Abstract
Purpose
This study aimed to identify the extent of antenatal care content received and associated factors among Ethiopian women.
Methods
A nationally representative Performance Monitoring for Action 2020 Ethiopian data were used. A multistage cluster sampling design was used to select 2855 pregnant or recently postpartum women nested within 217 enumeration areas. Female resident enumerators collected the data using a semi-structured questionnaire. Researchers dichotomized the number of ANC content received greater than or equal to 75 percentiles as adequate. Otherwise, it was considered inadequate. A multilevel Poisson regression was fitted. The result was reported using an incidence rate ratio with a 95% confidence interval and a p-value less than 0.05 was considered for statistical significance.
Results
The study revealed more than a quarter of pregnant women received adequate ANC content (27.8%; 95% CI: 23.8%, 32.2%). Multivariable analysis revealed urban residence (IRR = 1.09, 95% CI: 1.01, 1.21), attending secondary and above formal education (IRR = 1.08, 95% CI: 1.01, 1.16), maternal age 20–24 years (IRR = 1.10, 95% CI: 1.02, 1.19), and partner’s encouragement to attend clinic for antenatal care (IRR = 1.14, 95% CI: 1.05, 1.24) was significantly associated with receiving higher numbers of antenatal care content.
Conclusion
The proportion of women who received adequate antenatal care content in Ethiopia was low. Despite Ethiopia’s effort to improve maternal health services utilization, disparities among regions and between rural and urban exist. This study highlights the importance of ensuring high received antenatal care content, which is crucial for reducing pregnancy-related morbidity and mortality. This implies prompt intersectoral collaboration to promote female education, target older aged women, and rural resident women, encourage partner involvements during the antenatal care process, minimize regional variation, and strengthen the implementation of received ANC content policies and programs with the active participation of the stakeholders are priority issues.
Keywords: received, ANC contents, associated factors, Ethiopia
Introduction
The antenatal care (ANC) period is the opportune time for early diagnosis of obstetric conditions, creating awareness of pregnancy danger signs, discussing the benefits of breastfeeding, and family planning. Hence it is a vital element of the continuum of care for women and newborns.1–3 Ethiopia has adopted the World Health Organization (WHO) recommendation of a minimum of four focused ANC visits during pregnancy. The components include blood pressure screening; weight and uterine height measurements; check for pallor, fetal heartbeat, and lie; urine test for infection and protein; syphilis, hemoglobin, blood group, and rhesus (Rh) factor screening. The iron/folic acid supplementations, provision of insecticide-treated bed nets, tetanus toxoid vaccine, deworming, nutrition counseling, and birth preparedness are also recommended.4 Globally, only half of all pregnant women received a minimum of four recommended ANC visits. The WHO updated recommended minimum number of ANC contacts to eight to reduce perinatal deaths and improve women’s care experience.5,6
In low and middle-income countries (LMICs), 71% of neonatal mortality, 33% of stillbirths, and 54% of maternal mortality could be averted by increased coverage and quality of maternal health care.7 But, ANC quality lagged behind coverage (87%); only 54% received blood pressure screening, urine, and blood test.8 A retrospective study in Ethiopia showed only 53% received at least four components of the ANC.9 The Sustainable Development Goal 3 (SDG3) includes reducing the maternal mortality ratio to less than 70 per 100,000 live births, less than 12 newborn deaths per 1000 live births, and ensuring no baby is left behind by 2030, which addresses quality of care.10–13
Improving the content of care during ANC visits may foster ANC visit utilization and early initiation.14 A study indicated that perinatal mortality rate and newborn intensive care unit admission do not seem to decrease only by increasing the number of ANC visits.15 Previous studies have revealed that the effectiveness of ANC is critically affected by the number of ANC and the essential services covered during visits.16,17 Although these components were performed at higher rates; they were still not up to standard. A study based on a demographic health survey indicated that iron supplementation (80%), blood (83%), and urine (67%) sample collection were much more variable in health facilities across sub-Saharan Africa.18 Moreover, studies around the globe reported a low level of ANC content,19–21 and population-level coverage of ANC interventions had marked gaps that underscored the need to improve the quality of ANC services.18
The studies revealed that high socioeconomic status,9,20 education,9,22 parity,20,23 short distance to health facilities,9,22 living in urban areas,9,20,22 and certain administrative regions,20 planned pregnancies,20,24 media exposure,20,22 visiting skilled providers for ANC services,20 and visiting public or non-governmental organization (NGO) health facilities20 are associated with receiving the higher number of content of ANC. A study indicated providers were less likely to adhere to ANC guidelines when caring for a woman with a previous pregnancy complication.23 Further, staff shortage, lack of equipment, and consumables contributed to substandard ANC.25 The study indicates health workers failed to perform some required components stipulated in the focused ANC guideline which could not be always explained by the shortage of supplies.23 The healthcare quality given during ANC directly impacts women’s health and pregnancy outcomes.26
Moreover, studies at the sub-national and national levels focused on timing and number of ANC visits rather than ANC content and associated factors.27–35 Therefore, this study aimed to identify self-reported received ANC content and associated factors which may aid in designing guidelines and policies to improve maternal health, pregnancy outcomes, and child survival in Ethiopia.
Methods and Materials
Study Design, Area, and Period
The panel study design was employed in five regions and one city administration (Tigray, Afar, Amhara, Oromia, South Nation, Nationalities and People (SNNP), and Addis Ababa) in Ethiopia. The data were collected from October 2019 to September 2020.
The Data and Population
Addis Ababa University (AAU) and Johns Hopkins Bloomberg School of Public Health (JHBSPH) were launched a large-scale collaborative Performance Monitoring for Action (PMA Ethiopia) project in Ethiopia to generate timely data on reproductive, maternal, and newborn health (RMNH). Therefore, PMA Ethiopia was developed to provide national estimates of key RMNH indicators to identify gaps in RMNH care services through the panel study design.36
The study used weighted panel data from the PMA Ethiopia, which is a nationally representative sample. The survey covered 13,192 study respondents of which, 2855 women of reproductive age (15–49 years) were randomly selected for the panel study. In addition, women (household members or women who stay during their pregnancy or postpartum period at their parents’ home) who were pregnant or postpartum (less than eight weeks) and living in the panel’s region were also eligible for enrollment. Exclusion criteria included visitors to the household. Therefore, of those, 2855 women who were enrolled in the panel study, 1855 study participants who had at least one ANC visit were considered to analyze the received ANC content.
