Abstract
Objectives
High rates of depression, anxiety and stress are reported in tertiary health students. Mindfulness-based programs have been included in the training of health students to help them manage depression, anxiety and stress; however, to date, there has been no review of best practice implementation of mindfulness for health students. The aim of this review was to evaluate the outcomes of mindfulness-based practice for health students to inform best practice with this population.
Methods
A comprehensive search was conducted of three electronic databases (PsychINFO, Medline and Embase) guided by the five-step systematic process for conducting scoping reviews to investigate mindfulness-based intervention programs for students enrolled in a tertiary institution in a health-related course.
Results
Twenty-four papers met the eligibility criteria and were reviewed in detail. Findings suggested that mindfulness-based intervention approaches are useful in decreasing depression, anxiety and stress in health students; however, challenges exist in student engagement and retention. Generalization of results was limited by the heterogeneous population, intervention designs and delivery methods, as well as a lack of standardized outcome measures.
Conclusion
The inclusion of mindfulness-based programs within tertiary curricula can be an effective approach to assist with managing depression, stress and anxiety in health students. Providing academic credit to students, improving translation of skills to working with future clients, and embedding mindfulness-based programs within the curriculum could improve engagement and retention.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12671-021-01740-3.
Keywords: Health students, Mindfulness, Mental health, Anxiety, Stress
The transition into tertiary or post-secondary education (university or college) is a significant milestone in the lives of young adults. While many cope well, a large proportion of students experience high levels of stress, anxiety and depression. Ramón-Arbués et al., (2020) reported a moderate prevalence of depression and anxiety, and reported that 34.5% of college students experienced significant stress. An Australian report indicated that 83.2% of students in tertiary education in Australia felt stressed, 79% were anxious, 66% reported high psychological distress and greater than 50% experienced sleep disturbance (Rickwood et al., 2016). More concerning is the dramatic increase in mental health disorders and the limited availability of supports to meet service demands with this population (Auerbach et al., 2018).
A recent study of over 600,000 college students in the United States, reported rates of depression, anxiety, suicidal ideation and attempts doubled between 2007 and 2018, with the steepest increase occurring in the period from 2014 to 2018 (Duffy et al., 2019). Moreover, there is some emerging evidence that the COVID-19 pandemic resulted in further increases in anxiety and depression in college students compared to a similar stage of the previous academic year (Huckins et al., 2020).
The existence of mental health issues in students studying health-related programs at university or college is supported by recent studies; however, much of the research has focused on the mental health of medical students. Medical students are at a high risk of experiencing burnout given the academic pressure, perfectionist standards and demanding nature of medical practice (Nechita et al., 2014; Ray & Joseph, 2010; Ribeiro et al., 2017). While there are several studies that investigate the mental health of medical students, there is less research that has investigated the depression, stress and anxiety levels of students in other health professions such as, occupational therapy, physiotherapy, speech pathology, social work and psychology. Given the similarities between medical training and allied health training programs, the psychological problems experienced by students in all these courses is expected to be commensurate. Ribeiro et al., (2017) suggested that students’ resilience may be compromised, particularly in the transition to clinical placements in health-related courses. Moreover, students in these courses are often at an age where stress-related disorders are more common (Regehr et al., 2013).
The introduction of mindfulness-based programs is one approach used to assist in the management of student stress, anxiety and depression in this population. Mindfulness-based interventions have shown to be successful in cognitive and behavioural approaches for students experiencing depression, stress and anxiety (Hofmann & Gómez, 2017). Mindfulness refers to the state of bringing non-judgmental awareness to the present moment and is described as having two components: (1) self-regulation of attention and (2) orientating an individual to the present moment with curiosity, openness and acceptance (Bishop et al., 2004; Hofmann et al., 2010). Two common mindfulness-based interventions include mindfulness-based stress reduction (MBSR) and mindfulness-based cognitive therapy (MBCT) (Kabat-Zinn, 1982; Teasdale et al., 2000). Mindfulness-based stress reduction is an 8-week treatment program with regular 45 min per day of meditation practice. In contrast, MBCT incorporates mindfulness training with cognitive therapy but consists of the same program duration and associated home practice.
Numerous studies have reported the effectiveness of mindfulness programs in reducing the levels of stress and depression in university students (Regehr et al., 2013; Reid, 2013). Given the effectiveness of mindfulness programs with this population, there have been calls for the inclusion of mindfulness in the training of all health professionals to help address the increased psychological problems often experienced by this population with preliminary research supporting its effectiveness (Ruff & Mackenzie, 2009). A recent pilot study was completed with undergraduate speech pathology students in Perth, Western Australia. Students participated in wellness discussions, mindfulness activities and created a wellness plan (Lewis et al., 2019). Participants reported having new strategies to manage procrastination and stress, and welcomed the opportunity to discuss mental health management in a safe and supportive environment (Lewis et al., 2019).
Despite calls to include mindfulness programs in the training of health students to help them manage depression, anxiety and stress, to date, there has been no review of the literature on how to best achieve including and delivering this training to health students. This scoping review examined the effectiveness of mindfulness-based interventions for health students delivered at tertiary or post-secondary institutions (university or college) and how these programs were implemented with this population. The review will explore intervention characteristics, recruitment and retention and the most effective strategies in implementing mindfulness-based interventions to improve student well-being. This research will enhance understanding of the impact of mindfulness practice for health students and the most effective principles and strategies in implementing these practices to improve student well-being.
Methods
A scoping review was conducted following a systematic process for conducting scoping reviews as outlined by Arksey & O'Malley, (2005) and the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) (Tricco et al., 2018). Given the large heterogeneity of study designs and quality of the studies investigating the effectiveness of mindfulness-based interventions with health students, a scoping review was deemed more appropriate to summarise the current literature than a systematic review (Arksey & O'Malley, 2005). The five-step process by Arksey and O’Malley (2005) was used to provide structure to the process and improve the transparency of the findings. The five steps were: (1) identifying the research question; (2) identifying the relevant studies; (3) study selection; and (4) charting the data; (5) collating, summarizing and reporting the results.
Eligibility and Study Selection
Title and abstract screening were doubled-screened by the research team after duplicates were removed for eligibility. Full-text articles were obtained for articles that met eligibility criteria based on their title and abstract. Papers were included if the participants in the study were enrolled in a tertiary or higher education institution in a health-related course (university or college, graduate or undergraduate) and completed a mindfulness-based intervention with three or more sessions within the program. The health-related programs included in the search were medicine, nursing, pharmacy and allied health courses. The mindfulness-based intervention could be provided in any modality and was not restricted to being conducted on a university campus. Only studies that included one or more outcome measures for anxiety, stress and/or depression were included, and inclusion of a mindfulness-awareness measure was optional. Other disciplines, non-students, exercise based or non-intervention studies were excluded. All team members completed a review of the full-text articles that met the eligibility criteria. Any disagreements throughout the study selection process were resolved through discussion and consensus.
