ABSTRACT
Use of systems science can improve the dissemination and implementation (D&I) process. However, little is known about use of systems science in nutrition D&I research. The purpose of this article is to synthesize the ways in which systems science methodology is applied in nutrition D&I research. Scoping review methodology involved searching 6 academic databases for full-text, peer-reviewed, English articles published between 1970 and 2020 that employed systems science within nutrition D&I research. Data extraction included intervention type, population, study aim, methods, theoretical approach, outcomes, and results. Descriptive statistics and qualitative thematic analysis followed. Thirty-four retained articles qualitatively identified benefits (successful planning and organization of complex interventions) and challenges (limited resources, trainings, and lack of knowledge) to utilizing systems science in nutrition D&I research. Future research should work toward building knowledge capacity among nutrition practitioners by increasing available trainings and resources to enhance the utilization of systems science in nutrition D&I research.
Keywords: systems thinking, implementation science, nutrition, health behaviors, dissemination, science
Systems science can enhance development of complex nutrition interventions. This scoping review summarizes current use of systems science in nutrition behaviors and outcomes dissemination and implementation research and suggests that capacity-building trainings should be developed in this area.
Introduction
Dietary patterns describe the frequency, proportions, variety, and combination of different foods, drinks, and nutrients in the human diet (1). The current dietary patterns in the United States are associated with 4 of the 10 leading causes of death: heart diseases, some types of cancer, stroke, and type 2 diabetes (2). For example, many American do not consume enough fruits and vegetables (3) and overconsume added sugars, saturated fats, and salt (4), which can increase the risk of obesity and carries with it an increased risk of these chronic diseases (4–7). Luckily, nutrition interventions including education, programs, and policies can lead to positive changes in an individual's dietary behaviors, which can lower the risk of chronic diseases and enhance health (2).
Nutrition interventions describe any combination of strategies designed to motivate and facilitate the adoption of nutrition-related behaviors that encourage health and well-being (2). Current research shows that nutrition interventions such as i-COOK 4-H (8, 9) and Homestyles (10–13), which address childhood nutrition, the GetFRUVED (14, 15) intervention that encourages college student health behaviors (16–27), a mental health recovery and nutrition program, M4R2 (28, 29), and a culinary medicine educational program to improve health professional nutrition-related knowledge (30–32), can positively support healthy lifestyle changes. Despite the noted positive influences on health and well-being, current reviews evaluating the effectiveness of nutrition interventions on health behaviors have identified areas for improvement in implementation. There is a need to address the sustainability (33), replicability and adaptability (34) of interventions, methodological issues, lack of large-group interventions (35–37), and unclear identification or integration of the multiple interrelated factors that impact nutrition and dietary patterns (34, 38, 39).
Dissemination and implementation (D&I) research seeks to understand and overcome barriers to adoption, sustainability, and methodological issues of interventions that address complex problems (40). Health issues are increasingly recognized as complex problems embedded within our society, with multiple interacting components and undefined behaviors (40, 41). For example, implementation of a nutrition intervention to promote healthy dietary patterns in adults without consideration of the mix of factors that influence food consumption, including biological factors, cultural and social preferences, physical health, food access, and emotional and psychological well-being, can have limited impact. Solutions to complex problems often require intervening at many different levels, using multiple strategies, and engaging numerous actors and organizations (40), which can require new methodological approaches that address complexity with the implementation of nutrition interventions.
Systems thinking is a perspective that aims to interpret how things are connected to each other and within a larger system (42). A system is a set of elements or factors that are organized and interconnected and ultimately produce complex and dynamic behaviors that can evolve over time (43). Dynamic, complex, and interrelated are key terms among these definitions that inform many components of systems thinking and systems science methods. Methods of systems science, including systems dynamic modeling (SDM), systems network analysis (SNA), agent-based modeling (ABM), soft-systems approaches, cognitive and concept mapping, and other simulations have been developed to understand and identify systems' structure and behavior over time (44). Systems science methods are increasingly used to explain or predict real-world outcomes of large-scale interventions (42). In recent years, public health practitioners have been applying systems science and thinking to identify the factors that influence intervention efficacy and real-world application (45). Further, D&I research utilizes systems science to understand complex factors influencing successful interventions and to identify challenges (44). Current research for systems science and D&I research predominantly focuses on patient safety and the medical field (46–54), tobacco research (55, 56), obesity with a focus on planning and quantifying interrelated factors (57–60), and policy change (61–65). Although current evidence provides positive insights from using systems science in D&I health research, little is known about the utilization within nutrition. However, interest in the use of systems science in nutrition implementation research is increasingly recognized. For example, recent calls have been made to organize knowledge and interest in implementation science in nutrition (66–68) including the development of the Society for Implementation Science in Nutrition (68), yet there is a lack of reviews of the current state of research. Therefore, more research is needed to inform nutrition practitioners in order to lead to a greater capacity for factors that influence complex issues and interventions to enhance the health and well-being of communities (1, 40). Thus, the purpose of this article is to synthesize the ways in which systems science methodology is applied in nutrition D&I research.
Methods
Scoping reviews formulate research questions of interest, based on what is known or not known from the literature (69). A scoping review is particularly useful when a topic has not yet been extensively reviewed or is a complex issue (70), making it an ideal approach to map the application of systems science in nutrition D&I research. The methodology of this scoping review followed the guided framework developed by Levac and colleagues (71) and adapted by Arksey and O'Malley (72), which identifies 6 key guidelines including: identifying the research question, identifying relevant studies, study selection, charting the data, collating, summarizing, and reporting results and consultation. Step 6 is optional and was not applied in the current review.
Step 1: identify the research questions
How are systems science methods and systems thinking applied to nutrition D&I research?
What are the benefits and challenges of systems science and systems thinking within nutrition D&I research?
Step 2: identify relevant literature
The search strategy was approved by 2 authors (AEW and MDO) and involved a search of peer-reviewed English literature that was completed in July 2020 within 6 primary literature databases: PubMed, CINAHL, Web of Science, ProQuest, Scopus, and Agricola. Medical subject headings (MeSH) and keywords that were mapped to subject headings were used to define the search's scope to best capture relevant articles. Because the language of D&I research and systems science is complex, keywords consisted of relevant concepts related to systems science or systems thinking, diffusion of innovation or dissemination, implementation or interventions, nutrition behaviors and outcomes, and food. A full electronic search strategy is presented in Supplemental Table 1 for replicability.
Step 3: select the literature
Identified articles were screened for inclusion by 1 author (AEW). Inclusion criteria included full-text, peer-reviewed, English articles published between 1970 and 2020 describing studies that employed systems science within nutrition D&I research. Preliminary exclusion criteria sought to identify articles that were non-English articles, articles without an abstract or articles with only an abstract, and articles that did not address nutrition and nutrition-related D&I using systems science in some capacity through an intensive initial analysis of titles, keywords, and abstracts. Secondary exclusion primarily focused on whether an article did or did not mention systems science or thinking, systems analysis (i.e., network analysis, ABM, SDM, or conceptual modeling), or systems vocabulary (i.e., complexity, interrelated, and complex relations) within nutrition D&I research. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart guides were used to display the exclusion methodology and approved by a secondary reviewer (MDO) to ensure the search strategy was implemented with fidelity.
Step 4: chart the data
The primary researcher (AEW) extracted the data using a structured table adapted from Armstrong and colleagues (69) in accordance with the research questions identified in step 1. Study descriptions of interest included: title, authors, year of publication, study location, study population, organization of articles, systems methods and modeling or systems framing and language, aims, methodologies, context, theories, models or framework utilized, intervention type (i.e., planning, evaluation, implementation, dissemination), outcomes, and results to inform qualitative analysis. The final chart and study characteristics were reviewed collaboratively by the primary researcher (AEW) and a secondary researcher (RAW). Any discrepancies between the 2 researchers were identified and adaptations were mutually agreed.
