Abstract
Medical waste (MW) poses serious threats to environmental and public health. Throughout the world, existing challenges of medical waste management (MWM) have been heightened in the Covid-19 situation due to an increase in the massive amount of MW. Even before the pandemic, MWM has always been a concern in Bangladesh. The objectives of this research are to review the related national policy initiatives and guidelines in Bangladesh in comparison with the international guidelines, to evaluate the present scenario of the MWM system, and to explore the scope of Impact Assessment (IA) in improving the system. From the analysis, it has been found that several national guidelines have been formulated during this pandemic covering important issues related to the MWM system, which is commendable. Some of these guidelines comply with international guidelines, but there are inconsistencies among these. However, neither the previous MWM policy tools nor these guidelines are implemented accordingly. In this pandemic, an IA framework has also been published in Bangladesh, which is praiseworthy. Although no evidence could be found on its implementation either. Therefore, it is necessary to take initiative for the implementation of this IA framework. Thereby the policy makers will be able to identify the gaps prohibiting the implementation of the MWM policy tools and guidelines. This will enable them to take corrective actions accordingly to improve the MWM system by enhancing the preparedness and capacity against any possible future situations like pandemic overwhelming the MW situation in Bangladesh.
Keywords: Medical waste management (MWM), Health care facilities (HCFs), Policy initiatives and guidelines, Impact assessment (IA), Pandemic, Bangladesh
Introduction
Health care facilities (HCFs) are the basic requirement of every civilized society to protect the health of the community, the demand of which is growing around the world with an increased population [1–3]. Activities in the HCFs result in the generation of a huge amount of medical wastes (MW) [1, 2, 4–7]. Moreover, the growth in this sector combined with the increased use of disposable medical products is resulting in the generation of increased MW [2, 3, 8]. These MWs pose serious threats to environmental and public health, thus create a substantial concern [4, 5, 9–15]. Proper medical waste management (MWM) might not eradicate the complete risk but can minimize the impact on the environment and public health [4, 9, 16, 17]. Therefore, MWM is considered a critical issue throughout the world [5, 11, 18].
Worldwide, studies conducted on MWM mostly include literature review [2, 11, 19], management at HCFs [1, 9, 10, 15–17, 20, 21], and overall management [6, 7, 12, 13, 22–26]. There are also researches on specific aspects of the MWM system, like waste generation [3, 18], and alternative methods for waste treatment and disposal [8]. Potential environmental and health risks associated with MWM in the HCFs were also focused in a study conducted by Bokhoree, Beeharry [5].
The existing challenges of MWM have been magnified in the present Covid-19 pandemic situation leading to an abrupt collapse of the system [27–29]. It has given rise to the massive amount of MW especially due to excessive use of plastic products including personal protective equipment (PPE) [28, 30–33]. This infectious disease can spread easily from the pathogen contaminated MWs [28, 30, 31, 34]. The increased waste is also resulting in growing environmental consequences and challenges [28–36]. Therefore, proper MWM is necessary for preventing or reducing the spread of Covid-19 as well as protection of the environment [28–30, 36–38]. Since the MWM system at Covid-19 is not much different than the previous system, it is overwhelmed with the tremendous amount of infectious waste and their shifted composition in this pandemic [28, 39]. Therefore, effective and dynamic responsive changes with additional standard methods are necessary in the MWM system using existing resources and quick solutions [27, 28].
On the other hand, several studies have been carried out realizing the significance of different streams of waste management in the Covid-19 situation. The studies concentrated on the impact of the Covid-19 pandemic on solid waste management [31, 35, 40], municipality waste collection services [41], potential consequences on waste and wastewater services [42], plastic waste management [28, 32] among others. Zand and Heir [33] studied the environmental impacts of the Covid-19 pandemic with emphasis on the waste management sector in Iran. MWM-related studies focused on review on MW handling [30], disinfection and treatment technologies for MW [34, 43]. While, Yu, Sun [36] proposed a methodology to identify locations of temporary facilities and transportation strategies for effective MWM. In addition to these, several international guidelines have been developed on MWM [38, 39, 44]. WHO [45] has also developed a “Health-Care Waste Management Rapid Assessment Tool” which aims at “…reducing the disease burden caused by poor health care waste management (HCWM) through the promotion of best practices and the development of safety standards…”.
In the background of the importance of MWM, this research aims to evaluate the MWM system in the Covid-19 situation in Bangladesh, as one of the most densely populated developing countries in the world. The specific objectives of this research are three-fold-
1) To review the national policy initiatives and guidelines in Bangladesh addressing the MWM system during the Covid-19 situation in comparison with the international guidelines;
2) To review the present scenario of MWM system at Covid-19 situation in Bangladesh;
3) To explore the scope of impact assessment (IA) in improving the MWM system at the Covid-19 situation in Bangladesh.
Why MW is a concern in Covid-19 situation in Bangladesh?
Generally, the overall scenario of MW is alarming in Bangladesh due to the increasing number of HCFs generating a huge amount of MW [10]. According to ADB’s hazardous waste inventory of 2008, MW contributes to the second-largest volume of hazardous wastes in the country [46]. Though MWM has always been a great concern in a developing country like Bangladesh, policy measures in this regard are very recent. Country’s first-ever environmental assessment and action plan for the health, nutrition, and population (HNP) sector addressing MWM came to light in 2004, which was later upgraded in 2011 [4]. From 2005, training and awareness for MWM started being developed [4]. The first MWM Rules of Bangladesh was published in 2008 [47]. Some pits for disposal were constructed by 2009 and some Non-Government Organizations (NGOs) developed expertise and came forward for proper MWM [4, 16, 48].
However, appropriate application of the Rules regarding the MWM system is yet to be visible in Bangladesh [16, 48]. Very few HCFs started segregation of waste at source and standardized treatment of waste safeguarding environment [4, 16]. According to Dana [15], authorities and owners of HCFs also lack interest and are not bothered to improve or update their MWM methods as there is a cost involved. Most of them dump their unsegregated and untreated MW in open municipal bins and thereby threatening the environment and human health [4, 16, 48, 49]. More concerning is, that sometimes the waste remains in open bins for 2–3 days [16, 50, 51]. Furthermore, these wastes are handled by poorly educated and unskilled workers with no training and minimum guidance and supervision [52]. They even resale used infectious MW items like a syringe, needle, saline bag, blood bag, test tube, etc. [4, 16]. Apart from open municipal bins, there is also practice of dumping MW in pit near the HCF, open field, roadside, or into water bodies [51]. Some of the HCFs dispose of their untreated liquid chemical wastes into municipal drains [4]. Leaches from these wastes contaminate soil and groundwater through toxicity [15]. At the final stage of disposal, the municipality generally dumps the untreated MW along with the general wastes stream on vacant land or landfills [52]. Thus, mismanagement at each step of MWM in Bangladesh threatens both environment and human health [4, 15, 16, 52]. Along with these, lack of awareness, expertise, logistics (like storage in separate bins, transport facility or even protective gears of cleaners), manpower, and on top of that inadequate implementation of the legal provision hinders proper handling and proper management of MW in Bangladesh [4, 16, 48].
Therefore, even before the Covid-19 situation started, MWM has always been a concern in Bangladesh [53]. In normal condition, MW generation in Bangladesh is estimated around 0.5 kg/patient/day [16, 52]. Whereas, at the Covid-19 situation, this waste generation jumps to 3.4 kg/patient/day [44], which is about 6.8 times higher than normal conditions. In Bangladesh, one Covid-19 patient stays 7–8 days in HCF [54]. As of 5 July 2020, confirmed Covid-19 cased in Bangladesh were 162,417. According to WHO [55] “…Around 1 in every 5 people who are infected with COVID-19 develop difficulty in breathing and require hospital care…”. Accordingly, considering 20% of the total infected needing HCF care, approximately 32,483 (20% of 162,417) patients were admitted to HCFs in Bangladesh till 5 July 2020 since the outbreak. Therefore, since the outbreak, the estimation of cumulative MW at Covid-19 situation in Bangladesh till 5 July 2020 is about 828,316.5 kgs or about 913 tons. Even without considering the infectious waste generated by Covid-19-infected people receiving treatment at home, this amount is overwhelming. These MWs are mostly plastics which are hardly biodegradable and expected to exist longer in the environment if not treated and disposed properly [28, 32]. Failure in proper MWM at Covid-19 situation can even threaten biodiversity and wildlife of Bangladesh [56]. MW generated at this pandemic is expected to have major impact on environment and this alarming impact is yet to be discovered by Bangladesh.