Search Strategy
A systematic and comprehensive search of three databases (PsychINFO, Medline and Embase) was conducted. Each database thesaurus (subject headings and related terms) was checked to generate additional search terms. The search strategy was limited to articles published from 2009 to 2020, written in English and available online through university databases. Articles were limited from 2009 to 2020 given the significant proliferation of mindfulness-based intervention studies over the past 10 years (Goldberg et al., 2017). A free-text search was then conducted within the databases for literature published in the previous 12 months. The reference lists of all articles were searched for additional studies. All citations were exported to a reference manager. See supplementary materials for a full search strategy example.
Data Collection
A descriptive-analytical methodology was utilized to chart data (Arksey & O'Malley, 2005). The authors jointly developed a data chart extraction table to extract data. Data were extracted independently by the authors and results were discussed and continuously updated through an iterative process. The following data were extracted and collated: (1) author/s, year, journal, country of origin, paper type; (2) summary; (3) participant: demographics, enrollment (undergraduate/postgraduate), course discipline, cohort (e.g. first-year, final-year); (4) study design; (5) intervention style (face-to-face, web-based, self-guided, home practice); (6) intervention design (dosage and duration); (7) recruitment and retention, (8) intervention approach; (9) outcome measures (e.g. depression, anxiety, stress, understanding of mindfulness); (10) study findings; and (11) determination of inclusion with rationale.
To confirm data extraction reliability between reviewers, the research team independently extracted data from the final 24 papers. Disagreement was resolved through discussion and consensus by all the authors.
Results
Study Selection
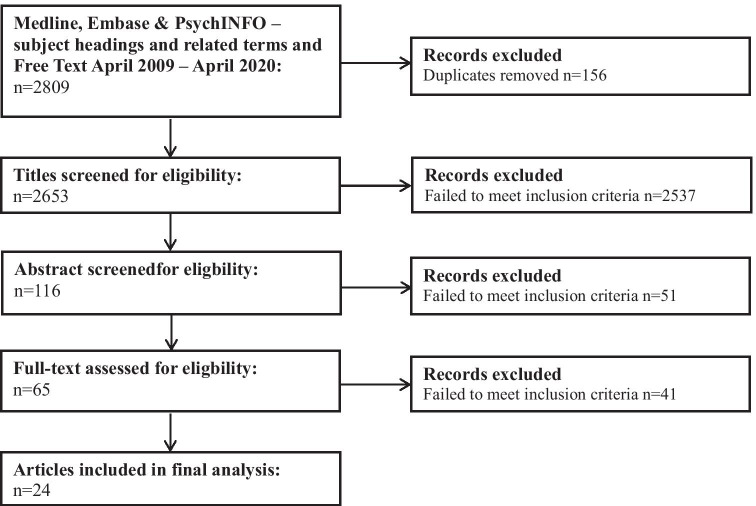
The initial search from the databases yielded 2809 articles, of which 156 were duplicates, Title screening from the remaining 2653 articles resulted in 2537 articles being excluded. From these 116 articles, abstract screening excluded a further 51 articles. The remaining 65 papers progressed to full-text review. Of these papers, 41 papers were excluded after the full-text review. A total of 24 papers met eligibility criteria and were included for data extraction, collation, summarising and reporting. Figure 1 represents the process undertaken for article selection.
Fig. 1.
Flow diagram for study selection
Study Location and Participants
A summary of the results is outlined in Table 1. The results from this review found that the majority of studies were from the United States (n = 12) and Europe (n = 5), and the remaining were from Australia and Asia (n = 6) and Brazil (n = 1). Most studies were conducted with students from medicine (n = 10), followed by combined health sciences (n = 5), nursing (n = 3), psychology (n = 3), speech pathology (n = 1), pharmacy (n = 1) and social work (n = 1). The ‘combined health science’ category included participants completing mixed medical and dental courses, nursing, occupational therapy, physical therapy or physiotherapy, counselling, education and sociology. Participants in the studies were at various levels of study including undergraduate (n = 7) and postgraduate (n = 6). Four studies included both undergraduate and postgraduate students, with six studies not reporting the level of study for their participants. Most studies (n = 21) had a higher ratio of female to male, with four studies having excluded male participants.
Table 1.
Population characteristics
| Author/s and year | Location | Participants and gender | Mean age (years) | Course | Enrolment |
|---|---|---|---|---|---|
| Barbosa et al. (2013) | USA |
Experimental: Female: n = 12 (72.3%) Male: n = 1 (27.7%) Control: Female: n = 14 (93.3%) Male: n = 1 (6.7%) |
X = 26.6 |
Experimental group: 2 Podiatric medicine 3 Physician assistant 3 Physical therapy 2 Occupational therapy 3 Nursing Control group: 5 Podiatric medicine 2 Physician assistant 4 Physical therapy 3 Occupational therapy 1 Nursing |
Postgraduate |
| Beck et al. (2017) | USA |
Experimental: n = 20 Control: n = 17 Female (100%) |
X = 21.16 |
Undergraduate Communication Sciences and Disorders (CSD) Graduate speech language pathology (SLP) program |
Experimental: - 9 postgraduate students - 11 undergraduates (7 seniors, 1 junior, 1 sophomore, 2 freshmen) Control: - 9 postgraduate students - 8 undergraduates (3 seniors, 2 juniors, 3 freshmen) |
| Burgstahler and Stenson (2019) | USA |
Cohort Females: n = 48 (71.6%) Males: n = 19 (28.4%) |
X = 20.0 | Pre-healthcare | Undergraduate |
| Call et al. (2014) | USA |
Hatha yoga: Female: n = 29 MBSR body scan: Female: n = 27 Female (100%) |
X = 22.73 | Introductory and advanced psychology | Undergraduate |
| de Vibe et al. (2013) | Norway |
Female: n = 219 (76.0%) Male: n = 69 (24.0%) |
