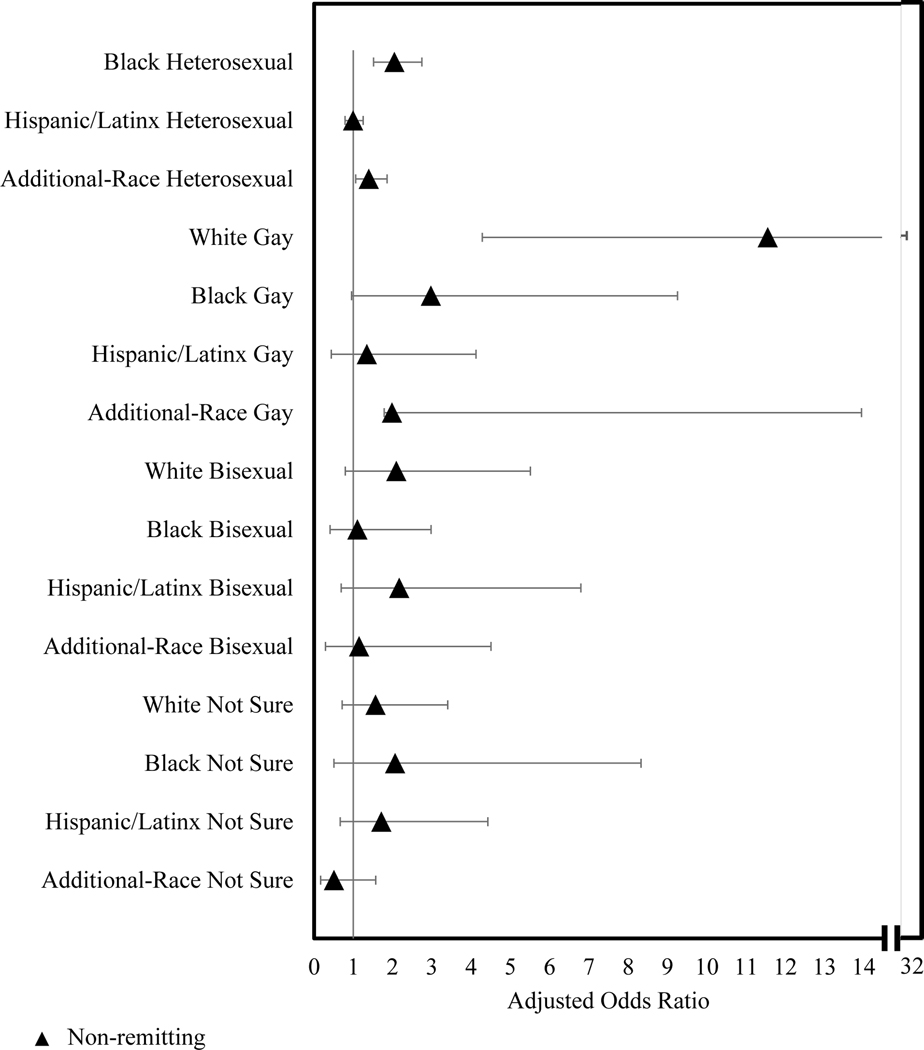
Among males and in models adjusted for demographics (Table IV Model I; Figure 1), all four sub-populations with significantly elevated odds of non-remitting asthma from unadjusted models remained—Black heterosexual (adjusted OR [AOR] 2.05; 95% CI: 1.52–2.75), additional-race heterosexual (AOR 1.40; 95% CI: 1.06–1.86), White gay (AOR 11.56; 95% CI: 4.29–31.14), and additional-race gay (AOR 1.99; 95% CI: 1.79–13.95) males.
Table IV:
Stepwise Adjusted Odds Ratios for Non-remitting Asthma by Sexual Identity (SI) and Race/Ethnicity (RE) Intersections among Males, YRBS, 2009–2017.