Methodology
This study has been carried out as a qualitative unsystematic descriptive review of national and international policies, legislations and guidelines, and newspaper articles based on Covid-19 MWM collected from secondary sources. For the first objective, different national policies, legislations, and guidelines on MWM in Bangladesh have been collected from the relevant websites of the Ministries in Bangladesh and international guidelines have been collected from the relevant websites of the international organizations. After data collection, a comparative analysis of the national and international policy guidelines has been drawn to understand the extent to which these national policy guidelines address the MWM at Covid-19 situation. For the second objective, relevant newspaper articles have been collected and reviewed to evaluate the MWM system at the Covid-19 scenario in Bangladesh. For the third objective, frameworks for IA regarding MWM in Bangladesh, especially for the Covid-19 situation have been explored and reviewed to understand the scope in this regard.
Policy initiatives and guidelines for Covid-19 MWM in Bangladesh
Leading legal and guideline documents for MWM in general and pandemic situation
For MWM in Bangladesh, the “Medical Waste (Management and Processing) Rules” has been promulgated in 2008 under the Environmental Conservation Act, 1995 [57] by the Ministry of Environment, Forest and Climate Change (MoEFCC). It has been prepared through the active participation of MoEFCC and the Ministry of Health and Family Welfare (MoHFW) with the objective of proper management of MW and thereby protecting the environment. Additionally, DGHS [58] has developed the “Manual for Hospital Waste Management” in 2001 which has been updated in 2010, to manage MW efficiently and economically with a minimal environmental and health impact. This manual is supported by the Rules [47].
In 2018, the “Hospital Infection Prevention and Control Manual” has been developed by the Quality Improvement Secretariat (QIS), Health Economics Unit, Health Services Division, MoHFW, in collaboration with USAID’s MaMoni Health Systems Strengthening Project [59]. The main purpose of this manual is to provide a guideline for HCFs laying down the policies and broad guidelines for infection prevention and control including guidelines for MWM referring to the Rules [47].
In 2019, the “National Strategy for WASH in HCFs 2019–2023: A Framework for Action” has been published by the Directorate General of Health Services (DGHS), MoHFW, funded by UNICEF [60]. This strategy is intended to improve the MWM system at all levels. The actions intended for this strategy included an update of the existing MWM system following WHO standards, develop a training curriculum for HCF regarding new guidelines, etc.
Management of MW and Covid-19 infectious wastes in HCF are similar, but additional provisions are required due to the amount of waste being generated at the Covid-19 situation [39]. Considering the importance, several guidelines and frameworks have been formulated to address the Covid-19 situation in Bangladesh, with some focusing on MW. Most of these documents have been imposed in March 2020. These documents are:
The “Guideline or Standard Operating Procedure (SOP) for Coronavirus (Covid-19) Related Waste Management in Hospital” formulated by the DGHS and the National Institute of Preventive and Social Medicine (NIPSOM) [61]. The first volume was published in March 2020. It applies to all HCFs those deal with Covid-19-related waste. The purpose is to provide guidance on MWM against coronavirus; and to save the health of the employee, visitor, and environment from the risk of produced waste for maintaining a safe, healthy, and productive working environment.
The “National Guideline for Health Care Provider on Infection Prevention and Control of Covid-19 pandemic in Healthcare Setting” has been formulated by the DGHS [37] and published in March 2020. According to the guideline, health care personnel for Covid-19 patients are at high risk of getting the infection. Therefore, precaution and prevention can be done by decontamination, management, and disposal of MW.
The “Guideline or Standard Operating Procedure (SOP) for Coronavirus (Covid-19) Disinfection and Environmental Infection Prevention” formulated by the DGHS; the Institute of Epidemiology, Disease Control and Research (IEDCR); and the World Health Organization (WHO) [62]. The first volume was published in March 2020 with the purpose to guide environmental cleanliness and disinfection to prevent Covid-19 spread, and to maintain a safe, clean, and healthy environment to ensure the safety of service providers, patients, and inspectors. Despite such focus, this document does not contain any guidelines for MW in HCF.
The “General Notice” was published by the department of environment (DoE), under the Environmental Conservation Act, 1995 [57] to control environmental pollution and prevention of the spread of coronavirus [63]. This document further refers to the Rules [47] for MWM.
Except for these documents, the importance of the MWM issue for the Covid-19 situation has been addressed in some other guidelines. They are:
The “Rational Use of Personal Protective Equipment (PPE) for Covid-19” has been imposed by the DGHS, IEDCR, UNICEF, and the WHO in March 2020 [64]. According to the document, all medical workers including cleaners in all areas should wear PPE appropriately. This document referred to the guideline for Coronavirus (Covid-19)-related HCFs Waste management [61].
The “National Guidelines on Clinical Management of Coronavirus Disease 2019 (COVID-19)” by the DGHS; and the WHO [65]. The seventh version of this document has been published in May 2020. According to the guideline, an effective infection control program requires an MWM, among others.
It can be said that the key legislative document on MWM of Bangladesh is, the Medical Waste (Management and Processing) Rules 2008 [47]. It is praiseworthy that several guidelines and frameworks have been formulated to address the Covid-19 situation in Bangladesh, with some focusing on MW. But these documents are not legally imposing leaving a wide scope of avoidance.
Designated authority
According to the Rules [47], the designated authority for MWM in Bangladesh consists of the director of the health department, a member from the divisional commissioner’s office, and a representative from DoE. For the management and processing of MW, third parties need a license. But the Rules are not applicable in case of MWM by City Corporation or Municipality. Whereas the MoHFW is responsible for in-house MWM at the large scale, and out-house MWM is the responsibility of the Ministry of Local Government and Rural Development (MoLGRD) including City Corporation or Municipality or can be contracted out through NGOs [4, 60, 63, 66]. In Dhaka, Bogra, and Khulna districts in Bangladesh, the out-house MWM is operated by NGOs with limited coverage in cities [4]. Thus, the Rules are not imposed on local responsible authorities resulting in a gap in the management process [4]. Moreover, it does not specifically designate a responsible authority for MWM at individual HCFs. But, this issue has been addressed in Hospital Infection Prevention and Control Manual” by QIS [59]. In this Manual, it is instructed to develop Hospital Infection Prevention and Control Subcommittee (HIPCSC) and Work Improvement Team in each HCFs including structure, role, and responsibilities of the committee and team.
While conflict of designated authority and responsibility is questionable in the existing MWM policies, responsible handling of Covid-19 MWM is also real concern in Bangladesh. To manage Covid-19 MW safely, responsibility and adequate resources should be assigned at HCFs [38]. This issue also received importance in the guidelines published in the Covid-19 situation. According to those, the nominated person from the relevant department would be liable to abide by the whole process at every HCF [61]. There should be designated trained staff or management officers for MWM [63]. The nominated waste cleaner is responsible for the maintenance of the MW logbook in prescribe format to observe the management process [61].
According to WHO and UNICEF [38], all the people handling MW should wear appropriate PPE and perform hand hygiene after removing it, which has also been suggested by DGHS, IEDCR [64] in Bangladesh. The local government should provide a Covid-19-labeled two-layer color-coded sustainable bag and bin for MW collection [63].
Despite such progressive documents, the problem of coordination among responsible authorities at different scales for MWM remains unaddressed, which poses great difficulties, especially in the Covid-19 situation.