X = 24 | Medicine and psychology | Unknown course level |
| Dyrbye et al. (2017) | USA |
Cohort 1: Female: n = 28 (58.3%) Male: n = 20 (41.7%) Cohort 2: Female: n = 26 (55.3%) Male: n = 21 (44.7%) |
Mode < 25 | Medicine |
Postgraduate - First year (across two cohorts) |
| Erogul et al. (2014) | USA |
Experimental: Female: n = 14 (46.7%) Male: n = 16 (53.3%) Control: Female: n = 12 (42.9%) Male: n = 16 (57.1%) |
X = 23.5 | Medicine |
Postgraduate - First year |
| Greeson et al. (2015) | USA |
Female: n = 29 (66.6%) Male: n = 15 (33.4%) |
Not stated | Medicine and scientific physicians (MD/PhD) |
Postgraduate - First year: 33 - Second year: 1 - Third year: 3 - Fourth year: 5 MD/PhD: 2 |
| Hassed et al. (2009) | Australia |
Female: n = 85 (57.4%) Male: n = 63 (42.6%) |
X = 18.77 | Medicine | Undergraduate |
| Kang et al. (2009) | Korea | Female: n = 21 (100% female) |
Experimental: X = 22.69 Control: X = 22.25 |
Nursing |
Unknown course level Juniors and seniors |
| Kuhlmann et al. (2016) | Germany |
Female: n = 67 (88.8%) Male: n = 13 (11.2%) |
X = 23.39 | Medicine and dentistry | Unknown course level |
| Lemay et al. (2019) | USA |
Female: n = 13 (76.5%) Male: n = 4 (23.5%) |
X = 20.17 |
Doctor of Pharmacy = 9 Other courses with ‘less rigourous demands’: 8 |
Post-graduate for Pharmacy students (experimental) Undergraduate for others (comparison) – both received intervention |
| Neto et al. (2020) | Brazil |
Female: n = 71 (50.4%) Male: n = 70 (49.6%) |
Experimenta:l X = 18.87 Control: M = 19.07 |
Medicine | Undergraduate |
| Newsome et al. (2012) | USA |
Female: n = 27 (87.1%) Male: n = 4 (12.9%) |
X = 29.26 | Helping professions (e.g. counselling, psychology, education, family-child science, nursing, sociology, communications, government, and physical therapy) |
Postgraduate 12 Undergraduate 19 |
| Phang et al. (2016) | Malaysia |
Females: n = 84 (62.2%) Males: n = 51 (37.8%) |
X = 22.23 | Medicine | Unknown course level |
| Phang et al. (2015) | Malaysia |
Experimental: Female n = 26 (70.3%) Male: n = 11 (29.7%) Control: Female: n = 31 (81.6%) Male: n = 7 (18.4%) |
X = 21.4 | Medicine |
Unknown course level Year one to three of studies |
| Rimes and Wingrove (2011) | UK | Female: n = 20 (100% female) | Not stated | Clinical psychology |
Postgraduate Trainees participating in doctoral training course - First year: 9 - Second year: 6 - Third year: 5 |
| Roulston et al. (2018) | UK |
Experimental: Female: n = 14 (93.3%) Male: n = 1 (6.7%) Control: Female: n = 11 (73.3%) Male: n = 4 (26.7%) |
X = 29 | Social work | Undergraduate |
| Shearer et al. (2016) | Korea |
Female: n = 42 (56.8%) Male: n = 32 (43.2%) |
Not stated | Psychology | Undergraduate |
| Song and Lindquist (2015) | USA |
Experimental: Female: n = 17 (81.0%) Male: n = 4 (19.0%) Control: Female: n = 19 (82.6%) Male: n = 4 (17.4%) |
X = 19 | Nursing | Undergraduate |
| Spadaro and Hunker (2016) | USA |
n = 26 Gender not stated |
Not stated | Nursing |
Postgraduate Undergraduate |
| Szuster et al. (2020) | USA |
n = 15 Gender not stated |
Not stated | Medicine | Postgraduate |
| van Dijk et al. (2017) | Netherlands |
Experimental: Female: n = 60 (83.3%) Male: n = 12 (16.7%) Control: Female: n = 71 (83.5%) Male: n = 14 (16.5%) |
Experimental: X = 23.7 Control: X = 23.3 |
Medicine | Undergraduate |
| Warnecke et al. (2011) | Australia |
Experimental: Female: n = 23 (74.2%) Male: n = 8 (25.8%) Control: Female: n = 19 (55.9%) Male: n = 15 (44.1%) |
X = 23.92 | Medicine |
Unknown course level - Final 2 years |
Study Design
Eleven of the 24 studies included were single cohort studies, seven randomized controlled trials and six control studies.
Recruitment
Many of the studies experienced difficulty recruiting and had lower than expected participant numbers (Barbosa et al., 2013; Dyrbye et al., 2017; Greeson et al., 2015; Kang et al., 2009). Small sample sizes were reported as a limitation in several studies (Barbosa et al., 2013; Kuhlmann et al., 2016; Phang et al., 2015; Rimes & Wingrove, 2011; Song & Lindquist, 2015; Spadaro & Hunker, 2016; Warnecke et al., 2011) or they reported that the study did not have adequate power (Beck et al., 2017). Various methods of recruitment were utilized. Ten of studies reported invitation emails, information sessions, social media invitations and flyers to recruit participants (Barbosa et al., 2013; Beck et al., 2017; Burgstahler & Stenson, 2019; Call et al., 2014; Erogul et al., 2014; Greeson et al., 2015; Newsome et al., 2012; Phang et al., 2015; Spadaro & Hunker, 2016; Warnecke et al., 2011). Four of the studies approached participants as part of the unit or course (Burgstahler & Stenson, 2019; Dyrbye et al., 2017; Hassed et al., 2009; Neto et al., 2020). Participants in one study were given a $50 voucher to participate (de Vibe et al, 2013) or a nominal amount (Kang et al, 2009). The remaining studies did not report recruitment methodology. Timetabling and time restraints were reported as contributing factors for poor recruitment in one study (Barbosa et al., 2013). A summary of the recruitment strategies is outlined in Table 2.
Table 2.
