Abstract
Shelter-in-place mandates and closure of nonessential businesses have been central to COVID19 response strategies including in Toronto, Canada. Approximately half of the working population in Canada are employed in occupations that do not allow for remote work suggesting potentially limited impact of some of the strategies proposed to mitigate COVID-19 acquisition and onward transmission risks and associated morbidity and mortality. We compared per-capita rates of COVID-19 cases and deaths from January 23, 2020 to January 24, 2021, across neighborhoods in Toronto by proportion of the population working in essential services. We used person-level data on laboratory-confirmed COVID-19 community cases and deaths, and census data for neighborhood-level attributes. Cumulative per-capita rates of COVID-19 cases and deaths were 3.3-fold and 2.5-fold higher, respectively, in neighborhoods with the highest versus lowest concentration of essential workers. Findings suggest that the population who continued to serve the essential needs of society throughout COVID-19 shouldered a disproportionate burden of transmission and deaths. Taken together, results signal the need for active intervention strategies to complement restrictive measures to optimize both the equity and effectiveness of COVID-19 responses.
Keywords: COVID-19, Essential workers, Disease transmission, Health inequity, Infectious disease
Abbreviations: CCM+, Case and Contact Management Solutions; DA, dissemination areas; IQR, interquartile range
Purpose
In Toronto, Canada's largest city, there were 170,023 COVID-19 cases and 3570 deaths as of July 6, 2021 [1]. In addition to testing and isolation, shelter-in-place mandates and the closure of nonessential businesses to reduce contacts were central to Toronto's COVID-19 response. However, many services remained open to support the general needs of society. Public Safety Canada defined “essential workers” in the context of ten infrastructure sectors, including health, food, transportation, and manufacturing [2]. Before the pandemic, it was estimated that 40% of the working population in Canada were employed in occupations amenable to remote work, with the lowest likelihood of remote work among lower income households [3]. Thus, it has been suggested that shelter-in-place mandates may be insufficient at protecting essential workers from COVID-19 and associated morbidity and mortality. In this study, we examined neighbourhood-level per-capita rates of COVID-19 cases and deaths by the proportion of the working population engaged in essential services across neighborhoods in Toronto, Canada.
Methods
We used person-level data on laboratory-confirmed COVID-19 cases and deaths from the provincial surveillance data (the Case and Contact Management Solutions database [4] which captures all laboratory-confirmed diagnoses of COVID-19 and clinical outcomes); and the Statistics Canada 2016 Census data for neighborhood-level attributes [5]. The study population comprised community cases and deaths reported between January 23, 2020 and January 24, 2021 (i.e., date of case reported to public health, and date of death) in Toronto, and excluding residents of long-term care homes. The data collection or ascertainment period however was up to January 31, 2021 to allow for delays in data entry of cases and/or deaths. Toronto has a population of 2.7 million, including 51.5% who self-identify as a visible minority (terminology used by Statistics Canada to classify individuals who do not identify as Indigenous and do not identify as Caucasian or white) [6]. We defined neighbourhoods by dissemination area (DA), the smallest geographic unit for which data on occupation were available. The median population size of a DA in Toronto is 450 (interquartile range, 446-768). We stratified the city's 3702 DAs into tertiles by ranking the proportion of the labor force in each DA engaged in essential services. For each DA, the proportion engaged in essential services was calculated using the denominator of the total labor force age ≥15 years and the numerator as number of persons in the labor force who reported occupations in one of the following National Occupational Classification categories: manufacturing, utilities, trades, transport, equipment operators, sales, services, health, resources, agriculture, production [5]. Strata 1, 2, and 3 comprised DAs across which a median of 27.8% (inter-quartile range [IQR] 23.4%-31.5%), 44.7% (IQR 40.0%-50.0%), and 62.9% (IQR 58.4%-68.0%) of the population, respectively, worked in essential services.
