Abstract
Objective
To evaluate the efficacy and safety of mesenchymal stem cells (MSCs) therapy in patients with tendon disorders enrolled in prospective clinical studies.
Methods
We systematically searched prospective clinical studies that investigated the effects of MSC administration on human tendon disorders with at least a 6-month follow-up period in the PubMed-MEDLINE, EMBASE, and Cochrane Library databases. The primary outcome of interest was the change in pain on motion related to tendon disorders. Meta-regression analyses were performed to assess the relationship between MSC dose and pooled effect sizes in each cell dose.
Results
Four prospective clinical trials that investigated the effect of MSCs on tendon disorders were retrieved. MSCs showed a significant pooled effect size (overall Hedges’ g pooled standardized mean difference=1.868; 95% confidence interval, 1.274–2.462; p<0.001). The treatment with MSCs improved all the aspects analyzed, namely pain, functional scores, radiological parameters (magnetic resonance image or ultrasonography), and arthroscopic findings. In the meta-regression analysis, a significant cell dose-dependent response in pain relief (Q=9.06, p=0.029) was observed.
Conclusion
Our meta-analysis revealed that MSC therapy may improve pain, function, radiological, and arthroscopic parameters in patients with tendon disorders. A strong need for large-scale randomized controlled trials has emerged to confirm the long-term functional improvement and adverse effects of MSC therapies in tendon disorders.
Keywords: Mesenchymal stem cells, Tendinopathy, Rotator cuff, Tennis elbow, Meta-analysis
INTRODUCTION
Mesenchymal stem cell (MSC) treatment is a new regenerative therapy for treating tendon disorders. Preclinical studies have reported that MSC therapy may increase the number of tenocytes and regenerate the injured tendon tissue [1-4]. While several studies with animals support the treatment of tendon disorders using MSCs, little is known about the efficacy and safety of MSCs to treat these conditions in humans. Although a few clinical reports suggested the therapeutic potentials of MSCs in tendon disorders, they are mostly case reports or case series.
A systematic review of MSC therapy on tendon disorder [5] analyzed three case series [6-8] and one matched non-randomized trial [9]. The authors concluded that MSC treatment is not yet suitable for clinical practice because the included studies are at high risk of bias. However, the result should be reconsidered, as three [6,7,9] of the four studies included in this review were not performed with isolated MSCs but with bone marrow aspirates or stromal vascular fractions cells. Moreover, this study was not conducted with a meta-analysis methodology, which combines the results from multiple studies. Furthermore, two current clinical studies [10,11] that used isolated MSCs on tendon disorder were not included in the review.
Although an increasing number of research studies on stem cell treatments have been published, no meta-analyses have been conducted on this topic to date. Furthermore, concerns regarding the possible adverse events of MSC treatments that were raised by physicians or scientists reluctant to the therapy [12] should be thoroughly reviewed. Thus, we performed an updated meta-analysis of the prospective clinical studies to evaluate the efficacy and safety of MSC therapies in patients with tendon disorders.
MATERIALS AND METHODS
The meta-analysis was conducted in accordance with the updated guidelines of the Preferred Reporting Items for Systematic review and Meta-Analysis Protocols (PRISMA-P) [13]. Searches on PubMed-MEDLINE, EMBASE, and the Cochrane Library were performed in March 2021 by using the following key terms and syntax: (Tendinopathy OR Tendon OR Tendon disorder OR Tendon injuries OR Tendinosis OR Tendinitis OR Tennis elbow OR Elbow Tendinopathy OR Lateral epicondylitis OR Lateral epicondylosis OR Golfer’s elbow OR Rotator cuff OR Rotator Cuff Injuries OR De Quervain disease OR Jumper’s knee OR Achilles tendon) AND (Stem cells OR Mesenchymal stem cells OR Progenitor cells OR Mother cells OR Multipotent OR Pluripotent OR Totipotent) AND Clinical studies [14,15]. An overview of the search strategy is presented in Supplement A. We included all prospective clinical studies that investigated the effects of MSC administration on tendon disorders. We imposed no language restriction. We also searched for unpublished and gray literature using the following databases and trial registries: World Health Organization Clinical Trial Register, EU clinical trials register, ClinicalTrials.gov, and OpenGrey.