| Model I: Demographics N = 10,323 | Model II: Model I + Selected Factors N = 8,293 | |||||
|---|---|---|---|---|---|---|
| n | AOR | 95% CI | n | AOR | 95% CI | |
| SI and RE Intersections | ||||||
| Heterosexual | ||||||
| White | 4871 | REF | -- | 4871 | REF | -- |
| Black | 1265 | 2.05 | (1.52,2.75) | 1265 | 2.01 | (1.47, 2.75) |
| Hispanic/Latinx | 1757 | 1.00 | (0.79,1.25) | 1757 | 1.02 | (0.80, 1.31) |
| Additional-Race | 1628 | 1.40 | (1.06,1.86) | 1628 | 1.44 | (1.04, 2.00) |
| Gay | ||||||
| White | 89 | 11.56 | (4.29,31.14) | 89 | 11.09 | (3.58, 34.38) |
| Black | 41 | 2.98 | (0.96,9.26) | 41 | 2.95 | (0.66, 13.14) |
| Hispanic/Latinx | 54 | 1.35 | (0.44,4.13) | 54 | 1.03 | (0.37, 2.85) |
| Additional-Race | 52 | 1.99 | (1.79,13.95) | 52 | 3.06 | (1.00, 9.39) |
| Bisexual | ||||||
| White | 116 | 2.10 | (0.80,5.51) | 116 | 2.64 | (0.91, 7.70) |
| Black | 42 | 1.11 | (0.41,2.98) | 42 | 1.11 | (0.36, 3.41) |
| Hispanic/Latinx | 63 | 2.17 | (0.69,6.80) | 63 | 1.96 | (0.45, 8.53) |
| Additional-Race | 61 | 1.15 | (0.29,4.51) | 61 | 1.08 | (0.21, 5.50) |
| Not Sure | ||||||
| White | 122 | 1.57 | (0.72,3.41) | 122 | 1.3 | (0.59, 2.88) |
| Black | 28* | 2.07 | (0.51,8.33) | 28* | 1.23 | (0.23, 6.66) |
| Hispanic/Latinx | 70 | 1.72 | (0.67,4.43) | 70 | 1.65 | (0.52, 5.22) |
| Additional-Race | 64 | 0.51 | (0.17,1.57) | 64 | 0.93 | (0.26, 3.35) |
| Selected Demographics * | ||||||
| Region | ||||||
| Northeast | 4354 | REF | -- | 4354 | REF | -- |
| Midwest | 1469 | 0.92 | (0.77,1.11) | 1469 | 1.05 | (0.84, 1.31) |
| South | 2379 | 0.66 | (0.54,0.82) | 2379 | 0.73 | (0.58, 0.91) |
| West | 2124 | 0.81 | (0.62,1.06) | 2124 | 0.74 | (0.56, 0.99) |
| Selected Variables | ||||||
| Cyberbullied | ||||||
| Yes | -- | -- | -- | 1017 | 1.39 | (0.96, 2.02) |
| No | -- | -- | -- | 7736 | REF | -- |
| Obese | ||||||
| Yes | -- | -- | -- | 1893 | 1.31 | (1.02, 1.68) |
| No | -- | -- | -- | 7882 | REF | -- |
Models were also adjusted for year of survey administration and age of respondent
Boldface indicates statistical significance (p<0.05)
Analyses performed with small sub-population
Figure 1. Non-remitting Asthma Forest Plot Odds Ratios for SM/REM vs White Heterosexual Male Youths.
Forest Plot of Table IV Model I. Model is adjusted for year of survey administration, age, and region.
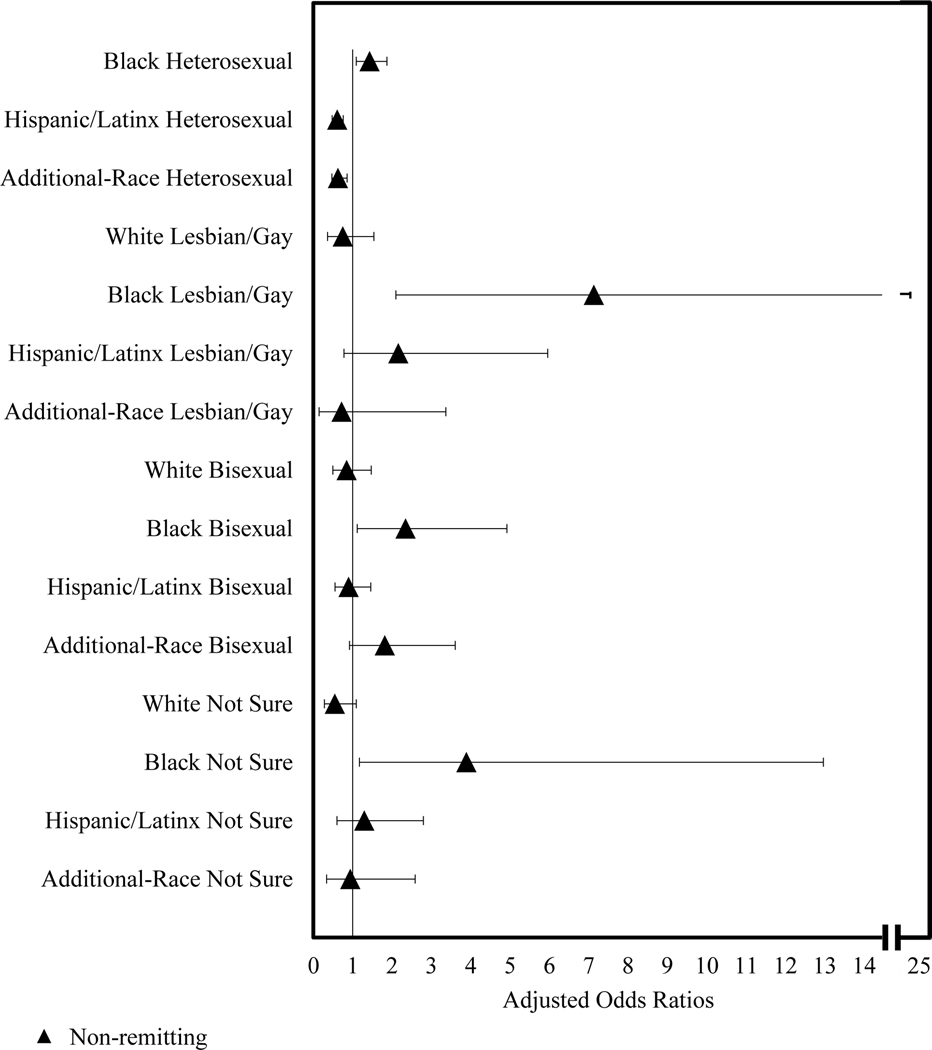
Among females and in models adjusted for demographics (Table V Model I; Figure 2), compared with unadjusted models, all four previous significant associations with non-remitting asthma remained—Black lesbian (AOR 7.13; 95% CI: 2.10–24.17), Black bisexual (AOR 2.35; 95% CI: 1.12–4.92), Hispanic/Latinx heterosexual (AOR 0.61; 95% CI: 0.48–0.76), and additional-race heterosexual (AOR 0.63; 95% CI: 0.47–0.86) females. A higher chance of non-remitting asthma among Black heterosexual (AOR 1.43; 95% CI: 1.09–1.87) and Black not sure females (AOR 3.89; 95% CI: 1.17–12.97) compared with White heterosexual females emerged.