We generated per-capita daily epidemic curves using 7-day rolling averages for cases and for deaths, and cumulative per-capita rates using census-reported population of each DA. We depicted trends in per-capita cases by the date of report to public health, and the per-capita trends in COVID-19 deaths by the date of death. The study period includes different periods of shelter-in-place restrictions with closure of non-essential workplaces. The first observed case in Toronto was reported January 23, 2020 and a work from home policy was instituted on March 25, 2020 and remained in effect throughout the study period [7]. The first shelter-in-place mandate took place between March 17 and May 18, 2020 and included, in addition to the work from home policy: closure of daycare and in-person education; suspension of non-essential health care services, in-person retail for non-essential goods, and in-person dining in restaurants and other food establishments; remote (phone/virtual) contact tracing and outbreak investigations by public health; closure of indoor and outdoor recreation facilities, prohibition of gatherings of more than five people except in the context of essential services [7] Essential services that continued onsite work included manufacturing, processing, shipping, and curbside pick-up of all goods (factories, distribution warehouses, stores); agriculture; mining; retail and wholesale of food; gas stations; pharmaceutical services; kitchen services for take-away or delivery by restaurants and food facilities; telecommunications and information technology; transportation providers; and essential health care services [7]. The region re-opened on May 18, 2020 and instituted the second-major restriction on November 23, 2020 which was similar to the first shelter-in-place with the following exceptions: nonessential in-store retail, daycare, and in-person education were continued [7]. On December 26, 2020 a more stringent shelter-in-pace mandate was re-instituted similar to the first shelter-in-place mandate with suspension on in-store retail for non-essential goods and closure of in-person education [[7], [8], [9]].
Results
Table 1 summarizes the characteristics of each stratum. The stratum with the highest concentration of essential workers (stratum 3) also includes the highest proportion of the population who self-identify as a visible minority, who reside in multigenerational households, and who earn the lowest income.
Table 1.
Characteristics of the three strata defined by concentration of essential workers, Toronto, Canada
| Concentration of essential workers | Proportion of labor force working in essential servicesMedian (IQR) | Proportion visible minorityMedian (IQR) | Income (CAD)Median (IQR) | Proportion multigenerational householdMedian (IQR) |
|---|---|---|---|---|
| Low (Stratum 1) |
27.8% (23.4-31.5%) | 23.1% (14.9-36.2%) | 59728 (49153-72614) | 3.2% (1.5-6.2%) |
| Medium (Stratum 2) |
44.7% (40.0-50.0%) | 41.8% (25.6-63.0%) | 45322 (38560-51947) | 8.3% (4.7-12.9%) |
| High (Stratum 3) |
62.9% (58.4-68.0%) | 70.8% (51.4-84.7%) | 37705 (31324-43255) | 12.2% (8.2-17.8%) |
For each DA, the proportion engaged in essential services was calculated using the denominator of the total labor force age ≥15 years; and the numerator as number of persons in the labor force who reported occupations in one of the following National Occupational Classification categories: manufacturing, utilities; trades, transport, equipment operators; sales, services; health; resources, agriculture, production.(5) The colors denoted here (red for stratum 1, green for stratum 2, and blue for stratum 3) correspond to the colors for the strata in Figure 1. Abbreviations: CAD (Canadian Dollar); IQR (inter-quartile range).
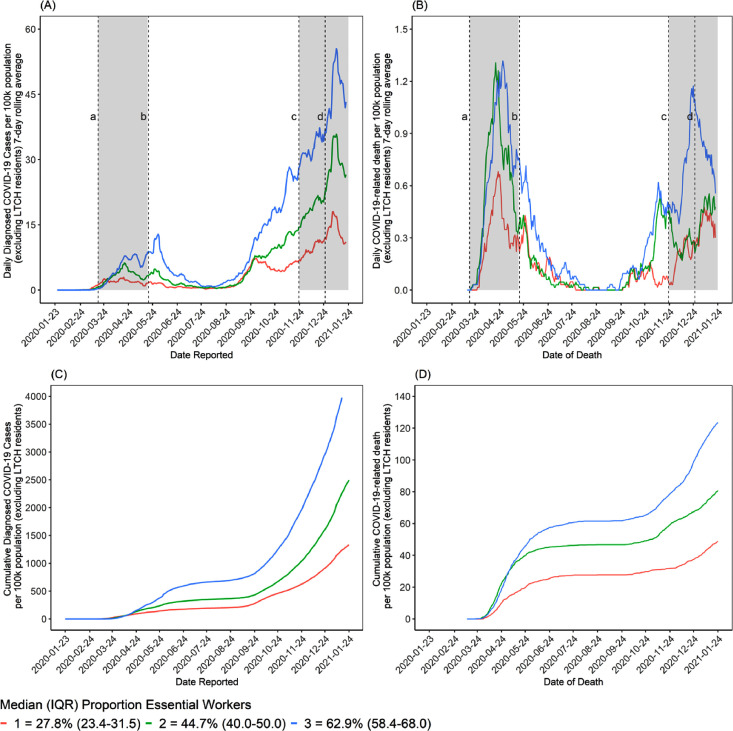
COVID-19 was initially concentrated in stratum 1 (smallest proportion of essential workers). By early April, per-capita cases were consistently higher in strata 2 and 3 (Fig. 1 A), and persisted during each period of closure of nonessential services. By the end of the study period, cumulative rates of cases per 100,000 were 1332, 2495, and 4355 in strata 1, 2, and 3, respectively; representing a 1.9-fold and 3.3-fold higher rate than stratum 1 (Fig. 1C and D).