Identified records were saved to the EndNote software (X7.2; Thomson Reuters). Two independent reviewers (WSC and SYL) screened all the titles and abstracts to identify relevant investigations. The inclusion criteria were as follows: (1) articles reporting a prospective clinical study with at least a 6-month follow-up that (2) described the effect of MSC therapy in patients with any tendon disorder. Although no limitations were set for the types of MSCs, that is, cell origin, either autologous or allogeneic, we excluded studies that did not use isolated MSCs such as bone marrow aspirates or stromal vascular fractions cells. Reviews, basic science articles, comments, letters, and protocols were excluded. When updates of earlier studies were available, we used only the most recent ones.
The primary outcome of interest was defined as pain on motion related to tendon disorders. All types of pain measurements such as visual analog scale or numerical rating scale were included. The secondary outcomes analyzed in this study were as follows: (1) joint function scores such as the Constance score, University of California Los Angeles (UCLA) score, modified Mayo Elbow Performance Index, or Shoulder Pain and Disability Index; (2) radiological parameters to measure tendon defects using magnetic resonance imaging (MRI) or ultrasonography; and (3) arthroscopic findings to measure tendon defects with a calibrated arthroscopic probe. For every eligible study, the following data were extracted and entered into a spreadsheet by the two reviewers (WSC and SYL): first author’s family name, year of publication, study design, types of tendon disorder, origin of the MSCs, number of patients, MSC injection methods, cell dose, follow-up duration, safety assessment, and efficacy measurement. We assessed publication bias using the Begg funnel plot [16] and Egger test [17].
Effect sizes were computed as standardized mean difference (SMD) measures [18], representing the magnitude of the pretest-posttest difference for each outcome. SMD was calculated separately for all the available control and treatment groups for each study. Heterogeneity between comparable studies was tested with the chisquare (χ2) and I2 tests. p-values >0.1 and I2 values <50% were considered statistically significant. As no significant heterogeneity was observed among the four studies (p=0.658 and I2=0.0%), we used a fixed-effects metaanalysis to quantify the pooled effect size of the studies included. In each analysis by outcome, the following parameters were also analyzed using the fixed-effects model: pain (p=0.093 and I2=47.0%), functional scores (p=0.313 and I2=15.3%), radiological parameters (p=0.406 and I2=0.0%), and arthroscopic findings (p=0.588 and I2=0.0%). In addition, we performed a meta-regression analysis to assess the relationship between the MSC dose and the pooled effect size in each cell dose. All analyses were performed using the Comprehensive Meta-Analysis version 3.3 software (Biostat, Englewood, NJ, USA). This study was exempted from the Institutional Review Board review, as no human subjects were involved.
RESULTS
The primary database search yielded 1,135 records. After duplicates were removed, the titles and abstracts of 897 articles were initially screened, of which 25 were selected for full-text review. The full-text articles were read, and four articles were considered relevant by qualitative analysis [8,10,11,19]. The studies selected for final inclusion or exclusion are shown in Fig. 1, and the characteristics of the included studies are summarized in Table 1. In terms of quantitative analysis, these four studies (published from 2015 to 2019) fulfilled our inclusion criteria.
Fig. 1.
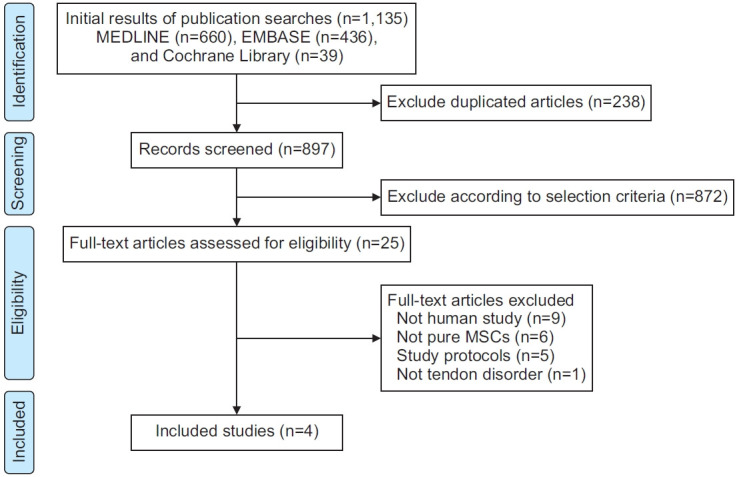
The Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISRMA) flow diagram detailing the selection process of relevant clinical studies.