The questionnaire was adopted from the Demographic Health Survey (DHS) tool and previous PMA Ethiopia tool and reviewed literature.36 The data were collected using an Open Data Kit (ODK) installed on a smartphone by experienced (those who were participated in the DHS data collection or the PMA Ethiopia surveys since 2014 or the SNNP panel survey in 2016), and trained female resident enumerators (REs). PMA Ethiopia collected information on individual and community-level factors and contents of ANC services received. The data was collected during this study period twice. First, the REs interviewed eligible women who were enrolled during a baseline assessment. Second, these individuals/women were followed and interviewed between five and eight weeks postpartum.
Sample Size and Sampling Technique
The sample size was retrospectively computed, assuming a 17.1% proportion of received ANC content,24 5% alpha, 27.8% alternative proportion, with 1855 final sample size to ensure the inclusion of adequate subjects in the analysis; hence, the power of the sample was greater than 99%. First, a census of all households in the selected EAs with a complete listing was compiled. Second, the supervisors randomly selected women aged 15–49 years who were pregnant or recently postpartum. Finally, eligible candidates who were randomly selected were enrolled in the study from the census. In this analysis, researchers chose 1855 women with at least one ANC visit from a total of 2855 participants enrolled in the panel study at baseline.
Variables and Measurements
The outcome variable was the number of components of ANC utilized. In the PMA Ethiopia, data were available for the recommended parts of ANC services. The standard ANC guidelines in Ethiopia state that every pregnant woman should get ANC from a skilled provider, including blood pressure screening, weight measure, blood testing, stool exam, urine samples test, HIV testing, syphilis testing, tetanus vaccine, iron supplementation, deworming, nutrition counseling, and discussion about birth preparedness and complication readiness. To obtain information on these twelve items of ANC content, each participant was asked “As part of ANC during this pregnancy, were any of the items performed or discussed at least once (ie, Yes, No). Was weight measured? Was blood pressure measured? Was a blood sample taken? Was a urine sample taken? Was a stool sample taken? Were you tested for syphilis? Were you tested for HIV? Were iron tablets provided? Was a tetanus vaccine provided? Was deworming medication provided? Was nutrition discussed? Were birth preparedness and complication readiness discussed?”
For this study, for birth preparedness and pregnancy complication readiness, ‘Yes’ was recorded if the woman discussed three items (ie, place of delivery, delivery by a skilled attendant, arrangement for transport for delivery) with her skilled provider during any ANC visit(s). Otherwise, ‘No’ was recorded.37–40 Although the women may have utilized the ANC items several times during the pregnancy, the response of any action was registered as single action and each of the ANC components had equal weight. Based on the woman’s response, researchers created a composite index of ANC content received which included a simple count of the number of care components received by the women.20,23,41 A minimum value of zero indicates that the woman did not receive any items and a maximum value (12) shows she has utilized all items. Furthermore, we dichotomized the received ANC content as those who received greater than or equal to 75 percentiles as received adequate ANC content and less than as inadequate.42,43
The study also included individual-level factors like maternal age (15–19, 20–24, 25–29, 30–34, 35–39, 40–49), educational status (never attended, primary, secondary, technical or vocational, and higher), marital status (others or married), a partner has other wives or women (yes or no), ever been pregnant (yes or no), current pregnancy desired (then, later or not at all), birth events (primipara, multipara, grand-multipara), and partner encouraged you to attend ANC (yes or no). Additionally, community-level factors were included, such as place of residence (urban or rural), regions (Tigray, Afar, Amhara, Oromia, SNNP, Addis Ababa), wealth quartile (lowest, lower, middle, higher, highest), and structural quality of care for ANC (ie, availability of ANC guideline, ANC checklist, blood pressure apparatus, hemoglobin test, urine dipstick protein test, iron tablets, folic acid tablets, tetanus toxoid vaccine, and insecticide-treated bed net)44 as explanatory variables. This structural quality of ANC was determined based on counted items ranging from 0 to 10 as a continuous variable of interest.45
Data Analysis
The downloaded data from the ODK aggregate server daily were cleaned using STATA version 16.1. Descriptive statistics such as frequency tables and percentages were used to tabulate the essential characteristics of the study participants using STATA version 16.1 software. Bivariate analysis was computed using explanatory and outcome variables; those variables with p-value < 0.20 were considered in the multivariable analysis. The EAs used by the Central Statistical Agency (CSA) were employed to construct sample weights. Two weights in the panel (household and female) were used throughout the analysis to adjust for the clustering effect of the study’s sampling design, non-response, and restore the representativeness. Multi-collinearity between explanatory variables was checked using variance inflation factors (VIF) before fitting the models and the mean VIF was less than 5% among independent variables. An intra-cluster correlation coefficient (ICC) was computed before considering the multilevel model since ICC of 5% with a cluster size of 20 per cluster can lead to underestimating the actual precision of estimates (type I error).46 Furthermore, a multilevel mixed-effects count model was used to account for the hierarchical nature of the PMA Ethiopia data and observe factors associated with the number of components of ANC received during pregnancy.
The number of received ANC content is a count variable; therefore, the Poisson regression model with a log link function was employed as a point of reference.47 Since Poisson regression assumes an equal variance of the distribution to its mean, the investigators checked model fitness and run the inferential multivariable analysis of the predictors and outcome variable, ie, models one, two, and three for community-, individual- and both community- and individual-level factors, respectively. Finally, a model comparison of multilevel mixed-effects Poisson regression best fit (ie, model III) to the data was decided using Akaike’s Information Criterion (AIC) and Bayesian Information Criterion (BIC), and the lower value of AIC or BIC a better fit of the model.48 The incidence rate ratios (IRRs) with the corresponding 95% confidence interval were reported for each explanatory variable using a p-value less than 0.05 to declare the statistical significance.