Step 5: collate, summarize, and report results
Descriptive statistics including frequency counts of study description categories including: systems science methods, tools and ideologies, intervention types (i.e., planning, evaluation, implementation, dissemination), and explicitly mentioned theory, models, and frameworks used in the included articles’ study designs were calculated using JMP Pro 14 (SAS Institute Inc). Qualitative data analysis, which is used to examine themes or patterns to organize, describe, and interpret a dataset (73), was conducted to identify and interpret themes from the study description categories, including articles’ aims, methods, outcomes, and results, using NVivo Pro 12 (QSR International). The benefits and challenges were assessed by analyzing specifically mentioned benefits and challenges by the authors of the included articles and independently identified by researchers. The qualitative data analysis was conducted by 2 trained researchers (AEW and RAW), one of whom generated initial codes that informed a coding dictionary and then developed themes to generate summative content. Then independent researchers discussed the coding dictionary to identify discrepancies and collectively agree upon themes.
Results
Publication and article characteristics
A total of 1854 articles were retrieved, of which 34 met inclusion criteria. Figure 1 shows the PRISMA flow diagram (74) of included and excluded studies. Most of the included articles were published in 2015 (20%) and 2018 (20%). The data sets described in the 34 articles employed 7 different research designs, in which reviews, including systematic, literature, or scoping reviews (37%), and case study analyses (20%) were more prominent. Most studies conducted research in locations within the United States (55.9%) and 44.1% of research was conducted within a global lens (i.e., multiple locations at once including in Africa, Europe, the United Kingdom, Australia, Canada, and low- and middle-income countries).
FIGURE 1.
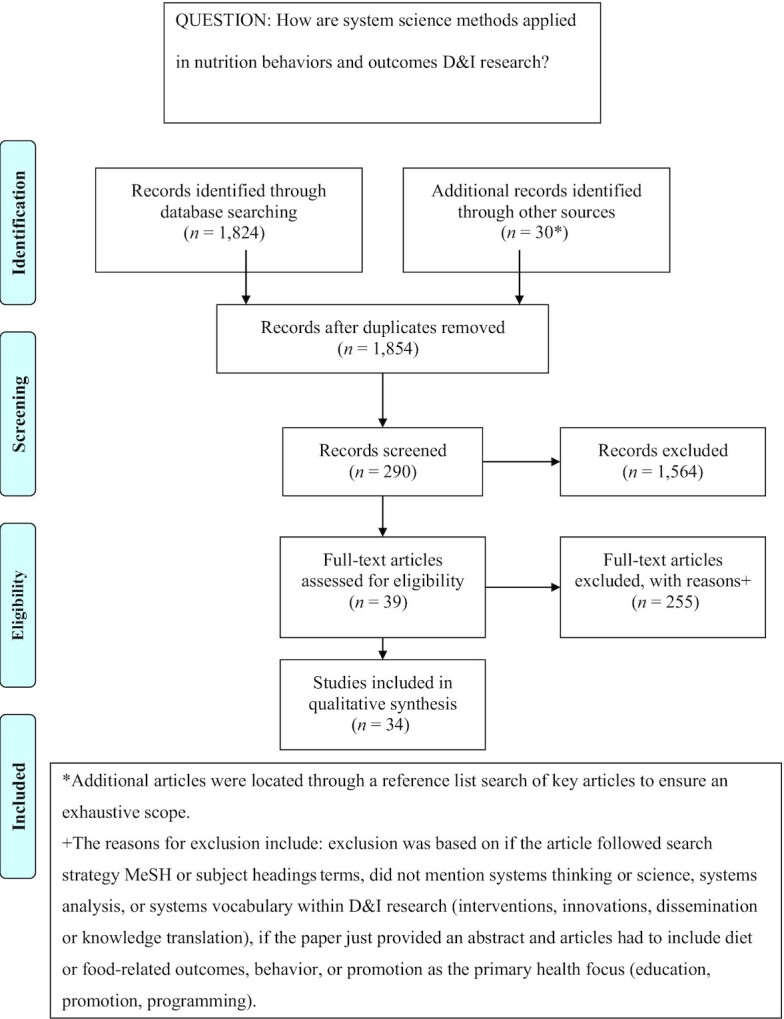
Flow diagram of the article screening process. D&I, dissemination and implementation.
Articles were grouped into 2 categories based on their utilization of systems science. Systems modeling (44.1%) included articles that employed systems dynamics, network analysis, or ABM. Systems framing and language (55.9%) described articles that depicted and identified elements of systems thinking including complexity, interrelations, and systems-related frameworks. Additionally, articles were sorted into their D&I intervention type or process including planning and organizing (29.4%), scope of implementation (29.4%), utilization and adoption of an intervention (20.6%), knowledge translation or dissemination (17.6%), training or curriculum development and implementation (2.94%), and implementation evaluation (2.94%). Lastly, articles were reviewed and classified for their nutrition topics including: 23.5% nutrition-related behaviors and outcomes (i.e., hypertension, smoking, physical activity, obesity, diabetes, BMI); 11.7% food, health, and nutrition policy; 11.7% health and nutrition education; 38.2% knowledge translation; 8.82% described intervention methods; and 5.88% health and food access. Table 1 provides a summary of these results.
TABLE 1.
Characteristics of included studies1
| First author, year (reference number) | Study aims | Category | Intervention type | Nutrition topic | Data collection | Theoretical perspective |
|---|---|---|---|---|---|---|
| Shelton RC, 2018 (94) | To examine and discuss conceptual and methodological issues in studying sustainability | Systems framing or language | Scope of Implementation | Intervention methods | Review | Dynamic sustainability framework |
| Stave KA, 2015 (95) | To explain and demonstrate the system dynamics approach for examining food systems closely | Systems modeling (SDM) | Planning and organizing interventions | Agriculture policy, nutrition education, communication, and behavior | Modeling | Whole systems approach |
| Brownson RC, 2018 (90) | To aid practitioners in building organizational-level capacity and assist researchers in conducting participatory research | Systems framing or language | Planning and organizing interventions | Methods to translate health information | Review | n/a |
| Erasmus E, 2016 (63) | To investigate the scope of health and systems education among partners in the organization | Systems framing or language | Scope of implementation | Food and health policy and systems | Cross-sectional | Social science theory |
| Yamey G, 2012 (75) | To understand how to scale up health tools in low- to middle-income countries | Systems framing or language | Scope of implementation | Health and food access | Qualitative Study | Diffusion of innovation |
| Glegg SMN, 2019 (104) | To comprehensively map ways social network analysis are used in D&I | Systems modeling (SNA) | Dissemination | Methods to translate health knowledge/information | Review | Whole systems approach |
| Hammer JM, 2010 (76) | To improve the understanding about what reasonably to expect from large group interventions and how best to design them | Systems framing or language | Planning and organizing interventions | Health and nutrition education | Case study | Large group intervention theory |
| Hitziger M, 2018 (97) | To improve the integration, governance, and coordination of implementing the One Health framework into practice | Systems framing or language | Utilization/adoption of evidence-based practices (EBPs) | Methods to translate health knowledge/information | Case study | One Health framework |
| Zhang J, 2015 (91) | To build an agent-based model (ABM) of adolescent BMI and test the impact of social influence on combined overweight and obesity prevalence in the population | Systems modeling (ABM) | Planning and organizing interventions | BMI and obesity (nutrition-related) | Secondary data analysis | Social learning theory |
| Kalim K, 2006 (86) | To describe systems thinking and illustrate its value in understanding the complexity of the diabetes national service framework | Systems modeling (SDM) | Planning and organizing interventions | Diabetes (nutrition-related disease) | Qualitative study | Systems thinking/systems theory |
| Johnston LM, 2014 (59) | To explore the utility of the intervention-level framework | Systems framing or language | Planning and organizing interventions | Obesity policy | Review | Intervention-level framework |
| Limbani F, 2019 (87) | To report the relationships, benefits, and challenges of process evaluation and complex interventions | Systems framing or language | Utilization/adoption of an EBP | Hypertension (nutrition-related disease) | Case study | n/a |
| Loyo HK, 2013 (77) | To align prevention efforts and maximize the effect of limited resources; to pioneer an innovative, systems-oriented approach to understand the dynamic dimensions of health protection policies | Systems modeling (SDM) | Planning and organizing interventions | Chronic disease/obesity policy (nutrition-related diseases) | Modeling | Whole systems approach |
| Luig T, 2018 (57) | To explore implementation strategies using the interactive systems framework | Systems framing or language | Utilization/adoption of an EBP | Methods to translate health knowledge/information | Qualitative study | Interactive systems framework |
| McGlashan J, 2016 (60) | To explore the application of network analysis to a community-developed causal-loop diagram (CLD) to advance understanding of the system drivers of obesity to plan for interventions | Systems modeling (SNA and SDM) | Planning and organizing interventions | Obesity (nutrition-related) | Modeling | Whole systems approach |
| Widener MJ, 2013 (85) | To contribute to the current discourse on food deserts by presenting an agent-based model (ABM) that tests several spatial and aspatial interventions | Systems modeling (ABM) | Planning and organizing interventions | Health and food access | Modeling | Whole systems approach |
| Nianogo RA, 2015 (88) | To review studies that used agent-based modeling (ABM) to study noncommunicable diseases as well as their risk factors in the context of public health | Systems science modeling (ABM) | Scope of implementation | Physical activity, diet, and diabetes (nutrition-related) | Review | Whole systems approach |