MWM system at Covid-19 situation according to the leading documents
Considering the infectious characteristics of the Covid-19 waste and its huge volume, the Covid-19 MWM becomes overwhelming and requires special attention [38, 39, 44]. Therefore, the capacity to manage the waste should also be increased at every step [38]. In the following sections, the MWM system focusing on the Covid-19 situation as per the policy guidelines in Bangladesh has been discussed and compared with international standards.
On-site separation and management
In the Covid-19 situation, waste separation at the source is of utmost importance to avoid multiple times handling of infected MW considering the risk [38, 39, 44]. Comparison among the national legislation and guidelines for MW separation at source is shown in Table 1. From the comparison, it can be observed that the classification as per the 2008 Rules is clearer and elaborate. The Rules [47] also state that MW should never be mixed with other wastes at any stage of management. The inclusion of such guidelines is commendable, but more consistency is necessary in this regard. Additional waste generated from PPE in the Covid-19 situation requires special attention [38]. DGHS and NIPSOM [61] and DGHS [37] provide directives regarding the disposal of PPE. According to the guidelines, PPE should be disposed of in a biohazard bag or color-coded bin, securely sealed, and labeled marking with the date, and disposing of after 72 h as normal. The disinfection of the reusable waste bins and transport carts is also important in the Covid-19 situation. This issue has been addressed by DGHS and NIPSOM [61], and DoE [63] stating that the reusable waste bins and transport carts should be covered and can be reused after disinfection routinely.
Table 1.
Comparison of the national legislation and guidelines for on-site MW separation
| Colour code | Medical waste (Management and Processing) Rules, 2008 [47] | National guideline for health care provider on infection prevention and control of Covid-19 pandemic in healthcare setting, 2020 [37] | Guideline or standard operating procedure (SOP) for coronavirus (Covid-19) related waste management in hospital, 2020 [61] | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Waste category | Type of waste | Type of Bin | Waste category | Type of waste | Type of Bin | Waste category | Type of waste | Type of Bin | |
| Black | General | Non-harmful, non-infectious, germfree | Perforated plastic bin | – | General: Leftover meals, administrative rubbish, and paper, sweeping | Two-layered biohazard bag or waste bag in the perforated bin. When a two-thirds portion of the bag would be filled up, it should be tied up appropriately and kept in a separate covered coloured labeled perforated bin | – | – | – |
| Yellow | Harmful | Anatomical, pathological, infectious | Perforated plastic bin | – | Clinical lab waste without a sharp object: Materials used in lab /patient care | – | – | – | |
| Red | Sharp | Infected, non-infected, bacterial, disinfected | Perforated thick plastic bin, box | – | Clinical waste with a sharp object: Needles or scalpel blades, knives broken glass material, etc. | – | Contaminated sharp waste | Two-layered biohazard bag or waste bag in the perforated bin. When a three-fourth portion of the bag would be filled up, it should be tied up appropriately and kept in a separate covered coloured labeled perforated bin | |
| Blue | Liquid | Harmful, non-harmful, infected, non-infected, bacterial, disinfected, chemical | Perforated plastic bowl, bin | – | Liquid: Vomiting, blood | – | Liquid waste | – | |
| Silver | Radioactive | Radioactive | Perforated lid box | – | – | – | – | – | |
| Green | Reusable | Non-harmful, non-infected, non-infected | Perforated plastic bin | – | Recyclable: Saline kits | – | – | – | |
On-site disinfection, treatment, and disposal
Considering the huge amount of waste generated at the HCFs at Covid-19 situation, on-site management including treatment and disposal has been preferred in the international guidelines [38, 39, 44]. According to these guidelines, the Covid-19 MW can be either treated and disposed of on-site or transported offsite for disposal after treatment at the source. Thus, onsite treatment of the waste is necessary. Then the treated waste can be disposed of on-site or offsite. Considering the amount of waste generated, it is important to increase the capacity of the HCFs to handle and treat their MW [38]. Various alternative MW treatment and disposal methods may need to be produced at HCF considering their capacity. Alongside, systems should be developed to ensure their sustained operation [38]. These methods should minimize the formation and release of chemicals or hazardous emissions, while open burning is discouraged due to the polluting emissions [39].
On the contrary, the MWM Rules [47] do not mention anything about disinfection, treatment, and disposal on site. It guides to treat MW centrally, where the MW are classified into eleven categories and thus corresponding methods for refining and disposing the waste are described accordingly. Despite the importance of considering the infectiousness of Covid-19 medical waste, the DoE [63] (Covid-19 MWM-related notification) complied with the 2008 Rule regarding offsite treatment. For the pandemic, DGHS and NIPSOM [61] have included a flow chart of MWM (Fig. 1) in their document which does not reflect the actual process at all, this is misleading. Therefore, these guidelines inconsistent with the international guidelines.
Fig. 1.
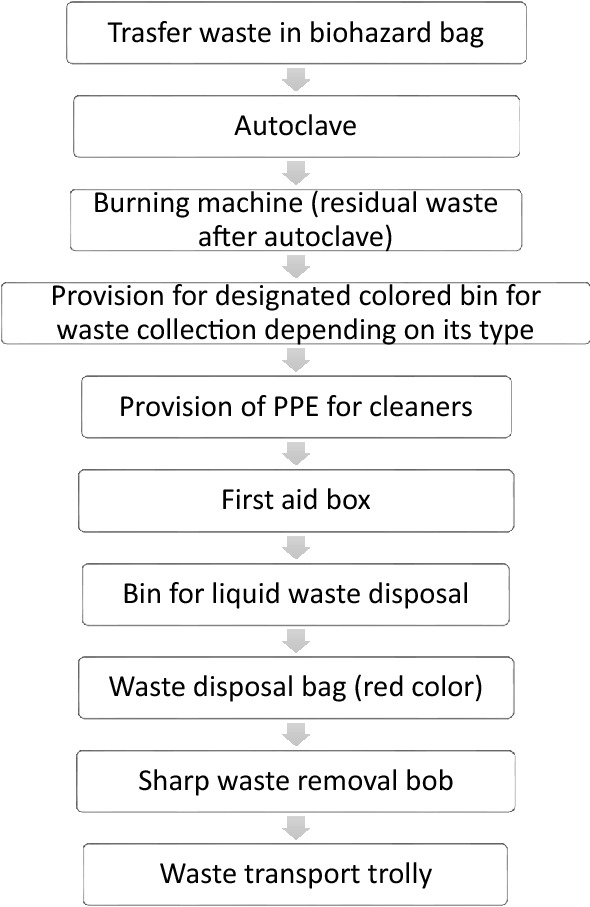
Process of MWM at HCFs as per the “Guideline or Standard Operating Procedure (SOP) for Coronavirus (Covid-19) Related Waste Management in Hospital” Source: [61], (p.1)
On the other hand, some other guidelines address on-site MW treatment and disposal. According to DGHS [37] and DoE [63], after tying up the waste bag, it should be disinfected keeping the bag sealed, and should be preserved in a covered bin labeled as Covid-19. This guideline is consistent with ADB [44]. DGHS and NIPSOM [61]; DGHS [37] and DoE [63] suggest decontaminating the infected waste by autoclave or chemical prohibiting reuse. DGHS and NIPSOM [61] and DGHS [37] adds to it that after disinfection, the waste should be incinerated (ideal) or burnt (if incineration is not available) in pits (> 8 feet deep) in premises, behind the HCF building. Though there remains some inconsistency, both guidelines propose the MW should be treated and burnt on site or should be sent to a sanitary landfill. The provision of burning contradicts with UNEP [39] considering the environmental concern. Though, many options for waste treatment and disposal on site have been included in the guidelines, the issue about capacity building of the HCFs has not been included in any of the national guidelines.