Ethical Approval
Ethical approval was received from Addis Ababa University, College of Health Sciences (AAU/CHS) (Ref: AAUMF 01–008) and the Johns Hopkins University Bloomberg School of Public Health (JHSPH) Institutional Review Board (FWA00000287) by PMA Ethiopia.36 The data use policy of PMA Ethiopia frankly stated datasets are anonymized (ie, no result is published in which communities or individuals can be identified) before it is made publicly available for download via the www.pmadata.org website. The PMA Ethiopia review submitted requests and granted access to indicated datasets. The data is treated as confidential and it is forbidden to make any effort to identify individual, household, or enumeration areas in the survey and use the data for marketing and commercial ventures.
Results
From 13,192 surveyed participants, 2855 eligible women enrolled in the panel study were followed up at six weeks postpartum, 2665 were interviewed at six weeks (+2 weeks) postpartum making the response rate 93%. Of those, 1855 (64.6%) study participants had at least one ANC visit (these study participants analyzed the proportion of received ANC components and associated factors).
Characteristics of the Women
The mean age of the study participants was 27 (+6.2) years. According to this result, 589 (31.8%), 1355 (73.1%), and 685 (36.9%) study participants were aged 25–29 years, rural residents, and never attended school, respectively. Further, 795 (42.9%) study participants were Oromia region residents, and 1764 (95.2%) study participants were married women. The results also revealed most 1253 (84.2%) study participants were encouraged by their partners to go to a clinic for ANC visits (Table 1).
Table 1.
Frequency and Percentages of Characteristics of Child-Bearing Age Women in Ethiopia, 2020
| Variable (n=1855) | Frequency (%) | Frequency (%) |
|---|---|---|
| Un–Weighted | Weighted | |
| Maternal age | ||
| 15–19 | 165 (8.9) | 204 (10.9) |
| 20–24 | 475 (25.6) | 451 (24.3) |
| 25–29 | 615 (33.2) | 589 (31.8) |
| 30–34 | 333 (17.9) | 331 (17.8) |
| 35–49 | 267 (14.4) | 278 (15.0) |
| Residence | ||
| Urban | 850 (45.8) | 498 (26.9) |
| Rural | 1005 (54.2) | 1355 (73.1) |
| Region | ||
| Tigray | 379 (20.4) | 153 (8.3) |
| Afar | 54 (2.9) | 12 (0.6) |
| Amhara | 376 (20.3) | 450 (24.3) |
| Oromia | 467 (25.2) | 795 (42.9) |
| SNNP | 377 (20.3) | 365 (19.7) |
| Addis Ababa | 202 (10.9) | 79 (4.3) |
| Educational status | ||
| Never attended | 579 (31.2) | 685 (36.9) |
| Primary | 665 (35.9) | 735 (39.7) |
| Secondary | 347 (18.7) | 258 (13.9) |
| Technical, vocational, and higher | 264 (14.2) | 176 (9.5) |
| Marital status | ||
| Othersa | 128 (6.9) | 89 (4.8) |
| Married | 1727 (93.1) | 1764 (95.2) |
| Marriage history | ||
| Only once | 1592 (86.9) | 1582 (86.4) |
| More than once | 241 (13.2) | 249 (13.6) |
| Wealth quartile | ||
| Lowest | 253 (13.6) | 318 (17.2) |
| Lower | 220 (11.9) | 304 (16.4) |
| Middle | 275 (14.8) | 379 (20.4) |
| Higher | 348 (18.8) | 400 (21.6) |
| Highest | 759 (40.9) | 452 (24.4) |
| Current pregnancy desired | ||
| Then | 1055 (70.8) | 988 (66.3) |
| Later or not at all | 435 (29.2) | 501 (33.7) |
| Birth events | ||
| Primipara | 440 (23.7) | 390 (21.0) |
| Multipara | 1155 (62.3) | 1140 (61.5) |
| Grand multipara | 260 (14.0) | 323 (17.4) |
| Husband or partner has other wives or women | ||
| No | 1703 (94.4) | 1685 (93.4) |
| Yes | 102 (5.7) | 248 (6.6) |
| Ever been pregnant | ||
| No | 101 (5.4) | 91.6 (4.9) |
| Yes | 1754 (94.6) | 1761.4 (95.1) |
| Partner encouraged you to go to a clinic for ANC | ||
| No | 194 (13.0) | 236 (15.8) |
| Yes | 1296 (86.9) | 1253 (84.2) |
Note: aWidowed or divorced or separated or never married.
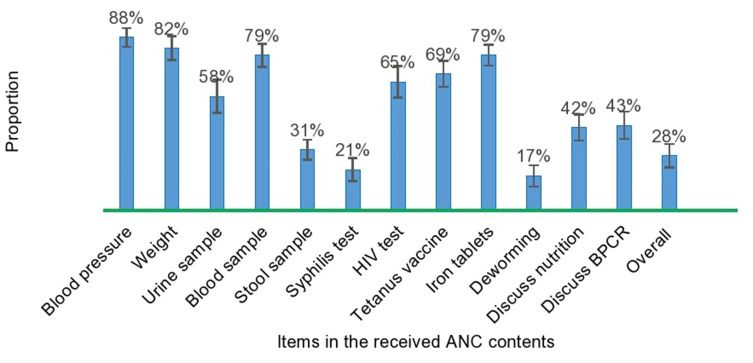
Women’s Received ANC Content
Among those who completed the panel study, 1855 (65%) pregnant or currently postpartum women had at least one ANC visit. From these, 1622 (88%) and 1520 (82%) received blood pressure screening and weight measurement at least once during ANC visits, respectively. Similarly, 1455 (79%) women’s blood and 1070 (58%) urine samples were taken at least once during ANC visits. In contrast, the proportion of women who were tested for syphilis, took deworming medication, received nutrition counseling, and discussed birth preparedness with their healthcare providers were 384 (21%), 324 (17%), 777 (42%), and 799 (43%), respectively. Furthermore, the study revealed that only one in four pregnant women received adequate ANC content (27.8%; 95% CI: 23.8%, 32.2%) (Figure 1).
Figure 1.