| Buchthal OV, 2015 (103) | To identify communication and collaboration patterns among organizations involved in nutrition education within a diverse community | Systems modeling (SNA) | Dissemination | Methods to translate health knowledge/information | Qualitative study | Whole systems approach |
| Peterson H, 2018 (82) | To describe the importance of implementation science in health | Systems framing or language | Scope of implementation | Methods to translate health knowledge/information | Review | Active implementation framework/interactive and synergistic framework |
| Phillips W, 2006 (102) | To investigate multilevel networks and their impact on diffusion of innovation | Systems framing or language | Dissemination | Methods to translate health knowledge/information | Case study | Systems of innovation |
| Ramaswamy R, 2019 (98) | To develop an interdisciplinary practice-focused curriculum to teach Master of Public Health (MPH) students D&I | Systems framing or language | Curriculum development | Health and nutrition education | Review | Kirkpatrick model of learning evaluation |
| Resnicow K, 2008 (92) | To provide a summary on chaos and complex adaptive systems (CAS) use in public health | Systems framing or language | Scope of implementation | Intervention methods | Review | Chaos theory/complex adaptive systems |
| Riley B, 2012 (78) | To integrate the lessons emerging from the literature with those of identified leaders in public health; to begin to identify useful principles to help public health better understand, assess, and shape the creation and use of EBP | Systems framing or language | Utilization/adoption of EBP | Methods to translate health knowledge/information | Review | Complex adaptive systems |
| Hammond R, 2014 (96) | Re-examine a “follow the average” hypothesis to test whether the central insight from the original model holds and explore what new insights can be gained from a more detailed and complex model | Systems modeling (ABM) | Planning and organizing interventions | BMI (nutrition-related) | Modeling | Whole systems approach |
| Smith T, 2016 (100) | To explore how communities translate evidence-based and promising health practices to rural contexts | Systems framing or language | Utilization/adoption of EBP | Methods to translate health knowledge/information | Case study | Interactive systems framework |
| Theobald S, 2018 (89) | To provide key features in implementation research in low-/middle-income countries | Systems framing or language | Scope of implementation | Methods to translate health knowledge/information | Case study | n/a |
| Wang Y, 2015 (93) | To review current strategies used to model health-related issues by using systems science | Systems modeling (SDM) | Scope of implementation | Obesity and noncommunicable chronic diseases (nutrition-related) | Review | Systems thinking/systems theory |
| Williams J, 2010 (83) | To explore how systems thinking might be used to guide state officials in developing a research-based evaluation plan for training programs and improve the understanding of the relationships and dependencies among units in an organization | Systems framing or language | Utilization/adoption of EBP | Health and nutrition education | Review | ABCD model approach inquiry: Phase A—Where do we want to be? Phase B—How will we know when we reached it? Phase C—Where are we now? Phase D—How do we get from here to our desired place? During the process, researchers continously consider the ongoing changes to the environment |
| Woltering L, 2019 (84) | To demonstrate the problems underlining successful scalability of the sustainable development goals | Systems framing or language | Scope of implementation | Intervention methods | Review | n/a |
| Li Y, 2015 (79) | To use ABM to help understand the potential impact of implementing lifestyle interventions | Systems modeling (ABM) | Utilization/adoption of EBP | Lifestyle intervention (smoking, overweight, diet, and physical activity) | Qualitative study | Whole systems approach |
| Yousefi-Nooraie R, 2015 (80) | Tested whether engagement of staff in the intervention and their behavior were associated with being chosen as information source | Systems modeling (SNA) | Dissemination | Methods to translate health knowledge/information | Longitudinal | Transactive memory principles/whole systems approach |
| Yousefi-Nooraie R, 2012 (101) | A quantitative social network analysis designed to understand how the staff of a health department in Canada turned to peers to seek information regarding research evidence to inform practice-based decisions | Systems modeling (SNA) | Dissemination | Methods to translate health knowledge/information | Cross-sectional | Whole systems approach/social capital theory/social influence theory |
| Yousefi-Nooraie R, 2014 (81) | To model how managers and professional consultants seek information to inform evidence-informed decisions in a public health department in Canada | Systems modeling (SNA) | Dissemination | Methods to translate health knowledge/information | Cross-sectional | Whole systems approach |
| Zenni E, 2006 (99) | To implement and evaluate the effectiveness of scenario-based learning in enhancing medical residents’ competencies of systems thinking to address patients | Systems framing or language | Evaluation | Health and nutrition education | Case study | Systems thinking/systems theory/adult learning theory |
ABM, agent-based modeling; CAS, complex adaptive system; CLD, causal-loop diagram; D&I, dissemination and implementation; EBP, evidence-based practice; n/a, not available; SDM, systems dynamic modeling; SNA, systems network analysis.
Qualitative analysis
Eight key themes emerged from the deductive qualitative thematic analysis of the 34 included articles that describe how systems science methods and framing were applied in nutrition D&I research. Each theme will be defined and highlight key aspects of systems science that should be addressed by individuals that are involved in nutrition implementation science. Further, the benefits and challenges and future research were analyzed from the qualitative data.
Engagement and leadership are defined as having strong strategic support to provide appropriate leadership that will promote nutrition and health-related partnerships and to enhance engagement with key community members that will be a part of the intervention. Engagement and leadership were key themes in 8 articles analyzed in this scoping review (57, 75–81). Six articles (57, 77–81) expressed that the involvement of key leadership encouraged the commitment and empowerment of other key stakeholders, which contributed to the success of systems science methods and framing in the analyzed articles.
Strategies for sustainable interventions are defined as practices that explicitly set out to improve nutrition behaviors and outcomes by outlining clear strategies and goals. Several (9 of 34) articles demonstrated that applying systems science to nutrition implementation had an effect on program effectiveness (82), the planning and organizing process (83), wide-scale adoption and scalability of interventions (84), evaluation and assessment (63), and organizational relationship building (76), and assisted in developing complex interventions (57, 60, 85).
Conceptualizing systems components is the recognition of the complex nature of nutrition D&I research including the acknowledgment of the interacting and evolving elements of the complex adaptive system. Articles (18 of 34) clearly conceptualized and discussed the systems components within their research. Many articles identified and employed a systems-approach methodology, which improved the recognition that nutrition and diet-related interventions are complex and dynamic (59, 77, 83, 86–90). Other articles acknowledged that linear ways of thinking hinder the nutrition implementation process, and that systems science demonstrates complexities, structure, and interrelations, which are important aspects in intervention design (91–93).
Interaction and dynamic relationships are methods or actions of specific activities to develop and maintain relationships among individuals and organizations. Articles identified relationship factors that influence implementation by applying systems science methods. Acknowledged factors included: contextual and organizational structures, and intervention and individual behavioral characteristics that impact nutrition D&I goals, plans, and sustainability (59, 83, 87, 92, 94–97).