Table 1.
Characteristics of the individual studies included
| Study | Region | Study period | Study design | N | Tendon disorder | MSC origin (type) | Injection method | MSC dose (cells) | F/U period (mo) | Safety | Efficacy |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary | Secondary | |||||||||||
| Lamas et al. [11], 2019 | Spain | Jan 2011–Nov 2012 | Double-blind randomized controlled trial | 13 | Full-thickness rotator cuff tear | Autologous bone marrow-derived MSCs | Surgical repair with attached with OrthADAPT membrane | 2.0×107 | 12 | Examined but not mentioned (the trial was stopped due to adverse effects) | Constant score | Tendon status by MRI pain (VAS) |
| Jo et al. [19], 2018 | South Korea | Jul 2015–Nov 2016 | Open-label, dose-escalation trial | 19 | Partial-thickness rotator cuff tear | Autologous adipose tissue-derived MSCs | Intratendinous injection under the US guidance, MSCs in 3 mL of saline | 1.0×107, 5.0×107, 1.0×108 | 6 | NCI-CTCAE v 4.0 | SPADI | Constant score, pain (VAS) shoulder MRI (tendon defects), arthroscopy |
| Lee et al. [8], 2015 | South Korea | May 2013–Sep 2014 | Open-label, conventional 3+3 cohort expansion design | 12 | Lateral epicondylitis | Allogeneic adipose tissue-derived MSCs | Intratendinous injection under the US guidance, MSCs with fibrin glue (total volume of 1 mL) | 1.0×106, 1.0×107 | 12 | Local/systemic tolerances, US exam | Pain (VAS) | Modified mayo elbow performance index, elbow US (tendon defects) |
| Havlas et al. [10], 2015 | Czech Republic | Oct 2012 | Prospective study with consecutive participants | 8 | Rotator cuff tear | Autologous bone marrow-derived MSCs | Arthroscopic repair and suspension of MSCs to the suture site | (1.0±0.45)×107 | 6 | Local and systematic adverse reactions (not clearly described) | Pain (VAS) | Constant score, UCLA score |
MSCs, mesenchymal stem cells; F/U, follow-up; MRI, magnetic resonance imaging; VAS, visual analog scale; US, ultrasonography; NCI-CTCAE, National Cancer Institute-Common Terminology Criteria for Adverse Events; SPADI, Shoulder Pain and Disability Index; UCLA, University of California at Los Angeles.
Three papers [8,10,19] were open-label prospective studies, while one [11] was a double-blind randomized controlled trial. The studies identified for meta-analysis included 52 participants. In two studies [8,19], adipose tissue-derived MSCs were used, and in the other two [10,11], bone marrow-derived MSCs were administered. The number of cells used in each study ranged from 106 to a maximum of 108. Regarding tendon disorder types, most of the studies conducted were on rotator cuff tears, but one study [8] was on lateral epicondylitis. The followup duration ranged from 6 to 12 months.
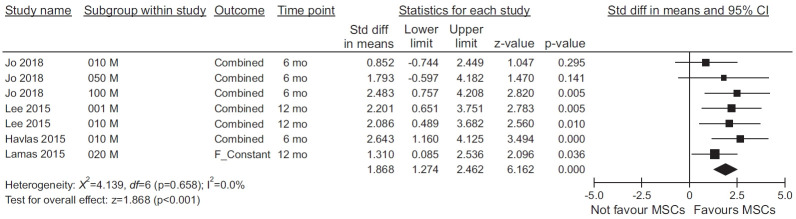
The MSC therapies showed a significant pooled effect size (overall Hedges’ g pooled SMD=1.868; 95% confidence interval [CI], 1.274–2.462; p<0.001) (Fig. 2). The pain parameters, functional scores, radiological parameters (MRI or ultrasonography findings), and arthroscopic findings all improved with MSC treatment (Fig. 3). In the meta-regression analysis, a significant cell dosedependent response in pain relief (Q=9.06, p=0.029) was observed (Fig. 4). While three studies reported mild adverse events after MSC injection, these were not severe and were relieved spontaneously (Table 2). Publication bias was not evident, as shown by the symmetrical Begg’s funnel plot (Supplement B), and the p-value for bias was 0.625 (Egger test; all four trials).