In addition to the solid MW, the wastewater generated in HCFs are highly polluted and infectious. For treating this heavy polluting wastewater from the HCFs, inclusion and operation of Effluent Treatment Plant (ETP) in the facilities is necessary to ensure the safety of the discharged wastewater. Considering this context, according to the Environmental Conservation Rules (ECR) 1997 of Bangladesh [67], HCFs are considered under red category polluting projects, for which inclusion of ETP within their plan is mandatory. In the MWM Rules and guidelines, different treatment options for wastewater have been mentioned, but none of them addressed the inclusion of on-site ETPs in the HCFs, though it is mandatory as per ECR, 1997. This also reflect the inconsistency among the Rules and guidelines.
Storage and transportation
According to UNEP [39], considering the overwhelming amount of MW generated during the Covid-19 situation, there should have a designated storage location inside each HCFs to accumulate the Covid-19 waste at the source. This issue has not been addressed in any of the national guidelines.
According to the DoE [47], the MW without being disinfected should not be preserved at HCFs for more than 48 h, which is consistent with UNEP [39]. But if it is necessary to preserve for more than 48 h, then the licensed third party should take permission from the corresponding local government to ensure that the waste would not have any negative effect on human health and the environment.
According to both DoE [47], DoE [63] the MW should be collected and transported from the outside of HCFs only by approved vehicle, by an approved person at time and procedure defined by the local government. Which comply with the international guidelines [39, 44]. But according to ADB [44], additional special vehicles should be used for transporting the Covid-19 MW considering the amount, where the loading area should be separated from the driver’s cabin. While collecting and transporting, the wastes should be kept separated and sealed [39].
Disposal
According to both the Rules and Covid-19 guidelines in Bangladesh, the treated waste should be transported and disposed of in a designated sanitary landfill [37, 47, 61, 63], which is consistent with international guidelines. According to UNEP [39], the Covid-19 MW should never be disposed of at open dumpsites at any point to prevent harmful consequences on human health and the environment. This issue has not been addressed in any of the guidelines in Bangladesh.
Table 2 shows a comparative analysis of national legislation and guidelines in Bangladesh with international guidelines for the MWM system at the Covid-19 situation. From the analysis, it can be said that the Rules for MWM is required to be amended to incorporate the Rules to enhance preparedness and capacity for accommodating with overwhelmed MW condition resulted due any possible future situations like pandemic. Such amendment is intended to be done as per the MoHFW [60]. But for immediate MWM at the Covid-19 situation, the published guidelines in Bangladesh are timely and appropriate. Despite this fact, all these guidelines need to be synchronized increase uniformity and elaboration. Especially, the guidelines for MW disinfection, treatment, and disposal at source would require rigorous revision and for MW collection and transportation would require more inclusion and detailing. All such revisions should be done complying with international standards considering human health and the environment.
Table 2.
Comparison of national legislation and guidelines in Bangladesh with international guidelines for MWM system at Covid-19 situation
| Covid-19 MWM system | International guidelines of ADB, UNEP, and WHO | Bangladesh legislation and guidelines | Special features | Remarks |
|---|---|---|---|---|
| Responsible authority | ||||
| At HCF | Yes | Yes |
All staffs should be trained All the people handling MW should wear appropriate PPE and perform hand hygiene after removing it |
|
| At local level | Yes | Yes | Local authorities should provide color-coded double-layered bag and bin to HCF | Inclusion of local authorities missing |
| General | ||||
| Should never be mixed with other wastes at any stage | Yes | Yes | ||
| Cleaners and waste handlers should wear PPE | Yes | Yes | Not included in all guidelines | |
| Source separation and management | ||||
| Minimize waste generation | Yes | No | ||
| Coloured perforated bins | Yes | Yes | Colour code as per the waste type | Not included in all guidelines |
| Leak proof coloured double-layered waste bags | Yes | Yes | Waste bags should be tied up and sealed appropriately after filled up |
Not included in all guidelines Inconsistency in the standard for filling up a waste bag |
| Guideline about PPE | Yes | Yes | PPE disinfection and separation | |
| Management of reusable waste bin | No | Yes | Should be disinfected before reuse | Commendable consideration |
| Disinfection, treatment, and disposal at source | ||||
| Alternative options | Yes | Yes | Suitable option considering the condition of the HCF |
Inconsistent among the guidelines Inconsistent with international standard Lacks detailing |
| Capacity building of HCF | Yes | No | ||
| Burning | No | Yes | Not suitable for human health and the environment | |
| Send untreated waste in a sanitary landfill | No | Yes | Not suitable for Covid-19 situation | |
| Storage and transport | ||||
| Storage on-site | Yes | No | ||
| Storage time | Yes | Yes | ||
| Designated time and procedure | Yes | Yes | Should be collected and transported at designated time and procedure | Lacks detailing regarding the procedure |
| Approved vehicle | Yes | Yes | Additional special vehicles with loading space separated from the driver’s cabin are not considered | |
| Keeping the waste separated while transporting | Yes | No | ||
| Disposal | ||||
| Designated sanitary landfill | Yes | Yes | ||
| Prohibition of dumping in open dumpsites at any point | Yes | No | ||
Scenario of MWM at Covid-19 situation in Bangladesh
Most of the HCFs do not get enough support from the local government waste management [68]. Several private and public HCFs mostly in Dhaka city have often claimed to follow proper methods to manage the MW [69, 70]. But according to existing literature, most of the HCFs dump MW at random places, mix up with general waste, and pile up openly outside the facility even at this pandemic [70–73].
In case of the collection of MW by waste collectors or NGOs from the HCFs, it is done in open vans, open drums, or garbage trucks, and also the vehicles used for transporting the waste are not managed properly [72–74]. MW is frequently found in municipal bins [74]. The openly piled wastes are then picked up by waste scavengers [73]. This is increasing the risk on the environment and the health of waste handlers as they do not use proper protective gears [71, 72, 75]. Considering the risk, MW workers reportedly left their jobs or are unwilling to collect resulting in a significant reduction in the number of waste handlers in Bangladesh [56, 74].
In some HCFs, the NGOs working with MWM collect wastes treat, and dump the residue [56, 74]. If this waste gets mixed with municipal wastes, it would not be in their scope to handle it [56]. On the other hand, increased demand for surgical masks and gloves and open dumping of such MW have also resulted in the washing and reselling of used masks and hand gloves [69, 73, 76].
It is evident that, HCFs are not equipped to treat and manage the highly contagious MW generated from the Covid-19 treatment [74]. Only a few have an on-site treatment system [73]. They mostly have a backyard and are putting their waste into a ditch or burning in a pit, while measures for environmental protection remain questionable [68, 70, 73, 74]. Though, on site ETP is mandatory for HCF in Bangladesh, it has not been included in any of the plans of the government HCFs, whereas only 5–6% of the private HCFs have ETP [77]. Thus, the operational capacity of many of these facilities is also questionable [73]. For central treatment of MW, there is only one incinerator in Dhaka which is not sufficient even in normal conditions [70, 78]. Thus, most of the MW remain untreated. Treated or untreated, these wastes are dumped in landfills. Alarmingly, the landfills also do not have sufficient capacity [79].
A legal notice has been served in early June 2020 to the Government to take necessary measures for MWM amidst the Covid-19 pandemic [80]. On 22 June 2020, Dhaka North and South City Corporations mentioned starting the process in collaboration with the concerned NGO, however, till mid-July, there was no visible progress in this [75]. Other municipalities were unable to develop Covid-19 WM mechanisms [75].
Thus, reflection and application of the policy guidelines cannot be observed at any step of the MWM system in the Covid-19 situation in Bangladesh.
Scope for IA in improving MWM system at Covid-19 situation in Bangladesh
From the analysis of national policy initiatives, guidelines, and scenario of MWM system at Covid-19 situation in Bangladesh, it can be observed that in documentation this issue has so far been addressed accordingly though, there remains some inconsistency. But the reflection of even these documents was not evident in practice. Therefore, it is necessary to analyze the gap and its impacts through IA.