The proportion of received ANC contents among women of reproductive age in Ethiopia, 2020.
Abbreviations: ANC, antenatal care; BPCR, birth preparedness, and complication readiness; HIV, human-immune-virus.
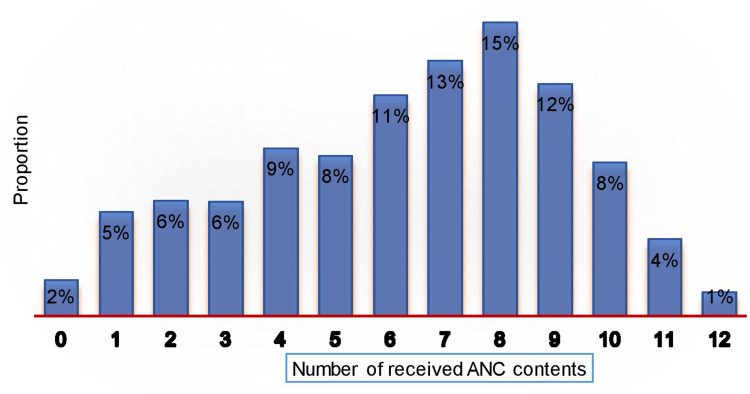
The number of received ANC content by pregnant or currently postpartum women ranged from zero to twelve items with a mean of 7.2 items, and a variance of 6.2 items (ie, over dispersion). The proportion of women who received zero and eight items was 18 (2%) and 302 (15%), respectively. However, only 26 (1%) of the pregnant or currently postpartum women received all the items in the guideline (Figure 2).
Figure 2.
Distribution of the number of ANC contents received by women of reproductive age in Ethiopia, 2020.
Factors Associated with Received ANC Content
The intraclass correlation coefficient in the empty model (null model) for received ANC content was 46% (95% CI: 38–54%). Hence, 46% of the total variance in received ANC content was attributable to differences across the clusters. The ICC in model I (community-level factors) revealed that 38% of the variation in the received ANC content among women was attributable to differences across the communities and an ICC in model II (individual-level factors) depicted that 42% (95% CI: 34–51%) of the variation in the received ANC content was attributable to differences across the clusters. Thus, about 38% (95% CI: 30–47%) of the received ANC content among the women in clusters was explained in the final model (Model III).
A women’s residence, administrative regions of dwelling, and wealth quintile showed significant association with ANC content received in model one. Similarly, maternal age, women’s educational status, and partner’s encouragement showed significant association in model two with received ANC content. Multivariable analysis of the final model revealed that rural residence, administrative regions of dwelling, maternal age, educational status, and partner’s encouragement to attend the clinic for ANC visit have a significant association with the number of received ANC content. Urban dwellers compared to rural (while holding the other variables constant in the model) were expected to have 1.09 times higher numbers of received ANC contents (IRR = 1.09, 95% CI: 1.01, 1.21). In addition, the region where women dwell was a significant predictor of the received ANC content score. Comparing to SNNP, women residing in Tigray (IRR = 1.18, 95% CI: 1.04, 1.34) and Amhara (IRR= 1.24, 95% CI: 1.09, 1.40) regions were more likely to receive more components of ANC.
In the same way, the incidence rate for women with the highest wealth quintile was 1.11 more likely to receive higher numbers of ANC content than women with the lowest wealth quintile (IRR= 1.11, 95% CI: 1.01, 1.23). Maternal age was a significant predictor of receiving ANC content. Hence, holding other variables constant, the incidence rate of women receiving higher numbers of ANC content increased for women whose age ranges from 20–24 (IRR = 1.10, 95% CI: 1.02, 1.19), 25–29 (IRR = 1.11, 95% CI: 1.02, 1.21), 30–34 (IRR = 1.15, 95% CI: 1.04, 1.27), and 35–49 (IRR= 1.13, 95% CI: 1.01, 1.27) compared to those from 15 to 19 years.
The educational status of the women was also a significant predictor who received higher ANC content scores. The incidence rate for a woman who was educated above secondary school was more likely to receive higher numbers of ANC content compared to women who never attended school (IRR = 1.08, 95% CI: 1.01, 1.16). The estimated rate ratio comparing women whose partner encouraged her to attend a clinic for ANC to her counterpart, given the other variables are held constant in the model, showed those were 1.14 times more likely to receive higher numbers of ANC content compared to their counterparts (IRR = 1.14, 95% CI: 1.05, 1.24) (Table 2).
Table 2.