Fig. 1.
Daily per-capita COVID-19 cases (a) and deaths (b) and cumulative per-capita COVID-19 cases (c) and deaths (d) by neighbourhood-level proportion of essential workers in Toronto, Canada (January 23, 2020 to January 24, 2021). The daily per-capita rate is depicted as a 7-day rolling average. Stratum 1 represents neighbourhoods with the smallest proportion of the population working in essential services, while stratum 3 represents neighbourhoods with the highest proportion of essential workers. Cases and deaths do not include residents of long-term care homes (LTCH). Essential services include: health, trades, transport, equipment, manufacturing, utilities, sales, services, and agriculture. In Fig. 1A and B, closure of nonessential workplaces are indicated by: (a) start of the first shelter-in-place mandate on March 17, 2020 to (b) the re-opening of the province on May 18, 2020; (c) the start of the second-major restriction on November 23; and (d) the start of a more stringent shelter-in-place mandate on December 26, 2020. By the end of the study period, cumulative rates of cases per 100,000 population were 1332, 2495, and 4355 in strata 1, 2, and 3, respectively; and cumulative rates of COVID-19 deaths per 100,000 population were 49, 81, and 123 in strata 1, 2, and 3, respectively.
Per-capita COVID-19 deaths were similarly concentrated in strata 2 and 3. By the end of the study period (Fig. 1B), cumulative rates of death per 100,000 in strata 1, 2, and 3 were 49, 81, and 123, respectively, representing a 1.9-fold and 2.5-fold higher rate in strata 2 and 3 than stratum 1 (Fig. 1C & D). The number of daily per capita cases among stratum 2 was consistently between strata 1 and 3. Daily per-capita deaths fluctuated over the course of the outbreak, demonstrating similarities with stratum 3 during the first lockdown and with stratum 1 during the second major restriction.
Conclusions
In the context of shelter-in-place mandates, there have been disproportionate risks and consequences of COVID-19 borne by those living in neighborhoods with higher proportions of essential workers. The findings are consistent with early studies foreshadowing that many occupations would not be amenable to remote work, and thus a subset of the population may experience sustained contact rates irrespective of restrictive measures [3]. Indeed, Google mobility indices for the region suggest person-time in workplaces remained high, indicative of onsite work [10], and are supported by studies in the United States which found that lower-income neighbourhoods were least likely to be able to reduce their mobility in response to shelter-in-place restrictions [11]. Our findings are also consistent with data suggesting a concentration of excess deaths among the essential service sector in California, United States [12].
Many essential services not amenable to remote work are associated with lower wages [3,13,14], and include seasonal, casual, or contract workers with unclear labor rights and a lack of traditional employment benefits, such as paid sick leave [[13], [14], [15]]. Precarious financial conditions among many essential workers may further limit bargaining power to demand adequate personal protective equipment and safe working conditions from employers or clients [16,17] In the province of Ontario, the second most common site of SARS-CoV-2 outbreaks after long-term care homes were workplaces [18], and in Toronto, a total of 829 workplace outbreaks were detected by July 5, 2021 [19]. Our analyses were conducted at the neighbourhood-level, and thus may reflect transmissions, and thus consquences, at the network level. For example, the beneficial impact of restrictive COVID-19 mitigation strategies may be further limited by the observed overlap in lower income essential work and multigenerational households, wherein workplace transmissions may be bidirectionally linked to – and amplified by - household transmissions [20]. As such, a concentration of deaths by neighbourhood-level essential work may also reflect household networks that include older adults at higher risk of severe disease.
Limitations of this descriptive study include examination of ecological-level measures, and thus we cannot infer an individual-level association between occupation and COVID-19 risk, although external data on individual-level data surrounding income and proxies for structural racism, such as self-identified visible minority, demonstrate a consistent pattern of elevated relative risks [1] Although some occupations are captured in routine surveillance data in Canada, many occupations are not, and characteristics of employment (remote or onsite/in-person) are rarely included [21]. Future work includes an explanatory analysis to examine and compare lags between cases and deaths at the neighbourhood-level, given changing testing criteria and demographics of transmissions and detection over time and disentangling the extent to which neighourhood-level case and deaths stem and intersect directly versus indirectly from workplace versus household exposures.