Fig. 2.
Forest plot of the pooled effect of mesenchymal stem cells (MSCs) on tendon disorders determined by a fixed-effects meta-analysis. Effect sizes are indicated as Hedges’ g standardized mean differences and 95% confidence intervals.
Fig. 3.
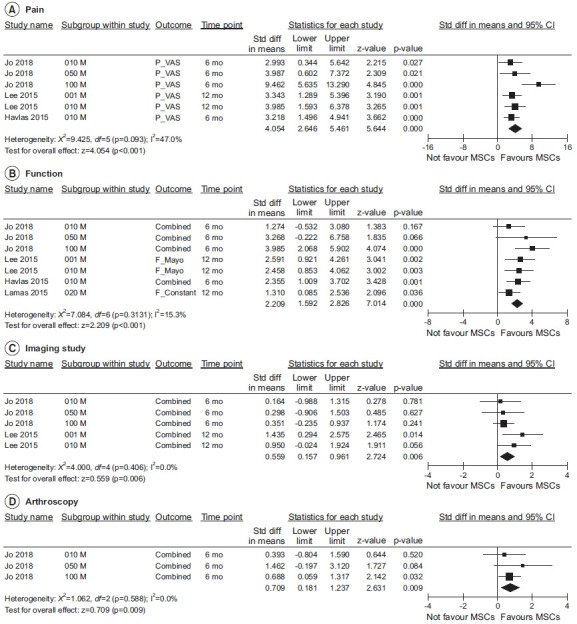
Forest plots of the effects of trial/cell dose-level characteristics of mesenchymal stem cells (MSCs) analyzed as outcome variables: (A) pain (primary outcome), (B) functional scores, (C) radiological parameters, and (D) arthroscopic findings.
Fig. 4.
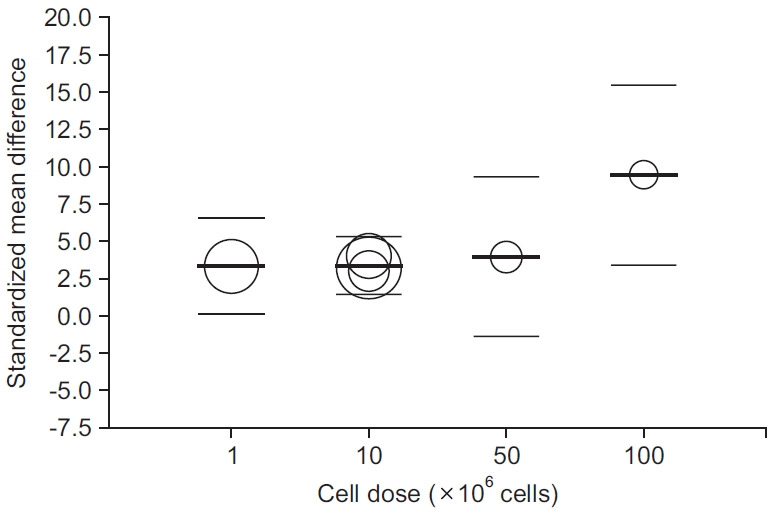
Meta-regression of the standardized mean differences in means for cell doses. The area of the circles is proportional to the weights of the studies in the regression.
Table 2.
Adverse events reported in individual studies included
| Study | Adverse events | N | Treatment | Prognosis | Treatment-related |
|---|---|---|---|---|---|
| Lamas et al. [11], 2019 | Supraclavicular cyst and subacromial inflammatory tissue (foreign body like reaction) | 4 | Surgery (remove the scaffold) | Recovered | Yes |
| Jo et al. [19], 2018 | Back pain | 3 | Rescue drug, physical therapy | Recovered | No |
| Right foot bruise, left trigger finger | 1 | Rescue drug, physical therapy | Recovered | No | |
| Cough | 1 | Medication | Recovered | No | |
| Left eye pain | 1 | Eye drop | Recovered | No | |
| Abdominal pain | 1 | Medication | Recovered | No | |
| Lee et al. [8], 2015 | Mild regional swelling | 6 | Observation | Recovered | Yes |
| Mild elbow joint effusion | 2 | Observation | Recovered | Yes | |
| Delayed elbow pain | 1 | Rescue drug | Recovered | No |
DISCUSSION
Potential evidence has shown that MSC injection improves pain, joint functional, radiological, and arthroscopic parameters in patients with tendon disorders. Although all the included studies had a small sample size, the results clearly presented MSC dose-dependent responses regarding pain relief. To the best of our knowledge, this is the first clinical meta-analysis describing the pooled effects of MSC therapies in patients with tendon disorders.