Table V:
Stepwise Adjusted Odds Ratios for Non-remitting Asthma by Sexual Identity (SI) and Race/Ethnicity (RE) Intersections among Females, YRBS, 2009–2017.
| Model I: Demographics N = 11,466 | Model II: Model I + Selected Factors N = 9,206 | |||||
|---|---|---|---|---|---|---|
| n | AOR | 95%CI | n | AOR | 95%CI | |
| SI and RE Intersections | ||||||
| Heterosexual | ||||||
| White | 5035 | REF | -- | 5035 | REF | -- |
| Black | 1281 | 1.43 | (1.09,1.87) | 1281 | 1.31 | (0.99, 1.73) |
| Hispanic/Latinx | 1727 | 0.61 | (0.48,0.76) | 1727 | 0.57 | (0.45, 0.73) |
| Additional-Race | 1512 | 0.63 | (0.47,0.86) | 1512 | 0.63 | (0.45, 0.88) |
| Lesbian/Gay | ||||||
| White | 119 | 0.75 | (0.36,1.54) | 119 | 0.32 | (0.14, 0.72) |
| Black | 62 | 7.13 | (2.10,24.17) | 62 | 4.62 | (1.18, 18.08) |
| Hispanic/Latinx | 70 | 2.16 | (0.78,5.96) | 70 | 1.32 | (0.49, 3.51) |
| Additional-Race | 46 | 0.72 | (0.15,3.37) | 46 | 3.79 | (0.88, 16.34) |
| Bisexual | ||||||
| White | 575 | 0.85 | (0.50,1.47) | 575 | 0.55 | (0.28, 1.08) |
| Black | 142 | 2.35 | (1.12,4.92) | 142 | 2.02 | (0.86, 4.75) |
| Hispanic/Latinx | 276 | 0.90 | (0.55,1.46) | 276 | 0.66 | (0.39, 1.10) |
| Additional-Race | 219 | 1.82 | (0.92,3.61) | 219 | 1.70 | (0.71, 4.05) |
| Not Sure | ||||||
| White | 173 | 0.55 | (0.28,1.09) | 173 | 0.38 | (0.16, 0.91) |
| Black | 59 | 3.89 | (1.17,12.97) | 59 | 3.52 | (0.84, 14.71) |
| Hispanic/Latinx | 88 | 1.30 | (0.60,2.80) | 88 | 1.05 | (0.46, 2.41) |
| Additional-Race | 82 | 0.94 | (0.34,2.59) | 82 | 1.53 | (0.57, 4.13) |
| Selected Demographics* | ||||||
| Region | ||||||
| Northeast | 4952 | REF | -- | 4952 | REF | -- |
| Midwest | 1700 | 0.94 | (0.78,1.13) | 1700 | 0.97 | (0.78, 1.20) |
| South | 2552 | 0.71 | (0.56,0.89) | 2552 | 0.73 | (0.55, 0.95) |
| West | 2262 | 0.95 | (0.75,1.20) | 2262 | 0.81 | (0.62, 1.07) |
| Selected Variables | ||||||
| Bullied | ||||||
| Yes | -- | -- | -- | 2754 | 1.49 | (1.16, 1.92) |
| No | -- | -- | -- | 8494 | REF | -- |
| Forced Sex | ||||||
| Yes | -- | -- | -- | 1244 | 1.53 | (1.10, 2.13) |
| No | -- | -- | -- | 8149 | REF | -- |
Models were also adjusted for year of survey administration and age of respondent
Boldface indicates statistical significance (p<0.05)
Figure 2. Non-remitting Asthma Forest Plot Odds Ratios for SM/REM vs White Heterosexual Female Youths.
Forest Plot of Table V Model I. Model is adjusted for year of survey administration, age, and region.
Adjusting for Correlates
Among males, being cyberbullied (AOR 1.39; 95% CI: 0.96–2.02) and having a BMIp>95 (AOR 1.31; 95% CI: 1.02–1.68) were the most robustly associated with non-remitting asthma (Table IV). Their inclusion in models reduced odds of non-remitting asthma for 9 subpopulations compared with models only adjusted for demographics. Most significant disparities in non-remitting asthma remained in the fully adjusted model; however, additional-race gay males (AOR: 3.06; 95% CI: 1.00–9.39; p=0.0504) lost significance.