The findings highlight a prevention gap with restrictive COVID-19 intervention strategies, including shelter-in-place mandates. Moving forward necessitates policies and programs that actively protect workers in occupations that remain onsite in the context of lockdowns. Public and occupational health strategies could include (1) primordial prevention aimed at keeping COVID-19 out of essential workplaces, including through paid leave facilitating people to stay home if they have symptoms or a known exposure [15]; (2) primary prevention designed to limit transmission within the workplace, such as onsite rapid testing, improved access to symptom assessments, and improved ventilation; (3) secondary prevention directed at limiting the size of the outbreak, including infection prevention and control measures, such as isolation, mass testing, and cohorting; and (4) tertiary prevention strategies targeted at limiting outbreak-related mortality, including temporary housing support to prevent transmission to households of essential workers [22]. The findings support the specific allocation of COVID-19 vaccines with community-led outreach strategies to ensure reach and access for essential workers and their households. Leveraging community-led vaccination strategies would be consistent with best practices in service delivery and likely would support optimal messaging, increased trust, and ultimately higher vaccine coverage [23].
In summary, data from a large urban center demonstrate that communities with a greater proportion of essential workers who continued serving the needs of society during COVID-19 disproportionately shouldered the burden of COVID-19 morbidity and mortality. The findings signal a need for active public and occupational health-oriented intervention strategies to complement restrictive measures to optimize both the equity and effectiveness of COVID-19 responses.
Ethics approval
The University of Toronto Health Sciences Research Ethics Board (protocol no. 39253) approved the study. We used Case and Contact Management Solutions (CCM)+ person-level data on laboratory-confirmed COVID-19 cases and deaths reported between January 23, 2020 and January 24, 2021. Such data are not currently publicly available. The analysis code, aggregated output data, and figures of per-capita daily epidemic curves and cumulative per-capita rates are publicly available on GitHub: https://git.io/J3GUP. We used Statistics Canada 2016 Census data for neighbourhood-level characteristics and the census data are publicly available on Statistics Canada:https://www150.statcan.gc.ca/n1/en/catalogue/98-401-X2016044.
Credit statement
Amrita Rao: Conceptualization, Interpretation of Results, Writing – Original draft preparation; Huiting Ma: Conceptualization, Methodology, Analysis, Data Curation, Visualization, Investigation, Interpretation of Results, Writing – Reviewing and Editing; Gary Moloney: Data Curation, Methodology, Interpretation of Results, Writing – Reviewing and Editing; Jeffrey C Kwong: Writing – Reviewing and Editing, Data Curation, Interpretation of Results; Peter Jüni: Methodology, Interpretation of Results, Writing – Reviewing and Editing; Beate Sander: Interpretation of Results, Writing – Reviewing and Editing; Rafal Kustra: Interpretation of Results, Writing – Reviewing and Editing; Stefan D Baral: Conceptualization, Interpretation of Results, Writing – Reviewing and Editing; Sharmistha Mishra: Conceptualization, Methodology, Data Curation, Interpretation of Results, Writing – Reviewing and Editing.
Acknowledgments
Acknowledgments
Reported COVID-19 cases were obtained from the Contact Management Solutions (CCM)+ via the Ontario COVID-19 Modelling Consensus Table and Ontario Ministry of Health. We thank Kristy Yiu (MAP Centre for Urban Health Solutions, St. Michael's Hospital) for support with data management, and the Ontario Community Health Profiles Partnership.
Funding
This work was supported by the Canadian Institutes of Health Research (grant no. VR5-172683).
Footnotes
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.City of Toronto. COVID-19: Status of Cases in Toronto 2021 [Available from: https://www.toronto.ca/home/covid-19/covid-19-latest-city-of-toronto-news/covid-19-status-of-cases-in-toronto/, Accessed dates Feb 26, 2021.
- 2.Public Safety Canada. Guidance on Essential Services and Functions in Canada During the COVID-19 Pandemic 2021 [Available from: https://www.publicsafety.gc.ca/cnt/ntnl-scrt/crtcl-nfrstrctr/esf-sfe-en.aspx, Accessed dates Feb 26, 2021.
- 3.Deng Z, Messacar D, Morissette R. Running the economy remotely: Potential for working from home during and after COVID-19: Statistics Canada; 2020 [Available from: https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00026-eng.htm, Accessed dates Feb 26, 2021.
- 4.Ministry of Health, Ontario. How Ontario is responding to COVID-19 2021 [Available from: https://www.ontario.ca/page/how-ontario-is-responding-covid-19, Accessed dates Feb 26, 2021.
- 5.Statistics Canada. National Occupational Classification (NOC) 2016 Version 1.3 [Available from: https://www23.statcan.gc.ca/imdb/p3VD.pl?Function=getVD&TVD=1267777, Accessed dates Feb 26, 2021.