Tendon injuries are a common health problem, which are defined as painful conditions occurring around tendons that limit the function of the affected tendons [20]. Tendons are susceptible to repeated use or degenerative condition. Injuries in those structures are rarely regenerated but repaired by scar tissue and fibrosis. The healed tissue presents inferior tensile strength and is prone to further injuries. Preclinical studies support that MSCs have a regenerative potential, as they can differentiate into targeted tissues and replace injured resident cells [1]. Therefore, MSC administration has been regarded as a possible curative treatment option for tendon degeneration.
Implanted stem cells survive in tendon defects, differentiate into the tenogenic cell lineage, and secrete their own extracellular matrix to promote tendon healing [4]. Mazzocca et al. [21] showed that bone marrow-derived stem cells differentiated into tendon-like cells. Lee et al. [4] also reported that transplanted human adipose tissue-derived stem cells survived for at least 4 weeks in the rat tendon injury model and released human-specific collagen type I and tenascin C (TnC). TnC expression is known to increase rapidly during the early period of recovery after tendon injuries and thereby used as a marker of tenogenic differentiation [22].
In this meta-analysis, three of the four included studies examined radiological data (MRI or ultrasonography) or arthroscopic findings after MSC injections. These tests could confirm that the injected cells not only relieved pain and improved functions but also regenerated the damaged tissue. Noteworthy, Jo et al. [19] conducted the second-look arthroscopic examination at 6 months after MSC injection and MRI follow-up. They reported that regenerated tendon tissues were identified in all the subjects regardless of the location and size of the tear. The defect volumes were decreased in the patients who received mid (5.0×107 cells) and high doses (1.0×108 cells). Although this is a macroscopic observation, it may be considered as strong supporting evidence for the regeneration effect of MSCs.
The benefits of MSCs in the treatment of tendon disorders are not confined to their differentiation potential alone. Another important biological mechanism that supports the use of MSC therapy is that MSCs release diverse cytokines, chemokines, and growth factors [1]. Several studies found that these secreted factors may stimulate their proliferation, allowing the promotion of tissue regeneration. The benefits of MSC-conditioned media proven by in vitro studies also encourage the paracrine effects of MSCs. Kinnaird et al. [23] found that the growth of endothelial cells and smooth muscle cells may be promoted by the use of medium conditioned with MSCs. This phenomenon might be partly explained by the presence of VEGF (vascular endothelial growth factor) and bFGF (basic fibroblast growth factor), which appeared in high levels in a MSC-conditioned medium [24]. They can recruit macrophages and endothelial cells into the injured site, allowing enhancement of the healing process.
The ability of the MSCs to produce a wide range of immunomodulatory factors has also attracted great attention [25]. Both in vitro and in vivo studies have elicited that MSCs can downregulate the excessive response of numerous immune cells such as T cells, B cells, dendritic cells, macrophages, and natural killer cells. MSCs can also induce regulatory T cells and thereby expand and maintain a long-lasting immune-modulating activity, which is similar to the role of catalysts. Considering that the inflammation-derived tissue damage is one of the key processes in most tendon disorders, immunomodulation induced by injected MSCs can also play an important role in promoting treating tendon diseases, in addition to their differentiation potential and paracrine effects [26].
Several concerns remain regarding the use of MSCs as a treatment option for tendon disorders. Potential long-term adverse events from the stem cell treatment have been poorly reported in several clinical studies. In the studies included in this meta-analysis, most of the reported adverse events were not related to the treatment (Table 2). The treatment-related side effects were mild joint effusion and regional swelling after allogeneic stem cell injection [8] or engrafted patch-related foreign body reaction [11]. The joint swelling spontaneously subsided, while the patch-related adverse event needed additional surgery. Considering the prognosis of the reported adverse events, these side effects might have come from the localized inflammatory response related to the treatment procedure itself, or immunological response against allogeneic cells, but are less likely to have arisen from the MSC itself.