Among females, being bullied (AOR 1.49; 95% CI: 1.16–1.92) and experiencing forced sex (AOR 1.53; 95% CI: 1.10–2.13) were the most robustly associated with non-remitting asthma (Table V). Their inclusion in models reduced the odds of non-remitting asthma for 12 subpopulations. Only Black lesbian females maintained significantly greater odds of asthma non-remission (AOR 4.62; 95% CI: 1.18–18.08). Four subpopulations (Hispanic/Latinx heterosexual, additional-race heterosexual, White lesbian, and White not sure) were significantly less likely than White heterosexual females to experience non-remitting asthma.
DISCUSSION
Consistent with prior work, we report differences in asthma remission by sex, with males having a higher prevalence than females.18 In partial agreement with the previous study on differences by race/ethnicity,23 we found significantly elevated rates of non-remitting asthma among Black males and females, as well as among additional-race males. Hispanic/Latinx females, however, experienced significantly lower rates of non-remitting asthma than White females. By sexual identity, only gay males were significantly more likely than their sex-matched heterosexual peers to have non-remitting asthma.
Furthermore, using an applied intersectional lens, we report disparities in asthma remission among SM/REM youth. Understanding that each subpopulation experiences distinct overlapping stigmatization helps to explain the varying magnitudes of disparities we report.24,25,30 Overall, 8 SM/REM minority subpopulations experienced significantly increased odds of non-remitting asthma compared with White heterosexual, sex-matched peers. There were no significant disparities among females by sexual identity alone; however, among SM/REM youth, significant disparities were found among Black heterosexual, lesbian, bisexual, and not sure females compared with White heterosexual females. Moreover, black females with a minority sexual identity, particularly lesbian and not sure identities, had higher odds of non-remitting asthma than did Black heterosexual females. These findings highlight the value of intersectionality-informed analyses, as worsened disparities among sexual minority females of color were not seen when examining only sexual identity, indicating that interlocking oppressions experienced by these sub-populations may be driving their distinct asthma outcomes.
For males, being cyberbullied or having a BMIp>95 tended to attenuate odds of non-remitting asthma among sub-populations, with additional-race gay males losing statistically significant increased odds of non-remitting asthma in fully adjusted models. The evidence suggests victimization and traditional risk factors like BMI may partially moderate disparities in asthma remission among marginalized populations. As described above, victimization may increase levels of minority stress among marginalized populations, initiating physiological (e.g., immune system dysregulation) and stress-linked coping behaviors (e.g., disordered eating that increases BMIp) that increase the risk for non-remitting asthma.24,30,31 Addressing the levels of stigmatization and minority stress that lead to such correlates could prove efficacious in reducing asthma remission disparities among male youth. Based on significantly elevated disparities, Black heterosexual; additional-race heterosexual; White gay; and additional-race gay male youth should receive special consideration in future asthma remission research and intervention.
For females, including being bullied and experiencing forced sex in fully adjusted models reduced the odds of non-remitting asthma for all subpopulations except additional-race heterosexual, lesbian, and not sure females. These variables eliminated the significantly higher odds of non-remitting asthma among Black heterosexual, bisexual, and not sure females. Of considerable note is the loss of statistical significance for increased odds of non-remitting asthma among Black bisexual females in the model including forced sex. Nationally, experiencing forced sex is most common among bisexual women and women of color.39 While the reasons for these higher levels of sexual victimization remain poorly studied, scholars have posited that such violence is linked directly to stereotypes and stigmatization of women of color and bisexual women (as well as among bisexual women of color).40 The evidence, then, in line with MST suggests that reducing occurrences of victimization and stigmatization may reduce risk for non-remitting asthma among marginalized female youth. Research into asthma remission among Black female youth, particularly those with a sexual minority identity, should be prioritized.
Interestingly, smoking status did not meet the significance cut-off for either fully-adjusted model. The lack of correlation may be explained by youth having not smoked long enough to see the observed patterns common in adults of smoking as a risk factor for non-remitting asthma.18 Having a BMIp>95%, however, was significantly associated with non-remission for males, indicating its potential role in pediatric non-remitting asthma.