Factors Associated with Received ANC Contents Among Child-Bearing Age Women in Ethiopia, 2020
| Variable (n=1855) | Model I | Model II | Model III (Final) |
|---|---|---|---|
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| Residence | |||
| Urban | 1.15 (1.04, 1.27) | 1.09 (1.01, 1.21)** | |
| Rural | 1.0 | 1.0 | |
| Region | |||
| Tigray | 1.19 (1.05, 1.34)** | 1.18 (1.04, 1.34)** | |
| Afar | 0.88 (0.60, 1.29) | 0.92 (0.63, 1.34) | |
| Amhara | 1.23 (1.08, 1.39)** | 1.24 (1.09, 1.40)** | |
| Oromia | 0.93 (0.81, 1.08) | 0.97 (0.85, 1.12) | |
| SNNP | 1.0 | 1.0 | |
| Addis Ababa | 1.12 (0.99, 1.25) | 1.10 (0.98, 1.24) | |
| Wealth quartile | |||
| Lowest | 1.0 | 1.0 | |
| Lower | 1.05 (0.97, 1.13) | 1.03 (0.94, 1.12) | |
| Middle | 1.03 (0.96, 1.11) | 1.01 (0.93, 1.09) | |
| Higher | 1.12 (1.03, 1.22)** | 1.08 (0.98, 1.18) | |
| Highest | 1.16 (1.05, 1.28)** | 1.11 (1.01, 1.23)** | |
| Structural quality of care for ANC | 0.99 (0.94, 1.04) | 0.99 (0.95, 1.05) | |
| Maternal age | |||
| 15–19 | 1.0 | 1.0 | |
| 20–24 | 1.12 (1.04, 1.22)** | 1.10 (1.02, 1.19)** | |
| 25–29 | 1.14 (1.04, 1.24)** | 1.11 (1.02, 1.21)** | |
| 30–34 | 1.18 (1.06, 1.30)** | 1.15 (1.04, 1.27)** | |
| 35–49 | 1.18 (1.05, 1.33)** | 1.13 (1.01, 1.27)** | |
| Educational status | |||
| Never attended | 1.0 | 1.0 | |
| Primary | 1.02 (0.97, 1.08) | 1.01 (0.95, 1.06) | |
| Secondary and above | 1.14 (1.06, 1.22)** | 1.08 (1.01, 1.16)** | |
| Marital status | |||
| Othersa | 1.0 | 1.0 | |
| Married | 0.97 (0.91, 1.02) | 0.97 (0.92, 1.02) | |
| Current pregnancy desired | |||
| Then | 1.01 (0.97, 1.06) | 1.01 (0.96, 1.05) | |
| Later or Not at all | 1.0 | 1.0 | |
| Birth events | |||
| Primipara | 1.09 (0.99, 1.19) | 1.05 (0.96, 1.14) | |
| Multipara | 1.04 (0.96, 1.12) | 1.01 (0.94, 1.09) | |
| Grand multipara | 1.0 | 1.0 | |
| Ever been pregnant | |||
| No | 1.0 | 1.0 | |
| Yes | 1.08 (0.97, 1.18) | 1.04 (0.94, 1.15) | |
| Partner encouraged you to go to a clinic for ANC | |||
| No | 1.0 | 1.0 | |
| Yes | 1.14 (1.06, 1.23)** | 1.14 (1.05, 1.24)** |
Notes: Model 0 – empty null model, baseline model without any explanatory variables; Model I– adjusted for only community-level factors; Model II – adjusted for only individual-level factors; Model III – adjusted for individual- and community-level factors (full model); aWidowed or divorced or separated or never married; 1.0, Reference; **Significant at p-value < 0.05.
Discussion
This study identified the prevalence of adequately received antenatal care components and associated factors among pregnant or recently postpartum women in Ethiopia. Hence, more than a quarter of the study participants received adequate components of ANC. Further, urban residents, older age, secondary and above formal school attendant women, and partner involvement in ANC decision-making were significant predictors of received ANC components in Ethiopia.
Our study revealed that the proportion of adequately received ANC contents was 28%. This result is in line with a study conducted in LMICs ranging from 10 to 50% in Jordan, Nigeria, Nepal, Colombia, and Haiti49 and studies in Bangladesh (22%),20 Zambia (29%),16 but lower than studies done in Ghana (48%),23 Myanmar (58%),41 Zambia (47.1%),50 and higher than studies in Nigeria (7%),22 twenty countries in sub-Saharan Africa (5%).51 The slow progress towards maternal and newborn survival due to ineffective care may be attributable to the gaps between globally recommended coverage indicators measuring contacts rather than the actual content.51 This implies that the received ANC content needs attention when designing and implementing policies and programs to ensure pregnant women receive adequate ANC components to improve maternal and newborn health.
In our study, rural women were less likely to receive higher recommended items in ANC content. Similarly, studies indicate that rural resident women were significantly less likely to have higher numbers of content items of ANC services.9,20,22,41 Rural women have substantially less or even absent transportation infrastructure which makes access to healthcare difficult and may contribute to the difference.52 The study also revealed long distances to health institutions and low media exposure among rural women contributed to inadequate received ANC components.22 Furthermore, health facilities in an urban setting are better endowed with resource allocations53 and might be due to the lower socio-economic condition, less accessibility, and limited healthcare services of rural women.20 There should be a concerted effort to improve accessibility, availability, and quality of ANC services among rural women and create awareness among key stakeholders for adequate received ANC components.
The region where women dwell was a significant predictor of higher numbers of received ANC components. The result is consistent with previous studies in Bangladesh where certain administrative regions associated with received ANC contents.20 Regions of dwelling are drivers of ANC service utilization54 indeed, influencing received ANC components. The variation in health-seeking behaviors, accessibility, and availability of quality services may explain the discrepancy of receiving ANC contents among the different geographical locations. Despite Ethiopia’s sustained efforts to enhance maternal and newborn health, wide regional disparities of received ANC components exist among women. Furthermore, a study is needed to identify factors responsible for this variation in Ethiopia.
The educational status of the women is also a significant predictor of the women who received ANC content. In the same way, previous studies showed that as education increases, number of received ANC content also increases.9,22,42,50,51,55 Relatively affordable and accessible health information for educated women compared to those who never attended schools may explain the associations.56 Furthermore, education fosters maternal healthcare awareness, appropriate need-based services utilization,17,20,57 household maternal decision-making ability,57 autonomy on their health,58 new values and attitudes that favor modern health care.59,60 These procedures might be expected and requested by educated women compared to those who never attended school.61 Hence, improving maternal education should be part of designing and implementing policies and programs for equitable progress to enhanced maternal newborn health.
An estimated rate ratio comparing women whose partner encouraged her to go to a clinic for ANC was more likely to receive more ANC contents. Similarly, women who have no problem getting permission from their partners were significantly more likely to have a higher number of items of contents of ANC service during their pregnancy.9 This might be due to awareness of access and use of services influenced by male’s participation in ANC,62 four or more ANC visits were significantly associated with male involvement in ANC63 and it impacted maternal health services uptake.64 A concerted effort is needed to improve received ANC components emphasizing partner involvement in ANC decision-making when designing and implementing policies and programs.
This study used weighted nationally representative data and employed multilevel regression which considers the clustering nature of the data. The analysis was performed on panel data which is less susceptible to bias. However, the study had some limitations, including social desirability and recall bias, since bias is inevitable as the information was self-reported. Additionally, there were women lost due to movement outside the study area, and after repeated follow-up visits, enumerators were still unable to locate the participants, resulting in loss of follow-up bias. In this analysis, discussion on nutrition, birth preparedness, and complication readiness was given equal weights with the other ANC components. However, these two crucial topics could not be standardized in terms of content, duration, and delivery mode of the information. Therefore, the participants were asked only whether these topics were covered or not. Furthermore, to display the broader picture and identify the barrier to ANC components received, further qualitative research including women, healthcare providers, and healthcare facilities is essential.