In Bangladesh, Environmental Impact Assessment (EIA) is mandatory as per ECR 1997, for red category polluting projects including HCFs, waste incinerators, and landfills, among the others [67]. In 2011, the “Environmental Assessment and Action Plan: For the Health, Population and Nutrition Sector Development Program (HPNSDP) 2011–2016” was formulated by the MoHFW [4]. The objectives of this plan included evaluating the then status of MW disposal and formulation of an action plan for management based on identified gaps. Suggested action plans incorporated building awareness and capacity, developing guidelines and manuals, budget and investment, private sector participation, and ensure the active role of authority. Thus, IA in the MWM sector in Bangladesh is not a brand-new concept. Despite these facts, its application is not satisfactory yet [81].
In this pandemic, another praiseworthy initiative by Bangladesh was the formulation of “Environment and social management framework for Bangladesh (ESMF): Covid-19 emergency response and pandemic preparedness project” by the DGHS published in May 2020 [66]. The framework lists sub-projects like construction, expansion, rehabilitation, and operation of HCFs as a response to Covid-19 pandemic; outlines purpose as providing tools and guidelines for environmental and social (ES) risk categorization, identifying risks, benefit, and impacts of project to minimize risk and enhance benefits; procedures to assess ES risks, and proposing mitigation measures at design and implementation level. The ESMF proposed two templates among others relevant to MWM concern in Covid-19. One identifies potential environmental, social, health, and safety issues associated with the construction and operation of HCFs; and Infection Control and Waste Management Plan (ICWMP) focuses on infection control and MWM practices in HCFs during the operation. Mitigation measures proposed to reduce ES risks in HCFs identified in this framework are:
Waste generation at HCFs should be minimized as much as possible without compromising health and hygiene, which complies with international guidelines. For example, reusable PPE should be encouraged as much as possible [82]. In this regard, HCFs should dedicate larger areas for temporary storage and disinfection of such reusable PPE on large scale. The inclusion of ETP at HCFs can help treat the wastewater produced from such disinfection along with the mainstream wastewater treatment. From a technical perspective, this measure is undoubtedly unavoidable and proper training to the HCF personnel can effectively reduce the waste generation [18, 83, 84]. However, the increased use and nature of disposable medical products make it difficult to reduce the waste generation in HCFs [2, 3, 8]. Therefore, researchers and manufactures may need to further research and work on reusable medical equipment as well as its scope to enable the HCFs to minimize waste generation and thus contribute to sustainability.
The initiatives required ensuring proper MW separation at HCFs for new development or up-gradation of the existing facility includes estimating potential waste; ensuring color-coded storage bins to be able to accommodate anticipated volume according to the type of waste, designing training for the healthcare providers to assist source separation of waste.
Waste minimization, reuse, and recycling using incinerator poses an environmental and social risk and thus should be avoided as much as possible. If it is the only option, then best practices should be implied to ensure safe use and shifting to alternative treatment at the earliest possible time. On this regard, onsite waste treatment and disposal capacity and technical appraisal of the existing facilities should be performed, and corrective measures should be taken if required.
Timely onsite collection and transport of packaged and labeled wastes in HCFs should be adopted using designated trolleys/carts and routes ensuring routine disinfection of pertaining tools and spaces. HCFs should also ensure hygiene and safety of involved supporting medical workers such as cleaners.
Waste storage areas should be designated in HCFs separately according to the type of waste and should be disinfected regularly and properly.
Infectious waste generated in the Covid-19 situation should be removed from the storage area within 24 h of generation- this statement in ESMF contradicts national as well as international guidelines about storage.
Disposal of residual MW from HCFs at offsite waste disposal facilities provided by local government or private sector should ensure appraisal of the facility and corrective measures as required. Technical adequacy, process capacity, performance record, and operator’s capacity of these sites should be examined, and in case of any gaps, corrective measures should be recommended and agreed upon with the government or the private sector operators.
Emergency Response Plan (ERP) should be developed at the HCFs to adequately address the emergency risk levels.
To prevent possible exposure, capacity building and training should involve all local players including medical workers, waste management workers, cleaners, as well as third-party waste management service providers.
To ensure proper monitoring of Covid-19 MW, an information management system should be developed at HCFs for tracking and recording the waste streams at different stages of the MWM system.
This framework might serve the purpose of Rapid Environmental Assessment (REA) of the HCFs in this pandemic. The major stages for REA here would have been collecting the baseline information, impacts identification and assessment, and designing mitigation measures. Though DGHS did not use the term REA, ESMF seems to cover the basic components through the templates. Therefore, the detailing in this document might be sufficient for now to address the primary concerns considering the urgency of the matter. However, to date, authors have not been able to find any documentation or information on such assessment being done for the HCFs. The issues in the framework comply with the international guidelines for MWM at this pandemic to some extent, but again, these measures are not enforced by law. While the urgency of upgrading the MWM system in a pandemic is unavoidable, assessing and mitigating the impacts of these are still a great challenge for Bangladesh in this situation.
So, despite being positive, IA based on this framework and corresponding mitigation measures may fail to serve the goals if inconsistency keep existing among the documents and no enforcement plan is considered.
Way forward
The ongoing Covid-19 pandemic is not the first in the history of pandemics and surely will not be the last. From the experience of Covid-19 we have learned that the appearance of a pandemic puts extra pressure on the MWM system, therefore needs the extra capacity of the system to absorb. Based on the above discussion, the following initiatives should be taken to improve the MWM system in Bangladesh and to ensure preparedness and adaptability of the system with changing circumstances resulted due to pandemic situations or other likely events in the future.
The legal documents for MWM, especially the Medical Waste (Management and Processing) Rules should be amended to integrate the missing links and to incorporate some of the guidelines to absorb the thrust of the overwhelmed MW condition resulting from pandemic like situations. While doing so, consistency among all the documents and compliance with international standards should be ensured. Coordination among responsible authorities at different scales for MWM is of prime importance for a successful implementation. Considering the limited public capacity, a strong, stable, and knowledgeable private sector is required to be developed to meet the additional demand of MWM attaining quality and quantity in pandemic situations. Proper enforcement and implementation of the legal documents should be ensured. Existing Environmental court should be utilized in such case. In addition to this, integrated inspection and monitoring system should be developed. Initiatives should be taken for IA at HCFs as per the ESMF [66] to implement the mitigation measures accordingly and thereby enhance their capacity for the MWM as per the legislation to make them prepared for any overwhelmed situation. Provision for need-based financial assistance should be considered by the Government for capacity building of different stakeholders involved in MWM in Bangladesh.
Conclusion
This research brings out the important concerns on emerging challenges in MWM due to the Covid-19 pandemic in Bangladesh, as one of the densely populated developing countries in the world. The key legislative document on MWM of Bangladesh is the Medical Waste (Management and Processing) Rules, 2008. Due to the poor implementation of legislation and policy guidelines, the MWM has always been a concern even before the pandemic. During the Covid-19 pandemic, the situation became overwhelmed and worse. However, this legal document still does not address the process for accommodating the emergencies like pandemics and resultant tremendous load of MW. To immediately tackle the MWM situation during the Covid-19 pandemic, several national guidelines have been published in Bangladesh which is timely and appropriate. Thus, the Covid-19 pandemic has raised the urgency from Government’s side. Nevertheless, these are not legally imposing. It is also dubious how much of the dedicated measures could be enforced in the lockdown with limited resources. The problem of coordination among responsible authorities at different scales for MWM remains unaddressed, which poses great difficulties, especially in the Covid-19 situation. These documents also need to be synchronized to increase uniformity and elaboration complying with international standards considering human health and the environment. On top of that, reluctance from HCFs owners, lack of knowledge of the caregivers, and general people will only worsen the situation. Therefore, no matter how many guidelines have been formulated, if not legally mandated, it will be difficult to protect the environment and human health from the impacts of mismanagement of MW generated in this pandemic. The newly formulated ESMF framework addresses this concern. However, there is no evidence of its implementation. In this scenario, only carrying out a rapid IA to analyze the gap is not enough but the implementation of the mitigation measures accordingly is of prime importance. This research will guide the policymakers to understand the gap in the MWM system in Bangladesh and thereby take necessary actions to improve the condition by addressing the gaps accordingly. Other developing countries with similar MWM condition may also realize the importance of preparedness and development of the adaptive capacity to accommodate future situations like the Covid-19 pandemic. As future scope of this study, research based on primary data collected from the HCFs and WM sites would aid in better understanding of the scenario on the implementation and bring out a comprehensive picture of compliance through comparison with the documents formulated.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
UB (roles: conceptualization; investigation; writing—original draft, review and editing); DH (roles: conceptualization; supervision; investigation; writing—original draft, review and editing).