Innovation and education defines systems science approaches to support and encourage the development of strategies to address complex nutrition behaviors and outcomes in D&I research. Articles identified that situating education and innovations within systems-oriented frameworks or theories assists stakeholders with design, evaluation, and self-efficacy in nutrition D&I research (59, 83, 96). Furthermore, the development of more trainings and curriculums that focus on applying systems science in nutrition D&I research is needed to enhance knowledge capacity and educational support among practitioners to increase utilization (76, 81, 84, 90, 92, 98, 99). The capacity-building theme elaborates more on increasing available resources and information for innovation and education.
Capacity building is increasing nutrition resources, education, support, and information within a system to encourage change among communities and organizations. Many articles discussed the need for capacity building among organizations to utilize systems science in nutrition D&I research (82, 87, 90, 92–94, 100). Likewise, articles identified that insufficient capacity was a major barrier to systems-oriented nutrition D&I research (63, 75, 77, 79, 90). Other articles referenced the need to address knowledge capacity gaps to increase self-efficacy in systems science and nutrition D&I research (57, 79, 82, 90, 101). Further, the communication and knowledge translation theme below elaborates on additional capacity-building barriers that influence self-efficacy in systems science and nutrition D&I research.
Communication and knowledge translation are mechanisms and processes that support communication of evidence-based information and practice among stakeholders within the system. Twelve articles reported the importance of effective communication (86) and community engagement (77, 100) in nutrition implementation research. Further, the application of systems science resulted in articles identifying the differences in knowledge translation among diverse populations (81, 88, 101). Lastly, articles noted minimal translation and understanding of systems science and D&I theories, models, or frameworks in different settings, which resulted in low self-efficacy and ultimately persistence of the evidence-based information practice gap in health (75, 100).
Monitoring and evaluation describes articulated methods to provide continuous feedback into the system to enhance effectiveness of nutrition D&I research. Articles cited utilizing systems science approaches to monitor and evaluate nutrition D&I research including process evaluation (87), SDM (77), network analysis (93), conceptual models (83), and ABM (79). However, many researchers cited the gap in the current literature for monitoring and evaluating nutrition D&I research including: designing and planning systems-oriented interventions (76); addressing scale-up approaches (75, 84); developing distinct health systems monitoring and evaluation methods (63, 94); development and evaluation of effective systems science competencies and tools (78, 82, 90, 98, 99); and fidelity of nutrition D&I interventions (57, 82, 83, 100, 102).
Benefits and challenges of systems science in nutrition D&I interventions
The 34 included articles were analyzed for the benefits and challenges, specifically stated by the authors and synthesized by the research team, of utilizing systems science in nutrition and diet-related behavior D&I research, as briefly described below. Table 2 provides a simple summary of the benefits and challenges from the qualitative analysis. Articles identified systems science methods as useful tools to strengthen D&I planning and predicting, organizing, communicating and knowledge translation, design, and implementation (76, 77, 83–86, 90, 92, 93, 95–98, 101, 103, 104). Many key challenges included capacity and resources for complex interventions (57, 82, 93), especially in rural contexts (100), and lack of training in systems science and nutrition D&I research (88–90, 93). Articles concluded that future research needs to focus predominantly on educating nutrition researchers and practitioners through trainings and curriculums to enhance systems science in nutrition D&I research (57, 89, 93, 95, 98).
TABLE 2.
Benefits and challenges to systems science methods in nutrition D&I1
| Benefits | Challenges |
|---|---|
| Provides methods for D&I planning and predicting | Methodological and conceptual challenges of measuring sustainability |
| Provides frameworks and models to organize and design implementation | Inconsistent knowledge translation in nutrition and diet research |
| Helps to understand and predict knowledge and communication patterns | Capacity building and resources to implement complex interventions |
| Systems science assisted in visualizing and modeling the complexities of nutrition D&I research | Limited “real-world” interventions and implications |
| Useful in understanding barriers for nutrition education and interventions | Inconsistent and varying language within D&I and systems science |
D&I, dissemination and implementation.
Discussion
Relatively few articles examined systems science in D&I research that focused on addressing nutrition behaviors and intervention methods, and most are recent; therefore, these results suggest an emerging area that deserves more attention. Furthermore, most articles identified by the inclusion process were reviews, which included commentaries, calls for application, or systematic reviews, but did not use systems methodologies. Additionally, the categorical analysis highlighted that systems science is more likely to be theoretically framed rather than utilized within research methodology, which mirrors findings from another systematic review (105), and suggests that prevention science, which includes nutrition interventions, has yet to take full advantage of these analytic approaches (106).
However, the articles that did use systems science methodologies and framing to implement an intervention, highlighted numerous key benefits in applying systems science to nutrition implementation including: planning and organizing potential policies and programs; predicting behavioral outcomes; and visualizing complexity of implementation. These findings reflect previous research by Burke and colleagues (44), which discusses the many implementation successes of 3 case studies that utilized the different models of systems science methods (SNA, SDM, and ABM). Furthermore, the qualitative findings from this review suggest that systems science framing and methods improved key aspects of nutrition D&I process and research such as conceptualizing systems components, methods of monitoring and evaluating, strategies for interventions, and relationships and leadership, echoing similar positive implications outlined by Riley and colleagues (40) and Luke and colleagues (107).
Although current research supports that systems science improves many aspects of health D&I research (40, 44, 107), our review found capacity-building barriers for systems science in nutrition implementation, including knowledge translation of D&I theories, models, and frameworks, as well as limited available educational trainings for nutrition researchers hindering systems science application in the field of nutrition D&I research. Therefore, the remainder of this discussion will reflect more deeply on how to build capacity among nutrition D&I researchers to apply systems science in the implementation process.
Current nutrition implementation researchers emphasize the importance of utilizing implementation science in nutrition interventions (66, 68, 108–111). Koorts and colleagues (112) reported a strong consensus among nutrition and physical activity academics that D&I research was important to reduce the research–practice gap in patients and communities and increase real-world implications of their own research. Nonetheless, a lack of D&I training and expertise, and misunderstanding of how to achieve real-world impact with D&I science hindered individuals’ involvement (112). To achieve desired real-world changes, Warren and colleagues (68) suggest that nutrition strategies need to invoke systems thinking during the implementation process. Similarly, Burke and colleagues (44) argue that successful health implementation cannot take place without acknowledging the complexity of real-world situations and that the tools from systems science are needed to model these interrelated factors. However, to utilize systems science in nutrition interventions, capacity building, including increasing resources and knowledge, is needed (113), which reflects the findings of our review. Additionally, research suggests that a lack of training and expertise in D&I science among nutrition researchers is a barrier to utilization (68, 112), again reflecting the present study's findings.
Existing evidence demonstrates effectiveness of D&I trainings among graduate students, postgraduates, and professionals in public health fields including mental health and cancer. These studies reported significant increases in knowledge of D&I skills (114), demonstrated capability to incorporate D&I into research practice (98), improved understanding of implementation challenges in health care (115), and enhanced understanding of relevant D&I theoretical approaches (115). These results suggest that D&I trainings for graduates, postgraduates, and professionals positively influence knowledge and understanding of D&I science, which has important implications when addressing our review results of current capacity barriers among nutrition researchers and practitioners. Likewise, an NIH-convened panel recognized that D&I trainings should teach trainees to employ methods and strategies from the field and equip them to draw on methods from other areas such as systems science (116). Our results reflect this emerging viewpoint of incorporating other disciplinary methods, such as systems science, within implementation science. Therefore, a nutrition-specific D&I training that incorporates systems science modeling and perspectives would benefit current and future nutrition researchers’ and practitioners’ implementation self-efficacy, skills, and motivations for real-world intervention effectiveness.
With regard to the structure of the proposed nutrition-specific D&I training, current higher-education institutions systems science curriculums in health show positive adult learning outcomes through active learning strategies (83, 98, 99, 117). Active learning techniques ask participants to engage by practicing skills, solving problems to complex programs, proposing solutions, and explaining ideas (118). Current research demonstrates advantages of active learning strategies, such as scenario-based case studies, in teaching systems science in health implementation research, including: an increased understanding of barriers to care (99); improved knowledge and skills of systems science in health (117); and acquisition of knowledge to apply systems science frameworks and theory to frame the implementation process (83, 98). Additionally, many researchers discuss the need for mentorship (114) and faculty engagement (98) to act as translators when simulating active learning techniques, which is similar to a collaborative learning approach (119). A collaborative learning approach describes the joint intellectual effort by students and teachers to acquire knowledge (120). Current curriculums teaching systems science employing collaborative teaching strategies report that students are able to critically examine the complex challenges within food, nutrition, and health programs (121). Chambers and colleagues (122) encourage implementation science training programs moving toward problem-solving and activity style learning. Thus, enhancement of learning outcomes among current and future adult nutrition researchers and practitioners should incorporate active learning strategies and collaborative learning approaches to the acquisition of knowledge and skills in the application of systems science in implementation.