Recruitment and retention
| Author/s and year | Recruitment and retention |
|---|---|
| Barbosa et al. (2013) |
General invitation email sent to a student population of about 1300 students describing study and offering two MBSR informational sessions 33 students attended informational sessions and screening surveys were administered to all prospective student participants |
| Beck et al. (2017) | Voluntary from information session at special interest groups. Recruitment script also read to first year graduate speech-language pathology students by a staff member during the first professional seminar meeting |
| Burgstahler and Stenson (2019) | Participants were recruited from two courses required for all pre-healthcare students |
| Call et al. (2014) |
Three mechanisms: (1) flyers posted in the psychology building, (2) mass testing for Introductory Psychology students, and (3) direct sign up for pretest survey for Introductory Psychology students Interested students asked to complete the Penn State Worry Questionnaire (PSWQ) and those reporting scores of 45 or higher were invited to participate in the study |
| de Vibe et al. (2013) | Participants were recruited by the researchers providing information in class. This was then followed up with an email inviting participants to visit a website for more information and to sign up to study. Students received book vouchers after they completed the T2 (follow-up) data collection point |
| Dyrbye et al. (2017) | All first-year students who matriculated at Mayo Clinic School of Medicine in 2014 (cohort 1) and 2015 (cohort 2) participated in the longitudinal mindfulness-based stress management course as a required part of the curriculum |
| Erogul et al. (2014) |
Of 185 first year med students, 42 approached for control (12 refused), 39 approached for intervention group (10 refused, 1 dropped out) Participants selected at random using a random number generator to select students who had been numbered according to their alphabetical order in the class This process blindly allocated 30 students to control and 30 to intervention. After random allocation, students were asked by email to consent to participate in the group to which they had been assigned. A proportion of students declined to participate and were replaced by other students selected at random from the remaining members of the class on a rolling basis until 30 control and 29 study participants was achieved. All participants gave written consent and were paid $50 at the conclusion of the data gathering |
| Greeson et al. (2015) | Recruited through electronic flyer and email announcements, in-class announcements by group facilitators. Initially, emails directed at first years only then extended to all years to provide equal opportunity; 44 volunteered, 40 attended first workshop, 36 completed the workshop and post-survey. Courses ran in 3 years (2007 n = 6, 2009 n = 15, 2011 n = 23) |
| Hassed et al. (2009) | Of the eligible student cohort of 270 students, 239 completed questionnaires at time point 1 and 162 at time point 2. Although 155 students completed questionnaires at both time point 1 and 2, outliers were detected in the data on mindfulness practice for seven of those students and were excluded, leaving a sample of 148. Program delivered to a whole cohort as an integrated part of core-curriculum. Participation in the study was voluntary |
| Kang et al. (2009) | Not specified. Study noted that ‘Students were recruited and notified of the purpose of the study from March 10 to 28, 2006’. Gift of ‘nominal’ value provided to participants in the study |
| Kuhlmann et al. (2016) | Voluntary extracurricular activity and students were introduced to the study design and the opportunity of participation at lectures and by written information. At the post-intervention assessment time point, 50€ vouchers were raffled among the participants as an acknowledgment of their participation. As a motivating incentive the participants of the control group received a 20€ voucher. Because of the low response rate, everyone who participated in the follow-up assessment received a 20€ voucher. Recruitment commenced, but was terminated before full sampling had been completed. A total of 228 signed informed consent, 80% (n = 183) completed baseline assessment and of this sample 61% (n = 112) returned post-measures. Due to an error in the online version of the baseline assessment, 13 participants had to be excluded from the evaluation. One participant dropped out before allocation to the study groups |
| Lemay et al. (2019) | Recruitment was conducted via an electronic flyer posted on the university and student social media pages and paper flyers posted throughout the campus library. 20 students recruited and 17 completed the study |
| Neto et al. (2020) | Students enrolled in a required course named “Introduction to University Life,” administered as a 2 hr weekly class over a period of 15 weeks. Allocated into two groups: an intervention group and a control group. 171 students recruited and 141 completed in analysis |
| Newsome et al. (2012) | Group members were recruited via postings and in-group announcements publicizing a group on self-care for helping professionals. They earned academic credit for participating in the group |
| Phang et al. (2016) | Participants were informed that the program would help them to cope with stress as well as further enhance their knowledge and experience in psychiatry. The intervention was embedded in a psychiatric posting curriculum. Due to ethical reasons, 31% of the participants with high depression (DASS-D > 28) and anxiety (DASS-A > 20) scores (identified with depression, anxiety and stress scale by Lovibond and Lovibond 1995) were given information on places to get counseling if they deemed it was necessary. However, they were not excluded from the study. Out of 135 students who participated in the program, 130 completed the program (attended at least three out of four sessions—75% attendance). Missing data was found in seven (5%) of the participants (including three who did not complete the program) |
| Phang et al. (2015) |
The intervention program was introduced as an extracurricular activity to students through emails, Facebook and blog under the name ‘Mindful-Gym: A Stress Management Program for Medical Students’. Those who expressed interest to participate in the program were included in the study; participation was on voluntary basis. Potential participants were informed that they were expected to attend 80% of all sessions in the program and to spend 3 to5 minutes daily to practice what they would learn from the program; else they would be excluded from the study. Broad inclusion criteria were intended for better generalizability of the effects of the program. 78 consented to participate, then 3 could not participate (low drop out) ‘First come, first served’ recruitment method |
| Rimes and Wingrove (2011) |
Invitation to participate Seven participants attended all eight sessions, six attended seven sessions, five attended six sessions, and two attended five sessions |
| Roulston et al. (2018) | Only students registered on the Bachelor of Social Work (BSW) degree were eligible to volunteer to attend of the six-week mindfulness course. Based on the nature of the course, 15 students could register to attend, and those expressing an interest were placed on a reserve list |
| Shearer et al. (2016) | 74 undergraduate students recruited from psychology courses at the University of Pennsylvania who consented to participate in the study in exchange for extra credit in a psychology course |
| Song and Lindquist (2015) | Flyers with inclusion criteria posted on website and community board in nursing school for 480 eligible undergrad nursing students were offered, 50 respondents for participation, 44 participated |
| Spadaro and Hunker (2016) | Invitation to participate sent via institutional email to all undergrad and graduate students in nursing study programs by program coordinator. Interested students replied by email |
| Szuster et al. (2020) | The program was integrated into the regular didactic curriculum for postgraduate first year non-surgical training programs |
| van Dijk et al. (2017) | Of 232 eligible students, 167 students (72%) participated. Informed the students about the trial during classroom teaching in the fifth month of their clerkships. Interested students left their email address and received an information leaflet by email within 2 days, thus enabling them to decide to participate (or not) outside of the teaching environment free of any external pressure. Students did not receive any incentives for participation. At 20 months post intervention, 67 of 83 MBSR students (81%) and 58 of 84 CAU students (69%) had remained in the study |
| Warnecke et al. (2011) |
From three schools, participants recruited via a face-to-face information session and an email inviting participation in the trial. Participants provided written consent. Of the 66 participants recruited, 32 were randomized to the treatment arm and 34 to the control arm or withdrew from trial after it began. The mindfulness intervention CD was given to the control group at the end of the 8-week trial period as an incentive to remain in the trial Only 64% (20⁄31) of participants completed this record of practice over the 8 weeks of the intervention |
Retention
Two studies provided course credit to participants (Newsome et al., 2012; Shearer et al., 2016), while three papers incorporated mindfulness as part of the curriculum to improve retention rates (Call et al., 2014; Hassed et al., 2009). The study that included the largest sample of participants (n = 288) used a financial reward at the final data collection point (de Vibe et al., 2013). This study reported the highest retention rate when participants were followed up after 6 years (de Vibe et al., 2013). One study raffled for a voucher to participants and due to low response rates, provided a 20 Euro voucher for all follow-up assessments (Kuhlmann et al., 2016). Another study informed participants that learning the techniques to cope with stress and improve mindful practice would assist in their professional careers, which attracted a sample of 135 participants (Phang et al., 2016). A summary of the retention strategies is outlined in Table 2.
Intervention
Intervention programs were delivered in a variety of formats. A summary of the intervention programs is outlined in Table 3. The length of program varied from three weeks to a full semester, with ten studies running programs for 8-week duration. Twenty of the programs were delivered with at least some face-to-face sessions, and 14 of these included self-guided programs which followed initial face-to-face sessions where participants were taught the principles of the practice of mindfulness.
Table 3.