Regarding the formulation of the asthma remission measure, we cannot confirm that a greater than 6 month period of symptom remission without medication occurred due to the wording of the questions in the YRBS. Thus, some respondents considered in our analyses to have entered asthma remission may not meet the clinical definition for this diagnosis. The term “asthma remission” has been used by many previous cross-sectional studies without a defined period of symptom remission.18 Additionally, the clinical definition of asthma remission is imprecise, with periods of no symptoms ranging from 6 months to 5 years to be considered in remission.17,18 The term “current asthma” has been used previously in epidemiological literature; however, current asthma studies use a different methodological approach.41–43 Studies using the term current asthma include respondents who have never had lifetime asthma. Thus, the term current asthma is in response to among the general population, how many youths have had asthma and still do. These studies estimate between 10–15% of youth have current asthma. Our study, however, along with other cross-sectional studies of asthma remission explore the absence of symptoms among lifetime asthmatics.18 Thus, the term asthma remission is in response to among people who have had asthma, how many of them no longer have asthma. The literature have estimated between 33% to 53% of youth asthmatics under 18 years have entered asthma remission, in line with our present estimate of 33.3%. Additionally, for adults with non-remitting asthma that began before age 16 years, the mean age of onset is at 7 years which is well below the age of the present analytic sample.44
Informing Clinical Practice and Asthma Management Guidelines
Asthma, unlike chronic conditions such as diabetes or cardiovascular disease, is not responsive to primary prevention or early intervention.45 However, similar to other chronic conditions, there are notable population-level health disparities impacting SM/REM populations.46 Despite the well-documented disparities, clinical guidelines of chronic conditions often do not include their mention.47–50 Included are the most referenced clinical guidelines for asthma—the Global Initiative for Asthma (GINA) and the Expert Panel Report (EPR) 3 Guidelines from the National Heart, Lung, and Blood Institute (NHLBI) published in 2007—which do not include considerations of the health inequalities among sexual or racial/ethnic minority populations.49,50 These considerations are similarly omitted from the recent focused updates to the EPR-3.51,52 Accordingly, we recommend GINA and future EPRs to include a section in their upcoming guidelines for the established disparities in asthma outcomes by marginalized status. The effects of structural issues such as stigmatization, discrimination, and oppression of marginalized persons on health disparities must be conceptualized by providers to begin combating their effects. To realize this goal, we recommend clinical asthma guidelines to include further research on the relation between social determinants of health, structural-level factors, and health disparities.53 The guidelines should specifically encourage health systems and providers to implement the National Standard for Culturally and Linguistically Appropriate Services (CLAS) in Health and Health Care from the U.S. Department of Health and Human Services.54 GINA and the EPR should consider adding the stigmatization of SM/REM populations to be assessed and addressed along with environmental factors, education, and comorbidities in the management of asthma.49,51 Further, culturally-tailored asthma practices from the peer-reviewed literature predominantly focus on race/ethnicity.55–62 We posit the need for the development of culturally-tailored asthma interventions for SM/REM youth; hence, these guidelines must be expanded to also include sexual identity and the impacts of multiple-marginalization.
Along with additional considerations for clinical asthma guidelines, we encourage providers, researchers, and health care systems to adopt a systematic approach for identifying and ameliorating disparities on the basis of marginalization.24,25,53 Such approaches include the examination of culturally-tailored interventions designed to impact health systems and patient- provider interaction, as well as ways to increase provider conceptualization of the structural issues at hand.
Limitations
The present study is not without limitations. All data were self-reported, and secondary data analyses of a cross-sectional dataset do not allow for any commentary on causality or control over the questions asked. Moreover, the “not sure” response to sexual identity could have meant students were unsure of the question—not necessarily that they were unsure of their sexual identity. The YRBS only includes adolescents who attend high school; results may not be representative of students who are home-schooled or do not attend school. The use of clinician-diagnosed asthma could have led to an underestimation of asthma among marginalized youth populations, as engaging with physicians to receive a diagnosis is less likely among these groups.63 The asthma remission variable had to be constructed using self-report measures with no specific time period mentioned, which could have introduced symptom perception bias.18 As most remission occurs between the ages of 14 and 21 years of ages and our sample falls toward the early part of this range, there could be an underestimation of asthma remission.19 Moreover, due to wording of the asthma questions, we cannot define the length of symptom remission or medication use. Thus, some respondents considered to have enter remission in the present study may not meet the clinical definition.
Adjusting for all known traditional correlates was also not possible.18 The small sample size of many sub-populations likely contributed to their not reaching significance. Specifically, the sample size for Black not sure males was fewer than 30 individuals and should be interpreted with caution.64 Finally, we used SM/REM youth sub-populations as proxies for intersectional oppression. Despite these limitations, our study is the first to explore and introduce inequalities in asthma remission by sexual identity and at the intersections of sexual identity and race/ethnicity. Our study is also the first to frame remission based on MST and intersectionality frameworks, which are critical to population health studies. Finally, we identified potential factors for non-remitting asthma among male and female SM/REM youth and, for the first time, suggested the role that victimization may play.
In total, asthma remission disparities exist by sexual identity, race/ethnicity, or both with those of marginalized status generally being more likely to experience non-remitting asthma. Viewed through the lens of intersectionality and MST, our findings provide empirical support that victimization may be associated with asthma non-remission. The construction of an asthma remission variable allowed for an innovative and comprehensive examination of the disparity subpopulations and correlates of non-remitting asthma among U.S. youth. Correlates such as being cyberbullied or BMIp>95% for males and being bullied or forced to engage in sex for females may partly explain the dipartites in asthma remission observed in our study. The present study, along with previously published literature on asthma prevalence and remission disparities experienced by marginalized persons, should be used to set a research agenda designed to improve asthma management.1,7–16,18
HIGHLIGHTS BOX.
- What is already known about this topic?
- 1.1. There are reported disparities in asthma remission by sex and race/ethnicity. Asthma remission negatively associates with asthma severity, smoking, and increased weight. Minority stress theory and intersectionality are imperative frameworks to study population health.
- What does this article add to our knowledge?
- 2.1 Sexual minority and/or racial/ethnic minority youth tend to be at higher risk for non-remitting asthma. Traditional risk factors and victimization are associated with increased odds of non-remitting asthma among these populations.
- How does this study impact current management guidelines
- 3.1. Asthma management guidelines should include population-level disparities on the basis of marginalization. Clinicians should stay up-to-date on cultural responsiveness training and implement the National Standard for Culturally and Linguistically Appropriate Services (CLAS) in practice.