Funding
Not applicable.
Declarations
Conflict of interest
Not applicable.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Alam I et al (2019) Assessment of bio-medical waste management in different hospitals in Aligarh city. In: Kalamdhad A, Singh J, Dhamodharan K (eds) Advances in waste management. Springer, Singapore, pp 501–510. 10.1007/978-981-13-0215-2_36 [Google Scholar]
- 2.Babanyara YY et al (2013) Poor medical waste management (MWM) practices and its risks to human health and the environment: a literature review. Int J Environ Chem Ecol Geol Geophys Eng 11(7):538–545. 10.5281/zenodo.1089052 [Google Scholar]
- 3.Patwary MA et al (2009) Quantitative assessment of medical waste generation in the capital city of Bangladesh. Waste Manag 29(8):2392–2397. 10.1016/j.wasman.2009.03.021 [DOI] [PubMed] [Google Scholar]
- 4.MoHFW (2011) Environmental assessment and action plan: for the health, population and nutrition sector development program (HPNSDP) 2011–2016. Ministry of Health and Family Welfare (MOHFW), the Government People’s Republic of Bangladesh (GoB). Dhaka, Bangladesh. Retrieved from http://webcache.googleusercontent.com/search?q=cache:uKLZ6yKyAOIJ:www.mohfw.gov.bd/index.php%3Foption%3Dcom_docman%26task%3Ddoc_download%26gid%3D359%26lang%3Den+&cd=3&hl=en&ct=clnk&gl=bd
- 5.Bokhoree C et al (2014) Assessment of environmental and health risks associated with the management of medical waste in Mauritius. APCBEE Procedia 9:36–41. 10.1016/j.apcbee.2014.01.007D [Google Scholar]
- 6.Lee CC, Huffman GL (1996) Medical waste management/incineration. J Hazard Mater 48:1–30 [Google Scholar]
- 7.Patwary MA, O’Hare WT, Sarker MH (2011) Assessment of occupational and environmental safety associated with medical waste disposal in developing countries: a qualitative approach. Saf Sci 49(8–9):1200–1207. 10.1016/j.ssci.2011.04.001 [Google Scholar]
- 8.Ghasemi MK, Yusuff RB (2016) Advantages and disadvantages of healthcare waste treatment and disposal alternatives: Malaysian scenario. Pol J Environ Stud 25(1):17–25. 10.15244/pjoes/59322 [Google Scholar]
- 9.Alam MZ, Islam MS, Islam MR (2013) Medical waste management: a case study on Rajshahi city corporation in Bangladesh. J Environ Sci Nat Resour 6(1):173–178 [Google Scholar]
- 10.Hasan MM, Rahman MH (2018) Assessment of healthcare waste management paradigms and its suitable treatment alternative: a case study. J Environ Public Health 2018:6879751. 10.1155/2018/6879751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hossain MS et al (2011) Clinical solid waste management practices and its impact on human health and environment—a review. Waste Manag 31(4):754–766. 10.1016/j.wasman.2010.11.008 [DOI] [PubMed] [Google Scholar]
- 12.Jang Y-C et al (2006) Medical waste management in Korea. J Environ Manag 80(2):107–115. 10.1016/j.jenvman.2005.08.018 [DOI] [PubMed] [Google Scholar]
- 13.Yong Z et al (2009) Medical waste management in China: a case study of Nanjing. Waste Manag 29(4):1376–1382 [DOI] [PubMed] [Google Scholar]
- 14.WHO (2018) Health-care waste. World Health Organization (WHO). Retrieved from https://www.who.int/news-room/fact-sheets/detail/health-care-waste
- 15.Dana T (2011) Hospital waste management: Bangladesh. OIDA Int J Sustain Dev 2(9):29–40 [Google Scholar]
- 16.Hassan MM et al (2008) Pattern of medical waste management: existing scenario in Dhaka city, Bangladesh. BMC Public Health 8(36). 10.1186/1471-2458-8-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manyele SV, Lyasenga TJ (2010) Factors affecting medical waste management in low level health facilities in Tanzania SV. Afr J Environ Sci Technol 4(5):304–318 [Google Scholar]
- 18.Cheng YW et al (2009) Medical waste production at hospitals and associated factors. Waste Manag 29(1):440–444. 10.1016/j.wasman.2008.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shareefdeen ZM (2012) Medical waste management and control. J Environ Prot 3(12):1625–1628. 10.4236/jep.2012.312179 [Google Scholar]
- 20.Patil GV, Pokhrel K (2005) Biomedical solid waste management in an Indian hospital: a case study. Waste Manag 25(6):592–599. 10.1016/j.wasman.2004.07.011 [DOI] [PubMed] [Google Scholar]
- 21.Silva CE et al (2005) Medical waste management in Brazil. Waste Manag 25:600–605. 10.1016/j.wasman.2004.03.002 [DOI] [PubMed] [Google Scholar]
- 22.Coker A et al (2009) Medical waste management in Ibadan, Nigeria: obstacles and prospects. Waste Manag 29(2):804–811. 10.1016/j.wasman.2008.06.040 [DOI] [PubMed] [Google Scholar]
- 23.Walkinshaw E (2011) Medical waste-management practices vary across Canada. Can Med Assoc J 183(18):E1307–E1308. 10.1503/cmaj.109-4032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rahman MS, Moumita C, Rikta K (2013) Medical waste management system: an alarming threat (a case study on Jessore Municipality, Bangladesh). J Environ Sci Nat Resour 6(2):181–189 [Google Scholar]
- 25.Sartaj M, Arabgol R (2015) Assessment of healthcare waste management practices and associated problems in Isfahan Province (Iran). J Mater Cycles Waste Manag 17(1):99–106. 10.1007/s10163-014-0230-5 [Google Scholar]
- 26.Ali M, Kuroiwa C (2009) Medical waste management and disposal, 1991. J Mater Cycles Waste Manag 11(3):251–257 [Google Scholar]
- 27.UN-Habitat (2020) Strategy guidance: solid waste management response to COVID-19. Retrieved from https://unhabitat.org/sites/default/files/2020/05/un-habitat_strategy_guidance_swm_reponse_to_covid19.pdf
- 28.Klemeš JJ et al (2020) Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew Sustain Energy Rev 127:109883. 10.1016/j.rser.2020.109883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.You S, Sonne C, Ok YS (2020) COVID-19’s unsustainable waste management. Science 368(6498):1438. 10.1126/science.abc7778 [DOI] [PubMed] [Google Scholar]
- 30.Hossain I et al (2020) Pandemic COVID-19 and Biomedical waste handling: a review study. J Med Sci Clin Res 8(5):497–502. 10.18535/jmscr/v8i5.88 [Google Scholar]