The safety issues related to the use of MSCs have already been sufficiently assessed in clinical trials in the field of internal medicine, in which MSCs are injected systemically. The POSEIDON trial [27] was designed to investigate the safety and efficacy of autologous and allogeneic MSC therapies for ischemic cardiomyopathy. The study reported that after trans-endocardial stem cell injection, the treated group showed improvement in structural and functional outcomes, while no serious adverse events, including immunologic reactions occurred. Indeed, the long-term adverse events from and possible teratogenicity of the stem cell treatment should be thoroughly considered. One animal study reported undesired cartilage formation after the injection of human MSCs in 81 rat tendon injury models [28]. While no histological evidence of tumor formation was found in the study, concerns for possible teratogenicity still remain.
Although numerous challenges still need to be overcome and analyzed, MSC therapy can be a promising treatment option for tendon disorders. Approximately 17% of patients with tendon disorders are known to have no effects after undergoing conservative treatment for >1 year [29]. In some patients, the rate of retear is fairly high, even after surgical repair for tendon injuries [19]. Thus, the limitations of the current therapies suggest a need for more fundamental regenerative treatments, and MSCs might offer a regenerating opportunity for the tendon by yielding a more robust repaired tissue [30]. For MSC injections to be established in tendon disorders, the aforementioned long-term safety issues should be better verified. Furthermore, well-designed clinical trials should be performed to support the evidence.
This meta-analysis has several limitations. First, we included a limited number of studies in our meta-analysis. Moreover, only one randomized controlled study was available. As MSCs have been applied for the treatment of tendon disorder for only a short time, the number of studies that fulfilled our criteria was limited. If a sufficient number of studies had been analyzed, more solid evidence could have been obtained. However, it is meaningful to combine the data through a meta-analysis because related studies are inadequate. Second, the outcome variables showed heterogeneity among the included trials. Three studies [10,11,19] used the Constant score for functional assessment, while one study used the modified Mayo Elbow Performance Index [8], and two studies additionally used the UCLA score [10] and Shoulder Pain and Disability Index [19], respectively. Although we used the combined pooled effect sizes to deal with this issue, the effect sizes should be cautiously interpreted from the clinical point of view. Furthermore, the heterogeneities of the MSC origin and target tissue were also limitations of this analysis. Two studies were performed with the administration of bone marrow-derived MSCs [10,11], while the other two studies used adipose tissue-derived MSCs [8,19]. The specific tendon disorders presented in the studies were also different, namely three studies aimed at treating the rotator cuff disease and one, lateral epicondylitis. And two studies added MSCs injection therapy to surgical treatment [10,11], and the other two studies confirmed the effect of MSCs injection therapy alone [8,19]. However, to assure that the mechanisms and efficacy of MSC therapies in tendon disorder are clear and evident, whether these treatments are suitable for not just a single specific tendinopathy but also for other tendon disorders, which may involve various musculoskeletal structure, must be evaluated.
In conclusion, our meta-analysis revealed that MSC therapy may improve pain, function, and radiological and arthroscopic parameters in patients with tendon disorders. Owing to the limited sample size of this meta-analysis and considering the increasing MSC applications, large-scale randomized controlled trials are strongly needed to confirm the long-term functional improvement and adverse effects of MSC therapies in tendon disorders.
Acknowledgments
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2019R1C1C100632).
Footnotes
No potential conflict of interest relevant to this article was reported.
Conceptualization: Cho WS, Chung SG, Kim W, Jo CH, Lee SH, Lee SY. Data curation: Cho WS, Lee SY. Formal analysis: Cho WS, Lee SY. Funding acquisition: Lee SY. Investigation: Cho WS, Chung SG, Kim W, Jo CH, Lee SH, Lee SY. Methodology: Cho WS, Lee SY. Project administration: Cho WS, Lee SY. Resources: Cho WS, Lee SY. Supervision: Chung SG, Kim W, Jo CH, Lee SH. Visualization: Cho WS, Lee SY. Writing – original draft: Cho WS, Lee SY. Writing – review & editing: Cho WS, Chung SG, Kim W, Jo CH, Lee SH, Lee SY.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via http://doi.org/10.5535/arm.21078.