In terms of population for the proposed capacity-building training, it is important to start to train future nutrition researchers and practitioners. Highly selective training programs limit the amount and type of people able to receive the education (116). Additionally, training should be available for people in a variety of implementation roles, including predoctoral, early career, and experienced practitioners (116). Therefore, the proposed curriculum should be available to a variety of nutrition practitioners including university nutrition and public health students, registered dietitians, and established researchers. To incentivize current students and future registered dietitians to complete the proposed curriculum, course developers should build courses from previously identified D&I competencies (123) and from the Society of Nutrition Education competencies (124) to help with validation and to institutionalize the proposed curriculum for future nutrition degree recipients. Lastly, additional incentives could include awarding continuous educational credits, for Registered Dietitians to maintain their licensure, for completion of such courses, and for funders to highlight emerging issues such as capacity building in nutrition through targeted strategies (e.g., funding announcements, training programs, or support for new research teams) (125).
Limitations
This study is not without limitations. First, only 1 author was involved in the screening process. Whereas the search strategy, inclusion/exclusion criteria, and data analysis were reviewed and approved collaboratively, the screening process was done during the initial COVID-19 pandemic lockdown, which made collaborating for the inclusion process challenging. Although the researcher who led the inclusion process is proficient in nutrition D&I research and systems thinking, the article screen process was done independently, which is a limitation of this scoping review. Further, the inconsistencies and adapting language surrounding the interdisciplinary fields of D&I and systems science challenged the development of key terms and inclusion criteria, and influenced the databases chosen. Given these challenges, this review aimed to be exhaustive; however, the complex nature of this subject matter might have excluded some research. Furthermore, not all databases used MeSH terms, key terms, or subject headings, which could influence the types of articles retrieved. Lastly, indexing of articles sometimes takes up to a year, which could have potentially impacted article retrieval and inclusion analysis.
Conclusions
This study demonstrates that systems science provides positive implementation approaches to design and translate nutrition behaviors and knowledge into practice. However, capacity-building barriers for systems science in nutrition implementation, including limited available educational trainings for nutrition researchers, hinder systems science application in the field of nutrition D&I research. Therefore, our results suggest that an active and collaborative teaching method for a nutrition-specific D&I curriculum for university nutrition and public health students, registered dietitians, and established researchers is likely to enhance systems science skills, which aligns well with current literature implications. It is also important to note that capacity needs to be built at a higher level (e.g., funding announcements, training programs, or support for new research teams) as well as to support the development of said curriculums and to incentivize participation.
Supplementary Material
ACKNOWLEDGEMENTS
We acknowledge Susan Arnold for her contributions to the development of the search strategy.
The authors’ responsibilities were as follows—AEW: designed the study, conducted the search, screened for inclusion, extracted data, synthesized the literature, and drafted the manuscript; RAW: contributed to data analysis, study refinement, and revisions to draft manuscript; MDO: verified data extraction, inclusion and exclusion criteria, and contributed to study refinement and revisions to draft manuscript; and all authors: read and approved the final manuscript.
Notes
This study was funded by West Virginia Agricultural and Forestry Experiment Station (WVA00745).
Author disclosures: The authors report no conflicts of interest.
Supplemental Table 1 is available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/cdn/
Abbreviations used: ABM, agent-based modeling; D&I, dissemination and implementation; MeSH, medical subject headings; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; SDM, systems dynamic modeling; SNA, systems network analysis.
Contributor Information
Ayron E Walker, Division of Animal and Nutritional Sciences, Davis College of Agriculture, Natural Resources and Design, West Virginia University, Morgantown, WV, USA.
Rachel A Wattick, Division of Animal and Nutritional Sciences, Davis College of Agriculture, Natural Resources and Design, West Virginia University, Morgantown, WV, USA.
Melissa D Olfert, Email: Melissa.olfert@mail.wvu.edu, Division of Animal and Nutritional Sciences, Davis College of Agriculture, Natural Resources and Design, West Virginia University, Morgantown, WV, USA.
References
- 1.Reedy J, Krebs-Smith S, Hammond R, Hennessy E. Advancing the science of dietary patterns research to leverage a complex systems approach. J Acad Nutr Diet. 2017;117(7):1019–22. [DOI] [PubMed] [Google Scholar]
- 2.Contento IR, Koch PA. Nutrition education: linking research, theory, and practice. 4th ed. Burlington (MA): Jones & Bartlett Learning; 2020. [Google Scholar]
- 3.Stewart H, Hyman J.. Americans still can meet fruit and vegetable dietary guidelines for $2.10–$2.60 per day. [Internet]. USDA Economic Research Service; 2019 [cited August 4, 2021]. Available from: https://www.ers.usda.gov/amber-waves/2019/june/americans-still-can-meet-fruit-and-vegetable-dietary-guidelines-for-210-260-per-day/. [Google Scholar]
- 4.Health and Human Services, United States Department of Agriculture . Dietary guidelines For Americans 2015–2020. USDA; 2015. [Google Scholar]
- 5.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: united states, 2015–2016. NCHS Data Brief no. 288 [Internet]. US Department of Health and Human Services; 2017 [cited August 4, 2021]. Available from: https://www.cdc.gov/nchs/data/databriefs/db288.pdf. [Google Scholar]
- 6.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Overweight and obesity: CDC report. CDC; 2009. [Google Scholar]
- 7.Centers for Disease Control and Prevention . Adult obesity causes and consequences: overweight and obesity. CDC; 2019. [Google Scholar]
- 8.Olfert M, Famodu O, Flanagan S, Smith E, Leary M. The effect of icook 4-H, a childhood obesity prevention program, on blood pressure and quality of life in youth and adults: a randomized control trial. J Child Obes. 2018;3(1):4. [Google Scholar]
- 9.White AA, Colby S, Franzen-Castle L, Kattelmann K, Olfert M. iCook: a 4-H program to promote culinary skills and family meals for obesity prevention. J Nutr Educ Behav. 2013;45(4):S91. [Google Scholar]
- 10.Eck K, Alleman GP, Quick V, Martin-Biggers J, Hongu N, Byrd-Bredbenner C. Evaluation of a childhood obesity prevention online training certificate program for community family educators. J Community Health. 2016;41(6):1187–95. [DOI] [PubMed] [Google Scholar]
- 11.Eck KM, Delaney CL, Olfert MD, Shelnutt KP, Byrd-Bredbenner C. “If my family is happy, then I am happy”: quality-of-life determinants of parents of school-age children. SAGE Open Med. 2019;7:2050312119828535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eck KM, Delaney CL, Shelnutt KP, Olfert MD, Byrd-Bredbenner C. Parenting advice school-age kids offer to parents to promote healthier child weight-related behaviors. J Nutr Educ Behav. 2020;52(3):290–8. [DOI] [PubMed] [Google Scholar]
- 13.Martin-Biggers J, Spaccarotella K, Delaney C, Koenings M, Alleman G, Hongu N, Worobey J, Byrd-Bredbenner C. Development of the intervention materials for the Homestyles obesity prevention program for parents of preschoolers. Nutrients. 2015;7(8):6628–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Colby S, Olfert M, Mathews A, Kattelmann K, Kidd T, Brown O, White A, Horacek T, Shelnutt K, Byrd-Bredbenner Cet al. “Get Fruved”: the RCT year. J Nutr Educ Behav. 2018;50(7):S116–17. [Google Scholar]
