Abstract
Background
Stress on medical education caused by COVID-19 has prompted medical schools to bar their students from onsite education at hospitals and clinics, limiting their educational experiences. Radiology is uniquely positioned to be a virtual rotation during this health crisis and beyond.
Purpose
To implement virtual radiology clerkships and evaluate educational outcomes.
Methods
We developed virtual radiology clerkships using best practices from adult education theory; emphasizing self-directed and interactive learning through recommended reading materials, pre-recorded lectures, video conferencing, web-based learning modules from the ACR, as well as multimodality radiology resources to allow students flexibility in their individual approach to the subject matter.
Results
The mean performance on standardized exams for our cohorts was 75% (range 50–96%), matching the national average of 75%. Surveys of medical students after the clerkship showed positive subjective feedback on the content and structure of the course.
Conclusions
Understanding of medical imaging is vital for student doctors to have a better understanding of applied anatomy, patient care strategies, appropriate use, and image interpretation. Radiology is uniquely positioned to be taught in a virtual format, or in a combination of online and in-person activities. Standardized examination performance for our institutional virtual radiology clerkships is comparable to performance on traditional courses. Virtual clerkships designed with adult learners in mind can help student doctors prepare for residency and future independent practice as they build knowledge and skills needed to provide high quality patient care.
Keywords: Radiology, Virtual, Medical education, Adult education
1. Introduction
As the world grapples with the COVID-19 pandemic, academic institutions at all education levels have moved classes online to protect the health and wellness of their students and educators. Clinical training is generally not well situated for a virtual format, as direct patient care requires the trainee's physical presence. The unique technological and image rich nature of diagnostic radiology allows for educators to quickly adopt virtual clerkships. Although virtual radiology medical student rotations have been carried out for several years before the coronavirus outbreak, few publications examined educational outcomes in comparison to traditional courses. Results from our institutional experience with virtual radiology clerkships demonstrate their effectiveness as a viable alternative to on site rotations.1
2. Purpose
The purpose of our clerkship is to meet the academic needs of medical students while providing a safe environment during the COVID 19 pandemic. To accomplish this goal, our institution designed and implemented a 100% virtual radiology clerkship. By taking the best practices from adult education theories, the clerkship emphasizes self-directed and interactive learning through video conferencing and web-based learning platforms.2
A further objective of the project was to improve our residents' ability to teach. A virtual learning environment serves as the stepping stone for a proactive learning experience not only for student physicians but also for radiology trainees. Our small group sessions were led by radiology residents who actively engaged medical students through cases, sharing important imaging findings and inputting feedback.
3. Methods
In response to students no longer being permitted to physically attend hospital-based clerkships on site during the Spring of 2020, our institution created a 100% remote learning course to replace the observership model rotation we had previously offered. This 4-week self-paced format, which was offered to students at the beginning of their 3rd year, combined several strategies appropriate for adult learners while promoting social/professional distancing and maintaining high quality radiology education.
At the beginning of the clerkship, each student was given an introductory textbook and a range of radiology resources appropriate for their level of training to allow an individualized approach to the subject matter. Our radiology residency faculty provided a series of pre-recorded lectures based on the Alliance of Medical Student Educators in Radiology (AMSER) curriculum with selected supplemental recorded lectures from Alexander Street Press and YouTube. Students also completed a complimentary set of case-based modules offered through Aquifer (subscription-based service) for a structured approach to imaging algorithms and relevant patient care management strategies. Students were required to complete Radiology Technology-Enhanced Appropriateness Criteria Home for Education Simulation (TEACHES) modules from the ACR and recommended interactive modules from the ACR eLearning Rotation that promotes evidence-based guidelines in regards to patient management strategies, resource utilization and patient safety.3
To further enhance the educational experience for both the medical students and radiology residents weekly live small group “hot seat style” sessions on zoom were held. During these resident-led sessions, students took turns interpreting high-yield patient cases with an Objective Structured Clinical Examinations (OSCE) style approach to evaluate the students' ability to provide a differential diagnosis and answer follow up questions (Fig. 1 ). A 4-week schedule was provided (Fig. 2 ) including “office hours” during which faculty members provided insight into the field of radiology and to address more difficult concepts for the students. Attendance at weekly resident-run morning conferences, weekly tumor board meetings and daily noon conferences through Webex was encouraged.