Intervention characteristics
| Author/s and year | Study design | Intervention style | Intervention | Outcome measures | Effectiveness of intervention |
|---|---|---|---|---|---|
| Barbosa et al. (2013) | Controlled before/after trial | Face-to-face and self-guided |
MBSR (Jon Kabat-Zinn) 1 × week × 8 weeks 2.5 h per week 1 × 8 h in 6th week |
Anxiety, stress, mindfulness, physician empathy | Significant decrease in anxiety and increase in empathy at weeks 8 and 11 compared with baseline |
| Beck et al. (2017) | Controlled before/after trial | Face-to-face |
Mindfulness procedure (Beck and Verticchio, 2014a) 1 × week × 7 weeks ~ 20 min |
Stress, mindfulness, self-compassion | Decreased perceived stress, negative aspects of perfectionism and biological markers of stress. Increase in self compassion |
| Burgstahler and Stenson (2019) | Single cohort, before/after trial | Online |
Mindfulness meditation intervention (Palouse online MBSR Meditation) 5–12 min practice per day × 8 weeks |
Anxiety, stress, mindfulness, heart rate variability | Significant increase in mindfulness. Significant decrease in stress and anxiety. Greater changes with longer duration of mindfulness sessions |
| Call et al. (2014) | Controlled before/after trial | Pre-recorded instructor/facilitator |
Hatha yoga and body scan (pre-recorded; narrated by Jon Kabat-Zinn) 3 × weeks for 3 weeks 45-min sessions |
Depression, anxiety, stress, mindfulness | Significantly greater reduction in anxiety and stress in the intervention group compared with controls. No significant difference in post-intervention mindfulness |
| de Vibe et al. (2013) | Controlled before/after trial | Pre-recorded instructor/facilitator |
MBSR program (based on Kabat-Zinn) 7 weeks 2.5 h per session |
Stress, mindfulness, mental distress | Moderate effect on mental distress and a small effect on subjective wellbeing and mindfulness. Higher level of programme attendance predictive of these changes. Significant results only for females |
| Dyrbye et al. (2017) | Single cohort, before/after trial | Face-to-face |
Stress Management and Resilience Training (SMART) program 10–12 h spread across a semester |
Stress, empathy, medical outcomes, resilience, happiness |
No apparent significant effect of program Mean mental quality of life and happiness declined and stress increased across the program |
| Erogul et al. (2014) | Randomised controlled trial | Face-to-face and self-guided |
MBSR 1 × week for 8 weeks 75 min per session |
Stress, mindfulness, compassion, resilience | Significant increase in self-compassion and reduction in perceived stress in the intervention group at the conclusion of the trial. Self-compassion changes maintained 6 months post-study but not perceived stress. No significant change in resilience after the intervention |
| Greeson et al. (2015) | Single cohort, before/after trial | Face-to-face and self-guided |
Mind–body medicine: a skill building and self-care workshop 1 × week for 4 weeks 1.5 h per session |
Stress, mindfulness, qualitative evaluation | Decrease in perceived stress and increase in mindfulness |
| Hassed et al. (2009) | Single cohort, before/after trial | Face-to-face and self-guided |
Health Enhancement Program (HEP): Essence and SRP: mindfulness-based stress management and cognitive therapy program (Hassed, 2002) 1 × week for 6 weeks 2-h duration |
Depression, anxiety, distress, quality of life | Significant improvement in depression and hostility subscales, but not in the anxiety subscale |
| Kang et al. (2009) | Controlled before/after trial | Face-to-face |
Mindfulness meditation 1 × week for 8 weeks 1.5 h per session |
Depression, anxiety, stress | Significant improvement in anxiety and stress scores but not depression in intervention group when compared with control group |
| Kuhlmann et al. (2016) | Single cohort, before/after trial | Face-to-face |
Yoga and meditation intervention 1 × week × 5 weeks 1.5 h per session |
Anxiety, stress, mindfulness | Significant decrease in stress and anxiety and significant increase in mindfulness |
| Lemay et al. (2019) | Randomised controlled trial | Face-to-face and self-guided |
MediMind: combination mindfulness and CBT 1 × week × 5 weeks 1.5 h per session |
Depression, anxiety, stress | No significant interaction effects on any of the outcome measures (high dropout rate of participants limited findings) |
| Neto et al. (2020) | Randomised controlled trial |
Face-to-face and self-guided 6 weeks |
Mindfulness course (Kabat-Zinn) 1 × week for 6 weeks 2-hsessions |
Depression, mindfulness, quality of life, religiousness | No significant differences between intervention and control groups in any of the outcome measures |
| Newsome et al. (2012) | Single cohort, before/after trial | Face-to-face and self-guided |
Qigong, yoga, sitting and walking meditation, body scan 1 × week for 8 weeks 1.5 h |
Anxiety, stress, mindfulness, empathy | Significant decrease in perceived stress. Significant increase in mindfulness and self-compassion. Effects lasted 4 weeks post-intervention |
| Phang et al. (2016) | Single cohort, before/after trial | Face-to-face and self-guided |
Mindfulness Based Cognitive Training (adapted from MBSR) 1 × week for 4 weeks 2 h per session |
Stress, mindfulness, general health, course feedback | Significant reduction in perceived stress and significant increase in mindfulness |
| Phang et al. (2015) | Single cohort, before/after trial | Face-to-face and self-guided |
Mindfulness Based Stress Management (MBSM) 1 × week for 5 weeks 2-h sessions |
Stress, mindfulness, general health, course feedback | Significant improvements in mindfulness, perceived stress, mental distress and self-efficacy at one week post intervention. At six months post intervention higher reported self-efficacy, but no difference in other outcome measures |
| Rimes and Wingrove (2011) | Single cohort, before/after trial | Face-to-face and self-guided |
Mindfulness Based Cognitive Therapy (MBCT) Based on Segal et al. (2002) 1 × week × 8 weeks Duration not specified |
Depression, stress, mindfulness, empathy, | Significant increase in self-compassion and mindfulness. More frequent home practice was associated with larger decreases in stress, anxiety and rumination and larger increases in empathy |
| Roulston et al. (2018) | Controlled before/after trial | Face-to-face and self-guided |
MBSR (Kabat-Zinn) 1 × week for 6 weeks 2 h per session |
Stress, resilience, course feedback | Significant changes in scores for well-being, stress and resilience for the intervention group, but not for the control group |
| Shearer et al. (2016) | Randomised controlled trial | Face-to-face |
MBSR (Kabat-Zinn) Dog therapy (active control) 1 × week for 4 weeks 1 h per session |
Depression, anxiety, mindfulness, heart reaction (ECG) |
Mindfulness intervention group showed significantly lower state anxiety than other groups. Dog therapy less anxiety than control Both dog therapy and mindfulness group had significantly less dysphoria than control. Mindfulness group exhibited more adaptation to physiological stress response than both other groups |
| Song and Lindquist (2015) | Randomised controlled trial | Face-to-face and self-guided |
Mindfulness Meditation 1 × week for 8 weeks 2 h per session |
Depression, anxiety, stress, mindfulness | Significantly greater decrease in depression, anxiety and stress. Significantly greater increase in mindfulness |
| Spadaro and Hunker (2016) | Single cohort, before/after trial | Online and online discussion forum |
Adapted MBSR 1 × week for 8 weeks Duration not specified |
Depression, anxiety, stress, cognition | Significant reduction in stress. Decreasing trend for anxiety |
| Szuster et al. (2020) | Single cohort, before/after trial | Face-to-face and self-guided |
Adapted MBSR Every 2 weeks over 8 weeks (4 sessions) 2 h per session |