- 15.Barr ML, Colby SE, Riggsbee K, Leischner K, Mathews AE, Vilaro MJ, Kattelmann KK, Olfert MD. Health behaviors of student community research partners when designing and implementing a healthy lifestyle intervention on college campuses. Behav Sci (Basel). 2018;8(11):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koenings MM, Olfert M, Kattelmann KK, Nitzke S. Pseudo-underage students' access to alcohol surrounding three college campuses. J Hunger Environ Nutr. 2013;8(1):95–105. [Google Scholar]
- 17.Kattelmann KK, White AA, Greene GW, Byrd-Bredbenner C, Hoerr SL, Horacek TM, Phillips BW, Koenings MM, Brown ON, Olfert MDet al. Development of Young Adults Eating and Active for Health (YEAH) internet-based intervention via a community-based participatory research model. J Nutr Educ Behav. 2014;46(2):S10–25. [DOI] [PubMed] [Google Scholar]
- 18.Morrell JS, Byrd-Bredbenner C, Quick V, Olfert M, Dent A, Carey GB. Metabolic syndrome: comparison of prevalence in young adults at 3 land-grant universities. J Am Coll Health. 2014;62(1):1–9. [DOI] [PubMed] [Google Scholar]
- 19.Kattelmann KK, Bredbenner CB, White AA, Greene GW, Hoerr SL, Kidd T, Colby S, Horacek TM, Phillips BW, Koenings MMet al. The effects of Young Adults Eating and Active for Health (YEAH): a theory-based web-delivered intervention. J Nutr Educ Behav. 2014;46(6):S27–41. [DOI] [PubMed] [Google Scholar]
- 20.Brown O, Quick V, Colby S, Greene G, Horacek TM, Hoerr S, Koenings M, Kidd T, Morrell J, Olfert Met al. Recruitment lessons learned from a tailored web-based health intervention project Y.E.A.H. (Young Adults Eating and Active for Health). Health Educ. 2015;115(5):470–9. [Google Scholar]
- 21.Colby S, Zhou W, Sowers MF, Shelnutt K, Olfert MD, Morrell J, Koenings M, Kidd T, Horacek TM, Greene GWet al. College students' health behavior clusters: differences by sex. Am J Health Behav. 2017;41(4):378–89. [DOI] [PubMed] [Google Scholar]
- 22.Olfert MD, Dent A, Wattick RA. Metabolic syndrome prevalence in students attending West Virginia University. J Clin Med. 2018;7(12):487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clark RL, Famodu OA, Holásková I, Infante AM, Murray PJ, Olfert IM, McFadden JW, Downes MT, Chantler PD, Duespohl MWet al. Educational intervention improves fruit and vegetable intake in young adults with metabolic syndrome components. Nutr Res. 2019;62:89–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hagedorn RL, McArthur LH, Hood LB, Berner M, Anderson Steeves ET, Connell CL, Wall-Bassett E, Spence M, Babatunde OT, Kelly BEet al. Expenditure, coping, and academic behaviors among food-insecure college students at 10 higher education institutes in the Appalachian and Southeastern regions. Curr Dev Nutr. 2019;3(6):nzz058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hagedorn RL, Olfert MD. Food insecurity and behavioral characteristics for academic success in young adults attending an Appalachian university. Nutrients. 2018;10(3):361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hagedorn RL, Pampalone AL, Hood LB, Yura CA, Morrow DF, Olfert MD. Higher education food insecurity toolkit development and feedback. J Nutr Educ Behav. 2020;52(1):64–72. [DOI] [PubMed] [Google Scholar]
- 27.Olfert MD, Wattick RA. Vegetarian diets and the risk of diabetes. Curr Diab Rep. 2018;18(11):101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wattick RA, Hagedorn RL, Olfert MD. Relationship between diet and mental health in a young adult Appalachian college population. Nutrients. 2018;10(8):957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wattick RA, Hagedorn RL, Olfert MD. Enhancing college student recovery outcomes through nutrition and culinary therapy. J Nutr Educ Behav. 2020;52(3):326–9. [DOI] [PubMed] [Google Scholar]
- 30.Santella ME, Hagedorn RL, Wattick RA, Barr ML, Horacek TM, Olfert MD. Learn first, practice second approach to increase health professionals’ nutrition-related knowledge, attitudes and self-efficacy. Int J Food Sci Nutr. 2020;71(3):370–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Olfert MD, Wattick RA, Hagedorn RL. Experiential application of a culinary medicine cultural immersion program for health professionals. J Med Educ Curric Dev. 2020;7:2382120520927396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Olfert MD, Wattick RA, Hagedorn RL. Experiences of multidisciplinary health professionals from a culinary medicine cultural immersion: qualitative analysis. J Med Educ Curric Dev. 2020;7:7396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Browne S, Minozzi S, Bellisario C, Sweeney MR, Susta D. Effectiveness of interventions aimed at improving dietary behaviours among people at higher risk of or with chronic non-communicable diseases: an overview of systematic reviews. Eur J Clin Nutr. 2019;73(1):9–23. [DOI] [PubMed] [Google Scholar]
- 34.Gwynn J, Sim K, Searle T, Senior A, Lee A, Brimblecombe J. Effect of nutrition interventions on diet-related and health outcomes of Aboriginal and Torres Strait Islander Australians: a systematic review. BMJ Open. 2019;9:e025291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brace AM, De Andrade FC, Finkelstein B. Assessing the effectiveness of nutrition interventions implemented among US college students to promote healthy behaviors: a systematic review. Nutr Health. 2018;24(3):171–81. [DOI] [PubMed] [Google Scholar]
- 36.da Silva Lopes K, Ota E, Shakya P, Dagvadorj A, Balogun O, Peña-Rosas J, De-Regil LM, Mori R. Effects of nutrition interventions during pregnancy on low birth weight: an overview of systematic reviews. BMJ Glob Health. 2017;2(3):e000389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fabbri A, Chartres N, Scrinis G, Bero L. Study sponsorship and the nutrition research agenda: analysis of randomized controlled trials included in systematic reviews of nutrition interventions to address obesity. Public Health Nutr. 2017;20(7):1306–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haby M, Chapman E, Clark R, Galvão L. Agriculture, food, and nutrition interventions that facilitate sustainable food production and impact health: an overview of systematic reviews. Rev Panam Salud Publica. 2016;40(1):48–56. [PubMed] [Google Scholar]
- 39.Oldroyd J, Burns C, Lucas P, Haikerwal A, Waters E. The effectiveness of nutrition interventions on dietary outcomes by relative social disadvantage: a systematic review. J Epidemiol Community Health. 2008;62(7):573–9. [DOI] [PubMed] [Google Scholar]
- 40.Riley B, Willis C, Holmes B, Finegood DI, Best AL, McIsaac J. Systems thinking and dissemination and implementation research. In: Brownson RC, Colditz GA, Proctor EK, editors. Dissemination and implementation research in health: translating science to practice. New York: Oxford University Press; 2017. p. 143–55. [Google Scholar]
- 41.Kreuter MW, De Rosa C, Howze EH, Baldwin GT. Understanding wicked problems: a key to advancing environmental health promotion. Health Educ Behav. 2004;31(4):441–54. [DOI] [PubMed] [Google Scholar]
- 42.Peters DH. The application of systems thinking in health: why use systems thinking?. Health Res Policy Syst. 2014;12(1):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Meadows DH. Thinking in systems: a primer. White River Junction (VT): Chelsea Green Publishing; 2008. [Google Scholar]
- 44.Burke JG, Lich KH, Neal JW, Meissner HI, Yonas M, Mabry PL. Enhancing dissemination and implementation research using systems science methods. Int J Behav Med. 2015;22(3):283–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Green LW. Public health asks of systems science: to advance our evidence-based practice, can you help us get more practice-based evidence?. Am J Public Health. 2006;96(3):406–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Waterson P. A critical review of the systems approach within patient safety research. Ergonomics. 2009;52(10):1185–95. [DOI] [PubMed] [Google Scholar]
- 47.Eisenberg JM. Continuing education meets the learning organization: the challenge of a systems approach to patient safety. J Contin Educ Health Prof. 2017;37(4):255–61. [DOI] [PubMed] [Google Scholar]
- 48.Aboumatar HJ, Thompson D, Wu A, Dawson P, Colbert J, Marsteller J, Kent P, Lubomski LH, Paine L, Pronovost P. Development and evaluation of a 3-day patient safety curriculum to advance knowledge, self-efficacy and system thinking among medical students. BMJ Qual Saf. 2012;21(5):416–22. [DOI] [PubMed] [Google Scholar]