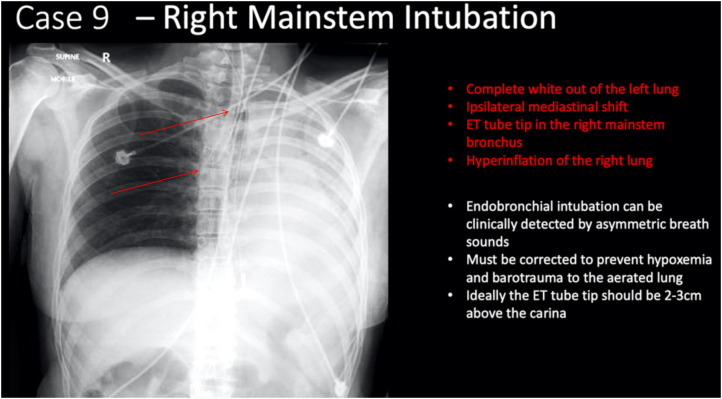
Fig. 1.
Example slide from “hot seat style” problem-based learning.
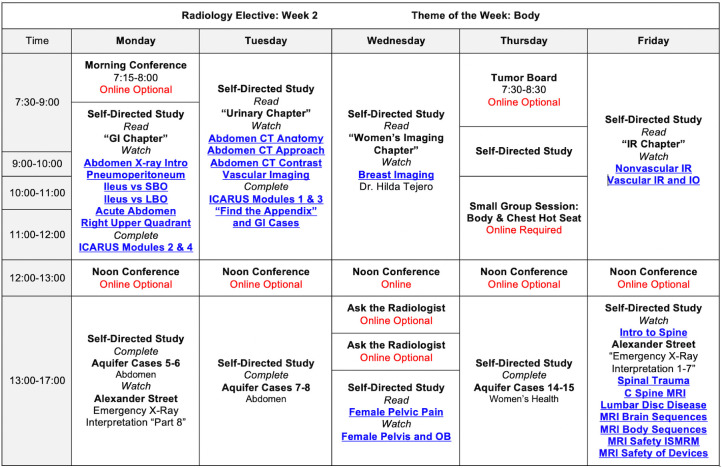
Fig. 2.
Sample schedule from a completely virtual 4-week radiology rotation.
During the final week of instruction, groups of students were tasked with creating a “grand rounds” style final presentation based on a patient scenario and evidence-based practice guidelines for the use of diagnostic imaging in similar cases. On completion of the course, student performance was assessed with the AMSER core examination, now relaunched as “ACR STARS”.
4. Results
The mean performance on the AMSER standardized exam for our cohorts was 75% (range 50–96%), matching the national average of 75%, t(40) = −0.14868, p = .881859 using a two-tailed t-test. Clerkship evaluations by the students showed positive subjective feedback on the content and structure. Participants emphasized that virtual self-directed learning allowed them to engage more fully in the material and use their time more effectively.
Residents reported improvement in their knowledge, leadership skills, search-patterns and ability to present findings in an eloquent manner.
5. Discussion
Best practices in adult learning are founded on the principles of andragogy. According to Cyril Houle and later expanded on by Malcom Knowles; adults benefit from greater control over their own education. By applying a greater emphasis on problem-centered and experiential learning, the subject matter had more direct relevance to their lives.6
All graduating medical students benefit from basic skills in image interpretation regardless of their chosen post graduate training path. Radiology training is vital for student doctors to have a better understanding of disease processes, applied anatomy and physiology and improving patient care strategies. Imaging interpretation skills are important for evaluation and management of patients, surgical planning, radiology-pathology correlation and to establish more effective discussions of medical imaging results with patients and their families. Physicians in medical and surgical fields should at least be able to recognize radiologic emergencies on call and to identify when to seek consultation of a radiologist; potentially quickening the path to diagnosis and treatment. Furthermore, understanding appropriate imaging criteria is crucial for optimal patients care, distribution of resources and prevention of unnecessary radiation exposure for patients.
Radiology instruction during medical school varies from little or no exposure to stand-alone clinical elective based on the institution. It has been shown that early radiology exposure allows students to better appreciate the role of imaging in medical practice.7 Radiology coursework also helps meet the Liaison Committee on Medical Education (LCME) accreditation requirements for the standards of medical knowledge, patient care, professionalism, systems-based practice, communication, and inter professional collaboration.8
Instruction in imaging interpretation provides an opportunity for students already considering a career in radiology to make a more confident and informed decision. New radiology residents with a robust background in the field will already possess fundamental building blocks for their future training.