- 6.Statistics Canada. Visible Minority and Population Group Reference Guide, Census of Population, 2016 [Available from: https://www12.statcan.gc.ca/census-recensement/2016/ref/guides/006/98-500-x2016006-eng.cfm, Accessed dates Feb 26, 2021.
- 7.Canadian Institute for Health Information. COVID-19 Intervention Timeline in Canada. 2021 [Available from: https://www.cihi.ca/en/covid-19-intervention-timeline-in-canada, Accessed dates Feb 26, 2021.
- 8.City of Toronto. COVID-19: Changes to City Services. 2021 [Available from: https://www.toronto.ca/home/covid-19/covid-19-latest-city-of-toronto-news/affected-city-services/, Accessed dates Feb 26, 2021.
- 9.Office of the Premier, Ontario. Ontario Announces Provincewide Shutdown to Stop Spread of COVID-19 and Save Lives. 2020 [Available from: https://news.ontario.ca/en/release/59790/ontario-announces-provincewide-shutdown-to-stop-spread-of-covid-19-and-save-lives, Accessed dates Feb 26, 2021.
- 10.Science Table: COVID-19 Advisory for Ontario. Ontario Dashboard 2021 [Available from: https://covid19-sciencetable.ca/ontario-dashboard/, Accessed dates Feb 26, 2021.
- 11.Weill JA, Stigler M, Deschenes O, Springborn MR. Social distancing responses to COVID-19 emergency declarations strongly differentiated by income. Proc Natl Acad Sci U S A. 2020;117(33):19658–19660. doi: 10.1073/pnas.2009412117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen YH, Glymour M, Riley A, Balmes J, Duchowny K, Harrison R, et al. Excess mortality associated with the COVID-19 pandemic among Californians 18-65 years of age, by occupational sector and occupation: March through November 2020. PLoS One. 2021;16(6) doi: 10.1371/journal.pone.0252454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Statistics Canada. General Social Survey: Canadians at Work and Home (GSS) 2016 [Available from: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5221 Accessed dates Feb 26, 2021.
- 14.The University of British Columbia. Research Brief: Ability to work from home and paid sick leave benefits by precarious employment and socioeconomic status. 2020
- 15.Thompson A, Stall NM, Born KB, Gibson JL, Allen U, Hopkins J, et al. Benefits of paid sick leave during the COVID-19 pandemic. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021;2(25):1–13. [Google Scholar]
- 16.Jones RP. Federal sickness benefit falls short of paid sick leave protections, advocates say 2021 [Available from: https://www.cbc.ca/news/politics/federal-sickness-benefit-paid-sick-leave-1.5872913#:∼:text=Politics-,Federal%20sickness%20benefit%20falls%20short%20of%20paid%20sick%20leave%20protections,enough%20people%20who%20need%20it, Accessed dates Feb 26, 2021.
- 17.O'Donnell J. Essential workers during COVID-19: At risk and lacking union representation 2020 [Available from: https://www.brookings.edu/blog/up-front/2020/09/03/essential-workers-during-covid-19-at-risk-and-lacking-union-representation/#:∼:text=COVID%2D19%20and%20New%20Labor%20Market%20Challenges&text=Recent%20estimates%20suggest%20that%20low,from%20home%20than%20their%20peers, Accessed dates Feb 26, 2021.
- 18.Likely source of infection: graphs and tables of COVID-19 data by source of infection and outbreak setting. 2021 [Available from: https://covid-19.ontario.ca/data/likely-source-infection, Accessed dates Feb 26, 2021.
- 19.City of Toronto. COVID-19: Active Outbreaks 2021 [Available from: https://www.toronto.ca/home/covid-19/covid-19-latest-city-of-toronto-news/covid-19-pandemic-data/covid-19-active-outbreaks-data/, Accessed dates Feb 26, 2021.
- 20.To protect frontline workers during and after COVID-19, we must define who they are 2020 [Available from: https://www.brookings.edu/research/to-protect-frontline-workers-during-and-after-covid-19-we-must-define-who-they-are/, Accessed dates Feb 26, 2021.
- 21.How Ontario is responding to COVID-19 2021 [Available from: https://www.ontario.ca/page/how-ontario-is-responding-covid-19, Accessed dates Feb 26, 2021.
- 22.Kisling LA, MD J. StatPearls. Treasure Island (FL); 2020. Prevention Strategies. [Google Scholar]
- 23.Watsa V. Hopkins clinics bring vaccines to Baltimore City communities 2021 [Available from: https://www.hopkinsmedicine.org/coronavirus/equity/community-vaccine-clinics.html, Accessed dates Feb 26, 2021.