- 49.Thompson DA, Cowan J, Holzmueller C, Wu AW, Bass E, Pronovost P. Planning and implementing a systems-based patient safety curriculum in medical education. Am J Med Qual. 2008;23(4):271–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McNab D, Bowie P, Morrison J, Ross A. Understanding patient safety performance and educational needs using the ‘safety-ii’ approach for complex systems. Educ Prim Care. 2016;27(6):443–50. [DOI] [PubMed] [Google Scholar]
- 51.Brimble MJ, Jones A. Using systems thinking in patient safety: a case study on medicines management. Nurs Manag (Harrow). 2017;24(4):28–33. [DOI] [PubMed] [Google Scholar]
- 52.Tetuan T, Ohm R, Kinzie L, McMaster S, Moffitt B, Mosier M. Does systems thinking improve the perception of safety culture and patient safety?. J Nurs Regul. 2017;8(2):31–9. [Google Scholar]
- 53.Braithwaite J, Churruca K, Long JC, Ellis LA, Herkes J. When complexity science meets implementation science: a theoretical and empirical analysis of systems change. BMC Med. 2018;16(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Braithwaite J, Zurynski Y, Ludlow K, Holt J, Augustsson H, Campbell M. Towards sustainable healthcare system performance in the 21st century in high-income countries: a protocol for a systematic review of the grey literature. BMJ Open. 2019;9(1):e025892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Siddiqi K, Sheikh A. Primary care respiratory medicine broadens its focus to include global respiratory health, tobacco control and implementation science. NPJ Prim Care Respir Med. 2017;27(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tengs TO, Osgood ND, Chen LL. The cost-effectiveness of intensive national school-based anti-tobacco education: results from the Tobacco Policy Model. Prev Med. 2001;33(6):558–70. [DOI] [PubMed] [Google Scholar]
- 57.Luig T, Asselin J, Sharma A, Campbell-Scherer D. Understanding implementation of complex interventions in primary care teams. J Am Board Fam Med. 2018;31(3):431–44. [DOI] [PubMed] [Google Scholar]
- 58.Bagnall A, Radley D, Jones R, Gately P, Nobles J, Van Dijk M, Blackshaw J, Montel S, Sahota P. Whole systems approaches to obesity and other complex public health challenges: a systematic review. BMC Public Health. 2019;19(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Johnston LM, Matteson CL, Finegood DT. Systems science and obesity policy: a novel framework for analyzing and rethinking population-level planning. Am J Public Health. 2014;104(7):1270–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McGlashan J, Johnstone M, Creighton D, de la Haye K, Allender S. Quantifying a systems map: network analysis of a childhood obesity causal loop diagram. PLoS One. 2016;11(10):e0165459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Joffe M, Mindell J. Complex causal process diagrams for analyzing the health impacts of policy interventions. Am J Public Health. 2006;96(3):473–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mabry PL, Marcus SE, Clark PI, Leischow SJ, Méndez D. Systems science: a revolution in public health policy research. Am J Public Health. 2010;100(7):1161–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Erasmus E, Lehmann U, Agyepong IA, Alwar J, de Savigny D, Kamuzora P, Mirzoev T, Nxumalo N, Tomson G, Uzochuwu Bet al. Strengthening post-graduate educational capacity for health policy and systems research and analysis: the strategy of the consortium for health policy and systems analysis in Africa. Health Res Policy Syst. 2016;14:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Maurya D, Mintrom M. Policy entrepreneurs as catalysts of broad system change: the case of social health insurance adoption in India. J Asian Public Policy. 2020;13(1):18–34. [Google Scholar]
- 65.Boumans D, Ferry M. Networks and efficient policy implementation: insights from cohesion policy. Evaluation. 2019;25(4):411–29. [Google Scholar]
- 66.Tumilowicz A, Ruel MT, Pelto G, Pelletier D, Monterrosa EC, Lapping K, Kraemer K, De Regil LM, Giles B, Mandana Aet al. Implementation science in nutrition: concepts and frameworks for an emerging field of science and practice. Curr Dev Nutr. 2019;3(3):nzy080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tumilowicz A, Neufeld LM, Pelto GH. Using ethnography in implementation research to improve nutrition interventions in populations. Matern Child Nutr. 2015;11(S3):55–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Warren AM, Frongillo EA, Rawat R. Building implementation science in nutrition. Adv Nutr. 2020;11(5):1392–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Armstrong R, Hall BJ, Doyle J, Waters E. ‘Scoping the scope’ of a Cochrane review. J Public Health. 2011;33(1):147–50. [DOI] [PubMed] [Google Scholar]
- 70.Mays N, Roberts E, Popay J. Synthesizing research evidence. : Fulop N, Allen P, Clarke A, Black N, Anderson S, . Studying the organization and delivery of health services: research methods. London: Routledge; 2001. p. 188–220. [Google Scholar]
- 71.Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 73.Daly J, Kellehear A, Gliksman M. The public health researcher: a methodological guide. Melbourne: Oxford University Press; 1997. [Google Scholar]
- 74.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yamey G. What are the barriers to scaling up health interventions in low and middle income countries? A qualitative study of academic leaders in implementation science. Glob Health. 2012;8(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hammer JM. Large group interventions as a tool for community visioning and planning. Community Dev J. 2010;41(2):209–22. [Google Scholar]
- 77.Loyo HK, Batcher C, Wile K, Huang P, Orenstein D, Milstein B. From model to action: using a system dynamics model of chronic disease risks to align community action. Health Promot Pract. 2013;14(1):53–61. [DOI] [PubMed] [Google Scholar]
- 78.Riley B, Norman CD, Best A. Knowledge integration in public health: a rapid review using systems thinking. Evid Policy. 2012;8(4):417–31. [Google Scholar]
- 79.Li Y, Kong N, Lawley M, Weiss L, Pagán JA. Advancing the use of evidence-based decision-making in local health departments with systems science methodologies. Am J Public Health. 2015;105(S2):S217–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yousefi-Nooraie R, Dobbins M, Marin A, Hanneman R, Lohfeld L. The evolution of social networks through the implementation of evidence-informed decision-making interventions: a longitudinal analysis of three public health units in Canada. Implement Sci. 2015;10(1):166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yousefi-Nooraie R, Dobbins M, Marin A. Social and organizational factors affecting implementation of evidence-informed practice in a public health department in Ontario: a network modelling approach. Implement Sci. 2014;9(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Peterson H, Haidar J, Fixsen D, Ramaswamy R, Weiner B, Leatherman S. Implementing innovations in global women's, children's, and adolescents' health: realizing the potential for implementation science. Obstet Gynecol. 2018;131(3):423–30. [DOI] [PubMed] [Google Scholar]
- 83.Williams J, Costich J, Hacker W, Davis J. Lessons learned in systems thinking approach for evaluation planning. J Public Health Manag Pract. 2010;16(2):151–5. [DOI] [PubMed] [Google Scholar]
- 84.Woltering L, Fehlenberg K, Gerard B, Ubels J, Cooley L. Scaling from “reaching many” to sustainable systems change at scale: a critical shift in mindset. Agric Syst. 2019;176:102652. [Google Scholar]
- 85.Widener MJ, Metcalf SS, Bar-Yam Y. Agent-based modeling of policies to improve urban food access for low-income populations. Appl Geogr. 2013;40:1–10. [Google Scholar]
- 86.Kalim K, Carson E, Cramp D. An illustration of whole systems thinking. Health Serv Manage Res. 2006;19(3):174–85. [DOI] [PubMed] [Google Scholar]
- 87.Limbani F, Goudge J, Joshi R, Maar MA, Miranda JJ, Oldenburg B, Parker G, Peasnates MA, Riddell MC, Salam Aet al. Process evaluation in the field: global learnings from seven implementation research hypertension projects in low-and middle-income countries. BMC Public Health. 2019;19(1):953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Nianogo RA, Arah OA. Agent-based modeling of noncommunicable diseases: a systematic review. Am J Public Health. 2015;105(3):e20–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Theobald S, Brandes N, Gyapong M, El-Saharty S, Proctor E, Diaz T, Wanji S, Elloker S, Raven J, Elsey Het al. Implementation research: new imperatives and opportunities in global health. Lancet. 2018;392(10160):2214–28. [DOI] [PubMed] [Google Scholar]