Searching queries
Funnel plot of standard error by standardized difference in means
REFERENCES
- 1.Young M. Stem cell applications in tendon disorders: a clinical perspective. Stem Cells Int. 2012;2012:637836. doi: 10.1155/2012/637836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barboni B, Russo V, Gatta V, Bernabo N, Berardinelli P, Mauro A, et al. Therapeutic potential of hAECs for early Achilles tendon defect repair through regeneration. J Tissue Eng Regen Med. 2018;12:e1594–e1608. doi: 10.1002/term.2584. [DOI] [PubMed] [Google Scholar]
- 3.Liao GP, Choi Y, Vojnits K, Xue H, Aroom K, Meng F, et al. Tissue engineering to repair diaphragmatic defect in a rat model. Stem Cells Int. 2017;2017:1764523. doi: 10.1155/2017/1764523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee SY, Kwon B, Lee K, Son YH, Chung SG. Therapeutic mechanisms of human adipose-derived mesenchymal stem cells in a rat tendon injury model. Am J Sports Med. 2017;45:1429–39. doi: 10.1177/0363546517689874. [DOI] [PubMed] [Google Scholar]
- 5.Pas HI, Moen MH, Haisma HJ, Winters M. No evidence for the use of stem cell therapy for tendon disorders: a systematic review. Br J Sports Med. 2017;51:996–1002. doi: 10.1136/bjsports-2016-096794. [DOI] [PubMed] [Google Scholar]
- 6.Pascual-Garrido C, Rolon A, Makino A. Treatment of chronic patellar tendinopathy with autologous bone marrow stem cells: a 5-year-followup. Stem Cells Int. 2012;2012:953510. doi: 10.1155/2012/953510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ellera Gomes JL, da Silva RC, Silla LM, Abreu MR, Pellanda R. Conventional rotator cuff repair complemented by the aid of mononuclear autologous stem cells. Knee Surg Sports Traumatol Arthrosc. 2012;20:373–7. doi: 10.1007/s00167-011-1607-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee SY, Kim W, Lim C, Chung SG. Treatment of lateral epicondylosis by using allogeneic adipose-derived mesenchymal stem cells: a pilot study. Stem Cells. 2015;33:2995–3005. doi: 10.1002/stem.2110. [DOI] [PubMed] [Google Scholar]
- 9.Hernigou P, Flouzat Lachaniette CH, Delambre J, Zilber S, Duffiet P, Chevallier N, et al. Biologic augmentation of rotator cuff repair with mesenchymal stem cells during arthroscopy improves healing and prevents further tears: a case-controlled study. Int Orthop. 2014;38:1811–8. doi: 10.1007/s00264-014-2391-1. [DOI] [PubMed] [Google Scholar]
- 10.Havlas V, Kotaska J, Konicek P, Trc T, Konradova S, Koci Z, et al. [Use of cultured human autologous bone marrow stem cells in repair of a rotator cuff tear: preliminary results of a safety study] Acta Chir Orthop Traumatol Cech. 2015;82:229–34. [PubMed] [Google Scholar]
- 11.Lamas JR, Garcia-Fernandez C, Tornero-Esteban P, Lopiz Y, Rodriguez-Rodriguez L, Ortega L, et al. Adverse effects of xenogenic scaffolding in the context of a randomized double-blind placebo-controlled study for repairing full-thickness rotator cuff tears. Trials. 2019;20:387. doi: 10.1186/s13063-019-3504-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wohn DY. Korea okays stem cell therapies despite limited peer-reviewed data. Nat Med. 2012;18:329. doi: 10.1038/nm0312-329a. [DOI] [PubMed] [Google Scholar]
- 13.Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. doi: 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- 14.Tsikopoulos K, Tsikopoulos I, Simeonidis E, Papathanasiou E, Haidich AB, Anastasopoulos N, et al. The clinical impact of platelet-rich plasma on tendinopathy compared to placebo or dry needling injections: a meta-analysis. Phys Ther Sport. 2016;17:87–94. doi: 10.1016/j.ptsp.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 15.Ranger TA, Wong AM, Cook JL, Gaida JE. Is there an association between tendinopathy and diabetes mellitus? A systematic review with meta-analysis. Br J Sports Med. 2016;50:982–9. doi: 10.1136/bjsports-2015-094735. [DOI] [PubMed] [Google Scholar]