Conclusions
These study results indicate the number of women who received the recommended ANC content in Ethiopia was low. Thus, the country is still far from achieving universal coverage of recommended ANC content. The findings imply that increasing received ANC components depends on a woman’s regions of dwelling, place of residence, age, educational status, and partner’s involvement in decision-making about ANC visits. Further, this study highlights the importance of ensuring high received antenatal care content, which is crucial for reducing pregnancy-related morbidity and mortality. Thus, policies and programs aimed at increasing received ANC contents, ie, the major strategic initiative of the health-sector transformation plan to provide quality ANC services can be realized primarily through promoting female education, reducing regional inequalities, targeting older age and rural resident women, and encouraging partner involvement in decision-making about ANC.
Acknowledgments
We would like to thank PMA Ethiopia for providing us the data. Our sincere appreciation also goes to Tara Wilfong for her great cooperation to edit the grammar and comment the manuscript.
Abbreviations
ANC, antenatal care; AIC, Akaike’s information criterion; BIC, Bayesian information criterion; DHS, demographic health survey; IRR, incidence rate ratio; LMICs, low- and middle-income countries; PMA, performance monitoring for action; SD, standard deviation; SNNP, south nation, nationalities, and people; WHO, World Health Organization.
Data Sharing Statement
The data used for this research are available upon reasonable request from the PMA Ethiopia website.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Tunçalp Ӧ, Pena‐Rosas JP, Lawrie T, et al. WHO recommendations on antenatal care for a positive pregnancy experience—going beyond survival. BJOG. 2017;124(6):860–862. doi: 10.1111/1471-0528.14599 [DOI] [PubMed] [Google Scholar]
- 2.Wang W, Hong R. Levels and determinants of continuum of care for maternal and newborn health in Cambodia-evidence from a population-based survey. BMC Pregnancy Childbirth. 2015;15(1):62. doi: 10.1186/s12884-015-0497-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ataguba JE-O, Uthman O. A reassessment of global antenatal care coverage for improving maternal health using sub-Saharan Africa as a case study. PLoS One. 2018;13(10):e0204822. doi: 10.1371/journal.pone.0204822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Federal Ministry of Health Ethiopia. Antenatal Care Module: 13. Providing Focused Antenatal Care. Addis Ababa: Federal ministry of health, Ethiopia; 2008. [Google Scholar]
- 5.Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2015;(7):CD000934. doi: 10.1002/14651858.CD000934.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tunçalp Ӧ, Pena-Rosas JP, Lawrie T, et al. WHO recommendations on antenatal care for a positive pregnancy experience-going beyond survival. BJOG. 2017;124(6):860–862. [DOI] [PubMed] [Google Scholar]
- 7.Bhutta ZA, Das JK, Bahl R, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet. 2014;384(9940):347–370. doi: 10.1016/S0140-6736(14)60792-3 [DOI] [PubMed] [Google Scholar]
- 8.Arsenault C, Jordan K, Lee D, et al. Equity in antenatal care quality: an analysis of 91 national household surveys. Lancet Glob Health. 2018;6(11):e1186–e1195. doi: 10.1016/S2214-109X(18)30389-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Woldeamanuel B, Belachew T. Risk factors associated with frequency of antenatal visits, number of items of antenatal care contents received and timing of first antenatal care visits in Ethiopia: multilevel mixed-effects analysis. Res Square. 2020;1–37. doi: 10.21203/rs.3.rs-110214/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hug L, Alexander M, You D, Alkema L. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: a systematic analysis. Lancet Glob Health. 2019;7(6):e710–e720. doi: 10.1016/S2214-109X(19)30163-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Health in 2015: From MDGs, Millennium Development Goals to SDGs, Sustainable Development Goals. 20 Avenue Appia, 1211 Geneva 27, Switzerland: World Health Organization; 2015:924156511X. [Google Scholar]
- 12.World Health Organization. Every Newborn Action Plan: Progress Report, May 2015. 20 Avenue Appia, 1211 Geneva 27, Switzerland: World Health Organization; 2015:9241508728. [Google Scholar]
- 13.Koblinsky M, Moyer CA, Calvert C, et al. Quality maternity care for every woman, everywhere: a call to action. Lancet. 2016;388(10057):2307–2320. doi: 10.1016/S0140-6736(16)31333-2 [DOI] [PubMed] [Google Scholar]
- 14.Chama-Chiliba CM, Koch SF. Utilization of focused antenatal care in Zambia: examining individual- and community-level factors using a multilevel analysis. Health Policy Plan. 2015;30(1):78–87. doi: 10.1093/heapol/czt099 [DOI] [PubMed] [Google Scholar]
- 15.Manjavidze T, Rylander C, Skjeldestad FE, Kazakhashvili N, Anda EE, Wilunda C. The impact of antenatal care utilization on admissions to neonatal intensive care units and perinatal mortality in Georgia. PLoS One. 2020;15(12):e0242991. doi: 10.1371/journal.pone.0242991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kyei NN, Chansa C, Gabrysch S. Quality of antenatal care in Zambia: a national assessment. BMC Pregnancy Childbirth. 2012;12(1):151. doi: 10.1186/1471-2393-12-151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nwaru BI, Wu Z, Hemminki E. Determinants of the use of prenatal care in rural China: the role of care content. Matern Child Health J. 2012;16(1):235–241. doi: 10.1007/s10995-010-0734-0 [DOI] [PubMed] [Google Scholar]