Acknowledgements
We thank Blair Turner for her contributions that assisted in the analyses of this manuscript.
Funding Acknowledgement
This research was funded under R01 AA024409 (PI: Phillips) by the National Institute on Alcohol Abuse and Alcoholism, as well as under K12 HL143959 (PI: Beach) by the National Heart, Lung, and Blood Institute and K12 HS026385 (PI: Kan) by the Agency for Healthcare Research and Quality.
Abbreviations:
- (CDC)
Centers for Disease Control and Prevention
- (SM/REM)
Sexual Minority and/or Racial/Ethnic Minority
- (YRBS)
Youth Risk Behavior Survey
- (BMIp)
Body Mass Index Percentile
- (GINA)
Global Initiative for Asthma
- (NHLBI)
National Heart, Lung, and Blood Institute
- (EPR)
Expert Panel Report
Footnotes
Disclaimer
The funding source had no role in the study design; collection, analysis, or interpretation of data; the writing of the report; nor in the decision to submit the article. The content solely represents the views of the authors and not necessarily the National Institutes of Health.
Conflict of Interest Disclosures
We declare no competing interests.
Human Participant Protection
All current study activities were classified as non–human participant research by the institutional review board at Northwestern University.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Most Recent National Asthma Data. Centers for Disease Control and Prevention; 2019. Available at: https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm.Accessed May 22, 2020. [Google Scholar]
- 2.Asthma. World Health Organization; 2017. Available at: https://www.who.int/en/news-room/fact-sheets/detail/asthma.Accessed May 22, 2020. [Google Scholar]
- 3.The Impact of Asthma. American Lung Association; 2018. Available at: https://www.lung.org/lung-health-and-diseases/lung-disease-lookup/asthma/learn-about-asthma/impact-of-asthma.html.Accessed June 4, 2019. [Google Scholar]
- 4.un HD, Knoebel E, Fenta Y, Gabriel SE, Leibson CL, Loftus EV Jr., et al. Asthma and proinflammatory conditions: a population-based retrospective matched cohort study. Mayo Clin Proc 2012;87:953–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Global Asthma Report. Auckland, New Zealand: Global Asthma Network; 2018. Available at: http://www.globalasthmareport.org/Global%20Asthma%20Report%202018.pdf.Accessed May 22, 2020. [Google Scholar]
- 6.Asthma Disparities. President’s Task Force on Environmental Health Risks and Safety Risks to Children; 2012. Available at: https://ptfceh.niehs.nih.gov/activities/asthma/index.htm.Accessed May 22, 2020. [Google Scholar]
- 7.Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, et al. Youth Risk Behavior Surveillance - United States, 2017. Morb Mortal Wkly Rep Surveill Summ 2018;67:1–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hill TD, Graham LM, Divgi V. Racial Disparities in Pediatric Asthma: A Review of the Literature. Curr Allergy Asthma Rep 2011;11:85–90. [DOI] [PubMed] [Google Scholar]
- 9.Cochran SD, Mays VM. Physical health complaints among lesbians, gay men, and bisexual and homosexually experienced heterosexual individuals: Results from the California quality of life survey. Am J Public Health 2007;97:2048–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Conron KJ, Mimiaga MJ, Landers SJ. A Population-Based Study of Sexual Orientation Identity and Gender Differences in Adult Health. Am J Public Health 2010;100:1953–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fredriksen-Goldsen KI, Kim HJ, Barkan SE. Disability among lesbian, gay, and bisexual adults: disparities in prevalence and risk. Am J Public Health 2012;102:e16–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Asthma Prevalence in California: A Surveillance Report. Richmond, CA: California Department of Public Health; 2017. Available at: https://www.cdph.ca.gov/Programs/CCDPHP/DEODC/EHIB/CPE/CDPH%20Document%20Library/Asthma_Surveillance_in_CA_Report_2017.pdf.Accessed May 22, 2020. [Google Scholar]
- 13.Heck JE, Jacobson JS. Asthma diagnosis among individuals in same-sex relationships. J Asthma 2006;43:579–84. [DOI] [PubMed] [Google Scholar]
- 14.Landers SJ, Mimiaga MJ, Conron KJ. Sexual Orientation Differences in Asthma Correlates in a Population-Based Sample of Adults. Am J Public Health 2011;101:2238–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meads C, Martin A, Grierson J, Varney J. Systematic review and meta-analysis of diabetes mellitus, cardiovascular and respiratory condition epidemiology in sexual minority women. BMJ Open 2018;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Curry CW, Felt D, Beach LB, Phillips GL II. Lifetime Asthma Prevalence and Correlates among U.S. Youth by Sexual Identity and Race/Ethnicity, 2009–2017. Am J Public Health 2020:e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carpaij OA, Nieuwenhuis MAE, Koppelman GH, van den Berge M, Postma DS, Vonk JM. Childhood factors associated with complete and clinical asthma remission at 25 and 49 years. Eur Respir J 2017;49. [DOI] [PubMed] [Google Scholar]