- 16.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101. [PubMed] [Google Scholar]
- 17.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Becker BJ. Synthesizing standardized mean‐change measures. Br J Math Stat Psychol. 1988;41:257–78. [Google Scholar]
- 19.Jo CH, Chai JW, Jeong EC, Oh S, Kim PS, Yoon JY, et al. Intratendinous injection of autologous adipose tissuederived mesenchymal stem cells for the treatment of rotator cuff disease: a first-in-human trial. Stem Cells. 2018;36:1441–50. doi: 10.1002/stem.2855. [DOI] [PubMed] [Google Scholar]
- 20.Andres BM, Murrell GA. Treatment of tendinopathy: what works, what does not, and what is on the horizon. Clin Orthop Relat Res. 2008;466:1539–54. doi: 10.1007/s11999-008-0260-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mazzocca AD, McCarthy MB, Chowaniec DM, Cote MP, Arciero RA, Drissi H. Rapid isolation of human stem cells (connective tissue progenitor cells) from the proximal humerus during arthroscopic rotator cuff surgery. Am J Sports Med. 2010;38:1438–47. doi: 10.1177/0363546509360924. [DOI] [PubMed] [Google Scholar]
- 22.Nemoto M, Kizaki K, Yamamoto Y, Oonuma T, Hashizume K. Tenascin-C expression in equine tendonderived cells during proliferation and migration. J Equine Sci. 2013;24:17–24. doi: 10.1294/jes.24.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kinnaird T, Stabile E, Burnett MS, Shou M, Lee CW, Barr S, et al. Local delivery of marrow-derived stromal cells augments collateral perfusion through paracrine mechanisms. Circulation. 2004;109:1543–9. doi: 10.1161/01.CIR.0000124062.31102.57. [DOI] [PubMed] [Google Scholar]
- 24.Yoon S, Kang JJ, Kim J, Park S, Kim JM. Efficacy and safety of intra-articular injections of hyaluronic acid combined with polydeoxyribonucleotide in the treatment of knee osteoarthritis. Ann Rehabil Med. 2019;43:204–14. doi: 10.5535/arm.2019.43.2.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liang X, Ding Y, Zhang Y, Tse HF, Lian Q. Paracrine mechanisms of mesenchymal stem cell-based therapy: current status and perspectives. Cell Transplant. 2014;23:1045–59. doi: 10.3727/096368913X667709. [DOI] [PubMed] [Google Scholar]
- 26.Squillaro T, Peluso G, Galderisi U. Clinical trials with mesenchymal stem cells: an update. Cell Transplant. 2016;25:829–48. doi: 10.3727/096368915X689622. [DOI] [PubMed] [Google Scholar]
- 27.Hare JM, Fishman JE, Gerstenblith G, DiFede Velazquez DL, Zambrano JP, Suncion VY, et al. Comparison of allogeneic vs autologous bone marrow–derived mesenchymal stem cells delivered by transendocardial injection in patients with ischemic cardiomyopathy: the POSEIDON randomized trial. JAMA. 2012;308:2369–79. doi: 10.1001/jama.2012.25321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Machova Urdzikova L, Sedlacek R, Suchy T, Amemori T, Ruzicka J, Lesny P, Havlas V, Sykova E, Jendelova P. Human multipotent mesenchymal stem cells improve healing after collagenase tendon injury in the rat. Biomed Eng Online. 2014;13:42. doi: 10.1186/1475-925X-13-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet. 2010;376:1751–67. doi: 10.1016/S0140-6736(10)61160-9. [DOI] [PubMed] [Google Scholar]
- 30.Carballo CB, Lebaschi A, Rodeo SA. Cell-based approaches for augmentation of tendon repair. Tech Shoulder Elb Surg. 2017;18:e6–e14. doi: 10.1097/BTE.0000000000000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Searching queries
Funnel plot of standard error by standardized difference in means