- 90.Brownson RC, Fielding JE, Green LW. Building capacity for evidence-based public health: reconciling the pulls of practice and the push of research. Annu Rev Public Health. 2018;39:27–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhang J, Tong L, Lamberson P, Durazo-Arvizu R, Luke A, Shoham D. Leveraging social influence to address overweight and obesity using agent-based models: the role of adolescent social networks. Soc Sci Med. 2015;125:203–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Resnicow K, Page SE. Embracing chaos and complexity: a quantum change for public health. Am J Public Health. 2008;98(8):1382–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wang Y, Xue H, Liu S. Applications of systems science in biomedical research regarding obesity and noncommunicable chronic diseases: opportunities, promise, and challenges. Adv Nutr. 2015;6(1):88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Shelton RC, Cooper BR, Stirman SW. The sustainability of evidence-based interventions and practices in public health and health care. Annu Rev Public Health. 2018;39(1):55–76. [DOI] [PubMed] [Google Scholar]
- 95.Stave KA, Kopainsky B. A system dynamics approach for examining mechanisms and pathways of food supply vulnerability. J Environ Stud Sci. 2015;5(3):321–36. [Google Scholar]
- 96.Hammond R, Ornstein J. A model of social influence on body mass index. Ann N Y Acad Sci. 2014;1331(1):34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hitziger M, Esposito R, Canali M, Aragrande M, Häsler B, Rüegg SR. Knowledge integration in One Health policy formulation, implementation and evaluation. Bull World Health Organ. 2018;96(3):211–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ramaswamy R, Mosnier J, Reed K, Powell BJ, Schenck AP. Building capacity for Public Health 3.0: introducing implementation science into an MPH curriculum. Implement Sci. 2019;14(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zenni E, Ravago L, Ewart C, Livingood W, Wood D, Goldhagen J. A walk in the patients' shoes: a step toward competency development in systems-based practice. Acad Pediatr. 2006;6(1):54–7. [DOI] [PubMed] [Google Scholar]
- 100.Smith T, Adimu T, Martinez A, Minyard K. Selecting, adapting, and implementing evidence-based interventions in rural settings: an analysis of 70 community examples. J Health Care Poor Underserved. 2016;27(4A):181–93. [DOI] [PubMed] [Google Scholar]
- 101.Yousefi-Nooraie R, Dobbins M, Brouwers M, Wakefield P. Information seeking for making evidence-informed decisions: a social network analysis on the staff of a public health department in Canada. BMC Health Serv Res. 2012;12:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Phillips W, Johnsen T, Caldwell N, Lewis MA. Investigating innovation in complex health care supply networks: an initial conceptual framework. Health Serv Manage Res. 2006;19(3):197–206. [DOI] [PubMed] [Google Scholar]
- 103.Buchthal OV, Maddock JE.. Mapping the possibilities: using network analysis to identify opportunities for building nutrition partnerships within diverse low-income communities. J Nutr Educ Behav. 2015;47(4):300–307.e1. [DOI] [PubMed] [Google Scholar]
- 104.Glegg SMN, Jenkins E, Kothari A. How the study of networks informs knowledge translation and implementation: a scoping review. Implement Sci. 2019;14(1):1–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Carey G, Malbon E, Carey N, Joyce A, Crammond B, Carey A. Systems science and systems thinking for public health: a systematic review of the field. BMJ Open. 2015;5(e009002):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lich KH, Ginexi EM, Osgood ND, Mabry PL. A call to address complexity in prevention science research. Prev Sci. 2013;14(3):279–89. [DOI] [PubMed] [Google Scholar]
- 107.Luke DA, Morshed AB, McKay VR, Combs TB. Systems science methods in dissemination and implementation research. In: Brownson RC, Colditz GA, Proctor EA, editors. Dissemination and implementation research in health: translating science to practice. 2nd ed.New York (NY): Oxford University Press; 2018. [Google Scholar]
- 108.Pérez-Escamilla R, Odle J. Implementation science in the field of nutrition: why is it so relevant?. Curr Dev Nutr. 2019;3(3):nzy086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sarma H, D'Este C, Ahmed T, Bossert TJ, Banwell C. Developing a conceptual framework for implementation science to evaluate a nutrition intervention scaled-up in a real-world setting. Public Health Nutr. 2021;24(S1):s7–s22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sarma H. Implementation science in nutrition: a summary and synthesis. Public Health Nutr. 2021;24(S1):s1–s6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Murofushi K, Badaracco C, County C, Gonzales-Pacheco D, Silzle C, Watowicz R, Moloney L. Implementation science in evidence-based nutrition practice: considerations for the registered dietitian nutritionist. J Acad Nutr Diet. 2021;121(7):1392–400. [DOI] [PubMed] [Google Scholar]
- 112.Koorts H, Naylor P-J, Laws R, Love P, Maple J-L, van Nassau F.. What hinders and helps academics to conduct dissemination and implementation (D&I) research in the field of nutrition and physical activity? An international perspective. Int J Behav Nutr Phy. 2020;17(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Gillespie S, van den Bold M.. Agriculture, food systems, and nutrition: meeting the challenge. Glob Chall. 2017;1(3):1600002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Padek M, Mir N, Jacob RR, Chambers DA, Dobbins M, Emmons KM, Kerner J, Kumanyika S, Pfund C, Proctor EKet al. Training scholars in dissemination and implementation research for cancer prevention and control: a mentored approach. Implement Sci. 2018;13(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Carlfjord S, Roback K, Nilsen P. Five years’ experience of an annual course on implementation science: an evaluation among course participants. Implement Sci. 2017;12(1):101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Proctor EK, Chambers DA. Training in dissemination and implementation research: a field-wide perspective. Transl Behav Med. 2017;7(3):624–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gonzalo JD, Haidet P, Blatt, B, Wolpaw DR. Exploring challenges in implementing a health systems science curriculum: a qualitative analysis of student perceptions. Med Educ. 2016;50:523–31. [DOI] [PubMed] [Google Scholar]
- 118.Center for Teaching Innovation. Active learning [Internet]. Cornell University; 2021 [cited on July 21, 2021]. Available from:https://teaching.cornell.edu/teaching-resources/engaging-students/active-learning. [Google Scholar]
- 119.Smith BLM, Jean T. What is collaborative learning? Pennsylvania State University: National Center on Postsecondary Teaching, Learning, and Assessment;1992. [Google Scholar]
- 120.MacGregor H, McKenzie A, Jacobs T, Ullauri A. Scaling up ART adherence clubs in the public sector health system in the Western Cape, South Africa: a study of the institutionalisation of a pilot innovation. Glob Health. 2018;14:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Clark S, Byker C, Niewolny K, Helms J. Framing an undergraduate minor through the civic agriculture and food systems curriculum. NACTA J. 2013;57(2):56–67. [Google Scholar]
- 122.Chambers DA, Proctor EK, Brownson RC, Straus SE. Mapping training needs for dissemination and implementation research: lessons from a synthesis of existing D&I research training programs. Transl Behav Med. 2017;7(3):593–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Padek M, Colditz G, Dobbins M, Koscielniak N, Proctor EK, Sales AE, Brownson RC. Developing educational competencies for dissemination and implementation research training programs: an exploratory analysis using card sorts. Implement Sci. 2015;10(1):114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Society for Nutrition Education and Behavior. Nutrition educator competencies [Internet]. 2016 [cited October 26, 2020]. Available from: https://www.sneb.org/nutrition-educator-competencies/ [Google Scholar]
- 125.Norton WE, Lungeanu A, Chambers DA, Contractor N. Mapping the growing discipline of dissemination and implementation science in health. Scientometrics. 2017;112(3):1367–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