- 18.Carpaij OA, Burgess JK, Kerstjens HAM, Nawijn MC, van den Berge M. A review on the pathophysiology of asthma remission. Pharmacol Ther 2019;201:8–24. [DOI] [PubMed] [Google Scholar]
- 19.Trivedi M, Denton E. Asthma in Children and Adults-What Are the Differences and What Can They Tell us About Asthma? Front Pediatr 2019;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beach LB, Turner B, Felt D, Marro R, Phillips GL 2nd. Risk Factors for Diabetes are Higher among Non-Heterosexual US High School Students. Pediatr Diabetes 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Watson RJ, Lewis NM, Fish JN, Goodenow C. Sexual minority youth continue to smoke cigarettes earlier and more often than heterosexuals: Findings from population-based data. Drug Alcohol Depend 2018;184:64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ortega AN, Calderon JG. Pediatric asthma among minority populations. Curr Opin Pediatr 2000;12:579–83. [DOI] [PubMed] [Google Scholar]
- 23.Javed A, Yoo KH, Agarwal K, Jacobson RM, Li XJ, Juhn YJ. Characteristics of Children with Asthma Who Achieved Remission of Asthma. J Asthma 2013;50:472–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychol Bull 2003;129:674–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crenshaw K. Mapping the Margins - Intersectionality, Identity Politics, and Violence against Women of Color. Stanford Law Review 1993;43:1241–99. [Google Scholar]
- 26.Collins PH. Gender, Black Feminism, and Black Political Economy. Ann Am Acad Pol Soc Sci 2000;568:41–53. [Google Scholar]
- 27.Yonas MA, Lange NE, Celedon JC. Psychosocial stress and asthma morbidity. Curr Opin Allergy Clin Immunol 2012;12:202–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Caponnetto P, Auditore R, Russo C, Alamo A, Campagna D, Demma S, et al. “Dangerous relationships”: asthma and substance abuse. J Addict Dis 2013;32:158–67. [DOI] [PubMed] [Google Scholar]
- 29.Calzo JP, Blashill AJ, Brown TA, Argenal RL. Eating Disorders and Disordered Weight and Shape Control Behaviors in Sexual Minority Populations. Curr Psychiatry Rep 2017;19:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lick DJ, Durso LE, Johnson KL. Minority Stress and Physical Health Among Sexual Minorities. Perspect Psychol Sci 2013;8:521–48. [DOI] [PubMed] [Google Scholar]
- 31.Denton FN. Minority Stress And Physical Health In Lesbians, Gays, And Bisexuals: The Mediating Role Of Coping Self-Efficacy. Theses and Dissertations-- Educational, School, and Counseling Psychology 2012. [Google Scholar]
- 32.Bowleg L. The problem with the phrase women and minorities: intersectionality-an important theoretical framework for public health. Am J Public Health 2012;102:1267–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med 2014;110:10–7. [DOI] [PubMed] [Google Scholar]
- 34.Lowry R, Johns MM, Robin LE, Kann LK. Social Stress and Substance Use Disparities by Sexual Orientation Among High School Students. Am J Prev Med 2017;53:547–58. [DOI] [PubMed] [Google Scholar]
- 35.Centers for Disease C, Prevention, Brener ND, Kann L, Shanklin S, Kinchen S, et al. Methodology of the Youth Risk Behavior Surveillance System−−2013. MMWR Recomm Rep 2013;62:1–20. [PubMed] [Google Scholar]
- 36.Reisner SL, Greytak EA, Parsons JT, Ybarra ML. Gender Minority Social Stress in Adolescence: Disparities in Adolescent Bullying and Substance Use by Gender Identity. J Sex Res 2015;52:243–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Friedman MS, Marshal MP, Guadamuz TE, Wei CY, Wong CF, Saewyc EM, et al. A Meta-Analysis of Disparities in Childhood Sexual Abuse, Parental Physical Abuse, and Peer Victimization Among Sexual Minority and Sexual Nonminority Individuals. American Journal of Public Health 2011;101:1481–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Johns MM, Lowry R, Rasberry CN, Dunville R, Robin L, Pampati S, et al. Violence Victimization, Substance Use, and Suicide Risk Among Sexual Minority High School Students - United States, 2015–2017. MMWR 2018;67:1211–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Walters ML, Chen J, Breiding MJ. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Findings on Victimization by Sexual Orientation. Atlanta, GA, 2013. [Google Scholar]
- 40.Johnson NL, Grove M. Why Us? Toward an Understanding of Bisexual Women’s Vulnerability for and Negative Consequences of Sexual Violence. J Bisex 2017;17:435–50. [Google Scholar]
- 41.Park S, Blanck HM, Sherry B, Jones SE, Pan L . Regular-Soda Intake Independent of Weight Status Is Associated with Asthma among US High School Students. J Acad Nutrand Diet 2013;113:106–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Han Y-Y, Forno E, Celedón JC. Health risk behaviors, violence exposure, and current asthma among adolescents in the United States. Pediatr Pulmonol 2019;54:237–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bakour C, O’Rourke K, Schwartz S, Wang W, Sappenfield W, Couluris M. Sleep duration, obesity, and asthma, in Florida adolescents: analysis of data from the Florida Youth Risk Behavior Survey (2009–2013). Sleep Breath 2017;21:1039–45. [DOI] [PubMed] [Google Scholar]