Depression, anxiety, professional satisfaction and course engagement | Significant reduction in burnout. Depression and anxiety screening scores trended towards improvement. Not maintained after 3 months (returned to pre-intervention levels) |
| van Dijk et al. (2017) | Randomised controlled trial | Face-to-face and self-guided |
MBSR (Kabat-Zinn) 1 × week for 8 weeks 2 h per session |
Mindfulness, empathy, psychological distress, life satisfaction | Small reduction in psychological distress and dysfunctional cognitions and a moderate increase in positive mental health, life satisfaction and mindfulness skill at 20-month follow-up. No significant effect on empathy |
| Warnecke et al. (2011) | Randomised controlled trial | Self-guided (recorded content) |
MBSR (Audio CD 'mindfulness') Home practice Everyday for 8 weeks 30 min |
Depression, anxiety, stress, mindfulness | Significant reductions in scores on Perceived Stress Scale (PSS) and anxiety component of the Depression, Anxiety and Stress Scale (DASS). Borderline significant effect on the stress component of DASS. Maintained at 8 weeks post-trial |
Mindfulness-Based Stress Reduction (MBSR), adapted MBSR or Mindfulness-Based Stillness Meditation (MBSM) were the most common interventions used, utilized in 11 of the interventions (Barbosa et al., 2013; Burgstahler & Stenson, 2019; de Vibe et al., 2013; Erogul et al., 2014; Neto et al., 2020; Phang et al., 2015; Roulston et al., 2018; Shearer et al., 2016; Spadaro & Hunker, 2016; van Dijk et al., 2017; Warnecke et al., 2011). Two studies (Phang et al., 2016; Rimes & Wingrove, 2011) incorporated mindfulness-based cognitive therapy (MBCT) while the remainder of the studies evaluated other interventions including yoga and body scanning (Call et al., 2014; Lemay et al., 2019; Newsome et al., 2012), combined mindfulness and cognitive behavioral therapy (Hassed et al., 2009; Kuhlmann et al., 2016), mindfulness meditation (Beck et al., 2017; Kang et al., 2009; Song & Lindquist, 2015) and stress and resilience training (Dyrbye et al., 2017; Greeson et al., 2015).
Outcome Measures
Only two studies (Hassed et al., 2009; Song & Lindquist, 2015) found a statistically significant decrease in measures of depression following mindfulness intervention, compared to seven papers that found no statistically significant differences (Kang et al., 2009; Kuhlmann et al., 2016; Neto et al., 2020; Rimes & Wingrove, 2011; Spadaro & Hunker, 2016; van Dijk et al., 2017; Warnecke et al., 2011). Nine studies found a statistically significant decrease in anxiety (Barbosa et al., 2013; Burgstahler & Stenson, 2019; Call et al., 2014; Kang et al., 2009; Lemay et al., 2019; Shearer et al., 2016; Song & Lindquist, 2015; van Dijk et al., 2017; Warnecke et al., 2011), and four studies found no statistically significant reduction in anxiety following mindfulness intervention (Hassed et al., 2009; Kuhlmann et al., 2016; Rimes & Wingrove, 2011; Spadaro & Hunker, 2016). Fifteen studies found a statistically significant decrease in stress (Burgstahler & Stenson, 2019; Call et al., 2014; de Vibe et al., 2013; Dyrbye et al., 2017; Erogul et al., 2014; Greeson et al., 2015; Kang et al., 2009; Lemay et al., 2019; Newsome et al., 2012; Phang et al., 2016; Phang et al., 2015; Roulston et al., 2018; Song & Lindquist, 2015; Spadaro & Hunker, 2016; Warnecke et al., 2011), while one paper reported a statistically significant reduction in psychological distress (van Dijk et al., 2017). Only one study reported no statistically significant decrease in stress (Kuhlmann et al., 2016) following mindfulness-based therapy. One study reported a statistically significant decrease for female participants only (Dyrbye et al., 2017), while another found statistically significant differences in stress levels for first-year psychology students only (Rimes & Wingrove, 2011).
Discussion
This scoping review identified 24 papers that used mindfulness-based intervention (MBI) approaches with students enrolled in tertiary or higher education institutions in a health-related course. These papers included results from nine countries, a wide range of health related courses, students at different levels of education, and reported varying recruitment and retention strategies, interventions and outcomes. The most common MBI approaches were based on mindfulness-based stress reduction (MBSR) principles (Kabat-Zinn, 1982). Various methods of delivery were utilized, including short courses and online delivery. Virtual instruction was considered a viable method of delivery when face-to-face sessions may not be available. Findings from this review suggest that despite differing intervention approaches and delivery, most had a positive effect on student’s mental health well-being.
These findings should be interpreted with some caution as weaknesses were identified in a few studies. While mindfulness interventions with health students seem to work, a number of studies reported that recruitment was voluntary, thus by nature, the participants were more likely to be more motivated to engage in mindfulness interventions. Moreover, this could also suggest that the students who would benefit the most from mindfulness-based interventions, may not have the motivation to participate, thus the impact of these interventions may be diluted. It was also noted in some of the studies that participants in most need of MBI were more likely to drop out of the program, reinforcing the potential benefits of MBI for people with significant mental health issues.
Study Location and Participants
All participants within the studies selected were enrolled in health professional university courses. A broad range of health professions were represented in the included studies, however, medical students comprised the largest group compared to any other single profession. Therefore, caution should be used in interpreting the results when generalizing to students from other health professions where factors contributing to increased anxiety, stress and depression or motivation to engage with mindfulness programs may differ.
Several of the studies included in this review noted an imbalance in the gender of the cohort of students recruited with some authors expressing concerns about this being a potential limitation of generalizing to the greater population. Gender-specific effects of mindfulness have been examined in some studies with a reported increased effect for female participants in reducing stress (de Vibe et al., 2013). Given many health professions have a greater proportion of females, with up to 97.5% of speech pathologists and 90.6% of occupational therapists being female, this may be less of an issue for these professions compared to professions with a higher proportion of males, such as medicine with 44% females and physiotherapy with 65.6% females (Australian Health Practitioner Regulation Agency, 2020; Speech Pathology Australia, 2015).
It is also important to note that 45% of studies included in this review were conducted in institutions within the United States (US). It is unclear as to whether students from this region may respond differently to mindfulness programs compared to students enrolled in other countries, or whether the educational system within the US may contribute to different levels of stress, anxiety or depression than in other parts of the world.
Engagement
Recruitment, retention and engagement were reported as a challenge in a number of the studies, and many studies included smaller sample sizes than planned. Despite multiple methods of recruitment, including emails, information sessions, social media and flyers, no method was identified as a superior method of recruitment. This highlights a broader challenge with this demographic in how to engage health students to prioritize activities to improve mental health given the high time demands and reluctance to seek proactive assistance.