- 31.Nzediegwu C, Chang SX (2020) Improper solid waste management increases potential for COVID-19 spread in developing countries. Resour Conserv Recycl 161:104947. 10.1016/j.resconrec.2020.104947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Silva ALP et al (2020) Rethinking and optimising plastic waste management under COVID-19 pandemic: policy solutions based on redesign and reduction of single-use plastics and personal protective equipment. Sci Total Environ 742:140565. 10.1016/j.scitotenv.2020.140565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zand AD, Heir AV (2021) Environmental impacts of new Coronavirus outbreak in Iran with an emphasis on waste management sector. J Mater Cycles Waste Manage 23(1):240–247. 10.1007/s10163-020-01123-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang J et al (2020) Disinfection technology of hospital wastes and wastewater: suggestions for disinfection strategy during coronavirus disease 2019 (COVID-19) pandemic in China. Environ Pollut 262:114665. 10.1016/j.envpol.2020.114665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kulkarni BN, Anantharama V (2020) Repercussions of COVID-19 pandemic on municipal solid waste management: challenges and opportunities. Sci Total Environ 743:140693. 10.1016/j.scitotenv.2020.140693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yu H et al (2020) Reverse logistics network design for effective management of medical waste in epidemic outbreaks: insights from the coronavirus disease 2019 (COVID-19) outbreak in Wuhan (China). Int J Environ Res Public Health 17(5):1770. 10.3390/ijerph17051770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.DGHS (2020) National guideline for health care provider on infection prevention and control of COVID 19 pandemic in healthcare setting. Directorate General of Health Services (DGHS), Ministry of Health and Family Welfare (MOHFW), the Government of the People’s Republic of Bangladesh (GoB). Dhaka, Bangladesh. Retrieved from https://dghs.gov.bd/images/docs/Guideline/IPC%20Module%20for%20COVID-19%20for%20frontline%20HCW_20.3.2020.pdf
- 38.WHO and UNICEF (2020) Water, sanitation, hygiene, and waste management for the COVID-19 virus: Interim guidance. World Health Organization and the United Nations Children’s Fund (UNICEF). Retrieved from https://apps.who.int/iris/bitstream/handle/10665/331846/WHO-2019-nCoV-IPC_WASH-2020.3-eng.pdf
- 39.UNEP (2020) Practical guideline for the handling, storage and disposal of Covid-19 infected wastes, including personnel protective equipment. United Nations Environment Programme (UNEP). Retrieved from https://www.humanitarianlibrary.org/sites/default/files/2020/06/UNEP_PRACTICAL%20GUIDELINE%20FOR%20COVID%2019%20WASTE%20MANAGEMENT%20UNEP-GSC-DOS.pdf
- 40.Nzeadibe TC, Ejike-Alieji AUP (2020) Solid waste management during Covid-19 pandemic: policy gaps and prospects for inclusive waste governance in Nigeria. Local Environ 25(7):527–535. 10.1080/13549839.2020.1782357 [Google Scholar]
- 41.Moonsammy S et al (2021) COVID-19 effects on municipality waste collection services for households: statistical modelling of perspectives from Guyana and Nigeria. J Mater Cycles Waste Manag 23:1678–1687. 10.1007/s10163-021-01225-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nghiem LD et al (2020) The COVID-19 pandemic: considerations for the waste and wastewater services sector. Case Stud Chem Environ Eng 1:100006. 10.1016/j.cscee.2020.100006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ma Y et al (2020) Suggested guidelines for emergency treatment of medical waste during COVID-19: Chinese experience. Waste Dispos Sustain Energy 2:81–84. 10.1007/s42768-020-00039-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.ADB (2020) Managing infectious medical waste during the COVID-19 Pandemic. Asian Development Bank (ADB). Retrieved from https://www.adb.org/sites/default/files/publication/578771/managing-medical-waste-covid19.pdf
- 45.WHO (2020) Health-care waste management rapid assessment tool. Retrieved from https://www.who.int/water_sanitation_health/facilities/waste/hcwmtool/en/?fbclid=IwAR1nYmf-KV4n_GfCMGv1ikObSvdkQE-RBZOZ-4Y8qr5vpWlZkha4ki-Q-GU
- 46.ADB (2010) Technical assistance consultant’s report on managing hazardous wastes, Bangladesh. Asian Development Bank (ADB). Retrieved from https://www.adb.org/sites/default/files/project-document/62596/38401-01-reg-tacr-01.pdf
- 47.DoE (2008) Medical waste (Management and Processing) Rules 2008. Department of environment (DoE), Ministry of Environment, Forest and Climate Change (MoEFCC), the Government of the People’s Republic of Bangladesh (GoB). Dhaka, Bangladesh. Retrieved from http://www.clcbd.org/document/133.html
- 48.Nuralam HM et al (2017) Healthcare waste management practices in Bangladesh: a case study in Dhaka city, Bangladesh. Int J Environ Chem Ecol Geol Geophys Eng 11(6):534–539 [Google Scholar]
- 49.The World Bank (2002) Health facility waste management study in Bangladesh. The World Bank. Dhaka, Bangladesh [Google Scholar]
- 50.Rashid S (1996) Medical waste disposal in Dhaka city: a survey. Unpublished thesis, North-South University. Dhaka, Bangladesh
- 51.Akter N, Kazi NM, Chowdhury MR (1999) Medical waste disposal in Dhaka City: an environmental evaluation. International center for diarrhoeal disease research, Bangladesh (ICDDR, B). Dhaka, Bangladesh
- 52.Biswas A, Amanullah ASM, Santra SC (2011) Medical waste management in the tertiary hospitals of Bangladesh: an empirical enquiry. ASA Univ Rev 5(2):149–158 [Google Scholar]
- 53.Sujan MA (2020) Untreated medical waste: a serious threat to public health. The Daily Star. Dhaka, Bangladesh. Retrieved from https://www.thedailystar.net/frontpage/news/untreated-medical-waste-serious-threat-public-health-1819624 [Google Scholar]
- 54.Tajmim T (2020) Changed discharge criteria triggers rise in Covid-19 recoveries. The Business Standard. Dhaka, Bangladesh. Retrieved from https://tbsnews.net/coronavirus-chronicle/covid-19-bangladesh/changed-discharge-criteria-triggers-rise-covid-19 [Google Scholar]
- 55.WHO (2020) Media statement: knowing the risks for COVID-19. Retrieved from https://www.who.int/indonesia/news/detail/08-03-2020-knowing-the-risk-for-covid-19
- 56.Amin MA (2020) World environment day: medical waste prolonging Covid-19, threatening biodiversity. The Dhaka Tribune. Dhaka, Bangladesh. Retrieved from https://www.dhakatribune.com/bangladesh/environment/2020/06/04/world-environment-day-friday-medical-waste-prolonging-covid-19-and-threatening-biodiversity [Google Scholar]
- 57.MoEFCC (1995) The Bangladesh Environmental Conservation Act, 1995. Ministry of Environment, Forest and Climate Change (MoEFCC), the Government of the People’s Republic of Bangladesh (GoB). Dhaka, Bangladesh. Retrieved from https://bangladeshbiosafety.org/wp-content/uploads/2017/05/Bangladesh_Environmental_Conservation_Act_1995.pdf
- 58.DGHS (2010) Manual for hospital waste management 2001 amended in 2010. Directorate general of health services (DGHS), Ministry of Health and Family Welfare (MOHFW), the Government of the People’s Republic of Bangladesh (GoB). Dhaka, Bangladesh
- 59.QIS (2018) Hospital infection prevention and control manual. Quality improvement secretariat (QIS), Health Economics Unit, Health Services Division, Ministry of Health and Family Welfare, the Government of the People’s Republic of Bangladesh (GoB), in collaboration with USAID’s MaMoni Health systems strengthening project. Dhaka, Bangladesh. Retrieved from http://qis.gov.bd/wp-content/uploads/2019/05/Hospital-Infection-Prevention-and-Control-Manual.pdf
- 60.MoHFW (2019) National strategy for WASH in health care facilities 2019–2023: A framework for action. Ministry of Health and Family Welfare (MOHFW), the Government of the People’s Republic of Bangladesh (GoB). Dhaka, Bangladesh