- 44.Mirabelli MC, Beavers SF, Chatterjee AB, Moorman JE. Age at asthma onset and subsequent asthma outcomes among adults with active asthma. Respiratory Medicine 2013;107:1829–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Savenije OEM, Kerkhof M, Koppelman GH, Postma DS. Predicting who will have asthma at school age among preschool children. J Allergy Clin Immunol 2012;130:325–31. [DOI] [PubMed] [Google Scholar]
- 46.Dyar C, Taggart TC, Rodriguez-Seijas C, Thompson RG, Elliott JC, Hasin DS, et al. Physical Health Disparities Across Dimensions of Sexual Orientation, Race/Ethnicity, and Sex: Evidence for Increased Risk Among Bisexual Adults. Arch Sex Behav 2019;48:225–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.American Diabetes Association. Standards of Medical Care in Diabetes—2020. Diabetes Care 2020;43:S1–S212. [DOI] [PubMed] [Google Scholar]
- 48.Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019;140:e596–e646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Global Strategy for Asthma Management and Prevention, 2020. Global Initiative for Asthma; 2020. Available at: www.ginasthma.org.Accessed June 15, 2020. [Google Scholar]
- 50.Guidelines for the Diagnosis and Management of Asthma (EPR-3). National Asthma Education and Prevention Program of the National Heart, Lung, and Blood Institute; 2007. Available at: https://www.nhlbi.nih.gov/health-topics/guidelines-for-diagnosis-management-of-asthma.Accessed June 15, 2020. [Google Scholar]
- 51.Update on Selected Topics in Asthma Management: A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group, Draft for Public Comment. National Asthma Education and Prevention Program of the National Heart, Lung, and Blood Institute; 2019. Available at: https://www.epr4workgroup.org/Asthma2020Guidelines/Shared%20Documents/Asthma-Guidelines-Report.pdf.Accessed June 15, 2020. [Google Scholar]
- 52.Expert Panel Working Group of the National Heart L, Blood Institute a, coordinated National Asthma E, Prevention Program Coordinating C, Cloutier MM, Baptist AP, et al. 2020 Focused Updates to the Asthma Management Guidelines: A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group. J Allergy Clin Immunol 2020;146:1217–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Metzl JM, Hansen H. Structural competency: theorizing a new medical engagement with stigma and inequality. Soc Sci Med 2014;103:126–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.National CLAS Standards. U.S. Department of Health and Human Services; 2018. Available at: https://thinkculturalhealth.hhs.gov/clas.Accessed June 16, 2020. [Google Scholar]
- 55.Sutherland ER, Busse WW, National Heart L, Blood Institute’s A. Designing clinical trials to address the needs of childhood and adult asthma: the National Heart, Lung, and Blood Institute’s AsthmaNet. J Allergy Clin Immunol 2014;133:34–8.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Press VG, Pappalardo AA, Conwell WD, Pincavage AT, Prochaska MH, Arora VM. Interventions to improve outcomes for minority adults with asthma: a systematic review. J Gen Intern Med 2012;27:1001–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Press VG, Hoch H. The Search for Culturally Tailored Inhaled Corticosteroid Adherence Interventions Continues: A Dearth of Effective Strategies for African Americans with Asthma. J Allergy Clin Immunol Pract 2019;7:1194–6. [DOI] [PubMed] [Google Scholar]
- 58.Asthma Resources for Health Professionals and School. Centers for Disease Control and Prevention; 2018. Available at: https://www.cdc.gov/asthma/healthcare.html.Accessed May 28, 2020. [Google Scholar]
- 59.Anise A, Hasnain-Wynia R. Patient-centered outcomes research to improve asthma outcomes. J Allergy Clin Immunol 2016;138:1503–10. [DOI] [PubMed] [Google Scholar]
- 60.Ahmed S, Steed L, Harris K, Taylor SJC, Pinnock H. Interventions to enhance the adoption of asthma self-management behaviour in the South Asian and African American population: a systematic review. NPJ Prim Care Respir Med 2018;28:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Federico MJ, McFarlane AE 2nd, Szefler SJ, Abrams EM. The Impact of Social Determinants of Health on Children with Asthma. J Allergy Clin Immunol Pract 2020;8:1808–14. [DOI] [PubMed] [Google Scholar]
- 62.Holsey CN, Collins P, Zahran H. Disparities in Asthma Care, Management, and Education Among Children With Asthma. Clinical pulmonary medicine 2013;20:172–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Racial and Ethnic Disparities in Health Care, Updated 2010. Philadelphia, PA: American College of Physicians; 2010. Available at: https://www.acponline.org/acp_policy/policies/racial_ethnic_disparities_2010.pdf.Accessed May 22, 2020. [Google Scholar]
- 64.How to Analyze YRBS Sexual Minority Data. Centers for Disease Control and Prevention; 2018. Available at: https://www.cdc.gov/healthyyouth/data/yrbs/pdf/2017/2017_analyze_sexual_minority_data.pdf.Accessed May 22, 2020. [Google Scholar]
- 65.2017 YRBS Data User’s Guide. Centers for Disease Control and Prevention; 2018. Available at: https://www.cdc.gov/healthyyouth/data/yrbs/pdf/2017/2017_YRBS_Data_Users_Guide.pdf.Accessed May 22, 2020. [Google Scholar]