Participants were recruited through voluntary channels, as an extracurricular activity, embedded within course content, or provided as an online or take-home task. This strategy may have resulted in the recruitment of participants who demonstrated higher motivation to undertake mindfulness training or, as authors of one study suggested, were more primed to focus on personal difficulties (Carpenter et al., 2019). There remains a lack of evidence to ascertain whether mindfulness programs offered as an extracurricular activity are more effective than embedded within health curricula.
From this review, the most successful strategy to encourage participation and engagement is embedding mindfulness-based intervention within the curriculum; however, this presents numerable challenges for educators and course designers in the presence of an already saturated curriculum in these courses. Another strategy that demonstrated some utility was highlighting to students the importance of mindfulness-based techniques and strategies to assist not only during tertiary studies but as lifelong skills as a future health professional (Newsome et al., 2012).
Recruitment and retention were commonly noted as challenges across a number of studies. While traditional extrinsic strategies such as gifts or prizes seemed to improve recruitment and retention of participants appeared to have an impact, linking the importance of managing the participant’s own mental health to the impact of delivering high-quality care to their clients and patients was also an effective strategy. Interestingly, the experience of the person who provides the MBI may be an important factor, but this was not reviewed exclusively, and a wide variety of people delivered the MBIs within this study.
Limitations and Future Research
Analysis of the methodological quality of the articles was not completed as this is a not key component of scoping reviews. Further, the heterogeneous populations, intervention designs and delivery methods, as well as a lack of standardized outcome measures, limited the ability to conduct a systematic and meta-analysis of the results. While these are common features of scoping reviews, the findings outlined in this paper should be interpreted with consideration of these limitations. Finally, the variability in study designs needs to be acknowledged, which made it difficult to draw definitive conclusions about the outcomes.
Given the majority of the research to date with health students has been completed with medical students, a large gap in research remains for investigating the impact of MBI with students from other health professions, particularly the allied health professions. While there appears to be more research completed with females than males, no gender effects have been reported. Future research could investigate the influence of gender on the effectiveness and use of MBI in this population. More rigorous randomized control trials and a systematic review over the history of mindfulness interventions is recommended to investigate effective engagement and retention in more detail, and comparing mode of delivery of MBI for allied health students.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to acknowledge Rosemary Crossdale’s contribution to this review. The authors received funding from a Curtin University Learning and Teaching grant to conduct this review. The authors declare no financial interest in any interventions included within this review.
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Arksey H, O'Malley L. Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, Demyttenaere K, Ebert DD, Green JG, Hasking P. WHO World Mental Health Surveys International College Student Project: Prevalence and distribution of mental disorders. Journal of Abnormal Psychology. 2018;127(7):623. doi: 10.1037/abn0000362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Health Practitioner Regulation Agency. (2020). Annual report 2019/2020.
- Barbosa P, Raymond G, Zlotnick C, Wilk J, Toomey R, III, Mitchell J., III Mindfulness-based stress reduction training is associated with greater empathy and reduced anxiety for graduate healthcare students. Education for Health: Change in Learning & Practice. 2013;26(1):9–14. doi: 10.4103/1357-6283.112794. [DOI] [PubMed] [Google Scholar]
- Beck AR, Verticchio H, Seeman S, Milliken E, Schaab H. A mindfulness practice for communication sciences and disorders undergraduate and speech language pathology graduate students: effects on stress self compassion, and perfectionism. American Journal of Speech Language Pathology. 2017;26(3):893–907. doi: 10.1044/2017_AJSLP-16-0172. [DOI] [PubMed] [Google Scholar]
- Burgstahler MS, Stenson MC. Effects of guided mindfulness meditation on anxiety and stress in a pre-healthcare college student population: A pilot study. Journal of American College Health. 2019;68(6):666–672. doi: 10.1080/07448481.2019.1590371. [DOI] [PubMed] [Google Scholar]
- Call D, Miron L, Orcutt H. Effectiveness of brief mindfulness techniques in reducing symptoms of anxiety and stress. Mindfulness. 2014;5(6):658–668. doi: 10.1007/s12671-013-0218-6. [DOI] [Google Scholar]
- Carpenter JK, Sanford J, Hofmann SG. The effect of a brief mindfulness training on distress tolerance and stress reactivity. Behavior Therapy. 2019;50(3):630–645. doi: 10.1016/j.beth.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vibe M, Solhaug I, Tyssen R, Friborg O, Rosenvinge JH, Sorlie T, Bjorndal A. Mindfulness training for stress management: a randomised controlled study of medical and psychology students. BMC Medical Education. 2013;13(1):1–11. doi: 10.1186/1472-6920-13-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy ME, Twenge JM, Joiner TE. Trends in mood and anxiety symptoms and suicide-related outcomes among US undergraduates, 2007–2018: Evidence from two national surveys. Journal of Adolescent Health. 2019;65(5):590–598. doi: 10.1016/j.jadohealth.2019.04.033. [DOI] [PubMed] [Google Scholar]
- Dyrbye LN, Shanafelt TD, Werner L, Sood A, Satele D, Wolanskyj AP. The impact of a required longitudinal stress management and resilience training course for first-year medical students. Journal of General Internal Medicine. 2017;32(12):1309–1314. doi: 10.1007/s11606-017-4171-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erogul M, Singer G, McIntyre T, Stefanov DG. Abridged mindfulness intervention to support wellness in first-year medical students. Teaching & Learning in Medicine. 2014;26(4):350–356. doi: 10.1080/10401334.2014.945025. [DOI] [PubMed] [Google Scholar]
- Goldberg SB, Tucker RP, Greene PA, Simpson TL, Kearney DJ, Davidson RJ. Is mindfulness research methodology improving over time? A Systematic Review. Plos ONE. 2017;12(10):e0187298. doi: 10.1371/journal.pone.0187298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greeson JM, Toohey MJ, Pearce MJ. An adapted four week mind body skills group for medical students: reducing, stress increasing mindfulness, and enhancing self-care. Explore: The Journal of Science & Healing. 2015;11(3):186–192. doi: 10.1016/j.explore.2015.02.003. [DOI] [PubMed] [Google Scholar]