- 61.DGHS and NIPSOM (2020) Guideline or standard operating procedure (SOP) for Coronavirus (Covid 19) related waste management in hospital. Directorate General of Health Services (DGHS), Ministry of Health and Family Welfare (MOHFW), the Government of the People’s Republic of Bangladesh (GoB); and National Institute of Preventive and Social Medicine (NIPSOM). Dhaka, Bangladesh. Retrieved from https://corona.gov.bd/storage/press-releases/May2020/86to1ep1DWaZJSkOtyw2.pdf
- 62.DGHS, IEDCR, and WHO (2020) Guideline or standard operating procedure (SOP) for Coronavirus (Covid 19) disinfection and environmental infection prevention. Directorate General of Health Services (DGHS), Ministry of Health and Family Welfare (MOHFW), the Government of the People’s Republic of Bangladesh (GoB); Institute of Epidemiology, Disease Control and Research (IEDCR); and World Health Orgaization (WHO). Dhaka, Bangladesh. Retrieved from https://www.dghs.gov.bd/images/docs/Notice/21_03_2020_SOP_Environmental%20Disinfectant%20210320.pdf
- 63.DoE (2020) General notice. Department of Environment (DoE), Ministry of Environment, Forest and Climate Change (MoEFCC), the Government of the People’s Republic of Bangladesh (GoB). Dhaka, Bangladesh
- 64.DGHS et al (2020) Rational use of personal protective equipment for Covid-19. Directorate General of Health Services (DGHS), Ministry of Health and Family Welfare (MOHFW), the Government of the People’s Republic of Bangladesh (GoB); Institute of Epidemiology, Desease Control and Research (IEDCR); UNICEF; and World Health Organization (WHO). Dhaka, Bangladesh. Retrieved from https://www.dghs.gov.bd/images/docs/Notice/20_03_2020_PPE_FINAL_WEBSITE.pdf
- 65.DGHS and WHO (2020) National Guidelines on Clinical Management of Coronavirus Disease 2019 (COVID-19). Disease Control Division, Directorate General of Health Services (DGHS), Ministry of Health and Family Welfare (MOHFW), the Government of the People’s Republic of Bangladesh (GoB); and World Health Organization (WHO), Dhaka, Bangladesh. Retrieved from http://file.portal.gov.bd/files/cs.sylhet.gov.bd/notices/245c5244_369b_4305_958d_1f70d99d6681/4c021caf6cf2915278aa3598e74f5c09.pdf
- 66.DGHS (2020) Environment and social management framework for Bangladesh: Covid-19 emergency response and pandemic preparedness project (p173757). Directorate General of Health Services (DGHS), Ministry of Health and Family Welfare (MOHFW), the Government of the People’s Republic of Bangladesh (GoB). Dhaka, Bangladesh. Retrieved from https://dghs.gov.bd/images/docs/Notice/Notice_15_06_2020_3.pdf
- 67.DoE (1997) The Bangladesh Environmental Conservation Rules, 1997. Department of Environment (DoE), Ministry of Environment, Forest and Climate Change (MoEFCC), the Government of the People’s Republic of Bangladesh (GoB). Dhaka, Bangladesh. Retrieved from http://extwprlegs1.fao.org/docs/pdf/bgd19918.pdf
- 68.Shovon FR (2020) Covid-19: improper disposal of PPE endangering lives, environment. The Dhaka Tribune. Dhaka, Bangladesh. Retrieved from https://www.dhakatribune.com/health/coronavirus/2020/05/13/covid-19-improper-disposal-of-ppe-endangering-lives-environment [Google Scholar]
- 69.Rahaman MZ (2020) Covid waste lack of disposal threatening public health. The Daily New Nation. Dhaka, Bangladesh. Retrieved from http://m.thedailynewnation.com/news/255601/covid-waste-lack-of-disposal-threatening-public-health [Google Scholar]
- 70.Asaduzzaman (2020) Fear of COVID-19 spread by medical waste. The Daily Prothom Alo. Dhaka, Bangladesh. Retrieved from https://www.prothomalo.com/bangladesh/article/1659124/ফেলে-রাখা-মেডিকেল-বর্জ্যে-করোনা-সংক্রমণের-ভয়
- 71.BBC Bangla (2020) Coronavirus: single use plastic waste is increasing in Bangladesh, potential health risk. The BBC Bangla. Dhaka, Bangladesh. Retrieved from https://www.bbc.com/bengali/news-52605492 [Google Scholar]
- 72.Joardar SS (2020) Will unplanned disposal of medical and other plastic wastes add to the Covid-19 concerns? The Business Standard. Dhaka, Bangladesh. Retrieved from https://tbsnews.net/thoughts/will-unplanned-disposal-medical-and-other-plastic-wastes-add-covid-19-concerns-92206 [Google Scholar]
- 73.Tayeb T (2020) What do we do with the refuse of our Covid-19 afflicted healthcare system? The Daily Star. Dhaka, Bangladesh. Retrieved from https://www.thedailystar.net/opinion/closer-look/news/what-do-we-do-the-refuse-our-covid-19-afflicted-healthcare-system-1929805 [Google Scholar]
- 74.Razzak MA (2020) Can Bangladesh cope with covid-19 medical waste? The Daily Star. Dhaka, Bangladesh. Retrieved from https://www.thedailystar.net/opinion/news/can-bangladesh-cope-covid-19-medical-waste-1897327 [Google Scholar]
- 75.Ahamad R (2020) No COVID-19 waste management in Bangladesh yet: infection risks grow, environment suffers damage. The New Age. Dhaka, Bangladesh. Retrieved from https://www.newagebd.net/article/109154/no-covid-19-waste-management-in-bangladesh-yet [Google Scholar]
- 76.The Financial Express (2020) Amid COVID-19, biomedical waste turning more hazardous. The Financial Express. Dhaka, Bangladesh. Retrieved from https://www.thefinancialexpress.com.bd/health/amid-covid-19-biomedical-waste-turning-more-hazardous-1586504008 [Google Scholar]
- 77.Devnath B, Roy P (2019) How liquid waste causes health risk. The Daily Star. Dhaka, Bangladesh. Retrieved from https://www.thedailystar.net/frontpage/news/how-liquid-waste-causes-health-risk-1830772?fbclid=IwAR0oSDpgaSbNyNPkf7-XnNNnNTwDN2lbs3Cmhw8QOeuWSEBqVwB_6MquqTA [Google Scholar]
- 78.Ali ML (2020) Another catastrophe due to Corona waste. The Daily Star. Dhaka, Bangladesh. Retrieved from https://www.thedailystar.net/bangla/মতামত/করোনা-বর্জ্যে-আরেক-বিপর্যয়-156797 [Google Scholar]
- 79.Roy R (2020) Significance of Covid-19 for environment. The Buiseness Standard. Dhaka, Bangladesh. Retrieved from https://tbsnews.net/bangla/মতামত/পরিবেশের-জন্য-কোভিড-১৯-এর-তাৎপর্য [Google Scholar]
- 80.Rahman M (2020) Amid COVID-19, biomedical waste turning more hazardous. The Dhaka Tribune. Dhaka, Bangladesh. Retrieved from https://www.dhakatribune.com/bangladesh/2020/06/09/legal-notice-outlines-necessary-measures-for-medical-waste-managem [Google Scholar]
- 81.Kabir SMZ, Momtaz S (2012) The quality of environmental impact statements and environmental impact assessment practice in Bangladesh. Impact Assess Proj Apprais 30(2):94–99. 10.1080/14615517.2012.672671 [Google Scholar]
- 82.Mahmood SU et al (2020) Strategies for rational use of personal protective equipment (PPE) among healthcare providers during the COVID-19 crisis. Cureus 12(5):e8248. 10.7759/cureus.8248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Diaz LF et al (2008) Characteristics of healthcare wastes. Waste Manag 28(7):1219–1226. 10.1016/j.wasman.2007.04.010 [DOI] [PubMed] [Google Scholar]
- 84.Moreira AMM, Günther WMR (2013) Assessment of medical waste management at a primary health-care center in São Paulo, Brazil. Waste Manag 33(1):162–167. 10.1016/j.wasman.2012.09.018 [DOI] [PubMed] [Google Scholar]