Radiology residency training should ideally equip the trainee with skills for an academic future career. Radiology education in medical schools should be designed with this in mind, ideally promoting resident-led small group sessions to serve as the foundation for a future should they pursue a career in graduate medical education. Engaging radiology residents in the process provides opportunities for them to actively review cases in a multi-disciplinary approach by considering medical/surgical management and up to date guidelines for patient care.
Traditional observership models of simply shadowing a radiologist in the reading room can be stymied by variable levels of student participation, faculty engagement and an unpredictable case variety to prompt necessary teaching points. Virtual radiology rotations have the potential to improve access to radiology teaching despite physical barriers, with standardized teaching files to better prepare student doctors for future practice. The COVID-19 pandemic forced many academic radiology departments to develop their own virtual electives or implement the ACR eRotation as a replacement for in-person activities.1 Strengths in the design of our virtual radiology clerkships included the ability for students to govern the pace and method of education; incorporating multimodality resources to further their knowledge and understanding. Small group “hot seat style” sessions and high value faculty presentations are opportunities to further engaged students and allowed them to connect radiology lessons with clinical practice. These activities also introduced transformational learning for students, allowing them to re-examine their own role and the role of medical imaging within a broader health system. Videoconferences and web-based learning platforms allowed for a variety of formats, with similar standardized exam results of these courses compared to traditional in person courses.4., 5.
6. Conclusion
Through our institutional experience we aim to demonstrate the effectiveness of virtual radiology clerkships as viable alternatives to on site rotations. The virtual learning environment serves as the steppingstone for a proactive learning experience not only for student physicians but also for radiology residents. Performance by students in this 100% virtual radiology clerkship matched that of other courses on a national standardized examination. The success of this approach holds promise for delivering high quality radiology experience for students who would otherwise be unable to complete a radiology clerkship due to logistical reasons or competing demands on their time for residency interviews, international volunteer trips, personal or family reasons, etc. Virtual radiology clerkships designed with andragogy and self-directed learning principles permit students to invest in their own learning process, building knowledge and skills needed to provide high quality patient care in the future.
All authors made substantial contributions to the design of the work; interpretation of data, drafting the work, revising it, final approval of the version to be published and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
The authors declare that they had full access to all of the data in this study and the authors take complete responsibility for the integrity of the data and the accuracy of the data analysis. Neither the authors nor their immediate family members have a financial relationship with a commercial organization that may have a direct or indirect interest in the content.
The authors declare no conflicts of interest.
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
References
- 1.ACR Radiology E-Rotation Compiled and Provided by Benjamin Hyatt Taragin, MD https://www.acr.org/-/media/ACR/Files/Member-Resources/Med-Students/Radiology-eLearning-Rotation.pdf accessed 4/10/20.
- 2.Slanetz P.J., Naeger D.M., Avery L.L., Deitte L.A. Mixed practice in radiology education-has the time Come? J Am Coll Radiol. 2020 Jul;17(7):976–978. doi: 10.1016/j.jacr.2019.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Lewis P, Shaffer K. AMSER National Medical Student Curriculum in Radiology. https://www.mededportal.org/doi/10.15766/mep_2374-8265.7897 accessed 4/15/20.
- 4.Durfee S.M., Goldenson R.P., Gill R.R., Rincon S.P., Flower E., Avery L.L. Medical student education roadblock due to COVID-19: virtual radiology core clerkship to the rescue. Acad Radiol. 2020 Oct;27(10):1461–1466. doi: 10.1016/j.acra.2020.07.020. Epub 2020 Jul 24. PMID: 32747181; PMCID: PMC7380233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alexander A.G., Deas D., Lyons P.E. An internet-based radiology course in medical school: comparison of academic performance of students on campus versus those with absenteeism due to residency interviews. JMIR Med Educ. 2018 May;4(1) doi: 10.2196/mededu.8747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Knowles M and Associates . Jossey-Bass; San Francisco: 1984. Andragogy in action: Applying modern principles of adult learning. [Google Scholar]
- 7.Gunderman R.B., Siddiqui A.R., Heitkamp D.E., Kipfer H.D. The vital role of radiology in the medical school curriculum. Am J Roentgenol. 2003;180(5):1239–1242. doi: 10.2214/ajr.180.5.1801239. [DOI] [PubMed] [Google Scholar]
- 8.LCME Standards, Publications, & Notification Forms 2020. https://lcme.org/publications/ Published. accessed 10/21/20.