- Hassed C, de Lisle S, Sullivan G, Pier C. Enhancing the health of medical students: outcomes of an integrated mindfulness and lifestyle program. Advances in Health Sciences Education. 2009;14(3):387–398. doi: 10.1007/s10459-008-9125-3. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Gómez AF. Mindfulness-based interventions for anxiety and depression. Psychiatric Clinics. 2017;40(4):739–749. doi: 10.1016/j.psc.2017.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huckins J, DaSilva AWW, Hedlund E, Rogers C, Nepal SJW, Obuchi M, Murphy E, Meyer M, Wagner D, Holtzheimer P, Campbell A. Mental health and behavior of college students during the early phases of the COVID-19 pandemic: Longitudinal smartphone and ecological momentary assessment study. Journal of Medical Internet Research. 2020;22(6):e20185. doi: 10.2196/20185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry. 1982;4(1):33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- Kang YS, Choi SY, Ryu E. The effectiveness of a stress coping program based on mindfulness meditation on the stress, anxiety, and depression experienced by nursing students in Korea. Nurse Education Today. 2009;29(5):538–543. doi: 10.1016/j.nedt.2008.12.003. [DOI] [PubMed] [Google Scholar]
- Kuhlmann SM, Huss M, Burger A, Hammerle F. Coping with stress in medical students: results of a randomized controlled trial using a mindfulness-based stress prevention training (MediMind) in Germany. BMC Medical Education. 2016;16(1):316. doi: 10.1186/s12909-016-0833-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemay V, Hoolahan J, Buchanan A. Impact of a yoga and meditation intervention on students' stress and anxiety levels. American Journal of Pharmaceutical Education. 2019;83(5):7001. doi: 10.5688/ajpe7001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis, A., Kirkman, A., & Holmes, L. (2019). Wellness in Allied Health students: the case for change. Health Education in Practice: Journal of Research for Professional Learning, 2(1). 10.33966/hepj.2.1.13447
- Nechita F, Nechita D, Pirlof M-C, Rogoveanu I. Biomedical education. Romanian Journal of Morphology and Embryology. 2014;55(3 Suppl):1263–1266. [PubMed] [Google Scholar]
- Neto AD, Lucchetti ALG, da Silva Ezequiel O, Lucchetti G. Effects of a required large-group mindfulness meditation course on first-year medical students' mental health and quality of life: A randomized controlled trial. Journal of General Internal Medicine. 2020;35(3):672–678. doi: 10.1007/s11606-019-05284-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newsome S, Waldo M, Gruszka C. Mindfulness group work: Preventing stress and increasing self-compassion among helping professionals in training. Journal for Specialists in Group Work. 2012;37(4):297–311. doi: 10.1080/01933922.2012.690832. [DOI] [Google Scholar]
- Phang CK, Chiang KC, Ng LO, Keng S-L, Oei TPS. Effects of brief group mindfulness-based cognitive therapy for stress reduction among medical students in a Malaysian university. Mindfulness. 2016;7(1):189–197. doi: 10.1007/s12671-015-0399-2. [DOI] [Google Scholar]
- Phang CK, Mukhtar F, Ibrahim N, Keng SL, MohdSidik S. Effects of a brief mindfulness-based intervention program for stress management among medical students: the Mindful-Gym randomized controlled study. Advances in Health Sciences Education. 2015;20(5):1115–1134. doi: 10.1007/s10459-015-9591-3. [DOI] [PubMed] [Google Scholar]
- Ramón-Arbués E, Gea-Caballero V, Granada-López JM, Juárez-Vela R, Pellicer-García B, Antón-Solanas I. The prevalence of depression, anxiety and stress and their associated factors in college students. International Journal of Environmental Research and Public Health. 2020;17(19):7001. doi: 10.3390/ijerph17197001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray I, Joseph D. Stress in medical students. JK Science. 2010;12(4):163. [Google Scholar]
- Regehr C, Glancy D, Pitts A. Interventions to reduce stress in university students: A review and meta-analysis. Journal of Affective Disorders. 2013;148(1):1–11. doi: 10.1016/j.jad.2012.11.026. [DOI] [PubMed] [Google Scholar]
- Reid DT. Teaching mindfulness to occupational therapy students: Pilot evaluation of an online curriculum. Canadian Journal of Occupational Therapy. 2013;80(1):42–48. doi: 10.1177/0008417413475598. [DOI] [PubMed] [Google Scholar]
- Ribeiro ÍJ, Pereira R, Freire IV, de Oliveira BG, Casotti CA, Boery EN. Stress and quality of life among university students: A systematic literature review. Health Professions Education. 2017;4(2):70–77. doi: 10.1016/j.hpe.2017.03.002. [DOI] [Google Scholar]
- Rickwood, D., Telford, N., O’Sullivan, S., Crisp, D., & Magyar, R. (2016). National Tertiary Student Wellbeing Survey 2016.
- Rimes KA, Wingrove J. Pilot study of Mindfulness-Based Cognitive Therapy for trainee clinical psychologists. Behavioural & Cognitive Psychotherapy. 2011;39(2):235–241. doi: 10.1017/S1352465810000731. [DOI] [PubMed] [Google Scholar]
- Roulston A, Montgomery L, Campbell A, Davidson G. Exploring the impact of mindfulnesss on mental wellbeing, stress and resilience of undergraduate social work students. Social Work Education. 2018;37(2):157–172. doi: 10.1080/02615479.2017.1388776. [DOI] [Google Scholar]
- Ruff KM, Mackenzie ER. The role of mindfulness in healthcare reform a policy paper. Explore: The Journal of Science and Healing. 2009;5(6):313–323. doi: 10.1016/j.explore.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Shearer A, Hunt M, Chowdhury M, Nicol L. Effects of a brief mindfulness meditation intervention on student stress and heart rate variability. International Journal of Stress Management. 2016;23(2):232–254. doi: 10.1037/a0039814. [DOI] [Google Scholar]
- Song Y, Lindquist R. Effects of mindfulness-based stress reduction on depression, anxiety, stress and mindfulness in Korean nursing students. Nurse Education Today. 2015;35(1):86–90. doi: 10.1016/j.nedt.2014.06.010. [DOI] [PubMed] [Google Scholar]
- Spadaro KC, Hunker DF. Apr). Exploring the effects of an online asynchronous mindfulness meditation intervention with nursing students on stress, mood, and cognition: A descriptive study. Nurse Education Today. 2016;39:163–169. doi: 10.1016/j.nedt.2016.02.006. [DOI] [PubMed] [Google Scholar]
- Speech Pathology Australia. (2015). 2015 Annual Report: A snapshot of Australia’s speechies.
- Szuster RR, Onoye JM, Eckert MD, Kurahara DK, Ikeda RK, Matsu CR. Presence, resilience, and compassion training in clinical education (PRACTICE): Evaluation of a mindfulness-based intervention for residents. The International Journal of Psychiatry in Medicine. 2020;55(2):131–141. doi: 10.1177/0091217419887639. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Segal ZV, Williams JMG, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology. 2000;68(4):615. doi: 10.1037/0022-006X.68.4.615. [DOI] [PubMed] [Google Scholar]
- Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annals of Internal Medicine. 2018;169(7):467–473. doi: 10.7326/m18-0850. [DOI] [PubMed] [Google Scholar]
- van Dijk I, Lucassen P, Akkermans RP, van Engelen BGM, van Weel C, Speckens AEM. Effects of mindfulness-based stress reduction on the mental health of clinical clerkship students: A cluster-randomized controlled trial. Academic Medicine. 2017;92(7):1012–1021. doi: 10.1097/ACM.0000000000001546. [DOI] [PubMed] [Google Scholar]
- Warnecke E, Quinn S, Ogden K, Towle N, Nelson MR. A randomised controlled trial of the effects of mindfulness practice on medical student stress levels. Medical Education. 2011;45(4):381–388. doi: 10.1111/j.1365-2923.2010.03877.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.