- 18.Kanyangarara M, Munos MK, Walker N. Quality of antenatal care service provision in health facilities across sub-Saharan Africa: evidence from nationally representative health facility assessments. J Glob Health. 2017;7(2):021101. doi: 10.7189/jogh.07.021101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kassaw A, Debie A, Geberu DM. Quality of prenatal care and associated factors among pregnant women at public health facilities of Wogera District, Northwest Ethiopia. J Pregnancy. 2020;2020:9592124. doi: 10.1155/2020/9592124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Islam MM, Masud MS, Akinyemi AI. Determinants of frequency and contents of antenatal care visits in Bangladesh: assessing the extent of compliance with the WHO recommendations. PLoS One. 2018;13(9):e0204752. doi: 10.1371/journal.pone.0204752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Afulani PA, Buback L, Essandoh F, Kinyua J, Kirumbi L, Cohen CR. Quality of antenatal care and associated factors in a rural county in Kenya: an assessment of service provision and experience dimensions. BMC Health Serv Res. 2019;19(1):684. doi: 10.1186/s12913-019-4476-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agho KE, Ezeh OK, Ogbo FA, Enoma AI, Raynes-Greenow C. Factors associated with inadequate receipt of components and use of antenatal care services in Nigeria: a population-based study. Int Health. 2018;10(3):172–181. doi: 10.1093/inthealth/ihy011 [DOI] [PubMed] [Google Scholar]
- 23.Amoakoh-Coleman M, Agyepong IA, Zuithoff NP, et al. Client factors affect provider adherence to clinical guidelines during first antenatal care. PLoS One. 2016;11(6):e0157542. doi: 10.1371/journal.pone.0157542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haile D, Habte A, Bogale B. Determinants of frequency and content of antenatal care in postnatal mothers in Arba Minch Zuria District, SNNPR, Ethiopia, 2019. Int J Womens Health. 2020;12:953–964. doi: 10.2147/IJWH.S261705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nyamtema AS, Jong AB-D, Urassa DP, Hagen JP, van Roosmalen J. The quality of antenatal care in rural Tanzania: what is behind the number of visits? BMC Pregnancy Childbirth. 2012;12(1):70. doi: 10.1186/1471-2393-12-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ekabua J, Ekabua K, Njoku C. Proposed framework for making focused antenatal care services accessible: a review of the Nigerian setting. ISRN Obstet Gynecol. 2011;2011:253964. doi: 10.5402/2011/253964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ewunetie AA, Munea AM, Meselu BT, Simeneh MM, Meteku BT. DELAY on first antenatal care visit and its associated factors among pregnant women in public health facilities of Debre Markos town, North West Ethiopia. BMC Pregnancy Childbirth. 2018;18(1):1–8. doi: 10.1186/s12884-018-1748-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Basha GW. Factors affecting the utilization of a minimum of four antenatal care services in Ethiopia. Obstet Gynecol Int. 2019;2019:5036783. doi: 10.1155/2019/5036783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tiruaynet K, Muchie KF. Determinants of utilization of antenatal care services in Benishangul Gumuz Region, Western Ethiopia: a study based on demographic and health survey. BMC Pregnancy Childbirth. 2019;19(1):115. doi: 10.1186/s12884-019-2259-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gidey G, Hailu B, Nigus K, Hailu T, Gerensea H, Gerensea H. Timing of first focused antenatal care booking and associated factors among pregnant mothers who attend antenatal care in Central Zone, Tigray, Ethiopia. BMC Res Notes. 2017;10(1):608. doi: 10.1186/s13104-017-2938-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yaya S, Bishwajit G, Ekholuenetale M, Shah V, Kadio B, Udenigwe O. Timing and adequate attendance of antenatal care visits among women in Ethiopia. PLoS One. 2017;12(9):e0184934. doi: 10.1371/journal.pone.0184934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weldemariam S, Damte A, Endris K, et al. Late antenatal care initiation: the case of public health centers in Ethiopia. BMC Res Notes. 2018;11(1):562. doi: 10.1186/s13104-018-3653-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wolde HF, Tsegaye AT, Sisay MM. Late initiation of antenatal care and associated factors among pregnant women in Addis Zemen primary hospital, South Gondar, Ethiopia. Reprod Health. 2019;16(1):73. doi: 10.1186/s12978-019-0745-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teshale AB, Tesema GA, Amo-Adjei J. Prevalence and associated factors of delayed first antenatal care booking among reproductive age women in Ethiopia; a multilevel analysis of EDHS 2016 data. PLoS One. 2020;15(7):e0235538. doi: 10.1371/journal.pone.0235538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tola W, Negash E, Sileshi T, Wakgari N, Salinas-Miranda A. Late initiation of antenatal care and associated factors among pregnant women attending antenatal clinic of Ilu Ababor Zone, southwest Ethiopia: a cross-sectional study. PLoS One. 2021;16(1):e0246230. doi: 10.1371/journal.pone.0246230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zimmerman L, Desta S, Yihdego M, et al. Protocol for PMA-Ethiopia: a new data source for cross-sectional and longitudinal data of reproductive, maternal, and newborn health. Gates Open Res. 2020;4(126):126. doi: 10.12688/gatesopenres.13161.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pervin J, Nu UT, Rahman AMQ, et al. Level and determinants of birth preparedness and complication readiness among pregnant women: a cross sectional study in a rural area in Bangladesh. PLoS One. 2018;13(12):e0209076. doi: 10.1371/journal.pone.0209076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Orwa J, Gatimu SM, Mantel M, et al. Birth preparedness and complication readiness among women of reproductive age in Kenya and Tanzania: a community-based cross-sectional survey. BMC Pregnancy Childbirth. 2020;20(1):636. doi: 10.1186/s12884-020-03329-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gebreyesus H, Berhe T, Teweldemedhin M. Birth preparedness as a precursor to reduce maternal morbidity and mortality among pregnant mothers in Medebay Zana District, Northern Ethiopia. BMC Res Notes. 2019;12(1):1–6. doi: 10.1186/s13104-019-4331-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smeele P, Kalisa R, van Elteren M, van Roosmalen J, van den Akker T. Birth preparedness and complication readiness among pregnant women admitted in a rural hospital in Rwanda. BMC Pregnancy Childbirth. 2018;18(1):1–7. doi: 10.1186/s12884-018-1818-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mugo NS, Mya KS, Raynes-Greenow C. Country compliance with WHO-recommended antenatal care guidelines: equity analysis of the 2015–2016 Demography and Health Survey in Myanmar. BMJ Glob Health. 2020;5(12):e002169. doi: 10.1136/bmjgh-2019-002169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Adhikari M, Chalise B, Bista B, Pandey AR, Upadhyaya DP. Sociodemographic correlates of antenatal care visits in Nepal: results from Nepal Demographic and Health Survey 2016. BMC Pregnancy Childbirth. 2020;20(1):513. doi: 10.1186/s12884-020-03218-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tafere TE, Afework MF, Yalew AW. Providers adherence to essential contents of antenatal care services increases birth weight in Bahir Dar City Administration, north West Ethiopia: a prospective follow up study. Reprod Health. 2018;15(1):163. doi: 10.1186/s12978-018-0610-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.World Health Organization. Service Availability and Readiness Assessment (SARA): An Annual Monitoring System for Service Delivery: Reference Manual. 20 Avenue Appia, 1211 Geneva 27, Switzerland: World Health Organization; 2013. [Google Scholar]
- 45.Defar A, Getachew T, Taye G, et al. Quality antenatal care services delivery at health facilities of Ethiopia, assessment of the structure/input of care setting. BMC Health Serv Res. 2020;20:1–9. doi: 10.1186/s12913-020-05372-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lovell DP, Omori T. Statistical issues in the use of the comet assay. Mutagenesis. 2008;23(3):171–182. doi: 10.1093/mutage/gen015 [DOI] [PubMed] [Google Scholar]
- 47.McCullagh P, Nelder JA. Generalized Linear Models. 2nd ed. London, UK: Chapman And Hall; 1989. [Google Scholar]
- 48.Spiegelhalter D, Best NG, Carlin BP, van der Linde A. Bayesian measures of model complexity and fit. Qual Control Appl Statist. 2003;48(4):431–432. [Google Scholar]
- 49.Benova L, Tunçalp Ö, Moran AC, Campbell OMR. Not just a number: examining coverage and content of antenatal care in low-income and middle-income countries. BMJ Glob Health. 2018;3(2):e000779. doi: 10.1136/bmjgh-2018-000779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Katemba BM, Bwembya P, Hamoonga TE, Chola M, Jacobs C. Demand side factors associated with quality antenatal care services: a case study of Lusaka District, Zambia. Front Public Health. 2018;6(285):285. doi: 10.3389/fpubh.2018.00285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Carvajal-Aguirre L, Amouzou A, Mehra V, Ziqi M, Zaka N, Newby H. Gap between contact and content in maternal and newborn care: an analysis of data from 20 countries in sub-Saharan Africa. J Glob Health. 2017;7(2):020501. doi: 10.7189/jogh.07.020501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Teijlingen E, Simkhada P, Stephens J, Simkhada B, Rogers S, Sharma S. Making the best use of all resources: developing a health promotion intervention in rural Nepal. Health Renaissance. 2012;10(3):229–235. doi: 10.3126/hren.v10i3.7141 [DOI] [Google Scholar]
- 53.Malawi Ministry of Health. Road Map for Accelerating the Reduction of Maternal and Neonatal Mortality and Morbidity in Malawi. Ministry of Health; 2007. [Google Scholar]
- 54.Tegegne TK, Chojenta C, Getachew T, Smith R, Loxton D. Antenatal care use in Ethiopia: a spatial and multilevel analysis. BMC Pregnancy Childbirth. 2019;19(1):399. doi: 10.1186/s12884-019-2550-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Khan REA, Ahmad TI, Noreen S, Ejaz A. Factors associated with the quality of Antenatal Care (ANC) services use in Bahawalpur. J Pak Med Assoc. 2020;70:1–8. [DOI] [PubMed] [Google Scholar]
- 56.Neupane S, Doku DT. Determinants of time of start of prenatal care and number of prenatal care visits during pregnancy among Nepalese women. J Community Health. 2012;37(4):865–873. doi: 10.1007/s10900-011-9521-0 [DOI] [PubMed] [Google Scholar]
- 57.Matsumura M, Gubhaju B. Women’s status, household structure and the utilization of maternal. Asia Pacific Popul J. 2001;16(1):23–44. doi: 10.18356/e8a4c9ed-en [DOI] [Google Scholar]
- 58.AbouZahr C, Wardlaw T. Antenatal care in developing countries: promises, achievements and missed opportunities-an analysis of trends, levels and differentials, 1990–2001. In: Antenatal Care in Developing Countries: Promises, Achievements and Missed Opportunities-An Analysis of Trends, Levels and Differentials, 1990–2001. World Health Organization; 2003:32. [Google Scholar]
- 59.Furuta M, Salway S. Women’s position within the household as a determinant of maternal health care use in Nepal. Int Fam Plan Perspect. 2006;32:17–27. doi: 10.1363/3201706 [DOI] [PubMed] [Google Scholar]
- 60.Sharma SK, Sawangdee Y, Sirirassamee B. Access to health: women’s status and utilization of maternal health services in Nepal. J Biosoc Sci. 2007;39(5):671–692. doi: 10.1017/S0021932007001952 [DOI] [PubMed] [Google Scholar]
- 61.Babalola S. Women’s education level, antenatal visits and the quality of skilled antenatal care: a study of three African countries. J Health Care Poor Underserved. 2014;25(1):161–179. doi: 10.1353/hpu.2014.0049 [DOI] [PubMed] [Google Scholar]
- 62.Muloongo H, Sitali D, Zulu JM, Hazemba AN, Mweemba O. Men’s perspectives on male participation in antenatal care with their pregnant wives: a case of a military hospital in Lusaka, Zambia. BMC Health Serv Res. 2019;19(1):463. doi: 10.1186/s12913-019-4294-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Natai CC, Gervas N, Sikira FM, et al. Association between male involvement during antenatal care and use of maternal health services in Mwanza City, Northwestern Tanzania: a cross-sectional study. BMJ Open. 2020;10(9):e036211. doi: 10.1136/bmjopen-2019-036211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Suandi D, Williams P, Bhattacharya S. Does involving male partners in antenatal care improve healthcare utilisation? Systematic review and meta-analysis of the published literature from low- and middle-income countries. Int Health. 2020;12(5):484–498. doi: 10.1093/inthealth/ihz073 [DOI] [PubMed] [Google Scholar]